Abstract
Objectives
To determine whether problem solving treatment combined with antidepressant medication is more effective than either treatment alone in the management of major depression in primary care. To assess the effectiveness of problem solving treatment when given by practice nurses compared with general practitioners when both have been trained in the technique.
Design
Randomised controlled trial with four treatment groups.
Setting
Primary care in Oxfordshire.
Participants
Patients aged 18-65 years with major depression on the research diagnostic criteria—a score of 13 or more on the 17 item Hamilton rating scale for depression and a minimum duration of illness of four weeks.
Interventions
Problem solving treatment by research general practitioner or research practice nurse or antidepressant medication or a combination of problem solving treatment and antidepressant medication.
Main outcome measures
Hamilton rating scale for depression, Beck depression inventory, clinical interview schedule (revised), and the modified social adjustment schedule assessed at 6, 12, and 52 weeks.
Results
Patients in all groups showed a clear improvement over 12 weeks. The combination of problem solving treatment and antidepressant medication was no more effective than either treatment alone. There was no difference in outcome irrespective of who delivered the problem solving treatment.
Conclusions
Problem solving treatment is an effective treatment for depressive disorders in primary care. The treatment can be delivered by suitably trained practice nurses or general practitioners. The combination of this treatment with antidepressant medication is no more effective than either treatment alone.
Key messages
Problem solving treatment is an effective treatment for depressive disorders in primary care
Problem solving treatment can be delivered by suitably trained practice nurses as effectively as by general practitioners
The combination of problem solving treatment and antidepressant medication is no more effective than either treatment alone
Problem solving treatment is most likely to benefit patients who have a depressive disorder of moderate severity and who wish to participate in an active psychological treatment
Introduction
Depressive disorders are common in primary care, the prevalence of both major and minor depression being 5%.1 Although antidepressant medication is both convenient and effective, there is considerable demand from patients for psychological treatment.2 Problem solving treatment has been developed in primary care as a brief (six session) structured psychological treatment that can be delivered by members of the primary healthcare team.
In primary care problem solving treatment has been shown to be effective for emotional disorders of poor prognosis3 and for major depression.4 The treatment has been shown to be effective when given by general practitioners, and community nurses can be trained in problem solving techniques.5
We examined whether a combination of problem solving treatment with antidepressant medication is more effective than either treatment alone. We also studied the effectiveness of problem solving treatment given by practice nurses compared with general practitioners when both have been trained in the technique.
Methods
Patients were recruited from the lists of 24 general practitioners working in Oxfordshire between May 1994 and September 1996.
Design
A randomised, controlled clinical trial was carried out to compare four treatments for major depression in primary care: problem solving treatment given by research general practitioners; problem solving treatment given by research practice nurses; antidepressant medication given by research general practitioners; and combined problem solving treatment and antidepressant medication. We chose a selective serotonin reuptake inhibitor as the antidepressant because this class of drug is widely used in primary care.
In calculating the sample size we chose the Hamilton rating scale for depression as the main outcome measure. The SD in a previous sample of patients with depressive disorder in primary care was 4.2.6 Assuming a clinically significant difference of 3 on the scale, we calculated that a sample size of 160 (that is, 40 per group) would result in a power of 0.90 at 5% significance based on comparisons of two groups at a time.
Selection criteria
General practitioners were asked to refer patients aged 18 to 65 years whom they judged to have a depressive disorder that required treatment but not urgent hospital referral. Patients were assessed within 48 hours to determine whether they met the inclusion criteria: probable or definite major depression on the research diagnostic criteria7; a score of 13 or above on the 17 item Hamilton rating scale for depression8; and a minimum duration of illness of four weeks.
Patients were excluded if they had an additional psychiatric disorder preceding the onset of depression; were receiving concurrent treatment with antidepressant medication or a psychological treatment, or both (patients had not to have taken any antidepressant drugs for at least a month); had brain damage, learning difficulties,schizophrenia, drug dependence, recent alcohol abuse, or physical illness precluding antidepressant medication; or had a clinical state inconsistent with participation in the research protocol—for example, psychotic features or serious suicidal intent.
