Abstract
OBJECTIVE
Although asthma is often inappropriately treated in children, little is known about what information pediatricians use to adjust asthma therapy. The purpose of this work was to assess the importance of various dimensions of patient asthma status as the basis of pediatrician treatment decisions.
PATIENTS AND METHODS
We conducted a cross-sectional, random-sample survey, between November 2005 and May 2006, of 500 members of the American Academy of Pediatrics using standardized case vignettes. Vignettes varied in regard to (1) acute health care use (hospitalized 6 months ago), (2) bother (parent bothered by the child’s asthma status), (3) control (frequency of symptoms and albuterol use), (4) direction (qualitative change in symptoms), and (5) wheezing during physical examination. Our primary outcome was the proportion of pediatricians who would adjust treatment in the presence or absence of these 5 factors.
RESULTS
Physicians used multiple dimensions of asthma status other than symptoms to determine treatment. Pediatricians were significantly more likely to increase treatment for a recently hospitalized patient (45% vs 18%), a bothered parent (67% vs 18%), poorly controlled symptoms (4–5 times per week; 100% vs 18%), or if there was wheezing on examination (45% vs 18%) compared with patients who only had well-controlled symptoms. Pediatricians were significantly less likely to decrease treatment for a child with well-controlled symptoms and recent hospitalization (28%), parents who reported being bothered (43%), or a child whose symptoms had worsened since the last doctor visit (10%) compared with children with well-controlled symptoms alone.
CONCLUSIONS
Pediatricians treat asthma on the basis of multiple dimensions of asthma status, including hospitalization, bother, symptom frequency, direction, and wheezing but use these factors differently to increase and decrease treatment. Tools that systematically assess multiple dimensions of asthma may be useful to help further improve pediatric asthma care.
Keywords: asthma, pediatrics, treatment, decision-making, survey
The extent to which pediatricians use guideline-based criteria in their decision-making regarding the assignment of treatment to children with asthma is not known. Historically, national asthma guidelines recommended the assessment of symptom frequency to step up or step down treatment and, ultimately, to control asthma at the lowest possible level of therapy.1 However, there is limited research on what specific information pediatricians actually use for asthma treatment and the relative importance of symptom frequency in the treatment decision-making process. Understanding those factors important to clinicians’ decision-making in asthma therapy is particularly salient when considering strategies for improving physician adherence with guideline-based asthma care.
As part of a project to develop an asthma assessment tool for clinicians, we conducted focus groups with 2 types of clinicians representative of physicians who provide asthma care to children: generalists (pediatricians and family practitioners) and asthma specialists (allergists). The purpose of the focus groups was to learn what patient information is important to these physicians in assigning treatment for their pediatric patients.2 We found that clinicians in both focus groups incorporate multiple dimensions of health into their treatment decisions for asthma. Symptom frequency assessment was considered important but not sufficient for assigning treatment. Three other concepts emerged as important to clinicians in treating their patients: a history of acute care use (as risk factor for future poor outcomes), bother (an indicator of the emotional burden of asthma), and direction (the trajectory of symptoms, ie, whether the symptoms have improved, worsened, or remained stable). These findings suggested the need to better understand the relative importance of these different dimensions of asthma to clinicians’ decision-making in asthma therapy.
Toward that end, the purpose of the current study was to assess the relative importance of different dimensions of asthma status, beyond symptom frequency, used by pediatricians to assign treatment for asthma. Specifically, we sought to determine the importance of acute care, bother, control, and direction on decision-making regarding treatment of asthma by conducting a national survey of practicing pediatricians. We hypothesized that recent acute care use (hospitalization 6 months previous), bother (parent was bothered by the child’s asthma), poor asthma control (symptoms 4–5 times per week), and direction (worsening symptoms) would each independently influence treatment decisions in case-based vignettes.
METHODS
Sample
Five-hundred physicians of the American Academy of Pediatrics were randomly selected from a membership list as a means to identify pediatricians. We estimated sample size requirements to demonstrate absolute differences of 20% in treatment tendency, by each of the 4 study factors, with α at .05 and power at 0.80. We expected a response rate of ≤50%, given that physician study subjects typically have modest response rates.3 Eligibility criteria included being a fellow in the American Academy of Pediatrics, living in the United States and/or territories, and being active in clinical practice. Exclusions included nonpediatricians, specialists who do not provide asthma care to children, and physicians in training.
Questionnaire
Standardized vignettes were used in this study, because a vignette-based approach has been shown to be a valid method for determining physician practices.4–8 Vignettes also have advantages over studies of actual practice, in that study conditions can be controlled and the number of confounding variables can be limited. A disadvantage, of course, is that the results do not represent actual practice.7 As part of their development, vignettes and survey questions were reviewed by practicing pediatricians for clarity and comprehensibility.
