Abstract
Purpose
To investigate the association of employment status with CHD and ischemic stroke among middle-aged women.
Methods
Proportional hazards regression was used to assess the association of employment status, incident CHD, and incident ischemic stroke among 7,058 women, aged 45-64 years at baseline (1987-89), from the Atherosclerosis Risk in Communities Study.
Results
After adjusting for age and race-field center, women employed outside the home had a decreased risk of CHD (hazard ratio (HR) =0.70, 95% confidence interval (95% CI) =0.56, 0.86) and ischemic stroke (HR=0.62, 95% CI=0.47, 0.84) compared to homemakers. Differences in cardiovascular disease risk factors partially accounted for the association of employment status and CHD (HR=0.79, 95% CI=0.63, 0.99) and stroke (HR=0.79, 95% CI=0.58, 1.08). Also, modest differences were noted when the results were stratified by education, with employed women having a lower risk of CHD (HR=0.65, 95% CI=0.45, 0.93) than homemakers among those with less than a high school education.
Conclusions
Women employed outside of the home had a lower risk of CHD and stroke compared to homemakers and for CHD, this association was stronger among women with less than a high school education. These findings suggest additional research into the varied occupational experiences of women, socioeconomic status, and health is warranted.
MeSH keywords: women, employment, coronary disease, stroke, socioeconomic status
Introduction
Women are an integral part of today's paid labor force and their participation rates continue to increase at a faster pace than those for men; in fact, women are projected to comprise just under half of the total labor force in the United States by 2015 1. As more women enter the work force, divergent theories have emerged about the potential health effects for women. The social causation hypothesis posits that employment outside of the home affects the health of women while the social selection hypothesis posits that healthy women are more likely to enter and remain in the work force than those with worse health profiles 2. Moreover, the multiple role theory suggests that women with more roles (e.g., family and employee roles) may have a better health profile than women with fewer roles 3, although the strength of this association may vary due to different levels of job demands and job control 4. Due to the fact that many women assume multiple roles as homemakers, primary caretakers for children and elderly parents, in addition to being employed outside of the home, the investigation of the health-employment relationship among women is complex.
Previous studies have reported inconsistent results for the association between employment status and cardiovascular health. For cardiovascular risk factors, employed women in the National Health Examination Survey had an increased risk of hypertension compared to homemakers 5. Also, employed, middle-aged women in the Allegheny County Study had lower high density lipoprotein (HDL) cholesterol 6, but no differences were reported for smoking, alcohol consumption, and body mass index. Other studies have reported a more favorable cardiovascular risk factor profile for women employed outside of the home. In the Rancho Bernardo Study, currently employed women had lower total cholesterol, lower fasting glucose, and lower systolic blood pressure 7. Also, in the National Health and Nutrition Examination Survey II and the Atherosclerosis Risk in Communities Study, employed women had a decreased risk of hypertension compared to homemakers 5,8. Similarly, inconsistent findings have been reported for mortality and coronary heart disease (CHD). In a cohort study in Alameda County, no association was reported between employment status and mortality 9. Conversely, employed women had a lower risk of mortality in a study of HMO participants in California and similar findings were reported in two other studies of employment status and mortality among women 10,11. In the Tecumseh Study, self-reported heart attacks were greater among homemakers, although no difference in diagnosed CHD was noted between employed women and homemakers 12. Also, homemakers had an increased risk of CHD in the National Health and Nutrition Survey 13, while no difference in CHD incidence between employed women and homemakers was reported in the Framingham Study 14.
Methodological differences make the comparison of results across studies difficult and may contribute to some of the inconsistent findings that have been reported for cardiovascular risk factors, mortality, and clinical CHD. Given the historical differences in occupational opportunities and financial remuneration available to women, the aim of this study was to investigate the association between current employment status and incident CHD, including fatal CHD, and to evaluate whether this association differed by age, race, or socioeconomic status over an average 14 years of follow-up among African-American and white women from four U.S. communities. Also, CHD and stroke share many of the same risk factors, but previous studies have not investigated the association between employment status and ischemic stroke. Thus, another aim of this study was to evaluate the association between current employment status and risk of incident ischemic stroke in this bi-racial cohort of middle-aged women in the Atherosclerosis Risk in Communities (ARIC) Study.
