Abstract
Objectives. We examined correlations between survival and race/ethnicity, age, and gender among persons who died from AIDS-related causes.
Methods. We estimated survival among 11 022 persons at 12, 36, and 60 months after diagnosis with AIDS in 1993 through 2001 and reported through 2003 to the Chicago Department of Public Health. We estimated hazard ratios (HRs) by demographic and risk characteristics.
Results. All demographic groups had higher 5-year survival rates after the introduction of highly active retroviral therapy (1996–2001) than before (1993–1995). The HR for non-Hispanic Blacks to Whites was 1.18 in 1993 to 1995 and 1.51 (P < .01) in 1996 to 2001. The HR for persons 50 years or older to those younger than 30 years was 1.63 in 1993–1995 and 2.28 (P < .01) in 1996–2001. The female-to-male HR was 0.90 in 1993–1995 and 1.20 (P < .02) in 1996–2001.
Conclusions. The risk of death was higher for non-Hispanic Blacks and Hispanics than for non-Hispanic Whites. Interventions are needed to increase early access to care for disadvantaged groups.
Several factors have led to increases in survival among persons with AIDS, including the use of immunologic criteria to define AIDS,1 earlier identification of and treatment for opportunistic diseases,2 and widespread use of highly active antiretroviral therapy (HAART).3,4 Although the expansion in the case definition and improvements in diagnosing and treating diseases resulted in modest improvements in survival times before the advent of HAART, controlled trials,5–7 clinic-based studies,8–10 and surveillance data5,11–14 found dramatic improvements in survival after December 1995, when HAART was recommended as the standard of care for persons with AIDS.3 The effect of the new treatment on AIDS mortality became apparent almost immediately. National HIV/AIDS-related mortality declined 28% from 1995 to 1996, an additional 45% from 1996 to 1997, and 28% from 1997 to 1998.15
Large urban centers have had the highest AIDS incidence rates16 since the disease was first described in 1981,17 and the city of Chicago is no exception. From 1981 through 2006, more than 23 000 AIDS cases were reported. Nearly 56% of those persons had died by 2006.18 After 1980, Chicago became unique among large US cities because its population was comprised of roughly equal numbers of non-Hispanic Blacks, non-Hispanic Whites, and Hispanics. In 1993, non-Hispanic Blacks and Whites each comprised approximately 38% of the population; 19% of city residents were Hispanic (predominately Mexican and Puerto Rican). Although non-Hispanic White adults in Chicago were more likely than were Whites across the nation to lack a high school diploma, they had a higher per capita income than did non-Hispanic Whites nationally. Non-Hispanic Blacks and Hispanics had per capita incomes similar to their counterparts nationally and substantially lower than that of non-Hispanic Whites.
By the end of 2001, Chicago's non-Hispanic White population had declined by 17% and its non-Hispanic Black population by 6%. The Hispanic population grew by 33%, with a declining proportion having a Puerto Rican background and increasing numbers originating from Central and South America. Although Chicago's non-Hispanic White population decreased in size, its relative wealth increased, with a per capita income 40% higher than that of non-Hispanic Whites nationally. The per capita incomes of non-Hispanic Blacks and Hispanics continued to mirror those of their counterparts nationally, and the income gap between these groups and Chicago's non-Hispanic White population increased.
Minorities, particularly non-Hispanic Blacks, are disproportionately affected by AIDS. For example, one third of the citizens of Chicago and nearly two thirds of its AIDS patients are non-Hispanic Blacks.
Because of the disproportionate effect of HIV/AIDS on some of Chicago's demographic groups and because we were aware of no previous studies that analyzed cause-specific AIDS mortality in relation to survival time, we conducted a survival analysis among persons diagnosed with AIDS between January 1993 and December 2001. Individuals were followed through 2003 to identify factors that predicted increased survival and to examine disparities in survival, particularly by demographic characteristics.
