Abstract
Placebo effects are beneficial health outcomes not related to the relatively direct biological effects of an intervention and can be elicited by an agent that, by itself, is inert. Understanding these placebo effects will help to improve clinical trial design, especially for interventions such as surgery, CNS-active drugs and behavioural interventions which are often non-blinded. A literature review was performed to retrieve articles discussing placebo implications of clinical trials, the neurobiology of placebo effects and the implications of placebo effect for several disorders of neurological relevance. Recent research in placebo analgesia and other conditions has demonstrated that several neurotransmitter systems, such as opiate and dopamine, are involved with the placebo effect. Brain regions including anterior cingulate cortex, dorsolateral prefrontal cortex and basal ganglia have been activated following administration of placebo. A patient's expectancy of improvement may influence outcomes as much as some active interventions and this effect may be greater for novel interventions and for procedures. Maximizing this expectancy effect is important for clinicians to optimize the health of their patient. There have been many relatively acute placebo studies that are now being extended into clinically relevant models of placebo effect.
Keywords: placebo effects, expectancy, cognition, clinical trials methods
Background
In clinical trials, substances or procedures that are designed to serve merely as control conditions may actually produce an effect on subjective or biomarker outcomes. These indirect effects of biologically inert substances or inactive procedures will be considered under the umbrella term placebo effects (Kaptchuk, 1998b; Guess et al., 2002; Oken, 2004; Benedetti et al., 2005). The term placebo effect will be used to refer to a physiological state anticipating and contributing to the occurrence of some future health-related outcome through learning, conditioning or other related process.
Other terms used to describe these effects include expectancy effects (Crow et al., 1999), context effects (Di Blasi et al., 2001) and meaning response (Brody and Brody, 2000; Moerman, 2002). Some placebo researchers have used the term expectancy narrowly to mean placebo effects due to anticipation that has been verbally or consciously mediated. Meaning response more clearly includes expectancy effects that impact health besides the placebo effect such as cultural effects (Moerman, 2002), uncertainty in diagnosis and prognosis (Thomas, 1987), the impact of pessimism and hopelessness on disease and function (Anda et al., 1993; Maruta et al., 2002) and the nocebo or negative placebo effect (Hahn, 1997; Barsky et al., 2002). Placebo effects also encompass neural systems not only simply related to anticipation or expectancy but also to the desire to achieve a particular goal (Price et al., 2008).
The actual intervention that elicits the placebo effect is referred to as the placebo. The placebo can be any clinical intervention including words, gestures, pills, devices and surgery (Chaput de Saintonge and Herxheimer, 1994). The term sham is sometimes used to describe a placebo intervention, such as in the context of surgery. Ethical issues related to use of placebo clinically or in clinical research trials have been discussed elsewhere (Bok, 2002; Temple, 2002).
Placebo effects do not include methodological factors resulting in improvement that are unrelated to an active alteration of outcome measures, e.g. natural history, regression to the mean (McDonald and Mazzuca, 1983), Hawthorne effect (Bouchet et al., 1996) and poor experimental designs such as subject biases (Clayden et al., 1974) or the purported inert control condition not being inert (Kienle and Kiene, 1997; Ader, 2000; Miller et al., 2004). The natural history is particularly problematic, since it is impossible to infer anything about the frequency or size of placebo effects without a control for the placebo condition. Unfortunately, it is rare in modern clinical trials to have untreated control groups. A recent systematic review of placebo effect found only 114 clinical trials out of all clinical trials spanning several decades that had both a placebo treatment arm as well as a non-treatment arm in a clinical trial (Hrobjartsson and Gotzsche, 2001). Subject biases resulting from non-blinding especially in a cross-over design may confound placebo research (Ader, 2000).
Placebo effects presumably have different mediators depending on the specific learned association and whether referring to acquisition of the association or the placebo response. The CNS is the primary location and mediator of the physiological basis of the placebo effects through its role in learning and memory and its outputs on sensory, motor and autonomic pathways as well as the immune and endocrine systems. People have individual traits that predispose them to be more or less responsive to certain stimuli; the interaction between the learned associations of the clinical situation and the person's particular biology produces a response. The response could be a basic physiological process such as modulation of sensory processing, release of neurotransmitters or alterations in hypothalamic-pituitary-adrenal axis or immune system activity. The placebo response could also be some more complex physiological process including change in mood, change in motivation/effort or cognitive set-shifting.
Learned associations producing placebo effects can be acquired through conditioning (Voudouris et al., 1989; Price et al., 1999; Wickramasekera, 2000; Siegel, 2002). The conditioned pharmacotherapeutic effect has been characterized in animal models (Ader and Cohen, 1982; Jones et al., 2008). While the relative contribution of conditioning to placebo effects remains uncertain (Montgomery and Kirsch, 1997; Benedetti et al., 2003; Kirsch, 2004; Stewart-Williams and Podd, 2004), non-conscious mechanisms such as conditioning may be particularly important for immune or endocrine placebo effects (Kirsch, 2004). Animal models are useful models of some components of placebo effects but are intrinsically limited placebo effect models since there are no verbally mediated expectancy changes. Conditioning in placebo research studies has consisted of exposure(s) prior to administration of placebo of either the active drug itself (Laska and Sunshine, 1973; Amanzio and Benedetti, 1999), or of an apparent effect of a placebo, e.g. due to surreptitiously turning down the pain intensity at the same time as placebo is administered (Voudouris et al., 1989). Since most adults have had previous exposures to clinical experiences such as taking oral analgesics, clear separation of conditioning from other aspects of the placebo response in human experiments is difficult.
Conditioning is only one aspect of the placebo effect. Many aspects of placebo effects, including verbal communication, encompass more top–down, cortically mediated changes in behaviour than the term conditioning usually implies. Some learned anticipations acquired over longer periods of time than are usually studied in the conditioning experiments may be related to: interactions between person and health care provider (Brody, 2000); health care setting and practitioner characteristics (Di Blasi et al., 2001); physical characteristics of a pill (Buckalew and Coffield, 1982); type of treatment (e.g. pill versus injection versus surgical) (Kaptchuk et al., 2000) and pill administration frequency (de Craen et al., 1999). Additionally, anticipation or expectancy can refer to a response expectancy or self-efficacy expectancy, that is, one's sense of being able to achieve an outcome (Caspi and Bootzin, 2002). Desire or motivation for improvement is another aspect of the placebo effect (Hyland et al., 2007; Price et al., 2008).
Trial designs and placebo effects
Placebo effects contribute to variability in outcome data from randomized double-blind trials. A systematic review of 117 ulcer studies found that the response rate in placebo arms varied from 0 to 100%, much more variable than the cimetidine or ranitidine response rates in the same studies (Moerman, 2000). However, simply considering these placebo effects to be noise or confounders in clinical trials is not helpful to understanding the mechanisms (Kaptchuk, 1998b). Even worse, excluding placebo responders during wash-in periods in clinical trials, as is now being occasionally done (van Dongen et al., 2000), is of questionable merit and ethics; placebo responders may be most likely to benefit from a biologically active treatment and their exclusion compromises the generalizability of clinical trial results (Kaptchuk, 1998a; Pablos-Mâendez et al., 1998). The patient's belief regarding their allocation to an active or placebo group may produce a greater effect than the active intervention drug itself, such as in surgery for Parkinson's disease (McRae et al., 2004), and acupuncture for adjunctive treatment for dental surgery (Bausell et al., 2005). Even with this information, patient expectancies are still not routinely assessed during clinical trials or incorporated into the analysis.
In routine clinical practice when patients are given a known drug, the effectiveness of the drug is a combination of a non-specific placebo effect and the biologically active effect. In double-blind placebo-controlled trials the direct biological effect is assumed to be the difference between the active and placebo arms. However, since the direct biological and non-specific placebo effects may not be simply additive, conclusions from double-blind placebo-controlled trials are not straightforward (Kleijnen et al., 1994; Kaptchuk, 1998b). Informed consent may alter the effectiveness of the placebo compared with the active agent in comparison to a situation where agents are administered without giving patients information concerning the study (Bergmann et al., 1994). For example, an interaction effect between informed consent and treatment has been noted by comparing clinical outcomes (beneficial or side effects) from an active drug between double-blind placebo-controlled and double-blind comparison trials (Kirsch and Weixel, 1988; Skovlund, 1991; Bergmann et al., 1994; Rochon et al., 1999). A non-steroidal anti-inflammatory drug (NSAID) produced significantly greater dropout rates related to ineffectiveness compared with the same drug being tested in an active drug comparison. On the other hand, patient dropouts were greater for adverse events in the trials in which the NSAID was compared with another drug than in placebo-controlled trials (Rochon et al., 1999). Thus, given the same active NSAID, subjects had different experiences based solely on whether the other arm of the trial was a placebo arm or an active drug arm, despite the fact the patient was not in that other arm but simply knew about it. Post-thoracotomy patients given saline but told it was pain medication had significantly less need for analgesic medication than those not told anything. Subjects told they were in a double-blind study of a pain medication (and so having a 50% chance of receiving pain medication or placebo) had a lowered need for analgesics following saline administration that was approximately half-way between the subjects not told anything during administration of saline and the subjects deceptively told they were getting an analgesic medication (Pollo et al., 2001).
The placebo effect may be disproportionately large for non-blinded therapies potentially resulting in what has been called the efficacy paradox (Walach, 2001). This may occur, for example, when a therapy has efficacy when compared with a drug, but little treatment effect when compared with an appropriate placebo or sham. While all therapies are held to the high standard of showing benefit over controls matched well for expectancy, the overall effect—the combination of the non-specific and specific effects—may be reasonably high with only a small specific effect. This may be the case for surgical procedures where non-specific beneficial effects may be very prominent but sham surgery is not often used as a control. This may apply similarly to other non-blinded procedures such as acupuncture where the incidental, non-specific effects may be components of the therapy (Paterson and Dieppe, 2005). While having a control group that is matched for expectancy or credibility to an active non-blinded intervention is critical (Shapiro, 1981), it may be difficult or potentially impossible to design such an ideal control group for certain interventions such as psychological and behavioural interventions.
There is some data to suggest that placebo effects are greater for psychological and self-rated measures than other objective measures of disease activity (Hrobjartsson and Gotzsche, 2001). A study that evaluated patients in placebo arms of rheumatoid arthritis drug trials found essentially no change over 6 months on the erythrocyte sedimentation rate but there was a significant improvement in articular index and morning stiffness (Porter and Capell, 1993). While placebo responses may be generally greater for self-ratings, there are many studies demonstrating changes in more objective outcome measures including C-reactive protein (Hashish et al., 1988), elevation of liver enzymes (Merz et al., 1997), changes in pulmonary function (Luparello et al., 1970; Butler and Steptoe, 1986; Kemeny et al., 2007), postprandial glucose (Sievenpiper et al., 2007) and the neurobiology studies (see subsequently).
