Abstract
Objectives To evaluate the impact of Mexico's conditional cash transfer programme on the quality of health care received by poor women. Quality is measured by maternal reports of prenatal care procedures received that correspond with clinical guidelines.
Methods The data describe retrospective reports of care received from 892 women in poor rural communities in seven Mexican states. The women were participating in an effectiveness study and randomly assigned to incorporation into the programme in 1998 or 1999. Eligible women accepted cash transfers conditional on obtaining health care and nutritional supplements, and participated in health education sessions.
Results Oportunidades beneficiaries received 12.2% more prenatal procedures compared with non-beneficiaries (adjusted mean 78.9, 95% Confidence Interval (CI): 77.5–80.3; P < 0.001).
Conclusion The Oportunidades conditional cash transfer programme is associated with better quality of prenatal care for low-income, rural women in Mexico. This result is probably a manifestation of the programme's empowerment goal, by encouraging beneficiaries to be informed and active health consumers.
Keywords: Economics, quality, Mexico, prenatal care, evaluation
KEY MESSAGES.
A growing body of evidence points to the importance of health care quality as a policy priority in low- and middle-income developed settings.
Most quality improvement interventions focus on in-service training and supply-side improvements. Few interventions consider the role of households, consumers or patients in improving the quality of care.
Being a beneficiary of a large-scale conditional cash transfer programme is associated with the receipt of more prenatal care procedures among low-income, rural women in Mexico.
Higher quality received among beneficiaries of the conditional cash transfer programme is probably attributable to the programme's effect in encouraging informed and active health consumers.
Background
Improving care quality has become an important policy priority in low- and middle-income nations. A growing body of evidence suggests that inadequate, inappropriate or harmful care is widespread (Chabilkuli et al. 2002; Chakraborty and Frick 2002; World Health Organization 2003; Obua et al. 2004; Zurovac et al. 2004; Tuan et al. 2005). Poor quality and unnecessary care have also contributed to increased morbidity and mortality among children and adults (Schofield and Ashworth 1997; Nolan et al. 2001; Barros et al. 2005). Most quality improvement initiatives in low-income settings focus on supply-side interventions, such as in-service training; supervision, audit and feedback; and upgrading equipment and supplies. Although widely assumed to be effective, evaluations of in-service training programmes have demonstrated mixed effects on health provider performance (Rowe et al. 2005). Supervision, audit and feedback have had moderate to large effects on health worker performance over the short-term, but the impact over the long-term is less clear (Siddiqi et al. 2005). While supplies and equipment could be a precondition for health care delivery, they do not ensure adherence to clinical guidelines or reduce practice variation.
Consumers and patients play a role in quality improvement initiatives. Evaluations of the Integrated Management of Childhood Illnesses (IMCI) programme demonstrated that supply-side strengthening has a limited effect on health where consumer demand for services is weak (Pariyo et al. 2005). Patient preferences that conflict with technical standards could also reduce the impact of interventions on quality and health outcomes (Berman 2000). US-based studies have shown that cash, vouchers or gifts are effective in encouraging patients to obtain health services or to continue treatment (Giuffrida and Torgerson 1997). In low- and middle-income settings, there is some evidence that financial incentives to individuals or households have improved health seeking behaviours (Ensor 2004). Conditional cash transfer programmes to poor households in Latin America have demonstrated increases in utilization and health status (LaGuarde et al. 2007). In addition, vouchers for reproductive health services have resulted in higher perceptions of quality and satisfaction among poor adolescents (Meuwissen 2006). It is assumed that financial incentives result in higher quality because people are encouraged to be more active consumers of health care. Although research has documented the impact of financial incentives for physicians on practice variation (Chaix-Couturier et al. 2000), there is little evidence about the relationships between household or individual financial incentives and the technical quality of care received.
This study examines the impact of a demand-side intervention to reduce poverty in Mexico. The intervention is embedded in a large-scale conditional cash transfer (CCT) programme that aimed, in part, to improve birth outcomes through better maternal nutrition and use of prenatal care. The programme (originally called PROGRESA and now called Oportunidades) uses money as an incentive for parents to invest in their children's health and education, thereby enabling their children to have the capability to escape poverty when they reach adulthood. To improve birth outcomes, Oportunidades’ cash transfers to beneficiary households are conditioned, in part, on women completing a prescribed prenatal care plan and attending an educational programme. A key component of the educational programme is empowering women to obtain quality care by providing them with information about care content, encouraging them to speak up for their rights with medical care providers, and giving the cash transfers directly to women.
Across diverse settings, CCTs have been successful in improving the use of health services as well as reducing child mortality, morbidity, anaemia and stunting (Bautista et al. 2004; Gertler 2004; Maluccio and Flores 2004; Morris et al. 2004; Rivera et al. 2004). However, none of these studies tries to sort out the specific pathways by which CCT programmes are effective. This study follows-on from previous research that demonstrated lower rates of infant mortality and better birth outcomes among beneficiaries (Barham 2005; Barber and Gertler 2008a). We hypothesize that one possible pathway for these health improvements is through higher quality care for beneficiaries. This study evaluates whether beneficiary women reported higher levels of health care procedures received that correspond with clinical guidelines.