We used 11 vignettes for these analyses (see Appendix 1 for example and Table 1 for concept map) with either low-intensity treatment (low-dose inhaled corticosteroid [ICS], eg, fluticasone [44 µg per puff], 2 puffs twice daily, and as-needed albuterol) or high-intensity treatment (high-dose ICS, eg, fluticasone [220 µg per puff], 2 puffs twice daily; long-acting inhaled β-agonist [LABA], leukotriene modifier [LTM]; and as-needed albuterol) to test whether each of the following factors affects stepping therapy up/down: (1) acute care: asthma hospitalization 6 months ago versus no emergency department hospitalization and/or intubation in the past 6 months; (2) bother: parent bothered by the child’s asthma versus not bothered; (3) control: wheeze and/or albuterol use once in the past 2 weeks versus wheeze and/or albuterol use 4 to 5 days per week in the past 2 weeks, reflecting well-controlled and poorly controlled status, respectively9; (4) direction: doing worse versus the same since the last visit; and (5) wheeze: the presence of wheezing on physical examination. The ages of children in the vignettes ranged from 5 to 10 years of age.
TABLE 1.
Concept Map of Vignettes
| Vignette | Treatment | Acute | Bother | Control | Direction | Wheeze |
|---|---|---|---|---|---|---|
| No. | Care | |||||
| 1a | Low intensity | No | No | Symptoms once per 2 wk | Unchanged | No |
| 2 | Low intensity | No | No | Symptoms once per 2 wk | Unchanged | Yes |
| 3 | Low intensity | Yes | No | Symptoms once per 2 wk | Unchanged | No |
| 4 | Low intensity | No | Yes | Symptoms once per 2 wk | Unchanged | No |
| 5 | Low intensity | No | No | Symptoms 4–5 times per wk | Unchanged | No |
| 6 | Low intensity | No | No | Symptoms once per 2 wk | Worse | No |
| 7b | High intensity | No | No | Symptoms once per 2 wk | Unchanged | No |
| 8 | High intensity | Yes | No | Symptoms once per 2 wk | Unchanged | No |
| 9 | High intensity | No | Yes | Symptoms once per 2 wk | Unchanged | No |
| 10 | High intensity | No | No | Symptoms once per 2 wk | Worse | No |
| 11 | High intensity | Yes | Yes | Symptoms once per 2 wk | Worse | No |
Low-intensity treatment indicates low ICS (fluticasone [44 µg per puff] 2 puffs twice per day) and albuterol as needed; high-intensity treatment, high ICS (fluticasone [220 µg per puff] 2 puffs twice per day), LABA, LTM, and albuterol as needed. Analyses compared vignettes 2, 3, 4, 5, and 6 with vignette 1 (stepping-up baseline), and vignettes 8, 9, 10, and 11 were compared with vignette 7 (stepping-down baseline).
Stepping-up baseline.
Stepping-down baseline.
The vignettes were of patients returning for a 3-month follow-up visit. On examination, all of the patients had good air movement, forced expiratory volume in 1 second at 90% predicted, and no other remarkable findings. A subset of vignettes reported the presence of faint wheezing on physical examination. The wheezing vignette was created to examine the influence of an abnormal physical examination finding in the absence of the 4 previously described factors (acute care, bother, control, and direction). For each vignette, physicians were asked if they would increase (step up), decrease (step down), or leave medications unchanged and, if they would change medications, to specify which medication(s) they would changes. This vignette protocol used by our research group has been reported previously.10 Physician demographic and practice information was collected. Specifically, physicians reported the volume of asthma patients seen on a weekly basis and rated their level of experience or expertise in treating asthma by using a 3-point Likert-type scale (limited, moderate, or extensive). This type of self-report of asthma experience has been shown to distinguish different levels of asthma expertise among physicians.11
Procedures
From November 2005 to May 2006, pediatricians were mailed a self-administered survey accompanied by a letter explaining the study purpose and a stamped return envelope. Nonrespondents received additional mailings at 2 and 4 weeks. A $10 remuneration was provided to all of the pediatricians with the first mailing. In addition, the first and second mailings were sent via US Postal Service Priority Mail. The study was approved by the Western Institutional Review Board (Spokane, WA).
Each pediatrician received 4 vignettes, because the burden of a longer survey was expected to reduce the response rate.12,13 The first 2 vignettes were the same for all of the respondents and represented baselines for stepping-up (well-controlled symptoms, low-dose therapy, unchanged from last visit, no emergency department visits or hospitalizations in the past 6 months, and not bothered by asthma) and stepping-down treatment (similar patient on high-dose therapy). We expected most respondents not to step up treatment in the first case and most to step down treatment in the second. Two other vignettes were randomly selected.
Analysis
Medians and proportions were used as appropriate. A χ2 test for differences in proportions was used to examine the effect of acute care, bother, control, direction, and wheeze on the proportion of physicians who would step up treatment in those on low-dose therapy and step down treatment for those on high-dose therapy.