Expectation plays a major role on subjective and behavioural effects of drugs affecting the CNS. This has been widely studied with the use of the balanced placebo design (Ross et al., 1962; Rohsenow and Marlatt, 1981; Lotshaw et al., 1996). In the simplest balanced placebo design, subjects are assigned to one of four groups: subjects are either given an active drug or placebo and either told they are getting an active drug or told they are getting placebo. Even though not having a control for the placebo condition, the balanced placebo has shed light on expectancy effects. For example, in a balanced placebo design among cocaine abusers, administration of methylphenidate when expecting to receive methylphenidate produces significantly increased brain glucose metabolism compared with administration of methylphenidate with expectation of simply receiving placebo (Volkow et al., 2003). Expectation of receiving caffeine produced dopamine release in the thalamus measured by raclopride positron emission tomography (PET) following administration of placebo (Kaasinen et al., 2004).
Individual differences and psychological factors impacting placebo effects
Perceived self-efficacy refers to a psychological construct concerning the belief in one's abilities to organize and execute behaviours with experimental manipulation of self-efficacy impacting stress, autonomic nervous system activation and neuroendocrine changes (Bandura, 1997). Health-related self-efficacy may be one mechanism of the placebo effect. Treatment regimens that actively engage the patient to have some sense of control over their disease process may produce better outcomes than those that are less actively engaging to the patient. Studies with adequate control groups that can clearly differentiate positive expectancy from self-management are lacking (Crow et al., 1999). High-success biofeedback that improves one's sense of control may improve clinical outcomes independent of the accuracy of the biofeedback (Holroyd et al., 1984). Adherence to a drug regimen may relate to an expectancy of the drug working or to this sense of control. Subjects more adherent to a placebo intervention do better than those less adherent to the placebo regimen even with gross major medical outcomes (Horwitz et al., 1990; Simpson et al., 2006). However, other than expectancy, subjects more adherent to a prescribed medical regimen may have some different characteristic such as personality or mood (Osterberg and Blaschke, 2005; Flegal et al., 2007) that may correlate to compliance and with some other aspects of medical intervention or health-promoting behaviour. A systematic review found that positive expectations of outcome were associated with better health outcomes (Mondloch et al., 2001).
Gender has usually not been associated with placebo effects. One study of botulinum toxin injections for migraine prophylaxis, did find that predictors of placebo responsiveness included male gender along with a history of opioid use and injections in the neck/shoulders (Schwedt et al., 2007). There have been inconsistent results from studies evaluating whether certain personality traits predispose some people to experience improvements from placebo administration more than others. While some studies have been negative (Freund et al., 1972; Buckalew et al., 1981), other studies suggest there may be some contribution to the placebo response from factors such as social acquiescence (McNair and Barrett, 1979), suggestibility or hypnotizability and absorption, which is the degree to which one can focus on a single theme (Evans, 1985; Challis and Stam, 1992; Raz, 2007). This lack of consensus on individual differences secondary to placebo administration may be related to an interaction between personality factors and the specific experimental condition. The individual response to placebo differed based on an optimism-pessimism scale in the 100% deceptive but not in the 50–50% conditional expectancy of receiving active drug (Geers et al., 2005). The effect of personality traits such as optimism on placebo response may be dependent on the specific treatment and context (Geers et al., 2007; Hyland et al., 2007). Uncertainty in diagnosis and prognosis produces expectancy effects on health outcomes (Thomas, 1987), possibly through some mechanism related to stress or anxiety. High levels of neuroticism, along with depression and anxiety, helped predict placebo analgesic response in patients with discogenic back pain (Wasan et al., 2006). Individual differences may contribute to variation in placebo effects in other ways. The individual experience of actual pain contributes significantly to neurotransmitter activity during placebo analgesia (Zubieta et al., 2006). Personality may relate to placebo responses either through the neurotransmitter systems thought to be related to these traits or to interactions with these traits. The mechanisms of anticipatory nausea and vomiting associated with chemotherapy overlap with the placebo effect. Higher anticipatory nausea and vomiting was not related to trait anxiety, depression or gender, but was related to measures of absorption and autonomic perception (Challis and Stam, 1992).
Treatment factors impacting placebo effects
Some early studies centred around physical aspects of tablets and capsules (Buckalew and Ross, 1981). Studies suggest that people's perceptions of pills are influenced by their colour (Schapira et al., 1970; Buckalew and Coffield, 1982). Other studies have suggested that capsules are perceived to be stronger than tablets (Buckalew and Coffield, 1982) and possibly larger pills stronger than smaller pills (Buckalew and Coffield, 1982). The number of pills also influences perception of pill strength (de Craen et al., 1999). In addition to physical factors relating to the placebo, even the brand name or overt symbolic association may be important (Branthwaite and Cooper, 1981). Injections elicit a stronger placebo effect than oral medications and surgery is likely better than the others in terms of eliciting placebo effects (de Craen et al., 2000; Kaptchuk et al., 2000).
Although sham surgery is only rarely used, the issue of clinician biases, necessity of blinded trials and placebo effect was dramatically raised by the classic studies that evaluated internal mammary artery ligation for treatment of angina (Cobb et al., 1959). In a trial of arthroscopic surgery for osteoarthritis of the knee, there was no difference in pain improvement between those getting actual procedures and those simply receiving incisions and sutures (Moseley et al., 2002). However, all three groups had a significant decline in their pain compared with their baseline. In terms of Parkinson disease surgery, the results are variable but there is likely a significant placebo effect in this case as well (Freed et al., 2001; McRae et al., 2004). There are ethical issues related to sham surgery as a control arm in clinical trials (Horng and Miller, 2002) but, despite objections by some people (Macklin, 2000), sham surgery control appears reasonable to many researchers and oversight groups (Freeman et al., 1999). It could be argued that, given the potential benefit of sham surgery secondary to placebo effects, the sham surgery should not be considered to have no potential benefit to the research subject.
Clinician and clinician–patient interaction factors impacting placebo effects
Expectancy may be affected by the personal history of patient–clinician interactions and shared experiences of the patient and clinician as well as other context and white-coat effects (Brody, 2000; Di Blasi et al., 2001). Placebo effects are even affected by the number of patient–clinician interactions (Ilnyckyj et al., 1997; Paternak and Zimmerman, 2007). The interaction with the health care provider may provide non-specific benefits such as stress reduction, decreased anxiety or improvement of mood. Some clinicians are perceived to be better clinicians than others as a result of personality or interaction style. This may impact outcomes independent of any specific treatment.
There have been studies trying to evaluate the effect of clinician personality traits or interaction style. In a study of analgesia for post-dental extraction pain, dental hygienists and dentists were instructed to be warm or neutral in their interaction style, i.e. engaging in more social conversation or not. The clinicians were also told to oversell or undersell the effectiveness of a pill to reduce anxiety and sensitivity to pain from the mandibular block injection. The pill was always a placebo in this single blind experiment. The effect of overselling compared with underselling the placebo was very significant on ratings of pain, anxiety and fear of injection. The interaction style had a smaller but still significant effect (Gryll and Karahn, 1978). An earlier study evaluating responsiveness to an anti-anxiety agent in 138 patients in three clinical sites found significant effects on outcome when the clinician was more positive and enthusiastic about medication compared with being less certain and experimental towards the medication (Uhlenhuth et al., 1966). In another study, instructions prior to receiving a lactate infusion affected pCO2 and respiratory rate. Subjects told the infusions may cause unpleasant bodily sensation similar to those experienced during periods of anxiety had greater increase in respiratory rate and decrease in pCO2 compared with subjects who were instructed they would have feelings of pleasant excitement (van der Molen and van den Hout, 1988).
Diagnosis and diagnostic testing may impact clinical outcomes. One study randomized patients who had symptoms without major pathology to several groups. Subjects were given a firm diagnosis by the physician and told they would be better in a few days or the physician told them s/he was not certain what was the matter. Patients were also randomized to receive a prescription or not in each group. Patients who were given a specific diagnosis and told they would get better did in fact get better more frequently than those not given a diagnosis (Thomas, 1987). This same study found that although giving a diagnosis had a significant impact, prescribing a drug as part of the management had no impact on outcomes. The ordering of diagnostic tests also appears to improve patient satisfaction and well-being. In one study, patients with non-specific chest pain felt not to be related to heart disease were randomized to receive no further testing or to have an electrocardiogram and creatine phosphokinase blood test. Patients receiving the diagnostic testing did significantly better in terms of their short-term disability and satisfaction with care (Sox et al., 1981).
Clinicians who provide too many negative details of an intervention may elicit a nocebo effect. While this was suggested in a small study looking at post-lumbar puncture headache (Daniels, 1981), it was not observed in a larger study of patients receiving new prescriptions for angiotensin-converting enzyme inhibitors, trimethoprim–sulfamethoxazole or NSAIDs (Lamb et al., 1994).
Clinicians who strongly advocate a new procedure for a disease often have significantly positive results. New procedures or drugs are initially heavily advocated for by clinicians but the interventions may have decreased efficacy over time. For example, the healing rate for cimetidine across over 50 controlled trials for peptic ulcer disease began decreasing in the 1980's while the response rate to a newer agent, ranitidine, remained stable across trials in the same time period (Moerman, 2002). More subtle clinician biases have also produced clinical changes in controlled studies (Levine and Gordon, 1984; Gracely et al., 1985).
Neurobiology of placebo effects
There has been increasing research on the neurobiology of placebo effects (Stoessl and de la Fuente-Fernandez, 2004; Benedetti et al., 2005; Colloca and Benedetti, 2005). Placebo effects presumably have multiple and different effectors depending on the specific context and type of learned anticipation. The placebo response systems need to be different to be able to produce analgesia through release of endogenous opioids (Levine et al., 1978; Amanzio and Benedetti, 1999), dopamine release in the basal ganglia or reduced subthalamic nucleus firing in Parkinson's disease (de la Fuente-Fernandez et al., 2001; Benedetti et al., 2004), anticipatory vomiting from chemotherapy (Challis and Stam, 1992), objective changes in pulmonary function in asthmatic adults (Butler and Steptoe, 1986), anti-tussive activity (Lee et al., 2005) or improvements in reaction time and mood with administration of placebo in amphetamine-like stimulant drug experiments (Buckalew, 1972; Mitchell et al., 1996). Additionally, there are likely further downstream effects. For example, placebo analgesia may be associated with decreased β-adrenergic activity of the heart as measured by decreased heart rate and low frequency heart rate variability (Pollo et al., 2003). Different patterns of neural activation during anticipation and during the placebo response have been demonstrated (Scott et al., 2007; Wager et al., 2007) and there are likely different processes during the time period of acquisition of expectancy compared with the period when a beneficial clinical response occurs. The currently best understood placebo effect is in analgesic responses. The placebo analgesia research relies heavily on modulation of sensory processing often assessed by subjective perception on acute experimental pain models in healthy subjects, but this research still sheds light on the underlying mechanisms of clinically relevant placebo effects.
