Abstract
AIM: To evaluate the effect of an intravenous bolus of mannitol in altering brain metabolites, brain water content, brain parenchyma volume, cerebrospinal fluid (CSF) volume and clinical signs in controls and in patients with acute liver failure (ALF) and acute-on-chronic liver failure (ACLF), by comparing changes in conventional magnetic resonance imaging (MRI), in vivo proton magnetic resonance spectroscopy (PMRS) and diffusion tensor imaging (DTI) before and after its infusion.
METHODS: Five patients each with ALF and ACLF in grade 3 or 4 hepatic encephalopathy and with clinical signs of raised intracranial pressure were studied along with five healthy volunteers. After baseline MRI, an intravenous bolus of 20% mannitol solution was given over 10 min in controls as well as in patients with ALF and ACLF. Repeat MRI for the same position was acquired 30 min after completing the mannitol injection.
RESULTS: No statistically significant difference was observed between controls and patients with ALF and ACLF in metabolite ratios, DTI metrics and brain volume or CSF volume following 45 min of mannitol infusion. There was no change in clinical status at the end of post-mannitol imaging.
CONCLUSION: The osmotic effect of mannitol did not result in significant reduction of brain water content, alteration in metabolite ratios or any change in the clinical status of these patients during or within 45 min of mannitol infusion.
Keywords: Mannitol, Acute liver failure, Acute-on-chronic liver failure, Proton MR spectroscopy, Diffusion tensor imaging
INTRODUCTION
Liver failure is a life-threatening condition following severe hepatocellular injury that affects many other organ systems, most notably the brain and kidneys[1]. Liver failure may develop in the absence of pre-existing liver disease i.e. acute liver failure (ALF) or when an acute insult is superimposed on a chronic liver disorder [acute-on-chronic liver failure (ACLF)[2,3]. Cerebral edema leading to raised intracranial pressure (ICP) is known to be a major complication in patients with ALF[4]. The pathophysiological mechanisms underlying development of cerebral edema and ICP in ALF are multifactorial[5,6]. Though the occurrence and nature of cerebral edema in ACLF is not well studied, anecdotal evidence from patients with ACLF suggests that hyponatremia is implicit in the progression to cerebral edema[7].
Presently, osmotic therapy is widely used to control cerebral edema and raised ICP. Mannitol is the most frequently used osmotically active agent in clinical practice[8]. It acts by increasing blood osmolarity, thereby establishing a concentration gradient across the intact blood-brain barrier (BBB) that forces movement of water from the edematous brain tissue to the intravascular space[9]. In controlled trials, mannitol has been shown to decrease the raised ICP level in ALF patients and is associated with improved survival[10]. Other experimental studies have suggested that mannitol infusion reduces the water content and volume of normal, but not of infarcted brain tissue[11,12].
Noninvasive imaging techniques such as magnetic resonance imaging (MRI) and computed tomography (CT) have been used to evaluate the brain water content changes after mannitol administration. Increased brain density of both edematous peritumoral white matter as well as normal gray and white matter on CT scans has been attributed to mannitol induced reduction in brain water content in patients with cerebral tumors[13]. Similarly, MR scans in patients with cerebral tumors detect reduced longitudinal relaxation time (T1) in edematous peritumoral white matter after mannitol infusion, which correlates with decrease in water content[14].
Newer MR imaging techniques such as proton magnetic resonance spectroscopy (PMRS) and diffusion tensor imaging (DTI) are considered to be more sensitive and accurate in assessing the changes in brain metabolites and brain water content within the intracellular and extracellular compartments[15]. Changes in brain osmolytes detected by the PMRS are indirect or proxy evidence for cerebral edema. PMRS changes (i.e. reduction of choline, myoinositol and N-acetyl aspartate peaks and increase in Gln-Glx peak) are well-known in liver cirrhosis and chronic liver failure, conditions where there is sufficient time for organic osmolytes to compensate for increased intracellular osmolarity caused by astrocytic accumulation of glutamine[16]. PMRS changes in ALF are not well documented and are unlikely to be so clear-cut since rapid onset of the syndrome does not allow sufficient time for compensatory mechanisms to counterbalance rapid changes in osmolarity due to rapid and massive accumulation of astrocytic glutamine in this condition[17]. In patients with hyponatremia, PMRS has revealed significantly lower levels of the organic osmolyte myoinositol which would normally compensate for the rising intracellular glutamine seen with acute liver injury[18].
DTI is a technique that is able to reveal and quantify the direction of water mobility in tissues, which in white matter is normally anisotropic because of axonal fibers running in parallel. The two commonly used DTI metrics are fractional anisotropy (FA) and mean diffusivity (MD). FA reflects the degree of anisotropy due to the hindrance of water molecules mobility caused by various physical barriers. MD is a measure of tissue water diffusivity and is dependent upon interactions between water molecules and the structural components at cellular and subcellular level[19]..
To the best of our knowledge, this is the first study evaluating the effect of mannitol on brain water content using DTI and PMRS in controls as well as in patients with ALF and ACLF. We hypothesize that the effect of bolus infusion of mannitol in reducing brain water content will be reflected by changes measured by conventional MRI, in-vivo PMRS and DTI. Since the peak effect of a single bolus in mobilizing fluid from tissues to the intravascular compartment according to the osmotic gradient is observed at about 45 min after infusion[14], it was decided to evaluate the effect of intravenous bolus of mannitol during the baseline MRI scan (pre-mannitol study) and after the completion of mannitol administration (post-mannitol study). The parameters compared between controls and patients, before and after mannitol infusion were (1) relative metabolite alterations in the right parietal region using in-vivo PMRS, (2) brain water content using DTI metrics, and (3) changes in the brain parenchyma volume as well as cerebrospinal fluid (CSF) volume. Changes were further correlated with the clinical outcome.
MATERIALS AND METHODS
Patients
In this study, we have included 5 ALF patients (3 males, 2 females; range, 14-46 years), and 5 ACLF patients (4 males, 1 female; range, 24-48 years). The patients with diagnosis of ALF and ACLF were admitted to the Gastroenterology intensive care ward and those who were clinically stable underwent imaging protocol. ALF was diagnosed in the presence of jaundice and encephalopathy with jaundice-to-encephalopathy interval being < 4 wk, and in the absence of clinical and radiological evidence of cirrhosis[20]. ACLF was diagnosed when there was acute hepatitis defined by abrupt (<4 wk) rise in serum bilirubin to ≥ 10 mg/dL and ALT to ≥ 5 times of normal (≥ 200 IU/L) on a patient with clinical, biochemical or ultrasonographic evidence of chronic liver disease (ascites, nodular and irregular liver, patent portal vein and portosystemic collaterals). Upper gastrointestinal endoscopy was done in the patients who recovered from encephalopathy to look for portal hypertension (esophageal varices ≥ grade II) as evidence of chronic liver disease. The etiology, baseline clinical profile and biochemical profile of ALF has been shown in Tables 1 and 2, respectively. All the patients had acute viral hepatitis; none of them had drug induced hepatitis. The etiology of acute and chronic liver disease, baseline clinical profile and biochemical profile in ACLF patients has been shown in Tables 3 and 4, respectively. None of these patients had history of prior neurological illness. Patients with history of significant alcohol intake over the previous six months were excluded since de-compensation could have been related to recent alcohol intake. Patients with ultrasonographic evidence of a mass lesion in the liver (hepatocellular carcinoma), portal vein thrombosis or biliary obstruction, or suspected sepsis at presentation were excluded, since the liver decompensation could have been related to these factors. Serum specimens were obtained from the study subjects and stored at -70°C until analysis. Etiological tests for cause of both acute hepatitis and chronic liver disease were done in patients with ALF and ACLF. These included IgM anti-hepatitis E virus, IgM anti-Hepatitis A virus (HAV), HBsAg, IgM anti-HAV, anti-HCV, antinuclear antibodies, anti smooth muscle antibodies, anti LKM, anti-mitochondrial antibodies, serum feritin, and Wilson’s disease work-up.
Table 1.