Disparities in AIDS survival may be influenced by many factors. Disparities in screening and early diagnosis can be caused by differences in recognition of risk; the importance of health relative to other concerns, such as economic subsistence and violence; negative consequences, such as social stigma, associated with receiving an HIV or AIDS diagnosis; and access to providers of screening services. For persons diagnosed with AIDS, survival may be influenced by differences in access to care providers; the quality of care provided, including the cultural competence of care providers and medical appropriateness of treatment; and the patient's ability to successfully adhere to treatment regimens. Health literacy has been shown to be an important mediator of disparities in adherence to AIDS medical treatment.19 Differences in health literacy between ethnic groups can be influenced by local structural factors. For example, urban public schools (including the Chicago public schools) have long been known for providing significantly lower-quality education in predominately minority than in White neighborhoods.20
METHODS
Data Sources and Study Population
The HIV/AIDS Reporting System database, developed by the Centers for Disease Control and Prevention and maintained by the Chicago Department of Public Health's Office of HIV/AIDS Surveillance, was the source of data on survival with AIDS. The state of Illinois requires that all cases of AIDS be reported within 7 days of diagnosis, regardless of whether the individual has been reported previously by another provider.21 Adults and adolescents (i.e., those 13 years and older) who were diagnosed with AIDS between January 1993 and December 2001 and reported to the Chicago Department of Public Health through June 2006 were eligible for inclusion.
We restricted our analyses to persons who identified themselves as non-Hispanic White, non-Hispanic Black, or Hispanic. These 3 groups represented 94% of the general population of Chicago22 and 99% of AIDS cases diagnosed between 1993 and 2001.18 In addition, we limited the study population to individuals who acquired AIDS through 3 major exposure categories: male-to-male sexual contact, injection drug use, or heterosexual contact.
Outcome and Exposure Variables
An individual was classified as having died if his or her name matched a death certificate in the electronic database of the state of Illinois's vital records database or a death certificate from the National Death Index. We searched underlying and contributing causes of death and other conditions present at the time of death with the following codes from the Manual of the International Statistical Classfication of Diseases, Injuries, and Causes of Death, Ninth Revision (ICD-9)23 and the International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10)24: for 1993 to 1998, ICD-9 codes 42 to 44; for 1999 to 2003, ICD-10 codes B20 to B24.
Deaths were searched only through 2003 because this was the most recent year of available death data in Illinois at the time of the study. If an individual with AIDS died of a cause that was not a direct result of his or her underlying HIV disease, we censored the individual's follow-up time on the date of death. Thus, deaths were HIV/AIDS specific, not all cause. If an individual had no corresponding match to a death record from the Illinois Department of Public Health or the National Death Index during the 2-year follow-up period, his or her follow-up time was censored on December 31, 2003.
Survival was examined in relation to several variables, including gender, race/ethnicity, mode of transmission, age, and era (pre-HAART era, 1993–1995, or HAART era, 1996–2001).
Statistical Methods
All analyses were performed with SAS version 9.13 (SAS Institute, Cary, North Carolina). We used the log-rank test of the Kaplan–Meier product-limit method to assess the assumption of homogeneity of survival in stratified subgroups. We examined the log (−log [survival]) plots to investigate the proportional hazards assumption. We used the adjusted survival curves obtained from the average covariates method in the Cox stratified regression model to estimate the percentage change in the proportion of persons surviving 1, 3, and 5 years after diagnosis with AIDS.
We modeled survival with multivariate Cox regression. The model assumed a constant baseline hazard for all persons; changes in the values of the covariates included in the model modified the baseline hazard. The main effects were modeled first and then all first-order interaction terms were checked. Next, we checked interaction between main effects and time. If we found an interaction between a variable and time, we used time as a stratifying variable.
RESULTS
Demographic and risk characteristics for individuals diagnosed with AIDS in the pre-HAART era (1993–1995) and HAART era (1996–2001) are shown in Table 1. Overall, 11 022 adults and adolescents were diagnosed with AIDS between January 1, 1993, and December 31, 2001. Of these, 5731 (51%) had died by December 31, 2003. Approximately 30% of deaths were attributable to causes related to AIDS. Most of the AIDS patients studied were male (81%) and non-Hispanic Black (62%). Nearly three quarters of the study population were aged 30 to 49 years at the time they were diagnosed with AIDS. Approximately 47% of cases were attributed to male-to-male sexual contact and 42% to injection drug use.
