Abstract
In an era of significant biomedical advances in the treatment of HIV, health disparities still persist. The participation of minority researchers brings new perspectives to health-disparities research. Mentoring is key to this process.
We present the multifaceted mentoring model that evolved in the Puerto Rico Comprehensive Center for the Study of HIV Disparities and the Mentoring Institute for HIV and Mental Health. The model includes (1) multi-institutional collaborations, (2) competency development, and (3) cross-disciplinary teams.
These aspects of the model provide guidelines for institutions seeking to formalize mentoring programs while addressing the complexities of health disparities. The competency development component is a powerful tool in assessing and supporting the researchers. Further explorations on the applicability of the model are encouraged.
UNDERSTANDING AND responding to health disparities among people living with HIV is a complex task. Significant biomedical advances in the diagnosis and treatment of HIV have not been enough to effectively overcome the inequities and disparities. HIV-disparity research aimed at increase our understanding of how to make substantial reductions in and effectively overcome disparities should address issues from a local perspective and in close contact with vulnerable populations.1 The selection of issues should respond to the issues' relevance within a given culture and to the potential of developing interventions to ameliorate disparities.2 The participation of minority researchers should enrich the findings and outcomes for reducing health disparities. They bring perspectives, trainings, experiences, and values that might be different from the mainstream. There is a need to address the lack of minority researchers, because they are often the driving force behind minority-related research.
Health disparities research entails diverse challenges, including (1) strengthening the infrastructure for research in universities that have close ties with the affected communities and (2) developing researchers with cultural competence and skills for interdisciplinary and transdisciplinary research. Mentoring is an essential element of this process.3,4 Studies indicate that mentoring can contribute to a greater productivity of researchers, especially minority researchers, in the biomedical and social fields.
We discuss the implementation and experiences of a multifaceted mentoring model that evolved in the Puerto Rico Comprehensive Center for the Study of HIV Disparities (PRCCHD) and the Puerto Rico Mentoring Institute for HIV and Mental Health Research (PRMI). Both initiatives foster meaningful research aimed at the elimination of HIV disparities and provide support to a new cadre of researchers.
The multifaceted mentoring model includes (1) establishing multi-institutional collaborations, (2) offering systematic and continuous training based on competency development, and (3) creating cross-disciplinary research teams in which mentors and mentees work together. Attention to these 3 facets produces synergy and provides the solid foundation needed to foster long-standing mentor–mentee relationships. Fundamental to this model is the understanding that mentoring is a process in which mentors and mentees jointly advance their commitment to scholarly pursuit. Mentoring is envisioned as a process for fostering systematic engagement while inspiring and empowering both mentee and mentor.4 Furthermore, mentoring provides a platform for researchers from different disciplines to understand what they share and to explore what lies beyond their disciplinary domains. The multifaceted mentoring model has the potential of being replicated in other contexts. We discuss the main features underlying the proposed model and highlight lessons learned and the major accomplishments of the PRCCHD and PRMI.
MULTI-INSTITUTIONAL COLLABORATION
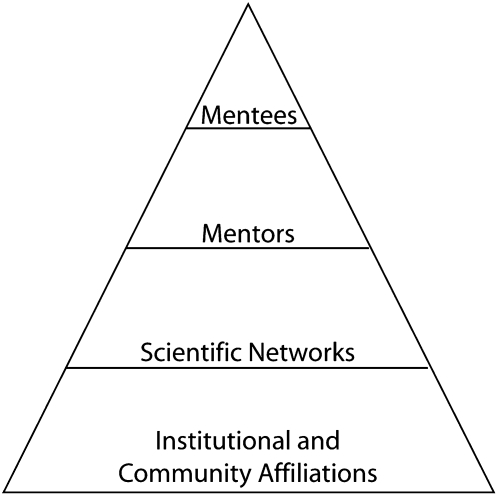
During the past 3 decades, universities, health-related institutions, and community-based organizations have procured resources to establish research centers and implement preventive and care initiatives for people living with HIV. Some of these institutions and organizations have targeted vulnerable populations. They have accumulated resources and expertise that is seldom shared. To properly mentor the next generation of researchers, it is imperative to intentionally create bridges between these institutions. The sharing of resources and ideas creates a solid foundation for comprehensive research that can be translated into valid preventive and care approaches for people living with HIV who are experiencing health-related disparities. As illustrated in Figure 1, the proposed mentoring model in based on the notion that the mentees are at the top of the pyramid; they benefit from the solid foundation provided by institutional and community affiliations, scientific networks, and mentors.