Clinical profile of acute liver failure patients
| Case | Age/Sex | Etiology | Grade of HE | Jaundice-HE interval (d) | HE duration at presentation (d) |
Clinical features of raised ICP |
||||
| DP | HT | B | PC | NH | ||||||
| 1 | 24/M | Hepatitis E | 4 | 7 | 2 | + | + | - | - | + |
| 2 | 14/M | Hepatitis B | 4 | 8 | 2 | + | + | - | + | + |
| 3 | 24/F | Hepatitis B | 4 | 23 | 2 | + | + | + | + | + |
| 4 | 46/F | Hepatitis E | 4 | 2 | 2 | + | + | + | + | + |
| 5 | 25/F | Hepatitis E | 3 | 2 | 1 | + | + | - | - | - |
HE: Hepatic encephalopathy; DP: Decerebrate posture; HT: Hypertension; B: Bradycardia; PC: Pupillary changes; NH: Neurogenic hyperventilation.
Table 2.
Biochemical profile of acute liver failure patients
| Case | Serum bilirubin (mg/dL) | ALT (U/L) | AST (U/L) | ALP (U/L) | INR | Serum sodium (mmol/L) | Serum potassium (mmol/L) | Serum creatinine (mg/dL) | Blood sugar (mg/dL, range) | Blood ammonia (μmol/dL) |
| 1 | 13.3 | 242 | 349 | 134 | 1.8 | 142 | 3.8 | 1.2 | 110-186 | |
| 2 | 26.4 | 1020 | 920 | 120 | 8.2 | 146 | 4.7 | 1.2 | 130-194 | 438 |
| 3 | 28.6 | 206 | 156 | 140 | 6.8 | 140 | 4.9 | 0.6 | 98-178 | 150 |
| 4 | 15.3 | 1688 | 276 | 210 | 5.5 | 145 | 4.3 | 0.6 | 130-188 | 265 |
| 5 | 21.5 | 232 | 142 | 146 | 2.8 | 143 | 3.6 | 0.4 | 88-176 | 182 |
ALT: Alanine transaminase; AST: Aspartate transaminase; ALP: Alkaline phosphatase; INR: International normalized ratio.
Table 3.
Clinical profile of acute-on-chronic liver failure patients
| Case | Age/Sex |
Etiology |
Grade of HE | Jaundice-HE interval (d) | HE duration at presentation (d) |
Clinical features of raised ICP |
|||||
| Acute | Chronic | DP | HT | B | PC | NH | |||||
| 1 | 48/M | Hepatitis E | Cryptogenic | 3 | 17 | 2 | + | + | - | - | + |
| 2 | 48/M | Hepatitis E | Chronic Hepatitis B | 4 | 15 | 3 | + | + | - | + | + |
| 3 | 24/F | Hepatitis E | Autoimmune | 3 | 22 | 1 | + | - | - | - | + |
| 4 | 45/F | Hepatitis E | Chronic Hepatitis C | 3 | 13 | 2 | + | + | - | + | + |
| 5 | 28/F | Hepatitis E | Chronic Hepatitis B | 3 | 7 | 2 | + | + | - | - | + |
HE: Hepatic encephalopathy; DP: Decerebrate posture; HT: Hypertension; B: Bradycardia; PC: Pupillary changes; NH: Neurogenic hyperventilation.
Table 4.
Biochemical profile of acute-on-chronic liver failure patients
| Case | Serum bilirubin (mg/dL) | ALT (U/L) | AST (U/L) | SAP (U/L) | INR | Serum sodium (mmol/L) | Serum potassium (mmol/L) | Serum creatinine (mg/dL) | Blood sugar (mg/dL, range) | Blood ammonia (μmole/dL) | Child score | MELD score |
| 1 | 18.8 | 346 | 274 | 148 | 2.6 | 143 | 3.7 | 1.2 | 130-194 | 180 | 12/15 | 30 |
| 2 | 17.2 | 254 | 142 | 165 | 2.4 | 144 | 4.9 | 0.9 | 98-210 | 280 | 13/15 | 29 |
| 3 | 25.7 | 636 | 524 | 164 | 3.7 | 136 | 4.5 | 0.5 | 98-166 | 261 | 13/15 | 33 |
| 4 | 25.1 | 240 | 320 | 97 | 3.9 | 145 | 3.9 | 0.9 | 108-210 | 310 | 14/15 | 34 |
| 5 | 10.2 | 279 | 151 | 79 | 2.25 | 137 | 4.3 | 0.8 | 89-189 | 210 | 13/15 | 24 |
ALT: Alanine transaminase; AST: Aspartate transaminase; SAP: Serum alkaline phosphatase; INR: International normalized ratio; MELD: Modified end stage liver disease.
Healthy controls
Five healthy controls (3 males, 2 females; range, 18-50 years) were also included in this study, who had no history of neurological or psychiatric illness, alcohol or drug abuse, and head injury or liver disease.
Management
Close monitoring and meticulous optimization of all metabolic derangements identified were done in all patients. Oxygenation was continuously monitored in each patient using pulse oximetry. Blood glucose level was monitored 6-hourly using a glucometer. Vital parameters, neurologic status and signs of raised ICP were checked 4-hourly. Raised ICP was diagnosed in presence of decerebrate posturing alone or, when two out of four of the following criteria were met, i.e. hypertension (supine blood pressure > 150/90 mmHg), bradycardia (pulse rate < 10/min for the expected pulse rate for the given body temperature), pupillary changes and neurogenic hyperventilation (hyperventilation in absence of metabolic or respiratory cause)[21]. ICP recordings were not done in any of these patients. However, the diagnosis of raised ICP was based on the clinical signs, imaging features of cytotoxic and interstitial edema on DTI. Sedation or muscle paralyzing agents were not used. We did not treat seizures prophylactically nor looked for subclinical seizures as prophylactic therapy for seizures as well as monitoring by EEG is not recommended in the management of ALF[22,23]. Arterial ammonia was measured in heparinized plasma by enzymatic method (RANDOX lab Ltd, UK) immediately before or within 6 h of imaging. Prior to infusion of mannitol infusion any metabolic derangement identified was corrected and all patients had been receiving standard anti-coma measures as well as other supportive measures such as head end elevation, oxygen supplementation, dextrose infusion to maintain normoglycemia. We did not hyperventilate our patients because this is not an established method for decreasing raised ICP, and our second aim was to see the effect of mannitol so we tried to avoid all other methods of decreasing ICP mentioned in literature[23,24].
An intravenous bolus of 20% mannitol solution (1 g/kg body weight) was given in controls as well as patients with ALF and ACLF after a baseline MRI scan (pre-mannitol study) for 10 min. After 30 min of mannitol injection, repeat MRI (post-mannitol study) for the same position was acquired. In post-mannitol study, both conventional T2-weighted and T1-weighted spin-echo (SE) imaging took a total time of 2.14 min and 1.34 min respectively, in vivo PMRS was done in 3.45 min and DTI data was acquired after 9.36 min and therefore the effect of mannitol was seen between 30-46 min (including time). The head was strapped to prevent any artifacts related to motion. The study protocol was approved by the institutional Ethics Committee and written informed consent was obtained from each subject or the nearest kin after explaining the nature of investigation to be carried out.
MRI protocol
Imaging was performed on a 1.5 tesla MRI scanner (Signa Lx Echo speed plus, General Electric Healthcare Technologies, Milwaukee, WI) equipped with an actively-shielded whole body magnetic field gradient set (allowing up to 33 mT/m) equipped with a quadrature birdcage receive and transmit radio frequency head coil. The routine imaging studies included the following: fast spin echo (FSE) T2-weighted images with repetition time (TR)/echo time (TE)/number of excitations (NEX) = 6000 ms/85 ms/4, and T1-weighted SE images with TR/TE/NEX = 1000 ms/14 ms/2. A total of 36 contiguous 3 mm thick axial sections were acquired with a 240 mm × 240 mm field of view (FOV) and image matrix of 256 × 256.