Methods
Study design and population
The ARIC Study is a prospective cohort study designed to investigate the etiology and natural history of atherosclerosis among 15,792 men and women, aged 45-64 years at baseline, from four U.S. communities: Forsyth County, North Carolina; Jackson, Mississippi (African-American participants only); northwest suburbs of Minneapolis, Minnesota; and Washington County, Maryland. The baseline clinical examination occurred between 1987-1989 with three additional clinical examinations occurring between 1990-1992, 1993-1995, and 1996-1998, respectively. The participants received annual follow-up telephone calls in between the clinical examinations to assess their vital status and hospitalizations, if any, for subsequent medical record review. Annual follow-up telephone calls continued after the last clinical examination and are currently ongoing to assess vital status and hospitalizations for medical record review. The ARIC Study received Institutional Review Board approval and written informed consent was obtained from all participants. Details of the design of the study and participation rates have been published 15,16.
Assessment of Employment Status
Current employment status was self-reported at the baseline examination (1987-89). Participants reported whether they were homemaking (not employed outside the home), employed at a job for pay (full-time or part-time), unemployed, or retired. Only participants who reported being currently employed or homemaking at the baseline examination were included in the present study. Because of limited information for unemployed and retired women, these women were excluded.
Assessment of Incident CHD and Ischemic Stroke Events
Incident CHD (myocardial infarction (MI) or fatal CHD event) and incident ischemic stroke events occurring between the baseline examination and December 31, 2004 among participants with no history of prevalent CHD (electrocardiogram evidence of MI or self-reported physician diagnosis) or prevalent stroke (self-reported physician diagnosis) were ascertained for this study. The standardized methods and quality control procedures used for the ascertainment of CHD and ischemic stroke events have been published 16,17 and a detailed protocol is available 18. Briefly, participants were evaluated at the triennial clinic examinations and they were contacted annually to assess any hospitalizations and changes in vital status. If a hospitalization was indicated, the participant's medical records were reviewed and abstracted for a possible CHD or stroke event. For CHD, medical records containing discharge diagnostic codes suggestive of CHD (International Classification of Disease, 9th Revision, Clinical Modification codes 402, 410-414, 427, 428, 518.4) or related screening conditions (e.g., diabetes, cardiac surgery) were obtained and abstracted for validation of a CHD event. For ischemic stroke, if any of the following occurred: 1) medical records contained discharge diagnostic codes suggestive of cerebrovascular events (International Classification of Disease, 9th Revision, Clinical Modification codes 430-438); 2) cerebrovascular keywords were present in discharge summary or nurse notes; 3) diagnostic CT scan or MRI with cerebrovascular findings; or 4) admission to neurological intensive care unit, the medical record of the participant was sent to a central location, and abstracted by a trained nurse for validation of a stroke event. If a participant was reported as deceased by next of kin or another designated contact person, then the date and location of death, and any hospitalizations prior to death were ascertained. When a participant was not located during annual follow-up, hospital records and the National Death Index were searched to determine vital status. A computer algorithm was used to discern the occurrence of a MI (based on diagnostic ECG patterns, cardiac enzyme levels, and chest pain), fatal CHD event (based on hospital notes, medical history, underlying cause of death, chest pain, and no evidence of other probable cause of death), or ischemic stroke event and these events were independently reviewed by physician reviewers. All MI, fatal CHD, and ischemic stroke events were validated by the ARIC Morbidity and Mortality Classification Criteria.
Assessment of Covariates
Demographic (age, race) and socioeconomic status (education, annual family income) variables were self-reported at baseline. Combined variables for race and ARIC field center were created for use in models because of the racial distribution of participants at the field centers. Trained study personnel and research technicians took all physical measurements and administered all questionnaires following a standardized protocol that included quality control measures. All covariates for this study were assessed at the baseline examination. Body mass index (kg/m2) was determined using height and weight measurements taken without shoes. Diabetes was defined as a fasting blood glucose ≥126mg/dl, non-fasting blood glucose ≥200mg/dl, use of hypoglycemic medication, or self-reported physician diagnosis. For systolic blood pressure (SBP), a random-zero mercury sphygmomanometer was used to measure blood pressure three times, five minutes apart, with the average of the second and third measurements used as the final assessment of SBP. The use of antihypertensive medications was determined based on medical information that was abstracted and coded from the medication bottles that the participants brought to clinic examinations or self-reported. HDL cholesterol was measured by the Warnick method 19 and LDL cholesterol was calculated based on the Friedewald formula 20 at a central lipid laboratory. Smoking status (current, former, never), general health perception (excellent, good, fair, or poor), health insurance, and frequency of routine clinical examinations (yearly, once every five years, less than once every five years, and none) were self-reported. Marital status was self-reported at the second clinic examination (1990-1992), so participants who were lost to follow-up or died prior to that visit had missing data for that variable.
