Abstract
AIM: To attempt rectal administration of rebamipide in the treatment of ischemic colitis patients with ulcers, and evaluate its effects.
METHODS: We compared 9 ischemic colitis patients (2 men, 7 women) with ulcers treated by bowel rest only from 2000 to 2005 (conventional therapy group), with 6 patients (2 men, 4 women) treated by rebamipide enema therapy in 2006 (rebamipide enema therapy group) and analyzed the mean duration of fasting and hospitalization, degree of ulcer healing, and decrease in WBC count for the two groups.
RESULTS: The mean duration of fasting and hospitalization were 2.7 ± 1.8 d and 9.2 ± 1.5 d in the rebamipide group and 7.9 ± 4.1 d and 17.9 ± 6.8 d in the control group, respectively, and significantly reduced in the rebamipide group (t = -2.915; P = 0.0121 and t = -3.054; P = 0.0092). As for the degree of ulcer healing at 7 d after admission, the ulcer score was reduced by 3.5 ± 0.5 (points) in the rebamipide group and 2.8 ± 0.5 (points) in the control group (t = 1.975; P = 0.0797), while the decrease in WBC count was 120.0 ± 55.8 (× 102/μL) in the rebamipide group and 85.9 ± 56.8 (× 102/μL) in the control group (t = 1.006; P = 0.3360).
CONCLUSION: In left-sided ischemic colitis patients with ulcers, rebamipide enema therapy significantly reduced the duration of fasting and hospitalization, recommending its use as a new and effective therapeutic alternative.
Keywords: Ischemic colitis, Rebamipide-enema, Fasting, Hospitalization, Ulcer healing, White blood cells
INTRODUCTION
Ischemic colitis was described in 1963 by Boley et al[1] as reversible occlusion of the blood supply to the colon. In 1966, Marston et al[2] proposed the term ischemic colitis, establishing it as a definite disease entity, and classified the condition into 3 types namely, transient, stricture, and gangrenous. Today, ischemic colitis is considered to be a common disease of the large intestine, and is thought to be caused by various factors including vascular factors such as ischemia and embolism[3–5], and intestinal factors such as constipation[6,7], irritable bowel syndrome[8,9], and history of intestinal surgery[10,11]. Endoscopically, ischemic colitis is characterized by edema, erythema, erosion, and ulceration of the colonic mucosa, and pathologically the condition is characterized by diffuse hemorrhage and edema in the submucosal layer, degeneration, desquamation and necrosis of the mucosal epithelium, congestion of the lamina propria, fibrin thrombi in the capillaries, and slight neutrophilic infiltration. According to Reeders et al ischemic colitis involves the left colon in 75% of the cases and the right colon in 8%[12].
While surgery is indicated for treatment of the gangrenous type of ischemic colitis, many patients with the transient or stricture types of the disease improve with bowel rest by fasting and parenteral fluid administration alone. However, healing is frequently delayed in patients with ulcerative lesions. We previously reported that ischemic colitis patients with ulcerative lesions require a significantly longer fasting period and duration of hospitalization as compared with those without ulcerative lesions[13]. A longer fasting period and longer duration of hospitalization pose problems, including stress associated with fasting and a high cost of long-term hospitalization.
Rebamipide is an anti-ulcer drug launched in various Asian countries, that has been reported to have ulcer healing effects[14,15], anti-inflammatory effects[15], suppressant effects against free radical production[16–19] and mucin secretion-inducing effects[20,21]. Recently, the efficacy of rebamipide enema in the treatment of ulcerative colitis has been reported in Japan[22–25].
In this retrospective cohort study, we evaluated the therapeutic effects of rebamipide solution administered as an enema in ischemic colitis patients with ulcerative lesions, with special attention paid to the fasting period and duration of hospitalization.
MATERIALS AND METHODS
Fifteen ischemic colitis patients (4 men, 11 women; mean age, 68 years) with ulcerative lesions who were admitted to our hospital during the 7 years between 2000 and 2006 were investigated in a non-randomized study. Nine ischemic colitis patients (2 men, 7 women; mean age, 68 years) with ulcerative lesions were treated by fasting and parenteral fluid administration during the 6 years between 2000 and 2005 (conventional therapy group). Six ischemic colitis patients (2 men, 4 women; mean age, 69 years) with ulcerative lesions were assigned to rebamipide enema therapy in addition to conventional therapy in 2006 (rebamipide enema therapy group). Patients who were admitted for other diseases but developed ischemic colitis during the course of those diseases were excluded. The diagnosis of ischemic colitis was made based on colonoscopic and histopathologic findings in biopsy specimens combined with the following three essential criteria: absence of prior antibiotics, negative cultures of feces or biopsy specimens for bacteria, and absence of history of inflammatory bowel disease (IBD). The age at onset, mode of onset, symptoms, and the location of the lesions were used as supplemental information.