Assignment
Patients were randomised individually to receive one of the four treatments after giving informed consent to participation in the study. Allocation to treatment group was made by a research worker, separate from both the assessors and therapists, using cards in sealed envelopes. The allocation schedule was generated by using a list of random numbers. Randomisation was stratified to ensure that all treatment groups included patients with depressive disorders of equivalent severity and chronicity.
Treatments
Treatment was usually given in the patient's home or local health centre. Patients in the three single treatment groups were offered six treatment sessions over 12 weeks (weeks 1, 2, 3, 5, 7, and 11). In the combined treatment group patients were offered six treatment sessions for drug treatment by the research general practitioner together with six problem solving treatment sessions by the research practice nurse. In all treatment groups one extra treatment session could be offered if the therapist thought it clinically necessary.
At the end of the 12 weeks' treatment patients were referred back to their general practitioners. For patients on medication the general practitioners were advised that if medication had been helpful it should be continued for a further four months before cautious withdrawal was considered.
Problem solving treatment
Problem solving treatment was given either by one of three research general practitioners or by one of two research practice nurses. Problem solving treatment focuses on the here and now and helps patients use their own skills and resources to function better. It is explained to patients that their psychological symptoms may be linked to psychosocial problems that they are facing. If these problems can be resolved the symptoms may improve. Problem solving occurs in the following stages:
Clarification and definition of problems
Choice of achievable goals
Generation of solutions
Choice of preferred solutions
Implementation of preferred solutions
Evaluation.6
The first treatment session lasts one hour, with subsequent sessions lasting 30 minutes. The treatment was set out in a treatment manual and was supervised by an experienced problem solving therapist (LMM-W).
Drug treatment
Drug treatment was given by the research general practitioners. Patients received either fluvoxamine (initial dose 100 mg) or paroxetine (initial dose 20 mg). Fluvoxamine was initially chosen for the study but a change to paroxetine was made because of its more widespread use in primary care. Drug treatment was given according to a treatment manual based on the manual used in the National Institute of Mental Health's collaborative research programme on treatment of depression.9 The aim of the drug treatment was to encourage patients' compliance with medication in a supportive and encouraging framework but with avoidance of specific psychological interventions. The dose could be varied according to the patient's clinical state. Compliance with medication was assessed by a count of returned pills.
Combined treatment
In the group allocated to combined treatment patients were given medication by the research general practitioner as if they were receiving medication alone. In addition, these patients saw one of the research practice nurses for the provision of problem solving treatment.
Assessments of outcome
Patients were assessed on four occasions: before treatment and at 6, 12, and 52 weeks. The assessments were made by one of two experienced research interviewers who were blind to the type of treatment given.
Four main outcome measures were recorded at each assessment. Two were rated by the interviewer: the clinical interview schedule (revised)—a measure of psychological symptoms developed for use in primary care10—and the Hamilton rating scale for depression8—a measure of the severity of depression. Two outcome measures were rated by the patient: the Beck depression inventory11—a measure of severity of depression—and the modified social adjustment scale12—a measure of social functioning.
Methods of analysis
The data were analysed with spss for Windows (version 7.5). To determine the efficacy of the four treatments, analyses of variance were computed for the four main outcome measures. An intention to treat analysis was used, with the last available result carried forward as necessary.
