Abstract
Purpose
Topotecan resistance can result from drug efflux by P-glycoprotein (Pgp) and breast cancer resistance protein (BCRP) as well as survival signals initiated by epidermal growth factor receptor family members. The present studies were done to determine the effect of combining topotecan and the dual epidermal growth factor receptor/HER2 inhibitor lapatinib in tissue culture, a murine xenograft model, and a phase I clinical trial.
Experimental Design
The effects of lapatinib on topotecan accumulation and cytotoxicity in vitro were examined in paired cell lines lacking or expressing Pgp or BCRP. Antiproliferative effects of the combination were assessed in mice bearing HER2+ BT474 breast cancer xenografts. Based on tolerability in this preclinical model, 37 patients with advanced-stage cancers received escalating doses of lapatinib and topotecan in a phase I trial.
Results
Lapatinib increased topotecan accumulation in BCRP- or Pgp-expressing cells in vitro, and the combination showed enhanced efficacy in HER2+ BT474 xenografts. In the phase I study, nausea, vomiting, diarrhea, and fatigue were dose limiting. The maximum tolerated doses were 1,250 mg/d lapatinib by mouth for 21or 28 days with 3.2 mg/m2 topotecan i.v. on days1, 8, and 15 of 28-day cycles. Pharmacokinetic analyses showed that combined drug administration resulted in decreased topotecan clearance consistent with transporter-mediated interactions. Seventeen (46%) patients had disease stabilization.
Conclusions
The lapatinib/topotecan combination is well tolerated and warrants further study.
The 4-anilinoquinazoline lapatinib is a potent and selective inhibitor of substrate phosphorylation catalyzed by the epidermal growth factor receptor (EGFR;ErbB1) and HER2 (1, 2). Lapatinib has also shown potent inhibition of growth in tumors overexpressing EGFR and/or HER2 in vitro and in vivo (1, 3, 4). Phase I trials indicated that lapatinib was well tolerated up to 1,800 mg/d, with diarrhea and rash as dose-limiting toxicities (DLT; ref. 5). Based on subsequent clinical trials, lapatinib has been approved for the treatment of trastuzumab-resistant HER2+ breast cancer in the United States (5–7).
The camptothecin derivative topotecan is a water-soluble topoisomerase I inhibitor that has activity against several human malignancies, including relapsed ovarian cancer and small cell lung cancer (8). Topotecan is well tolerated in these disorders, with neutropenia being the principal toxicity at doses above 4 mg/m2/wk (8).
Previous studies have indicated that sensitivity of tumor cells to topoisomerase I poisons can be affected by several cellular processes. For example, survival signaling initiated by receptor tyrosine kinases, such as EGFR and HER2/Neu, inhibits camptothecin- or topotecan-induced cytotoxicity (9–11), providing the rationale for current therapies that include EGFR-directed agents and irinotecan (12). In addition, drug efflux mediated by the ATP-binding cassette (ABC) transporters P-glycoprotein (Pgp;ABCB1) and breast cancer resistance protein (BCRP;ABCG2;reviewed in refs. 13–16) can affect cellular topotecan accumulation and cytotoxicity in vitro (17–22) as well as topotecan distribution in vivo (23, 24).
Constitutive Pgp expression is observed in normal colon, adrenal gland, bile duct, renal epithelium, and bone marrow stem cells, as well as in tumors derived from these tissues (25). Likewise, constitutive BCRP expression is observed in liver, kidney, brain, placenta, intestine, and colon (26) as well as cancers derived from these sites (27). Because these transporters can affect drug accumulation in cancer cells, there has been substantial interest in identifying inhibitors of these transporters and assessing their ability to modulate the efficacy of affected agents (28, 29).
Translational Relevance.
Signaling by the epidermal growth factor receptor and HER2 has previously been shown to modulate sensitivity to topoisomerase I inhibitors. In the present study, Molina et al. have examined the effects of combining the dual epidermal growth factor receptor/HER2 inhibitor lapatinib with the topoisomerase I poison topotecan in tissue culture, a murine xenograft model, and a phase I clinical trial. In cell lines that overexpress P-glycoprotein (ABCB1) or breast cancer resistance protein (ABCG2), lapatinib enhances topotecan accumulation and cytotoxicity. In a xenograft model that overexpresses HER2 but not ABCB1 or ABCG2, lapatinib enhances the antitumor efficacy of topotecan. In the phase I trial, lapatinib (1,250 mg/d for 21 or 28 days) could be safely administered with topotecan, although the maximum tolerated dose of topotecan (3.2 mg/m2/d on days 1, 8, and 15 of each 28-day cycle) was lower than the maximum tolerated dose of single-agent topotecan. Pharmacokinetic analysis suggested that lapatinib diminished clearance of topotecan by routes other than glomerular filtration. Collectively, these results not only provide new understanding of the interactions between lapatinib and topotecan but also suggest that the lapatinib/topotecan combination, which is well tolerated, warrants further clinical investigation.
Several compounds, including certain 4-anilinoquinazolines, have previously been shown to inhibit ABC transporters. In particular, our group and others have shown that the EGFR tyrosine kinase inhibitors CI-1033 and gefitinib inhibit the transport activities of BCRP and Pgp (21, 30, 31). More recent studies indicate that lapatinib is also an inhibitor of BCRP and Pgp (32). Based on these data, we examined the effect of lapatinib on topotecan accumulation and cytotoxicity in BCRP-and Pgp-expressing cell lines in vitro, assessed the tolerability and antitumor activity of lapatinib and topotecan in a murine xenograft model in vivo, and did a phase I study to evaluate the safety, tolerability, and pharmacokinetics of the lapatinib/topotecan combination in patients with advanced solid tumors.
Materials and Methods
Compounds and materials
For tissue culture studies, lapatinib and topotecan were dissolved in DMSO at 1,000 times the indicated final concentrations. For murine xenograft studies, lapatinib powder (GW572016F) was formulated in aqueous hydroxypropylmethylcellulose:Tween 80 (0.5%:0.1%) and administered orally as a suspension. Topotecan (SKF-104864-A) was dissolved in water at the required concentration before i.p. administration. For human studies, lapatinib and topotecan were standard commercially available formulations.
Murine monoclonal anti-EGFR and rabbit polyclonal anti-HER2 were purchased from Becton Dickinson and Upstate Biological. Murine monoclonal anti-lamin A and anti-heat shock protein 90 were kind gifts from Frank McKeon (Harvard Medical School, Boston, MA) and David Toft (Mayo Clinic, Rochester, MN).
Cell culture studies
Paired AuxB1 and CHRC5 Chinese hamster ovary cells that differ in Pgp expression (33) were cultured in α-MEM with ribonucleosides and deoxyribonucleosides, 10% heat-inactivated fetal bovine serum, 100 units/mL penicillin G, and 100 µg/mL streptomycin as previously described (18). MDA-MB-231 cells stably transfected with BCRP or empty vector were cultured in Iscove’s modified essential medium containing 10% heat-inactivated fetal bovine serum, 100 units/mL penicillin G, and 100 µg/mL streptomycin as previously described (21). Whole-cell lysates were prepared from logarithmically growing cells and subjected to immunoblotting as previously described (34).
To evaluate topotecan accumulation, cell lines were trypsinized, sedimented at 100 × g for 6 min, resuspended in their respective medium, and incubated with diluent or 20 µmol/L topotecan in the presence of increasing lapatinib concentrations for 20 to 30 min at 37°C. All samples contained 0.2% (v/v) DMSO. At the end of the incubation, each sample was subjected to flow microfluorimetry on a Becton Dickinson FACScan flow cytometer using an excitation wavelength of 488 nm and an emission wavelength of 585 nm as previously described (18).