Conventional therapy and rebamipide enema therapy groups were compared with respect to age, gender, location of lesions, hematological and blood chemistry findings, performance status (0-4 based on the WHO performance scale: 0, asymptomatic; 1, symptomatic but completely ambulant; 2, symptomatic, up and about > 50% of waking hours; 3, symptomatic, confined to bed or chair > 50% of waking hours, but not bed- or chair-bound; 4, bed- or chair-bound), prevalence of underlying diseases (hypertension, hyperlipidemia, diabetes mellitus, chronic atrial fibrillation, cerebral infarction, constipation, history of abdominal surgery), oral medication, mean fasting period, mean duration of hospitalization, degree of ulcer healing, and decrease in WBC count. The breakdown of the oral medication was: antihypertensive agent 5 cases, digitalis 1 case in the conventional therapy group, and antihypertensive agent 1 case, diuretic 1 case in the rebamipide enema therapy group. For evaluation of the degree of ulcer healing, the ulcerative lesions were classified into stages according to the Sakita-Miwa classification of gastric ulcers[26] (Table 1), then the stage was converted into numerical scores as follows: A1: 6 points, A2: 5 points, H1: 4 points, H2: 3 points, S1: 2 points, S2: 1 point. The difference between the score at baseline (time of diagnosis) and the score at the follow-up examination was calculated and divided by the number of days between the baseline and the follow-up examinations for evaluation of the therapeutic effects. The result was corrected to the value at 7 d from the baseline and used for the analysis. To further strengthen the objectivity of the evaluation, the decrease in WBC count was calculated by subtracting the WBC count at the follow-up examination from that at the baseline, and divided by the number of days between the baseline and follow-up examinations. The value obtained was corrected to the value at 7 d from the baseline for use in the analysis.
Table 1.
Stage classification of gastric ulcer by Sakita-Miwa and its translation into numerical expression[26]
| Stages | Manifestation | |
| Active stage | A1 (6p) | The surrounding mucosa is edematously swollen and no regenerating epithelium is seen endoscopically |
| A2 (5p) | The surrounding edema has decreased, the ulcer margin is clear, and a slight amount of regenerating epithelium is seen in the ulcer margin. A red halo in the marginal zone and a white slough circle in the ulcer margin are frequently seen. Usually, converging mucosal folds can be followed right up to the ulcer margin | |
| Healing stage | H1 (4p) | The white coating is becoming thin and the regenerating epithelium is extending into the ulcer base. The gradient between the ulcer margin and the ulcer floor is becoming flat. The ulcer crater is still evident and the margin of the ulcer is sharp. The diameter of the mucosal defect is about one-half to two-thirds that of A1 |
| H2 (3p) | The defect is smaller than in H1 and the regenerating epithelium covers most of the ulcer floor. The area of white coating is about a quarter to one-third that of A1 | |
| Scarring stage | S1 (2p) | The regenerating epithelium completely covers the floor of ulcer. The white coating has disappeared. Initially, the regenerating region is markedly red. Upon close observation, many capillaries can be seen. This is called “red scar” |
| S2 (1p) | In several months to a few years, the redness is reduced to the color of the surrounding mucosa. This is called “white scar” |
Colonoscopy was performed in all the patients within 3 d of admission or within 5 d of onset of the symptoms. Colonoscopic follow up was conducted in a total of 11 patients, including all the patients in the rebamipide group. Treatment included bowel rest by fasting and parenteral fluid administration in all the patients, oral antiflatulent agents in 4 patients (23.5%), and administration of antibiotics in 4 patients (23.5%); none of the patients needed intravenous hyperalimentation. Treatment was provided in all patients within 5 d of onset of the symptoms. Oral food intake was allowed when the abdominal pain resolved. If no symptomatic recurrence was noted after the start of oral food intake, the patient was discharged.
For rebamipide enema therapy, 150 mg of rebamipide was suspended in 60 mL of warm water and administered through Nelaton’s catheter once daily. The subjects remained in the left lateral decubitus position for 30 min. The period of administration varied depending on individual patient needs. The mean duration of treatment was 7 ± 1.6 d in the rebamipide enema therapy group. This study was allowed by the institutional ethical committee. Prior to the administration of rebamipide enema, all the patients were provided with a thorough explanation of the treatment, and informed consent was obtained from each of them.
Statistical analysis
Data are expressed as mean ± SD or percentage. The percentage of females and the distribution of the lesion location, performance status, and underlying systemic diseases in the two groups were evaluated by the Fisher’s exact test. Other data were evaluated by Student’s t-test after log-transformation of skewed variables. All data analyses were performed with the StatView 5.0. Statistical significance was set at P < 0.05.
RESULTS
Fifteen patients (4 men, 11 women; mean age, 68 years) were eligible for the analyses. The location of the lesions with allowance given for partial overlapping of the lesions, was the sigmoid colon in 66.7%, descending colon in 66.7%, transverse colon in 20.0%, and the rectum or ascending colon in 0% of the patients. In relation to the number of episodes of ischemic colitis experienced by the patients, 93.3% of the patients had suffered from one episode and 6.7% had suffered from two episodes.