Sample Size
At baseline, the ARIC Study included 8685 women participants. This study excluded women who were not white or African-American and African-American participants at the Maryland and Minnesota field centers (n=22) due to the small number and to explore effect modification by race. Women who were retired (n=945), unemployed (n=237), missing employment status (N=18), had prevalent CHD (n=314), or prevalent stroke (n=91) were also excluded resulting in a sample size of 7058. During an average follow-up period of 14 years, 418 CHD events and 219 ischemic stroke events occurred.
Statistical analysis
Age-adjusted proportions and means for traditional cardiovascular disease (CVD) risk factors were obtained from logistic regression and general linear regression 21, while age-adjusted incidence rates for CHD and ischemic stroke were obtained from Poisson regression 22. Cox proportional hazards regression was used to assess the association of employment status with CHD and stroke using a complete case analysis. The proportional hazards assumption was evaluated using log-log plots and time dependent covariates included in the model and no violations were noted. The regression models were adjusted for age, race-field center, socioeconomic status, CVD risk factors, and health care variables. Effect modification by age, race, education, income, and marital status was investigated based on reports from previous studies 4,5,8,23,24 but no effect modifiers were significant for CHD or ischemic stroke using an a priori significance of p<0.15. Due to concerns about residual confounding, additional analyses were stratified by education to examine whether the association between employment status and CHD events differed by socioeconomic status. All statistical analyses were performed using SAS version 9.1 (Cary, NC).
Results
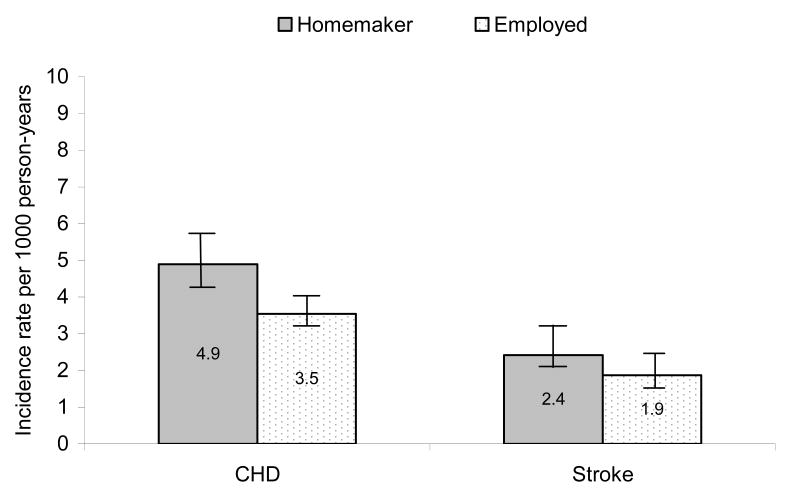
The characteristics of the study participants by employment status at baseline are presented in Table 1. Overall, the majority of the women were employed outside of the home (75%). Differences between homemakers and women employed outside the home were noted for demographic, socioeconomic, and cardiovascular risk factors. The mean age was slightly lower for women employed outside of the home (52 years) compared to homemakers (55 years). African-American women comprised a smaller proportion of the homemaking group (21%) than those employed outside of the home (33%). Employed women were more likely to have advanced education levels, higher incomes, and more favorable CVD risk profiles than homemakers. Also, the incidence rate per 1000 person-years for both CHD and ischemic stroke was lower among women employed outside the home than among homemakers (Figure 1).
Table 1.