To do clonogenic assays, cells were plated in 35-mm dishes, allowed to adhere overnight, treated with increasing concentrations of topotecan in the presence of diluent or lapatinib for 24 h, washed, and incubated in drug-free medium for 7 to 8 d as previously described (18, 21). Colonies were stained with Coomassie blue and manually counted.
Tumor xenografts
BT474 human breast carcinoma xenografts (1, 3) are HER2+ and do not express Pgp or BCRP. They were maintained by serial transplantation of tumor fragments in female CB-17 severe combined immunodeficient (SCID) mice (Charles River Laboratories). The research complied with national legislation and with company policy on the Care and Use of Animals as well as related codes of practice. Tumors were initiated by trocar implantation of 1 mm3 tumor fragments s.c. in the axillary region of female SCID mice. Therapy was initiated following establishment of tumors. Lapatinib was administered by oral gavage to groups of eight female mice at doses of 0 (vehicle), 30, 60, or 100 mg/kg for 21 d on a twice daily schedule with the two doses being administered 6 to 8 h apart.6 Topotecan was administered i.p., alone or concurrently with lapatinib, as a single dose on days 1, 5, and 9 (every 4 d × 3 schedule) from the initiation of therapy at doses of 6 or 10 mg/kg/d. Tumor measurements were made through the skin using electronic calipers with direct data entry into a spreadsheet format at twice weekly intervals. Tumor volume (mm3) was estimated according to the following formula: [tumor length (mm) × tumor width (mm)2] / 2. Unless otherwise indicated, % inhibition was calculated from measurements taken the day after the last treatment. Decreases in tumor volume were reported as % inhibition, calculated as 100 × [1 - (average growth of the drug-treated population / average growth of the vehicle control population)].
For each study, an analysis of covariance was fit to the tumor size of each mouse after 21 d of drug treatment [the day after the last dose of lapatinib (day 56 for study 1 and day 70 for study 2)]. The treatment group was used as the explanatory variable, and initial tumor size was used as a covariate. This type of analysis considers the initial tumor size when evaluating the effect of the treatment groups on tumor size on day 21. The analysis was done on the natural log of the tumor size on day 21 to satisfy the assumption of homoscedasticity in the analysis of covariance. Some of the treatment groups were dropped from the analyses due to toxicity or insufficient sample size. All pairwise comparisons were made across the treatment groups. As these were planned comparisons, no adjustment was made for multiple comparisons. The P values associated with the difference between treatment groups were considered significant when P < 0.05.
Patient selection
Patients with histologic or cytologic evidence of metastatic or locally advanced cancer for which there was no established curative or life-prolonging therapy were eligible for this study. Eligibility criteria also included age ≥18 y; Eastern Cooperative Oncology Group performance status ≤2; prior radiation completed at least 3 wk before study enrollment; and adequate bone marrow (platelets ≥100,000/AL, absolute neutrophil count >1,500/AL, hemoglobin ≥9 g/dL), hepatic (total bilirubin ≤2.0 times the upper limit of normal, aspartate transaminase ≤5 times normal, if liver involvement), and renal (serum creatinine ≤1.5 times the upper limit of normal) function as assessed within 1 wk of starting therapy. Other eligibility variables included an echocardiogram with an ejection fraction >50% and a life expectancy of ≥12 wk. All patients were required to give written informed consent under Federal and institutional guidelines.
Study design and treatments
This was a phase I, open-label, multiple-dose study to describe the toxicity profile and identify the maximum tolerated dose (MTD) of i.v. topotecan administered on days 1, 8, and 15 combined with lapatinib given orally for 21 d (cohort 1) or 28 d (cohort 2) of 28-d cycles. Pharmacokinetic analyses were done to quantify any observed interactions between the two agents.
Cohort 1 used a standard cohort of three design (35) evaluating escalating oral doses of 750, 1,000, and 1,250 mg/d of lapatinib for 21 d and i.v. doses of 2.4, 3.2, and 4.0 mg/m2 topotecan on days 1, 8, and 15 of each 28-d cycle. The incidence and severity of adverse events were evaluated and coded according to the National Cancer Institute Common Toxicity Criteria (version 3.0). Response to therapy was determined using a modified Response Evaluation Criteria in Solid Tumors (36). All objective responses were required to be confirmed 4 wk later. The MTD was defined as the dose level below the lowest dose level that induced DLT in at least one third of patients (at least two of a maximum of six new patients) with three patients treated at a given dose level combination and observed for at least 4 wk to assess toxicity. DLT was defined as an adverse event during cycle 1 attributed (possibly, probably, or definitely related) to the study treatment that included grade 4 neutropenia of >5 d of duration; platelets <25,000/AL; hemoglobin <6.5 g/dL; serum creatinine >2 times baseline; grade 3 nausea, vomiting, or diarrhea despite maximal supportive treatment; any other grade 3 nonhematologic event; any grade 4 laboratory abnormality; and any persistent adverse event that resulted in dose delays after the first cycle, even if the event was not grade 3 in severity.
Cohort 2 used a similar cohort of three design evaluating escalating doses of 1,000 and 1,250 mg/d of lapatinib for 28 d and doses of 3.2 mg/m2 of topotecan i.v. given on days 1, 8, and 15 of each 28-d cycle. An additional 10 patients were treated at the MTD of this cohort to more completely evaluate the safety and tolerability.
Pharmacokinetic analysis
During cycle 1 only, lapatinib was delayed until day 2 to allow pharmacokinetic analyses. Blood samples for topotecan were collected into prechilled heparinized tubes before drug administration and 0.25, 0.5, 0.75, 1.0, 2, 4, 6, 8, 12, and 24 h after beginning the infusion on days 1 and 8. Plasma was isolated by centrifugation (4,000 × g for 5 min) at 4°C. Topotecan plasma concentrations were measured after protein precipitation and extraction into acetonitrile by liquid chromatography-tandem mass spectrometry using a TurboIonSpray Interface with multiple reaction monitoring. The method was sensitive (50 pg/mL), precise (within 7%), and accurate (within 15%). Blood samples for lapatinib were collected in tubes containing EDTA 0.25, 0.5, 1, 1.5, 2, 2.5, 3, 4, 6, 8, 12, 16, and 24 h after administering the oral dose on days 7 and 8. Plasma was isolated by centrifugation (1,000 × g for 10 min). Plasma samples were stored at −70°C until analyzed. Lapatinib plasma concentrations were measured using a previously published liquid chromatography-tandem mass spectrometry method (37) with a sensitivity of 5 ng/mL lapatinib, precision within 15%, and accuracy within 15% of nominal.
Topotecan and lapatinib plasma concentration-time data were analyzed by noncompartmental methods using the program WinNonlin version 4.1 (Pharsight Corp.). The apparent terminal elimination rate constants (kz) were determined by linear least-squares regression through the terminal linear portion of the graph of the log plasma concentration versus time. The apparent elimination half-life (t1/2) was calculated as 0.693/kz. Areas under the plasma concentration-time curves (AUC) were determined using the linear trapezoidal rule from time zero to the time of the last detectable sample (Clast). AUCs through infinite time (AUC0-∞) were calculated by adding the value Clast/kz to AUC(0-t). Topotecan plasma clearance (CLp) was calculated as dose/AUC0-∞. Maximum observed plasma concentration (Cmax) and the time to reach maximum plasma concentration (Tmax) for each patient were derived from the plasma concentration-time profile. Clearance of topotecan by mechanisms other than renal glomerular filtration (CLNRF) was calculated by subtracting creatinine clearance (CLCR) from CLp. CLCR was calculated by the Cockcroft-Gault method. Pharmacokinetic variables were compared between treatments by ANOVA (SAS). The statistical significance of each comparison was determined by the deviation from inclusion of 1.00 in the 90% confidence limits for the mean of all individual treatment ratios.