The rebamipide enema therapy group consisted of 6 patients (2 men, 4 women), with an average age of 69 years (41-85), and the lesion was located in the left colon in all the patients. The conventional therapy group consisted of 9 patients (2 men, 7 women), with an average age of 68 years (35-87), and the lesion was located in the left colon in 8 patients. There were no statistically significant differences in any of the background factors between the groups, including the prevalence of hypertension, hyperlipidemia, diabetes mellitus, atrial fibrillation, cerebral infarction and chronic constipation, history of abdominal surgery, oral medication, performance status, and hematological and blood chemistry findings (Tables 2 and 3).
Table 2.
Clinical features of the ischemic colitis patients: Comparison between the rebamipide and conventional therapy groups
| Conventional group (n = 9) | Rebamipide group (n = 6) | Statistical significance | |
| Age (mean, range, yr) | 68 ± 19 (35-87) | 69 ± 16 (41-85) | NS |
| Percentage of females (%) | 77.8 | 66.7 | NS |
| Lesion location: left colon (%) | 88.9 | 100 | NS |
| Performance status 0-1 (%) | 77.8 | 100 | NS |
| WBC count (× 103/μL) | 12.3 ± 4.7 | 13.5 ± 5.3 | NS |
| CRP (mg/dL) | 2.6 ± 4.1 | 1.7 ± 1.8 | NS |
| K (mEq/L) | 3.8 ± 0.4 | 4.2 ± 0.5 | NS |
| Total cholesterol (mg/dL) | 179.3 ± 30.6 | 191.2 ± 63.0 | NS |
| TG (mg/dL) | 93.3 ± 41.0 | 131.2 ± 74.2 | NS |
| LDH (IU/L) | 190.0 ± 42.8 | 202.8 ± 18.2 | NS |
| CPK (IU/L) | 80.7 ± 38.9 | 118.0 ± 76.6 | NS |
Values are the mean ± SD. The percentage of females and the lesion location were evaluated by the Fisher’s exact test. Other data were evaluated by Student’s t-test after skewing the values by log transformation. WBC: White blood cell; CRP: C-reactive protein; K: Potassium; TG: Triglyceride; LDH: Lactate dehydrogenase; CPK: Creatinine phosphokinase.
Table 3.
Underlying disease: Comparison between the rebamipide and conventional therapy groups n (%)
| Conventional group (n = 9) | Rebamipide group (n = 6) | Statistical significance | |
| Hypertension | 6 (66.7) | 2 (33.3) | NS |
| Hyperlipidemia | 0 | 3 (50.0) | NS |
| Diabetes mellitus | 1 (11.1) | 1 (16.7) | NS |
| Atrial fibrillation | 1 (11.1) | 0 | NS |
| Cerebral infarction | 1 (11.1) | 0 | NS |
| Chronic constipation | 5 (55.6) | 1 (16.7) | NS |
| Medications | |||
| Antihypertensive agents | 5 (55.6) | 1 (16.7) | NS |
| Others | 1 (11.1) | 1 (16.7) | NS |
| History of abdominal surgery | 4 (44.4) | 3 (50.0) | NS |
Values are expressed in percentages. Percentages were evaluated by the Fisher’s exact test.
The mean fasting period and mean duration of hospitalization were 2.7 ± 1.8 d and 9.2 ± 1.5 d respectively, in the rebamipide enema therapy group, as compared with 7.9 ± 4.1 d and 17.9 ± 6.8 d respectively, in the conventional therapy group. Both the fasting period (P = 0.0121) and the duration of hospitalization (P = 0.0092) were significantly shorter in the rebamipide enema therapy group (Table 4). As for the degree of ulcer healing, the ulcer score was reduced by 3.5 ± 0.5 (points) in the rebamipide enema therapy group and 2.8 ± 0.5 (points) in the conventional therapy group (P = 0.0797), with the interval between the baseline and follow-up examinations being 6.5 ± 0.8 d and 7.7 ± 2.7 d respectively (P = 0.3293). The WBC count was decreased by 12.0 ± 5.6 (× 103/μL) in the rebamipide enema therapy group and 8.6 ± 5.7 (× 103/μL) in the conventional therapy group (P = 0.3360), with the interval between the baseline and follow-up examinations of 5.8 ± 1.7 d and 5.4 ± 1.5 d, respectively (P = 0.7515). Thus, both the degree of ulcer healing and the decrease in WBC count tended to be favorable in the rebamipide enema therapy group compared to the conventional therapy group, but there was no significant difference in either parameter between the two groups (Table 4). No adverse events were noted in any of the patients.
Table 4.