In vivo proton MR spectroscopy
The controls, ALF and ACLF patients underwent in vivo PMRS during the pre-mannitol study and post-mannitol study after the completion of intravenous mannitol administration to determine the changes in the brain metabolites. Spectra were obtained by using a water suppressed localized single voxel SE sequence with TR/TE = 3000 ms/35 ms. A voxel of 2 cm × 2 cm × 2 cm was located mainly in the right parietal region of the brain[25] in all the cases, containing part of white matter and gray matter (putamen and caudate nucleus) (Figure 1A). After global shimming, voxel shimming was performed, and a full width at half maximum of 4-6 Hz was achieved in all the cases. For evaluation and quantification of all individual spectra, the LC-Model software package (Version 6.0; Stephen Provencher, Ontario, Canada) was used for processing the MRS data. The process of determining peak intensities of the different metabolites is described in detail elsewhere[26]. The metabolite ratios of N-acetylaspartate (NAA), choline (Cho), glutamine (Gln), glutamine/glutamate (Glx), and myoinositol (mI) were calculated with respect to creatine (Cr).
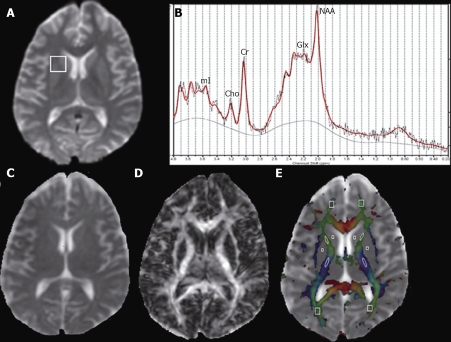
Figure 1.
Conventional magnetic resonance imaging (MRI) and diffusion tensor imaging (DTI) were performed at three days after the onset of encephalopathy in a 29-year-old man with acute liver failure (ALF) before the mannitol administration. A: Axial T2-weighted imaging at the level of third ventricle does not show any visible abnormality; B: Localized proton spectrum from 2 cm × 2 cm × 2 cm voxel placed on right parietal region (A) shows the metabolite ratios with respect to Cr (NAA/Cr = 1.35, Cho/Cr = 0.34, Gln/Cr = 2.57, Glx/Cr = 4.12, mI/Cr = 0.45); C: Mean diffusivity (MD) map, [anterior limb of internal capsule (ALIC) = 0.68, posterior limb of internal capsule (PLIC) = 0.65, caudate nuclei (CN) = 0.67, putamen (P) = 0.60, thalamus (TH) = 0.66, frontal white matter (FWM) = 0.66, occipital white matter (OWM) = 0.67, corpus callosum (CC) = 0.60, cingulum = 0.70, frontal cortex = 0.63, parietal cortex = 0.70, occipital cortex = 0.63]; D: Fractional anisotropy (FA) map, (ALIC = 0.32, PLIC = 0.34, CN = 0.09, putamen = 0.08, thalamus = 0.11, FWM = 0.33, OWM = 0.38, CC = 0.53, cingulum = 0.45, frontal cortex = 0.16, parietal cortex = 0.10, occipital cortex = 0.12). The cut off value for the color-coded FA for display is kept at 0.2 (E) above which the color-coded regions reflect the white matter only [red (right-left), green (anterior-posterior), and blue (superior-inferior)]. Cho: Choline; Cr: Creatine; Gln: Glutamine; Glx: Glutamine/glutamate; mI: Myoinositol; NAA: N-acetylaspartate.
DTI protocol
DTI data were acquired using a single-shot echo-planar dual SE sequence with ramp sampling[27]. The diffusion-weighted acquisition parameters were: b-factor = 0 s/mm2, 1000 s/mm2, slice thickness = 3 mm with no gap, number of slices = 34-38, FOV = 240 mm × 240 mm, TR = 8 s, TE = 100 ms and NEX = 8. The acquisition matrix was 128 × 80 and the homodyne algorithm was used to construct the κ-space data to 128 × 128 and zero-filled to generate an image matrix of 256 × 256. The diffusion tensor encoding used was the balanced rotationally invariant[28] dodecahedral scheme with 10 uniformly distributed directions over the unit hemisphere.
DTI data processing and analysis
The magnitude averaged data were transferred to a workstation for further analysis. In general, the DTI data analysis involves three major steps: pre-processing, processing, and post-processing.
Data pre-processing
The data were distortion corrected for shear, scale, rotation, and translation using the Automated Image and Registration package[29]. The removal of scalp to isolate the brain in the collected raw images was done, in all the cases, by an automated stripping procedure[30]. Subsequent DTI processing did not require any filtering, as justified by the absence of unprocessed voxels.
Data processing
The distortion corrected data were then interpolated to attain isotropic voxels and decoded to obtain the tensor field for each voxel. The tensor field data were then diagonalized using the analytical diagonalization method[31] to obtain the eigenvalues (λ1, λ2 and λ3) and the three orthonormal eigenvectors (e1, e2 and e3). The orthogonality of the computed eigenvectors and the correctness of the eigenvalues were checked using random sampling at a number of voxels. The correctness observed was up to an order of 10-17, indicating that no iterative refinement of the computed eigenvalues/vectors was needed. The tensor field data was then used to compute the DTI metrics such as mean diffusivity (Equation 1) and fractional anisotropy (Equation 2) for each voxel.
MD = (λ1 + λ2 + λ3)/3 Equation 1
FA(λ1, λ2, λ3) = Sqrt{[(λ1 - λ2)2 (λ2 - λ3)2 (λ1 - λ3)2]/2(λ12 + λ22 + λ32)} Equation 2
Data post-processing and quantification
JAVA based software was used to calculate various DTI derived metrics (MD and FA)[32]. To show homogenous distribution of metabolites within the brain, we selected major white matter and deep gray matter regions for region-of-interest(s) (ROI’s) analysis, because it has been reported in the previous studies that the changes are widespread in both the gray and the white matter in patients with hepatic encephalopathy[33]. For quantitative analysis, the DTI derived FA and MD maps were displayed and overlaid on images with different contrasts to facilitate the ROI’s placement. Elliptical and/or rectangular ROI’s varying from 2 × 2 and 6 × 6 pixels were placed on right and left anterior (ALIC) and posterior (PLIC) limb of internal capsule, right and left caudate nuclei (CN), right and left putamen (P), right and left thalamus (TH), right and left periventricular white matter of frontal (FWM) and occipital (OWM) lobes, right and left cingulum and corpus callosum (CC) at the level of third ventricle for DTI metrics quantifi-cation in these controls as well as patients (Figure 1E). Rectangular ROI’s were also placed at the level of frontal cortex, parietal cortex and occipital cortex to quantify the various DTI metrics.
The total brain volume changes (brain parenchyma as well as CSF volume) before and after the intravenous infusion of mannitol was also measured in all subjects on the T2-weighted images using the in-house JAVA based software.
Statistical analysis
Before statistical analysis, left and right measurements for all regions were pooled together. Mann-Whitney rank sum test was performed between the pre-mannitol study and post-mannitol study to see the statistical significant difference in the metabolite ratios (with respect to Cr), DTI metrics (FA and MD), brain parenchyma volume as well as CSF volume for controls (n = 5), ALF (n = 5) and ACLF (n = 5) patients. A P value of less than or equal to 0.05 was considered to be statistically significant. All the statistical analyses were performed using the statistical package for social sciences. (SPSS, V12, Inc, Chicago, USA).
RESULTS
Imaging findings
All patients in ALF and ACLF groups had grade 3 or grade 4 hepatic encephalopathy when they were subjected to MRI study after excluding all the metabolic factors which might contribute to altered mental state. All of these patients had imaging features of cytotoxic and interstitial edema on DTI suggestive of raised ICP. These patients were then treated with mannitol infusion and repeat MRI for the same position was acquired as shown in Tables 567, respectively. We compared the clinical signs and MR changes in both group of patients as well as controls pre and post mannitol infusion. None of the patients with ALF and ACLF showed significant clinical improvement in terms of the grade of encephalopathy and appearance of defined clinical signs of cerebral edema and MR findings.
Table 5.