TABLE 1.
Demographic and Risk Characteristics of Persons Diagnosed With AIDS Before and After the Introduction of Highly Active Antiretroviral Therapy: Chicago, 1993–2001
| Characteristic | Pre-HAART Era, 1993–1995, No. (%) | HAART Era, 1996–2001, No. (%) | Total, No. (%) |
| Gender | |||
| Male | 4 353 (83.5) | 4 514 (77.8) | 8 867 (80.5) |
| Female | 863 (16.6) | 1 292 (22.3) | 2 155 (19.6) |
| Race/Ethnicity | |||
| Non-Hispanic Black | 2 966 (56.9) | 3 858 (66.5) | 6 824 (61.9) |
| Non-Hispanic White | 1 527 (29.3) | 1 102 (19) | 2 629 (23.9) |
| Hispanic | 723 (13.9) | 846 (14.6) | 1 569 (14.2) |
| Mode of transmission | |||
| Male-to-male sexual contact | 2 524 (51.1) | 2 250 (42.8) | 4 774 (46.8) |
| Injection drug use | 2 040 (41.3) | 2 218 (42.2) | 4 258 (41.8) |
| Heterosexual contact | 376 ( 7.6) | 790 (15) | 1 166 (11.4) |
| Age at diagnosis, y | |||
| 13–29 | 735 (14.3) | 736 (12.8) | 1 471 (13.5) |
| 30–49 | 3 849 (74.5) | 4 248 (73.6) | 8 097 (74.1) |
| ≥ 50 | 573 (11.1) | 788 (13.7) | 1 361 (12.5) |
| Opportunistic diseases | |||
| Pneumocystis carinii pneumonia | 489 (9.4) | 469 ( 8.1) | 958 (8.7) |
| Kaposi's sarcoma | 88 (1.7) | 67 ( 1.2) | 155 (1.4) |
| Othera | 2 865 (54.9) | 2 496 (43.8) | 5 361 (48.6) |
| No disease specified | 1 774 (34) | 2 774 (47.8) | 4 548 (41.3) |
| Vital status | |||
| Alive | 1 681 (32.2) | 3 628 (62.5) | 5 309 (48.2) |
| Deceased | 3 535 (67.8) | 2 178 (37.5) | 5 731 (51.2) |
| Deaths from AIDS | 2 159 (41.4) | 1 157 (19.9) | 3 316 (30.1) |
| Deaths from other causes | 1 376 (26.4) | 1 021 (17.6) | 2 397 (21.8) |
| Total | 5 216 (47.3) | 5 806 (52.7) | 11 022 (100) |
Note. HAART = highly active antiretroviral therapy.
All diseases except Pneumocystis carinii pneumonia and Kaposi's sarcoma.
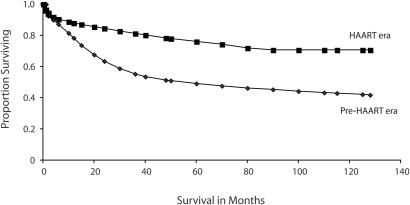
Cumulative adjusted 1-, 3-, and 5-year AIDS survival probabilities are shown in Table 2. Overall, 5-year survival improved from 49% in the pre-HAART era to 76% in the HAART era. Figure 1 shows adjusted AIDS survival curves in the pre-HAART and HAART eras. All groups experienced increases in AIDS survival across these 2 periods, but not all at the same rate.
TABLE 2.