Duration of fasting, duration of hospitalization and reduction in the ulcer score: Comparison between the rebamipide and conventional therapy groups
| Conventional group (n = 9) | Rebamipide group (n = 6) | Statistical significance | |
| Duration of fasting (d) | 7.9 ± 4.1 | 2.7 ± 1.8 | P = 0.0121 |
| Duration of hospitalization (d) | 17.9 ± 6.8 | 9.2 ± 1.5 | P = 0.0092 |
| Degree of ulcer healing1 (points) | 2.8 ± 0.5 (n = 5) | 3.5 ± 0.5 | P = 0.0797 |
| WBC decrease2 (× 103/μL) | 8.6 ± 5.7 | 12.0 ± 5.6 | P = 0.3360 |
Values are the mean ± SD.
The ulcer lesion was scored according to the Sakita-Miwa classification of the stage of gastric ulcer, then the difference between the baseline score (at the time of diagnosis) and at the time of the follow-up colonoscopy was divided by the number of days between the baseline and the follow-up examination, to correct the results to the value on d 7 (A1: 6 points, A2: 5 points, H1: 4 points, H2: 3 points, S1: 2 points, S2: 1 point).
Difference in value between that measured at admission and that measured at the time of the follow-up was divided by the number of days between the two examinations to correct the results to the value on d 7.
In a representative case of a 41-year-old man with ischemic colitis with ulcerative lesions located in the transverse colon, descending colon and sigmoid colon, who was treated by rebamipide enema for 7 d, the fasting period was 6 d and the duration of hospitalization was 10 d (Figures 1 and 2).
Figure 1.
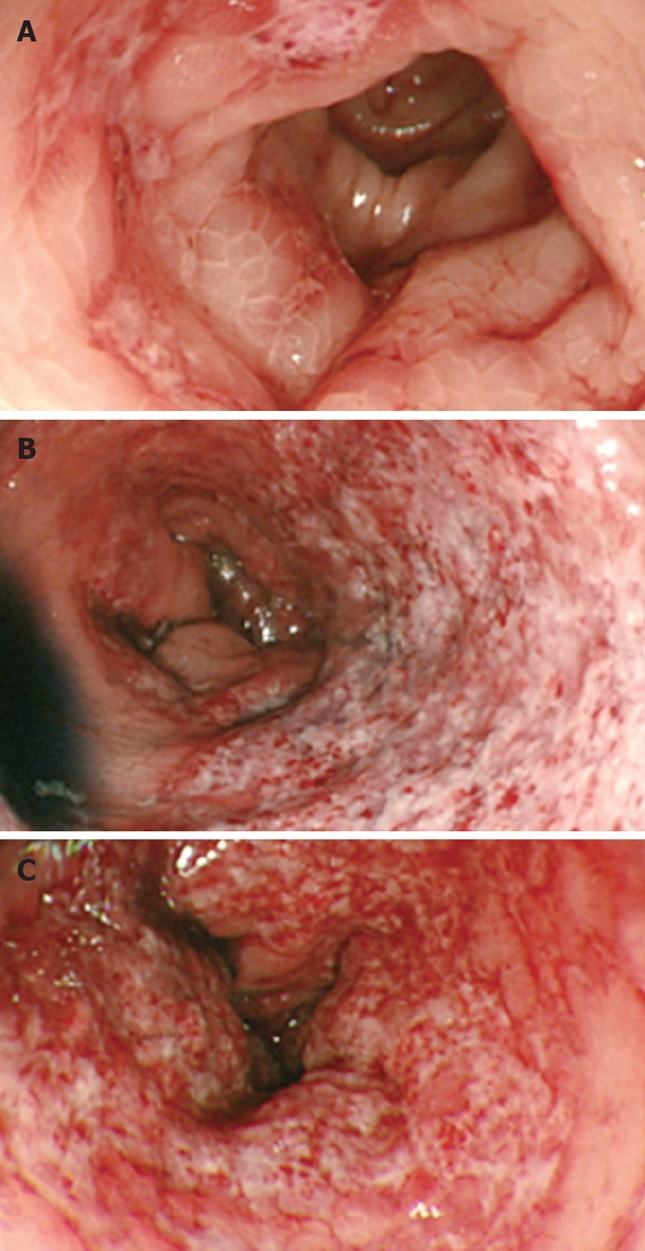
Colonoscopic findings at the time of diagnosis of ischemic colitis. A: Transverse colon; B: Descending colon; C: Sigmoid colon.
Figure 2.