Results
Cell culture studies
Previous studies have shown that topotecan is effluxed from cells by Pgp and BCRP. In view of results showing that other 4-anilinoquinazoline – based EGFR inhibitors can modulate these transporters, we examined the effects of lapatinib on intracellular topotecan accumulation and cytotoxicity in paired cell lines differing in BCRP or Pgp expression. These studies used MDA-MB-231 cells stably transfected with empty vector or BCRP (21) as well as AuxB1 and its Pgp-overexpressing derivative CHRC5 (18, 33). Earlier studies not only documented transporter overexpression in the MDA-MB-231/BCRP and CHRC5 lines but also showed low but detectable transporter expression in the MDA-MB-231/empty vector and AuxB1 cells (18, 21). In the context of the studies described below, these cell lines were also assayed for EGFR and HER2 expression (Supplementary Fig. S1). Consistent with earlier reports (38, 39), the MDA-MB-231–derived clones expressed very low levels of EGFR and HER2 compared with cell lines with EGFR overexpression or HER2 amplification. Likewise, in accord with earlier studies (40, 41), the Chinese hamster ovary–derived cell lines expressed only low levels of HER2 and undetectable levels of EGFR.
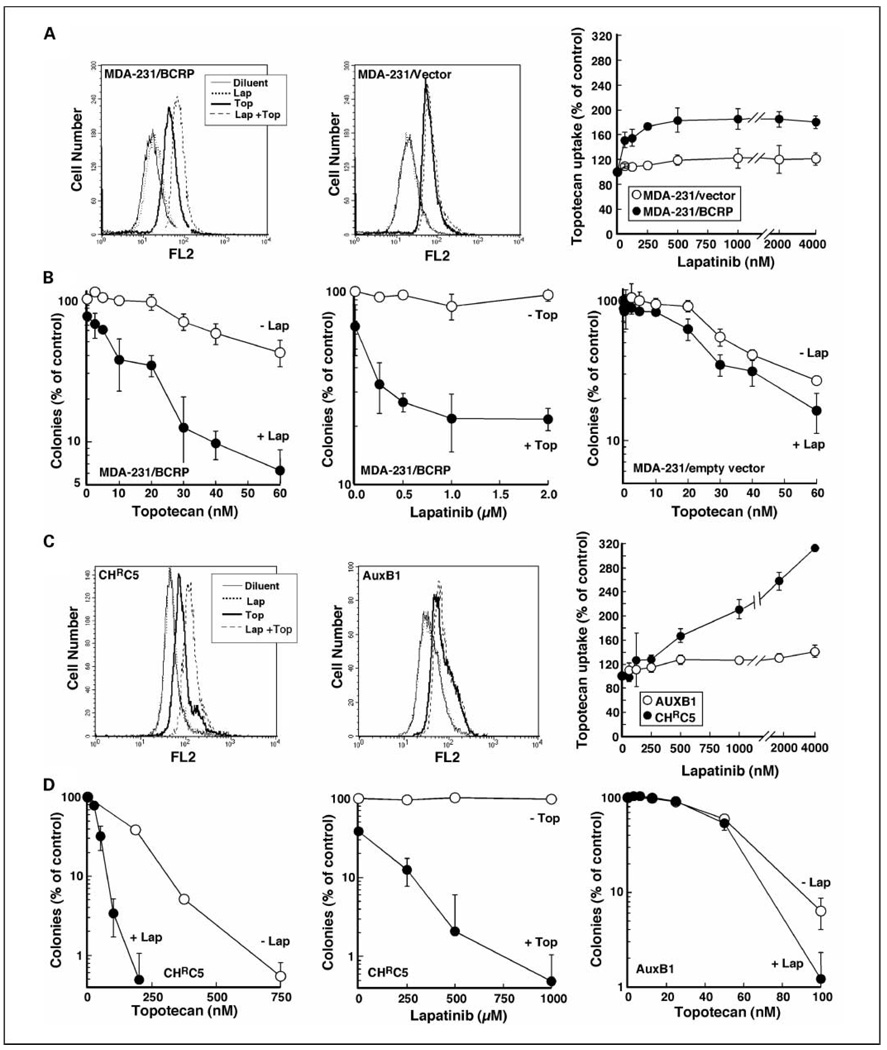
To assess whether lapatinib affects BCRP-mediated topotecan efflux, MDA-MB-231/BCRP and MDA-MB-231/empty vector cells were incubated with topotecan in the presence of diluent or lapatinib (Fig. 1A). Analysis of topotecan accumulation by flow cytometry showed that lapatinib increased topotecan steady-state accumulation in BCRP-expressing cells (Fig. 1A, left). In particular, the increase in intracellular topotecan was half-maximal at 250 nmol/L lapatinib (Fig. 1A, right). At 1,000 nmol/L lapatinib, steady-state intracellular topotecan was 190 ± 20% (mean ± SD, n = 4) of accumulation in the absence of lapatinib. Consistent with these results, clonogenic assays done after exposure of cells to one or both drugs simultaneously for 24 hours revealed that lapatinib enhanced the antiproliferative effects of topotecan in MDA-MB-231/BCRP cells (Fig. 1B, left), with half-maximal effects at 250 nmol/L lapatinib (Fig. 1B, middle). In contrast, lapatinib had little effect on intracellular topotecan (Fig. 1A, middle) or topotecan-induced inhibition of colony formation (Fig. 1B, right) in MDA-MB-231 cells transfected with the empty vector.
Fig. 1.
Lapatinib enhances topotecan uptake and cytotoxicity in tumor cells overexpressing BCRP or Pgp. A and C, left, after cells that overexpress BCRP (MDA-MB-231/BCRP) or Pgp (CHRC5) were incubated with DMSO,1 µmol/L lapatinib (Lap) in DMSO, topotecan (Top) in DMSO, or lapatinib and topotecan (Lap + Top) simultaneously for 20 to 30 min, topotecan accumulation was assayed by flow microfluorimetry. All samples contained 0.2% (v/v) DMSO. Middle, cells that express lower endogenous levels of BCRP (MDA-MB-231/empty vector) or Pgp (AuxB1) were used as controls. Right, summary of results as a function of lapatinib concentration. The values shown were corrected by subtracting the minimal fluorescence attributable to lapatinib at the corresponding concentrations. Points, mean of three independent experiments; bars, SD. B and D, left, after treatment for 24 h with the indicated concentration of topotecan or diluent in the presence or absence of1 µmol/L lapatinib, cells were washed and allowed to form colonies. Middle, ABC transporter-overexpressing cells were treated for 24 h with varying concentrations of lapatinib in the presence or absence of 40 nmol/L topotecan (B, middle) or 200 nmol/L topotecan (D, middle) and then assayed for colony formation. Right, MDA-MB-231/empty vector (B, right) orAuxB1cells (D, right) were treated for 24 h with the indicated concentration of topotecan or diluent in the presence or absence of 1 µmol/L lapatinib, washed, and allowed to form colonies. Points, mean of triplicate plates; bars, SD. Similar results were observed in three independent experiments.