Characteristics of women participants at the baseline examination by employment status, the Atherosclerosis Risk in Communities Study (1987-1989)
| Variable | Homemakers N=1790 |
Employed N=5268 |
|---|---|---|
| Mean age, years (SD) | 55.0 (5.6) | 52.4 (5.2)*** |
| Race (n, %) | ||
| African-American | 372 (20.8) | 1723 (32.7)*** |
| White | 1418 (79.2) | 3545 (67.3) |
| Field center (n, %) | ||
| Forsyth County, North Carolina | 451 (25.2) | 1239 (23.5)*** |
| Jackson, Mississippi | 341 (19.1) | 1540 (29.2) |
| Minneapolis, Minnesota | 386 (21.6) | 1427 (27.1) |
| Washington County, Maryland | 612 (34.2) | 1062 (20.2) |
| Education (n, %) | ||
| Less than high school | 582 (32.5) | 981 (18.6)*** |
| Completed high school | 828 (46.3) | 2305 (43.8) |
| Some college or more | 379 (21.2) | 1978 (37.5) |
| Missing | 1 (0.0) | 4 (0.0) |
| Annual family income, dollars (n, %) | ||
| < 16,000 | 502 (28.0) | 1180 (22.4)*** |
| 16,000-24,999 | 260 (14.5) | 769 (14.6) |
| 25,000-34,999 | 292 (16.3) | 872 (16.6) |
| 35,000-49,999 | 257 (14.4) | 975 (18.5) |
| ≥ 50,000 | 421 (23.5) | 1358 (25.8) |
| Missing | 58 (3.2) | 114 (2.2) |
| Marital status (n, %)a | ||
| Unmarried | 248 (13.9) | 1467 (27.8)*** |
| Married | 1368 (76.4) | 3392 (64.4) |
| Missing | 174 (9.7) | 409 (7.8) |
| General health perception (n, %) | ||
| Excellent | 565 (31.6) | 2128 (40.4)*** |
| Good | 844 (47.2) | 2374 (45.1) |
| Fair | 296 (16.5) | 547 (10.4) |
| Poor | 70 (3.9) | 104 (2.0) |
| Missing | 15 (0.8) | 115 (2.1) |
| Frequency of routine clinical examination | ||
| Yearly | 894 (49.9) | 2731 (51.8)*** |
| Less than every 5 years | 55 (3.1) | 234 (4.4) |
| More than every 5 years | 356 (19.9) | 1095 (20.8) |
| Never | 482 (26.9) | 1205 (22.9) |
| Missing | 3 (0.2) | 3 (0.0) |
| Health Insurance | ||
| Yes | 1542 (86.1) | 4796 (91.0)*** |
| No | 245 (13.7) | 467 (8.9) |
| Missing | 3 (0.2) | 5 (0.0) |
| Mean BMI (kg/m2)b | 28.0 | 27.7 |
| Mean systolic blood pressure (mmHg)b | 120.7 | 119.4* |
| Anti-hypertensive medication use (%)b | 27.2 | 23.6** |
| Mean LDL cholesterol (mg/dL)b | 136.3 | 134.2 |
| Mean HDL cholesterol (mg/dL)b | 56.7 | 58.6*** |
| Diabetic (%)b | 13.6 | 9.5*** |
| Current smoker (%)b | 23.9 | 24.0 |
Marital status was not assessed until the second examination (1990-1992).
Adjusted for age.
p<0.05
p<0.01
p<0.001
Figure 1.
Age-adjusted incidence rates (per 1000 person-years) for CHD and ischemic stroke by employment status among women participants in the Atherosclerosis Risk in Communities Study, 1987-1989
The hazard ratios and 95% confidence intervals for the association of employment status with incident CHD and incident ischemic stroke are presented in Table 2. In analyses adjusted for age and race-field center, employed women had a decreased risk of incident CHD (HR=0.70, 95% CI=0.56, 0.86). After adjustment for education and family income, this association was only modestly attenuated; additional adjustment for CVD risk factors and health care further attenuated this association (HR=0.77, 95% CI=0.61, 0.97). Women employed outside of the home also had a decreased risk of ischemic stroke than homemakers (HR=0.62, 95% CI=0.47, 0.84), but this association was attenuated and no longer significant after adjustment for socioeconomic status, CVD risk factors, and health care (HR=0.84, 95% CI=0.61, 1.16).
Table 2.
Hazard ratios (HR) and 95% confidence intervals (CI) for the association of employment status with CHD and ischemic stroke among women in the Atherosclerosis Risk in Communities Study
| Model | CHD | Ischemic Stroke | ||
|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | |
| Model 1 | ||||
| Employed | 0.70 | 0.56, 0.86 | 0.62 | 0.47, 0.84 |
| Homemakers | 1.00 | 1.00 | ||
| Model 2 | ||||
| Employed | 0.74 | 0.59, 0.91 | 0.66 | 0.49, 0.90 |
| Homemakers | 1.00 | 1.00 | ||
| Model 3 | ||||
| Employed | 0.79 | 0.63, 0.99 | 0.79 | 0.58, 1.08 |
| Homemakers | 1.00 | 1.00 | ||
| Model 4 | ||||
| Employed | 0.77 | 0.61, 0.97 | 0.84 | 0.61, 1.16 |
| Homemakers | 1.00 | 1.00 | ||
Model 1: adjusted for age and race-field center.
Model 2: adjusted for model 1 variables plus education and family income.
Model 3: adjusted for model 2 variables plus body mass index, systolic blood pressure, anti-hypertensive medication use, HDL cholesterol, LDL cholesterol, diabetes, and smoking status.
Model 4: adjusted for model 3 variables plus general health perception, frequency of clinical examination, and health insurance.