To determine the effects of the treatments in producing clinical recovery at the end of treatment (12 weeks) we performed an intention to treat Pearson χ2 analysis of the proportion of patients who had recovered. Patients were deemed to have clinically recovered if their score on the Hamilton rating scale for depression was 7 or less; patients with scores of 8-12 were deemed partially recovered; and patients with scores of 13 or more were deemed not recovered.13
Results
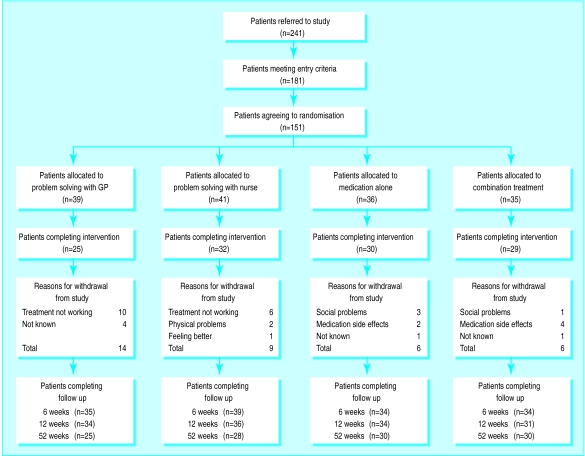
The figure shows a trial profile of the patients referred to the study. Sixty patients did not meet the entry criteria (largely because the depression was not of sufficient severity). A further 30 were eligible but refused because they thought the study would not help (16), did not want medication (eight), were feeling better (three), were moving (two), or thought there were too many questions (one). This left 151 patients who met the entry criteria (144 with definite and seven with probable major depression) and agreed to randomisation. There were no significant differences in age, sex, and severity of depression between eligible patients who agreed to participate in the study and those who did not. The demographic and clinical characteristics of the treatment groups at baseline are shown in table 1.
Table 1.
Demographic and clinical features of treatment groups at baseline. Figures are numbers (percentage) of patients unless stated otherwise
| Patient characteristics | Problem solving (GP) (n=39) | Problem solving (nurse) (n=41) | Medication (n=36) | Combination treatment (n=35) | Total sample (n=151) |
|---|---|---|---|---|---|
| Mean (range) age (years) | 36 (20-58) | 33 (21-46) | 34 (19-58) | 35 (19-62) | 35 ( 19-62) |
| Women | 33 | 28 | 31 | 24 | 116 |
| Married or cohabiting | 19 (49) | 21 (51) | 17 (47) | 18 (51) | 75 (50) |
| Employed/studying | 27 (69) | 35 (85) | 26 (72) | 25 (71) | 113 (75) |
| Social class I, II, IIIa | 26 (67) | 34 (83) | 23 (64) | 22 (63) | 99 (66) |
| Education after 16 years | 14 (36) | 16 (41) | 9 (25) | 8 (23) | 47 (31) |
| White | 38 (98) | 39 (95) | 32 (89) | 34 (97) | 143 (95) |
| Duration of depression >6 months | 13 (33) | 13 (32) | 12 (33) | 13 (37) | 51 (34) |
| Previous episode of depression requiring treatment | 24 (62) | 24 (58) | 19 (53) | 19 (54) | 84 (55) |
| Family history of depression | 13 (33) | 21 (51) | 18 (50) | 16 (46) | 68 (45) |
| Saw psychiatrist before study | 6 (16) | 5 (12) | 5 (14) | 8 (23) | 24 (16) |
Treatment received
Of the 151 patients who entered the trial, 116 (77%) completed the full course of treatment. Patients receiving problem solving treatment alone had a mean number of 4.6 treatment sessions (range 1-7); patients receiving combination treatment had a mean number of 5.2 problem solving treatment sessions (range 1-7). Patients receiving medication did so for a mean number of 10.7 weeks (range 2-12). Two patients received fluvoxamine at a final dose of 150 mg and five patients at a final dose of 100 mg. Two patients received paroxetine at a final dose of 10 mg, 46 at 20 mg, 15 at 30 mg, and one at 40 mg.
Outcome
Table 2 shows the results at baseline and at 6 weeks, 12 weeks, and 52 weeks for all patients for whom results were available on the four main outcome measures. All four groups improved during treatment. There were no significant differences between the four treatment groups at 6, 12, or 52 weeks. Table 3 shows the numbers of patients who recovered in each group at 12 and 52 weeks according to the predetermined recovery. There was no significant difference in outcome at either point.
Table 2.
