Abstract
Wireless capsule endoscope (WCE) for the investigation of the small bowel is an approved technique both in adults and children (more than 10 years old). The present review provides data on the indications, diagnostic yield, adverse events and limitations of the WCE technique in children and tries to predict the future of WCE usage in this population of patients.
Keywords: Capsule, Wireless, Pediatric, Children
INTRODUCTION
The concept of a wireless capsule endoscope (WCE) for the investigation of the small bowel, was introduced in 2000[1], soon to be followed by a commercially available product both in Europe and the USA[2].
Soon after its first reports in adult patients, the advantages of this imaging technique turned WCE into an experimental and later an approved technique in the diagnostic arsenal of pediatric gastroenterology (from the age of 10 years old) worldwide.
The present review will provide data on the indications, diagnostic yield, adverse events and limitations of PillCam SB technique in children and try to predict the future of WCE. An electronic search of MEDLINE was done (up to May 15, 2007), limiting full citations to papers published in English while reviewing abstracts in any language.
PEDIATRIC PATIENTS AND WCE
Age range
In 2001, the Food and Drug Administration approved WCE, then referred to as M2A, and now PillCam SB (Given Imaging, Yoqneam, Israel) as an adjunct tool for the evaluation of small-intestinal disorders and later (2003) as a first line modality for the evaluation of small-intestinal disorders. In 2004, WCE was approved as a diagnostic tool for children not younger than 10 years of age. As will be discussed later, the main limitation in children is the need to swallow this 27 mm × 11 mm relatively large pill. Using any of the traditional endoscopy assisted methods of ingestion, successful WCE examinations were reported in children as young as 2.5 years and 3 years of age[3,4]. Interestingly, in a recent report from China, 6 out of 16 pediatric studies (37%), were done in children younger the 10 years[5].
Clinical indications
The literature on the use of WCE in children is limited. In adults, the main indications include obscure gastrointestinal bleeding (OGIB), iron deficiency anemia, suspected Crohn’s disease, small intestinal tumors and refractory celiac disease. Nevertheless, any small bowel disease/pathology manifested beyond the reach of the endoscope might be an indication for WCE. Similarly, in children, the main indications include OGIB and suspected Crohn’s disease, though many other indications for the use of WCE were described and are summarized in Table 1. In this review we evaluated the available literature on the use of WCE in children on theses two main topics (suspected intestinal inflammation and OGIB) and mention some others.
Table 1.
Pediatric indications for the use of WCE
| Pediatric indications for the use of WCE |
| Intestinal inflammation |
| Crohn's disease |
| Celiac disease |
| Occult or obscure intestinal bleeding |
| Vascular malformations |
| Vasculitis (Henoch-Schönlein Purpura) |
| Meckel's diverticulum |
| Protein-losing enteropathies |
| Intestinal lymphangiectasia |
| Miscellaneous |
| Peutz-Jeghers syndrome |
| Familial and nonfamilial polyposis |
| Eosinophilic enteropathy |
| Food allergy |
| Mucosal injury |
| Drugs |
| Chemotherapy |
| Radiotherapy |
| Graft versus host disease |
| Malignancy |
| Chronic abdominal pain |
Intestinal inflammation Crohn’s disease
There are 5 studies in the pediatric literature looking at suspected Crohn’s disease. A prospective pediatric study evaluating small bowel pathologies[6] found that, among 10 out of 20 patients, multiple lesions consistent with Crohn’s disease were found using PillCam SB. Not less important, small-bowel Crohn’s disease was ruled out in 8 patients. In another study[7], WCE was used in 12 patients with suspected Crohn’s disease not diagnosed by gastroscopy, colonoscopy, and small-bowel follow-through examinations that were carried out in all of the patients. Here too, WCE identified lesions suggestive of Crohn’s disease in seven of the 12 (58.3%), the majority of the lesions being in the ileum. In a prospective cohort of children[8], 16 patients with suspected small bowel Crohn’s disease (10 newly diagnosed; 6 known cases), underwent WCE which was compared with standard investigation. All of the patients had preceding upper gastrointestinal endoscopy and ileocolonoscopy, and the majority had a barium meal and follow-through. In all patients with CD who had successful WCE studies (12/16), small bowel disease was identified (11/12 active disease, 1/12 chronic disease) by PillCam SB. In this study, ileocolonoscopy and WCE complemented each other with respect to the extent of the disease. In a retrospective review of 46 WCE studies in children[9] (a denominator was not provided), among 9 children with newly diagnosed small intestinal Crohn’s disease, seven (78%) had their treatment changed after WCE was done. Finally, PillCam SB was able to suggest the diagnosis of Crohn’s disease in 2 adolescents with abdominal pain, protein loosing enteropathy and anemia with negative radiologic and endoscopic evaluation[10].