Adjusted Probability Estimates of 1-, 3-, and 5-Year Survival Among Persons Diagnosed With AIDS Before and After the Introduction of Highly Active Antiretroviral Therapy: Chicago, 1993–2001
| Pre-HAART Era, 1993–1995 |
HAART Era, 1996–2001 |
|||||
| Characteristic | 1 Year | 3 Years | 5 Years | 1 Year | 3 Years | 5 Years |
| Gender | ||||||
| Male | 0.81 | 0.58 | 0.51 | 0.86 | 0.77 | 0.72 |
| Female | 0.78 | 0.55 | 0.49 | 0.88 | 0.82 | 0.77 |
| Race/ethnicity | ||||||
| Non-Hispanic Black | 0.78 | 0.54 | 0.46 | 0.87 | 0.79 | 0.73 |
| Non-Hispanic White | 0.79 | 0.56 | 0.52 | 0.90 | 0.86 | 0.83 |
| Hispanic | 0.80 | 0.59 | 0.55 | 0.88 | 0.83 | 0.79 |
| Mode of transmission | ||||||
| Male-to-male sexual contact | 0.77 | 0.53 | 0.48 | 0.90 | 0.85 | 0.81 |
| Injection drug use | 0.79 | 0.57 | 0.49 | 0.86 | 0.77 | 0.70 |
| Heterosexual contact | 0.85 | 0.59 | 0.53 | 0.90 | 0.83 | 0.78 |
| Age at diagnosis, y | ||||||
| 13–29 | 0.85 | 0.60 | 0.53 | 0.92 | 0.87 | 0.81 |
| 30–49 | 0.78 | 0.56 | 0.49 | 0.89 | 0.82 | 0.77 |
| ≥ 50 | 0.68 | 0.45 | 0.41 | 0.76 | 0.66 | 0.63 |
| Total | 0.78 | 0.55 | 0.49 | 0.88 | 0.81 | 0.76 |
Note. HAART = highly active antiretroviral therapy.
FIGURE 1.
Adjusted survival curves of AIDS patients in Chicago before (1993–1995) and after (1996–2001) the introduction of highly active antiretroviral therapy (HAART).
Table 3 shows adjusted hazard ratios for AIDS death and 95% confidence intervals by era for variables included in our final model, including gender, race/ethnicity, age, mode of transmission, and type of opportunistic disease. In almost every instance, the hazard ratio increased from the pre-HAART to the HAART era, implying disproportionate rates of improvement in AIDS survival times across eras.
TABLE 3.
Adjusted Hazard Ratios for Survival for Persons Diagnosed With AIDS Before and After the Introduction of Highly Active Antiretroviral Therapy: Chicago, 1993–2001
| Pre-HAART Era, 1993–1995 |
HAART Era, 1996–2001 |
|||
| Characteristic | HR (95% CI) | P | HR (95% CI) | P |
| Gender | ||||
| Male (Ref) | 1.00 | 1.00 | ||
| Female | 0.90 (0.79 , 1.03) | .12 | 1.20 (1.03, 1.40) | .02 |
| Race/ethnicity | ||||
| Non-Hispanic Black | 1.18 (1.06, 1.31) | <.01 | 1.51 (1.26, 1.80) | <.01 |
| Non-Hispanic White (Ref) | 1.00 | 1.00 | ||
| Hispanic | 0.94 (0.81, 1.09) | >.05 | 1.22 (0.97, 1.53) | .10 |
| Mode of transmission | ||||
| Male-to-male sexual contact (Ref) | 1.00 | 1.00 | ||
| Injection drug use | 0.94 (0.85, 1.04) | .22 | 1.30 (1.14, 1.49) | <.01 |
| Heterosexual contact | 0.89 (0.74, 1.08) | .25 | 0.94 (0.76, 1.16) | .54 |
| Age at diagnosis, y | ||||
| 13–29 (Ref) | 1.00 | 1.00 | ||
| 30–49 | 1.19 (1.05, 1.35) | .01 | 1.23 (1.02, 1.49) | .03 |
| ≥ 50 | 1.63 (1.38, 1.93) | <.01 | 2.28 (1.82, 1.49) | <.01 |
| Opportunistic diseases | ||||
| Pneumocystis carinii pneumonia (Ref) | 1.00 | 1.00 | ||
| Kaposi's sarcoma | 1.11 (0.79, 1.55) | .55 | 0.99 (0.53, 1.85) | .97 |
| Other | 1.15 (0.99, 1.33) | .07 | 1.50 (1.22, 1.86) | .01 |
| None | 0.50 (0.43, 0.59) | <.01 | 0.55 (0.44, 0.69) | <.01 |
Note. HAART = highly active antiretroviral therapy; HR = hazard ratio; CI = confidence interval. Cox regression model used to adjust for gender, race/ethnicity, mode of transmission, age at diagnosis, and opportunistic diseases.