There are many brain systems that contribute to the placebo effect. The dopamine system has several elements relevant for placebo effect (Fricchione and Stefano, 2005; Irizarry and Licinio, 2005). Dopamine is critical in associating an environmental stimulus to the anticipation of a reward (Schultz, 2006) as well as being released during behaviour to obtain a reward (Phillips et al., 2003). Dopamine release in the striatum was enhanced with a placebo dopaminergic agent in a group of Parkinson's patients as determined by raclopride PET scanning (de la Fuente-Fernandez et al., 2001). It is uncertain if this effect was specific to the dopaminergic deficit in neostriatal motor pathways in Parkinson's disease or if it was a more general expectancy related to dopamine changes in the nucleus accumbens or other nearby modulatory regions that are less specifically associated with Parkinson's disease. In a small study of placebo analgesia, there was a correlation between striatal dopamine receptor binding potential and pain thresholds but not with placebo induced elevations of pain thresholds (Martikainen et al., 2005). Dopamine release in the nucleus accumbens as demonstrated with raclopride PET scanning was found to be directly correlated with degree of placebo analgesia (Scott et al., 2007). It has been theorized that dopamine signalling as a marker for discrepancy between predicted and actual reward may be the critical aspect for its role in the placebo effect (Irizarry and Licinio, 2005). Dopamine release in the anterior cingulate cortex (ACC) associated with expectancy of reward in a monetary gaming task has been associated with dopamine release in the same region with placebo analgesia (Scott et al., 2007). The temporal course of this signalling is discounted for longer periods to the expected reward, highlighting the potential differences between a clinical intervention given as a single dose or over a longer time period. Additionally, the anterior cingulate, an area rich in dopamine receptors as well as opioid receptors has been activated by placebo analgesia (see subsequently).
The endogenous opioid system is critically important for placebo analgesia and likely plays a role for other placebo effects. The role of opioids has been demonstrated by the ability of naloxone, an opioid receptor blocker, to antagonize placebo analgesia (Levine et al., 1978; Amanzio and Benedetti, 1999). Additionally, the opioid-mediated analgesic placebo response is enhanced with proglumide, a cholecystokininantagonist that modulates opioid activity, even though proglumide has no analgesic effect on its own (Benedetti, 1996). The involvement of the opioid system has been documented by neuroimaging with PET visualizing activation of mu-opiod receptor mediated neurotransmission with placebo analgesia (Zubieta et al., 2005; Wager et al., 2007). The key role of the opioid system in pain signalling is highlighted by overlap between brain areas activated by pain and by placebo analgesia (e.g. ACC) and by correlations between cortical activation areas and subcortical regions, such as periaqueductal grey, which are more clearly related to pain (Petrovic et al., 2002; Pariente et al., 2005). The endogenous opioid system may be relevant for many other neural functions than signalling related to pain (Ribeiro et al., 2005), and has already been postulated to have a more general role in placebo effects (Stefano et al., 2001).
Another projection system that may relate to the placebo effect is the serotonin system through its relationship with mood and stress (Lucki, 1998). One trial found that changes in brain glucose metabolism using PET were in similar brain regions of patients responding to placebo and to fluoxetine during treatment of depression, including increases in prefrontal, anterior cingulate and other cortical and subcortical regions (Mayberg et al., 2002). Unfortunately, the placebo arm contained some counselling or other active intervention. This highlights the difficulty of evaluating placebo effects in depression because of the reliance on data from placebo arms of clinical trials that do not have an adequate control group for studying placebo effects.
Neuroimaging techniques have implicated specific brain regions in placebo effect. The ACC is an important anatomical component of the dopaminergic as well as opioid system and has been activated during placebo analgesia (Petrovic et al., 2002; Lieberman et al., 2004; Koyama et al., 2005; Zubieta et al., 2005; Bingel et al., 2006; Kong et al., 2006; Wager et al., 2004, 2007), placebo anxiety relief (Petrovic et al., 2005), mood improvement in the placebo arm of an antidepressant trial (Mayberg et al., 2002) and improvements in mood associated with administration of placebo (Mayberg et al., 2002). Using an analysis technique to evaluate interactions of activation areas on functional neuroimaging, placebo analgesia ACC activation has correlated with activation in periaqueductal grey (Petrovic et al., 2002; Bingel et al., 2006; Wager et al., 2007).
The two-way communication between the brain and the immune system (Ader et al., 2001), contributes to aspects of the placebo response, both in its potential relationship to conditioning and in relationships mediated by stress and HPA axis activity (Ader, 2002). A beneficial immunosuppressive effect was obtained with placebo through conditioning of administration of cyclophosphamide with saccharine in a murine systemic erythematosus model (Ader and Cohen, 1982). Even a commonly used clinical immune marker, the tuberculin reaction, can be significantly diminished through conditioning (Smith and McDaniel, 1983). A small study suggested that conditioning can play a role in the treatment of neurological illness in humans. Pairing cyclophosphamide treatment for multiple sclerosis with a gustatory stimulus (anise-flavoured syrup) on five occasions resulted in the lowering of peripheral leucocyte counts in 8 of 10 subjects simply with administration of the anise-flavoured syrup (Giang et al., 1996).
Current experimental methodologies for placebo research
Studying placebo effects requires a control for the placebo condition. These studies require some deception, ranging from simply not informing subjects of the intention of the study to overt deception about the drug they are receiving. There are ethical guidelines guiding deception in a research study. These guidelines include the study should be minimal risk, there is no other way to answer the scientific question and there is a debriefing at the end of the study where subjects are told about the deception and they have the right to withhold their data (National Bioethics Advisory Commission, 2001; American Psychological Association, 2002). Research on acute placebo analgesia often uses a control condition where nothing is administered although other controls have been used. Much has been learned with this experimental paradigm although the application of knowledge learned from acute experimental pain in healthy subjects to the clinical condition is not straightforward (Vase et al., 2002). There are limited numbers of studies where anticipation of analgesia is developed by pill-taking over weeks (Lieberman et al., 2004). Another paradigm for studying placebo effects uses hidden versus open administration of active agents (Colloca et al., 2004) in postoperative patients with pain as well as in Parkinson's disease and in anxiety. While this is clearly relevant to the clinical situation, it is important to note that longer term administration of placebos in conventional clinical trials may produce less of an effect than that observed in many of the experimental placebo studies simply evaluating the immediate placebo effect (Hrobjartsson and Gotzsche, 2001; Vase et al., 2002). It has been observed that a clinical response from a placebo may be less sustainable than a response from an active agent (Fedele et al., 1989; Quitkin et al., 1991; Turner et al., 1994), and the sustainability of the placebo response remains to be explored.
Stress response and placebo effects
A clinical intervention may provide cognitive benefits due to stress reduction, decreased anxiety or improvement of mood. Mesolimbic and mesocortical modulations of the stress may be one mechanism of the clinically beneficial expectancy effect (Fricchione and Stefano, 2005). Level of anxiety correlated with placebo analgesia effect and this relationship was independent of the opioid system (Vase et al., 2005). Reduction in negative emotions may be a critical component of placebo analgesia (Vase et al., 2005) and perceived stress may impact placebo responsiveness to cognitive enhancement (Oken et al., 2008). Cortisol has also been altered by experimental manipulation of expectancy in placebo analgesia studies (Benedetti et al., 2003; Johansen et al., 2003). A formal meta-analysis suggested that non-suppression of cortisol on a dexamethasone suppression test predicted poorer response to placebo (Ribeiro et al., 1993). Many aspects of psychoneuroimmunology (Ader et al., 2001) may also contribute to aspects of the placebo response, both in its potential relationship to conditioning and in relationships mediated by stress that are affected by many facets of medical provider–patient interactions.
Placebo studies in clinical conditions
Pain
The pain system is the best-studied model of placebo effect (Turner et al., 1994). Following removal of impacted third mandibular molars, the reduction in pain perception from an inert substance experienced by placebo responder subjects could be attenuated with administration of naloxone while others without a placebo response had no change in pain when administered naloxone (Levine et al., 1978; Levine and Gordon, 1984). The latency of the improvement in pain ratings following intravenous administration of inert drug was >5 min. The response to placebo was greater in subjects who had higher initial pain ratings (Levine et al., 1979).
While naloxone may reverse placebo analgesia, there is another component of the placebo analgesic effect that is not blocked with naloxone (Gracely et al., 1983). From more recent research it appears that only some of the placebo analgesic effect is mediated via opioid pathways (Benedetti, 1996; Benedetti et al., 1997). In an ischaemic arm pain model in healthy humans, subjects were given either an opiate (morphine) or NSAID (ketorolac). Analgesia observed on the following day when subjects were given saline but told it was an active drug is presumably related to placebo effect. This improvement, postulated to be partially related to conditioning, can be blocked completely with naloxone following morphine days but not following ketorolac (Amanzio and Benedetti, 1999). In another study using the same experimental pain model, subjects were given either open or hidden injections of analgesic. Subjects had greater pain tolerance following open injection compared with hidden injections of analgesics and the greater pain tolerance in the open condition was associated with a significantly greater variability (Amanzio et al., 2001). Administration of naloxone following open administration of ketorolac decreased the analgesic response to be the same as that following hidden administration, suggesting that the improvement in analgesic response in the open condition compared with the hidden condition was mediated through opioid pathways. The authors reached similar conclusions in patients post-thoracotomy who could not be given naloxone (Amanzio et al., 2001). The variability being greater in the open condition is important: the measure being evaluated, total analgesic dose required by the patients, was significantly lower in the open than hidden condition but still had a greater variance. In some sense, responsiveness to placebo varied more across subjects than truly blinded (i.e. not knowing whether any medication was administered) response to analgesics.
In addition to opioids, cholecystokinin has been related to placebo analgesic effect (Benedetti et al., 1997). Proglumide, a cholecystokinin antagonist, has been shown to increase the placebo effect in an experimental pain condition (Benedetti, 1996). Of some interest, this effect was only seen in placebo responders and placebo non-responders had no change in pain with proglumide.