Additional experiments examined the effect of lapatinib on topotecan action in paired cell lines expressing different amounts of Pgp (33). These studies showed that 1,000 nmol/L lapatinib increased intracellular topotecan in CHRC5 cells, which express high levels of Pgp, to 220 ± 20% (n = 3) of the steady-state accumulation observed in the absence of lapatinib (Fig. 1C, left and right). The effects were more modest in AuxB1 cells (Fig. 1C, middle), which express lower levels of Pgp (33). In agreement with these results, lapatinib also enhanced the antiproliferative effects of topotecan in colony-forming assays in CHRC5 cells (Fig. 1D, left and middle) much more than in AuxB1 cells (Fig. 1D, right).
Collectively, these results show that lapatinib is able to enhance topotecan accumulation in cells that overexpress BCRP or Pgp. In addition, lapatinib enhances the antiproliferative effects of topotecan in these cells, possibly reflecting effects on the endogenously expressed EGFR and HER2 as well as topotecan uptake.
Animal studies
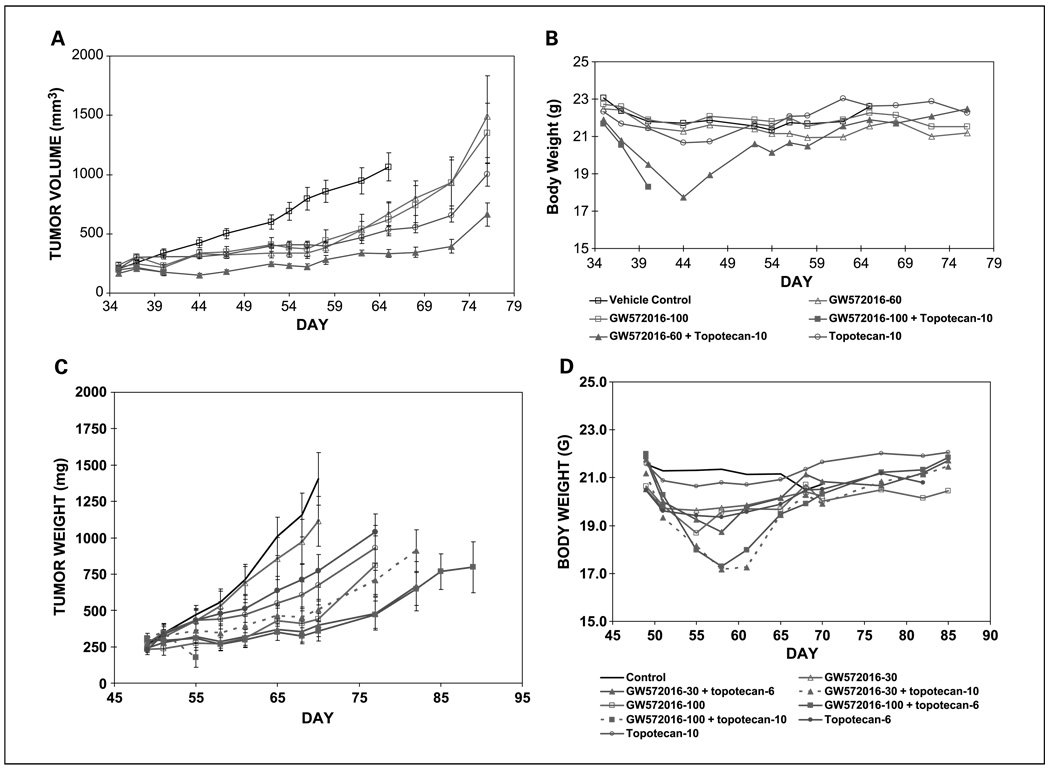
To assess the effects of the lapatinib/topotecan combination in vivo, mice bearing HER2+ BT474 breast adenocarcinoma xenografts, a model previously shown to be responsive to lapatinib (1,3), were treated orally with lapatinib for 21 days in conjunction with i.p. topotecan on every 4 days × 3 schedule. Twice daily oral administration of lapatinib resulted in inhibition of BT474 tumor growth after 21 days of treatment (day 56: 79% at 60 mg/kg and 77% at 100 mg/kg of lapatinib in study 1;day 70: 26% at 30 mg/kg and 82% at 100 mg/kg in study 2; Fig. 2A and C, respectively). Modest inhibition of tumor growth was also observed in mice treated with topotecan alone (66% at 10 mg/kg in study 1 and 53% and 65% at 6 and 10 mg/kg, respectively, in study 2). In study 1, mice receiving 100 mg/kg lapatinib and 10 mg/kg topotecan concomitantly died during the first 2 weeks of treatment, showing that full doses of both agents were not tolerable. Mice treated with 60 mg/kg lapatinib and 10 mg/kg topotecan showed maximum body weight loss of 19.1% (Fig. 2B) and had significant tumor growth inhibition relative to topotecan alone (Fig. 2A). In study 2, mice treated with 100 mg/kg lapatinib and 6 mg/kg topotecan had a maximum body weight loss of 21%, whereas mice treated with 30 mg/kg lapatinib and 6 mg/kg topotecan had a maximum body weight loss of 13.9% (Fig. 2D). Both combinations had significantly greater tumor growth inhibition than either agent alone (Fig. 2C). Two mice treated with 30 mg/kg lapatinib and 10 mg/kg topotecan died within the first 2 weeks of treatment (days 12 and 13). Tumor growth inhibition for the remaining six mice was significant compared with lapatinib alone after 21 days of treatment (Fig. 2D).
Fig. 2.
Lapatinib enhances the antitumor effects and toxicity of topotecan in vivo. CB-17 SCID mice bearing BT474 human breast cancer xenografts were treated with the indicated doses of topotecan alone (i.p. on every 4 d × 3 schedule) or in combination with oral lapatinib as indicated in Materials and Methods. A and C, estimated tumor volumes. B and D, columns, mean weights in groups of eight mice subjected to each treatment; bars, SD.
Phase I study results
In view of these potentially promising preclinical results, a phase I clinical trial of the lapatinib/topotecan combination was done. Thirty-seven patients enrolled in two cohorts (Table 1) received an overall median of 2 (range, 1–20) courses of therapy at six different dose levels (Table 2). The median age of study participants was 56 years (range, 33–74). Overall, 73% of patients were female. Most patients were relatively asymptomatic from their cancers, with 51% and 41% having Eastern Cooperative Oncology Group performance status of 0 and 1, respectively. Tumor types included melanoma and sarcoma as well as renal cell, ovarian, lung, pancreatic, stomach, esophageal, and salivary gland carcinomas.
Table 1.
Patient characteristics
| Variable, n (%) | Cohort 1 (n = 18) | Cohort 2 (n = 19) | Overall (N = 37) |
|---|---|---|---|
| Age, median (range) | 55 (33–74) | 60 (35–74) | 56 (33–74) |
| No. cycles received, median (range) | 2 (1–6) | 3 (1–20) | 2 (1–20) |
| Gender | |||
| Female | 10 (55.6%) | 17 (89.5%) | 27 (73%) |
| Male | 8 (44.4%) | 2 (10.5%) | 10 (27%) |
| Performance score | |||
| 0 | 9 (50.0%) | 10 (52.6%) | 19 (51.4%) |
| 1 | 7 (38.9%) | 8 (42.1%) | 15 (40.5%) |
| 2 | 2 (11.1%) | 1 (5.3%) | 3 (8.1%) |
Table 2.