Methods
The programme
In 1997, Mexico established Oportunidades (originally called PROGRESA), a poverty-reduction programme to break the intergenerational transmission of poverty by providing incentives for parents to invest in the human capital of children. Cash transfers from Oportunidades are conditional on family members obtaining health and education services. A unique feature of the programme was the deliberate decision to give the cash transfers directly to the mother or female head of household (Adato et al. 2000b). Programme beneficiaries were phased-in based on federal resource availability, which in turn allowed for an ethical evaluation of programme effectiveness. During its first 3 years, the programme succeeded in covering almost all eligible families living in rural areas. Coverage expanded from some 300 000 rural families in 1997 to approximately 2.6 million in 2000. Currently, the programme covers approximately 5 million low-income families (more than 20% of all families in Mexico) living in both urban and rural areas (Ministry of Social Development 2008). The programme has been described previously in detail; in this paper, we present the elements that are important to this study for eligibility and programme administration in rural areas.
The rural programme established eligibility in two stages: the programme first identified marginalized communities, and then identified low-income households within those communities (Skoufias et al. 1999). Once enrolled, households received benefits for a minimum of 3 years conditional on meeting programme requirements. To prevent migration into treatment communities, new households were unable to enrol until the next certification period. Participating households receive cash transfers for health and education. The monthly health stipend is conditional on each family member obtaining regular clinic consultations, and attending pláticas (health education talks) and monthly meetings for the principal beneficiary, usually the mother in the household. Oportunidades required that households prove compliance via certification at public clinics and schools; about 1% of households were denied the cash transfer due to non-compliance (Adato et al. 2000a). The health transfer is fixed at approximately US$15 per household per month (Ministry of Social Development 2003). The education transfer is based on school grade and sex. The maximum monthly benefit cap for health and education together equals approximately US$90 and US$160 for families with primary and high school children, respectively (Parker and Teruel 2005). Total transfers for health and education average 17 to 20% of pre-programme rural per capita household consumption (Gertler et al. 2004).
The Oportunidades’ health requirements are extensive and vary primarily by age. Specifically for pregnant women, five prenatal visits are required, with an emphasis on monitoring the pregnancy's progression; and the prevention, detection and control of obstetric and perinatal risk factors. In addition to obtaining health care, nutritional supplements are required for pregnant and lactating women.
Oportunidades also mandates attendance at monthly educational and programmatic meetings. Participating adults are required to attend monthly pláticas, which emphasize prevention and reduction of health risks. Specific to this analysis, pregnant women are required to attend meetings about what to expect from prenatal care consultations, the clinical content of this care, maternal nutrition and other reproductive health information. Monthly meetings also take place between beneficiary women and promotoras, or elected beneficiary representatives, to ensure that the programme's objectives and requirements are understood. Promotoras receive training about how the programme operates, answer questions and complete monitoring forms. In health, they also carry out patient appointment reminders and act as a communication link between the health centres and the communities. A key objective of both the educational sessions and the meetings with the promotoras is encouraging beneficiary women to be proactive in obtaining their right to social services (Adato et al. 2000b).
Design and data sources
The Government of Mexico commissioned an independent evaluation of the overall programme impact on education, health, nutrition and poverty. Planned as a randomized intervention, the study was conducted in seven central states (Guerrero, Hidalgo, Michoacán, Puebla, Querétaro, San Luis Potosí and Veracruz) representing the largest programme area. The evaluation was based on a sample of 506 communities in these seven states, which were among the first to receive programme benefits (Berhman and Todd 1999). The 506 treatment communities were randomly selected using probabilities proportionate to the size of communities, from 6400 communities scheduled for the second and third waves of incorporation into the programme. Of the 506 experimental communities, 306 were randomly assigned to the treatment group to be incorporated in the second wave and the remaining to the control group to be incorporated in the third wave. The eligible households in treatment communities were scheduled to receive benefits starting in April 1998, and control communities started to receive benefits in December of 1999.
A fertility survey was fielded in 2003 to evaluate the programme's impact on reproductive health outcomes, using a sub-set of the original communities. The survey used a two-stage stratified sampling design. Communities were randomly selected based on a probability sample proportionate to the number of women of reproductive age. Within each community, a predetermined number of households was randomly selected based on the average number of women of reproductive age. All eligible women were interviewed in selected households. Written consent for participation was obtained from the mother or household head. The project was approved by the Human Subjects and Ethics Committee of the National Institute of Public Health, Mexico. Among women identified as respondents, 74% fully completed interviews. The most common reason cited for incompletion was not at home (5.1%); 1.8% refused to be interviewed.
The sample in these analyses includes women who were eligible for Oportunidades, experienced a singleton live birth between 1997 and 2003, received prenatal care and reported about these procedures, and lived in the original treatment or control communities. In addition, we omitted women who were pregnant at the time of the survey because they did not receive a full course of care. The final sample size is 892 women (180 non-beneficiary and 712 beneficiary births).