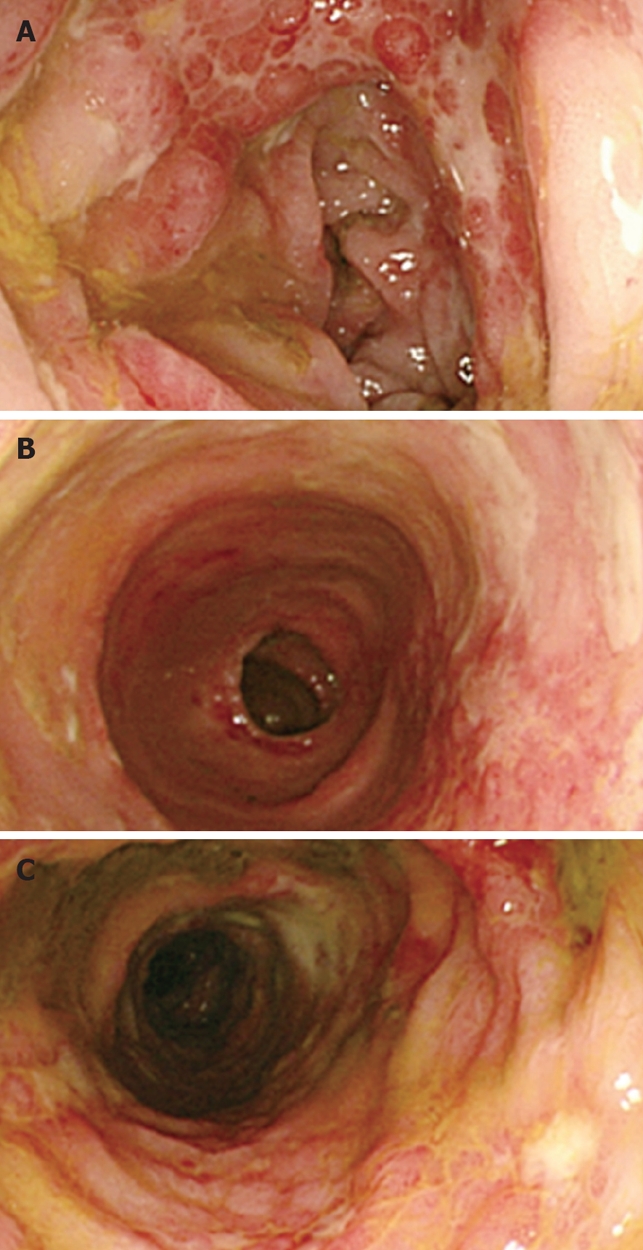
Colonoscopic findings at the time of evaluation at 1 wk after the start of rebamipide enema therapy. A: Transverse colon; B: Descending colon; C: Sigmoid colon.
DISCUSSION
With the aging of population in Japan and around the world, atherosclerosis and malignancy are two of the major diseases facing our nation. Epidemiological data in Japan reveal that malignant neoplasms rank first as the cause of death, while heart diseases and cerebrovascular diseases together account for about 30% of all deaths, which represents the percentage of deaths caused by malignant neoplasms. Since the prevalence of atherosclerotic diseases may be expected to increase further with the accelerated aging of populations, an increase in the incidence of ischemic colitis is also inevitable. In fact, we have documented an annual increase in the prevalence of ischemic colitis in our care-providing area.
We previously reported that the fasting period and the duration of hospitalization were significantly prolonged in ischemic colitis patients with ulcerative lesions[13], and sought suitable treatment methods to shorten these parameters. In this study, we evaluated the effects of rebamipide enema therapy in these patients. Rebamipide is an anti-ulcer drug used to treat peptic ulcer, that has been demonstrated to enhance the production of endogenous prostaglandin E2 via COX-2 and thereby act as a gastric mucosal protectant[27–29], to promote mucin production[20,21], and to suppress the production of free radicals, such as hydroxyl radicals and superoxide ions[16–19]. Farhadi et al reported that rebamipide suppressed the production of reactive oxygen species by neutrophils in the presence of plasma and rectal perfusate in patients with ulcerative colitis[30]. It has been reported that in ulcerative colitis, excessive oxygen and free radicals produced by activated neutrophils and macrophages intensify the microcirculatory disorder and lipid peroxidation to aggravate the intestinal mucosal disorder; thus they play important roles in the mechanism of development of inflammation in this disease. Makiyama et al reported that the use of rebamipide enema therapy in addition to conventional therapy in patients with ulcerative colitis yielded favorable responses, and classified this therapy as a promising new strategy for the treatment of moderate or less than severe distal colitis or as a supplemental therapy during steroid withdrawal[22,23]. Furuta et al and Miyata et al likewise reported that rebamipide enema therapy was effective in patients with ulcerative colitis[24,25]. Oral administration of rebamipide at a dose of 300 mg daily has also been reported to result in remarkable improvement in patients with multiple small intestinal erosions[31].
Limited studies have discussed the mechanism of development of ischemic colitis. Ichihara et al produced an experimental model of ischemic colitis in rats, and reported that the development of lesions was clearly suppressed when the superoxide scavenger, liposomal-encapsulated superoxide dismutase (L-SOD), was administered. Based on this they suggested that the production of superoxide anions may be closely involved in the pathogenesis of ischemic colitis[32]. In hydrogen peroxide-induced hemorrhagic lesions of the gastric mucosa in the rat, rebamipide suppressed inactivation of SOD activity in a dose-dependent manner[33], suggesting that rebamipide might contribute to healing in ischemic colitis by suppressing the production of free radicals.