Multivariable logistic regression was used to assess independent effects of the 5 factors on stepping up and down treatment by including all 5 of the factors in both models (separate models for stepping up and stepping down treatment were constructed). P values of <.05 were considered statistically significant. Analyses were performed by using Stata 8.0 (Stata Corp, College Station, TX).
RESULTS
Respondent Characteristics
There were 335 respondents, representing 69% of potentially eligible respondents. The respondents resided in 44 US states and territories. Although data on nonrespondents were limited to their mailing address, there were no statistically significant differences in respondents and nonrespondents by region of the country. The majority of pediatricians rated their experience treating asthma as moderate (59%; Table 2). Most respondents were in private practice, located most commonly in suburban settings (46%) rather than urban (36%) or rural (13%) settings. Nearly all of the respondents (93%) reported currently treating asthma patients every week. Analyses were restricted to only those respondents who reported currently treating children with asthma (310 of 335).
TABLE 2.
Physician Demographic and Practice Characteristics
| Physician Characteristic | Pediatricians |
|---|---|
| (n = 310), % | |
| Primary employer | |
| Private practice | 67.9 |
| University medical school | 5.8 |
| Community hospital | 13.3 |
| Government | 2.3 |
| Managed care | 6.8 |
| Other | 3.9 |
| Experience treating asthma | |
| Extensive | 35.5 |
| Moderate | 61.8 |
| Limited | 2.6 |
| Weekly volume of asthma patients seen | |
| Do not see patients | 3 |
| None | 1 |
| 1–5 per wk | 20 |
| 6–10 per wk | 32 |
| 11–20 per wk | 25 |
| >20 per wk | 19 |
Tendency to Step Up From Low-Intensity Treatment
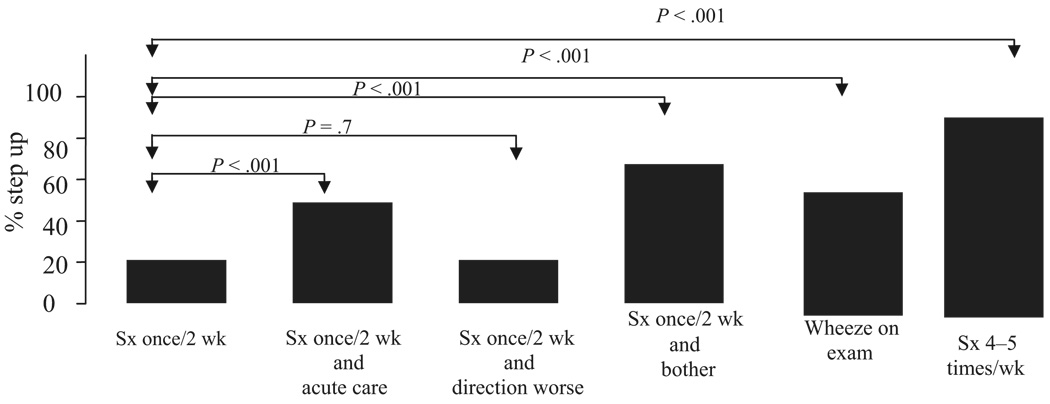
As expected for the baseline scenario for stepping up treatment, most pediatricians (82%) would not step up treatment for a patient on low-intensity therapy with well-controlled symptoms (1 time in the past 2 weeks [Fig 1]). Not surprisingly, pediatricians were significantly more likely to step up treatment for a patient on low-intensity therapy when persistent (4–5 times per week) rather than when well-controlled symptoms were present (100% vs 18%; P < .001) or if wheezing was present on physical examination (45% vs 18%; P < .001), even if there was a history of only well-controlled symptoms.
FIGURE 1.
The impact of acute care, bother, control, direction, and wheeze on the tendency of pediatricians to step up treatment under each studied vignette. In each case, the patient was one who was already receiving low-dose ICS. The first bar represents the proportion of pediatricians who would step up treatment for patients with mild intermittent symptoms (1 time in past 2 weeks). In this case, 18% of pediatricians would step up therapy. The other bars represent the proportion of pediatricians who would step up treatment of patients with only 1 key factor changed (acute care, direction, bother, wheeze, or control; persistent symptoms 4–5 times per week). Each studied factor significantly increased the propensity to step up treatment. For example, the second bar represents the case of symptoms 1 time in the past 2 weeks, as well as history of acute care (hospitalization 6 months ago). In this case, pediatricians were significantly more likely to step up treatment than if they had had no acute care visits (45% of pediatricians; P <.001). Sx indicates symptoms.
Among patients with well-controlled symptoms (1 time in the past 2 weeks) on low-intensity treatment, a substantially greater proportion of pediatricians would step up treatment if the patient had been hospitalized 6 months ago (45% vs 18%), if the parent was bothered by their child’s asthma (67% vs 18%), or if the patient had a positive history of hospitalization, worse symptoms, and parents bothered by the child’s asthma (97% vs 18%; P < .001 for all of the comparisons). In contrast, if the symptoms were worse than on the previous visit, few pediatricians recommended stepping up treatment (16% vs 18%; P < .6). Regardless of the factor that led to a step up in treatment, pediatricians most often chose to increase the ICS dose (48%), whereas 32% would add LTM and 31% would add LABA (sums to >100% because some would make >1 change).