As mentioned earlier, PET and fMRI studies in healthy subjects during experimental pain have demonstrated that areas of activation by opioid and placebo analgesia were similar. The spatial extent and degree of cerebral activation was often greater for the opioid effect than for the placebo effect. There were differences in activation between the high and low placebo responders.
Parkinson's disease
Using a conservative definition of what would constitute a clinically relevant, objective placebo response in a clinical trial, researchers observed that one-sixth of subjects improved on placebo treatment (Goetz et al., 2000, 2002). There was not a no-treatment control group in these studies. Also, the objective improvement on the Unified Parkinson's Disease Rating Scale was not related to improvements in subjective changes raising the question of examiner biases. In a systematic review of the placebo effect in Parkinson's disease, responsiveness to placebo did not relate to age, gender, religion, level of education or duration of Parkinson's disease (Shetty et al., 1999; Goetz et al., 2000).
Patients with Parkinson's disease had PET scans using [11C]raclopride PET scanning without administration of any drugs and following blinded administration of placebo or apomorphine. Subjects receiving placebo demonstrated significant decrease in raclopride binding in the neostriatum consistent with endogenous dopamine release. The raclopride binding changes reflecting dopamine release in the caudate and putamen were ∼20% (de la Fuente-Fernandez et al., 2001). Motor testing was not performed at the same time since changes in motor performance would directly alter the PET scanning, so it is unclear how the PET results directly relate to motor improvements.
Expectancy effects related to surgery in Parkinson's disease have produced effects comparable with the surgery itself. Subjects believing they received real surgery had better outcomes than those believing it was sham surgery, whether or not they actually received the real or sham surgery (McRae et al., 2004). In a small number of Parkinson's disease patients who had subthalamic stimulators in place, there was better motor performance when subjects believed the stimulator was functioning compared with being told the stimulator was being turned down (Pollo et al., 2002) and there appeared to be increased subthalamic firing rates related to the placebo effect (Benedetti et al., 2004).
Multiple sclerosis
Some intervention studies have had more than one assessment prior to beginning active treatment so the placebo effect can be partially evaluated by comparing the placebo treatment data to the baseline period data. The placebo control group in one interferon β-1a study had a 20% decrease in MRI lesion number compared with the baseline period (OWIMS, 1999). In another interferon β-1a trial with just a single baseline assessment there was also a placebo-group improvement in MRI, as assessed by the number of gadolinium-enhanced lesions (Jacobs et al., 1996). However, given the unpredictable course of the disease, it is difficult to clearly differentiate placebo effect from natural history in the published multiple sclerosis trials.
Epilepsy
Significant improvements in frequency of seizures, usually defined as a >50% reduction, are not uncommon in placebo arms of anticonvulsant trials (Cereghino et al., 2000; Jones et al., 2002). However, as with multiple sclerosis, the disease course is relatively unpredictable and no trials have directly evaluated the placebo effect with a natural history control. Most current anticonvulsant trials are add-on or comparison trials so further data on placebo effect may be limited. Patients with non-epileptic seizures of psychogenic origin, may have their typical spells induced by placebo (saline injection, tilt table manoeuvre or simple suggestion) but a high false positive rate should preclude its routine clinical use (Bazil et al., 1994).
Ageing and dementia
Healthy 65-to- 85-year-old subjects taking a pill they are told was a cognitive enhancer performed better on word list delayed recall and several other cognitive tests than those not taking any pill (Oken et al., 2008). There was a suggestion this placebo effect was greater in subjects with higher self-rated stress as well as in older subjects. An improvement in cognition has also been seen during the first 1–2 months of double-blind placebo-controlled trials in Alzheimer disease (Rogers et al., 1996; Wilcock et al., 2000). These effects were not large and averaged only 0.5–1 point on the 70-point Alzheimer Disease Assessment Scale-Cognitive Subscale. These short-term improvements in placebo arms of trials are perhaps related to learning effect but some of the outcome measures are not very sensitive to learning effects and the learning effect would be expected to carry over into succeeding test sessions but it does not. Additionally, many patients with Alzheimer disease in clinical trials who have received placebo fare better than comparable prior natural history control data. Although this may also be related to placebo effect, there are other explanations as well, including subject selection and Hawthorne effects.
Subjects with Alzheimer disease are likely to have diminished or absent placebo effects at some point in the disease, perhaps related to frontal dysfunction. One recent study evaluated placebo analgesia in patients with Alzheimer disease through comparison of open and covert administration of lidocaine (Benedetti et al., 2006). The Alzheimer disease patients, with a mean Mini-Mental State Examination (MMSE) score of 24, demonstrated a placebo effect evidenced by increased effect of the open administration compared with covert administration of analgesic. At the time of follow-up a year later, with a reported mean MMSE score of 15.6, there was no longer evidence of a placebo effect. The size of the placebo effect was not correlated with MMSE but was correlated with performance on a frontal lobe assessment battery, with less impaired frontal function associated with greater expectancy effects.
Conclusions
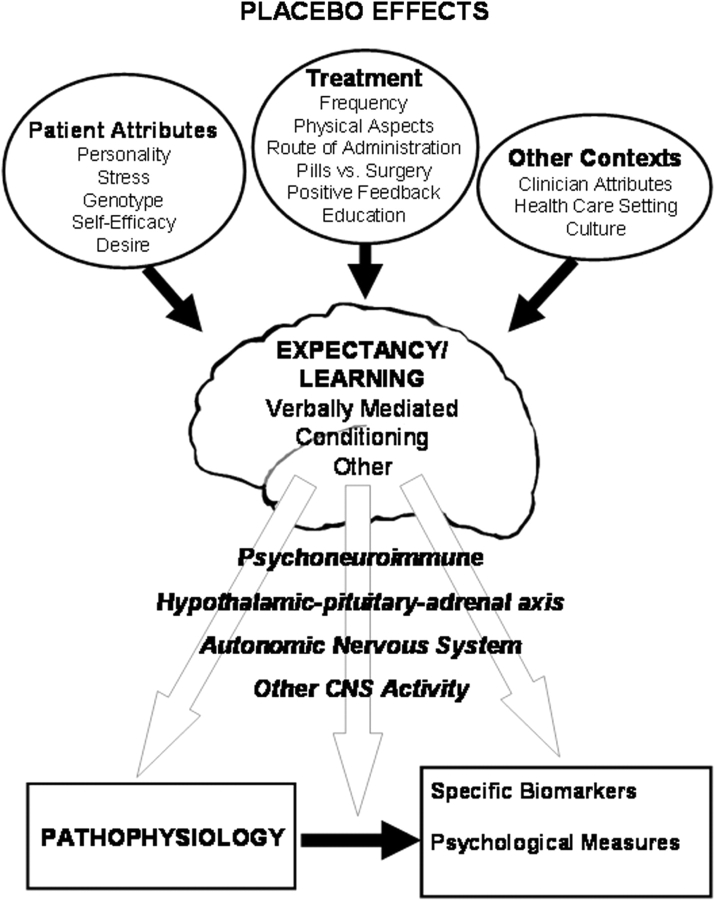
There are factors related to a clinical interaction that may produce improvement in patient outcomes without directly affecting the underlying pathophysiology of a disease. Methodological artefacts have contributed to confusion about these factors. However, there are clearly effects on outcomes that are dependent on patient expectations, whether these expectations are related to culture, previous interactions with the clinical setting, verbal communication, conditioning or some combination of these factors (Fig. 1). These placebo effects are mediated through changes in neocortical and subcortical systems. It will be helpful to have a biological understanding of the placebo effect in order to try to maximize people's health beyond simply the power of positive thinking. It is likely that some therapies and therapists have been successful in improving people's health because of their utilization of these beneficial effects. Sustaining these effects is important and many current placebo effect studies actually serve to extinguish the beneficial placebo response through lack of reinforcement of the response. Additionally, improving clinical trial design and interpretation will require a better understanding and characterization of non-specific responses comprising the placebo effect, potentially to ensure intervention groups are better matched on placebo responsiveness (or at least on expectancy of improvement), especially for non-blinded interventions.
Fig. 1.
Theoretical model of issues impacting development of expectancy and how brain outputs may produce a placebo effect.
Acknowledgement
This work was supported in part by funding from the National Institutes of Health U19 AT002656.
