Abstract
Objective
Rates of obesity among children have been rising in recent years. Information on the prevalence of obesity in children living in rural communities is needed. We report the prevalence of overweight and obesity in children enrolled in grades 4 to 6 who live in rural areas of Louisiana, U.S.
Methods and Procedures
These data were collected as baseline assessment for the Louisiana (LA) Health project. Height, weight, and estimates of body fat (using body impedance analysis) were collected on 2709 children. Average age was 10.5 years and the sample composition was 57.3% girls, 61.7% African-American, 36.0% Caucasian, and 2.3% other minority. A majority of children (77%) met the criterion for poverty status.
Results
The distribution of body mass index (BMI) percentile was highly skewed toward obesity. The most frequent BMI percentile scores were 98th and 99th percentile. Using Centers for Disease Control and Prevention (CDC) norms, the overall prevalence of obesity was 27.4% and for overweight was 45.1% of which 17.7% were between the 85th and 95th percentile. The prevalence of childhood overweight and obesity were much higher than the national norm and this increased prevalence was observed in both genders and in Caucasian and African American children.
Discussion
The prevalence of childhood overweight and obesity was found to be much higher in rural and primarily poor (77%) children living in Louisiana when compared to national norms. This observation suggests that rural children from Louisiana may be experiencing an epidemic of obesity that exceeds national prevalence estimates.
Keywords: childhood obesity, population studies, rural health, childhood gender differences, ethnicity
The prevalence of childhood obesity has been rising at alarming rates over the past 20 years (1, 2). Recently, the American Academy of Pediatrics (3) recommended that childhood obesity should be defined as a BMI percentile (based on CDC charts) ≥ 95th percentile and childhood overweight should be defined as a BMI percentile ≥ 85th and < 95th percentiles. Similar, but slightly different cut-off BMI values have been proposed for international standards (4). The most recent national survey from the National Nutrition and Health Survey (NHANES) in 2003-2006 (1) reported that 31.9% of children between the ages of 2 and 19 years were overweight or obese (1).
In the context of the growing epidemic of childhood obesity, there has been increased interest in the prevalence of obesity in specific populations (5–9). Few studies have examined childhood overweight or obesity in rural children living in the U.S (10).
The aims of this study were to: 1) describe distributions of BMI, BMI percentile scores, and estimated percent body fat, as measured by bioelectric impedance analysis (BIA) in a relatively large sample of mostly poor (77%) children from rural Louisiana, U.S. and 2) compare the prevalence of overweight and obesity to the 2003–2006 NHANES survey report of a representative national (U.S.) sample. Secondary aims were to compare BMI and estimated percent body fat for boys and girls and two ethnic groups (Caucasian and African American) and to report the prevalence data using the international classification system (4).
Methods and Procedures
Participants
Research participants were recruited for the LA Health project (11) A total of 2709 students in grades 4 to 6 were enrolled and measured at baseline, which represented 44% of the total number of eligible students. The students were recruited from 43 public schools in small towns and rural (12) areas of Louisiana. The recruitment strategy called for recruiting all students in the 43 schools who were in grades 4 to 6, without regard to weight status, gender, or ethnicity. The data reported in this paper were collected as baseline assessments for the three-year randomized controlled trial for prevention of excessive weight gain in children (11).
Assessment Measures
Body Mass Index Percentile scores and body composition
Height was measured using a stadiometer (Seca 225 Hite-Mobile height rod). Weight was asessed using Tanita (model TBF-310) scales that measured body weight and body composition, using bioelectric impedance analysis (BIA). Height and weight were converted to body mass index (BMI = kg/m2). BMI was converted to percentile scores based on gender and age using norms provided by the CDC in 2000. Using BMI percentile scores, children were classified using the criteria recommended by the American Academy of Pediatrics (3): underweight (< 5th percentile), normal weight (≥ 5th and < 85th percentiles) overweight (≥ 85th and < 95th percentiles, and obese (≥ 95th percentile).