FIGURE 1.
Mentee's sources of support and collaboration.
As a first step or facet in establishing a mentoring program, the PRCCHD and the PRMI formalized multi-institutional collaborations among the 3 schools of medicine in Puerto Rico and other professional schools like those of public health, dentistry, psychology, and pharmacy. Before long, these partnerships broadened to include institutions in the United States, specialized research centers, and community-based organizations that work with populations with HIV or other vulnerable populations. The box on this page illustrates the diversity of the institutions currently involved. The mentees have access to these institutions, mainly through their mentors.
Selected Institutions to Which Mentees Have Access Through Their Mentors.
Institutions in the United States:
Department of Medicine, Obstetrics–Gynecology, Brown Medical School, Providence, RI
HIV Research Section—AIDS Office, San Francisco, CA
Frank Porte Graham Center (Child Development Center), University of North Carolina, Chapel Hill
The Futures Group; Center for HIV/AIDS, Washington, DC
Center for the Study of Culture, Health, and Human Development, University of Connecticut, Storrs
Huntsman Cancer Institute, University of Utah
Epidemiology and Biostatistics Department, Case Western University
The Institute of Human Virology, University of Maryland
College of Pharmacy, Nova Southeastern University
Centers in Puerto Rico:
Retrovirus Research Center, Bayamón
AIDS Research Center, Ponce School of Medicine
Clinical Research Center Specialized Research Programs
University Center for Psychological Services and Research, University of Puerto Rico (UPR), Rio Piedras Campus
Center for Evaluation and Sociomedical Research, Graduate School of Public Health, Medical Sciences Campus, UPR
Clinical Psychology Program, Ponce School of Medicine
Behavioral Sciences Research Institute, Medical Sciences Campus, UPR
Adolescent Medicine Trials Network, Medical Sciences Campus, UPR
FILIUS Institute of Disability and Rehabilitation Research, UPR
Consolidating partnerships and understanding the culture of collaborating institutions are incremental processes that should constantly be monitored and promoted. In the case of the integration of academic institutions, academic administrators should be reminded of what they gain, and tangible results should be shared. Participating faculty should have an opportunity to advance their own learning and research careers, and the mentees need to feel inspired and empowered to make a difference in the highly structured and sometimes intimidating world of research and scholarly pursuit. It is desirable that collaborations be extended beyond universities because service institutions can also provide valuable resources and mentors that could substantially enrich research opportunities and create meaningful career paths for mentees.
One of the main challenges of the process of obtaining collaborations among institutions is understanding their fundamental values and characteristics. The institutional value system is closely related to motivations and incentives that could facilitate the recruitment and retention of mentors and mentees. It is important to consider some caveats related to traditional versus minority institutions. In addition, it is essential to give special attention to the selection of mentors and mentees. They become the face of the collaborative effort.
Mainstream Versus Minority Institutions
There are several salient issues that relate to minority investigators and their career advancement. We describe some of the issues confronted by minority investigators according to type of institution: traditional or mainstream versus mostly minority institutions. Minority institutions are defined by the Higher Education Act (HEA) according to the enrollment of minority students (minority students should exceed 50% of its total enrollment). Traditional or mainstream institutions have a greater proportion of White faculty and students compared to minority institutions, which comprise a larger proportion of non-White individuals.5 In general, traditional institutions have more resources and better infrastructure. Educational institutions strive for diversity and have developed unique strategies to increase the diversity among students and faculty. Examples of minority institutions include the historically Black colleges and universities or Hispanic-serving institutions. It is important to make the distinction between traditional and minority institutions because particular issues and corrective actions regarding allocation and management of resources might be different.
For a minority faculty or investigator based in a traditional or mainstream institution with more resources and better infrastructure, there are additional roles and assumed responsibilities that might add to the workload, creating conflict with time and duties. For example, a Hispanic investigator at a mainstream institution might have to represent the “Hispanic” perspective as part of his or her job, whereas the participation of other nonminority investigators is more diluted because there is a larger pool of potential members for the committees or activities. In addition, it is expected that this minority individual serve as a mentor to other minority individuals in the given institution. This might place a minority faculty or investigator at a disadvantage with other faculty, therefore affecting the time availability for productivity. This situation of having to participate in specific committees might give some clout to the particular individual, but it comes at the expense of additional personal time and effort.