The association of employment status with CHD and ischemic stroke was also evaluated stratified by education because of possible residual confounding by socioeconomic position (Table 3). For CHD, a modest gradient was noted across the continuum of education. The association was strongest among those with less than a high school education, with women employed outside of the home having a decreased risk of CHD (HR=0.61, 95% CI=0.42, 0.87) after adjustment for covariates. The association was somewhat weaker for women who completed high school (HR=0.84, 95% CI=0.58, 1.21), and weakest among those with some college or more where there was no difference between women employed outside the home and homemakers (HR=1.12, 95% CI=0.63, 2.01). No consistent patterns were noted for ischemic stroke.
Table 3.
Hazard ratios (HR) and 95% confidence intervals (CI) for the association of employment status with CHD and ischemic stroke, stratified by education level, among women in the Atherosclerosis Risk in Communities Study
| CHD | Ischemic Stroke | |||||
|---|---|---|---|---|---|---|
| Less Than High School | Completed High School | Some College or More | Less Than High School | Completed High School | Some College or More | |
| Model* | HR (95% CI) | |||||
| Employed | 0.61 (0.42, 0.87) | 0.84 (0.58, 1.21) | 1.12 (0.63, 2.01) | 0.98 (0.61, 1.57) | 0.77 (0.46, 1.31) | 0.72 (0.32, 1.59) |
| Homemakers | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
Adjusted for age, race-field center, family income, body mass index, systolic blood pressure, anti-hypertensive medication use, HDL cholesterol, LDL cholesterol, diabetes, smoking status, general health perception, frequency of clinical examination, and health insurance.
Discussion
In this study of middle-aged women in the United States, women employed outside of the home had a decreased risk of incident CHD and ischemic stroke compared to homemakers, and for CHD, this association was stronger among women with less than a high school education. The potential pathways for the manifestation of adverse clinical events prominently include traditional CVD risk factors, so the persistence of an association after adjustment for these factors suggests that other factors may play a role in the association between employment status and CHD.
An earlier study reported no difference in incidence of CHD by employment status among women in the United States 14. Several factors may account for the contrasting results observed in that study including different participant composition (all white), the inclusion of angina in the definition of CHD, and an earlier time period (1960s) when the transition of married women into the work force was in the beginning stages 14. Our finding of a decreased risk of CHD events (fatal and non-fatal) among women employed outside of the home is comparable to the previous finding reported by Reviere et al.13 of a higher risk of CHD among homemakers. The association observed in our study did not vary for fatal or non-fatal events but it persisted after adjustment for socioeconomic and cardiovascular factors.
In this study, employed women had a decreased risk of ischemic stroke that had not been previously reported. Recently, two Swedish studies investigated employment characteristics and ischemic stroke among employed women and reported conflicting findings, with one suggesting no association between job stress and ischemic stroke 25 and the other suggesting low social support at work was associated with an increased risk of stroke 26. Stroke and CHD share many of the same risk factors, but the association between employment status and ischemic stroke was weaker in this study and explained by traditional risk factors.
Women may self-select into homemaking or employment outside of the home based on their socioeconomic status and financial and material resources available. In this study, homemakers had a lower education level than employed women and a graded association was noted by education level, with employed women having a lower risk of incident CHD than homemakers among those with less than a high school education while no association was noted among women with some college or more. These findings are similar to previous studies that have also identified education level as an effect modifier of the association between employment status and health 23,24. The stronger association among those with less than a high school education may be due to several factors such as less opportunity and fewer resources, given that other studies of employment and social class have reported that persons with an advanced education who experience unemployment are more benignly affected than persons with less formal education because of the protective nature of a higher paying labor market 27 or a household with an overall higher socioeconomic position 28; however, comprehensive measures of wealth and social position were not available to further evaluate socioeconomic position in this study.
There has been some debate about the influence of the healthy worker effect on women's participation in the work force, based on the premise that women who are healthier are more likely to enter and remain in the work force. In this study, homemakers had a worse CVD risk factor profile at baseline than women employed outside the home. We did not assess employment status until middle-age so it is possible that the women in our study could have self-selected into homemaking or employment outside of the home due to their health status prior to participating in this study. While we attempted to lessen the influence of the healthy worker effect by performing a prospective analysis of incident events and adjusting for CVD risk factors and other health care variables, some women may have self-identified as homemakers several years prior to this study due to poor or declining health.