Demographic Data
Birthdates for each child were reported by the parent who consented for the child’s participation in the study and were confirmed by school records. Gender and racial/ethnic status were both self-reported by the child and were confirmed by school records.
Socioeconomic Status
Socioeconomic status (SES) was defined using data from the School Lunch program (13) provided by the Louisiana State Board of Education.
Procedures
The primary data (height, weight, BIA, and gender and ethnic/racial group) were measured for each individual child during the period of September to November, 2006. These data were collected in a secure, private environment at the child’s school.
Statistical Methods
Linear mixed models were used to evaluate gender and race difference on BMI percentile and percent body fat. Gender, race, and the gender by race interaction were included in the model as fixed effects, with the school treated as a random effect. Socioeconomic status was entered in statistical models as a covariate. When evaluating the association of gender and ethnicity, only African American and Caucasian participants were included in the analyses. For these analyses, data of 64 participants (2.3%) of “other ethnic” status were not included. All analyses were performed using Statistical Analysis Software (17) 9.1. Alpha level p < 0.05 was selected for the interpretation of all statistical analyses.
Results
Description of the Sample
The study sample (N = 2709) included 1553 (57.3%) girls and 1156 (42.7%) boys. A majority of the sample reported African American (Non-Hispanic Black) ethnicity (n = 1671; 61.7%); 974 (36.0%) were Caucasian (Non-Hispanic White). The average age of the sample was 10.5 years old (age range = 8 to 15years). The average BMI percentile was 69.8 and the average estimated percent body fat was 25.1%.
Based on data from the school lunch program, 77.0% of the participants were classified as low SES, 7.5% were classified as low to moderate SES, and 15.4% were classified as moderate to high SES. SES was not a significant factor in any statistical model; hence SES was not included in the analyses reported in the paper.
Body Mass Index Percentile
Complete Sample
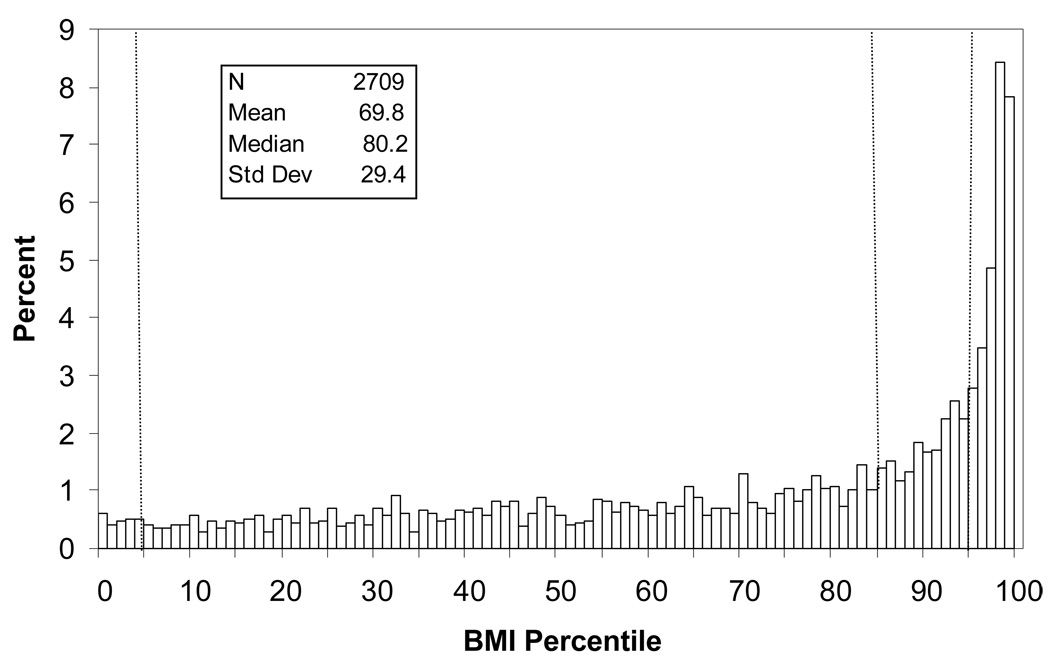
Figure 1 presents the frequency distribution for BMI %tile for the 2709 participants in the LA Health sample at baseline, which was highly skewed toward obesity. The most frequent BMI percentile scores were the 98th and 99th percentiles. The dashed lines represent the 5th, 85th, and 95th percentiles. Approximately 45% of the sample met the criteria for overweight or obese.