In accordance with adult studies and some of the studies cited, the North American Society for Gastroenterology Hepatology and Nutrition[11] concluded that WCE is increasingly being used in the detection of obscure small bowel lesions and now has a proven role in the identification of Crohn’s disease of the small intestine. It was concluded that the sensitivity of WCE at identifying small bowel ulceration or stricture appears to be superior to conventional barium radiography and enteroclysis, but this conclusion was made based on adult literature[12,13].
From adult studies, it is clear that WCE may have other important roles such as the assessment of mucosal healing of the small intestine, defining the extent of disease and providing evidence for distinction between Crohn’s and UC in patients with indeterminate colitis[2].
Celiac disease
Endoscopy with intestinal mucosa biopsies is still considered the gold standard in diagnosing celiac disease. However, in adults, there is mounting evidence that WCE may be useful in the evaluation of patients with already diagnosed celiac disease[14]. In a recent study, in adults, evaluating the role of WCE in the diagnosis of celiac disease, findings regarding the degree of intestinal mucosal atrophy showed only moderate agreement with the histologic pattern[15]. The authors concluded that WCE cannot be an alternative to biopsy, but a duodenal biopsy should be done when an atrophic mucosal pattern is observed in patients undergoing WCE for other reasons. In adults, a consensus expert panel suggested that WC endoscopists should be able to recognize celiac disease, and for the time being, WCE might be an option in patients unable or unwilling to undergo conventional upper GI endoscopy[16]. Data in children are lacking to evaluate and apply these statements in children.
Obscure gastrointestinal bleeding and other sources of bleeding
WCE is the imaging method of choice in adults with OGIB[17]. In a cohort of patients from Canada, among four patients with obscure bleeding, WCE confirmed a diagnosis of vascular malformations in three. In that study, WCE was more accurate identifying the precise source of bleeding compared with angiography[6]. In another study from England[8] a possible source of bleeding was identified in all 6 patients suffering from chronic anemia and OGIB. In that study, WCE had a higher diagnostic yield compared to a combination of gastroduodenoscopy and ileocolonoscopy.
WCE was reported to be helpful in evaluating and directing treatment options in chronic Henoch-Schonlein Purpura vasculitis[18]. Similarly, it has been found helpful in monitoring the effect of therapy in patients with blue rubber bleb nevus syndrome[19]. Other miscellaneous diagnoses of PillCam SB are bleeding varices, angiodysplastic lesions, jejunal hemangioma, Meckel’s diverticulum and bleeding lymphonodular hyperplasia[20–23].
Miscellaneous
As reviewed recently[20], WCE is used to diagnose and survey small bowel polyps in children with familial polyposis and those with Peutz-Jeghers syndrome. It may also be used to diagnose malignancies[24], intestinal lymphangiectasia[25], as well increasing number of entities summarized in Table 1. It is clear that with time, many of these entities will become more established indications for performing WCE. Future studies should delineate the role of WCE compared to other imaging modalities for some of these entities.
Advantages and limitations
WCE is clearly advantageous for evaluating small bowel pathologies when the child is able to swallow the capsule as it is a procedure that is free of anesthesia and its risks. Often, we are able to select those patients who will readily swallow the capsule (using candies of increasing sizes) and train some who were afraid to swallow big candies[26]. When the patient can not swallow the capsule due to any reason (including swallowing disorders, dysphagia, gastroparesis) the capsule can be safely introduced to the duodenum using various techniques and a standard endoscope (Figure 1)[20,27].
Figure 1.
