Abstract
Mindfulness meditation training has stress reduction benefits in various patient populations, but its effects on biological markers of HIV-1 progression are unknown. The present study tested the efficacy of an 8-week Mindfulness-based stress reduction (MBSR) meditation program compared to a 1-day control seminar on CD4+ T lymphocyte counts in stressed HIV infected adults. A single-blind randomized controlled trial was conducted with enrollment and follow-up occurring between November 2005 and December 2007. A diverse community sample of 48 HIV-1 infected adults was randomized and entered treatment in either an 8-week MBSR or a 1-day control stress reduction education seminar. The primary outcome was circulating counts of CD4+ T lymphocytes. Participants in the 1-day control seminar showed declines in CD4+ T lymphocyte counts whereas counts among participants in the 8-week MBSR program were unchanged from baseline to post-intervention (time × treatment condition interaction, p = .02). This effect was independent of antiretroviral (ARV) medication use. Additional analyses indicated that treatment adherence to the mindfulness meditation program, as measured by class attendance, mediated the effects of mindfulness meditation training on buffering CD4+ T lymphocyte declines. These findings provide an initial indication that mindfulness meditation training can buffer CD4+ T lymphocyte declines in HIV-1 infected adults.
Keywords: Mindfulness, Meditation, HIV, AIDS, Mindfulness-based stress reduction, Stress, Intervention, CD4
1. Introduction
Although great advances have been made in antiretroviral (ARV) treatment of HIV-1 infection, there is still variability in treatment outcome (May et al., 2006). Psychological stress may account for some of this variability, as animal and human studies have demonstrated that stress accelerates HIV-1 disease pathogenesis and impairs the biological impact of ARV treatment (for review, see Cohen et al., 2007; Cole et al., 2001; Ironson et al., 2005). Consistent with this, recent studies indicate that behavioral stress management interventions may improve biological indicators of HIV-1 pathogenesis (Antoni et al., 2006; Petrie et al., 2004, cf. Crepaz et al., 2008), but it is unknown whether mindfulness meditation impacts HIV-1 progression (Ospina et al., 2007; Robinson et al., 2003).
The Mindfulness-based stress reduction (MBSR) program (Kabat-Zinn, 1982) is a standardized and manualized 8-week mindfulness meditation training intervention that has been shown to reduce stress and improve self-reported health outcomes in a variety of patient populations (Brown et al., 2007). In the MBSR program, participants practice a series of guided mindfulness meditation exercises in weekly classes and at home daily (e.g., body awareness, mindful stretching, sitting meditation, and mindfulness in daily life practices). It is thought that the MBSR program helps participants bring a more open and receptive awareness to their present moment experiences in daily life, facilitating a greater recognition and regulation of stress (Brown et al., 2007). Currently, few investigations have examined the effects of MBSR on immune outcomes or biological stress pathways, but initial studies in this area indicate that MBSR may have salutary effects on antibody titer response to influenza vaccination (Davidson et al., 2003), cytokine signaling in cancer patients (Carlson et al., 2007, 2003), and NK cell numbers and cytotoxic activity in HIV patients (Robinson et al., 2003). Further, some recent evidence suggests that MBSR may reduce total daily salivary cortisol output at follow-up (Carlson et al., 2007), an effect that may be consistent with stress reduction. An initial pilot study of MBSR in HIV-1 indicated that mindfulness meditation training can impact immune system function (Robinson et al., 2003), but did not assess markers of HIV-1 pathogenesis, such as CD4+ T lymphocytes and HIV viral load. Thus, a single blind randomized controlled trial was conducted to test whether an 8-week MBSR program buffers CD4+ T lymphocyte declines in a community sample of HIV-1 infected adults.