In a multivariate model (Table 3), 4 of the 5 studied factors, acute care, bother, control, and wheeze (but not direction), remained independent significant predictors of the tendency to step up therapy. When considering only patients with well-controlled symptoms, bother was associated with the greatest odds of stepping up therapy.
TABLE 3.
Multivariate Predictors of Tendency to Step Up Therapy From Low-Intensity Treatment or to Step Down Therapy From High-Intensity Treatment (n = 310)
| Predictor | Step Up Therapy (Low-Intensity Treatment) |
Step Down Therapy (High- Intensity Treatment) |
||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Control (not well-controlled vs well-controlled symptoms) | NAa | NAa | NAb | NAb |
| Bother | 13.40 | 7.70–23.40 | 0.72 | 0.40–1.20 |
| Direction worse | 1.30 | 0.60–2.60 | 0.11 | 0.05–0.23 |
| Acute care | 5.50 | 3.00–9.80 | 0.37 | 0.22–0.62 |
| Wheeze | 6.80 | 4.00–11.70 | NAc | NAc |
OR indicates odds ratio; CI, confidence interval.
No OR is calculable, because 100% of respondents recommended stepping up therapy for patients without well-controlled symptoms and no respondents recommended other treatment options (eg, decrease therapy or make no change in therapy).
No vignette of a patient with poorly controlled asthma symptoms while on a high-intensity treatment regimen was presented.
No vignette of a patient with wheezing on physical exam while on a high-intensity treatment regimen was presented.
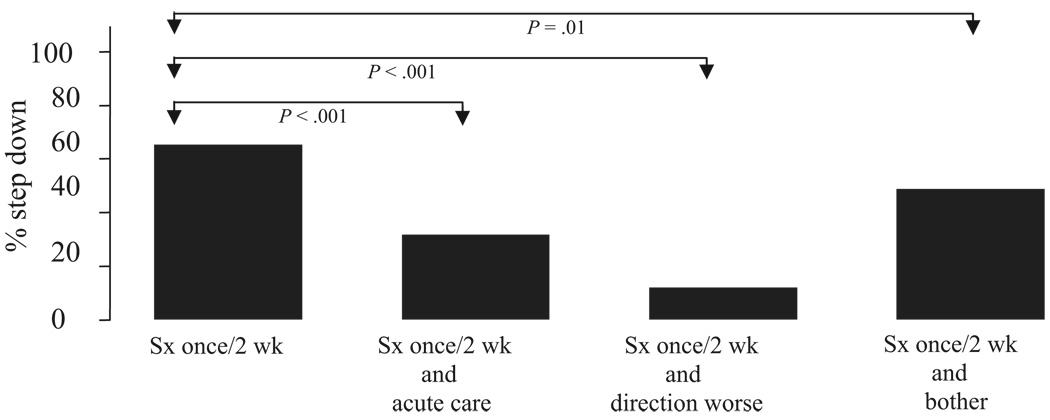
Tendency to Step Down From High-Intensity Treatment
For the patient with well-controlled symptoms (1 time in the past 2 weeks) on a stable regimen for the past 6 months of high-dose ICS, LABA, and LTM, 60% of pediatricians would step down treatment (Fig 2). Markedly fewer would step down treatment if a similar patient had been hospitalized in the past 6 months (28% vs 60%; P < .001), the parent was bothered by the child’s asthma (43% vs 60%; P = .01), or symptoms were worse than on the last visit (10% vs 60%; P < .001). No one recommended decreasing treatment in the presence of a patient with a history of all 3 of the factors present (hospitalization, parents bothered by the child’s asthma, and report of worse symptoms; 0% vs 60%; P < .0001). Pediatricians most often would decrease ICS (46%). Discontinuing the LABA was the next most common change (22%), followed by decreasing or discontinuing the LTM (10%) and stopping the ICS (6%).
FIGURE 2.
The impact of acute care, bother, control, and direction on the tendency of pediatricians to step down treatment under each studied vignette (no pediatricians recommended decreasing treatment for a patient with a history of acute care, worse symptoms, and parents who were bothered by the child’s asthma). In each case, the patient was one who was already receiving high-dose ICS, LABA, and LTM for the past 6 months. The first bar represents the proportion of pediatricians who would step down treatment of patients with mild intermittent symptoms (1 time in past 2 weeks). In this case, 60% of pediatricians would step down therapy. The other bars represent the proportion of pediatricians who would step down treatment with only 1 key factor changed (acute care, direction, and bother). Each studied factor significantly decreased the propensity to step down treatment. For example, the second bar represents the case of symptoms 1 time in the past 2 weeks, as well as history of acute care (hospitalization 6 months ago). In this case, pediatricians were significantly less likely to step down treatment than if they had had no acute care visits (28% of pediatricians; P <.001). Sx indicates symptoms.