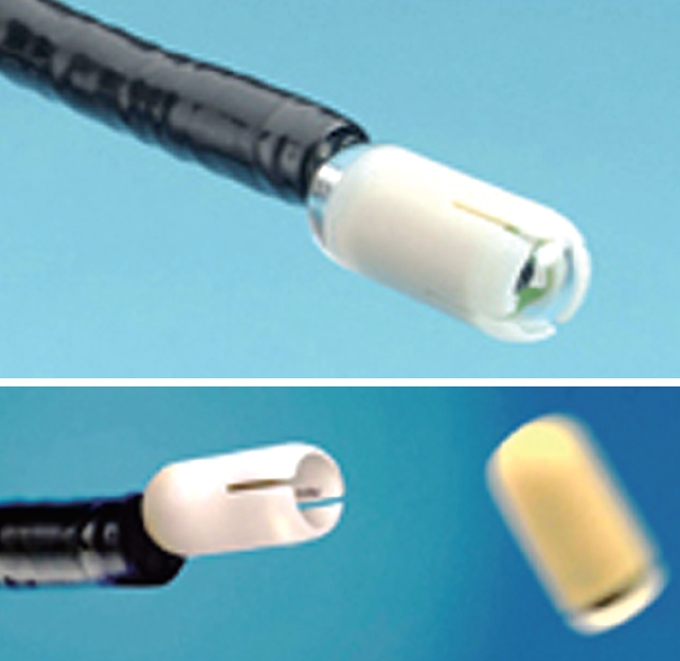
An introducing device for the capsule endoscope.
The main adverse event when using the capsule is capsule retention mainly due to strictures. Studies in adults have demonstrated the usefulness of using a Patency capsule (see accompanying article) and predicting the uneventful passage of the capsule using a Patency capsule has also been reported in children[6,20]. In adults, capsule retention was reported in 13% (95% CI, 5.6%-28%) of patients with known CD, but only in 1.6% (95% CI, 0.2%-10%) with suspected Crohn’s disease[28]. Capsule retention occurred in children, but not in adults with suspected Crohn’s disease. In a cohort of 45 children undergoing WCE, nine subjects (20%) had adverse events[9]. Of these patients, five had delayed passage from the stomach with 2 patients requiring endoscopic retrieval and 4 had delayed passage from the small intestine (more than 5 d). Three of the 4 patients with intestinal retention underwent surgery (one underwent ileocolic resection 2 mo later) and one responded to steroids. In the study from Canada[6], all 30 capsule studies were well tolerated, although 1 capsule was retained owing to an inflammatory stenosis. The capsule was eventually expelled after corticosteroid therapy. No capsule retention occurred in a Chinese series of 16 patients[5]. Figure 2 shows a device used to introduce the capsule endoscope to the stomach.
Figure 2.

A device used to introduce the capsule endoscope into the stomach.
CONCLUSION
The North American Society for Gastroenterology Hepatology and Nutrition recently stated that regarding WCE in Crohn’s disease, “Drawbacks of WCE include the cost of the test, as well as the potential risk of capsule impaction in strictured areas of the small bowel. Future studies may determine whether capsule endoscopy should be performed as a routine examination on new-onset patients with colitis and normal contrast studies. At this time, we recommend that this test be used primarily when CD of the small bowel is strongly suspected but cannot be documented by other modalities”[11].
Thus, in summary, WCE is a promising diagnostic tool for small bowel imaging both in adults and children. A smaller capsule may allow younger children to use it with out the need of traditional endoscopy.