Dose escalation and occurrence of DLTs
| Dose level | Lapatinib (mg) | Topotecan (mg/m2) | No. patients | No. DLTs |
|---|---|---|---|---|
| Cohort 1 | ||||
| 0* | 750 | 2.4 | 3 | 0 |
| 1 | 750 | 3.2 | 3 | 0 |
| 2 | 1,000 | 3.2 | 3 | 0 |
| 3 | 1,250 | 3.2 | 6 | 1 |
| 4 | 1,250 | 4.0 | 3 | 2 |
| Cohort 2 | ||||
| 0* | 1,000 | 3.2 | 3 | 0 |
| 1 | 1,250 | 3.2 | 6 | 0 |
Starting dose level.
Adverse events
All 37 patients were evaluable for analysis of toxicity. Adverse events for cohort 1 were mild through dose level 2. At dose level 3, one patient with a disease progression–associated decrease in renal function experienced grade 4 neutropenic fever after topotecan administration. No other potential DLTs were observed in five additional patients at this dose level. At dose level 4, two patients experienced a DLT (one grade 3 diarrhea and one grade 3 nausea and vomiting). Accordingly, the MTD for cohort 1 was dose level 3, which consisted of 1,250 mg lapatinib orally four times daily for 21 days and 3.2 mg/m2 topotecan i.v. on days 1, 8, and 15 of each 28-day cycle. The MTD for cohort 2 was dose level 1, which consisted of 1,250 mg lapatinib orally four times daily for 28 days and 3.2 mg/m2 topotecan i.v. on days 1, 8, and 15 of each 28-day cycle. When no DLTs were observed in the initial 9 patients of cohort 2 during the dose escalation, an additional 10 patients were enrolled at the MTD. Although no grade 4 events were observed in this expansion cohort, there were 14 grade 3 treatment-related events in six patients (2 dehydration, 2 diarrhea, 4 nausea, 2 vomiting, 1 leukopenia, 1 thrombocytopenia, 1 neutropenia, and 1 fatigue).
The cycle 1 and total treatment-related grade 3 and 4 adverse events are summarized in Table 3. The most common nonhematologic events were fatigue (13%), diarrhea (11%), nausea (11%), and emesis (8%). The diarrhea and the nausea and vomiting resolved quickly and completely with standard anti-diarrheal and anti-emetic therapy, respectively. The MTD and recommended phase II dose of the combination is 1,250 mg/d lapatinib for 28 days and 3.2 mg/m2 topotecan i.v. on days 1, 8, and 15 of a 28-day cycle.
Table 3.
All cycles grade 3/grade 4 adverse events at least possibly related to treatment
| Patients with at least one |
Cycle 1, n (%)* |
All cycles, n (%)* |
|---|---|---|
| Any grade 3+ toxicity | 13 (34.2%) | 16 (42.1%) |
| Any grade 4+ toxicity | 1 (2.6%) | 1 (2.6%) |
| Grade 3+ heme toxicity | 5 (13.2%) | 6 (15.8%) |
| Grade 4+ heme toxicity | — | — |
| Grade 3+ nonheme toxicity | 9 (23.7%) | 11 (28.9%) |
| Grade 4+ nonheme toxicity | 1 (2.6%) | 1 (2.6%) |
| Toxicities† | Grade 3 | Grade 4 | Grade 3 | Grade 4 |
|---|---|---|---|---|
| Hematologic | ||||
| Neutropenia | 3 (7.9%) | 5 (13.2%) | ||
| Leukopenia | 2 (5.3%) | 2 (5.3%) | ||
| Anemia | 1 (2.6%) | |||
| Thrombocytopenia | 2 (5.3%) | 2 (5.3%) | ||
| Nonhematologic | ||||
| Dehydration | 2 (5.3%) | 2 (5.3%) | ||
| Rash | 1 (2.6%) | 1 (2.6%) | ||
| Diarrhea | 3 (7.9%) | 4 (10.5%) | ||
| Fatigue | 4 (10.5%) | 5 (13.2%) | ||
| Febrile neutropenia | 1 (2.6%) | 1 (2.6%) | ||
| Nausea | 4 (10.5%) | 4 (10.5%) | ||
| Vomiting | 3 (7.9%) | 3 (7.9%) |
Out of a total of 37 patients evaluable for toxicity.
The same patient could have multiple toxicities.
Antitumor activity
The median number of cycles administered was 2 (range, 1–6) in cohort 1 and 3 (range, 1–20) in cohort 2. Eight patients (44.4%) in cohort 1 and nine (47%) in cohort 2 had stable disease lasting for a median of 2 cycles after being initially documented (range, 1–18 cycles).
Pharmacokinetic analysis
Eleven patients participated in pharmacokinetic studies. Data from two patients, however, were excluded from analysis of lapatinib pharmacokinetics because one withdrew before completing the day 7 and 8 assessments and another had uninterpretable data secondary to deteriorating health status. Two patients were excluded from analysis of topotecan pharmacokinetics due to absence of plasma concentration data on day 8. Pharmacokinetic variables for topotecan and lapatinib, following administration of each drug alone and both drugs together, are summarized in Table 4.
Table 4.
Summary of topotecan and lapatinib pharmacokinetics
| Drug | Topotecan alone (day 1)* | Lapatinib + topotecan (day 8)* | Day 8:day 1 ratio† |
|---|---|---|---|
| Topotecan (n = 9) | |||
| Cmax (ng/mL) | 162 (146–178) | 128 (102–154) | 0.79 (0.66–0.92) |
| AUC0–24 h (h·ng/mL) | 432 (329–535) | 510 (323–697) | 1.18 (1.07–1.29) |
| CLp (L/h/m2) | 7.28 (5.35–8.91) | 6.14 (4.27–8.01) | 0.84 (0.76–0.92) |
| CLNRF (L/h/m2) | 5.25 (3.99–6.51) | 4.11 (2.72–5.50) | 0.78 (0.68–0.88) |
| t1/2 (h) | 4.30 (4.09–4.51) | 4.35 (3.96–4.74) | 1.01 (0.96–1.06) |
| Vss (L/m2) | 30.5 (26.5–34.5) | 30.1(23.9–36.3) | 0.99 (0.90–1.08) |
| Lapatinib alone (day 7)* | Lapatinib + topotecan (day 8)* | Day 8:day 7 ratio† | |
| Lapatinib (n = 9) | |||
| Cmax (µg/mL) | 1.89 (1.33–2.68) | 2.33 (1.78–3.05) | 1.24 (1.00–1.52) |
| Tmax (h) | 3.00 (2.59–8.00)‡ | 4.00 (1.50–12.0)‡ | 0.25 (−4.00 to 9.00)§ |
| AUC0–24 h (h·µg/mL) | 23.3 (14.5–37.3) | 31.7 (22.6–44.5) | 1.36 (1.04–1.78) |
Geometric mean and 95% confidence intervals unless otherwise indicated.
Geometric least squares mean ratio and 90% confidence intervals unless otherwise indicated.
Median and range.
Median and range of pairwise differences.