A multivariate model showed that acute care and direction (worse symptoms) would each independently reduce the tendency to step down therapy, although bother would not (Table 3). In contrast to stepping up therapy, the strongest factor other than symptom frequency in influencing the decision to step down therapy was direction.
DISCUSSION
This study shows that treatment decisions of practicing pediatricians are influenced by multiple dimensions of asthma health, including acute health care use, bother, control, direction, and wheezing. The presence of each of these factors (except direction) independently influenced pediatricians to step up asthma therapy. Operationally, these factors may represent future risk for poor outcomes (acute care), less-than-optimal quality of life (bother), disease activity (control), trajectory of disease state (direction), and current clinical evidence of disease activity. Overall, our findings suggest that pediatricians are likely to increase asthma therapy based on multiple different indicators of worsening asthma.
Despite the equally important goal of reducing asthma therapy when indicated, pediatricians in our study seemed far less willing to step down therapy, even when these same dimensions of asthma health indicated controlled asthma. Multiple studies now suggest that many patients with well-controlled asthma can have their asthma therapy safely reduced,14–16 which is compatible with national asthma guideline recommendations to step down asthma therapy when appropriate. Stepping down treatment may be useful to minimize risks for adverse effects of medication and to better define disease severity and responsiveness to treatment.17 Pediatricians should be sensitive to minimizing exposures to therapies that are not needed, particularly given parental concerns about adverse effects from inhaled steroid therapies.18,19 Parents may address their concerns of overtreatment by pediatricians through reduced adherence with asthma therapy. Effective tools and strategies for pediatric asthma management should underscore the importance of titrating therapy down, according the child’s overall asthma status.
We anticipated that symptom frequency would have a strong effect on treatment assignment but were uncertain how other factors (acute care, bother, and direction) would affect prescribing recommendations, particularly the parent report of being bothered by the child’s asthma. The substantial impact of parental bother on treatment decisions of pediatricians suggests that clinicians endorse a family centered approach to asthma management. This consideration of patient preferences and quality of life by pediatricians is suggested in national asthma guidelines (creating a partnership for patient education) but not formally operationalized into the medication titration regimens of the guideline. The incorporation of bother by pediatricians in this study may also reflect a “global” screening approach to asthma assessment that has been commonly reported among clinicians20–22 despite the risks of inaccurate assessment with this strategy. Although report of “worse” asthma status alone did not prompt physicians to increase treatment, these physicians may have appreciated that the patient’s symptoms were still well controlled and therefore, appropriately did not warrant an increase in asthma therapy.
Asthma guidelines have stressed symptom control as a key factor in assigning asthma treatment, but our study shows that the decision to increase or decrease therapy is influenced by multiple dimensions of asthma status that act differently and independently on pediatrician decision-making. In the decision to increase or step up therapy, symptom frequency was most influential, followed by bother, presence of wheezing on physical examination, and then acute care, but not worsening symptoms (direction), which had no significant effect. In the decision for pediatricians to step down therapy, direction (ie, symptom lability or qualitatively worse symptoms) was most influential and then acute care, whereas bother had no significant effect. Historically, national asthma guidelines have recommended that pediatricians incorporate these factors into their treatment decisions but do not offer an operational schema to incorporate this multidimensional, differential decision-making approach to titrate treatment. However, the latest version of the national asthma guidelines has incorporated the concept of “risk” into the treatment titration scheme, which suggests that concepts in addition to symptom frequency may be operationalized in the treatment schema of future guidelines. We recently conducted a similar vignette-based survey study among adult pulmonologists and family practitioners10 and found that acute care, bother, control, and direction were also influential in determining a physician’s decision to assign treatment for their patients with asthma (wheeze on examination was not assessed in the other 2 physician groups). Studies are needed to learn whether such a multidimensional approach to asthma assessment would result in increased physician adherence with asthma guidelines and improved asthma outcomes (eg, improved symptom control).
This 2006 study suggests an increase in the willingness of pediatricians to prescribe ICSs for persistent asthma, likely resulting from the growing influence of various national and local care asthma guidelines on training and practice.1,23 In a 2001 study conducted by Cabana et al,24 53% of pediatricians reported that they would prescribe inhaled steroids for a patient with daily symptoms. In our survey, 100% of pediatricians recommended inhaled steroids for a patient with symptoms 4 to 5 days per week. This study suggests that pediatricians today may be more aware of indications for use of inhaled steroids in asthma and may be less concerned about possible adverse effects. However, reports in other studies of modest rates of inhaled steroid use among pediatricians25–28 must be reconciled with our findings. One possible explanation is that, in practice, physicians are less willing to prescribe inhaled steroids than is suggested by their responses to hypothetical scenarios of asthma control. Pediatric care typically involves assessing the child’s overall health concerns (eg, growth and development, vaccinations, etc), and routine asthma assessment may not provide the pediatrician with as much detail as the scenarios of this study. If so, this suggests that improved asthma screening and assessment tools that provide pediatricians with information on multiple dimensions of asthma status might increase the rate of appropriate inhaled steroid prescribing.