2. Methods
2.1. Participants
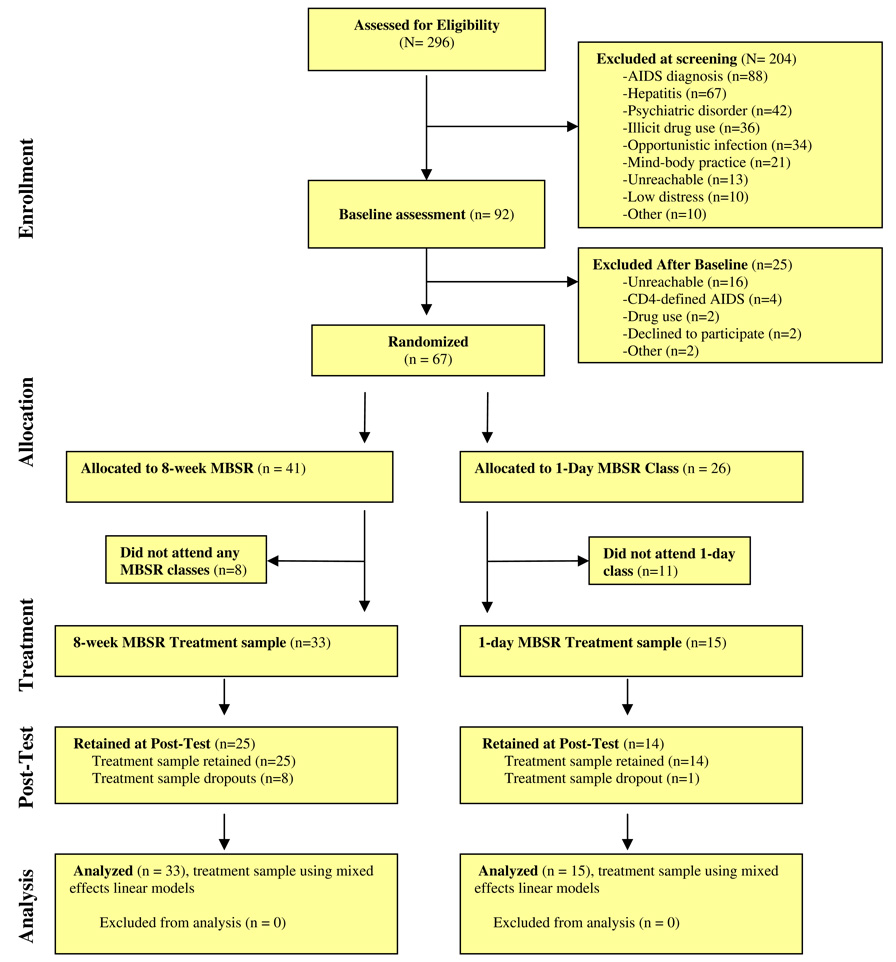
Study participants were recruited through HIV/AIDS community agencies in Los Angeles. To qualify for the study, participants had to be diagnosed HIV-positive for >6 months, English-speaking, and over age 18. In order to recruit a sample who was at risk for stress-associated CD4+ T lymphocyte declines (Cohen et al., 2007), participants had to report at least minimal symptoms of psychological distress at baseline as measured by depressive symptomatology (>4 on the Patient Health Questionnaire-9(PHQ-9)) (Spitzer et al., 2000). Participants were excluded for any substance abuse or psychiatric treatment in the past 30 days, were currently diagnosed with AIDS (or had CD4+ T lymphocytes <200 cells/mm3), had hepatitis, or indicated a regular mind-body practice (e.g., tai chi, meditation) in the past six months. A CONSORT flowchart (Fig. 1) depicts the flow of participants retained at each phase of the trial.
Fig. 1.
CONSORT flowchart of participants retained at each stage of the trial.
2.2. Procedure
All study procedures were approved by the UCLA IRB, and written informed consent was obtained from all participants prior to baseline. Participants were enrolled and completed the baseline assessment over a four-month period, and were then randomized to either the 8-week MBSR or 1-day control intervention.