This study is an open label study by the non-randomization, and the small study population may be a weak point. In this study, the degree of ulcer healing and decrease in WBC count were used as objective indicators in the evaluation of healing. No significant difference in either parameter was observed between the treatment and previously untreated groups. However, the results did suggest that the healing of the lesions was accelerated to a greater extent in the rebamipide enema therapy group compared to the conventional therapy group.
The mechanism underlying the efficacy of rebamipide in the treatment of ischemic colitis remains unclear; however, it is assumed that the effect of the drug in suppressing free radical production and accelerating ulcer healing account for its efficacy in patients of ischemic colitis with ulcerative lesions.
Figures 1 and 2 show colonoscopic photographs of the large intestine in a patient who responded to rebamipide enema therapy. In this patient, skip ulcer lesions were present extending from the transverse to the sigmoid colon. Comparison of colonoscopic images of the large intestine obtained at the time of diagnosis (Figure 1) with those obtained at the time of follow-up 7 d after the initiation of rebamipide enema therapy (Figure 2) clearly revealed a more pronounced healing tendency toward the anal end. In regard to the effect of 5-ASA enema therapy and the site of the colon reached by the drug given as an enema in patients with ulcerative colitis, Bodegraven et al[34] and Otten et al[35] reported that following administration of 60 mL and 50 mL of 5-ASA, respectively, the drug reached between the sigmoid colon and the descending colon. The present results of rebamipide enema therapy are considered to be related to its effect of accelerating ulcer healing within the range of the colonic segments reached by the drug. As for the dosage of rebamipide, the dose was set at 150 mg in this study, although a dose finding study may be necessary in the future.
In conclusion, rebamipide enema therapy significantly shortened the fasting period and the duration of hospitalization in left-sided ischemic colitis patients with ulcerative lesions. Based on these findings, rebamipide enema therapy appears to be a promising new therapy in ischemic colitis patients with ulcerative lesions.
COMMENTS
Background
Authors have recently reported that the duration of fasting and hospitalization were significantly prolonged in ischemic colitis patients with ulcers.
Research frontiers
In this study, the authors attempted rectal administration of rebamipide for the treatment of ischemic colitis patients with ulcers, and evaluated its effects, including on the duration of fasting and hospitalization.
Applications
Rebamipide enema therapy shortened the fasting and hospitalization period in left-sided ischemic colitis patients with ulcerative lesions. We recommend rebamipide enema therapy in left-sided ischemic colitis patients with ulcerative lesions.
Peer review
This is a retrospective study involving a small number of patients with left-sided ischemic colitis with ulcer, collected over a period of 5-6 years, compared with rebamipide therapy. The study shows promising results. It’s an interesting paper.
Peer reviewer: Ahmed Helmy, PhD, Department of Liver Transplantation, King Faisal Specialist Hospital & Research Center, Dept. pf Liver transplantation, Hepatobiliary & Pancreatic Surgery, King Faisal Specialist Hospital & Research Center, MBC 72, Riyadh 3354, Saudi Arabia
S- Editor Li DL L- Editor Laber P E- Editor Ma WH
References
- 1.Boley SJ, Schwartz S, Lash J, Sternhill V. Reversible vascular occlusion of the colon. Surg Gynecol Obstet. 1963;116:53–60. [PubMed] [Google Scholar]
- 2.Marston A, Pheils MT, Thomas ML, Morson BC. Ischaemic colitis. Gut. 1966;7:1–15. doi: 10.1136/gut.7.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tohda G, Higashi S, Sumiyoshi K, Sakumoto H, Kato C, Kane T. Evaluation of clinical features of ischemic colitis:comparison between young and elderly. Dig Endosc. 2005;17:123–130. [Google Scholar]