We acknowledge that there are potential limitations to our findings. First, we have used a vignette-based approach to study physician treatment recommendations rather than examining what is actually happening in their clinical practice. However, using a vignette-based study design is a valid method to estimate physician care practices.4–8 Furthermore, comparisons of actual clinical practices may be confounded by differences between physicians in patient case mix (eg, differences in asthma severity, sociodemographics, etc) and health care systems; reviews of charts and administrative data are susceptible to incomplete data.29–31 Vignettes are also a preferable method for standardizing patient factors and/or manipulating certain patient variables to isolate the potential effect of a given factor on physician practice.6 Our objective was to learn whether a particular set of factors beyond symptom frequency is important to pediatricians’ decision-making regarding treatment assignment for asthma. Our findings may not be generalizable to other types of physicians, although we have now conducted this study among 3 different types of physicians—pediatricians, pulmonologists, and family practitioners—and the findings have been consistent across all 3 of the groups. Our findings also may not be generalizable to other pediatricians, although our participants were randomly selected and represent diverse geographic and clinical practice settings. Additional studies are needed to determine whether our findings are replicable.
CONCLUSIONS
This study shows that pediatricians seem to use multiple dimensions of asthma status, in addition to symptom control, in their decisions to titrate asthma therapy. However, pediatricians seem to be more sensitive to changes in these dimensions of asthma status for increasing rather than decreasing asthma therapy. Overall, our findings suggest that symptom control alone may be sufficient for practicing pediatricians to assign treatment, but other dimensions of asthma status are important, too. Although a multidimensional approach is endorsed by national and international asthma guidelines, pediatricians may find appealing the development of a clinically pragmatic, easy-to-use tool that incorporates multiple dimensions of asthma status that are important to treatment assignment and titration of treatment.
What’s Known on This Subject
Although asthma is often inappropriately treated in children, most studies have focused on how physicians assess and incorporate symptom frequency into treatment of asthma. Little is known about what other clinical information (eg, history of hospitalization) pediatricians use to adjust asthma therapy.
What This Study Adds
We have shown that multiple dimensions of asthma health are important to assign treatment. Pediatricians may find appealing a clinical tool that incorporates multiple dimensions of asthma status that are important to treatment.
Abbreviations
- ICS
inhaled corticosteroid
- LABA
long-acting β-agonist
- LTM
leukotriene modifier
APPENDIX Sample Vignette
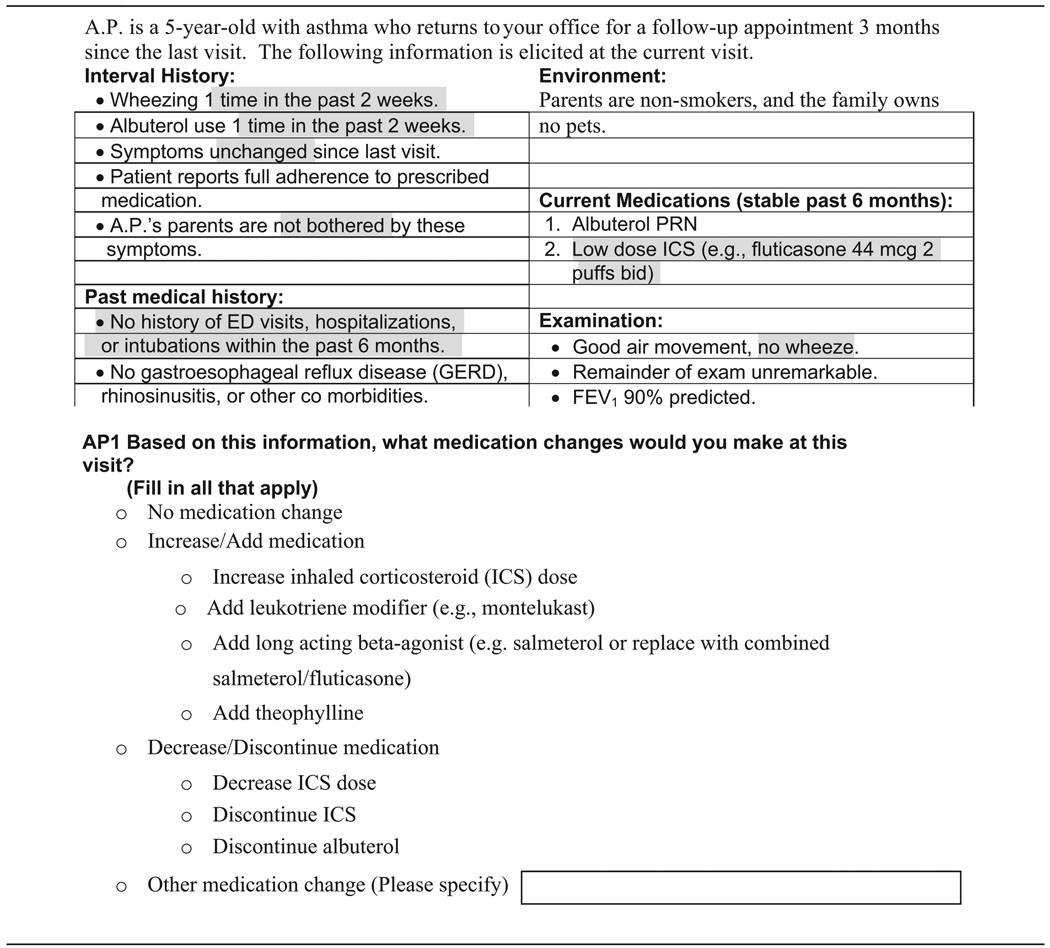 |
Sample vignette. This example of 1 of the 11 vignettes represents the “floor” for comparison of studied factors. The shaded areas highlight where there were variations by vignette (eg, wheezing 1 time in the past 2 weeks versus wheezing 4 –5 times per week).