The 8-week MBSR program (Kabat-Zinn, 1990) included eight weekly 120-min group sessions, a day-long retreat in the seventh week, and daily home mindfulness meditation practice. The group sessions consisted of instructor-guided mindfulness body awareness activities, mindfulness meditations, mindful stretching, and group discussions. A six-hour day-long retreat in week 6–7 of the MBSR program focused on integrating and elaborating on the exercises the participants learned during the 8-week course. Finally, participants were instructed to practice 30 min of audio-guided mindfulness exercises each day at home during the 8-week program. The one-day stress education MBSR program was a condensed version of the 8-week MBSR program. Participants in this condition attended a day-long 6 h seminar where they received information, instruction, and practice in the same mindfulness practices taught in the 8-week program, including group discussions. Instructors did not discuss or encourage participants to start home or daily-life mindfulness practices in the one-day MBSR condition. The one-day MBSR program was administered between weeks 4–6 during the 8-week program.
Post-intervention assessment of CD4+ T lymphocyte levels was completed for all participants within two-weeks of the last session of the 8-week program. Participants were enrolled on a rolling basis, and randomized in one of four cohorts between February 2006 and October 2007. A 2:1 (8-week MBSR, one-day education) randomization schedule was employed, and study assessment personnel were blind to participant condition.
2.3. Measures
Peripheral blood CD4+ T lymphocyte levels and concentrations of HIV-1 RNA were assessed at baseline and post-intervention. CD4+ T lymphocyte levels were determined by flow cytometry and complete blood count by a licensed clinical reference laboratory, and plasma HIV-1 RNA concentrations were assayed by an Amplicor HIV-1 Monitor assay (Roche Diagnostics, Indianapolis, IN). MBSR treatment adherence was assessed by MBSR class attendance. A measure of total class attendance was determined by summing the number of hours of MBSR class attended from attendance sheets by study staff (2 h for each MBSR class, 6 h for the one-day MBSR retreat, and 6 h for the 1-day education intervention).
2.4. Statistical analysis
Statistical analyses were conducted on the treatment participants (N = 48), and on the entire randomized sample (N = 67). Treatment participants (N = 48) were defined as those who attended at least one study class. Data were analyzed using mixed effects linear models treating study condition and time (baseline vs. post-intervention) as fixed effects. Primary analyses modeled time as a repeated measure, subject condition, and a time × treatment interaction term. Ancillary analyses with covariates and treatment adherence modeled these variables as fixed effects predictors.
3. Results
Participants in both treatment arms indicated moderate psychological distress at baseline (M = 9.8, SD = 3.7), and levels of psychological distress were not significantly different between treatment groups at baseline (Table 1). The two treatment groups did not differ on any other measured characteristics at baseline (Table 1). As shown in Table 1, control participants had slightly higher CD4+ T lymphocytes at baseline, greater ARV use at post-intervention, and had a higher proportion of heterosexual participants, although these differences did not reach conventional levels of statistical significance (all p’s > .08). These differences would be expected to favor the control group and thus could not account for any positive intervention effects observed. It is also possible that these differences could reflect different study populations due to study dropout rates or other factors. To minimize any potential confounding effects, ancillary analyses were conducted (described below) to control for ARV use, number of days between the pre-and post-test assessments, sexual orientation, and age.
Table 1.