Glossary
Abbreviations:
- ACC
anterior cingulate cortex
- MMSE
Mini-Mental State Examination
- NSAID
non-steroidal anti-inflammatory drug
- PET
positron emission tomography
References
- Ader R. The placebo effect: if it's all your head, does that mean you only think you feel better? Adv Mind Body Med. 2000;16:7–11. doi: 10.1054/ambm.2000.0181. [DOI] [PubMed] [Google Scholar]
- Ader R. Conditioned immunomodulation: research needs and directions. Brain Behav Immun. 2002;17:S51–7. doi: 10.1016/s0889-1591(02)00067-3. [DOI] [PubMed] [Google Scholar]
- Ader R, Cohen N. Behaviorally conditioned immunosuppression and murine systemic lupus erythematosus. Science. 1982;215:1534–6. doi: 10.1126/science.7063864. [DOI] [PubMed] [Google Scholar]
- Ader R, Felten DL, Cohen N, editors. Psychoneuroimmunology. San Diego: Academic Press; 2001. [Google Scholar]
- Amanzio M, Benedetti F. Neuropharmacological dissection of placebo analgesia: expectation-activated opioid systems versus conditioning-activated specific subsystems. J Neurosci. 1999;19:484–94. doi: 10.1523/JNEUROSCI.19-01-00484.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amanzio M, Pollo A, Maggi G, Benedetti F. Response variability to analgesics: a role for non-specific activation of endogenous opioids. Pain. 2001;90:205–15. doi: 10.1016/S0304-3959(00)00486-3. [DOI] [PubMed] [Google Scholar]
- American Psychological Association. Ethical principles of psychologists and code of conduct. Am Psychol. 2002;57:1060–73. [PubMed] [Google Scholar]
- Anda R, Williamson D, Jones D, Moacera C, Eaker E, Glassman A, et al. Depressed affect, hopelessness, and the risk of ischemic heart disease in a cohort of U.S. adults. Epidemiology. 1993;4:285–94. doi: 10.1097/00001648-199307000-00003. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: the exercise of control. New York: W. H. Freeman and Company; 1997. [Google Scholar]
- Barsky AJ, Saintfort R, Rogers MP, Borus JF. Nonspecific medication side effects and the nocebo phenomenon. JAMA. 2002;287:622. doi: 10.1001/jama.287.5.622. [DOI] [PubMed] [Google Scholar]
- Bausell RB, Lao L, Bergman S, Lee WL, Berman BM. Is acupuncture analgesia an expectancy effect? Preliminary evidence based on participants’ perceived assignments in two placebo-controlled trials. Eval Health Prof. 2005;28:9–26. doi: 10.1177/0163278704273081. [DOI] [PubMed] [Google Scholar]
- Bazil CW, Kothari M, Luciano D, Moroney J, Song S, Vasquez B, et al. Provocation of non-epileptic seizures by suggestion in a general seizure population. Epilepsia. 1994;35:768–70. doi: 10.1111/j.1528-1157.1994.tb02509.x. [DOI] [PubMed] [Google Scholar]
- Benedetti F. The opposite effects of the opiate antagonist naloxone and the cholecystokinin antagonist proglumide on placebo analgesia. Pain. 1996;64:535–43. doi: 10.1016/0304-3959(95)00179-4. [DOI] [PubMed] [Google Scholar]
- Benedetti F, Amanzio M, Casadio C, Oliaro A, Maggi G. Blockade of nocebo hyperalgesia by the cholecystokinin antagonist proglumide. Pain. 1997;71:135–40. doi: 10.1016/s0304-3959(97)03346-0. [DOI] [PubMed] [Google Scholar]
- Benedetti F, Arduino C, Costa S, Vighetti S, Tarenzi L, Rainero I, et al. Loss of expectation-related mechanisms in Alzheimer's disease makes analgesic therapies less effective. Pain. 2006;121:133–44. doi: 10.1016/j.pain.2005.12.016. [DOI] [PubMed] [Google Scholar]
- Benedetti F, Colloco L, Torre E, Lanotte M, Melcarne A, Pesare M, et al. Placebo-responsive Parkinson patients show decreased activity in single neurons of subthalamic nucleus. Nat Neurosci. 2004;7:587–8. doi: 10.1038/nn1250. [DOI] [PubMed] [Google Scholar]
- Benedetti F, Mayberg HS, Wager TD, Stohler CS, Zubieta J-K. Neurobiological mechanisms of the placebo effect. J Neurosci. 2005;25:10390–402. doi: 10.1523/JNEUROSCI.3458-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benedetti F, Pollo A, Lopiano L, Lanotte M, Vighetti S, Rainero I. Conscious expectation and unconscious conditioning in analgesic, motor, and hormonal placebo/nocebo responses. J Neurosci. 2003;23:4315–23. doi: 10.1523/JNEUROSCI.23-10-04315.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergmann J-F, Chassany O, Gandiol J, Deblois P, Kanis JA, Segrestaa J-M, et al. A randomised clinical trial of the effect of informed consent on the analgesic activity of placebo and naproxen in cancer pain. Clin Trials Metaanal. 1994;29:41–7. [PubMed] [Google Scholar]
- Bingel U, Lorenz J, Schoell E, Weiller C, Buchel C. Mechanisms of placebo analgesia: rACC recruitment of a subcortical antinocideptive network. Pain. 2006;120:8–15. doi: 10.1016/j.pain.2005.08.027. [DOI] [PubMed] [Google Scholar]
- Bok S. Ethical issues in use of placebo in medical practice and clinical trials. In: Guess HA, Kleinman A, Kusek JW, Engel LW, editors. The science of the placebo. London: Br Med J Books; 2002. pp. 53–74. [Google Scholar]
- Bouchet C, Guillemin F, Briancon S. Nonspecific effects in longitudinal studies: impact on quality of life measures. J Clin Epidemiol. 1996;49:15–20. doi: 10.1016/0895-4356(95)00540-4. [DOI] [PubMed] [Google Scholar]
- Branthwaite A, Cooper P. Analgesic effects of branding in treatment of headaches. Br Med J. 1981;282:1576–8. doi: 10.1136/bmj.282.6276.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody HM. The placebo response. J Fam Pract. 2000;49:649–54. [PubMed] [Google Scholar]
- Buckalew L. An analysis of experimental components in a placebo effect. Psychol Rec. 1972;22:113–9. [Google Scholar]
- Brody H, Brody D. Three perspectives on the placebo response: expectancy, conditioning, and meaning. Adv Mind Body Med. 2000;16:216–32. doi: 10.1054/ambm.2000.0183. [DOI] [PubMed] [Google Scholar]
- Buckalew L, Coffield KE. An investigation of drug expectancy as a function of capsule color and size and preparation form. J Clin Psychopharmacol. 1982;2:245–8. [PubMed] [Google Scholar]
- Buckalew L, Ross S. Relationship of perceptual characteristics to efficacy of placebos. Psychol Rep. 1981;49:955–61. doi: 10.2466/pr0.1981.49.3.955. [DOI] [PubMed] [Google Scholar]
- Buckalew L, Ross S, Starr JB. Nonspecific factors in drug effects: placebo personality. Psychol Rep. 1981;48:3–8. doi: 10.2466/pr0.1981.48.1.3. [DOI] [PubMed] [Google Scholar]
- Butler C, Steptoe A. Placebo responses: an experimental study of psychophysiological processes in asthmatic volunteers. Br J Clin Psychol. 1986;25:173–83. doi: 10.1111/j.2044-8260.1986.tb00693.x. [DOI] [PubMed] [Google Scholar]
- Caspi O, Bootzin RR. Evaluating how placebos produce change: logical and causal traps and understanding cognitive explanatory mechanisms. Eval Health Prof. 2002;25:436–64. doi: 10.1177/0163278702238056. [DOI] [PubMed] [Google Scholar]
- Cereghino JJ, Biton V, Abou-Khalil B, Dreifuss F, Gauer LJ, Leppik I. Levetiracetam for partial seizures. Neurology. 2000;55:236–42. doi: 10.1212/wnl.55.2.236. [DOI] [PubMed] [Google Scholar]
- Challis GB, Stam HJ. A longitudinal study of the development of anticipatory nausea and vomiting in cancer chemotherapy patients: the role of absorption and autonomic perception. Health Psychol. 1992;11:181–9. doi: 10.1037//0278-6133.11.3.181. [DOI] [PubMed] [Google Scholar]
- Chaput de Saintonge DM, Herxheimer A. Harmessing placebo effects in health care. Lancet. 1994;344:995–8. doi: 10.1016/s0140-6736(94)91647-0. [DOI] [PubMed] [Google Scholar]
- Clayden JR, Bell JW, Pollard P. Menopausal flushing: double-blind trial of a non-hormonal medication. Br Med J. 1974;1:409–12. doi: 10.1136/bmj.1.5905.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobb LA, Thomas GI, Dillard DH, Merendind KA, Bruce RA. An evaluation of internal-mammary-artery ligation by a double-blind technic. N Engl J Med. 1959;260:1115–8. doi: 10.1056/NEJM195905282602204. [DOI] [PubMed] [Google Scholar]
- Colloca L, Benedetti F. Placebos and painkillers: is mind as real as matter? Nat Rev Neurosci. 2005;6:545–51. doi: 10.1038/nrn1705. [DOI] [PubMed] [Google Scholar]
- Colloca L, Lopiano L, Lanotte M, Benedetti F. Overt versus covert treatment for pain, anxiety, and Parkinson's disease. Lancet Neurol. 2004;3:679–84. doi: 10.1016/S1474-4422(04)00908-1. [DOI] [PubMed] [Google Scholar]
- Crow R, Gage H, Hampson S, Hart J, Kimber A, Thomas H. The role of expectancies in the placebo effect and their use in the delivery of health care: a systematic review. Health Technol Assess. 1999;3:1–48. [PubMed] [Google Scholar]
- Daniels AM. Headache, lumbar pucture, and expectation. Lancet. 1981;1:1003. doi: 10.1016/s0140-6736(81)91771-2. [DOI] [PubMed] [Google Scholar]
- de Craen AJ, Moerman DE, Heisterkamp SH, Tytgat GN, Tijssen JG, Kleijnen J. Placebo effect in the treatment of duodenal ulcer. J Clin Pharmacol. 1999;48:853–60. doi: 10.1046/j.1365-2125.1999.00094.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Craen AJM, Tijssen JGP, de Gens J, Kleijnen J. Placebo effect in the acute treatment of migraine: subcutaneous placebos are better than oral placebo. J Neurol. 2000;247:183–8. doi: 10.1007/s004150050560. [DOI] [PubMed] [Google Scholar]
- de la Fuente-Fernandez R, Ruth TJ, Sossi V, Schulzer M, Calne DB, Stoessl AJ. Expectation and dopamine release: mechanism of the placebo effect in Parkinson's disease. Science. 2001;293:1164–6. doi: 10.1126/science.1060937. [DOI] [PubMed] [Google Scholar]