- 4.Collet T, Even C, Bouin M, Lecluse E, Piquet MA, Crampon D, Grollier G, Dao T, Verwaerde JC. Prevalence of electrocardiographic and echocardiographic abnormalities in ambulatory ischemic colitis. Dig Dis Sci. 2000;45:23–25. doi: 10.1023/a:1005440822707. [DOI] [PubMed] [Google Scholar]
- 5.Hourmand-Ollivier I, Bouin M, Saloux E, Morello R, Rousselot P, Piquet MA, Dao T, Verwaerde JC. Cardiac sources of embolism should be routinely screened in ischemic colitis. Am J Gastroenterol. 2003;98:1573–1577. doi: 10.1111/j.1572-0241.2003.07483.x. [DOI] [PubMed] [Google Scholar]
- 6.Matsumoto T, Iida M, Kimura Y, Nanbu T, Fujishima M. Clinical features in young adult patients with ischaemic colitis. J Gastroenterol Hepatol. 1994;9:572–575. doi: 10.1111/j.1440-1746.1994.tb01563.x. [DOI] [PubMed] [Google Scholar]
- 7.Habu Y, Tahashi Y, Kiyota K, Matsumura K, Hirota M, Inokuchi H, Kawai K. Reevaluation of clinical features of ischemic colitis. Analysis of 68 consecutive cases diagnosed by early colonoscopy. Scand J Gastroenterol. 1996;31:881–886. doi: 10.3109/00365529609051996. [DOI] [PubMed] [Google Scholar]
- 8.Friedel D, Thomas R, Fisher RS. Ischemic colitis during treatment with alosetron. Gastroenterology. 2001;120:557–560. doi: 10.1053/gast.2001.21177. [DOI] [PubMed] [Google Scholar]
- 9.Miller DP, Alfredson T, Cook SF, Sands BE, Walker AM. Incidence of colonic ischemia, hospitalized complications of constipation, and bowel surgery in relation to use of alosetron hydrochloride. Am J Gastroenterol. 2003;98:1117–1122. doi: 10.1111/j.1572-0241.2003.07418.x. [DOI] [PubMed] [Google Scholar]
- 10.Welch M, Baguneid MS, McMahon RF, Dodd PD, Fulford PE, Griffiths GD, Walker MG. Histological study of colonic ischaemia after aortic surgery. Br J Surg. 1998;85:1095–1098. doi: 10.1046/j.1365-2168.1998.00791.x. [DOI] [PubMed] [Google Scholar]
- 11.Fanti L, Masci E, Mariani A, Chiesa R, Jannello A, Melissano G, Castellano R, Guerini S, Tittobello A. Is endoscopy useful for early diagnosis of ischaemic colitis after aortic surgery? Results of a prospective trial. Ital J Gastroenterol Hepatol. 1997;29:357–360. [PubMed] [Google Scholar]
- 12.Green BT, Tendler DA. Ischemic colitis: a clinical review. South Med J. 2005;98:217–222. doi: 10.1097/01.SMJ.0000145399.35851.10. [DOI] [PubMed] [Google Scholar]
- 13.Matsumoto S, Tsuji K, Shirahama S. Clinical investigation of 41 patients with ischemic colitis accompanied by ulcer. World J Gastroenterol. 2007;13:1236–1239. doi: 10.3748/wjg.v13.i8.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arakawa T, Higuchi K, Fujiwara Y, Watanabe T, Tominaga K, Sasaki E, Oshitani N, Yoshikawa T, Tarnawski AS. 15th anniversary of rebamipide: looking ahead to the new mechanisms and new applications. Dig Dis Sci. 2005;50 Suppl 1:S3–S11. doi: 10.1007/s10620-005-2800-9. [DOI] [PubMed] [Google Scholar]
- 15.Arakawa T, Kobayashi K, Yoshikawa T, Tarnawski A. Rebamipide: overview of its mechanisms of action and efficacy in mucosal protection and ulcer healing. Dig Dis Sci. 1998;43:5S–13S. [PubMed] [Google Scholar]
- 16.Ogino K, Hobara T, Ishiyama H, Yamasaki K, Kobayashi H, Izumi Y, Oka S. Antiulcer mechanism of action of rebamipide, a novel antiulcer compound, on diethyldithiocarbamate-induced antral gastric ulcers in rats. Eur J Pharmacol. 1992;212:9–13. doi: 10.1016/0014-2999(92)90065-c. [DOI] [PubMed] [Google Scholar]
- 17.Yoshikawa T, Naito Y, Tanigawa T, Kondo M. Free radical scavenging activity of the novel anti-ulcer agent rebamipide studied by electron spin resonance. Arzneimittelforschung. 1993;43:363–366. [PubMed] [Google Scholar]
- 18.Naito Y, Yoshikawa T, Tanigawa T, Sakurai K, Yamasaki K, Uchida M, Kondo M. Hydroxyl radical scavenging by rebamipide and related compounds: electron paramagnetic resonance study. Free Radic Biol Med. 1995;18:117–123. doi: 10.1016/0891-5849(94)00110-6. [DOI] [PubMed] [Google Scholar]
- 19.Sakurai K, Sasabe H, Koga T, Konishi T. Mechanism of hydroxyl radical scavenging by rebamipide: identification of mono-hydroxylated rebamipide as a major reaction product. Free Radic Res. 2004;38:487–494. doi: 10.1080/1071576042000209808. [DOI] [PubMed] [Google Scholar]