Measurement of variables
Quality is measured from maternal reports of prenatal procedures received that correspond with national guidelines (Ministry of Health 1993). Reports about health care procedures received have been used in previous studies to represent quality (Kogan et al. 1994; Barber et al. 2007). The survey collected data about 13 services conducted by health care providers as a part of routine prenatal care. These services can be divided into three domains: history-taking and diagnostics (took blood sample, took a urine sample, asked about bleeding, asked about discharge); physical examination (took blood pressure, weighed the mother, measured her uterine height, conducted a pelvic exam); and prevention and case management (administered tetanus toxoid, provided iron supplements, provided advice about family planning, provided advice about lactation, and recorded appointment information). Omitted are questions relating to the nutritional supplements, which are not universally indicated in the prenatal protocol. The responses were summed up, and the quality scores represent the proportion of the total.
Programme participation is measured using information from two sources: the fertility module detailing the date of birth, and administrative records about the date in which the first cash transfer was received. A beneficiary birth is defined as a birth that occurred after the household received their first cash transfer. Non-beneficiary births are births that occurred among eligible women but before they started to receive cash transfers. Because the actual date of incorporation into the programme was random, beneficiary status is not determined by household decision-making (Gertler et al. 2004). In addition, a previous study found no relationships between the programme and fertility decisions (Steklov et al. 2006).
From the fertility module, we also collected information about maternal characteristics and prior birth outcomes. Household and community socio-economic baseline characteristics are collected from the 1997 census, which provides data prior to intervention. From census data, information included household education, age and demographics of household members, information about large assets, and community characteristics, including infrastructure and distance to capital.
The analyses
The dependent variables are the summary quality scores and the scores for three separate domains of history-taking and diagnostics, physical examination, and prevention. Regressions are estimated using a set of covariates to reduce idiosyncratic variation and improve the power of the estimates. Specifically, all regressions include the following independent variables: maternal age, the number of prior pregnancies, and prior miscarriage or abortion, educational level and age of the head of household, maternal educational level, household size, the proportion of male and female family members aged 0 to 5 and 6 to 17 years, a household assets index (the proportion with ownership of land, home ownership, refrigerator, gas heater, television, internal water in household, and electricity in household), altitude, distance to the capital city and whether there was a health centre in the community. Variables were squared if the relationships were non-linear.
The adjusted means for the quality scores and each of the three domains are generated using community fixed-effects regressions. Multivariate regression models are used to predict the quality score while holding constant at their mean values the individual, household and community characteristics. The main results report the adjusted mean procedures received. The models take into account intra-cluster correlation because the interventions were randomized at the community level. Statistical analyses were done using STATA (release Stata 9.2, Stata Corp, College Station, Texas). Statistical significance was declared at conventional levels.
Results
Table 1 compares the maternal and infant characteristics, and baseline demographics and socio-economics between non-beneficiary and beneficiary births. The sampling strategy resulted in a well-balanced sample for analyses. One significant difference is noted. Non-beneficiaries had a higher number of prior pregnancies (5.3 compared with 4.7 among beneficiaries).
Table 1.
Descriptive statistics
| Variables | Non-beneficiary (mean, standard deviation)a | Beneficiary (mean, standard deviation)a | Difference | P-value |
|---|---|---|---|---|
| Baseline household socio-economics and demographics | ||||
| Household assets index (0-1)b | 0.42 (0.18) | 0.40 (0.17) | −0.02 | 0.266 |
| Indigenous-speaking household (%) | 30.73 | 38.29 | 7.56 | 0.088 |
| Educational level of household head (yrs) | 3.63 (2.68) | 3.53 (2.59) | −0.10 | 0.716 |
| Age of household head (yrs) | 41.31 (8.77) | 40.07 (9.79) | −1.24 | 0.134 |
| Maternal educational level (yrs) | 4.01 (2.62) | 3.95 (2.77) | −0.06 | 0.809 |
| Household size | 6.56 (2.26) | 6.41 (2.35) | −0.15 | 0.495 |
| Males, 0–5 years in household (%) | 15.30 | 14.10 | −1.20 | 0.237 |
| Females, 0–5 years in household (%) | 15.37 | 14.60 | −0.77 | 0.522 |
| Males, 6–17 years in household (%) | 14.47 | 15.29 | 0.82 | 0.522 |
| Females, 6–17 years in household (%) | 15.83 | 13.95 | −1.88 | 0.135 |
| Maternal and infant characteristics | ||||
| Maternal age (yrs) | 30.00 (6.37) | 29.58 (6.70) | −0.42 | 0.437 |
| Total prior pregnancies | 5.27 (2.55) | 4.73 (2.60) | −0.53 | 0.011 |
| Prior miscarriage or abortion (%) | 7.22 | 6.18 | −1.04 | 0.600 |
| Baseline community characteristics | ||||
| Distance to urban centre (km) | 109.94 (43.78) | 112.30 (43.28) | 2.37 | 0.590 |
| Health centre in community (%) | 78.40 | 81.18 | 2.78 | 0.642 |
| Female wages, formal employment (pesos per month) | 141.27 (482.27) | 155.90 (532.51) | 14.63 | 0.666 |
| Male wages, formal employment (pesos per month) | 262.14 (1256.98) | 258.21 (1118.93) | −3.94 | 0.939 |
| No. with data | 180 | 712 |
Notes:
aUnless otherwise indicated.
bIncludes land ownership, home ownership, internal water source, electricity, and ownership of a refrigerator, television and heater.