The situation might be different for individuals who are based in more traditional minority institutions (defined as those who serve a given percentage of minority students, for example). Historically, these institutions have fewer resources, which could render them less competitive in the world of externally funded research. This is the case of universities in Puerto Rico. Investigators who succeed in obtaining external funding and publish in scientific literature are often asked by those around him or her to serve as mentor and supporter and to review manuscripts and proposals. This might constitute an additional burden on a person who is already working hard. There is a need to increase the pool of minority researchers so that the burden is not placed on a specific individual. One solution to address this need is the establishment of structured programs to mentor individuals and encourage them to pursue careers in the study of health disparities and cultural competence.
Mentors and Mentees
What makes a good mentor? How are they chosen? A mentor is needed for scientific ideas and methodology, for emotional support, and for leadership and guidance within the institution and with the broader aspects of the career. A mentor is also needed to establish a network of collaborators and to be introduced into specific circles of limited access.6,7 They need to understand and deal with the politics of the institution. There might be gender issues as well as minority-related issues to which the mentors must be sensitive. Given all of the roles expected from a mentor, it would be very difficult for a single person to fulfill all of these needs. So, a mentee needs to be able to engage different people for the various needs according to the priorities and timing of the events. If the mentees are not able to juggle the potentially diverse and conflicting advice from different mentors, they might confront serious and potential dilemmas. A structured program that takes into account the different needs and ways to respond to those needs might protect the mentees from unnecessary conflict.8
Not every successful investigator can become a good mentor, and actually, some very successful investigators might discourage junior investigators because of a lack of interest in the junior investigator's development or a limited research focus. A good mentor needs to be able to provide guidance without being too directive; to allow the mentee to choose his or her topic of interest, apart from the mentors'; and to be able to listen to new ideas and allow for a wider discussion and analysis of the research question and the methodology that might be used to answer it. The mentor needs to be able to communicate with the other mentors in a respectful, professional, and productive way. A mentor needs to have the social skills and maturity to create the best environment for the growth and scientific (funding) independence of the mentee. By the same token, a mentee needs to have enough communication skills to get the best from his or her mentors, needs to be focused, persistent, eager to ask questions, and willing to accept some guidance. Good social skills are also essential for the mentees.9
Because senior researchers are busy, it is important to choose individuals with enough experience but sufficient openness to engage in activities with junior investigators. This is a delicate balance, and mentors need training as well. It is also important, as previously mentioned, to create a cadre (pool) of mentors from diverse backgrounds with different perspectives of the scientific method and pursuit so that the investigators being mentored benefit from looking at the problem in question with different eyes. They might even ask different questions just because of these exposures.10 One of the major accomplishments of the PRCCHD has been its ability to retain 100% of its mentors. The 15 mentors provide expertise in a wide range of disciplines and approaches, including clinical specialties and subspecialties, clinical research, transcultural and comparative research, health promotion and disease prevention, behavioral epidemiology, quantitative analysis, qualitative and ethnographic methodologies, and epidemiology biostatistics, among others.
A successful mentoring program needs to recruit mentees who have the best chances of developing into independent investigators. The program might be judged by the number of funded applications or publications its mentees are able to publish over a given (usually limited) amount of time. A program needs to identify the best candidates. Most programs will have a structured application form, and the candidates will need to write a concept proposal. This will identify good candidates on paper but not necessarily those with the best skills for collaborative research. Methods for identifying candidates also should include observing their interaction with others during specific workshops in which a project could be conceptualized. Large institutions might have a larger pool of candidates compared with smaller or geographically isolated places. The selection of candidates with the social skills, attitude, training, and commitment will be key to the success of the program.10
In the PRCCHD, this method of selecting mentees has rendered excellent results. Ninety percent of the junior investigators have remained affiliated to the center for more than 5 years and have demonstrated significant advancement. Most of them have designed a career plan and identified accomplishments, needs, aspirations, and strategic actions. These plans have become a tool for focusing efforts and assessing progress.