Figure 1.
BMI %tile distribution for the complete LA Health sample. The dashed lines are provided to distinguish underweight (< 5th %tile), overweight (≥ 85th %tile), and obese (≥ 95th %tile).
Table 1 summarizes the classification of children in terms of BMI status. Very few children (2.5%) were underweight. A slight majority (52.4%) was normal weight; 17.7% were overweight, and 27.4% were classified as obese.
Table 1.
Prevalence of overweight and obesity as determined by percentiles compared to NHANES surveys from 1963–94 by gender and ethnicity.
| Boys | Girls | ||||
|---|---|---|---|---|---|
| Weight Status BMI Percentile |
Total Sample | Caucasian | African American |
Caucasian | African American |
| Underweight percentile < 5 |
68(2.5%) | 16(3.6%) | 15(2.2%) | 16(3.0%) | 19(1.9%) |
| Normal Weight 5≤percentile <85 |
1421(52.4%) | 231(52.3%) | 385(56.0%) | 271(50.9%) | 504(51.3%) |
| Overweight 85≥percentile <95 |
479(17.7%) | 88(19.9%) | 108(15.7%) | 107(20.1%) | 167(17.0%) |
| Obese percentile ≥95 |
741(27.4%) | 107(24.2%) | 180(26.2%) | 138(25.9%) | 293(29.8%) |
| Total | 2709 | 442 | 688 | 532 | 983 |
Comparison of Boys and Girls as a Function of Gender and Ethnicity
To examine differences in BMI percentile associated with gender and ethnicity, the sub-sample of 2645 Caucasian and African American children was studied. Logistic regression was used to test for different prevalence rates associated with gender, ethnicity, or the interaction of gender and ethnicity. There were no differences in the prevalence of overweight/obesity or non-overweight status (Table 1) across the four groups, p = 0.09. A comparison of BMI percentile values in a Gender X Ethnic Group Analysis of Variance indicated a statistically significant main effect for gender (p < 0.02) with girls (M = 70.8±0.8) having higher BMI percentiles than boys (M = 67.9±0.9). The Ethnicity main effect and the Gender X Ethnicity interaction were not statistically significant (p > 0.05).
Comparison of BMI %tiles to CDC Norms
Table 3, presents the prevalence of childhood obesity and overweight/obese status of the LA Health sample with the latest NHANES data 2003–2006, for comparative purposes. Since the age range for children in the LA Health sample (8 to 15 years) overlaps the younger and older NHANES samples, this table includes statistics from both age ranges, i.e., 6 to 11 years and 12 to 19 years, for African-American and Caucasian boys and girls. The percentage of overweight/obese children of the LA Health sample is consistently higher than reported in NHANES 2003–2004, but this difference is primarily attributable to the very high rates of childhood obesity (25.8% for boys and 28.5% for girls) in the LA Health sample.
Table 3.