Topotecan pharmacokinetics were altered to a small but statistically significant extent when administered with lapatinib. Topotecan AUC0–24 h increased by 18% (7–29%) in the presence of lapatinib. Lapatinib had no effect on topotecan t1/2 or Vss, consistent with the increase in AUC being due to a decrease in CLp. The geometric mean CLp was 7.28 L/h/m2 when topotecan was administered alone on day 1 and 6.14 L/h/m2 when topotecan was administered with lapatinib on day 8. This small (16%) but statistically significant decrease in CLp was further assessed by estimating the partial clearance of topotecan by mechanisms other than renal filtration, CLNRF. Assuming that glomerular filtration rate was not altered by lapatinib, estimated values of CLNRF suggested a small statistically significant decrease of 22% (12–32%) when topotecan was administered with lapatinib. CLNRF was 72% of CLp when topotecan was administered alone but reduced to 66% of CLp when topotecan and lapatinib were administered together. Ratios of topotecan CLNRF in the presence of lapatinib to CLNRF in the absence of lapatinib were fit to a competitive inhibition model based on the Dixon (42) equation, CLNRF ratio = 1 / (1 + Ci / Ki), where Ci = concentration of inhibitor (lapatinib steady-state Cmin) and Ki = the inhibitory constant (lapatinib concentration producing 50% inhibition). The results displayed in Supplementary Fig. S2 indicated a Ki of 2,349 ng/mL (±35%) or 4 µmol/L.
There was also a trend toward higher lapatinib concentrations in the presence of topotecan. The geometric mean Cmax was 1.89 µg/mL 3 hours following the 1,250 mg dose of lapatinib administered alone on day 7 and 2.33 µg/mL 4 hours after administration with topotecan on day 8. Mean lapatinib AUC0–24 h was also higher when administered with topotecan than with lapatinib alone (31.7 versus 23.3 h·µg/mL). However, these differences were not significant, and there was no apparent relationship to topotecan dose or concentration.
Discussion
In the present study, we report the effects of combining topotecan and lapatinib in preclinical experiments and in a phase I clinical study in patients with advanced solid tumors. The preclinical studies suggest that lapatinib enhances the efficacy of topotecan by at least two mechanisms. The phase I study, which to our knowledge is the first report of a clinical trial examining the effect of a 4-anilinoquinazoline tyrosine kinase inhibitor on topotecan tolerability and pharmacokinetics in vivo, shows that coadministration of topotecan and lapatinib is feasible in the clinical setting.
In the preclinical studies, lapatinib increased topotecan steady-state accumulation in cell lines overexpressing either BCRP or Pgp but not in cells with low endogenous levels of BCRP or Pgp (Fig. 1A and C). This observation was consistent with recently published data indicating that lapatinib is a substrate and inhibitor of both Pgp and BCRP at clinically achievable concentrations (32). Thus, lapatinib joins other 4-anilinoquinazoline tyrosine kinase inhibitors, including CI-1033 and gefitinib, as modulators of ABC transporter action.
In further experiments, lapatinib also enhanced the antiproliferative effects of topotecan in colony-forming assays (Fig. 1B and D). This enhancement was greater in cells that express higher levels of BCRP or Pgp (Fig. 1B and D, left versus right), suggesting that the ability of lapatinib to increase topotecan accumulation is likely playing a role. Previous studies showing that survival signaling initiated by receptor tyrosine kinases such as EGFR and HER2 inhibits camptothecin- or topotecan-induced cytotoxicity (9–11), coupled with our observation of low levels of EGFR or HER2 in the cell lines used for these studies (Supplementary Fig. S1), raised the possibility that inhibition of signaling by EGFR and HER2 is also contributing to the enhanced antiproliferative effects of the combination in vitro.
In a parallel series of experiments, the effects of the lapatinib/topotecan combination were examined in SCID mice bearing BT474 HER2+ tumor xenografts. This combination exhibited toxicity at high doses in the mouse studies (Fig. 2B and D), suggesting that it might not be possible to administer both agents together at full doses in the clinical setting. However, decreasing the topotecan dose from 10 mg/kg to 6 mg/kg decreased the toxicity, and the combination with either 100 or 30 mg/kg of lapatinib6 had significantly greater tumor growth inhibition than either agent alone (Fig. 2A and C). Because the BT474 cells do not express Pgp or BCRP, the efficacy of the combination in the xenograft studies likely reflects the effect of inhibiting HER2 signaling that can impede topotecan action.
In the ensuing phase I study, the combination of lapatinib and topotecan in patients with advanced solid tumors was well tolerated, with only mild toxicities in the form of diarrhea, nausea, vomiting, and one episode of neutropenic fever. We recommend a phase II dose of 1,250 mg lapatinib orally once daily for 28 days and 3.2 mg/m2 topotecan i.v. on days 1, 8, and 15 of a 28-day cycle.
In this study, higher systemic exposure to topotecan was observed when the two drugs were administered together compared with topotecan alone (Table 4). The observation of higher systemic topotecan exposure when the two drugs were administered together provides a plausible explanation for the lower tolerated doses of topotecan when administered with lapatinib (3.2 mg/m2/wk topotecan × 3 in the combination compared with a MTD of 4 mg/m2/wk × 3 for topotecan alone). Higher systemic topotecan exposure in the combination is consistent with reduced topotecan clearance in the presence of lapatinib and likely reflects inhibition of topotecan transporters by lapatinib. In this context, it is interesting to note that one of the patients in this study whose participation was halted due to a decline in renal function exhibited the greatest decrease in topotecan clearance in the presence of lapatinib. Despite the long washout time between these unrandomized assessments of topotecan pharmacokinetics relative to topotecan half-life, the potential for a carryover effect cannot be excluded, and these exploratory findings deserve further evaluation in a randomized study.
The affinity of lapatinib and topotecan for the same transporters provides a mechanism for the observed pharmacokinetic interaction. Clearance of topotecan seems to occur primarily through two mechanisms: biliary secretion (43), which may involve BCRP and Pgp, and renal excretion, which may involve OAT3 or Pgp (44). Each of these transporters has been found to be inhibited by lapatinib (32). As indicated in Table 4, lapatinib seemed to decrease the clearance of topotecan by mechanisms other than renal glomerular filtration, which may include renal tubular secretion and biliary secretion, both of which are transporter-mediated processes. Analysis of these data (Supplementary Fig. S1) indicated an inhibitory constant (Ki) nearly identical to the 2,300 ng/mL (3.9 µmol/L) in vitro Ki for lapatinib inhibition of Pgp (32), suggesting that inhibition of this transporter was the predominant mechanism of altered topotecan clearance. Lapatinib has also been found to inhibit OAT3 but at concentrations an order of magnitude higher (32). BCRP, which is likewise expressed in the kidney (45), is inhibited at lower concentrations of lapatinib (in vitro Ki, 14 ng/mL, 0.025 µmol/L) but is also present in lower abundance relative to Pgp. Therefore, the observed effects on topotecan clearance seem to be primarily due to lapatinib-mediated Pgp inhibition. The extent to which this inhibition affected biliary versus renal clearance of topotecan could not be determined from these data, as the relative contributions of Pgp to these routes are incompletely understood, and urinary recovery of topotecan was not measured in the present study. The apparently inconsistent decrease in topotecan Cmax might be due to its insensitivity to changes in CLp and its sensitivity to infusion rate. Although lapatinib concentrations also seemed to be higher in the presence of topotecan, this difference was marginally significant and is unlikely to reflect transporter inhibition by topotecan, which was present at molar concentrations 10-fold lower than lapatinib.
In this phase I clinical trial, stable disease was observed in 46% of patients. This stable disease lasted a median of 2 cycles after documentation (range, 1–18). Phase II studies are required to better evaluate the clinical utility of this combination.