- Di Blasi Z, Harkness E, Ernst E, Georgiou A, Kleijnen J. Influence of context effects on health outcomes: a systematic review. Lancet. 2001;357:757–62. doi: 10.1016/s0140-6736(00)04169-6. [DOI] [PubMed] [Google Scholar]
- Evans FJ. Expectancy, therapeutic instructions, and the placebo response. In: White L, Tursky B, Schwartz GE, editors. Placebo: theory, research, and meachnisms. New York: The Guilford Press; 1985. pp. 215–28. [Google Scholar]
- Fedele L, Marchini M, Acaia B, Garagiola U, Tiengo M. Dynamics and significance of placebo response in primary dysmenorrhea. Pain. 1989;36:43–7. doi: 10.1016/0304-3959(89)90110-3. [DOI] [PubMed] [Google Scholar]
- Flegal KE, Kishiyama S, Zajdel D, Haas M, Oken BS. Adherence to yoga and exercise interventions in a 6-month clinical trial. BMC Complement Altern Med. 2007;7:37. doi: 10.1186/1472-6882-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freed CR, Greene PE, Breeze RE, Tsai W-Y, DuMouchel W, Kao R, et al. Transplantation of embryonic dopamine neurons for severe Parkinson's disease. N Engl J Med. 2001;344:710–9. doi: 10.1056/NEJM200103083441002. [DOI] [PubMed] [Google Scholar]
- Freeman TB, Vawter DE, Leaverton PE, Godbold JH, Hauser RA, Goetz CG, et al. Use of placebo surgery in controlled trials of a cellular-based therapy for Parkinson's disease. N Engl J Med. 1999;341:988–92. doi: 10.1056/NEJM199909233411311. [DOI] [PubMed] [Google Scholar]
- Freund J, Krupp G, Goodenough D, Preston LW. The doctor-patient relationship and drug effect. Clin Pharmacol Ther. 1972;13:172–80. doi: 10.1002/cpt1972132172. [DOI] [PubMed] [Google Scholar]
- Fricchione G, Stefano GB. Placebo neural systems: nitric oxide, morphine and the dopamine brain reward and motivation circuitries. Med Sci Monit. 2005;11:MS54–65. [PubMed] [Google Scholar]
- Geers AL, Helfer SG, Kosbab K, Weiland PE, Landry SJ. Reconsidering the role of personality in placebo effects: dispositional optimism, situational expectations, and the placebo response. J Psychosom Res. 2005;58:121–7. doi: 10.1016/j.jpsychores.2004.08.011. [DOI] [PubMed] [Google Scholar]
- Geers AL, Koshab K, Helfer SG, Weiland PE, Wellman JA. Further evidence for individual differences in placebo responding: an interactionist perspective. J Psychosom Res. 2007;62:563–70. doi: 10.1016/j.jpsychores.2006.12.005. [DOI] [PubMed] [Google Scholar]
- Giang DW, Goodman AD, Schiffer RB, Mattson DH, Petrie M, Cohen N, et al. Conditioning of cyclophosphamide-induced leukopenia in humans. J Neuropsychiatry. 1996;8:194–201. doi: 10.1176/jnp.8.2.194. [DOI] [PubMed] [Google Scholar]
- Goetz CG, Leurgan S, Raman R, Group PS. Placebo-associated improvements in motor function: comparison of subjective and objective sections of the UPDRS in early Parkinson's disease. Mov Disord. 2002;17:283–8. doi: 10.1002/mds.10024. [DOI] [PubMed] [Google Scholar]
- Goetz CG, Leurgan S, Raman R, Stebbins G. Objective changes in motor function during placebo treatment in PD. Neurology. 2000;54:710–9. doi: 10.1212/wnl.54.3.710. [DOI] [PubMed] [Google Scholar]
- Gracely RH, Dubner R, Wolskee PJ, Deeter WR. Placebo and naloxone can alter postsurgical pain by separate mechanisms. Nature. 1983;306:264–5. doi: 10.1038/306264a0. [DOI] [PubMed] [Google Scholar]
- Gracely RH, Dubner R, Deeter WR, Wolskee PJ. Clinicians' expectation influence placebo analgesia. Lancet. 1985;1:43. doi: 10.1016/s0140-6736(85)90984-5. [DOI] [PubMed] [Google Scholar]
- Gryll SL, Karahn M. Situational factors contributing to the placebo effect. Psychophamacology. 1978;57:253–61. doi: 10.1007/BF00426747. [DOI] [PubMed] [Google Scholar]
- Guess HA, Kleinman A, Kusek JW, Engel LW, editors. The science of placebo. London: BMJ Books; 2002. [Google Scholar]
- Hahn RA. The nocebo phemomenon: concept, evidence, and implications for public health. Prev Med. 1997;26:607–11. doi: 10.1006/pmed.1996.0124. [DOI] [PubMed] [Google Scholar]
- Hashish I, Hai HK, Harvey W, Feinmann C, Harris M. Reduction of postoperative pain and swelling by ultrasound treatment: a placebo effect. Pain. 1988;33:303–11. doi: 10.1016/0304-3959(88)90289-8. [DOI] [PubMed] [Google Scholar]
- Holroyd KA, Penzien DB, Hursey KG, Tobin DL, Rogers L, Holm JE, et al. Change mechanisms in EMG biofeedback training: cognitive changes underlying improvements in tension headache. J Consult Clin Psychol. 1984;52:1039–53. doi: 10.1037//0022-006x.52.6.1039. [DOI] [PubMed] [Google Scholar]
- Horng S, Miller FG. Is placebo surgery unethical. N Engl J Med. 2002;347:137–9. doi: 10.1056/NEJMsb021025. [DOI] [PubMed] [Google Scholar]
- Horwitz RI, Viscoli CM, Berkman L, Donaldson RM, Horwitz S, Murray CJ, et al. Treatment adherence and risk of death after a myocardial infarction. Lancet. 1990;336:542–5. doi: 10.1016/0140-6736(90)92095-y. [DOI] [PubMed] [Google Scholar]
- Hrobjartsson A, Gotzsche PC. Is the placebo powerless? An analysis of clinical trials comparing placebo with no treatment. N Engl J Med. 2001;344:1594–620. doi: 10.1056/NEJM200105243442106. [DOI] [PubMed] [Google Scholar]
- Hyland ME, Whalley B, Geraghty AWA. Dispositional predictors of placebo responding: a motivational interpretation of flower essence and gratitude therapy. J Psychosom Res. 2007;62:331–40. doi: 10.1016/j.jpsychores.2006.10.006. [DOI] [PubMed] [Google Scholar]
- Ilnyckyj A, Shanahan F, Anton PA, Cheang M, Bernstein CN. Quantification of the placebo response in ulcerative colitis. Gastroenterology. 1997;112:1854–8. doi: 10.1053/gast.1997.v112.pm9178676. [DOI] [PubMed] [Google Scholar]
- Irizarry KJL, Licinio J. An explanation for the placebo effect? Science. 2005;307:1411–2. doi: 10.1126/science.307.5714.1411. [DOI] [PubMed] [Google Scholar]
- Jacobs LD, Cookfair DL, Rudick RA, Herndon RM, Richert JR, Salazar AM, et al. Intramuscular interferon beta-1a for disease progression in relapsing multiple sclerosis. Ann Neurol. 1996;39:285–94. doi: 10.1002/ana.410390304. [DOI] [PubMed] [Google Scholar]
- Johansen O, Brox J, Flaten MA. Placebo and nocebo responses, cortisol, and circulating beta-endorphin. Psychosom Med. 2003;65:786–90. doi: 10.1097/01.psy.0000082626.56217.cf. [DOI] [PubMed] [Google Scholar]
- Jones MW, Blume WT, Guberman A, Lee MA, Pillay N, Weaver DE, et al. Remacemide hydrochloride as an add-on therapy in epilepsy: a randomized, placebo-controlled trial of three dose levels (300, 600 and 800 mg/day) in a B.I.D. regimen. Seizure. 2002;11:104–13. doi: 10.1053/seiz.2002.0589. [DOI] [PubMed] [Google Scholar]
- Jones RE, Moes N, Zwickey H, Cunningham CL, Gregory WL, Oken B. Treatment of experimental autoimmune encephalomyelitis with alpha lipoic acid and associative conditioning. Brain, Behavior and Immunity. 2008;22:538–43. doi: 10.1016/j.bbi.2007.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaasinen V, Aalto S, Nagren K, Rinne JO. Expectation of caffeine induces dopaminergic responses in humans. Eur J Neurosci. 2004;19:2352–6. doi: 10.1111/j.1460-9568.2004.03310.x. [DOI] [PubMed] [Google Scholar]
- Kaptchuk TJ. Concerns about run-in periods in randomized trials. JAMA. 1998a;279:1526–7. [PubMed] [Google Scholar]
- Kaptchuk TJ. Powerful placebo: the dark side of the randomised controlled trial. Lancet. 1998b;351:1722–5. doi: 10.1016/S0140-6736(97)10111-8. [DOI] [PubMed] [Google Scholar]
- Kaptchuk TJ, Goldman P, Stone DA, Stason WB. Do medical devices have enhanced placebo effects? J Clin Epidemiol. 2000;53:786–92. doi: 10.1016/s0895-4356(00)00206-7. [DOI] [PubMed] [Google Scholar]
- Kemeny ME, Rosenwasser LJ, Panettieri RA, Rose RM, Berg-Smith SM, Kline JN. Placebo response in asthma: a robust and objective phenomenon. J Allergy Clin Immunol. 2007;119:1375–81. doi: 10.1016/j.jaci.2007.03.016. [DOI] [PubMed] [Google Scholar]
- Kienle GS, Kiene H. The powerful placebo effect: fact or fiction? J Clin Epidemiol. 1997;50:1311–8. doi: 10.1016/s0895-4356(97)00203-5. [DOI] [PubMed] [Google Scholar]
- Kirsch I. Conditioning, expectancy, and the placebo effect: comment on Stewart-Williams and Podd. Psychol Bull. 2004;130:341–3. doi: 10.1037/0033-2909.130.2.341. [DOI] [PubMed] [Google Scholar]
- Kirsch I, Weixel LJ. Double-blind versus deceptive administration of a placebo. Behav Neurosci. 1988;102:319–23. doi: 10.1037//0735-7044.102.2.319. [DOI] [PubMed] [Google Scholar]
- Kleijnen J, de Craen AJ, van Everdingen J, Krol L. Placebo effect in double-blind clinical trials: a review of interactions with medications. Lancet. 1994;344:1347–9. doi: 10.1016/s0140-6736(94)90699-8. [DOI] [PubMed] [Google Scholar]
- Kong J, Gollub RL, Rosman IS, Webb JM, Vangel MG, Kirsch I, et al. Brain activity associated with expectancy-enhanced placebo analgesia as measured by functional magnetic resonance imaging. J Neurosci. 2006;26:381–8. doi: 10.1523/JNEUROSCI.3556-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koyama T, McHaffie JG, Laurienti PJ, Coghill RC. The subjective experience of pain: Where expectations become reality. Proc Natl Acad Sci. 2005;102:12950–5. doi: 10.1073/pnas.0408576102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamb GC, Green SS, Heron J. Can physicians warn patients of potential side effects without fear of causing those side effect? Arch Intern Med. 1994;154:2753–6. doi: 10.1001/archinte.1994.00420230150018. [DOI] [PubMed] [Google Scholar]