Prevalence of overweight and obesity by gender and ethnicity using the IOTF BMI cut-offs (4)
| Boys | Girls | ||||
|---|---|---|---|---|---|
| Weight Status | Total Sample | Caucasian | African American |
Caucasian | African American |
| Normal | 1513(55.9%) | 259(58.6%) | 417(60.1%) | 285(53.6%) | 519(52.8%) |
| Overweight | 606(22.4%) | 103(23.3%) | 129(18.8%) | 131(24.6%) | 232(23.6%) |
| Obese | 590(21.8%) | 80(18.1%) | 142(20.6%) | 116(21.8%) | 232(23.6%) |
| Total | 2709 | 442 | 688 | 532 | 983 |
International Reference System (4)
Table 3 summarizes the weight classification of the LA Health sample using international standards reported by Cole, et al (4). Generally, relative to the U.S. system, the international system derives higher prevalence rates of overweight and lower prevalence rates of obesity and this pattern was observed in the LA Health sample. Differences in the prevalence of overweight/obesity as a function of gender, ethnicity, and the interaction of gender and ethnicity were compared using logistic regression. An effect associated with gender was found (p < 0.001). Girls had a higher prevalence of overweight and obesity in comparison to boys. The odds ratio indicated a protective effect associated with male gender, odds ratio = 0.88; 95% CI: 0.81 – .95.
Estimated percent Body Fat
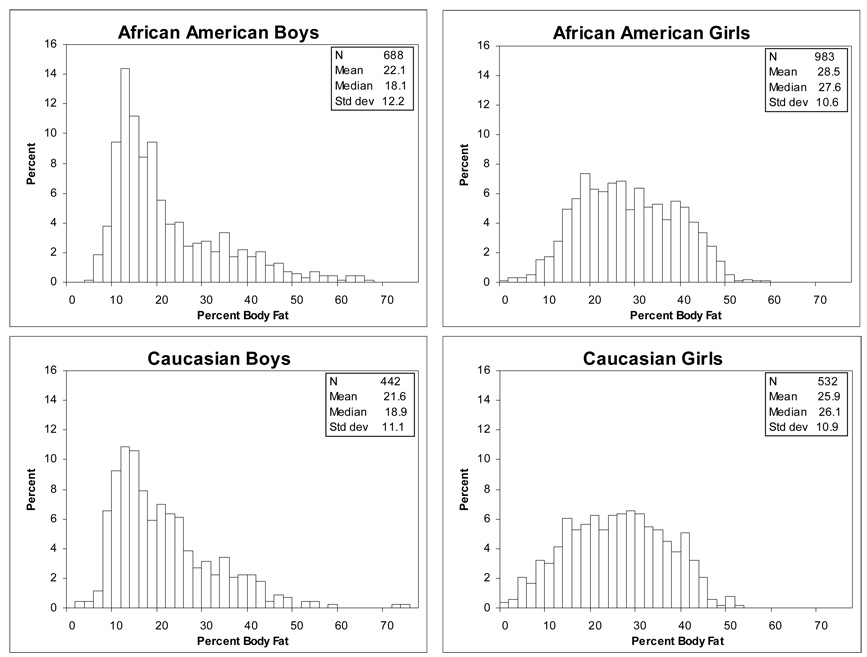
There are well established gender differences in body composition as measured by BIA (14). The sub-sample of Caucasian and African American boys and girls was studied to test for gender and ethnic differences in percent body fat. The interaction of age and gender was a significant covariate (p < 0.0001). Age was positively correlated with percent body fat of girls (r = 0.17, p < 0.0001), but was negatively correlated with percent body fat of boys (r = −0.12, p = 0.0001). A statistically significant main effect for gender was observed (F = 34.05, p < 0.0001). The distributions are depicted in Figure 2. Girls (M = 27.4±0.4) had higher percent body fat than boys (M = 22.0± 0.4). A significant main effect for ethnicity was also found (F = 10.99, p = 0.001). African American children (M = 25.2±0.4) had higher percent body fat than Caucasian children (M = 23.9±0.5).
Figure 2.
Estimated percent body fat distributions for Caucasian and African American boys and girls.
Discussion
The findings of this study should be interpreted recognizing certain limitations. The study sample was recruited for participation in an obesity prevention study and was not a random sample of children living in rural areas. In addition, the sample contained a wide range of ages and, thus, levels of maturation. Tanner stage was not documented in the study, so we were unable to control for the effect of maturation on body composition, which is highly variable during pubertal development. The children resided in Louisiana and the findings should not be generalized to all children, all rural children, or all children living in the southern United States. Nevertheless, the sample was quite large and was drawn from a diverse set of communities across the state of Louisiana. The recruitment strategy aimed to recruit all students, not just those who were overweight or obese. Nevertheless it is possible that this recruitment strategy did not result in a representative sample of the student populations. The sample also included a large number of African American children. Height, weight, and body impedance were carefully measured for each child by qualified technicians.