COMPETENCY DEVELOPMENT
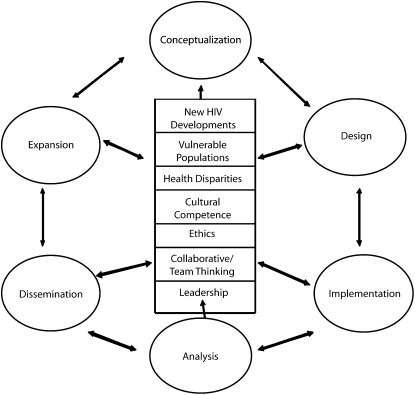
An integral part of the multifaceted framework for mentoring is the development of a series of core and cross-cutting research competencies among the mentees. Investigators' development activities aimed at research productivity, personal development, and career guidance are indispensable. Six core areas of competencies have been identified as essential to the pursuit of an integrated approach to research. These are conceptualization, research design, implementation, analysis, dissemination, and expansion. In addition, the participants, no matter the stage of their research development, need to be continuously exposed to cross-cutting knowledge and skills related to HIV and health disparities. Figure 2 illustrates the core and cross-cutting competencies that are developed through continuous training opportunities.
FIGURE 2.
A competency model showing core and cross-cutting domains.
Note. The ovals illustrate core domains, which are influenced by cross-cutting domains depicted in the middle. Source. Adapted from the competency model developed by the Association of Schools of Public Health.11
The PRCCHD and the PRMI offer didactic and experiential activities to facilitate the acquisition of core and cross-cutting research competencies. Examples are onsite visits to the research facilities of the mentors, seminars, retreats, workshops, and interactive writing seminars, among others. The periodicity and continuity of the activities guarantee the emergence and sustainability of personal and professional relationships among team members of different disciplines.10 In addition to their training and mentoring role, the senior researchers participate in defining the scope and the upcoming plans related to the development of competencies.
In the PRCCHD and the PRMI, individual and group mentoring opportunities are carefully designed so that the mentors can offer their unique expertise. These enable, empower, and inspire the participants in the acquisition of the core and cross-cutting competencies. Having a well-defined set of competencies facilitates the delimitation of expectations between mentors and mentees and provides the basis for monitoring progress and assessing outcomes. The mentees have the opportunity to share and obtain feedback from peers and mentors on methodological and analytic issues related to their projects. Seminars and workshops are ideal for this type of exchange.
While engaged in the competency development facet, it is preferable that the mentees have some control over a research project. This can occur by being a principal investigator in a pilot study funded by a developmental grant or by institutional funds. The mentees at the PRCCHD are actively engaged in a research project. The involvement in a research project provides the opportunity for hands-on learning and one-on-one mentoring. The mentor's participation is expected at all the stages of the research process—providing the guidance and skills needed during the earlier stages (i.e., conceptualization, design, and implementation) as well as the later stages (i.e., analysis, dissemination, and expansion). It should be noted that the later stages need more commitment and time.
It is essential to carefully match mentors to mentees by area of interest and professional characteristics. Mentors should be involved in externally funded research related to HIV or health disparities, have an appreciation of the minority culture, have previous mentoring experience with minority researchers, and be knowledgeable of the research process.12
During the implementation of the competency-development component of the model at the PRCCHD and the PRMI, special attention was given to the cross-cutting competencies. To study health disparities, researchers must take into account the cultural context of race and ethnicity in the populations under investigation. In our institution, the study of health disparities has emphasized differences among socially marginalized segments of the population. As illustrated in Table 1, researchers are studying vulnerable populations such as drug users, commercial sex workers, and people living with HIV to examine the effects of factors like discrimination, bias, and prejudice on their health status (downstream determinants). They focus on social determinants of health such as poverty, violence, and barriers in the access to health care (upstream determinants).12 It is imperative that researchers develop skills to address issues in an ethical and culturally competent way, collaborate in interdisciplinary teams, and become leaders and accept responsibility in reducing HIV health disparities.
TABLE 1.