After we adjusted for race/ethnicity, age, mode of transmission, and type of first opportunistic disease, we found that in the pre-HAART era, women were 10% less likely than were men to die from AIDS. However, in the HAART era, females were 20% more likely than were men to die from AIDS.
Similarly, in the pre-HAART era, the hazard of AIDS death was 18% greater for non-Hispanic Blacks and 6% lower for Hispanics than for non-Hispanic Whites. In the HAART era, however, the hazard of death for both non-Hispanic Blacks and Hispanics increased in comparison with the hazard for non-Hispanic Whites: non-Hispanic Blacks were 51% more likely to die and Hispanics were 22% more likely to die than were non-Hispanic Whites.
In both the pre-HAART and HAART eras, the hazard of death from AIDS increased with age at AIDS diagnosis. There was little difference in the hazard of death among persons aged 30 to 49 years and those aged 13 to 29 years by era, but the risk of AIDS death among persons aged 50 years and older compared with those aged 13 to 29 years increased considerably by era (Table 3). Persons 50 years and older were 63% more likely to die in the pre-HAART era and were 128% more likely to die in the HAART era than were those aged 13 to 29 years. There was no statistically significant difference in AIDS survival between heterosexuals or injection drug users and men who had sex with men in the pre-HAART era. In the HAART era, however, drug users were 30% more likely to die from AIDS than were men who had sex with men, after adjustment for gender, race/ethnicity, and age at AIDS diagnosis.
DISCUSSION
Our study showed increased survival times with AIDS in the HAART era compared with the pre-HAART era, a result that is consistent with the results of several similar analyses.5,25,26 Each group studied had improved 1-, 3- and 5-year survival rates from the pre-HAART era to the HAART era. These improvements were likely a result of increased provider recognition of and treatments for opportunistic diseases, particularly Pneumocystis carinii pneumonia and Mycobacterium avium complex. Also, AIDS diagnoses made earlier in the course of the disease, resulting from inclusion of immunologic criteria in the AIDS case definition, likely increased survival.1
Several studies have demonstrated increases in survival time as a result of opportunistic disease prophylaxis.6–8 A national study that used surveillance data to analyze AIDS survival found that the median survival time improved from 11 months for AIDS diagnoses made in 1984 to 46 months for AIDS diagnoses made in 1995.27–29 Another recent study demonstrated that treatment for Pneumocystis carinii pneumonia and Mycobacterium avium complex in 1993 to 1995 increased survival 24.4 months (2.0 years). Survival increased 93.7 months (7.8 years) among individuals from the earliest years of the study who survived long enough to receive HAART.30
Although our data indicated significant improvement in survival among all groups studied, the rate at which survival improved was not uniform. Furthermore, it was these differences in the rate of improvement that accounted for higher hazard rates in the HAART era. For example, the hazard of death among non-Hispanic Blacks compared with non-Hispanic Whites increased from 18% in the pre-HAART era to 51% in the HAART era. However, the disparity stemmed not from decreases in survival among non-Hispanic Blacks but from disproportionate gains in survival among non-Hispanic Whites, a disparity we also observed for other demographic characteristics. This pattern echoed patterns in survival observed in the early 1990s. A nationally representative study of persons with HIV showed that women and non-Hispanic Blacks received a lower quality of care than did other HIV-infected persons.31
Non-Hispanic Blacks were found to have poorer survival than Whites because they had more-advanced disease when they sought care and treatment; they also had less exposure to Pneumocystis carinii pneumonia prophylaxis.30 Of 9 studies published between 1985 and 1991, 4 found a decrease in survival for non-Hispanic Blacks compared with non-Hispanic Whites,29–35 4 found no difference in survival,33,36–38 and 1 found an increase in survival.33,39 In several of these studies, after control for socioeconomic differences, there was no difference found in survival by race/ethnicity.40
A survival analysis of HIV to AIDS progression from 1994 to 2005 showed that non-Hispanic Blacks and Hispanics were 45% more likely to progress to AIDS within 12 months than were non-Hispanic Whites. This suggests that nonHispanic Blacks may have been unaware of their HIV status longer, or entered primary care later, than non-Hispanic Whites.41 If non-Hispanic Whites were more likely to seek health care earlier in the course of their disease, there might have been more time to manage treatment effectively. It is not clear, however, to what degree, if any, delayed progression from HIV to AIDS among non-Hispanic Whites contributed to increases in survival. HIV reporting in Illinois began in 1999, which provided only 2 years of overlap with our data.