Table 2 reports the frequencies for each of the criterion used in the quality index. Beneficiaries reported higher percentages for all of the criteria. Those significantly different at the 5% level include a urine sample, blood pressure and information about the appointment recorded. The summary quality scores and those for each of the three domains (history taking, physical and prevention) are significantly different between the two groups. The summary quality score for beneficiaries (78.4%) is significantly higher than that for non-beneficiaries (72.4%, P < 0.01).
Table 2.
Defining quality: the percentage of prenatal care procedures received by beneficiary status
| Non-beneficiary | Beneficiary | Average | Difference | P-value | |
|---|---|---|---|---|---|
| Panel A. Prenatal procedures and quality scores | |||||
| History-taking and diagnostics (mean) | 54.72 | 62.82 | 61.18 | 8.09 | <0.01 |
| Standard deviation (SD) | [32.98] | [32.10] | [32.42] | ||
| Asked about bleeding | 71.11 | 75.84 | 74.89 | 4.73 | 0.21 |
| Asked about discharge | 71.67 | 77.11 | 76.01 | 5.44 | 0.16 |
| Blood sample taken | 41.11 | 49.02 | 47.42 | 7.91 | 0.10 |
| Urine sample taken | 35.00 | 49.30 | 46.41 | 14.30 | <0.01 |
| Physical examination (mean) | 76.25 | 82.13 | 80.94 | 5.88 | <0.01 |
| Standard deviation (SD) | [28.00] | [21.69] | [23.20] | ||
| Blood pressure taken | 85.00 | 94.10 | 92.26 | 9.10 | <0.01 |
| Weighed | 92.22 | 95.08 | 94.51 | 2.86 | 0.15 |
| Uterine height measured | 82.78 | 88.34 | 87.22 | 5.56 | 0.06 |
| Pelvic exam | 45.00 | 50.98 | 49.78 | 5.98 | 0.16 |
| Prevention and case management | 83.56 | 87.87 | 87.00 | 4.31 | 0.05 |
| Standard deviation (SD) | [26.50] | [21.48] | [22.63] | ||
| Tetanus toxoid immunization | 89.44 | 93.12 | 92.38 | 3.68 | 0.11 |
| Iron supplements | 80.56 | 85.81 | 84.75 | 5.25 | 0.11 |
| Advised about lactation | 90.00 | 91.01 | 90.81 | 1.01 | 0.67 |
| Advised about family planning methods | 85.56 | 88.34 | 87.78 | 2.78 | 0.31 |
| Recorded appointments | 72.22 | 81.04 | 79.26 | 8.82 | 0.01 |
| Summary quality scores | 72.44 | 78.39 | 77.19 | 5.96 | <0.01 |
| Standard deviation (SD) | [25.17] | [20.14] | [21.37] |
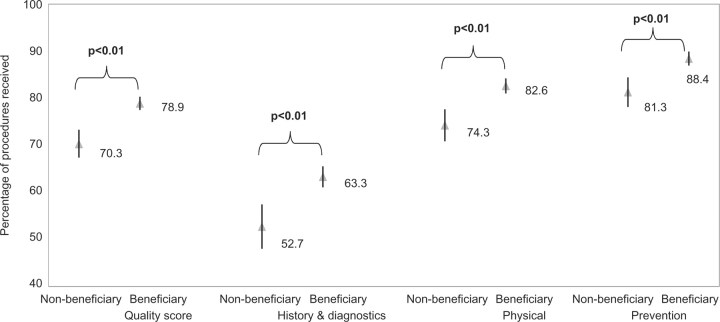
Figure 1 reports the adjusted mean quality scores overall and for each domain. For the adjusted quality scores overall, beneficiaries received 12.2% more procedures compared with non-beneficiaries (P < 0.01). The results are consistent for each of the three domains. Beneficiaries received 20.1% more procedures for history-taking and diagnostics, 11.3% more for physical examination, and 8.8% more for prevention and case management (all P < 0.01). It is notable that the quality scores for beneficiaries have much narrower confidence intervals compared with those for non-beneficiaries.
Figure 1.
Adjusted mean quality received and 95% Confidence Intervals (C.I.) for non-beneficiary and beneficiary births.