Peer reviewer: Roberto de Franchis, Professor, Department of Medical Sciences, University of Milano, Via Pace 9, Milano 20122, Italy
S- Editor Zhong XY L- Editor Negro F E- Editor Ma WH
References
- 1.Iddan G, Meron G, Glukhovsky A, Swain P. Wireless capsule endoscopy. Nature. 2000;405:417. doi: 10.1038/35013140. [DOI] [PubMed] [Google Scholar]
- 2.Cave DR. Technology Insight: current status of video capsule endoscopy. Nat Clin Pract Gastroenterol Hepatol. 2006;3:158–164. doi: 10.1038/ncpgasthep0416. [DOI] [PubMed] [Google Scholar]
- 3.Kavin H, Berman J, Martin TL, Feldman A, Forsey-Koukol K. Successful wireless capsule endoscopy for a 2.5-year-old child: obscure gastrointestinal bleeding from mixed, juvenile, capillary hemangioma-angiomatosis of the jejunum. Pediatrics. 2006;117:539–543. doi: 10.1542/peds.2005-0710. [DOI] [PubMed] [Google Scholar]
- 4.Aabakken L, Scholz T, Ostensen AB, Emblem R, Jermstad T. Capsule endoscopy is feasible in small children. Endoscopy. 2003;35:798. doi: 10.1055/s-2003-41595. [DOI] [PubMed] [Google Scholar]
- 5.Ge ZZ, Chen HY, Gao YJ, Gu JL, Hu YB, Xiao SD. Clinical application of wireless capsule endoscopy in pediatric patients for suspected small bowel diseases. Eur J Pediatr. 2007;166:825–829. doi: 10.1007/s00431-006-0331-9. [DOI] [PubMed] [Google Scholar]
- 6.Guilhon de Araujo Sant’Anna AM, Dubois J, Miron MC, Seidman EG. Wireless capsule endoscopy for obscure small-bowel disorders: final results of the first pediatric controlled trial. Clin Gastroenterol Hepatol. 2005;3:264–270. doi: 10.1016/s1542-3565(04)00715-3. [DOI] [PubMed] [Google Scholar]
- 7.Arguelles-Arias F, Caunedo A, Romero J, Sanchez A, Rodriguez-Tellez M, Pellicer FJ, Arguelles-Martin F, Herrerias JM. The value of capsule endoscopy in pediatric patients with a suspicion of Crohn's disease. Endoscopy. 2004;36:869–873. doi: 10.1055/s-2004-825854. [DOI] [PubMed] [Google Scholar]
- 8.Thomson M, Fritscher-Ravens A, Mylonaki M, Swain P, Eltumi M, Heuschkel R, Murch S, McAlindon M, Furman M. Wireless capsule endoscopy in children: a study to assess diagnostic yield in small bowel disease in paediatric patients. J Pediatr Gastroenterol Nutr. 2007;44:192–197. doi: 10.1097/01.mpg.0000252196.91707.ff. [DOI] [PubMed] [Google Scholar]
- 9.Moy L, Levine J. Wireless capsule endoscopy in the pediatric age group: experience and complications. J Pediatr Gastroenterol Nutr. 2007;44:516–520. doi: 10.1097/MPG.0b013e3180335548. [DOI] [PubMed] [Google Scholar]
- 10.Barkay O, Moshkowitz M, Reif S. Crohn’s disease diagnosed by wireless capsule endoscopy in adolescents with abdominal pain, protein-losing enteropathy, anemia and negative endoscopic and radiologic findings. Isr Med Assoc J. 2005;7:216–218. [PubMed] [Google Scholar]
- 11.Bousvaros A, Antonioli DA, Colletti RB, Dubinsky MC, Glickman JN, Gold BD, Griffiths AM, Jevon GP, Higuchi LM, Hyams JS, et al. Differentiating ulcerative colitis from Crohn disease in children and young adults: report of a working group of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition and the Crohn’s and Colitis Foundation of America. J Pediatr Gastroenterol Nutr. 2007;44:653–674. doi: 10.1097/MPG.0b013e31805563f3. [DOI] [PubMed] [Google Scholar]
- 12.Eliakim R, Fischer D, Suissa A, Yassin K, Katz D, Guttman N, Migdal M. Wireless capsule video endoscopy is a superior diagnostic tool in comparison to barium follow-through and computerized tomography in patients with suspected Crohn’s disease. Eur J Gastroenterol Hepatol. 2003;15:363–367. doi: 10.1097/00042737-200304000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Marmo R, Rotondano G, Piscopo R, Bianco MA, Siani A, Catalano O, Cipolletta L. Capsule endoscopy versus enteroclysis in the detection of small-bowel involvement in Crohn’s disease: a prospective trial. Clin Gastroenterol Hepatol. 2005;3:772–776. doi: 10.1016/s1542-3565(05)00483-0. [DOI] [PubMed] [Google Scholar]