It has been hypothesized that the association between employment and health may differ by occupation type because of varying levels of job strain. Job strain is usually self-reported and subject to self-perception, so there have been conflicting findings with most studies reporting a positive association between job strain and CHD risk 29,30, while other studies have reported no association between a high level of job strain and incident CHD 31 or mortality 30 among women. In supplemental analyses, this study found a stronger association of employment outside of the home with incident CHD among manual workers (e.g., service) than non-manual workers (i.e. managerial and professional), but no similar association was noted for ischemic stroke. Data on self-employment or business ownership was not available at baseline so the occupation titles may not fully capture the role of the participants and this study had limited power to stratify by the specific occupation groups. Other factors, such as psychological characteristics, may also play a role in the relation between employment status and CHD. Homemaking characteristics, such as low control in the home environment, have been associated with depression 32,33 and depression has been associated with an increased risk of morbidity and mortality 34,35. Our study did not have data on depression at baseline, so this could have partially contributed to the association observed with CHD events.
The state of being married may have positive or negative effects on women's health 36. Married women may benefit from the additional income and social support within the home that may not be available to unmarried women. In our study, marital status was not available until the second clinic examination, so those who were lost to follow-up or died prior to the second visit were missing marital status. Therefore, marital status was not included in the main models presented because women whose marital status changed during the 3 years between examinations would be misclassified. In supplemental analyses that included marital status from the second examination, the effect estimates did not appreciably change for CHD or ischemic stroke.
This study has several limitations. Employment status was assessed at baseline, when the women were 45-64 years of age. We did not collect data on work history over the life course at the baseline examination, so our data may not reflect the primary occupation held most of the women's adult lives. Women may cycle in and out of the work force during their adult years due to maternity leave, child-rearing, family obligations, or involuntary unemployment, but this study did not have data available to assess the influence of intermittent work force participation on incident CHD or ischemic stroke; however, a previous study did report that intermittent work force participation was not associated with higher rates of morbidity 37. Also, the ARIC Study did not include an assessment of specific employment characteristics such as full-time versus part-time, contract work (e.g., temporary, fixed contract, on call), or duration spent in workforce, so we were unable to investigate whether the associations observed in this study may have differed by these factors. Women employed full-time have better health than women employed part-time 2, so a more specific definition of employment status may be used to examine differences among employed women. Retired and unemployed women were excluded from this study because of a lack of occupation information; however, these women had a poorer CVD risk factor profile than employed women and homemakers which suggests that additional research into the association between employment status and CHD is needed. Another limitation is that our study only included middle-aged women. Different results may be expected among older women, who are likely to have had more experience in the workforce than younger women. Despite these limitations, this study has several strengths. Participants were from a large, community-based cohort, which included both white and African-American women in the United States. Trained personnel and a standardized protocol were used to measure variables and outcomes. Also, over 14 years of follow-up were available to evaluate incident CHD and ischemic stroke events.
In summary, employment outside of the home was associated with a decreased risk of ischemic stroke and CHD in this study and this association was slightly more pronounced for CHD events and among women with less than a high school education. Given the increasing magnitude of women's contribution to the labor force, these findings suggest additional research into the varied occupational experiences of women, morbidity, and mortality is warranted.
Acknowledgments