Selected Studies Conducted by Mentees and Disciplines of the Team Members: Puerto Rico Center for the Study of Health Disparities, 2004–2009
| Research Studies | Disciplines of Team Members |
| Adaptation and piloting of an HIV prevention intervention utilizing the rapid HIV test in women at risk for HIV | Medicine, public health education, psychology |
| Abuse, felt stigma, and drug regimen adherence in people living with HIV/AIDS | Medicine, psychology |
| HCV risk-reduction intervention as a second HIV comorbidity prevention | Epidemiology, medicine, education |
| Cultural competence and HIV-related social stigma in a cohort of health care providers and students in Puerto Rico | Psychology, dental medicine, public health |
| Spanish translation and cultural adaptation of the primary assessment tool (PCAT) for the HIV/AIDS population | Psychology, public health, health policy |
| Exploring the level of knowledge and communication skills of mothers with HIV/AIDS | Psychology, medicine-pediatrics, public health |
| Validation of technology for self-administered surveys: a crossover study to compare tablet PC and paper surveys in Hispanic populations | Medicine, evaluation research, informatics, dental medicine |
| Factors affecting the early versus late diagnosis of HIV infection in a cohort of HIV-infected patients | Medicine, public health, demography |
CROSS-DISCIPLINARY RESEARCH TEAMS
Establishing cross-disciplinary research teams is a facet of the proposed mentoring model to which time and resources are devoted with a high sense of priority. As stated, the issues related to HIV health disparities are complex. Interventions are successful when they are based on an appropriate level of multidisciplinary and interdisciplinary strategies. It is important for the next cadre of researchers to work in teams in which discipline lines are crossed to advance knowledge that incorporates perspectives and approaches in a comprehensive way.
Researchers are part of a social group of their disciplines. To work with members of an interdisciplinary team, they must recognize, respect, and value the diversity in perspectives, ideologies, and beliefs of the different disciplines. Using a model of cultural competence will facilitate more-effective collaboration between disciplines and provide opportunities for new insights. Through awareness of one's own disciplinary culture and a sensitivity to others, interdisciplinary research and practice may provide creative solutions to important problems.13–15
It is important to facilitate and monitor the formation of research teams with the participation of young researchers (mentees) from different institutions and from different professional backgrounds and medical specialties. To reinforce those cross-cultural partnerships among the young investigators, the mentors assigned to them should also be representative of different disciplines and culture. Ideally, each mentee and the mentee's research group should be assigned a local (i.e., institutional) and an external, noninstitutional mentor to create a synergetic effect toward collaboration, leading to the proper projection of local issues to the global or expanded community.13–15
Other than having a local mentor and an external mentor, mentees should be able to access a pool of senior researchers and scholars (scholarly mentors) of national recognition affiliated with universities and research centers in the United States and worldwide. This guarantees that research results transcend to global knowledge. When selecting and forming the group of mentors and collaborators, it is important to make sure that they provide depth and breadth of expertise in clinical research, transcultural and comparative research, health promotion, behavioral epidemiology, quantitative analysis, qualitative and ethnographic methodologies, and biostatistics, among other things. This pool of experienced researchers should be responsible for creating opportunities for cross-discipline approaches to health.10
Health disparities are associated with factors such as patients' perceived discrimination and mistrust in the health care system, poor or ineffective communication between patients and physicians, and health care providers' lack of cultural competence and sensitivity.14 Cultural competence is needed to make health care services more responsive to underserved populations. To move the research focus and stimulate impact from a local response to a global one, an understanding of different cultural contexts is required. To be culturally competent, a researcher needs to respect the values, attitudes, beliefs, and lifestyles of all cultures. Researchers must learn to address these differences in their design, data collection, methodology, and analysis. Most researchers have not received training to work from this perspective and have the tendency to assume the cultural perspective of the majority. The mentoring process is critical in fostering this switch in perspective toward cultural competency among investigators.
Among the accomplishments of the PRCCHD has been the formation of 8 interdisciplinary research teams, of which 5 are based in more than one institution. As illustrated in the box on page S66, all the research projects address issues related to HIV, health disparities, and vulnerable populations. All the research teams have presented their results in local, national, and international conferences and published their results in peer-reviewed journals. Important paths of scholarship have been established in HIV, health disparities, mixed methodology, instrument and intervention adaptation, and in the science of mentoring.
CONCLUSIONS
The multifaceted mentoring model was developed to enhance the dynamic, reciprocal relationship between senior and beginner researchers, with the aim of contributing to the development of both. Mentorship should go beyond one-on-one partnerships and encourage minority investigators to work in areas such as health disparities and HIV. The experience of the PRCCHD and the PRMI in designing and implementing this innovative approach to mentoring has proven to be effective in supporting minority investigators who are capable of working with more than 1 institution. The main lesson learned during the implementation of the model is that mentoring seems to be instrumental in maintaining young researchers engaged in the field. They are constantly disseminating their findings to affect service. They have adopted cross-disciplinary approaches in their research queries with the intention of reducing health disparities.