- Laska E, Sunshine A. Anticipation of analgesia a placebo effect. Headache. 1973;13:1–11. doi: 10.1111/j.1526-4610.1973.hed1301001.x. [DOI] [PubMed] [Google Scholar]
- Lee PCL, Jawad MSM, Hull JD, West WHL, Shaw K, Eccles R. The antitussive effect of placebo treatment on cough associated with acute upper respiratory infection. Psychosom Med. 2005;67:314–7. doi: 10.1097/01.psy.0000155667.59662.92. [DOI] [PubMed] [Google Scholar]
- Levine JD, Gordon NC. Influence of the method of drug administration on analgesic response. Nature. 1984;312:755–6. doi: 10.1038/312755a0. [DOI] [PubMed] [Google Scholar]
- Levine JD, Gordon NC, Bornstein JC, Fields HL. Role of pain in placebo analgesia. Proc Natl Acad Sci. 1979;76:3528–31. doi: 10.1073/pnas.76.7.3528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine JD, Gordon NC, Fields HL. The mechanism of placebo analgesia. Lancet. 1978;2:654–7. doi: 10.1016/s0140-6736(78)92762-9. [DOI] [PubMed] [Google Scholar]
- Lieberman MD, Jarcho JM, Berman S, Naliboff BD, Suyenobu BY, Mandelkern M, et al. The neural correlates of placebo effects: a disruption account. Neuroimage. 2004;22:447–55. doi: 10.1016/j.neuroimage.2004.01.037. [DOI] [PubMed] [Google Scholar]
- Lotshaw SC, Bradley JR, Brooks LR. Illustrating caffeine's pharmacological and expectancy effects utilizing a balanced placebo design. J Drug Educ. 1996;26:13–24. doi: 10.2190/UUCL-E5V6-XC25-5MC6. [DOI] [PubMed] [Google Scholar]
- Lucki I. The spectrum of behaviors influenced by serotonin. Biol Psychol. 1998;44:151–62. doi: 10.1016/s0006-3223(98)00139-5. [DOI] [PubMed] [Google Scholar]
- Luparello TJ, Leist N, Lourie CH, Sweet P. The interaction of psychologic stimuli and pharmacologic agents on airway reactivity in asthmatic subjects. Psychosom Med. 1970;32:509–13. doi: 10.1097/00006842-197009000-00009. [DOI] [PubMed] [Google Scholar]
- Macklin R. Placebo surgery in trials of therapy for Parkinson's disease. N Engl J Med. 2000;342:353–5. doi: 10.1056/NEJM200002033420512. [DOI] [PubMed] [Google Scholar]
- Martikainen IK, Hagelberg N, Mansikka H, Hietala J, Nagren K, Scheinin H. Association of striatal dopamine D2/D3 receptor binding potential with pain but not tactile sensitivity or placebo analgesia. Neurosci Lett. 2005;376:149–53. doi: 10.1016/j.neulet.2004.11.045. [DOI] [PubMed] [Google Scholar]
- Maruta T, Colligan RC, Malinchoc M, Offord KP. Optimism-pessimism assessed in the 1960s and self-reported health status 30 years later. Mayo Clin Proc. 2002;77:748–53. doi: 10.4065/77.8.748. [DOI] [PubMed] [Google Scholar]
- Mayberg HS, Silva JA, Brannan SK, Tekell JL, Mahurin RK, McGinnis S, et al. The functional neuroanatomy of the placebo effect. Am J Psychiatry. 2002;159:728–37. doi: 10.1176/appi.ajp.159.5.728. [DOI] [PubMed] [Google Scholar]
- McDonald CJ, Mazzuca SA. How much of the placebo ‘effect’ is really statistical regression? Stat Med. 1983;2:417–27. doi: 10.1002/sim.4780020401. [DOI] [PubMed] [Google Scholar]
- McNair DM, Barrett JE. Two Bass Scale factors and response to placebo and anxiolytic drugs. Psychopharmacology. 1979;65:165–70. doi: 10.1007/BF00433044. [DOI] [PubMed] [Google Scholar]
- McRae C, Cherin E, Yamazaki G, Diem G, Vo AH, Russell D, et al. Effects of perceived treatment on quality of life and medical outcomes in a double-blind placebo surgery trial. Arch Gen Psychiatry. 2004;61:412–20. doi: 10.1001/archpsyc.61.4.412. [DOI] [PubMed] [Google Scholar]
- Merz M, Seiberling M, Hoxter G, Holting M, Wortha H. Elevation of liver enzymes in multiple dose trials during placebo treatment: are they predictable? J Clin Pharmacol. 1997;37:791–8. doi: 10.1002/j.1552-4604.1997.tb05626.x. [DOI] [PubMed] [Google Scholar]
- Miller FG, Emanuel EJ, Rosenstein DL, Straus SE. Ethical issues concerning research in complementary and alternative medicine. JAMA. 2004;291:599–604. doi: 10.1001/jama.291.5.599. [DOI] [PubMed] [Google Scholar]
- Mitchell SH, Laurent CL, de Witt H. Interaction of expectancy and the pharmacological effects of d-amphetamine: subjective effects and self-administration. Psychophamacologia. 1996;125:371–8. doi: 10.1007/BF02246020. [DOI] [PubMed] [Google Scholar]
- Moerman DE. Cultural variations in the placebo effect: ulcers, anxiety, and blood pressure. Med Anthropol Q. 2000;14:51–72. doi: 10.1525/maq.2000.14.1.51. [DOI] [PubMed] [Google Scholar]
- Moerman DE. Explanatory mechanisms for placebo effects: cultural influences and the meaning response. In: Guess HA, Kleinman A, Kusek JW, Engel LW, editors. The science of the placebo. London: BMJ Books; 2002. pp. 77–107. [Google Scholar]
- Mondloch MV, Cole DC, Frank JW. Does how you do depend on how you think you'll do? A systematic review of the evidence ofr a relation between patients’ recovery expectations and health outcomes. Can Med Assoc J. 2001;165:174–9. [PMC free article] [PubMed] [Google Scholar]
- Montgomery GH, Kirsch I. Classical conditioning and the placebo effect. Pain. 1997;72:107–13. doi: 10.1016/s0304-3959(97)00016-x. [DOI] [PubMed] [Google Scholar]
- Moseley JB, O’Malley K, Petersen NJ, Menke TJ, Brody BA, Kuykendall DH, et al. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002;347:81–8. doi: 10.1056/NEJMoa013259. [DOI] [PubMed] [Google Scholar]
- National Bioethics Advisory Commission. 2001. Ethical and policy issues in research involving human participants. [PubMed] [Google Scholar]
- Oken BS. Placebo effect: clinical perspectives and potential mechanisms. In: Oken BS, editor. Complementary therapies in neurology: an evidence-based approach. New York: Parthenon Publishing; 2004. pp. 199–230. [Google Scholar]
- Oken BS, Flegal K, Zajdel D, Kishiyama S, Haas M, Peters D. Expectancy effect: impact of pill administration on cognitive performance in healthy seniors. J Clin Exp Neuropsychol. 2008;30:7–17. doi: 10.1080/13803390701775428. [DOI] [PubMed] [Google Scholar]
- Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–97. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- OWIMS. Evidence of interferon beta-1a dose response in relapsing-remitting MS: The OWIMS study. Neurology. 1999;53:679–86. doi: 10.1212/wnl.53.4.679. [DOI] [PubMed] [Google Scholar]
- Pablos-Mâendez A, Barr RG, Shea S. Run-in periods in randomized trials: implications for the application of results in clinical practice. JAMA. 1998;279:222–5. doi: 10.1001/jama.279.3.222. [DOI] [PubMed] [Google Scholar]
- Pariente J, White P, Frackowiak RSJ, Lewith G. Expectancy and belief modulate the neuronal substrates of pain treated by acupuncture. NeuroImage. 2005;25:1161–7. doi: 10.1016/j.neuroimage.2005.01.016. [DOI] [PubMed] [Google Scholar]
- Paternak MA, Zimmerman M. Therapeutic effect of follow-up assessments on antidepressant and placebo response rates in antidepressant efficacy trials. Br J Psychiatry. 2007;190:287–92. doi: 10.1192/bjp.bp.106.028555. [DOI] [PubMed] [Google Scholar]
- Paterson C, Dieppe P. Characteristic and incidental (placebo) effects in complext interventions such as acupuncture. Br Med J. 2005;330:1202–5. doi: 10.1136/bmj.330.7501.1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrovic P, Dietrich T, Fransson P, Andersson J, Carlsson K, Ingvar M. Placebo in emotional processing—induced expectations of anxiety relief activate a generalized modulatory network. Neuron. 2005;46:957. doi: 10.1016/j.neuron.2005.05.023. [DOI] [PubMed] [Google Scholar]
- Petrovic P, Kalso E, Petersson KM, Ingvar M. Placebo and opioid analgesia - imaging a shared neuronal network. Science. 2002;295:1737–40. doi: 10.1126/science.1067176. [DOI] [PubMed] [Google Scholar]
- Phillips PEM, Stuber GD, Helen MAV, Wightman RM, Carelli RM. Subsecond dopamine release promotes cocaine seeking. Nature. 2003;422:614–8. doi: 10.1038/nature01476. [DOI] [PubMed] [Google Scholar]
- Pollo A, Amanzio M, Arslanian A, Casadio C, Maggi G, Benedetti F. Response expectancies in placebo analgesia and their clinical relevance. Pain. 2001;93:77–84. doi: 10.1016/S0304-3959(01)00296-2. [DOI] [PubMed] [Google Scholar]
- Pollo A, Torre E, Lopiano L, Rizzone M, Lanotte M, Cavanna A, et al. Expectation modulates the response to subthalamic nucleus stimulation in Parkinsonian patients. Neuroreport. 2002;13:1383–6. doi: 10.1097/00001756-200208070-00006. [DOI] [PubMed] [Google Scholar]
- Pollo A, Vighetti S, Rainero I, Benedetti F. Placebo analgesia and the heart. Pain. 2003;102:125–33. doi: 10.1016/s0304-3959(02)00345-7. [DOI] [PubMed] [Google Scholar]
- Porter DR, Capell HA. The ‘Natural’ history of active rheumatoid arthritis over 3-6 Months — an analysis of patients enrolled into trials of potential disease-modifying anti-rheumatic drugs, and treated with placebo. Br J Rheumatol. 1993;32:463–6. doi: 10.1093/rheumatology/32.6.463. [DOI] [PubMed] [Google Scholar]
- Price DD, Finniss DG, Benedetti F. A comprehensive review of the placebo effect: recent advances and current thought. Ann Rev Psychol. 2008;59(2):1–2. doi: 10.1146/annurev.psych.59.113006.095941. 26. [DOI] [PubMed] [Google Scholar]
- Price DD, Milling LS, Kirsch I, Duff A, Montgomery GH, Nicholls SS. An analysis of factors that contribute to the magnitude of placebo analgesia in an experimental paradigm. Pain. 1999;83:147–56. doi: 10.1016/s0304-3959(99)00081-0. [DOI] [PubMed] [Google Scholar]