Peak integrals relative to those of creatine (mean ± SD) in right parietal white and gray matter in healthy controls, acute liver failure (ALF) patients and acute-on-chronic liver failure (ACLF) patients before the intravenous infusion of mannitol (pre-mannitol study) and after receiving mannitol (post-mannitol study)
| Metabolites |
Study |
||||||||
|
Control (n = 5) |
ALF patient (n = 5) |
ACLF patient (n = 5) |
|||||||
| Pre-mannitol | Post-mannitol | P | Pre-mannitol | Post-mannitol | P | Pre-mannitol | Post-mannitol | P | |
| NAA/Cr | 1.25 ± 0.16 | 1.23 ± 0.17 | 0.92 | 1.20 ± 0.13 | 1.27 ± 0.32 | 0.75 | 0.90 ± 0.35 | 0.58 ± 0.29 | 0.18 |
| Cho/Cr | 0.24 ± 0.06 | 0.24 ± 0.08 | 0.75 | 0.18 ± 0.09 | 0.16 ± 0.07 | 0.47 | 0.20 ± 0.05 | 0.20 ± 0.03 | 0.75 |
| Gln/Cr | 1.44 ± 1.06 | 1.18 ± 0.94 | 0.35 | 3.04 ± 1.32 | 2.52 ± 1.56 | 0.25 | 1.44 ± 0.30 | 2.42 ± 1.44 | 0.60 |
| Glx/Cr | 2.84 ± 0.98 | 2.70 ± 1.21 | 0.60 | 4.46 ± 1.48 | 4.38 ± 1.61 | 0.92 | 2.85 ± 0.70 | 3.85 ± 2.13 | 0.35 |
| mI/Cr | 0.57 ± 0.48 | 0.49 ± 0.34 | 0.92 | 0.56 ± 0.15 | 0.47 ± 0.16 | 0.18 | 0.41 ± 0.17 | 0.89 ± 1.14 | 0.81 |
Cr: Creatine; NAA: N-acetylaspartate; Cho: Choline; Gln: Glutamine; Glx: Glutamine/glutamate; mI: Myoinositol.
Table 6.
Summary of fractional anisotropy values (mean ± SD) from different white and gray matter regions in controls, patients with acute liver failure (ALF) and acute-on-chronic liver failure (ACLF) before the intravenous infusion of mannitol (pre-mannitol study) and after receiving mannitol (post-mannitol study)
| Region |
Study |
||||||||
|
Control (n = 5) |
ALF patient (n = 5) |
ACLF patient (n = 5) |
|||||||
| Pre-mannitol | Post-mannitol | P | Pre-mannitol | Post-mannitol | P | Pre-mannitol | Post-mannitol | P | |
| ALIC | 0.36 ± 0.05 | 0.37 ± 0.04 | 0.60 | 0.30 ± 0.03 | 0.30 ± 0.02 | 0.47 | 0.32 ± 0.02 | 0.33 ± 0.02 | 0.56 |
| PLIC | 0.49 ± 0.05 | 0.48 ± 0.05 | 0.60 | 0.33 ± 0.02 | 0.34 ± 0.01 | 0.12 | 0.45 ± 0.03 | 0.40 ± 0.03 | 0.08 |
| CN | 0.11 ± 0.00 | 0.11 ± 0.00 | 0.47 | 0.09 ± 0.01 | 0.09 ± 0.01 | 0.60 | 0.08 ± 0.01 | 0.09 ± 0.01 | 0.56 |
| P | 0.09 ± 0.01 | 0.09 ± 0.01 | 0.92 | 0.06 ± 0.01 | 0.07 ± 0.01 | 0.92 | 0.06 ± 0.02 | 0.08 ± 0.01 | 0.15 |
| TH | 0.15 ± 0.01 | 0.14 ± 0.01 | 0.12 | 0.12 ± 0.00 | 0.12 ± 0.01 | 0.92 | 0.14 ± 0.01 | 0.15 ± 0.03 | 0.77 |
| FWM | 0.31 ± 0.03 | 0.30 ± 0.03 | 0.92 | 0.30 ± 0.03 | 0.32 ± 0.07 | 0.92 | 0.32 ± 0.04 | 0.36 ± 0.07 | 0.56 |
| OWM | 0.38 ± 0.06 | 0.38 ± 0.07 | 0.92 | 0.38 ± 0.04 | 0.37 ± 0.05 | 0.92 | 0.35 ± 0.04 | 0.31 ± 0.02 | 0.15 |
| CC | 0.53 ± 0.04 | 0.54 ± 0.06 | 0.92 | 0.44 ± 0.06 | 0.45 ± 0.02 | 0.35 | 0.50 ± 0.04 | 0.51 ± 0.05 | 0.77 |
| Cingulum | 0.36 ± 0.03 | 0.37 ± 0.04 | 0.75 | 0.44 ± 0.07 | 0.41 ± 0.03 | 0.25 | 0.38 ± 0.03 | 0.36 ± 0.03 | 0.56 |
| Frontal cortex | 0.12 ± 0.01 | 0.11 ± 0.00 | 0.47 | 0.12 ± 0.04 | 0.12 ± 0.04 | 0.60 | 0.14 ± 0.02 | 0.11 ± 0.02 | 0.08 |
| Parietal cortex | 0.12 ± 0.01 | 0.12 ± 0.01 | 0.75 | 0.11 ± 0.01 | 0.10 ± 0.01 | 0.75 | 0.14 ± 0.01 | 0.11 ± 0.03 | 0.39 |
| Occipital cortex | 0.11 ± 0.02 | 0.12 ± 0.03 | 0.47 | 0.14 ± 0.05 | 0.10 ± 0.03 | 0.25 | 0.10 ± 0.05 | 0.13 ± 0.03 | 0.39 |
ALIC: Anterior limb of internal capsule; PLIC: Posterior limb of internal capsule; CN: Caudate nuclei; P: Putamen; TH: Thalamus; FWM: Frontal white matter; OWM: Occipital white matter; CC: Corpus callosum.
Table 7.
Summary of mean diffusivity values (mean ± SD) in units of 10-3 mm2/s from different white and gray matter regions in controls, patients with acute liver failure (ALF) and acute-on-chronic liver failure (ACLF) before the intravenous infusion of mannitol (pre-mannitol study) and after receiving mannitol (post-mannitol study)
| Region |
Study |
||||||||
|
Control (n = 5) |
ALF patient (n = 5) |
ACLF patient (n = 5) |
|||||||
| Pre-mannitol | Post-mannitol | P | Pre-mannitol | Post-mannitol | P | Pre-mannitol | Post-mannitol | P | |
| ALIC | 0.76 ± 0.07 | 0.76 ± 0.05 | 0.60 | 0.68 ± 0.02 | 0.68 ± 0.02 | 0.75 | 0.72 ± 0.02 | 0.71 ± 0.08 | 0.56 |
| PLIC | 0.74 ± 0.06 | 0.75 ± 0.05 | 0.75 | 0.67 ± 0.03 | 0.67 ± 0.02 | 0.92 | 0.65 ± 0.03 | 0.65 ± 0.04 | 0.77 |
| CN | 0.73 ± 0.02 | 0.74 ± 0.02 | 0.75 | 0.68 ± 0.01 | 0.69 ± 0.02 | 0.92 | 0.69 ± 0.02 | 0.69 ± 0.09 | 0.25 |
| P | 0.69 ± 0.01 | 0.70 ± 0.06 | 0.25 | 0.64 ± 0.03 | 0.63 ± 0.01 | 0.47 | 0.69 ± 0.02 | 0.69 ± 0.06 | 0.39 |
| TH | 0.72 ± 0.03 | 0.71 ± 0.03 | 0.92 | 0.66 ± 0.02 | 0.66 ± 0.04 | 0.92 | 0.71 ± 0.02 | 0.74 ± 0.05 | 0.56 |
| FWM | 0.77 ± 0.06 | 0.76 ± 0.07 | 0.75 | 0.67 ± 0.01 | 0.66 ± 0.05 | 0.92 | 0.65 ± 0.02 | 0.66 ± 0.13 | 0.25 |
| OWM | 0.76 ± 0.05 | 0.76 ± 0.07 | 0.92 | 0.66 ± 0.03 | 0.66 ± 0.05 | 0.75 | 0.76 ± 0.11 | 0.68 ± 0.05 | 0.56 |
| CC | 0.74 ± 0.07 | 0.74 ± 0.07 | 0.92 | 0.74 ± 0.09 | 0.74 ± 0.08 | 0.92 | 0.77 ± 0.09 | 0.77 ± 0.09 | 0.77 |
| Cingulum | 0.72 ± 0.05 | 0.72 ± 0.09 | 0.75 | 0.72 ± 0.10 | 0.72 ± 0.04 | 0.75 | 0.73 ± 0.03 | 0.70 ± 0.06 | 0.56 |
| Frontal cortex | 0.69 ± 0.07 | 0.69 ± 0.04 | 0.92 | 0.68 ± 0.04 | 0.68 ± 0.05 | 0.92 | 0.65 ± 0.05 | 0.70 ± 0.03 | 0.08 |
| Parietal cortex | 0.68 ± 0.06 | 0.68 ± 0.05 | 0.92 | 0.68 ± 0.01 | 0.68 ± 0.03 | 0.47 | 0.69 ± 0.04 | 0.63 ± 0.04 | 0.08 |
| Occipital cortex | 0.67 ± 0.07 | 0.67 ± 0.06 | 0.92 | 0.66 ± 0.02 | 0.66 ± 0.05 | 0.92 | 0.69 ± 0.06 | 0.62 ± 0.03 | 0.15 |
ALIC: Anterior limb of internal capsule; PLIC: Posterior limb of internal capsule; CN: Caudate nuclei; P: Putamen; TH: Thalamus; FWM: Frontal white matter; OWM: Occipital white matter; CC: Corpus callosum.