Mean scores on four main outcome scales at baseline and 6, 12, and 52 weeks after treatment
| Outcome measures (No for whom data available) | Mean scores (95% CI)
|
P value | |||
|---|---|---|---|---|---|
| Problem solving (GP) | Problem solving (nurse) | Medication alone | Combination | ||
| Hamilton rating scale for depression: | |||||
| Baseline (151) | 20.5 (18.9 to 22.1) | 20.5 (19.1 to 21.9) | 20.2 (19.1 to 21.4) | 19.8 (18.5 to 21.1) | 0.90 |
| 6 weeks (139) | 12.7 (10.4 to 15.1) | 10.4 (8.1 to 12.8) | 10.7 (8.2 to 13.2) | 10.8 (8.5 to 13.1) | 0.48 |
| 12 weeks (135) | 8.5 (5.8 to 11.2) | 8.7 (6.1 to 11.3) | 6.2 (3.7 to 8.6) | 7.5 (5.2 to 9.9) | 0.47 |
| 52 weeks (113) | 5.8 (2.7 to 8.8) | 5.9 (3.4 to 8.3) | 7.2 (5.1 to 9.2) | 5.7 (3.4 to 7.9) | 0.77 |
| Beck depression inventory: | |||||
| Baseline (151) | 29.1 (26.4 to 31.8) | 30.3 (27.9 to 32.8) | 30.2 (27.7 to 32.7) | 30.0 (27.3 to 32.6) | 0.89 |
| 6 weeks (142) | 19.7 (16.2 to 23.2) | 16.1 (12.5 to 19.6) | 15.1 (10.9 to 19.3) | 16.3 (12.9 to 19.7) | 0.30 |
| 12 weeks (135) | 12.2 (8.3 to 16.2) | 13.0 (9.4 to 16.7) | 11.8 (7.8 to 15.8) | 9.3 (6.6 to 12.0) | 0.51 |
| 52 weeks (113) | 9.6 (4.6 to 14.7) | 11.5 (6.8 to 16.2) | 11.5 (6.9 to 16.2) | 8.6 (5.3 to 11.9) | 0.71 |
| Clinical interview schedule: | |||||
| Baseline (151) | 29.6 (27.4 to 31.9) | 28.6 (26.6 to 30.7) | 29.3 (27.3 to 31.2) | 29.0 (26.5 to 31.5) | 0.93 |
| 6 weeks (139) | 19.0 (15.4 to 22.7) | 16.4 (12.7 to 20.0) | 14.0 (10.1 to 17.9) | 14.0 (10.8 to 17.3) | 0.16 |
| 12 weeks (135) | 12.4 (8.1 to 16.6) | 11.9 (8.2 to 15.7) | 9.8 (6.1 to 13.5) | 9.6 (6.3 to 12.9) | 0.62 |
| 52 weeks (n =113) | 8.2 (3.8 to 12.5) | 8.6 (4.6 to 12.6) | 11.5 (7.3 to 15.6) | 9.7 (5.9 to 13.6) | 0.65 |
| Social adjustment scale: | |||||
| Baseline (151) | 2.8 (2.6 to 2.9) | 3.0 (2.9 to 3.1) | 2.9 (2.7 to 3.0) | 2.9 (2.7 to 3.1) | 0.17 |
| 6 weeks (139) | 2.3 (2.2 to 2.5) | 2.4 (2.2 to 2.6) | 2.3 (2.0 to 2.5) | 2.3 (2.1 to 2.5) | 0.90 |
| 12 weeks (127) | 2.1 (1.8 to 2.3) | 2.2 (2.0 to 2.4) | 2.0 (1.8 to 2.3) | 1.9 (1.7 to 2.1) | 0.38 |
| 52 weeks (105) | 1.8 (1.6 to 2.0) | 2.0 (1.8 to 2.2) | 2.1 (1.8 to 2.3) | 1.9 (1.7 to 2.1) | 0.40 |
Table 3.