Discussion, limitations and conclusions
This study uses data from an evaluation of Mexico's conditional cash transfer programme to examine the programme's impact on quality of care. We find that beneficiaries received 12.2% additional prenatal procedures. There could be a number of different explanations for these findings. Beneficiaries could have received higher quality as a result of the programme's compliance requirements to obtain a certain number of visits or to obtain health care from the public sector. Alternatively, beneficiaries could have used the additional financial resources to purchase diagnostics; supply-side quality improvements could have occurred; or the programme could have increased the demand for quality care by beneficiaries. We examine each of these possible explanations in turn.
First, higher quality could have resulted from the programme's compliance requirements. As a programme conditionality, beneficiaries were required to obtain health care, and more prenatal visits could have resulted in more procedures received. However, our previous research found no significant differences between beneficiaries and non-beneficiaries for ever use of prenatal care, number of prenatal consultations, or the proportion of women obtaining the minimum number of visits set forth in the clinical guidelines (Barber and Gertler 2008a). This suggests that higher utilization could not explain the higher number of prenatal procedures received. Alternatively, higher quality could have resulted from the programme requirement to obtain services from the public sector. Our previous research found that quality in the Mexican public sector is significantly higher compared with private alternatives for the rural poor (Barber et al. 2007). Separately, we evaluated whether beneficiary women in this sample were more likely to use public services. We found, however, no significant differences in the use of public services between beneficiaries and non-beneficiaries. The programme compliance requirements to obtain more visits or care from the public sector, therefore, do not explain the higher quality received.
A second possible explanation is the financial resources to pay for more care. Although health care is free for the uninsured in Mexico, government facilities refer for diagnostics, which implies additional out-of-pocket costs. However, we find that beneficiaries received higher scores for all three quality domains. In addition to the programme's effect on history-taking and diagnostics, beneficiaries also received higher scores for the physical examination and for prevention—neither of which is related to patient out-of-pocket payments. This suggests that the ability to purchase more diagnostics could account for some of the difference, but does not fully does not explain the higher quality received by beneficiaries.
Third, increases in quality could have resulted from a supply-side response to the increase in service demand. There was some intention by the government to increase supplies and human resources in anticipation of higher utilization in programme areas (Adato et al. 2000a). However, to the authors’ knowledge, no specific quality improvements were actually implemented. A survey of 317 clinics conducted 1 year after programme implementation reported shortages of medical and auxiliary personnel, equipment and drugs (Adato et al. 2000a). Separately, we investigated this possible explanation by generating a set of hypothetical beneficiaries. Hypothetical beneficiaries were women who lived in the treatment areas and gave birth after the start of the programme (April 1998), but were ineligible for the Oportunidades programme. Hypothetical non-beneficiaries were women who lived in the control areas and gave birth after November 2000, but were ineligible for Oportunidades. If supply-side improvements had occurred, the hypothetical beneficiaries would have also benefited. However, we found that hypothetical beneficiaries did not receive higher quality compared with hypothetical non-beneficiaries who delivered prior to programme initiation in the same communities (Barber and Gertler 2008b). This suggests that, consistent with anecdotal knowledge, supply-side changes in quality did not occur.
Eliminating these alternatives, we conclude that the increases in quality received among beneficiaries probably resulted from the programme's empowerment aim to increase women's capabilities in becoming informed and active health consumers. Such capabilities could have been strengthened through some combination of pláticas emphasizing the importance of health care, regular meetings that made explicit the health care requirements, social support, and financial resources.
This finding is consistent with qualitative research in which beneficiaries reported personal changes, including increased self-confidence, and freedom of movement and association (Adato et al. 2000a). Qualitative research reported that medical doctors providing care to beneficiaries describe positive attitudinal changes with regard to health care, prevention and self-care, and patient participation. One doctor commented that ‘beneficiaries are the ones who request the most from us’; and a large proportion of health care providers reported that beneficiary patients are ‘very demanding’. Together, this evidence suggests that Oportunidades empowered women to insist on better care by informing them of the content of care and by giving them skills to negotiate better quality from health care providers.
This study has several limitations. The measurement of quality is a contentious issue with little consensus on methods and analytical approaches. The quality scores are defined as the proportion of prenatal procedures received. The criteria were developed by the Mexican Population Council, who identified aspects of evidence-based care that were considered important in this setting, and correspond with the national clinical guidelines. Measurement error is reduced because maternal reports focus on receipt of concrete procedures rather than perceptions or satisfaction, which correlate poorly with objective quality measures (Speizer et al. 2000) and vary by prior health service use and expectations, socio-economic status, and coexisting medical conditions (Brook et al. 2000). Women may have given positive responses about services received if they perceived that future programme benefits were dependent on their responses. However, this would have applied to the study's non-beneficiary and beneficiary groups equally, because the sample was limited to women who received benefits during the life of the programme. To evaluate recall bias, we ran regressions predicting quality as explained by child year of birth for beneficiaries and non-beneficiaries. The year dummy variables were not significant predictors of quality; therefore, we do not find evidence that women with longer recall periods are systematically reporting any fewer procedures. The study is also limited to rural areas and initial years of programme implementation. Anecdotal reports suggest that health service demand increased as the programme expanded, and this may have had a negative effect on quality (Nigenda and Gonzalez-Robledo 2005).