Footnotes
The authors have indicated they have no financial relationships relevant to this article to disclose.
Reprints Information about ordering reprints can be found online: http://www.pediatrics.org/misc/reprints.shtml
REFERENCES
- 1.National Asthma Education and Prevention Program. Expert panel report: guidelines for the diagnosis and management of asthma—update on selected topics: 2002. J Allergy Clin Immunol. 2002;110(5 suppl):S142–S219. [PubMed] [Google Scholar]
- 2.Patino CM, Riekert KA, Quartey RI. Howard-Hopkins Center for Reducing Asthma Disparities. Development of the Asthma Control and Communication Instrument (ACCI) Am J Respir Crit Care Med. 2005;2:A254. [Google Scholar]
- 3.Asch DA, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50(10):1129–1136. doi: 10.1016/s0895-4356(97)00126-1. [DOI] [PubMed] [Google Scholar]
- 4.Walter SD, Cook DJ. Confidence in life-support decisions in the intensive care unit: a survey of healthcare workers. Canadian Critical Care Trials Group. Crit Care Med. 1998;26(1):44–49. doi: 10.1097/00003246-199801000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Dresselhaus TR, Peabody JW, Luck J, Bertenthal D. An evaluation of vignettes for predicting variation in the quality of preventive care. J Gen Intern Med. 2004;19(10):1013–1018. doi: 10.1007/s11606-004-0003-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Englund L, Tibblin G, Svardsudd K. Variations in sick-listing practice among male and female physicians of different specialities based on case vignettes. Scand J Prim Health Care. 2000;18(1):48–52. doi: 10.1080/02813430050202569. [DOI] [PubMed] [Google Scholar]
- 7.Peabody JW, Luck J, Glassman P, et al. Measuring the quality of physician practice by using clinical vignettes: a prospective validation study. Ann Intern Med. 2004;141(10):771–780. doi: 10.7326/0003-4819-141-10-200411160-00008. [DOI] [PubMed] [Google Scholar]
- 8.Shekelle PG, Kravitz RL, Beart J, Marger M, Wang M, Lee M. Are nonspecific practice guidelines potentially harmful? A randomized comparison of the effect of nonspecific versus specific guidelines on physician decision making. Health Serv Res. 2000;34(7):1429–1448. [PMC free article] [PubMed] [Google Scholar]
- 9.National Heart, Lung, and Blood Institute. Bethesda, MD: National Heart, Lung, and Blood Institute; Guidelines for the Diagnosis and Management of Asthma: Expert Panel Report No. 2. 1997 Report 97-4051.