Baseline characteristics of the treatment sample participants
| Characteristic | MBSR 8-week program (N = 33) | MBSR 1-day seminar (N = 15) | Difference statistic |
|---|---|---|---|
| Age [mean (SD)] | 40(9) | 42(11) | t(46) = −.78, p = 0.44 |
| Gender | χ2(1) = .19, p = 0.66 | ||
| Male | 30 | 13 | |
| Female | 3 | 2 | |
| Ethnicity | χ2(4) = 5.20, p = 0.27 | ||
| African American | 13 | 11 | |
| Latino/hispanic | 8 | 2 | |
| Caucasian | 9 | 2 | |
| Native American | 1 | 0 | |
| Other | 2 | 0 | |
| Sexual Orientation | χ2(2) = 4.42, p = 0.11 | ||
| Homosexual | 23 | 6 | |
| Heterosexual | 9 | 7 | |
| Bisexual | 1 | 2 | |
| Employment Status | χ2(2) = .37, p = 0.83 | ||
| Unemployed | 19 | 10 | |
| Part-time | 6 | 2 | |
| Full-time | 8 | 3 | |
| Average family monthly income | χ2(2) = 2.65, p = 0.27 | ||
| 0–800 dollars | 12 | 9 | |
| 801–2500 dollars | 11 | 4 | |
| >2501 dollars | 10 | 2 | |
| Smoking status | χ2(1) = .22, p = 0.64 | ||
| Smoker | 13 | 7 | |
| Non-smoker | 20 | 8 | |
| ARV use at baseline | 8 | 5 | χ2(1) = .43, p = 0.51 |
| ARV use at post-intervention | 11 | 9 | χ 2(1) = 3.02, p = 0.08 |
| Year of HIV diagnosis [mean year (SD)] | 1999(6.5) | 1999(5.4) | t(46) = −.28, p = 0.78 |
| CD4+ T lympho cytes (cells/mm3) [mean(SD)] | 618(224) | 757(327) | t(46) = −1.72, p = 0.09 |
| PHQ-9 distress at baseline [mean(SD)] | 10.1(3.6) | 9.1(4.0) | t(46) = −.92, p = 0.36 |
The average participant in the study was male, African American, homosexual, unemployed, and not on ARV medication. Participants on ARV medications indicated an average self-reported adherence of M = .45 (SD = 76) missed doses in the past week at baseline and M = .71 (SD = 1.14) at post-intervention. Participants who completed all assessments (N = 38) were compared to study dropouts (N = 29) on all baseline characteristics. Study dropouts were significantly younger than study completers, t(65) = 2.26, p = .03, but no other significant differences emerged. Dropout rates in the treatment sample in the 8-week MBSR condition (N = 8) and the 1-day control condition (N = 1) were not significantly different (χ2(1) = 2.10, p = .15). Although not significant, a greater proportion of participants in the 8-week condition dropped out, and is likely due to the more demanding and time intensive nature of this program.
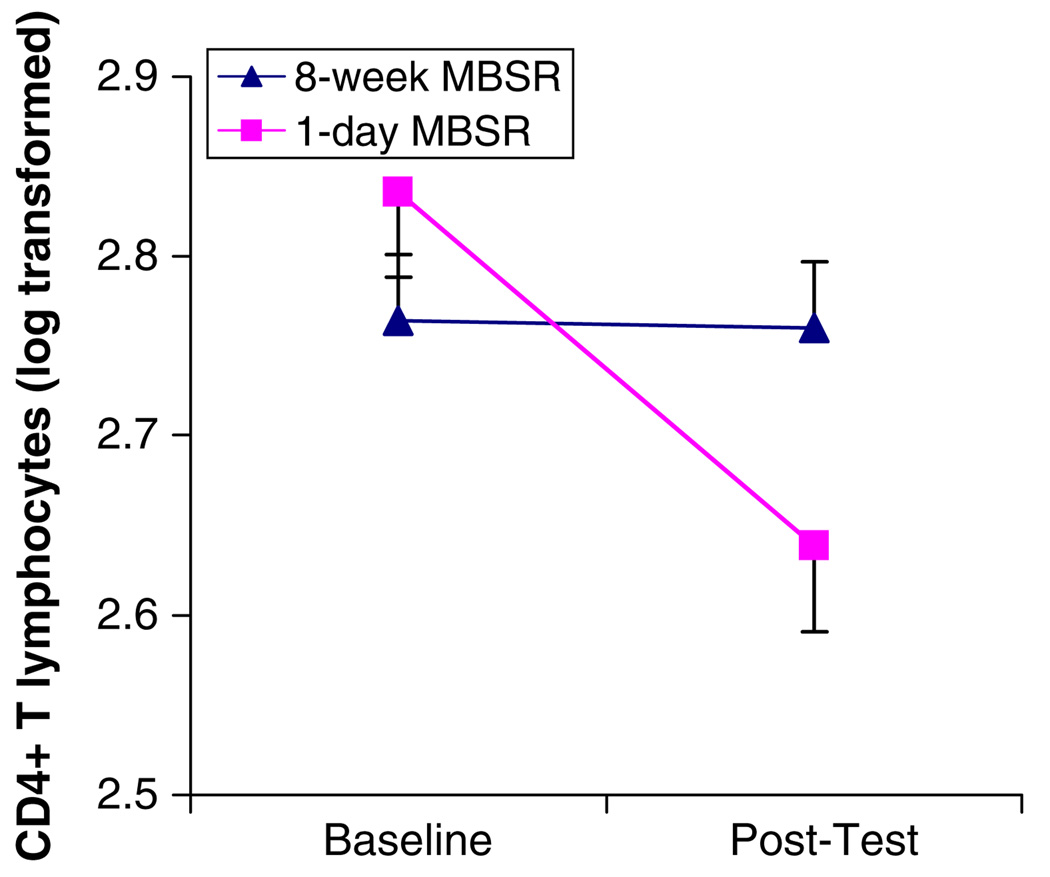