- Quitkin FM, McGrath PJ, Rabkin JG, Stewart JW, Harrison W, Ross DC, et al. Different types of placebo response in patients receiving antidepressants. Am J Psychiatry. 1991;148:197–203. doi: 10.1176/ajp.148.2.197. [DOI] [PubMed] [Google Scholar]
- Raz A. Hypnobo: perspectives on hypnosis and placebo. Am J Clin Hypn. 2007;50:29–36. doi: 10.1080/00029157.2007.10401595. [DOI] [PubMed] [Google Scholar]
- Ribeiro SC, Kennedy SE, Smith YR, Stohler CS, Zubieta J-K. Interface of physical and emotional stress regulation through the endogenous opioid system and [mu]-opioid receptors. Prog Neuropsychopharmacol Biol Psychiatry. 2005;29:1264–80. doi: 10.1016/j.pnpbp.2005.08.011. [DOI] [PubMed] [Google Scholar]
- Ribeiro SCM, Tandon R, Grunhaus L, Greden JF. The DST as a predictor of outcome in depression: a meta-analysis. Am J Psychiatry. 1993;150:1618–29. doi: 10.1176/ajp.150.11.1618. [DOI] [PubMed] [Google Scholar]
- Rochon PA, Binns MA, Litner JA, Litner GM, Fischbach MS, Eisenberg D, et al. Are randomized control trial outcomes influenced by the inclusion of a placebo group? a systematic review of nonsteroidal antiinflammatory drug trials for arthritis treatment. J Clin Epidemiol. 1999;52:113–22. doi: 10.1016/s0895-4356(98)00149-8. [DOI] [PubMed] [Google Scholar]
- Rogers SL, Friedhoff LT, Group at DS. The efficacy and safety of donepezil in patients with Alzheimer's disease: results of a US multicenter, randomized, double-blind, placebo-controlled trial. Dementia. 1996;7:293–303. doi: 10.1159/000106895. [DOI] [PubMed] [Google Scholar]
- Rohsenow DJ, Marlatt GA. The balanced placebo design: methodological considerations. Addict Behav. 1981;6:107–22. doi: 10.1016/0306-4603(81)90003-4. [DOI] [PubMed] [Google Scholar]
- Ross S, Krugman AD, Lyerly SB, Clyde DJ. Drugs and placebos: a model design. Psychol Rep. 1962;10:383–92. [Google Scholar]
- Schapira K, McClelland HA, Griffiths NR, Newell DJ. Study on the effects of tablet colour in the treatment of anxiety states. Br Med J. 1970;1:446–9. doi: 10.1136/bmj.2.5707.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schultz W. Behavioral theories and the neurophysiology of reward. Ann Rev Psychol. 2006;57:87–115. doi: 10.1146/annurev.psych.56.091103.070229. [DOI] [PubMed] [Google Scholar]
- Schwedt TJ, Hentz JG, Dodick DW. Factors associated with the prophylactic effect of placebo injections in subjects enrolled in a study of botulinum toxin for migraine. Cephalalgia. 2007;27:528–34. doi: 10.1111/j.1468-2982.2007.01332.x. [DOI] [PubMed] [Google Scholar]
- Scott DJ, Stohler CS, Egnatuk CM, Want H, Koeppe RA, Zubieta JK. Individual differences in reward responding explain placebo-induced expectations and effects. Neuron. 2007;55:325–36. doi: 10.1016/j.neuron.2007.06.028. [DOI] [PubMed] [Google Scholar]
- Shapiro DA. Comparative crediblity of treatment rationales: three tests of expectancy theory. Br J Clin Psychol. 1981;20:111–22. doi: 10.1111/j.2044-8260.1981.tb00504.x. [DOI] [PubMed] [Google Scholar]
- Shetty N, Friedman JH, Kieburtz K, Marshall FJ, Oakes D. The placebo response in Parkinson's disease. Clin Neuropharmacol. 1999;22:207–12. [PubMed] [Google Scholar]
- Siegel S. Explanatory mechanisms for placebo effects: Pavlovian conditioning. In: Guess HA, Kleinman A, Kusek JW, Engel LW, editors. The science of the placebo. London: BMJ Books; 2002. [Google Scholar]
- Sievenpiper JL, Eztagha A, Dascalu A, Vuksan V. When a placebo is not a ‘placebo'l a placebo effect on postprandial glycaemia. Br J Clin Pharmacol. 2007;64:546–9. doi: 10.1111/j.1365-2125.2007.02929.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson SH, Eurich DT, Majumdar SR, Padwal RS, Tsuyuki RT, Varney J, et al. A meta-analysis of the association between adherence to drug therapy and mortality. Br Med J. 2006;333:15–20. doi: 10.1136/bmj.38875.675486.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skovlund E. Should we tell trial patients that they might receive placebo? Lancet. 1991;337:1041. doi: 10.1016/0140-6736(91)92701-3. [DOI] [PubMed] [Google Scholar]
- Smith GR, McDaniel SM. Psychologically mediated effect on the delayed hypersensitivity reaction to tuberculin in humans. Psychosom Med. 1983;45:65–70. doi: 10.1097/00006842-198303000-00009. [DOI] [PubMed] [Google Scholar]
- Sox HC, Margulies I, Sox CH, Alto P. Psychologically medicated effects of diagnostic tests. Ann Inter Med. 1981;95:680–5. doi: 10.7326/0003-4819-95-6-680. [DOI] [PubMed] [Google Scholar]
- Stefano GB, Fricchione GL, Slingsby BT, Benson H. The placebo effect and relaxation response: neural processes and their coupling to constitutive nitric oxide. Brain Res Brain Res Rev. 2001;35:1–19. doi: 10.1016/s0165-0173(00)00047-3. [DOI] [PubMed] [Google Scholar]
- Stewart-Williams S, Podd J. The placebo effect: dissolving the expectancy versus conditioning debate. Psychol Bull. 2004;130:324–40. doi: 10.1037/0033-2909.130.2.324. [DOI] [PubMed] [Google Scholar]
- Stoessl AJ, de la Fuente-Fernandez R. Willing oneself better on placebo–effective in its own right. Lancet. 2004;364:227–8. doi: 10.1016/S0140-6736(04)16689-0. [DOI] [PubMed] [Google Scholar]
- Temple R. Placebo controlled trials and active controlled trials: ethics and inference. In: Guess HA, Kleinman A, Kusek JW, Engel LW, editors. The science of the placebo. London: BMJ Books; 2002. pp. 209–26. [Google Scholar]
- Thomas KB. General pratice consultations: is there any point in being positive? Br Med J. 1987;294:1200–2. doi: 10.1136/bmj.294.6581.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner JA, Deyo RA, Loeser JD, Von Korff M, Fordyce WE. The importance of placebo effects in pain treatment and research. JAMA. 1994;271:1609–14. [PubMed] [Google Scholar]
- Uhlenhuth EH, Rickels K, Fisher S, Park LC, Lipman RS, Mock J. Drug, doctor's verbal attitude and clinic setting in the symptomatic response to pharmacotherapy. Psychopharmacologia. 1966;9:392–418. doi: 10.1007/BF00406450. [DOI] [PubMed] [Google Scholar]
- van der Molen GM, van den Hout MA. Expectancy effects on respiration during lactate infusion. Psychosom Med. 1988;50:439–43. doi: 10.1097/00006842-198807000-00011. [DOI] [PubMed] [Google Scholar]
- van Dongen M, van Rossum E, Kessels A, Sielhorst H, Knipschild P. The efficacy of ginkgo for elderly people with dementia and age-associated memory impairment: new results of a randomized clinical trial. J Am Geriatr Soc. 2000;48:1183–94. doi: 10.1111/j.1532-5415.2000.tb02589.x. [DOI] [PubMed] [Google Scholar]
- Vase L, Riley JL, III, Price DD. A comparison of placebo effects in clinical analgesic trials versus studies of placebo analgesia. Pain. 2002;99:443–52. doi: 10.1016/S0304-3959(02)00205-1. [DOI] [PubMed] [Google Scholar]
- Vase L, Robinson ME, Verne GN, Price DD. Increased placebo analgesia over time in irritable bowel syndrome (IBS) patients is associated with desire and expectation but not endogenous opioid mechanisms. Pain. 2005;115:338–47. doi: 10.1016/j.pain.2005.03.014. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Wang G-J, Ma Y, Fowler JS, Zhu W, Maynard L, et al. Expectation enhances the regional brain metabolic and the reinforcing effects of stimulants in cocaine abusers. J Neurosci. 2003;23:11461–8. doi: 10.1523/JNEUROSCI.23-36-11461.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voudouris NJ, Peck CL, Coleman G. Conditioned response models of placebo phenomena: further support. Pain. 1989;38:109–16. doi: 10.1016/0304-3959(89)90080-8. [DOI] [PubMed] [Google Scholar]
- Wager TD, Rilling JK, Smith EE, Sokolik A, Casey KL, Davidson RJ, et al. Placebo-induced changes in FMRI in the anticipation and experience of pain. Science. 2004;303:1162–7. doi: 10.1126/science.1093065. [DOI] [PubMed] [Google Scholar]
- Wager TD, Scott DJ, Zubieta JK. Placebo effects on human µ—opioid activity during pain. PNAS. 2007;104:11056–61. doi: 10.1073/pnas.0702413104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walach H. The efficacy paradox in randomized controlled trials of CAM and elsewhere: beware of the placebo trap. J Altern Complement Med. 2001;7:213–8. doi: 10.1089/107555301300328070. [DOI] [PubMed] [Google Scholar]
- Wasan AD, Kaptchuk TJ, Davar G, Jamison RN. The association between psychopathology and placebo analgesia in patients with discogenic back pain. Pain Med. 2006;7:217–28. doi: 10.1111/j.1526-4637.2006.00154.x. [DOI] [PubMed] [Google Scholar]
- Wickramasekera I. How to produce not only powerful but, more importantly, reliable placebo healing and analgesia. Adv Mind Body Med. 2000;16:211–6. doi: 10.1054/ambm.2000.0183. [DOI] [PubMed] [Google Scholar]
- Wilcock G, Lilienfeld S, Gaens E. Efficacy and safety of galantamine in patients with mild to moderate Alzheimer's disease: multicentre randomised controlled trial. Galantamine International-1 Study Group. Br Med J. 2000;321:1445–9. doi: 10.1136/bmj.321.7274.1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zubieta J-K, Bueller JA, Jackson LR, Scott DJ, Xu Y, Koeppe RA, et al. Placebo effects mediated by endogenous opioid activity on mu opioid receptors. J Neurosci. 2005;25:7754–62. doi: 10.1523/JNEUROSCI.0439-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zubieta J-K, Yau W-Y, Scott DJ, Stohler CS. Belief or need? Accounting for individual variations in the neurochemistry of the placebo effect. Brain Behav Immun. 2006;20:15–26. doi: 10.1016/j.bbi.2005.08.006. [DOI] [PubMed] [Google Scholar]