- 14.Rondonotti E, de Franchis R. Diagnosing coeliac disease: is the videocapsule a suitable tool? Dig Liver Dis. 2007;39:145–147. doi: 10.1016/j.dld.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 15.Biagi F, Rondonotti E, Campanella J, Villa F, Bianchi PI, Klersy C, De Franchis R, Corazza GR. Video capsule endoscopy and histology for small-bowel mucosa evaluation: a comparison performed by blinded observers. Clin Gastroenterol Hepatol. 2006;4:998–1003. doi: 10.1016/j.cgh.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 16.Cellier C, Green PH, Collin P, Murray J. ICCE consensus for celiac disease. Endoscopy. 2005;37:1055–1059. doi: 10.1055/s-2005-870310. [DOI] [PubMed] [Google Scholar]
- 17.Mazzarolo S, Brady P. Small bowel capsule endoscopy: a systematic review. South Med J. 2007;100:274–280. doi: 10.1097/SMJ.0b013e31802fa05a. [DOI] [PubMed] [Google Scholar]
- 18.Preud’Homme DL, Michail S, Hodges C, Milliken T, Mezoff AG. Use of wireless capsule endoscopy in the management of severe Henoch-Schonlein purpura. Pediatrics. 2006;118:e904–e906. doi: 10.1542/peds.2005-3111. [DOI] [PubMed] [Google Scholar]
- 19.De Bona M, Bellumat A, De Boni M. Capsule endoscopy for the diagnosis and follow-up of blue rubber bleb nevus syndrome. Dig Liver Dis. 2005;37:451–453. doi: 10.1016/j.dld.2004.12.014. [DOI] [PubMed] [Google Scholar]
- 20.Seidman EG, Dirks MH. Capsule Endoscopy in the Pediatric Patient. Curr Treat Options Gastroenterol. 2006;9:416–422. doi: 10.1007/BF02738531. [DOI] [PubMed] [Google Scholar]
- 21.Kovacs M, Davidovics S, Gyurus P, Racz I. [Identification of a Meckel's diverticulum bleeding by urgent capsule endoscopy] Orv Hetil. 2006;147:2003–2006. [PubMed] [Google Scholar]
- 22.Tabbers MM, Bruin KF, Benninga MA, Vieira-Travassos D, Oudshoorn JH. Capsule endoscopy in a child with a jejunal hemangioma. Endoscopy. 2006;38 Suppl 2:E46. doi: 10.1055/s-2006-944679. [DOI] [PubMed] [Google Scholar]
- 23.Wu JF, Liou JH, Lien HC, Hsu WM, Fang YJ, Chang MH, Ni YH. Bleeding from ileal nodular lymphoid polyposis identified by capsule endoscopy. J Pediatr Gastroenterol Nutr. 2004;39:295–298. doi: 10.1097/00005176-200409000-00014. [DOI] [PubMed] [Google Scholar]
- 24.Chiarugi M, Galatioto C, Lippolis P, Zocco G, Seccia M. Gastrointestinal stromal tumour of the duodenum in childhood: a rare case report. BMC Cancer. 2007;7:79. doi: 10.1186/1471-2407-7-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rao R, Shashidhar H. Intestinal lymphangiectasia presenting as abdominal mass. Gastrointest Endosc. 2007;65:522–523, discussion 523. doi: 10.1016/j.gie.2006.10.026. [DOI] [PubMed] [Google Scholar]
- 26.Shamir R, Hino B, Hartman C, Berkowitz D, Eshach-Adiv O, Eliakim R. Wireless video capsule in pediatric patients with functional abdominal pain. J Pediatr Gastroenterol Nutr. 2007;44:45–50. doi: 10.1097/01.mpg.0000239737.64240.72. [DOI] [PubMed] [Google Scholar]
- 27.Barth BA, Donovan K, Fox VL. Endoscopic placement of the capsule endoscope in children. Gastrointest Endosc. 2004;60:818–821. doi: 10.1016/s0016-5107(04)02052-8. [DOI] [PubMed] [Google Scholar]
- 28.Cheifetz AS, Kornbluth AA, Legnani P, Schmelkin I, Brown A, Lichtiger S, Lewis BS. The risk of retention of the capsule endoscope in patients with known or suspected Crohn’s disease. Am J Gastroenterol. 2006;101:2218–2222. doi: 10.1111/j.1572-0241.2006.00761.x. [DOI] [PubMed] [Google Scholar]