- 20.Okayama M, Tsubouchi R, Nishio H, Kato S, Takeuchi K. Protective effect of intra-rectal administration of rebamipide on dextran sulfate sodium-induced rat colitis. Digestion. 2004;70:240–249. doi: 10.1159/000083716. [DOI] [PubMed] [Google Scholar]
- 21.Ishihara K, Komuro Y, Nishiyama N, Yamasaki K, Hotta K. Effect of rebamipide on mucus secretion by endogenous prostaglandin-independent mechanism in rat gastric mucosa. Arzneimittelforschung. 1992;42:1462–1466. [PubMed] [Google Scholar]
- 22.Makiyama K, Takeshima F, Kawasaki H, Zea-Iriarte WL. Anti-inflammatory effect of rebamipide enema on proctitis type ulcerative colitis: a novel therapeutic alternative. Am J Gastroenterol. 2000;95:1838–1839. doi: 10.1111/j.1572-0241.2000.02154.x. [DOI] [PubMed] [Google Scholar]
- 23.Makiyama K, Takeshima F, Hamamoto T. Efficacy of rebamipide enemas in active distal ulcerative colitis and proctitis: a prospective study report. Dig Dis Sci. 2005;50:2323–2329. doi: 10.1007/s10620-005-3055-1. [DOI] [PubMed] [Google Scholar]
- 24.Furuta R, Ando T, Watanabe O, Maeda O, Ishiguro K, Ina K, Kusugami K, Goto H. Rebamipide enema therapy as a treatment for patients with active distal ulcerative colitis. J Gastroenterol Hepatol. 2007;22:261–267. doi: 10.1111/j.1440-1746.2006.04399.x. [DOI] [PubMed] [Google Scholar]
- 25.Miyata M, Konagaya T, Kakumu S, Mori T. Successful treatment of severe pouchitis with rebamipide refractory to antibiotics and corticosteroids: a case report. World J Gastroenterol. 2006;12:656–658. doi: 10.3748/wjg.v12.i4.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kaneko E, Hoshihara Y, Sakaki N, Harasawa S, Ashida K, Asaka M, Asaki S, Nakamura T, Kobayashi K, Kajiyama G, et al. Peptic ulcer recurrence during maintenance therapy with H2-receptor antagonist following first-line therapy with proton pump inhibitor. J Gastroenterol. 2000;35:824–831. doi: 10.1007/s005350070019. [DOI] [PubMed] [Google Scholar]
- 27.Kleine A, Kluge S, Peskar BM. Stimulation of prostaglandin biosynthesis mediates gastroprotective effect of rebamipide in rats. Dig Dis Sci. 1993;38:1441–1449. doi: 10.1007/BF01308601. [DOI] [PubMed] [Google Scholar]
- 28.Sun WH, Tsuji S, Tsujii M, Gunawan ES, Kawai N, Kimura A, Kakiuchi Y, Yasumaru M, Iijima H, Okuda Y, et al. Induction of cyclooxygenase-2 in rat gastric mucosa by rebamipide, a mucoprotective agent. J Pharmacol Exp Ther. 2000;295:447–452. [PubMed] [Google Scholar]
- 29.Murata H, Yabe Y, Tsuji S, Tsujii M, Fu HY, Asahi K, Eguchi H, Kawano S, Hayashi N. Gastro-protective agent rebamipide induces cyclooxygenease-2 (COX-2) in gastric epithelial cells. Dig Dis Sci. 2005;50 Suppl 1:S70–S75. doi: 10.1007/s10620-005-2809-0. [DOI] [PubMed] [Google Scholar]
- 30.Farhadi A, Keshavarzian A, Fitzpatrick LR, Mutlu E, Zhang Y, Banan A. Modulatory effects of plasma and colonic milieu of patients with ulcerative colitis on neutrophil reactive oxygen species production in presence of a novel antioxidant, rebamipide. Dig Dis Sci. 2002;47:1342–1348. doi: 10.1023/a:1015382800434. [DOI] [PubMed] [Google Scholar]
- 31.Niwa Y, Nakamura M, Omiya N, Itoh A, Hirooka Y, Goto H. Ileal cancer and erosions in the small intestine revealed by capsule endoscopy. Endoscopy. 2007;39 Suppl 1:E7–E8. doi: 10.1055/s-2006-944792. [DOI] [PubMed] [Google Scholar]
- 32.Ichihara T, Nagahata Y, Urakawa T, Saitoh Y. [Experimental study on the etiology of ischemic colitis] Nippon Geka Gakkai Zasshi. 1994;95:7–13. [PubMed] [Google Scholar]
- 33.Sakurai K, Yamasaki K. Protective effect of rebamipide against hydrogen peroxide-induced hemorrhagic mucosal lesions in rat stomach. Jpn J Pharmacol. 1994;64:229–234. doi: 10.1254/jjp.64.229. [DOI] [PubMed] [Google Scholar]
- 34.van Bodegraven AA, Boer RO, Lourens J, Tuynman HA, Sindram JW. Distribution of mesalazine enemas in active and quiescent ulcerative colitis. Aliment Pharmacol Ther. 1996;10:327–332. doi: 10.1111/j.0953-0673.1996.00327.x. [DOI] [PubMed] [Google Scholar]
- 35.Otten MH, De Haas G, Van den Ende R. Colonic spread of 5-ASA enemas in healthy individuals, with a comparison of their physical and chemical characteristics. Aliment Pharmacol Ther. 1997;11:693–697. doi: 10.1046/j.1365-2036.1997.00199.x. [DOI] [PubMed] [Google Scholar]