The aims of the study were to describe the distributions of body mass index and percent body fat and to compare the BMI distribution to the 2003–2004 NHANES prevalence rates of overweight and obesity. The primary finding was that children from the LA Health sample were frequently overweight or obese and that the prevalence rates of obesity for the LA Health sample significantly exceeded those reported nationally (1). When BMI was evaluated in terms of international standards (4), a similarly high rate of obesity was observed. Estimates of percent body fat suggested that the high prevalence of overweight and obesity corresponded to relatively high levels of adiposity.
It is noteworthy that prevalence rates of overweight/obesity were generally more similar than different across boys and girls and Caucasians and African American children. In all groups, the prevalence of obesity was remarkably high. The finding of exceptionally high rates of obesity in ethnic minority groups (Native American, African American, and Hispanic children) has been reported in one recent study of rural children in Oklahoma. This study (10), however, reported much lower rates of obesity in Caucasian children.
In conclusion, the results of this cross-sectional study of a relatively large sample of children living in rural areas of Louisiana indicated that the prevalence of overweight and obesity was much higher than that observed nationally. Of considerable importance is the finding that the high rates of obesity were not specific to boys or girls or Caucasians or African Americans. The problem of obesity was found to be widespread, broadly and equally affecting children from different ethnic groups and both boys and girls from lower and higher SES families. These data suggest a strong need to investigate the extent of this problem, using appropriate methods to recruit a representative sample, in other rural areas. Such research might identify risk factors that are unique to rural environments so that effective interventions for this major public health risk can be tailored to the needs of rural children.
Table 2.
Prevalence of overweight and obesity in comparison to NHANES survey data collected from 2003–2006 by gender and ethnicity.
| Boys | Girls | ||||||
|---|---|---|---|---|---|---|---|
| NHANES 2003–2006 (6–11yrs) | NHANES 2003–2006 (12–19yrs) | LA Health (8–15 yrs) | NHANES 2003–2006 (6–11yrs) | NHANES 2003–2006 (12–19yrs) | LA Health (8–15 yrs) | ||
| All | Overweight/Obese | 33.9±2.2 | 34.9±1.9 | 42.9±1.5 | 32.6±2.4 | 33.3±1.8 | 46.6±1.3 |
| Obese | 18.0±1.7 | 18.2±1.5 | 25.8±1.3 | 15.8±1.4 | 16.8±1.5 | 28.5±1.1 | |
| African | Overweight/Obese | 33.8±3.6 | 32.1±1.8 | 41.9±1.9 | 40.1±2.3 | 44.5±1.5 | 46.8±1.6 |
| American | Obese | 18.6±2.6 | 18.5±1.3 | 26.2±1.7 | 24.0±2.0 | 27.7±1.9 | 29.8±1.5 |
| Caucasian | Overweight/Obese | 31.7±3.6 | 34.5±2.6 | 44.1±2.4 | 31.5±3.6 | 31.7±2.4 | 46.1±2.2 |
| Obese | 15.5±2.8 | 17.3±2.0 | 24.2±2.0 | 14.4±2.1 | 14.5±2.0 | 25.9±1.9 | |
Acknowledgements
The authors greatly appreciate the assistance and support that the LA Health project has received from Kerry Davidson, Ph.D., the LA GEAR UP program, and the LA Board of Regents. We would also like to thank the superintendents, principals, and staff at each of the schools in the project and express our appreciation to the LA Health research staff that collected these data. Finally, we acknowledge the valuable critique of an earlier version of this manuscript by Claude Bouchard, Ph.D. and Peter Katzmarzyk, Ph.D.