To determine the effects of the MBSR and control programs, mixed effects linear models analyzed log-transformed and raw CD4+ T lymphocyte counts in both the treatment (N = 48) and randomized (N = 67) samples. A mixed effects linear model on the treatment sample revealed a significant time × treatment interaction on log10CD4+ T lymphocytes, F(1,45) = 5.70, p = .02 (Fig. 2) and raw (non log-transformed) CD4+ T lymphocytes (Table 2), F(1,44) = 5.03, p = .03. Specifically, the 8-week MBSR participants had a raw mean increase of 20 CD4+ T lymphocytes, whereas the 1-day control participants had a raw mean decrease of 185 CD4+ T lymphocytes from baseline to post-intervention (Table 2). Analyses of the entire randomized (N = 67) sample, which included participants who never received any treatment, showed the same pattern of results, F(1,57) = 3.15, p = .08. The potential clinical impact of this finding was assessed by counting participants with CD4-defined AIDS (<200 cells/mm3) at post-intervention. No participants had CD4-defined AIDS at baseline; 14% (N = 2) of participants in the control condition reached CD4-defined AIDS at post-intervention compared to 0% (N = 0) of participants in the 8-week MBSR condition.
Fig. 2.
Log transformed CD4+ T lymphocytes at baseline and post-intervention in the treatment sample (N = 48). Vertical lines indicate standard errors of the means.
Table 2.
Baseline and post-intervention means and standard errors for CD4+ T lymphocytes in the 8-week and 1-day MBSR treatment participants (N = 48)
| Lymphocyte counts (cells/mm3) |
8-Week MBSR | 1-Day MBSR | ||
|---|---|---|---|---|
| Baseline M (SE) | Post-M (SE) | Baseline-M (SE) | Post-M (SE) | |
| CD4+ T | 618(47) | 628(52) | 757(70) | 572(71) |
| Lymphocytes | ||||
Ancillary analyses using mixed effects linear models explored the role of confounding factors on the time × treatment CD4+ T lymphocyte effect. The inclusion of ARV medication status at baseline and post-intervention (binary variables: on or off ARVs) as covariates did not affect the strength of the time × treatment interaction on CD4+ T lymphocytes (F(1,45) = 5.50, p = .02), indicating that mindfulness meditation training buffers CD4+ T lymphocyte declines in participants both on and off ARV treatment regimens. Additional analyses explored the potential confounding effects of variability in the number of days between the baseline CD4+ T lymphocyte measure and the initiation of the 8-week MBSR class, sexual orientation (0 = heterosexual, 1 = homosexual or bisexual), and participant age in three separate mixed effects linear models. Similar to ARV medication status, the time × treatment interaction on log10CD4+ T lymphocytes remained statistically significant after control for variability in the number of days between the baseline measure and the initiation of the 8-week MBSR class (F(1,45)=5.66, p = .02), sexual orientation (F(1,45)=5.64, p = .02), or participant age (F(1,45) = 5.51, p = .02).