The 3 facets of the mentoring model discussed are generalizable to other contexts. They provide guidelines for institutions or programs that are seeking to support and formalize mentoring programs for researchers while guaranteeing a productivity that responds to the complexities of health disparities. It should be emphasized that the competency-development component proved to be a powerful tool to help us assess and support the deficiencies and strengths of the researchers. Furthermore, the features of the model can be useful to institutions that are in the process of promoting a long-lasting mentoring culture based on collaboration. Further explorations on the impact and applicability of the unique facets described here are encouraged.
Acknowledgments
This work has been supported by the Puerto Rico Comprehensive Center for the Study of HIV Disparties through a grant from the National Center for Research Resources (NCRR; grant 5U54RR019507-05) and the Puerto Rico Mentoring Institute for HIV and Mental Health Research (PRMI) through a grant from the National Institute of Mental Health (NIMH; grant 1R25MH 083617-01). S. E. Rabionet received support from the NCRR (grant 5U54RR019507-05) and the NIMH (grant 1R25MH 083617-01). C. D. Zorrilla received support from the NCRR (grant 5U54RR019507-05), the National Institute of Allergy and Infectious Diseases (NIAID; grant 1U01 A169415-01), the NIMH (grant 1R25MH 083617-01) and the Research Center for Minority Institutions (RCMI; grant G12RR-03051-01). L. E. Santiago received support from the NCRR (grant 5U54RR019507-05), the NIAID (grant 1U01 A169415-01), and the RCMI (grant G12RR-03051-016).
Human Participation Protection
No approval was required.
References
- 1.Ostlin P, Braveman P, Dachs JN, et al. Priorities for research to take forward the health equity policy agenda. Bull World Health Organ. 2005;83:948–953 [PMC free article] [PubMed] [Google Scholar]
- 2.Mullins CD, Blatt L, Gbarayor CM, Keri-Yang HW, Baquet C. Health disparities: a barrier to high-quality care. Am J Health Syst Pharm. 2005;62:1873–1882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Green BL, Rivers BM, Arekere DM. Mentoring: a framework for developing health disparities researchers. Health Promot Pract. 2006;7:336–345 [DOI] [PubMed] [Google Scholar]
- 4.Fuller SS. Enabling, empowering, inspiring: research and mentorship through the years. Bull Med Libr Assoc. 2000;88:1–10 [PMC free article] [PubMed] [Google Scholar]
- 5.US Department of Education United States Department of education lists of postsecondary minority institutions. Available at: http://www.ed.gov/about/offices/list/ocr/edlite-minorityinst.html. Accessed January 3, 2009
- 6.Allen SL. Mentoring: the magic partnership. Can Oper Room Nurs J. 2006;24:30–35 [PubMed] [Google Scholar]
- 7.Sambunjak D, Straus SE, Marusic A. Mentoring in academic medicine: a systematic review. 2006; 296:1103–1115 [DOI] [PubMed] [Google Scholar]
- 8.Ramani S, Grupen L, Kachur EK. Twelve tips for developing effective mentoring. Med Teach. 2006;28:404–408 [DOI] [PubMed] [Google Scholar]
- 9.Schrubbe KF. Mentoring: A critical component for professional growth and academic success. J Dent Educ. 2004;68(3):324–328 [PubMed] [Google Scholar]
- 10.Molloy JC. Development of networks: literature review and future research. Career Dev Int. 2005;10:536–547 [Google Scholar]
- 11.Calhoun JG, Ramiah K, Weist M, Shortell S. Development of competency model for the Master in Public Health degree. Am J Public Health. 2008;98:1598–1607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Doemland J. An introduction to upstream determinants of health. Am J Prev Med. 2002;22:23–2911777675 [Google Scholar]
- 13.Reich SM, Reich JA. Cultural competence in the interdisciplinary collaborations: a method for respecting diversity in research partnerships. Am J Community Psychol. 2006;38:51–62 [DOI] [PubMed] [Google Scholar]
- 14.Winkelman M. Cultural Awareness Sensitivity and Competence. Peosta, IA: Eddie Bower Publishing; 2005 [Google Scholar]
- 15.Zambrano RE, Molnar C, Baras-Muñoz H, Salas-Lopez D. Cultural competency as it intersects with racial/ethnic, linguistic, and class disparities in managed healthcare organizations. Am J Manag Care. 2004;10(suppl):37–44 [PubMed] [Google Scholar]