In vivo MR spectroscopy
The mean metabolites ratios calculated for the controls, ALF patients and ACLF patients are shown in Table 5. In all these subjects, no statistical significant difference was observed in the ratios of NAA/Cr, Cho/Cr, Gln/Cr, Glx/Cr, and mI/Cr between the pre-mannitol study (Figure 1B) and post-mannitol study (Figure 2B).
Figure 2.
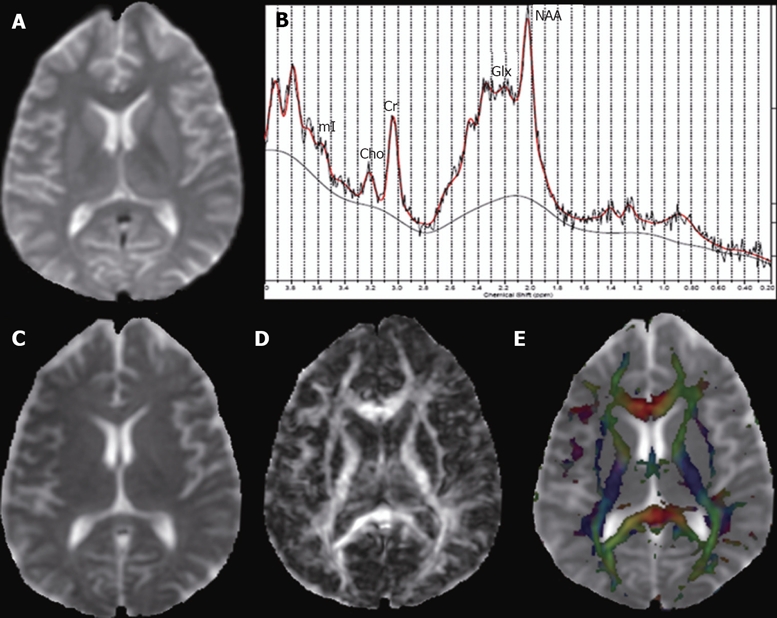
Repeat MRI and DTI were performed after 30 min of mannitol infusion on the same ALF patient as in Figure 1 to look for any mannitol effect on imaging. In post-mannitol study, the effect of mannitol was quantified between 30-46 min. A: Axial T2-weighted image; B: Localized proton spectrum from the same region as in Figure 1A shows NAA/Cr = 1.83, Cho/Cr = 0.29, Gln/Cr = 2.60, Glx/Cr = 4.57, mI/Cr = 0.32; C: Mean diffusivity (MD) map, [anterior limb of internal capsule (ALIC) = 0.67, posterior limb of internal capsule (PLIC) = 0.70, caudate nuclei (CN) = 0.70, putamen (P) = 0.63, thalamus (TH) = 0.62, frontal white matter (FWM) = 0.66, occipital white matter (OWM) = 0.60, corpus callosum (CC) = 0.70, cingulum = 0.72, frontal cortex = 0.69, parietal cortex = 0.66, occipital cortex = 0.62]; D: Fractional anisotropy (FA) map, (ALIC = 0.32, PLIC = 0.34, CN = 0.08, putamen = 0.06, thalamus = 0.13, FWM = 0.30, OWM = 0.43, CC = 0.46, cingulum = 0.40, frontal cortex = 0.10, parietal cortex = 0.12, occipital cortex = 0.08) at the level of third ventricle. E: There is no significant change in the MD and FA values, and metabolite ratios mentioned here compared to what is mentioned in Figure 1. Cho: Choline; Cr: Creatine; Gln: Glutamine; Glx: Glutamine/glutamate; mI: Myoinositol; NAA: N-acetylaspartate.
Changes in DTI metrics
The mean MD and FA values extracted from ROI’s in controls, ALF patients and ACLF patients are summarized in Tables 6 and 7, respectively. None of the DTI metrics showed any significant difference between the pre-mannitol study (Figure 1C and D) and post-mannitol study (Figure 2C and D) in controls as well as ALF and ACLF patients.
Changes in total brain volume
In all subjects, no significant change was found in both brain parenchyma volume as well as CSF volume before mannitol administration and at 45 min after the completion of mannitol infusion (Table 8).
Table 8.
Change in brain volume and cerebrospinal fluid (CSF) volume values (mean ± SD) in units of cubic centimeter from different white and gray matter regions in controls, patients with acute liver failure (ALF) and acute-on-chronic liver failure (ACLF) before the intravenous infusion of mannitol (pre-mannitol study) and after receiving mannitol (post-mannitol study)
| Volume |
Study |
||||||||
|
Control (n = 5) |
ALF Patient (n = 5) |
ACLF Patient (n = 5) |
|||||||
| Pre-mannitol | Post-mannitol | P | Pre-mannitol | Post-mannitol | P | Pre-mannitol | Post-mannitol | P | |
| Brain volume | 1303.47 ± 54.95 | 1308.88 ± 64.95 | 0.75 | 1130.76 ± 86.73 | 1162.39 ± 77.75 | 0.47 | 1096.85 ± 79.55 | 1076.90 ± 71.63 | 0.60 |
| CSF volume | 84.05 ± 4.88 | 85.10 ± 6.46 | 0.60 | 73.77 ± 19.72 | 73.27 ± 19.53 | 0.47 | 76.77 ± 18.68 | 83.84 ± 22.09 | 0.12 |
DISCUSSION
In case of patients with abnormal liver function or liver failure, detoxification of ammonia into glutamine by glutamine synthetase occurs in the brain astrocytes[34,35]. It has been reported that the facilitated transport system operates to maintain the normal level of the nitrogen-rich osmolytes[36]. This process is energy dependent and requires normal metabolic conditions to operate. However, in case of patients with liver failure such a favorable milieu is not present. This suggests the increased concentration of nitrogen-rich compounds in brain of patients with liver failure, as also reported in previous studies[37,38]. It has been reported that the increased concentration of glutamine in these patients is associated with increased brain water content resulting in cerebral edema[39,40]. The use of hypertonic solutions for pulling out water initially from extracellular space and eventually from the intracellular compartment, along with clinical improvements in these patients, has been reported[41].
In the present study, no significant change in the relative concentration of various metabolites in controls, ALF and ACLF patients after mannitol administration was observed, and this finding was associated with no change in the brain water content as well as in the clinical condition of patients. It has been reported that decreased myoinositol concentration is associated with compensatory response to the osmotic gradient induced by the high level of glutamine[17]. In case of controls and ALF patients, no significant decrease in mI/Cr ratio after mannitol infusion suggests that the osmotic gradient due to mannitol might not be able to shift the myoinositol osmolyte across the BBB to compensate the intracellular osmolarity caused by accumulation of astrocytic glutamine. In case of ACLF patients, the slight increase in Gln/Cr, Glx/Cr and mI/Cr was seen after the infusion of mannitol; however, it did not reach the level of statistical significance. This further confirms that the osmotic gradient due to mannitol is not able to influence the efflux of organic osmolytes across the BBB. The lack of significant change in PMRS findings may be due to the fact that this was an acute study in which the pre- and post-mannitol studies were spaced 45 min apart. It is well known that the proxy changes of cerebral edema picked up by PMRS (i.e. depletion of choline, myoinositol, N-acetyl aspartate) are due to osmolyte shifts that occur over a prolonged timeframe and not in minutes[42,43].