The Atherosclerosis Risk in Communities Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts N01-HC-55015, N01-HC-55016, N01-HC-55018, N01-HC-55019, N01-HC-55020, N01-HC-55021, and N01-HC-55022. The authors thank the staff and participants of the ARIC study for their important contributions.
List of Abbreviations and Acronyms
- ARIC
Atherosclerosis Risk in Communities Study
- CHD
Coronary Heart Disease
- CI
Confidence Interval
- CVD
Cardiovascular Disease
- HDL
High-density lipoprotein
- HR
Hazard Ratio
- LDL
Low-density lipoprotein
- MI
Myocardial infarction
- SBP
Systolic blood pressure
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mosisa A, Hipple S. Trends in labor force participation in the United States. Mon Labor Rev. 2006;129(10):35–57. [Google Scholar]
- 2.Ross CE, Mirowsky J. Does employment affect health? J Health Soc Behav. 1995;36(3):230–243. [PubMed] [Google Scholar]
- 3.Froberg D, Gjerdingen D, Preston M. Multiple roles and women's mental and physical health: what have we learned? Women Health. 1986;11(2):79–96. doi: 10.1300/J013v11n02_06. [DOI] [PubMed] [Google Scholar]
- 4.Amick BC, 3rd, McDonough P, Chang H, Rogers WH, Pieper CF, Duncan G. Relationship between all-cause mortality and cumulative working life course psychosocial and physical exposures in the United States labor market from 1968 to 1992. Psychosom Med. 2002;64(3):370–81. doi: 10.1097/00006842-200205000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Rose KM, Newman B, Bennett T, Tyroler HA. Employment status and high blood pressure in women: variations by time and by sociodemographic characteristics. Ann Epidemiol. 1997;7(2):107–14. doi: 10.1016/s1047-2797(96)00127-5. [DOI] [PubMed] [Google Scholar]
- 6.Ickovics JR, Morrill AC, Meisler AW, Rodin J, Bromberger JT, Matthews KA. Employment and coronary risk in women at midlife: a longitudinal analysis. Am J Epidemiol. 1996;143(2):144–50. doi: 10.1093/oxfordjournals.aje.a008723. [DOI] [PubMed] [Google Scholar]
- 7.Kritz-Silverstein D, Wingard DL, Barrett-Connor E. Employment status and heart disease risk factors in middle-aged women: the Rancho Bernardo Study. Am J Public Health. 1992;82(2):215–9. doi: 10.2105/ajph.82.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rose KM, Newman B, Tyroler HA, Szklo M, Arnett D, Srivastava N. Women, employment status, and hypertension: cross-sectional and prospective findings from the Atherosclerosis Risk in Communities (ARIC) Study. Ann Epidemiol. 1999;9(6):374–82. doi: 10.1016/s1047-2797(99)00015-0. [DOI] [PubMed] [Google Scholar]
- 9.Kotler P, Wingard DL. The effect of occupational, marital and parental roles on mortality: the Alameda County Study. Am J Public Health. 1989;79(5):607–12. doi: 10.2105/ajph.79.5.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rose KM, Carson AP, Catellier D, Diez Roux AV, Muntaner C, Tyroler HA, et al. Women's employment status and mortality: The atherosclerosis risk in communities study. J Women's Health (Larchmt) 2004;13(10):1108–1118. doi: 10.1089/jwh.2004.13.1108. [DOI] [PubMed] [Google Scholar]
- 11.Sorlie PD, Backlund E, Keller JB. US mortality by economic, demographic, and social characteristics: the National Longitudinal Mortality Study. Am J Public Health. 1995;85(7):949–56. doi: 10.2105/ajph.85.7.949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ebi-Kryston KL, Higgins MW, Keller JB. Health and other characteristics of employed women and homemakers in Tecumseh, 1959-1978: II. Prevalence of respiratory and cardiovascular symptoms and illnesses, mortality rates and physical and physiological measurements. Women and Health. 1990;16(2):23–39. doi: 10.1300/J013v16n02_03. [DOI] [PubMed] [Google Scholar]
- 13.Reviere R, Eberstein IW. Work, marital status, and heart disease. Health Care Women Int. 1992;13(4):393–9. doi: 10.1080/07399339209516016. [DOI] [PubMed] [Google Scholar]
- 14.Haynes SG, Feinleib M. Women, work and coronary heart disease: prospective findings from the Framingham heart study. Am J Public Health. 1980;70(2):133–41. doi: 10.2105/ajph.70.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jackson R, Chambless LE, Yang K, Byrne T, Watson R, Folsom A, et al. Differences between respondents and nonrespondents in a multicenter community-based study vary by gender ethnicity. The Atherosclerosis Risk in Communities (ARIC) Study Investigators. J Clin Epidemiol. 1996;49(12):1441–46. doi: 10.1016/0895-4356(95)00047-x. [DOI] [PubMed] [Google Scholar]
- 16.The ARIC Investigators. The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. Am J Epidemiol. 1989;129(4):687–702. [PubMed] [Google Scholar]
- 17.White AD, Folsom AR, Chambless LE, Sharret AR, Yang K, Conwill D, et al. Community surveillance of coronary heart disease in the Atherosclerosis Risk in Communities (ARIC) Study: methods and initial two years' experience. J Clin Epidemiol. 1996;49(2):223–33. doi: 10.1016/0895-4356(95)00041-0. [DOI] [PubMed] [Google Scholar]