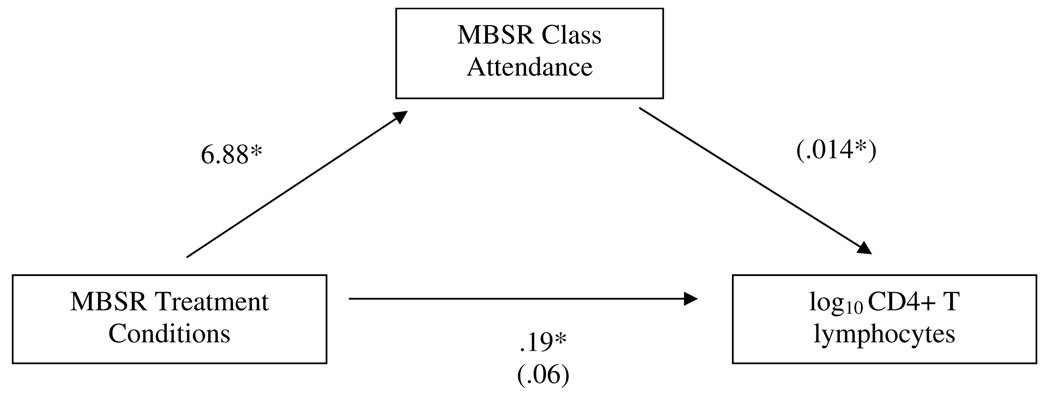
Mediation analyses were consistent with the hypothesis that mindfulness meditation treatment adherence explained the observed time × treatment interaction on log10CD4+ T lymphocytes. Treatment participants attended 12.5 (SD = 7.6) class hours in the 8-week MBSR program and 6 (SD = 0) class hours in the 1-day education control. As shown in Fig. 3, a series of mixed effects linear models assessed statistical mediation (Baron and Kenny, 1986). In a model with the treatment sample (N = 48) where class attendance and the time £ treatment interaction were entered simultaneously, MBSR class attendance predicted greater CD4+ T lymphocytes at follow-up (b = .014, t(74) = 2.09, p = .04), and the path between the time × treatment interaction and log CD4+ T lymphocytes was no longer significant (b = .06, t(56) = .56, p = .58). This finding indicates that the frequency of class attendance could potentially account for as much as 2/3 of the total effect of the experimental conditions on CD4+ T lymphocytes.
Fig. 3.
Mediation analyses in the treatment sample (N = 48). MBSR class attendance mediates the time × treatment interaction on log10 CD4+ T lymphocytes. Numbers represent b coefficients, with parentheses representing b coefficients when MBSR treatment condition and MBSR class attendance are entered simultaneously. *p < .05.
As previous findings have found effects of behavioral stress management in reducing HIV RNA levels in participants with detectable levels of HIV RNA at baseline (Antoni et al., 2006), exploratory analyses examined the effects of mindfulness meditation training on HIV RNA levels in the sub-sample of participants with detectable baseline levels of HIV RNA (N = 30). No differences in baseline HIV RNA levels were observed between the 8-week MBSR (M = 46,880 copies/ mL, SD = 12,830) and 1-day control sub-sample (M = 12,700 copies/ mL, SD = 25,660) participants with detectable levels of HIV RNA (t(28) = 1.19, p = .24). Consistent with the limited statistical power available in this small sub-sample, no significant effects were observed on HIV RNA (time × treatment interaction, p = .41).
4. Discussion
CD4+ T lymphocyte depletion is a hallmark characteristic of HIV-1 pathogenesis and progression to AIDS. The present study provides initial evidence that a behaviorally targeted mindfulness meditation stress-reduction program can buffer CD4+ T lymphocyte declines in an ethnically diverse sample of HIV-1 infected adults. Additional analyses suggested that the mindfulness meditation treatment effects on CD4+ T lymphocytes are independent of ARV treatment status. These data are consistent with the possibility that mindfulness meditation training may have direct effects on CD4+ T lymphocyte distributions (e.g., via effects on haematopoiesis, T-cell redistribution dynamics, or T-cell turnover in lymphoid tissues) (McCune, 2001). A second possibility is that mindfulness meditation training effects on CD4+ T lymphocytes may be explained in part through reductions in HIV RNA levels. A number of studies provide strong links between stress and HIV viral replication (e.g., Cole et al., 1998; Sloan et al., 2007), and stress management programs have been shown to reduce HIV RNA levels in some studies (e.g., Antoni et al., 2006; Petrie et al., 2004). The present study was not appropriately powered to examine the effects of mindfulness meditation training on HIV RNA levels, which is an important pathway that should be examined in future studies with larger samples.