We did not find any significant change in the DTI metrics (FA and MD) in controls as well as in patients with ALF and ACLF at 45 min after the completion of mannitol administration. In controls, insignificant change in either FA or MD values in normal brain tissues (white matter and gray matter) suggest that mannitol has no effect on the microstructural integrity and brain water content. This finding is in line with the previous study, which showed no change in the brain water content in normal white matter and cortex of patients with cerebral tumors[14]. The possible explanation could be due to the high hydraulic resistance of the capillaries in the normal brain tissues, and therefore mannitol might not be able to withdraw water osmotically from normal brain tissues[14]. Cascino et al have shown that the increased brain density of both edematous peritumoral white matter and normal gray and white matter on CT is related to the mannitol induced reduction in brain water content in patients with cerebral tumors[13]. They found that the maximum changes occurred after 36 min of mannitol infusion[13]. Bell et al showed that mannitol significantly reduced longitudinal relaxation time (T1) of oedematous peritumoral white matter and tumor tissue but did not have any significant effect on the normal white matter or cortex[14]. The maximum decrease in brain water content was found after 30 min of mannitol infusion, which was associated with the reduction in T1 values[14].
The effect of mannitol in patients with liver failure depends on the nature of cerebral edema. It has been reported that the nature of cerebral edema in case of ALF is predominantly cytotoxic along with some interstitial component[44]. However, the nature of cerebral edema in ACLF has yet to be described. The result from unpublished data suggests the predominant interstitial component of edema in ACLF[45]. In a previous study, the reduction in brain water content has been reported after mannitol administration in ALF patients by the observed decrease in ICP, as well as reversal of the clinical signs and concluded that the operative edema is of the cytotoxic type that resolved after mannitol treatment[10]. However, in the current study no change in the FA and MD values in patients with ALF and ACLF suggests any effect of mannitol on the brain water content along with the microstructural integrity. The BBB is known to be disrupted in both conditions of ALF and ACLF resulting in the interstitial component of cerebral edema. The tight endothelial junctions of the BBB open in both these conditions; however, the extent to which these endothelial junctions of BBB open is different. Hartwell et al also have reported no significant change in the water content of the edematous white matter after mannitol infusion in cats. This finding was explained based on the changes in the BBB that extended beyond the region of central necrosis induced by the cold lesion, which may have resulted in the disturbance of osmotic gradient[12]. In our study, no change in the brain water content as depicted by no change in the MD values in ALF and ACLF patients after mannitol infusion can be explained on the basis of the disruption of BBB due to the presence of interstitial component of cerebral edema. This may affect the mannitol induced osmotic gradient across the BBB and result in no withdrawal of water from the edematous brain tissue to the intravascular space.
Our above results are further supported by no significant change in the brain parenchyma volume and CSF volume in controls and patients with ALF and ACLF. In our study, we have explained the action of mannitol only on the basis of the osmotic gradient across the BBB, which is known to affect the brain volume of the normal tissue[11]. The cerebral blood flow is an important hemodynamic parameter that is shown to be reduced after mannitol administration[46,47]. Although in our study we do rule out the possibility of an osmotic gradient across the BBB, other vascular factors such as changes in cerebral blood flow, blood viscosity and oxygen delivery at the tissue level might be responsible for the effects of mannitol[12]. However, in our patients we did not quantify the cerebral blood flow and ICP. The use of ICP monitoring in ALF is a subject of ongoing debate. ICP monitoring is used variably across the world, with some centers not considering it useful and other using it regularly. In our study and, in fact, in most of the centers in our country direct ICP measurement is not used. The clinical signs used in our study are the reliable clinical signs of raised ICP, provided that other causes like brain hemorrhage or intracranial space occupying lesion which may cause raised ICP are excluded. However, these clinical signs are not uniformly present in all cases, but if at all present these signs are suggestive of raised ICP. In our study, all the patients had these clinical signs. In a landmark study, Canalese et al measured cerebral edema by the presence of defined clinical signs as well as continuous monitoring of ICP in two different groups in their study[10]. Among the patients who received mannitol, cerebral edema was considered to have developed in 17 patients, in nine on evidence from continuous intracranial monitoring and in eight on the basis of clinical signs[10]. In those patients who died, ICP was monitored with either clinical signs of cerebral edema or direct measurement; when brain autopsy was done, a close correlation was found between the evidence of cerebral edema in life and findings at the autopsy of brain, whereas there was no evidence of correlation in the four other patients whose ICP was not raised and who had no clinical features of cerebral edema[10]. Acharya et al in their study of clinical profile of ALF patients and predictors of mortality from tropical country had also used similar clinical signs to monitor cerebral edema[21]. The AASLD guidelines for management of ALF mentioned ICP monitoring either by direct measurement or by obvious clinical signs[23]. Stravitz et al reported that there are insufficient data to recommend ICP monitor placement in all patients with ALF; however, according to these authors all patients who are candidate for orthotopic liver transplantation (OLT) should undergo ICP monitoring[20]. In our study, all the patients were managed conservatively and none had finances for OLT. Nevertheless, it is true without ICP monitoring we can not quantify ICP, and this is one of limitations of our study since we did not measure ICP. However, the monitoring of response can be done by improvement of clinical signs or reduction of ICP, and obviously reduction in ICP would have been the best way to see the amount of response. There is no relationship of dosing of mannitol according to the severity of ICP. AASLD guidelines suggested the main role of ICP monitoring to detect early rise in intracranial pressure even before the development of clinical signs, and ICP should be maintained below 20-25 mmHg if possible. So once clinical features of raised ICP appear, it means intracranial pressure has significantly raised[23].
The absence of changes in the clinical status of these patients further supports that there is likely no significant effect of mannitol on their clinical management in this time window. However, the effect of mannitol over days is more difficult to assess due to other co-variates used for its management that might also contribute for the survival of some of these patients.
The osmotic effect of mannitol in the reduction of brain water content does not have any significant immediate effect on the clinical status in ALF and ACLF patients. The effect of other vascular factors that may alter the ICP indirectly will be the subject for future study to assess the mannitol effect using other noninvasive techniques such as perfusion imaging.
This is a first pilot study to see the direct effect of mannitol in ALF and ACLF patients. The conclusion of our study is that mannitol does not have an early effect (single dose effect seen in 45 min). However, we cannot conclude by saying that mannitol does not have any role in the management of ALF and ACLF patients, as previous studies[10] have shown that average response to mannitol therapy comes after 3 doses. Therefore, from our study, we cannot comment upon the delayed effect of mannitol with multiple doses. We plan to study the delayed effect of mannitol with more than one dose of mannitol in future.
COMMENTS
Background
Cerebral edema plays a major role in the outcome of both acute liver failure (ALF) and acute-on-chronic liver failure (ACLF). Bolus intravenous infusion of mannitol has been widely used to treat episodes of raised intracranial pressure (ICP) in these conditions. However, there are no data available regarding the effect of mannitol infusions on brain water content in ALF and ACLF, using sensitive imaging techniques.
Research frontiers
This is a pilot study to see the acute effect of mannitol in ALF and ACLF patients. The conclusion of our study is that mannitol does not have an early effect (single dose effect seen in 45 min). However, we cannot conclude by saying that mannitol does not have any role in the management of ALF and ACLF patients, as previous studies have shown that average response to mannitol therapy comes after three doses of mannitol. Therefore, from our study, we cannot comment upon the late effect of mannitol with multiple doses. The osmotic effect of mannitol in the reduction of brain water content does not have any significant immediate effect on the clinical status in ALF and ACLF patients. The effect of other vascular factors that may alter the ICP indirectly will be the subject for future study to assess the mannitol effect using other noninvasive techniques such as perfusion imaging.