Limitations
A significant limitation to our study, and to other studies that have used surveillance data to estimate survival trends with AIDS, was the lack of individual-level data on the use of HAART and the lack of data on serial CD4 counts and viral loads. However, a study of persons with AIDS in New York City demonstrated that nearly three quarters of individuals treated at city clinics were receiving HAART by the end of 1997.28 This suggests that the recommended guidelines were followed by a majority of providers treating patients with HIV/AIDS.2
We did not have sufficient data on Asian Americans, Pacific Islanders, American Indians, or Alaskan Natives to include in our study. In addition, because of significant delays in processing electronic death files, it was difficult to establish the causes of death according to the ICD-10 codes. We were unable to extend follow-up time beyond 2003. More recent survival data would allow for better estimates of the hazard of death in the HAART era.
Conclusions
We found significantly increased survival with AIDS in the HAART era compared with the pre-HAART era. All groups we studied had improved survival rates, although not all groups benefited to the same extent. Differential rates in improvement, rather than increased morbidity and mortality, explain the disparities in the hazard ratios by race/ethnicity across eras. These findings have significant implications for prevention and care organizations: rather than focusing on the reasons for disparities, examining protective factors in non-Hispanic Whites and emulating them in other populations may prove more effective. In Chicago, for example, a useful strategy may be to assess protective factors in both Blacks and Whites and tailor interventions that will extend these protections to the Hispanic population.
Enhancing existing efforts to prevent HIV-infected individuals from infecting susceptible individuals and developing new interventions to increase early recognition of disease and to remove barriers to accessing care will help Chicago's disadvantaged population to achieve even greater increases in survival. In addition, effective community-level interventions to reduce health disparities require public engagement and support, but the frequency and appropriateness of media coverage of disparities are inadequate, despite a growing body of academic literature.42 This is another issue that should be addressed in intervention development and planning.
Acknowledgments
The authors gratefully thank C. Kempler for her assistance with matching the AIDS surveillance data with the death files.
Note. The findings and conclusions in this article are those of the authors and do not necessarily represent the view of the Chicago Department of Public Health.
Human Participant Protection
No protocol approval was needed for this study.
References
- 1.Centers for Disease Control and Prevention 1993 revised classification system for HIV infection and expanded surveillance definition for AIDS among adolescents and adults. MMWR Recomm Rep. 1992;41(RR-17):1–19 [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention USPHS/IDSA guidelines for the prevention of opportunistic infections in persons infected with human immunodeficiency virus: a summary. MMWR Recomm Rep. 1995;44(RR-8):1–34 [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention Guidelines for the use of antiretroviral agents in HIV-infected adults and adolescents. MMWR Recomm Rep. 1998;47(RR-5):43–82 [PubMed] [Google Scholar]