We do not examine in this study whether the differences in quality are clinically significant. However, there is good reason to believe that these procedures could have an impact on maternal and child health outcomes. Although anaemia, for example, results from different factors including nutritional deficiencies and infectious diseases, the provision of iron folate is considered beneficial. Iron supplements during pregnancy have been demonstrated effective in reducing maternal anaemia, and in increasing mean birth weight and reducing the incidence of low birth weight (Villar et al. 2003). In addition, wide variations in adherence to clinical guidelines and implementation of basic procedures have been documented for prenatal and curative care in Mexico (Bojalil et al. 1998; Barber 2006; Bautista-Arredondoa et al. 2006). Programme beneficiaries are comprised of the poorest 20% of the population, characterized by high rates of modifiable risk factors that could plausibly be addressed by high quality health care. Moreover, two case-control studies in Mexico have reported relationships between adherence to prenatal and neonatal care guidelines and birth outcomes (Coria-Soto et al. 1996; Cruz-Anguiano et al. 2004). In future research, the relationships between the improvements in quality and better birth outcomes are investigated (Barber and Gertler 2008b).
In summary, a growing body of evidence suggests that inadequate health care quality is a major problem in low-income settings, and contributes to poor health outcomes. Interventions to address quality have focused primarily on in-service training; few programmes consider the role of households, consumers or patients in improving quality or performance. We conclude that the Oportunidades conditional cash transfer programme is associated with better quality of prenatal care for low-income, rural women in Mexico. This result is probably a manifestation of the programme's empowerment goal, by encouraging beneficiaries to be informed and active health care consumers. Our results contribute evidence about interventions that can improve quality, and draw attention to the role of households and consumers in promoting high quality care. These findings are also applicable to other large-scale incentive-based welfare programmes that employ conditional cash transfers and health utilization requirements.
Acknowledgements
We thank participants of seminars at the National Institute of Public Health, Cuernavaca, Mexico, and the University of California, Berkeley, for comments and suggestions.
This research was funded by the National Institutes of Health (NIH) Fogarty International Center grant number TW006084 and the National Institute of Child Health and Human Development. The funding source has no role in the analysis or interpretation of the data.
PJG and SLB jointly conceived the research topic, formulated the research design, analyzed the data, interpreted the results, and wrote the manuscript. Both authors have full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis, and decided to submit the manuscript for publication. Both authors declare that they have no competing or conflict of interest.
References
- Adato M, Coady D, Ruel M. An operations evaluation of PROGRESA from the perspective of beneficiaries, promotoras, schools directors, and health staff. Washington, DC: International Food Policy Research Institute; 2000a. [Google Scholar]
- Adato M, de la Brière B, Mindek D, Quisumbing A. The impact of PROGRESA on women's status and intrahousehold relations. Washington, DC: International Food Policy Research Institute; 2000b. [Google Scholar]
- Barber SL. Public and private prenatal care providers in urban Mexico: how does their quality compare? International Journal of Quality in Health Care. 2006;18:306–13. doi: 10.1093/intqhc/mzl012. [DOI] [PubMed] [Google Scholar]
- Barber SL, Bertozzi SM, Gertler PJ. Variations in prenatal care quality for the rural poor in Mexico. Health Affairs. 2007;26:w310–23. doi: 10.1377/hlthaff.26.3.w310. [DOI] [PubMed] [Google Scholar]
- Barber SL, Gertler PJ. The impact of Mexico's conditional cash transfer program, Oportunidades, on birth weight. Tropical Medicine and International Health. 2008a;13 doi: 10.1111/j.1365-3156.2008.02157.x. doi:10.1111/j.1365-3156.2008.02157.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber SL, Gertler PJ. 2008b. Empowering women: how Mexico's conditional cash transfer program raised prenatal care quality and birth weight. Working Paper. [Google Scholar]
- Barham T. Social Science Research Network; 2005. Providing a healthier start to life: the impact of conditional cash transfers on infant mortality. Working Paper Series. [Google Scholar]
- Barros F, Victora C, Barros A, et al. The challenge of reducing neonatal mortality in middle-income countries: findings from three Brazilian birth cohorts in 1982, 1993, and 2004. The Lancet. 2005;365:847–54. doi: 10.1016/S0140-6736(05)71042-4. [DOI] [PubMed] [Google Scholar]