Innovations and breakthroughs
This is the first study evaluating the effect of mannitol on brain water content using diffusion tensor imaging (DTI) and proton magnetic resonance spectroscopy (PMRS) in controls as well as in patients with ALF and ACLF. We hypothesize that the effect of bolus infusion of mannitol in reducing brain water content will be reflected by changes measured by conventional magnetic resonance effect (MRI), in vivo PMRS and DTI. Since the peak effect of a single bolus in mobilizing fluid from tissues to the intravascular compartment according to the osmotic gradient is observed at about 45 min after infusion, it was decided to evaluate the effect of intravenous bolus of mannitol during the baseline MRI scan (pre-mannitol study) and after the completion of mannitol administration (post-mannitol study).
Applications
Conventional MRI, DTI and PMRS can be used as a diagnostic modality to demonstrate the raised ICP in ALF and ACLF patients noninvasively. The purpose of this paper is to establish whether mannitol has any role in the reduction of brain water content, alteration in metabolite ratios or any change in the clinical status of ALF and ACLF patients during or within 45 min of mannitol infusion, and to know about the exact duration and dose of mannitol to show response after therapy.
Peer review
This is the first study evaluating the effect of mannitol on brain water content using DTI and PMRS in controls as well as in patients with ALF and ACLF. The osmotic effect of mannitol in the reduction of brain water content does not have any significant immediate effect on the clinical status in ALF and ACLF patients. The effect of other vascular factors that may alter the ICP indirectly will be the subject for future study to assess the mannitol effect using other noninvasive techniques such as perfusion imaging.
Supported by The Indian Council of Medical Research (Saksena S), India; New Delhi (Nath K), India; The National Institute of Mental Health, MH58284 and MH06595 (Thomas MA)
Peer reviewer: Dr. Mercedes Susan Mandell, Department of Anesthesiology, University of Colorado Health Sciences Center, Leprino Office Building, 12401 E. 17th Ave, B113, Aurora 80045, United States
S- Editor Zhong XY L- Editor Li M E- Editor Yin DH
References
- 1.Bauer M, Winning J, Kortgen A. Liver failure. Curr Opin Anaesthesiol. 2005;18:111–116. doi: 10.1097/01.aco.0000162827.74270.32. [DOI] [PubMed] [Google Scholar]
- 2.Sass DA, Shakil AO. Fulminant hepatic failure. Liver Transpl. 2005;11:594–605. doi: 10.1002/lt.20435. [DOI] [PubMed] [Google Scholar]
- 3.Jalan R, Williams R. Acute-on-chronic liver failure: pathophysiological basis of therapeutic options. Blood Purif. 2002;20:252–261. doi: 10.1159/000047017. [DOI] [PubMed] [Google Scholar]
- 4.Vaquero J, Fontana RJ, Larson AM, Bass NM, Davern TJ, Shakil AO, Han S, Harrison ME, Stravitz TR, Munoz S, et al. Complications and use of intracranial pressure monitoring in patients with acute liver failure and severe encephalopathy. Liver Transpl. 2005;11:1581–1589. doi: 10.1002/lt.20625. [DOI] [PubMed] [Google Scholar]
- 5.Jalan R. Pathophysiological basis of therapy of raised intracranial pressure in acute liver failure. Neurochem Int. 2005;47:78–83. doi: 10.1016/j.neuint.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 6.Vaquero J, Chung C, Cahill ME, Blei AT. Pathogenesis of hepatic encephalopathy in acute liver failure. Semin Liver Dis. 2003;23:259–269. doi: 10.1055/s-2003-42644. [DOI] [PubMed] [Google Scholar]
- 7.Wright G, Jalan R. Management of hepatic encephalopathy in patients with cirrhosis. Best Pract Res Clin Gastroenterol. 2007;21:95–110. doi: 10.1016/j.bpg.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 8.Diringer MN, Zazulia AR. Osmotic therapy: fact and fiction. Neurocrit Care. 2004;1:219–233. doi: 10.1385/NCC:1:2:219. [DOI] [PubMed] [Google Scholar]
- 9.Bruce DA, Berman WA, Schut L. Cerebrospinal fluid pressure monitoring in children: physiology, pathology and clinical usefulness. Adv Pediatr. 1977;24:233–290. [PubMed] [Google Scholar]
- 10.Canalese J, Gimson AE, Davis C, Mellon PJ, Davis M, Williams R. Controlled trial of dexamethasone and mannitol for the cerebral oedema of fulminant hepatic failure. Gut. 1982;23:625–629. doi: 10.1136/gut.23.7.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Videen TO, Zazulia AR, Manno EM, Derdeyn CP, Adams RE, Diringer MN, Powers WJ. Mannitol bolus preferentially shrinks non-infarcted brain in patients with ischemic stroke. Neurology. 2001;57:2120–2122. doi: 10.1212/wnl.57.11.2120. [DOI] [PubMed] [Google Scholar]
- 12.Hartwell RC, Sutton LN. Mannitol, intracranial pressure, and vasogenic edema. Neurosurgery. 1993;32:444–450; discussion 450. [PubMed] [Google Scholar]
- 13.Cascino T, Baglivo J, Conti J, Szewczykowski J, Posner JB, Rottenberg DA. Quantitative CT assessment of furosemide- and mannitol-induced changes in brain water content. Neurology. 1983;33:898–903. doi: 10.1212/wnl.33.7.898. [DOI] [PubMed] [Google Scholar]
- 14.Bell BA, Smith MA, Kean DM, McGhee CN, MacDonald HL, Miller JD, Barnett GH, Tocher JL, Douglas RH, Best JJ. Brain water measured by magnetic resonance imaging. Correlation with direct estimation and changes after mannitol and dexamethasone. Lancet. 1987;1:66–69. doi: 10.1016/s0140-6736(87)91908-8. [DOI] [PubMed] [Google Scholar]
- 15.Grover VP, Dresner MA, Forton DM, Counsell S, Larkman DJ, Patel N, Thomas HC, Taylor-Robinson SD. Current and future applications of magnetic resonance imaging and spectroscopy of the brain in hepatic encephalopathy. World J Gastroenterol. 2006;12:2969–2978. doi: 10.3748/wjg.v12.i19.2969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Verma A, Saraswat VA, Radha Krishna Y, Nath K, Thomas MA, Gupta RK. In vivo 1H magnetic resonance spectroscopy-derived metabolite variations between acute-on-chronic liver failure and acute liver failure. Liver Int. 2008;28:1095–1103. doi: 10.1111/j.1478-3231.2007.01648.x. [DOI] [PubMed] [Google Scholar]
- 17.Cordoba J, Gottstein J, Blei AT. Glutamine, myo-inositol, and organic brain osmolytes after portocaval anastomosis in the rat: implications for ammonia-induced brain edema. Hepatology. 1996;24:919–923. doi: 10.1002/hep.510240427. [DOI] [PubMed] [Google Scholar]
- 18.Restuccia T, Gomez-Anson B, Guevara M, Alessandria C, Torre A, Alayrach ME, Terra C, Martín M, Castellví M, Rami L, et al. Effects of dilutional hyponatremia on brain organic osmolytes and water content in patients with cirrhosis. Hepatology. 2004;39:1613–1622. doi: 10.1002/hep.20237. [DOI] [PubMed] [Google Scholar]
- 19.Le Bihan D. Looking into the functional architecture of the brain with diffusion MRI. Nat Rev Neurosci. 2003;4:469–480. doi: 10.1038/nrn1119. [DOI] [PubMed] [Google Scholar]