The major limitations of the study include a small sample size and high attrition rates, no long-term follow-up assessments, and an insufficient sample size to determine if mindfulness meditation training impacts HIV-1 RNA levels. Additionally, although not significantly different at traditional statistical thresholds, 1-day control participants had higher numbers of CD4+ T lymphocytes at baseline compared to 8-week MBSR participants. It is possible that this baseline difference could be driving the overall effects described in this report, so an additional ANCOVA analysis compared the 8-week and 1-day groups on post-test log10CD4+ T lymphocytes, while controlling for baseline levels of log10CD4+ T lymphocytes (in participants with complete pre-and post-test data, N = 39). Although underpowered, this analysis was consistent with the mixed model findings indicating that 1-day control participants had lower CD4+ T lymphocytes than 8-week MBSR participants at post-test (p = .06). Despite these limitations, the present findings provide a first indication that a low-cost group-based mindfulness meditation training program can buffer CD4+ T lymphocyte declines, and that this occurs in direct proportion to the amount of mindfulness meditation training received. Although more studies are needed to determine the clinical impact of this program, these findings suggest that mindfulness meditation training may be a beneficial adjunct for stressed HIV-1 infected adults.
In summary, an 8-week mindfulness meditation and stress reduction program can buffer CD4+ T lymphocyte declines in a diverse community sample of HIV-1 infected adults. Well-controlled studies with larger samples are needed to determine if mindfulness meditation training interventions can positively impact biological indicators of immunopathogenesis in HIV-1 infection, but the present findings provide a promising first indication that mindfulness meditation may have benefit as a complementary adjunct treatment for HIV-1.
Acknowledgments
J.D. Creswell had full access to all of the data and takes responsibility for the integrity and accuracy of the data. We thank the UCLA Mindful Living Project team and our MBSR instructors (C. Baum, H. Blumenfeld, and G. Kamler) for their assistance in this study. This study was supported by a National Institute of Mental Health (NIMH) postdoctoral research fellowship (T32MH-019925-09) to the first author, a seed grant from the Cousins Center for Psychoneuroimmunology at UCLA, and the UCLA General Clinical Research Center (NIH/NCRR #M01-RR00865). No financial interests or conflicts of interest are declared.
Footnotes
Clinical Trials Registration: clinicaltrials.gov, Identifier: NCT00600561.
References
- Antoni MH, Carrico AW, Duran RE, Spitzer S, Penedo F, Ironson G, Fletcher MA, Klimas N, Schneiderman N. Randomized clinical trial of cognitive behavioral stress management on human immunodeficiency virus viral load in gay men treated with highly active antiretroviral therapy. Psychosomatic Medicine. 2006;68:143–151. doi: 10.1097/01.psy.0000195749.60049.63. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality & Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Brown KW, Ryan RM, Creswell JD. Mindfulness: theoretical foundations and evidence for its salutary effects. Psychological Inquiry. 2007;18:1–27. [Google Scholar]
- Carlson LE, Speca M, Faris P, Patel KD. One year pre-post intervention follow-up of psychological, immune, endocrine and blood pressure out comes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients. Brain, Behavior, and Immunity. 2007;21:1038–1049. doi: 10.1016/j.bbi.2007.04.002. [DOI] [PubMed] [Google Scholar]
- Carlson LE, Speca M, Patel KD, Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosomatic Medicine. 2003;65:571–581. doi: 10.1097/01.psy.0000074003.35911.41. [DOI] [PubMed] [Google Scholar]
- Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. JAMA. 2007;298:1685–1687. doi: 10.1001/jama.298.14.1685. [DOI] [PubMed] [Google Scholar]