In summary, this study showed a very manageable safety and tolerability profile of lapatinib and topotecan in combination at less than single-agent MTDs to accommodate the inhibitory effect of lapatinib on topotecan transport by ABC transporters. Based on the tolerability of this regimen and its favorable effects in vivo, a phase II trial of this combination in patients with ovarian cancer is in progress.
Acknowledgments
We thank Brenda Hippert, Lorelei Hanson, Diane Doty, Jill Piens, Martha Joy, and the Mayo Clinical Research Unit staff for their contributions to the clinical trial; Barry Keith, Doris Murray, Teresa Hopper, and James Onori for the in vivo xenograft studies; Buffy Hudson-Curtis for the statistics for the in vivo studies; Paula Schneider, Kevin Peterson, and the staff of the Mayo Clinic Flow Cytometry and Optical Morphology Shared Resource for the tissue culture studies; and Deb Strauss in preparing the manuscript.
Grant support: GlaxoSmithKline, R01 CA73709 (S.H. Kaufmann), and P30 CA15083.
Footnotes
Note: Supplementary data for this article are available at Clinical Cancer Research Online (http://clincancerres.aacrjournals.org/).
These doses in mice have been shown to produce exposures comparable with those in patients at therapeutic doses. In particular, mice dosed orally twice daily at 30, 60, and 100 mg/kg of lapatinib display AUC of 5, 29, and 94 h·µg/mL, and Cmax of 1, 4, and 9 µg/mL, respectively. At the approved human therapeutic dose of 1,250 mg four times daily, AUC ranges from 23 to 56 µg/mL and Cmax from1 to 4 µg/mL.
Disclosure of Potential Conflicts of Interest
S.D. Rubin, R. Friedman, K.M. Koch, T.M. Gilmer, R.J. Mullin, and R.C. Jewell are employed by GlaxoSmith Kline.
References
- 1.Rusnak DW, Lackey K, Affleck K, et al. The effects of the novel, reversible epidermal growth factor receptor/ErbB-2 tyrosine kinase inhibitor, GW2016, on the growth of human normal and tumor-derived cell lines in vitro and in vivo. Mol Cancer Ther. 2001;1:85–94. [PubMed] [Google Scholar]
- 2.Moy B, Kirkpatrick P, Kar S, Goss P. Lapatinib. Nat Rev Drug Discov. 2007;6:431–432. doi: 10.1038/nrd2332. [DOI] [PubMed] [Google Scholar]
- 3.Konecny GE, Pegram MD, Venkatesan N, et al. Activity of the dual kinase inhibitor lapatinib ( GW572016) against HER-2-overexpressing and trastuzumab-treated breast cancer cells. Cancer Res. 2006;66:1630–1639. doi: 10.1158/0008-5472.CAN-05-1182. [DOI] [PubMed] [Google Scholar]
- 4.Rusnak DW, Alligood KJ, Mullin RJ, et al. Assessment of epidermal growth factor receptor (EGFR, ErbB1) and HER2 (ErbB2) protein expression levels and response to lapatinib (Tykerb, GW572016) in an expanded panel of human normal and tumour cell lines. Cell Prolif. 2007;40:580–594. doi: 10.1111/j.1365-2184.2007.00455.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moy B, Goss PE. Lapatinib: current status and future directions in breast cancer. Oncologist. 2006;11:1047–1057. doi: 10.1634/theoncologist.11-10-1047. [DOI] [PubMed] [Google Scholar]
- 6.Mayer EL, Lin NU, Burstein HJ. Novel approaches to advanced breast cancer: bevacizumab and lapatinib. J Natl Compr Canc Netw. 2007;5:314–323. doi: 10.6004/jnccn.2007.0026. [DOI] [PubMed] [Google Scholar]
- 7.Higa GM, Abraham J. Lapatinib in the treatment of breast cancer. Expert Rev Anticancer Ther. 2007;7:1183–1192. doi: 10.1586/14737140.7.9.1183. [DOI] [PubMed] [Google Scholar]
- 8.Sparreboom A, Zamboni WC. Chabner BA, Longo DL. Cancer chemotherapy and biotherapy. 4th ed. Lippincott Williams & Wilkins; 2006. Topoisomerase I-targeting drugs; pp. 371–413. [Google Scholar]
- 9.Ciardiello F, Bianco R, Damiano V, et al. Antitumor activity of sequential treatment with topotecan and anti-epidermal growth factor receptor monoclonal antibody C225. Clin Cancer Res. 1999;5:909–916. [PubMed] [Google Scholar]
- 10.Ciardiello F, Caputo R, Bianco R, et al. Antitumor effect and potentiation of cytotoxic drugs activity in human cancer cells by ZD-1839 (Iressa), an epidermal growth factor receptor-selective tyrosine kinase inhibitor. Clin Cancer Res. 2000;6:2053–2063. [PubMed] [Google Scholar]
- 11.Knuefermann C, Lu Y, Liu B, et al. HER2/PI-3K/Akt activation leads to a multidrug resistance in human breast adenocarcinoma cells. Oncogene. 2003;22:3205–3212. doi: 10.1038/sj.onc.1206394. [DOI] [PubMed] [Google Scholar]
- 12.Vokes EE, Chu E. Anti-EGFR therapies: clinical experience in colorectal, lung, and head and neck cancers. Oncology (Huntingt) 2006;20:15–25. [PubMed] [Google Scholar]
- 13.Ling V. Multidrug resistance: molecular mechanisms and clinical relevance. Cancer Chemother Pharmacol. 1997;40 Suppl:S3–S8. doi: 10.1007/s002800051053. [DOI] [PubMed] [Google Scholar]
- 14.Kruh GD, Belinsky MG. The MRP family of drug efflux pumps. Oncogene. 2003;22:7537–7552. doi: 10.1038/sj.onc.1206953. [DOI] [PubMed] [Google Scholar]
- 15.Doyle LA, Ross DD. Multidrug resistance mediated by the breast cancer resistance protein BCRP (ABCG2) Oncogene. 2003;22:7340–7358. doi: 10.1038/sj.onc.1206938. [DOI] [PubMed] [Google Scholar]
- 16.Szakacs G, Paterson JK, Ludwig JA, Booth-Genthe C, Gottesman MM. Targeting multidrug resistance in cancer. Nat Rev Drug Discov. 2006;5:219–234. doi: 10.1038/nrd1984. [DOI] [PubMed] [Google Scholar]
- 17.Chen AY, Yu C, Potmesil M, Wall ME, Wani MC, Liu LF. Camptothecin overcomes mdrl-mediated resistance in human KB carcinoma cells. Cancer Res. 1991;51:6039–6044. [PubMed] [Google Scholar]
- 18.Hendricks CB, Rowinsky EK, Grochow LB, Donehower RC, Kaufmann SH. Effect of P-glycoprotein expression on the accumulation and cytotoxicity of topotecan (SK&F 104864), a new camptothecin analogue. Cancer Res. 1992;52:2268–2278. [PubMed] [Google Scholar]
- 19.Maliepaard M, van Gastelen MA, de Jong LA, et al. Overexpression of the BCRP/MXR/ABCP gene in a topotecan-selected ovarian tumor cell line. Cancer Res. 1999;59:4559–4563. [PubMed] [Google Scholar]
- 20.Brangi M, Litman T, Ciotti M, et al. Camptothecin resistance: role of the ATP-binding cassette (ABC), mitoxantrone-resistance half-transporter (MXR), and potential for glucuronidation in MXR-expressing cells. Cancer Res. 1999;59:5938–5946. [PubMed] [Google Scholar]