Grant Support: This project was supported by the National Institute for Child Health and Human Development of the National Institutes of Health (R01 HD048483) and the U.S. Department of Agriculture (58-6435-4-90). The clinical trial number for this project is: NCT00289315. In addition, this work was partially supported by the CNRU Center Grant #1P30 DK072476 entitled “Nutritional Programming: Environmental and Molecular Interactions” sponsored by NIDDK.
References
- 1.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US chidren and adolescents, 2003–2006. JAMA. 2008 May 5;299(20):2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999–2000. JAMA. 2002 Oct 9;288(14):1728–1732. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- 3.Krebs NF, Himes JH, Jacobson D, Nicklas TA, Guilday P, Styne D. Assessment of child and adolescent overweight and obesity. Pediatrics. 2007 Dec;120 Suppl 4:S193–S228. doi: 10.1542/peds.2007-2329D. [DOI] [PubMed] [Google Scholar]
- 4.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000 May 6;320(7244):1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Henry SL, Courtney A, Tietyen J, et al. Prevalence of childhood obesity in Kentucky 2003. J Ky Med Assoc. 2004 Feb;102(2):48–52. [PubMed] [Google Scholar]
- 6.Haque F, de la Rocha AG, Horbul BA, Desroches P, Orrell C. Prevalence of childhood obesity in northeastern Ontario: a cross-sectional study. Can J Diet Pract Res. 2006 Autumn;67(3):143–147. doi: 10.3148/67.3.2006.143. [DOI] [PubMed] [Google Scholar]
- 7.Moayeri H, Bidad K, Aghamohammadi A, et al. Overweight and obesity and their associated factors in adolescents in Tehran, Iran, 2004–2005. Eur J Pediatr. 2006 Jul;165(7):489–493. doi: 10.1007/s00431-006-0101-8. [DOI] [PubMed] [Google Scholar]
- 8.Langendijk G, Wellings S, van Wyk M, Thompson SJ, McComb J, Chusilp K. The prevalence of childhood obesity in primary school children in urban Khon Kaen, northeast Thailand. Asia Pac J Clin Nutr. 2003;12(1):66–72. [PubMed] [Google Scholar]
- 9.Bassett DR, Jr., Tremblay MS, Esliger DW, Copeland JL, Barnes JD, Huntington GE. Physical activity and body mass index of children in an old order Amish community. Med Sci Sports Exerc. 2007 Mar;39(3):410–415. doi: 10.1249/mss.0b013e31802d3aa7. [DOI] [PubMed] [Google Scholar]
- 10.Eichner JE, Moore WE, Perveen G, Kobza CE, Abbott KE, Stephens AL. Overweight and obesity in an ethnically diverse rural school district: the healthy kids project. Obesity. 2008 Feb;16(2):501–504. doi: 10.1038/oby.2007.60. [DOI] [PubMed] [Google Scholar]
- 11.Williamson DA, Champagne CM, Harsha D, et al. Louisiana (LA) Health: Design and Methods for a Childhood Obesity Prevention Program in Rural Schools. Contemp Clin Trials. doi: 10.1016/j.cct.2008.03.004. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hart LG, Larson EH, Lishner DM. Rural definitions for health policy and research. Am J Public Health. 2005 Jul;95(7):1149–1155. doi: 10.2105/AJPH.2004.042432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vieweg VR, Johnston CH, Lanier JO, Fernandez A, Pandurangi AK. Correlation between high risk obesity groups and low socioeconomic status in school children. South Med J. 2007 Jan;100(1):8–13. doi: 10.1097/01.smj.0000253479.03665.6f. [DOI] [PubMed] [Google Scholar]
- 14.Heymsfield SB, Shen W, Want Z, Baumgartner RN, Allison DB, Ross R. Evaluation of Total and Regional Adiposity. In: Bray GA, Bouchard C, editors. Handbook of Obesity: Etiology and Pathophysiology. Second ed. New York: Marcel Dekker, Inc.; 2004. pp. 33–79. [Google Scholar]