Number (%) of patients recovered at end of treatment (12 weeks) and at 52 week follow up
| Recovery | Problem solving (GP)
|
Problem solving (nurse)
|
Medication alone
|
Combination
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 12 weeks | 52 weeks | 12 weeks | 52 weeks | 12 weeks | 52 weeks | 12 weeks | 52 weeks | ||||
| Recovered (Hamilton ⩽7) | 20 (51) | 24 (62) | 22 (54) | 23 (56) | 24 (67) | 20 (56) | 21 (60) | 23 (66) | |||
| Partially recovered (Hamilton 8-12) | 5 (13) | 6 (15) | 6 (15) | 8 (20) | 4 (11) | 9 (25) | 5 (14) | 5 (14) | |||
| Not recovered (Hamilton ⩾13) | 14 (32) | 9 (23) | 13 (32) | 10 (24) | 8 (22) | 7 (19) | 9 (26) | 7 (21) | |||
Discussion
An important finding from this study is the lack of any significant difference between the four treatment groups. From this we drew two conclusions. Firstly, the combination of problem solving treatment and antidepressant medication is no more effective than either treatment alone. Secondly, there is no difference in outcome if the problem solving treatment is given by a suitably trained general practitioner or by a suitably trained practice nurse.
A second important finding is that patients in all groups showed a notable improvement over the 12 week treatment period. This improvement was maintained in all groups at the 52 week follow up. In the absence of a placebo group it is necessary to compare the proportion of patients recovered in this study with those in other studies. Detailed meta-analyses of the efficacy of treatments for depression in primary care were published by the depression guideline panel in the United States.14 In these analyses the percentage of patients with major depression who have recovered after 12 weeks of treatment are as follows: selective serotonin reuptake inhibitors 47%, behavioural therapy 55%, cognitive psychotherapy 47%, and combination therapies 35%-54%. In a previous study that evaluated the use of problem solving treatment for major depression in primary care, 27% of patients recovered in the placebo group.4
This study provides follow up data at 52 weeks, which is longer than most follow up periods for depressive disorder in primary care. The follow up was naturalistic, and general practitioners were free to provide whatever treatment was appropriate for their patients.Only about two thirds of patients overall were fully recovered at a year whatever treatment had been given. These results provide evidence that depressive disorders in primary care may be of lengthy duration even with appropriate treatment.
The nurses in this study were experienced problem solving therapists who had participated in a previous study that evaluated problem solving treatment. The general practitioners received theoretical training in problem solving treatment from an experienced therapist and then treated five patients under supervision before starting the trial. It may be that the results achieved by such a research team would be better than those in routine general practice.
When should problem solving treatment be given?
The results of this study provide further evidence that problem solving treatment is effective for the treatment of depressive disorders in primary care. An important clinical question needs to be answered: what is the place for problem solving treatment among other treatments for depressive disorders in primary care? How should the general practitioner choose between problem solving treatment and antidepressant medication or between problem solving treatment and alternative psychological treatments?
The provision of any psychological treatment depends on the availability of suitably trained therapists. Although problem solving is a simple treatment, therapists need both theoretical and practical training before they can be deemed competent in its delivery. At present most general practitioners do not have time to offer problem solving treatment themselves nor do they have access to a suitably trained therapist. If general practitioners are to have a meaningful alternative to antidepressant medication in the treatment of depressive disorders there will need to be an investment in the training of problem solving therapists. A training package for use by practice nurses has been evaluated.5 Patient preference is important; they should be willing to participate actively in a collaborative treatment process.
The severity of the depression is probably also important. In our experience, although some patients with quite severe depressive disorders can be successfully treated with problem solving treatment,15 it is more difficult to treat patients in whom poor concentration and lack of motivation are important components of their illness. Thus problem solving is probably more suitable for moderate depressive disorders than for the more severe illnesses.
Conclusions
Problem solving treatment is a goal orientated, collaborative, and active process and focuses on the here and now. Patients gain a clear sense of involvement in the process of recovery. Problem solving treatment is suitable for primary care because it is relatively brief and can be delivered by primary care nurses. The first challenge for the future is to provide training for interested practice nurses in delivering the treatment as evaluated. Secondly, a briefer adaptation of problem solving techniques that can be used by the general practitioners in their regular consultations needs to be evaluated.
Figure.