- 21.Erlichman C, Boerner SA, Hallgren CG, et al. The HER tyrosine kinase inhibitor CI1033 enhances cytotoxicity of 7-ethyl-10-hydroxycamptothecin and topotecan by inhibiting breast cancer resistance protein-mediated drug efflux. Cancer Res. 2001;61:739–748. [PubMed] [Google Scholar]
- 22.Maliepaard M, van Gastelen MA, Tohgo A, et al. Circumvention of breast cancer resistance protein (BCRP)-mediated resistance to camptothecins in vitro using non-substrate drugs or the BCRP inhibitor GF120918. Clin Cancer Res. 2001;7:935–941. [PubMed] [Google Scholar]
- 23.Zhuang Y, Fraga CH, Hubbard KE, et al. Topotecan central nervous system penetration is altered by a tyrosine kinase inhibitor. Cancer Res. 2006;66:11305–11313. doi: 10.1158/0008-5472.CAN-06-0929. [DOI] [PubMed] [Google Scholar]
- 24.de Vries NA, Zhao J, Kroon E, Buckle T, Beijnen JH, van Tellingen O. P-glycoprotein and breast cancer resistance protein: two dominant transporters working together in limiting the brain penetration of topotecan. Clin Cancer Res. 2007;13:6440–6449. doi: 10.1158/1078-0432.CCR-07-1335. [DOI] [PubMed] [Google Scholar]
- 25.Goldstein LJ, Galski H, Fojo A, et al. Expression of a multidrug resistance gene in human cancers. J Natl Cancer Inst. 1989;81:116–124. doi: 10.1093/jnci/81.2.116. [DOI] [PubMed] [Google Scholar]
- 26.Maliepaard M, Scheffer GL, Faneyte IF, et al. Subcellular localization and distribution of the breast cancer resistance protein transporter in normal human tissues. Cancer Res. 2001;61:3458–3464. [PubMed] [Google Scholar]
- 27.Diestsra JE, Scheffer GL, Catala I, et al. Frequent expression of the multi-drug resistance-associated protein BCRP/MXR/ABCP/ABC tumours detected by the BXP-21monoclonal antibody in paraffin-embedded material. J Pathol. 2002;198:213–219. doi: 10.1002/path.1203. [DOI] [PubMed] [Google Scholar]
- 28.Leonard GD, Polgar O, Bates SE. ABC transporters and inhibitors: new targets, new agents. Curr Opin Investig Drugs. 2002;3:1652–1659. [PubMed] [Google Scholar]
- 29.McDevitt CA, Callaghan R. How can we best use structural information on P-glycoprotein to design inhibitors? Pharmacol Ther. 2007;113:429–441. doi: 10.1016/j.pharmthera.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 30.Nakamura Y, Oka M, Soda H, et al. Gefitinib (“Iressa,” ZD1839), an epidermal growth factor receptor tyrosine kinase inhibitor, reverses breast cancer resistance protein/ABCG2-mediated drug resistance. Cancer Res. 2005;65:1541–1546. doi: 10.1158/0008-5472.CAN-03-2417. [DOI] [PubMed] [Google Scholar]
- 31.Leggas M, Panetta JC, Zhuang Y, et al. Gefitinib modulates the function of multiple ATP-binding cassette transporters in vivo. Cancer Res. 2006;66:4802–4807. doi: 10.1158/0008-5472.CAN-05-2915. [DOI] [PubMed] [Google Scholar]
- 32.Polli JW, Humphreys JE, Harmon KA, et al. The role of efflux and uptake transporters in lapatinib (Tykerb, GW572016) disposition and drug interactions. Drug Metab Dispos. 2008;36:695–701. doi: 10.1124/dmd.107.018374. [DOI] [PubMed] [Google Scholar]
- 33.Riordan JR, Deuchars K, Kartner N, Alon N, Trent J, Ling V. Amplification of P-glycoprotein genes in multidrug-resistant mammalian cell lines. Nature. 1985;316:817–819. doi: 10.1038/316817a0. [DOI] [PubMed] [Google Scholar]
- 34.Arnt CR, Chiorean MV, Heldebrant MP, Gores GJ, Kaufmann SH. Synthetic Smac/DIABLO peptides enhance the effects of chemotherapeutic agents by binding XIAP and cIAP1 in situ. J Biol Chem. 2002;277:44236–44243. doi: 10.1074/jbc.M207578200. [DOI] [PubMed] [Google Scholar]
- 35.Ratain MJ, Mick R, Schilsky RL, Siegler M. Statistical and ethical issues in the design and conduct of phase I and II clinical trials of new anticancer agents. J Natl Cancer Inst. 1993;85:1637–1643. doi: 10.1093/jnci/85.20.1637. [DOI] [PubMed] [Google Scholar]
- 36.Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000;92:205–216. doi: 10.1093/jnci/92.3.205. [DOI] [PubMed] [Google Scholar]
- 37.Hsieh S, Tobien T, Koch K, Dunn J. Increasing throughput of parallel on-line extraction liquid chromatography/electrospray ionization tandem mass spectrometry system for GLP quantitative bioanalysis in drug development. Rapid Commun Mass Spectrom. 2004;18:285–292. doi: 10.1002/rcm.1327. [DOI] [PubMed] [Google Scholar]
- 38.Half E, Tang XM, Gwyn K, Sahin A, Wathen K, Sinicrope FA. Cyclooxygenase-2 expression in human breast cancers and adjacent ductal carcinoma in situ. Cancer Res. 2002;62:1676–1681. [PubMed] [Google Scholar]
- 39.Lev DC, Kim LS, Melnikova V, Ruiz M, Ananthaswamy HN, Price JE. Dual blockade of EGFR and ERK1/2 phosphorylation potentiates growth inhibition of breast cancer cells. Br J Cancer. 2004;91:795–802. doi: 10.1038/sj.bjc.6602051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Olsson P, Gedda L, Goike H, et al. Uptake of a boronated epidermal growth factor-dextran conjugate in CHO xenografts with and without human EGF-receptor expression. Anticancer Drug Des. 1998;13:279–289. [PubMed] [Google Scholar]
- 41.Gilmer TM, Cable L, Alligood K, et al. Impact of common epidermal growth factor receptor and HER2 variants on receptor activity and inhibition by lapatinib. Cancer Res. 2008;68:571–579. doi: 10.1158/0008-5472.CAN-07-2404. [DOI] [PubMed] [Google Scholar]
- 42.Dixon M. The determination of enzyme inhibitor constants. Biochem J. 1953;55:170–171. doi: 10.1042/bj0550170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jonker JW, Smit JW, Brinkhuis RF, et al. Role of breast cancer resistance protein in the bioavailability and fetal penetration of topotecan. J Natl Cancer Inst. 2000;92:1651–1656. doi: 10.1093/jnci/92.20.1651. [DOI] [PubMed] [Google Scholar]
- 44.Masumoto S, Yoshida K, Ishiguro N. Involvement of rat and human organic anion transporter 3 in the renal tubular secretion of topotecan [(S)-9-dimethylaminomethyl-10-hydroxy-camptothecin hydrochloride] J Pharmacol Exp Ther. 2007;322:1246–1252. doi: 10.1124/jpet.107.123323. [DOI] [PubMed] [Google Scholar]
- 45.Huls M, Brown CDA, Windass AS, et al. The breast cancer resistance protein transporter ABCG2 is expressed in the human kidney proximal tubule apical membrane. Kidney Int. 2007;10:1038–1044. doi: 10.1038/sj.ki.5002645. [DOI] [PubMed] [Google Scholar]