- 20.Stravitz RT, Kramer AH, Davern T, Shaikh AO, Caldwell SH, Mehta RL, Blei AT, Fontana RJ, McGuire BM, Rossaro L, et al. Intensive care of patients with acute liver failure: recommendations of the U.S. Acute Liver Failure Study Group. Crit Care Med. 2007;35:2498–2508. doi: 10.1097/01.CCM.0000287592.94554.5F. [DOI] [PubMed] [Google Scholar]
- 21.Acharya SK, Dasarathy S, Kumer TL, Sushma S, Prasanna KS, Tandon A, Sreenivas V, Nijhawan S, Panda SK, Nanda SK, et al. Fulminant hepatitis in a tropical population: clinical course, cause, and early predictors of outcome. Hepatology. 1996;23:1448–1455. doi: 10.1002/hep.510230622. [DOI] [PubMed] [Google Scholar]
- 22.Bhatia V, Batra Y, Acharya SK. Prophylactic phenytoin does not improve cerebral edema or survival in acute liver failure--a controlled clinical trial. J Hepatol. 2004;41:89–96. doi: 10.1016/j.jhep.2004.03.017. [DOI] [PubMed] [Google Scholar]
- 23.Polson J, Lee WM. AASLD position paper: the management of acute liver failure. Hepatology. 2005;41:1179–1197. doi: 10.1002/hep.20703. [DOI] [PubMed] [Google Scholar]
- 24.Ede RJ, Gimson AE, Bihari D, Williams R. Controlled hyperventilation in the prevention of cerebral oedema in fulminant hepatic failure. J Hepatol. 1986;2:43–51. doi: 10.1016/s0168-8278(86)80007-1. [DOI] [PubMed] [Google Scholar]
- 25.Thomas MA, Huda A, Guze B, Curran J, Bugbee M, Fairbanks L, Ke Y, Oshiro T, Martin P, Fawzy F. Cerebral 1H MR spectroscopy and neuropsychologic status of patients with hepatic encephalopathy. AJR Am J Roentgenol. 1998;171:1123–1130. doi: 10.2214/ajr.171.4.9763008. [DOI] [PubMed] [Google Scholar]
- 26.Provencher SW. Automatic quantitation of localized in vivo 1H spectra with LCModel. NMR Biomed. 2001;14:260–264. doi: 10.1002/nbm.698. [DOI] [PubMed] [Google Scholar]
- 27.Le Bihan D. Diffusion and Perfusion Magnetic Resonance Imaging-Applications to functional MRI. Vol. 14. New York: Raven Press Ltd; 1995. [Google Scholar]
- 28.Hasan KM, Parker DL, Alexander AL. Comparison of gradient encoding schemes for diffusion-tensor MRI. J Magn Reson Imaging. 2001;13:769–780. doi: 10.1002/jmri.1107. [DOI] [PubMed] [Google Scholar]
- 29.Woods RP, Mazziotta JC, Cherry SR. MRI-PET registration with automated algorithm. J Comput Assist Tomogr. 1993;17:536–546. doi: 10.1097/00004728-199307000-00004. [DOI] [PubMed] [Google Scholar]
- 30.Purwar A, Gupta RK, Sarma MK, Bayu G, Singh A, Divya DKS, Saksena S, Trivedi R, Mishra AM, Haris M, et al. De-scalping of the brain in echo planar DT-MRI. Proc International Society of Magnetic Resonance in Medicine. New York: Raven Press Ltd; 2006. p. 325. [Google Scholar]
- 31.Hasan KM, Basser PJ, Parker DL, Alexander AL. Analytical computation of the eigenvalues and eigenvectors in DT-MRI. J Magn Reson. 2001;152:41–47. doi: 10.1006/jmre.2001.2400. [DOI] [PubMed] [Google Scholar]
- 32.Purwar A, Rathore DK, Rathore RKS, Gupta RK. A DTI analysis tool. Proc of European Society of Magnetic Resonance in Medicine. New York: Raven Press Ltd; 2006. p. 644 (Abstract number). [Google Scholar]
- 33.Cordoba J, Alonso J, Rovira A, Jacas C, Sanpedro F, Castells L, Vargas V, Margarit C, Kulisewsky J, Esteban R, et al. The development of low-grade cerebral edema in cirrhosis is supported by the evolution of (1)H-magnetic resonance abnormalities after liver transplantation. J Hepatol. 2001;35:598–604. doi: 10.1016/s0168-8278(01)00181-7. [DOI] [PubMed] [Google Scholar]
- 34.Martinez-Hernandez A, Bell KP, Norenberg MD. Glutamine synthetase: glial localization in brain. Science. 1977;195:1356–1358. doi: 10.1126/science.14400. [DOI] [PubMed] [Google Scholar]
- 35.Brusilow SW, Traystman R. Hepatic encephalopathy. N Engl J Med. 1986;314:786–787; author reply 787. [PubMed] [Google Scholar]
- 36.Lee WJ, Hawkins RA, Vina JR, Peterson DR. Glutamine transport by the blood-brain barrier: a possible mechanism for nitrogen removal. Am J Physiol. 1998;274:C1101–C1107. doi: 10.1152/ajpcell.1998.274.4.C1101. [DOI] [PubMed] [Google Scholar]
- 37.Record CO, Buxton B, Chase RA, Curzon G, Murray-Lyon IM, Williams R. Plasma and brain amino acids in fulminant hepatic failure and their relationship to hepatic encephalopathy. Eur J Clin Invest. 1976;6:387–394. doi: 10.1111/j.1365-2362.1976.tb00533.x. [DOI] [PubMed] [Google Scholar]
- 38.Norenberg MD. Astrocytic-ammonia interactions in hepatic encephalopathy. Semin Liver Dis. 1996;16:245–253. doi: 10.1055/s-2007-1007237. [DOI] [PubMed] [Google Scholar]
- 39.Haussinger D, Laubenberger J, vom Dahl S, Ernst T, Bayer S, Langer M, Gerok W, Hennig J. Proton magnetic resonance spectroscopy studies on human brain myo-inositol in hypo-osmolarity and hepatic encephalopathy. Gastroenterology. 1994;107:1475–1480. doi: 10.1016/0016-5085(94)90552-5. [DOI] [PubMed] [Google Scholar]
- 40.Blei AT, Larsen FS. Pathophysiology of cerebral edema in fulminant hepatic failure. J Hepatol. 1999;31:771–776. doi: 10.1016/s0168-8278(99)80361-4. [DOI] [PubMed] [Google Scholar]
- 41.Larsen FS. Optimal management of patients with fulminant hepatic failure: targeting the brain. Hepatology. 2004;39:299–301. doi: 10.1002/hep.20071. [DOI] [PubMed] [Google Scholar]
- 42.Rovira A, Grive E, Pedraza S, Rovira A, Alonso J. Magne-tization transfer ratio values and proton MR spectroscopy of normal-appearing cerebral white matter in patients with liver cirrhosis. AJNR Am J Neuroradiol. 2001;22:1137–1142. [PMC free article] [PubMed] [Google Scholar]
- 43.Rovira A, Cordoba J, Raguer N, Alonso J. Magnetic resonance imaging measurement of brain edema in patients with liver disease: resolution after transplantation. Curr Opin Neurol. 2002;15:731–737. doi: 10.1097/01.wco.0000044771.39452.8d. [DOI] [PubMed] [Google Scholar]
- 44.Saksena S, Rai V, Saraswat VA, Rathore RS, Purwar A, Kumar M, Thomas MA, Gupta RK. Cerebral diffusion tensor imaging and in vivo proton magnetic resonance spectroscopy in patients with fulminant hepatic failure. J Gastroenterol Hepatol. 2008;23:e111–e119. doi: 10.1111/j.1440-1746.2007.05158.x. [DOI] [PubMed] [Google Scholar]
- 45.Nath K, Gupta RK, Trivedi R, Yellapu RK, Rai V, Saraswat VA, Purwar A, Rathore DKS, Rathore RKS. Diffusion tensor imaging in patients with acute-on-chronic liver failure. Proc International Society of Magnetic Resonance in Medicine. New York: Raven Press Ltd; 2007. p. 675; Epub ahead of print. [Google Scholar]
- 46.Wendon JA, Harrison PM, Keays R, Williams R. Cerebral blood flow and metabolism in fulminant liver failure. Hepatology. 1994;19:1407–1413. [PubMed] [Google Scholar]
- 47.Muizelaar JP, Lutz HA 3rd, Becker DP. Effect of mannitol on ICP and CBF and correlation with pressure autoregulation in severely head-injured patients. J Neurosurg. 1984;61:700–706. doi: 10.3171/jns.1984.61.4.0700. [DOI] [PubMed] [Google Scholar]