- 4.Porter K, Babiker A, Bhaskaran K, et al. Determinants of survival following HIV-1 serovconversion after the introduction of HAART. Lancet. 2003;362:1267–1274 [DOI] [PubMed] [Google Scholar]
- 5.Lee LM, Karon JM, Selik R, Neal JJ, Fleming PL. Survival after AIDS diagnosis in adolescent and adults during the treatment era, United States, 1984–1997. JAMA. 2001;285:1308–1315 [DOI] [PubMed] [Google Scholar]
- 6.Pallela FJ, Delaney KM, Moorman AC, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. N Engl J Med. 1998;338:853–860 [DOI] [PubMed] [Google Scholar]
- 7.Pezzotti P, Napoli PA, Acciai S, et al. Increasing survival time after AIDS in Italy: the role of new combination antiretroviral therapies. AIDS. 1999;13(2):249–255 [DOI] [PubMed] [Google Scholar]
- 8.McNaghten AD, Hanson DL, Jones JL, Dworkin MS, Ward JW. Effects of antiretroviral therapy and opportunistic illness primary chemoprophylaxis on survival after AIDS diagnosis. AIDS. 1999;13:1687–1695 [DOI] [PubMed] [Google Scholar]
- 9.Vittinghoff E, Scheer S, O'Malley P, Colfax G, Holmberg SD, Buchbinder SP. Combination antiretroviral therapy and recent declines in AIDS incidence and mortality. J Infect Dis. 1999;179:717–720 [DOI] [PubMed] [Google Scholar]
- 10.Detels R, Munoz A, McFarlane G, et al. Effectiveness of potent antiretroviral therapy on time to AIDS and death in men with known HIV infection duration. JAMA. 1998;280:1497–1503 [DOI] [PubMed] [Google Scholar]
- 11.Harper DM, Thomas SD. Leading Causes of Death in Chicago 1989–1999. Chicago, IL: Chicago Department of Public Health Epidemiology Program; 2002 [Google Scholar]
- 12.Minino AM, Arias E, Kochanek KD, Murphy SL, Smith BL. Deaths: final data for 2000. Natl Vital Stat Rep. 2002;50(15):1–119 [PubMed] [Google Scholar]
- 13.Hoyert DL, Arias E, Smith BL, Murphy SL, Kochanek KD. Final data for 1999. Natl Vital Stat Rep. 2001;49(8):1–113 [PubMed] [Google Scholar]
- 14.Murphy SL. Deaths: Final data for 1998. Natl Vital Stat Rep. 2000;48(11):1–105 [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention Slidesets. Available at: http://www.cdc.gov/hiv/graphics/images/l285/l285–4.htm. Accessed June 1, 2007
- 16.Steinberg S, Fleming P. The geographic distribution of AIDS in the United States: is there a rural epidemic? J Rural Health. 2000;16(1):11–19 [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention Pneumocystis pneumonia—Los Angeles. MMWR Morb Mortal Wkly Rep. 1981;30:250–252 [PubMed] [Google Scholar]
- 18.STD/HIV/AIDS Chicago—Winter 2006. Chicago, IL: Office of HIV/AIDS Surveillance; 2007 [Google Scholar]
- 19.Osborn CY, Paasche-Orlow MK, Davis TC, et al. Health literacy: an overlooked factor in understanding HIV health disparities. Am J Prev Med. 2007;33(5):374–378 [DOI] [PubMed] [Google Scholar]
- 20.Darling-Hammond L. Brookings Institution. Unequal opportunity: race and education. Available at: http://www.brookings.edu/articles/1998/spring_education_darling_hammond.aspx. Accessed February 1, 2008
- 21. Ill. Admin. Code tit 77, §693 (2001). Also available at: http://www.ilga.gov/commission/jcar/admincode/077/077006930000200R.html. Accessed June 1, 2007.