Trial profile in study of treatment of depression in primary care
Acknowledgments
We are grateful to our therapists—Julie Wiseman, Nicole Coulon, Sandra Harrison, and Khalida Quereshi—and our research interviewers—Adrienne Garrod and Alison Bond. We are particularly grateful to the general practitioners who referred patients into the study and of course the patients who took part.
Footnotes
Funding: Medical Research Council.
Competing interests: None declared.
References
- 1.Blacker CVR, Clare AW. The prevalence and treatment of depression in general practice. Psychopharmacology. 1998;95:S14–S17. doi: 10.1007/BF00172624. [DOI] [PubMed] [Google Scholar]
- 2.Priest RG, Vize C, Roberts A, Tylee A. Lay people's attitudes to treatment of depression. BMJ. 1996;313:838–859. doi: 10.1136/bmj.313.7061.858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Catalan J, Gath DH, Bond A, Day A, Hall L. Evaluation of a brief psychological treatment for emotional disorders in primary care. Psychol Med. 1991;21:1013–1018. doi: 10.1017/s0033291700030002. [DOI] [PubMed] [Google Scholar]
- 4.Mynors-Wallis LM, Gath DH, Lloyd-Thomas A, Tomlinson D. Randomised controlled trial comparing problem solving treatment with amitriptyline and placebo for major depression in primary care. BMJ. 1995;310:441–445. doi: 10.1136/bmj.310.6977.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mynors-Wallis LM, Davies I, Gray A, Gath DH, Barbour F. Randomised controlled trial and cost analysis of problem-solving treatment for emotional disorders by community nurses in primary care. Br J Psychiatry. 1997;170:113–119. doi: 10.1192/bjp.170.2.113. [DOI] [PubMed] [Google Scholar]
- 6.Gath DH, Mynors-Wallis LM. Problem-solving treatment in primary care. In: Clark DM, Fairburn CG, editors. Science and practice of cognitive behaviour therapy. Oxford: Oxford University Press; 1997. [Google Scholar]
- 7.Spitzer RL, Endicott V, Robins E. Research diagnostic criteria: rationale and reliability. Arch Gen Psychiatry. 1978;36:773–782. doi: 10.1001/archpsyc.1978.01770300115013. [DOI] [PubMed] [Google Scholar]
- 8.Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6:278–296. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- 9.Fawcett J, Epstein P, Fiester SJ, Ellan I, Autry J. Clinical management. Imipramine/placebo administration manual. Psychopharmacol Bull. 1987;23:309–324. [PubMed] [Google Scholar]
- 10.Lewis G, Pelosi AJ. Measuring psychiatric disorder in the community. A standardised assessment for use by lay interviewers. Psychol Med. 1982;22:465–486. doi: 10.1017/s0033291700030415. [DOI] [PubMed] [Google Scholar]
- 11.Beck AT, Ward CH, Mendelson M. An inventory for measuring depression. Arch Gen Psychiatry. 1962;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 12.Cooper P, Osborn M, Gath DH, Feggetter G. Evaluation of a modified self-report measure of social adjustment. Br J Psychiatry. 1982;141:68–75. doi: 10.1192/bjp.141.1.68. [DOI] [PubMed] [Google Scholar]
- 13.Frank E, Prien RF, Jarrett RB, Keller MB, Kupfer DJ, Lavori PW, et al. Conceptualization and rationale for consensus definitions of terms in major depressive disorder: remission, recovery, relapse, and recurrence. Arch Gen Psychiatry. 1991;48:851–855. doi: 10.1001/archpsyc.1991.01810330075011. [DOI] [PubMed] [Google Scholar]
- 14.Depression Guideline Panel. Depression in primary care. 2. Treatment of major depression. Rockville, MD: US Department of Health and Human Services; 1993. (Clinical practice guidelines No 5). [Google Scholar]
- 15.Mynors-Wallis LM, Gath DH. Predictors of treatment outcome for major depression in primary care. Psychol Med. 1997;27:731–736. doi: 10.1017/s0033291796004126. [DOI] [PubMed] [Google Scholar]