- Bautista S, Bertozzi S, Gertler P, Gutierrez JP, Hernandez M. The impact Oportunidades on health status, morbidity, and service utilization among beneficiary population: short-term results in urban areas and medium term results in rural areas (in Spanish) Cuernavaca, Mexico: National Institute of Public Health; 2004. [Google Scholar]
- Bautista-Arredondoa S, Mane A, Bertozzi SM. Economic impact of antiretroviral therapy prescription decisions in the context of rapid scaling-up of access to treatment: lessons from Mexico. AIDS. 2006;20:101–109. doi: 10.1097/01.aids.0000198096.08444.53. [DOI] [PubMed] [Google Scholar]
- Berhman J, Todd P. A report on the sample sizes used for the evaluation of the education, health, and nutrition program (PROGRESA) of Mexico. Washington, DC: International Food Policy Research Institute; 1999. [Google Scholar]
- Berman P. Organization of ambulatory care provision: a critical determinant of health system performance in developing countries. Bulletin of the World Health Organization. 2000;78:791–802. [PMC free article] [PubMed] [Google Scholar]
- Bojalil R, Espinosa P, Martinez H, Palafox M, Romero G, Gutierrez G. The quality of private and public primary health care management of children with diarrhoea and acute respiratory infections in Tlaxcala, Mexico. Health Policy and Planning. 1998;13:323–31. doi: 10.1093/heapol/13.3.323. [DOI] [PubMed] [Google Scholar]
- Brook RH, McGlynn EA, Skekelle P. Defining and measuring quality of care: a perspective from US researchers. International Journal for Quality in Health Care. 2000;12:281–95. doi: 10.1093/intqhc/12.4.281. [DOI] [PubMed] [Google Scholar]
- Chabilkuli N, Schneider H, Blaauw D, Zwi AB, Brugha R. Quality and equity of private sector care for sexually transmitted diseases in South Africa. Health Policy and Planning. 2002;17:40–6. doi: 10.1093/heapol/17.suppl_1.40. [DOI] [PubMed] [Google Scholar]
- Chaix-Couturier C, Durand-Zaleski I, Jolly D, Durieux P. Effects of financial incentives on medical practice: results from a systematic review of the literature and methodological issues. International Journal for Quality in Health Care. 2000;12:133–42. doi: 10.1093/intqhc/12.2.133. [DOI] [PubMed] [Google Scholar]
- Chakraborty S, Frick K. Factors influencing private health providers’ technical quality of care for acute respiratory infections among under-five children in rural West Bengal, India. Social Science and Medicine. 2002;55:1579–87. doi: 10.1016/s0277-9536(01)00292-1. [DOI] [PubMed] [Google Scholar]
- Coria-Soto IL, Bobadilla JL, Notzon F. The effectiveness of antenatal care in preventing intrauterine growth retardation and low birth weight due to preterm delivery. International Journal for Quality in Health Care. 1996;8:13–20. doi: 10.1093/intqhc/8.1.13. [DOI] [PubMed] [Google Scholar]
- Cruz-Anguiano V, Talavera JO, Vazquez L, et al. The importance of quality of care in perinatal mortality: a case-control study in Chiapas, Mexico. Archives of Medical Research. 2004;35:554–62. doi: 10.1016/j.arcmed.2004.11.014. [DOI] [PubMed] [Google Scholar]
- Ensor T. Consumer-led demand side financing in health and education and its relevance for low and middle income countries. International Journal of Health Planning and Management. 2004;19:267–85. doi: 10.1002/hpm.762. [DOI] [PubMed] [Google Scholar]
- Gertler PJ. Do conditional cash transfers improve child health? Evidence from PROGRESA's control randomized experimenmt. American Economic Review. 2004;94:336–41. doi: 10.1257/0002828041302109. [DOI] [PubMed] [Google Scholar]
- Gertler PJ, Martinez S, Rubio M. The impact of Oportunidades on micro-enterprise and agricultural production activities in rural Mexico. Cuernavaca: Mexico: National Institute of Public Health; 2004. Technical Document No. 19. [Google Scholar]
- Giuffrida A, Torgerson DJ. Should we pay the patient? Review of financial incentives to enhance patient compliance. British Medical Journal. 1997;315:703–7. doi: 10.1136/bmj.315.7110.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kogan MD, Alexander GR, Kotelchuck M, Nagey DA. Relation of the content of prenatal care to the risk of low birth weight: maternal reports of health behavior advice and initial prenatal care procedures. Journal of the American Medical Association. 1994;271:1340–5. [PubMed] [Google Scholar]
- LaGuarde M, Haines A, Palmer N. Conditional cash transfers for improving uptake of health interventions in low- and middle-income countries: a systematic review. Journal of the American Medical Association. 2007;298:1900–10. doi: 10.1001/jama.298.16.1900. [DOI] [PubMed] [Google Scholar]
- Maluccio JA, Flores R. Impact evaluation of a conditional cash transfer program: the Nicaraguan Red de Protección Social. Washington, DC: International Food Policy Research Institute; 2004. Food Consumption and Nutrition Division Discussion Paper No. 184. [Google Scholar]
- Meuwissen LE, Gorter AC, Knottnerus AJA. Perceived quality of reproductive care for girls in a competitive voucher programme: a quasi-experimental intervention study, Managua, Nicaragua. International Journal for Quality in Health Care. 2006;18:35–42. doi: 10.1093/intqhc/mzi073. [DOI] [PubMed] [Google Scholar]