- Cole SW, Korin YD, Fahey JL, Zack JA. Norepinephrine accelerates HIV replication via protein kinase A-dependent effects on cytokine production. Journal of Immunology. 1998;161:610–616. [PubMed] [Google Scholar]
- Cole SW, Naliboff BD, Kemeny ME, Griswold MP, Fahey JL, Zack JA. Impaired responses to HAART in HIV-infected individuals with high autonomic nervous system activity. Proceedings of the National Academy of Sciences of the United States of America. 2001;98:12695–12700. doi: 10.1073/pnas.221134198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crepaz N, Passin WF. Meta-analysis of cognitive-behavioral interventions on HIV-positive persons’ mental health and immune functioning. Health Psychology. 2008;27:4–14. doi: 10.1037/0278-6133.27.1.4. [DOI] [PubMed] [Google Scholar]
- Davidson RJ, Kabat-Zinn J, Schumacher J, Rosenkranz M, Muller D, Santorelli SF, Urbanowski F, Harrington A, Bonus K, Sheridan JF. Alterations in brain and immune function produced by mindfulness meditation. Psychosomatic Medicine. 2003;65:564–570. doi: 10.1097/01.psy.0000077505.67574.e3. [DOI] [PubMed] [Google Scholar]
- Ironson G, O’Cleirigh C, Fletcher MA, Laurenceau JP, Balbin E, Klimas N, Schneiderman N, Solomon G. Psychosocial factors predict CD4 and viral load change in men and women with human immunodeficiency virus in the era of highly active antiretroviral treatment. Psychosomatic Medicine. 2005;67:1013–1021. doi: 10.1097/01.psy.0000188569.58998.c8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. General Hospital Psychiatry. 1982;4:33–47. doi: 10.1016/0163-8343(82)90026-3. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress Pain and Illness. New York, NY: Dell Publishing; 1990. [Google Scholar]
- May MT, Sterne JA, Costagliola D, Sabin CA, Phillips AN, Justice AC, Dabis F, Gill J, Lundgren J, Hogg RS, de Wolf F, Fatkenheuer G, Staszewski S, D’Arminio Monforte A, Egger M. HIV treatment response and prognosis in Europe and North America in the first decade of highly active antiretroviral therapy: a collaborative analysis. Lancet. 2006;368:451–458. doi: 10.1016/S0140-6736(06)69152-6. [DOI] [PubMed] [Google Scholar]
- McCune JM. The dynamics of CD4+ T-cell depletion in HIV disease. Nature. 2001;410:974–979. doi: 10.1038/35073648. [DOI] [PubMed] [Google Scholar]
- Ospina MB, Bond K, Karkhaneh M, Tjosvold L, Vandermeer B, Liang Y, Bialy L, Hooton N, Buscemi N, Dryden DM, Klassen TP. Meditation practices for health: state of the research. Evidence Report/Technology Assessment (Full Report) 2007:1–263. [PMC free article] [PubMed]
- Petrie KJ, Fontanilla I, Thomas MG, Booth RJ, Pennebaker JW. Effect of written emotional expression on immune function in patients with human immunodeficiency virus infection: a randomized trial. Psychosomatic Medicine. 2004;66:272–275. doi: 10.1097/01.psy.0000116782.49850.d3. [DOI] [PubMed] [Google Scholar]
- Robinson FP, Mathews HL, Witek-Janusek L. Psycho-endocrine-immune response to mindfulness-based stress reduction in individuals infected with the human immunodeficiency virus: a quasiexperimental study. Journal of Alternative and Complementary Medicine New York. 2003;9:683–694. doi: 10.1089/107555303322524535. [DOI] [PubMed] [Google Scholar]
- Sloan EK, Capitanio JP, Tarara RP, Mendoza SP, Mason WA, Cole SW. Social stress enhances sympathetic innervation of primate lymph nodes: mechanisms and implications for viral pathogenesis. Journal of Neuroscience. 2007;27:8857–8865. doi: 10.1523/JNEUROSCI.1247-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Kroenke K, Hornyak R, McMurray J. Validity and utility of the PRIME-MD patient health questionnaire in assessment of 3000 obstetric-gynecologic patients: the PRIME-MD Patient Health Questionnaire Obstetrics-Gynecology Study. American Journal of Obstetrics and Gynecology. 2000;183:759–769. doi: 10.1067/mob.2000.106580. [DOI] [PubMed] [Google Scholar]