- 10.Diette GB, Patino CM, Merriman B, et al. Patient factors that physicians use to assign asthma treatment. Ann Intern Med. 2007;167(13):1360–1366. doi: 10.1001/archinte.167.13.1360. [DOI] [PubMed] [Google Scholar]
- 11.Wu AW, Young Y, Skinner EA, et al. Quality of care and outcomes of adults with-asthma treated by specialists and generalists in managed care. Arch Intern Med. 2001;161(21):2554–2560. doi: 10.1001/archinte.161.21.2554. [DOI] [PubMed] [Google Scholar]
- 12.Cummings SM, Savitz LA, Konrad TR. Reported response rates to mailed physician questionnaires. Health Serv Res. 2001;35(6):1347–1355. [PMC free article] [PubMed] [Google Scholar]
- 13.Jepson C, Asch DA, Hershey JC, Ubel PA. In a mailed physician survey, questionnaire length had a threshold effect on response rate. J Clin Epidemiol. 2005;58(1):103–105. doi: 10.1016/j.jclinepi.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 14.Lemanske RF, Sorkness CA, Mauger EA, et al. Inhaled corticosteroid reduction and elimination in patients with persistent asthma receiving salmeterol: a randomized controlled trial. JAMA. 2001;285(20):2594–2603. doi: 10.1001/jama.285.20.2594. [DOI] [PubMed] [Google Scholar]
- 15.Peters SP, Anthonisen N, Castro M, et al. Randomized comparison of strategies for reducing treatment in mild persistent asthma. N Engl J Med. 2007;356(20):2027–2039. doi: 10.1056/NEJMoa070013. [DOI] [PubMed] [Google Scholar]
- 16.Gibson PG, Powell H, Ducharme F. Long-acting beta2-agonists as an inhaled corticosteroid-sparing agent for chronic asthma in adults and children. Cochrane Database Syst Rev. 2005;4 doi: 10.1002/14651858.CD005076.pub2. CD005076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bacharier LB. “Step-down” therapy for asthma: why, when, and how? J Allergy Clin Immunol. 2002;109(6):916–919. doi: 10.1067/mai.2002.124665. [DOI] [PubMed] [Google Scholar]
- 18.Chambers CV, Markson L, Diamond JJ, Lasch L, Berger M. Health beliefs and compliance with inhaled corticosteroids by asthmatic patients in primary care practices. Respir Med. 1999;93(2):88–94. doi: 10.1016/s0954-6111(99)90296-2. [DOI] [PubMed] [Google Scholar]
- 19.Conn KM, Halterman JS, Fisher SG, Yoos HL, Chin NP, Szilagyi PG. Parental beliefs about medications and medication adherence among urban children with asthma. Ambul Pediatr. 2005;5(5):306–310. doi: 10.1367/A05-004R1.1. [DOI] [PubMed] [Google Scholar]
- 20.Halterman JS, Yoos HL, Kaczorowski JM, et al. Providers underestimate symptom severity among urban children with asthma. Arch Pediatr Adol Med. 2002;156(2):141–146. doi: 10.1001/archpedi.156.2.141. [DOI] [PubMed] [Google Scholar]
- 21.Halterman JS, McConnochie KM, Conn KM, et al. A potential pitfall in provider assessments of the quality of asthma control. Ambul Pediatr. 2003;3(2):102–105. doi: 10.1367/1539-4409(2003)003<0102:appipa>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 22.Halterman JS, Yoos HL, Kitzman H, Anson E, Sidora-Arcoleo K, McMullen A. Symptom reporting in childhood asthma: a comparison of assessment methods. Arch Dis Child. 2006;91(9):766–770. doi: 10.1136/adc.2006.096123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Institutes of Health. Bethesda, MD: National Institutes of Health; Global Initiative for Asthma, Global Strategy for Asthma Management and Prevention. 2002 Report 02-3659.
- 24.Cabana MD, Rand CS, Becher OJ, Rubin HR. Reasons for pediatrician nonadherence to asthma guidelines. Arch Pediatr Adol Med. 2001;155(9):1057–1062. doi: 10.1001/archpedi.155.9.1057. [DOI] [PubMed] [Google Scholar]
- 25.Diette GB, Skinner EA, Markson LE, et al. Consistency of care with national guidelines for children with asthma in managed care. J Pediatr. 2001;138(1):59–64. doi: 10.1067/mpd.2001.109600. [DOI] [PubMed] [Google Scholar]
- 26.Finkelstein JA, Lozano P, Farber HJ, Miroshnik I, Lieu TA. Underuse of controller medications among Medicaid-insured children with asthma. Arch Pediatr Adol Med. 2002;156(6):562–567. doi: 10.1001/archpedi.156.6.562. [DOI] [PubMed] [Google Scholar]
- 27.Halterman JS, Aligne CA, Auinger P, McBride JT, Szilagyi PG. Inadequate therapy for asthma among children in the United States. Pediatrics. 2000;105(1 pt 3):272–276. [PubMed] [Google Scholar]
- 28.Ortega AN, Gergen PJ, Paltiel AD, Bauchner H, Belanger KD, Leaderer BP. Impact of site of care, race, and Hispanic ethnicity on medication use for childhood asthma. Pediatrics. 2002;109(1) doi: 10.1542/peds.109.1.e1. Available at: www.pediatrics.org/cgi/content/full/109/1/e1. [DOI] [PubMed] [Google Scholar]
- 29.Green J, Wintfeld N. how accurate are hospital discharge data for evaluating effectiveness of care. Med care. 1993;31(8):719–731. doi: 10.1097/00005650-199308000-00005. [DOI] [PubMed] [Google Scholar]
- 30.Lloyd SS, Rissing JP. Physician and coding errors in patient records. JAMA. 1985;254(10):1330–1336. [PubMed] [Google Scholar]
- 31.Rethans JJ, Martin E, Metsemakers J. To what extent do clinical notes by general-practitioners reflect actual medical performance: a study using simulated patients. Br J Gen Pract. 1994;44(381):153–156. [PMC free article] [PubMed] [Google Scholar]