- 22.US Bureau of the Census. 2000 Census: Internet release, April 2, 2001. Available at: http://factfinder.census.gov/servlet/DTSubjectShowTablesServlet?_ts=228058750543. Accessed February 1, 2007 [Google Scholar]
- 23.Manual of the International Statistical Classfication of Diseases, Injuries, and Causes of Death, Ninth Revision. Geneva, Switzerland: World Health Organization; 1977 [Google Scholar]
- 24.International Statistical Classification of Diseases and Related Health Problems, 10th Revision. Geneva, Switzerland: World Health Organization; 1992 [Google Scholar]
- 25.Karon JM, Rosenberg PS, McQuillan G, et al. Prevalence of HIV infection in the United States, 1984 to 1992. JAMA. 1996;276:126–131 [PubMed] [Google Scholar]
- 26.Lemp GF, Payne SF, Neal D, Temelso T, Rutherford GW. Survival trends for patients with AIDS. JAMA. 1990;263(3):492–496 [PubMed] [Google Scholar]
- 27.Rothenberg R, Woelfel M, Stoneburner R, Milberg J, Parker R, Truman B. Survival with the acquired immunodeficiency syndrome. Experience with 5833 cases in New York City. N Engl J Med. 1987;317:1297–1302 [DOI] [PubMed] [Google Scholar]
- 28.Blum S, Tejinder PS, Gibbons J, et al. Trends in survival among persons with acquired immunodeficiency syndrome in New York City. The experience of the first decade of the epidemic. Am J Epidemiol. 1994;139(4):351–361 [DOI] [PubMed] [Google Scholar]
- 29.Chang HG, Morse DL, Noonan C. Survival and mortality patterns of an acquired immunodeficiency syndrome (AIDS) cohort in New York State. Am J Epidemiol. 1992;138:341–349 [DOI] [PubMed] [Google Scholar]
- 30.Walensky RP, Paltiel AD, Losina E, et al. The survival benefits of AIDS treatment in the United States. J Infect Dis. 2006;194:11–19 [DOI] [PubMed] [Google Scholar]
- 31.Easterbrook PJ, Keruly J, Creagh-Kirk T, Richman DD, Chaisson RE, Moore RD. Racial and ethnic differences in outcome in zidovudine -treated patients with advanced HIV disease. Zidovudine Epidemiology Study Group. JAMA. 1991;266(19):2713–2718 [PubMed] [Google Scholar]
- 32.King WD, Wong MD, Shapiro MF, Landon BE, Cunningham WE. Does racial concordance between HIV positive patients and their physicians affect the time to receipt of protease inhibitors? J Gen Intern Med. 2004;19(11):1146–1153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Curtis JR, Patrick DL. Race and survival time with AIDS: a synthesis of the literature. Am J Public Health. 1993;83:1425–1428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moore RD, Hidalgo J, Sugland BW, Chaison RE. Zidovudine and the natural history of the acquired immunodeficiency syndrome. N Engl J Med. 1991;324:1412–1416 [DOI] [PubMed] [Google Scholar]
- 35.Harris JE. Improved short-term survival of AIDS patients initially diagnosed with Pneumocystis carinii pneumonia, 1984 through 1987. JAMA. 1990;263(3):397–401 [PubMed] [Google Scholar]
- 36.Creagh-Kirk T, Doi P, Andrews E, et al. Survival experience among patients with AIDS receiving zidovudinc: follow-up of patients in a compassionate plea program. JAMA. 1988;260:3009–3015 [PubMed] [Google Scholar]
- 37.Lagakos S, Fischl MA, Stein DS, Lim L, Volberding P. Effects of zidovudine therapy in minority and other subpopulations with early HIV infection. JAMA. 1991;266:2709–2712 [PubMed] [Google Scholar]
- 38.Justice A, Feinstein AR, Wells CK. A new prognostic staging system for the acquired immunodeficiency syndrome. N Engl J Med. 1989;20:1388–1393 [DOI] [PubMed] [Google Scholar]
- 39.Friedland GH, Saltzman B, Vileno J, Freeman K, Schrager LK, Klein RS. Survival differences in patients with AIDS. J Acquir Immune Defic Synd. 1991;4:144–153 [PubMed] [Google Scholar]
- 40.Chaisson RE, Keruly JC, Moore RD. Race, gender, drug use, and progression of human immunodeficiency virus disease. N Engl J Med. 1995;333(12):751–756 [DOI] [PubMed] [Google Scholar]
- 41.Christiansen D, Benbow N. Race/Ethnicity and Time From HIV Diagnosis to AIDS, Chicago, 1999–2005. Presented at: Annual Conference of State and Territorial Epidemiologists, Atlantic City, New Jersey, June 24–28, 2007 [Google Scholar]
- 42.Amzel A, Ghosh C. National newspaper coverage of minority health disparities. J Natl Med Assoc. 2007;99(10):1120–1125 [PMC free article] [PubMed] [Google Scholar]