- Ministry of Health. Mexico City: Government of Mexico; 1993. Clinical Procedural Norm 007-SSA2-1993 for Prenatal Care, Delivery, Post-Partum, and Newborns (in Spanish) [Google Scholar]
- Ministry of Social Development (SEDESOL) Mexico City: Government of Mexico; 2003. Agreement for issue and publication of the operational rules of the Oportunidades program for human development for the fiscal year 2003 (in Spanish) [Google Scholar]
- Ministry of Social Development (SEDESOL) Mexico City: Government of Mexico; 2008. Oportunidades program for human development. General information: Report of monetary support (in Spanish) [Google Scholar]
- Morris S, Flores R, Olinto P, Medina J. Monetary incentives in primary health care and effects on use and coverage of preventive health care interventions in rural Honduras: cluster randomized trial. The Lancet. 2004;364:2030–37. doi: 10.1016/S0140-6736(04)17515-6. [DOI] [PubMed] [Google Scholar]
- Nigenda G, Gonzalez-Robledo LM. Lessons offered by Latin American cash transfer programmes, Mexico's Oportunidades and Nicaragua's SPN. Implications for African countries. London: DFID Health Systems Resource Centre; 2005. [Google Scholar]
- Nolan T, Angos P, Cunha AJ, et al. Quality of hospital care for seriously ill children in less-developed countries. The Lancet. 2001;357:106–10. doi: 10.1016/S0140-6736(00)03542-X. [DOI] [PubMed] [Google Scholar]
- Obua C, Ogwal-Okeng JW, Waako P, Aupont O, Ross-Degnan D. Impact of an educational intervention to improve prescribing by private physicians in Uganda. East African Medical Journal. 2004 Feb;(Suppl):S17–24. [PubMed] [Google Scholar]
- Pariyo GW, Gouws E, Bryce J, Burnham G the Uganda IMCI Impact Study Team. Improving facility-based care for sick children in Uganda: training is not enough. Health Policy and Planning. 2005;20(Suppl. 1):58–63. doi: 10.1093/heapol/czi051. [DOI] [PubMed] [Google Scholar]
- Parker S, Teruel GM. Randomization and social program evaluation: The case of Progresa. Annals of the American Academy of Political and Social Sciences. 2005;599:199–219. [Google Scholar]
- Rivera JA, Sotres-Alvarez D, Habicht JP, Shamah T, Villalpando S. Impact of the Mexican program for education, health, and nutrition (Progresa) on rates of growth and anemia in infants and young children: a randomized effectiveness study. Journal of the American Medical Association. 2004;291:2563–70. doi: 10.1001/jama.291.21.2563. [DOI] [PubMed] [Google Scholar]
- Rowe AK, de Savigny D, Lanata CL, Victoria CG. How can we achieve and maintain high-quality performance of health workers in low-resource settings? The Lancet. 2005;366:1026–35. doi: 10.1016/S0140-6736(05)67028-6. [DOI] [PubMed] [Google Scholar]
- Schofield C, Ashworth A. Why have mortality rates for severe malnutrition remained so high? Bulletin of the World Health Organization. 1996;74:223–9. [PMC free article] [PubMed] [Google Scholar]
- Siddiqi K, Newell J, Robinson M. Getting evidence into practice: what works in developing countries? International Journal for Quality in Health Care. 2005;17:447–53. doi: 10.1093/intqhc/mzi051. [DOI] [PubMed] [Google Scholar]
- Skoufias E, Davis B, Berhman J. Washington, DC: International Food Policy Research Institute; 1999. An evaluation of the selection of beneficiary households in Progresa: final report. [Google Scholar]
- Speizer IS, Bollen KA. How well do perceptions of family planning service quality correspond to objective measures? Evidence from Tanzania. Studies in Family Planning. 2000;31:163–77. doi: 10.1111/j.1728-4465.2000.00163.x. [DOI] [PubMed] [Google Scholar]
- Steklov G, Winters P, Todd J, Regalia F. Demographic externalities from poverty programs in developing countries: experimental evidence from Latin America. Washington, DC: American University; 2006. Department of Economics Working Paper Series No. 2006–1. [Google Scholar]
- Tuan T, Dung VT, Neu I, Dibley MJ. Comparative quality of private and public health services in rural Vietnam. Health Policy and Planning. 2005;20:319–27. doi: 10.1093/heapol/czi037. [DOI] [PubMed] [Google Scholar]
- Villar J, Merialdi M, Gülmezoglu AM, et al. Nutritional interventions during pregnancy for the prevention or treatment of maternal morbidity and preterm delivery: an overview of randomized controlled trials. Journal of Nutrition. 2003;133:1606S–25S. doi: 10.1093/jn/133.5.1606S. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Antenatal care in developing countries: promises, achievements, and missed opportunities. An analysis of trends, levels, and differentials 1990–2001. Geneva: World Health Organization; 2003. [Google Scholar]
- Zurovac D, Rowe A, Ochola S, et al. Predictors of the quality of health worker treatment practices for uncomplicated malaria at government health facilities in Kenya. International Journal of Epidemiology. 2004;33:1080–91. doi: 10.1093/ije/dyh253. [DOI] [PubMed] [Google Scholar]