- 18.National Heart Lung and Blood Institute (NHLBI) Atherosclerosis Risk in Communities (ARIC) Study Protocol. Operations Manual 2: Cohort Component Procedures. Version 2.0. Chapel Hill, NC: ARIC Coordinating Center, School of Public Health, The University of North Carolina at Chapel Hill; 1987. [Google Scholar]
- 19.Warnick GR, Mayfield C, Benderson J, Chen JS, Albers JJ. HDL cholesterol quantitation by phosphotungstate-Mg2+ and by dextran sulfate-Mn2+-polyethylene glycol precipitation, both with enzymic cholesterol assay compared with the lipid research method. Am J Clin Pathol. 1982;78(5):718–23. doi: 10.1093/ajcp/78.5.718. [DOI] [PubMed] [Google Scholar]
- 20.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499–502. [PubMed] [Google Scholar]
- 21.Zhao DY. Logistic regression adjustment of proportions and its macro procedure. SAS Users Group International Conference (SUGI) 22; San Diego, CA. 1998. paper 227. [Google Scholar]
- 22.Zhao DY. Poisson regression adjustment of event rates and its macro procedure adj_pois. SAS Users Group International Conference (SUGI) 24; Miami, FL. 1999. paper 256. [Google Scholar]
- 23.Arber S. Class, paid employment and family roles: making sense of structural disadvantage, gender and health status. Soc Sci Med. 1991;32(4):425–36. doi: 10.1016/0277-9536(91)90344-c. [DOI] [PubMed] [Google Scholar]
- 24.Artazcoz L, Borrell C, Benach J, Cortes I, Rohlfs I. Women, family demands and health: the importance of employment status and socio-economic position. Soc Sci Med. 2004;59(2):263–74. doi: 10.1016/j.socscimed.2003.10.029. [DOI] [PubMed] [Google Scholar]
- 25.Kuper H, Adami HO, Theorell T, Weiderpass E. The socioeconomic gradient in the incidence of stroke: a prospective study in middle-aged women in Sweden. Stroke. 2007;38(1):27–33. doi: 10.1161/01.STR.0000251805.47370.91. [DOI] [PubMed] [Google Scholar]
- 26.Andre-Petersson L, Engstrom G, Hedblad B, Janzon L, Rosvall M. Social support at work and the risk of myocardial infarction and stroke in women and men. Soc Sci Med. 2007;64(4):830–41. doi: 10.1016/j.socscimed.2006.10.020. [DOI] [PubMed] [Google Scholar]
- 27.Wright EO. Class counts: comparative studies in class analysis. New York: Cambridge University Press; 1997. [Google Scholar]
- 28.Krieger N. Women and social class: a methodological study comparing individual, household, and census measures as predictors of black/white differences in reproductive history. J Epidemiol Community Health. 1991;45(1):35–42. doi: 10.1136/jech.45.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Belkic KL, Landsbergis PA, Schnall PL, Baker D. Is job strain a major source of cardiovascular disease risk? Scand J Work Environ Health. 2004;30(2):85–128. doi: 10.5271/sjweh.769. [DOI] [PubMed] [Google Scholar]
- 30.Eaker ED, Sullivan LM, Kelly-Hayes M, D'Agostino RB, Sr, Benjamin EJ. Does job strain increase the risk for coronary heart disease or death in men and women? The Framingham Offspring Study. Am J Epidemiol. 2004;159(10):950–8. doi: 10.1093/aje/kwh127. [DOI] [PubMed] [Google Scholar]
- 31.Lee S, Colditz G, Berkman L, Kawachi I. A prospective study of job strain and coronary heart disease in US women. Int J Epidemiol. 2002;31(6):1147–53. doi: 10.1093/ije/31.6.1147. discussion 1154. [DOI] [PubMed] [Google Scholar]
- 32.Bromberger JT, Matthews KA. Employment status and depressive symptoms in middle-aged women: a longitudinal investigation. Am J Public Health. 1994;84(2):202–6. doi: 10.2105/ajph.84.2.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Griffin JM, Fuhrer R, Stansfeld SA, Marmot M. The importance of low control at work and home on depression and anxiety: do these effects vary by gender and social class? Soc Sci Med. 2002;54(5):783–98. doi: 10.1016/s0277-9536(01)00109-5. [DOI] [PubMed] [Google Scholar]
- 34.Ariyo AA, Haan M, Tangen CM, Rutledge JC, Cushman M, Dobs A, et al. Depressive symptoms and risks of coronary heart disease and mortality in elderly Americans. Cardiovascular Health Study Collaborative Research Group. Circulation. 2000;102(15):1773–9. doi: 10.1161/01.cir.102.15.1773. [DOI] [PubMed] [Google Scholar]
- 35.Everson SA, Roberts RE, Goldberg DE, Kaplan GA. Depressive symptoms and increased risk of stroke mortality over a 29-year period. Arch Intern Med. 1998;158(10):1133–8. doi: 10.1001/archinte.158.10.1133. [DOI] [PubMed] [Google Scholar]
- 36.Kiecolt-Glaser JK, Newton TL. Marriage and health: his and hers. Psychol Bull. 2001;127(4):472–503. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- 37.Hibbard JH, Pope CR. Health effects of discontinuities in female employment and marital status. Soc Sci Med. 1993;36(8):1099–104. doi: 10.1016/0277-9536(93)90128-q. [DOI] [PubMed] [Google Scholar]