Abstract
Purpose
To describe ocular biometry relationships in older white adults.
Methods
Ocular dimensions were measured with partial coherence laser interferometry (IOL Master, Carl Zeiss, Germany) in 1968 persons (ages 58–100 years, 59% female) seen at the fourth examination of the Beaver Dam Eye Study. Generalized estimating equations modeled age, gender, height, and education associations with ocular dimensions: axial length (AL), corneal curvature radius (CR), anterior chamber depth (ACD).
Results
The mean AL was 23.69mm, CR 7.70mm, and ACD 3.11mm. Participants younger than 65 years had larger eyes (longer AL, greater CR, and deeper ACD) than persons 75 years and older. AL was 23.86mm, 23.66mm, and 23.55mm in people younger than 65 years, 65 to 74 years, and 75 years or older, respectively. Generally larger eyes were observed for men (vs women), for taller (> 178 cm vs ≤ 158 cm) and for more educated (16+ vs < 12 years) persons. Adjustment for height accounted for all gender differences. Age differences in AL were attenuated (P=0.06) after adjustment for both height and education.
Conclusions
In this older white population, age and gender variation in ocular dimensions is partially explained by differences in stature and education.
Keywords: axial length, corneal curvature, aging, education, stature
Biometric measurements of the globe, such as axial length, corneal curvature, and anterior chamber depth, have been found to differ by gender and age from childhood through adulthood.1–5 These measures also differ by stature5–9 as well as education level.9–11 Age, gender, stature, and education are all interrelated (e.g. older adults are more likely to be shorter and less likely to be highly educated). Axial length, in particular, is an important determinant of refraction,4,12,13 which has shown strong relationships to age and education.2,13–19
Although there have been studies that have assessed the inter-relationships of ocular biometry measures with age, gender, stature, and education, the majority of these studies have been confined to Asian and Hispanic populations.1,2 Some of these studies have found that axial length is shorter in older people and in women,2,6 while others have reported height and education relationships with various biometry measures.5–7,20–22 However, there is very little understanding about the complex inter-relationships among age, gender, height, and education with ocular biometry measurements in older white adults. Further understanding of such relationships may provide insight into trends and patterns of myopia13–19 that have been observed.
In the Beaver Dam Eye Study, a population-based cohort study of age-related eye diseases, we had the opportunity to add measurements of ocular dimensions at the fourth examination. In this primary report on these measures we describe the relationships between ocular biometry components with age, gender, height, and education in this Caucasian adult population.
Methods
Study Population
The Beaver Dam Eye Study is a population-based cohort study of eye disease in adults. Ocular dimensions were measured during the fourth examination of the cohort. The study began in 1988 with a private census of the population of Beaver Dam, WI. All individuals (5924) between the ages of 43 and 84 years were identified and invited for a baseline examination from 1988–1990. Follow-up examinations were performed every 5 years after this with the fourth examination occurring from May 2003 to May 2005. At each examination, participation rates were over 80% with the primary reason for non-participation being death. At each examination, living non-participants were older, less educated, had poorer vision, higher blood pressure, and smoked more than participants.23–26 Informed consent was obtained at each examination with institutional review board approval. Tenets of the Declaration of Helsinki were followed. Similar protocols were followed during each examination. Using the NIH classification of race, 99% of the population was classified as “white”.
Measurements
Ocular biometry measures were added for the fourth examination, and those data are used in this report. The relevant portions of this examination, summarized here, include: standardized non-cycloplegic refraction using an automated refractor (Humphrey, San Leandro CA) with further modification if resulting visual acuity was 20/40 or worse;27 ocular biometry using partial coherence laser interferometry (IOL Master, Carl Zeiss, Germany) for axial length (AL), anterior chamber depth (ACD), and radius of corneal curvature (CR); measurements of height and weight; questions about education; and assessment of lens status using standardized lens photography and grading.28
Height and weight were measured on a Health-O-Meter scale after participant had removed shoes, keys, wallets, etc. Weight was measured to nearest quarter pound and converted to kilograms by multiplying by 0.4536. Height was measured to nearest quarter inch and converted to centimeters by multiplying by 2.54. If unable to measure (3% of population), self-reported height and weight were used. Education was assessed with the question: “What was the highest year of school or college you completed?” During slit lamp examination, the examiner assessed lens status.
Ocular biometry was measured following manufacturer’s recommendations on 1976 (83%) participants prior to pupillary dilation (1962 both eyes, 6 right eye only, 8 left eye only). Reasons for not measuring ocular biometry (right eye) included: off-site exams (n=243), physical limitations (n=41), not enough time (n=56), and other/unspecified/refusal/inability (n=67). The average of the two corneal curvature meridians was used for analysis of CR. ACD measurements were not included in the analyses in persons without a lens or with an intraocular lens (n=269). Comparison of characteristics of those included for various analyses is shown in Table 1. In general, those included in analyses were younger and after age adjustment were less likely to have diabetes, were taller, and were less likely to have cataract and age-related macular degeneration. There were no differences in education or refraction (spherical equivalent).
Table 1.
Comparison of Participants at Fourth Exam Phase of Beaver Dam Eye Study to Those Included in Analyses.
| Whole Population | With AL Measure | With CR Measure | With ACD Measure | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | N | Mean (SD) / % | N | Mean (SD) / % | P valuea | N | Mean (SD) / % | P valuea | N | Mean (SD) / % | P valuea |
| Age (years) | 2375 | 71.9 (9.1) | 1967 | 70.3 (8.0) | *** | 1962 | 70.3 (8.0) | *** | 1675 | 69.1 (7.4) | *** |
| Sex (% male) | 2375 | 41.3% | 1967 | 42.7% | -- | 1962 | 42.9% | -- | 1675 | 44.4% | ** |
| Education (years) | 2365 | 12.7 (2.7) | 1962 | 12.9 (2.6) | -- | 1957 | 12.9 (2.6) | -- | 1671 | 12.9 (2.7) | -- |
| Income ($1K) | 2358 | 55.0 (20.3) | 1965 | 54.6 (19.2) | *** | 1961 | 54.5 (19.3) | *** | 1674 | 54.9 (18.7) | *** |
| Height (cm) | 2336 | 164.5 (9.8) | 1961 | 164.7 (9.7) | ** | 1956 | 164.7 (9.6) | * | 1671 | 165.2 (9.6) | -- |
| Weight (kg) | 2350 | 80.3 (18.8) | 1960 | 81.3 (18.7) | -- | 1955 | 81.4 (18.7) | -- | 1670 | 82.2 (18.6) | -- |
| Current smoker (%) | 2368 | 8.7% | 1967 | 9.4% | -- | 1962 | 9.4% | -- | 1675 | 9.8% | -- |
| Hypertensive (%) | 2323 | 65.6% | 1965 | 63.7% | -- | 1960 | 63.7% | -- | 1675 | 63.2% | -- |
| Diabetes (%) | 2233 | 15.8% | 1949 | 14.2% | *** | 1945 | 14.3% | *** | 1659 | 13.4% | *** |
| Spherical equivalent (diopters) | 1819 | .38 (2.4) | 1670 | .33 (2.3) | -- | 1666 | .33 (2.3) | -- | 1654 | .32 (2.3) | -- |
| IOP (mmHg) | 2189 | 15.1 (3.3) | 1952 | 15.1 (3.3) | + | 1948 | 15.1 (3.3) | -- | 1663 | 15.2 (3.3) | *** |
| Any cataract (%) | 1694 | 35.0% | 1604 | 32.9% | * | 1601 | 32.7% | * | 1588 | 32.6% | ** |
| Early AMD (%) | 2111 | 13.6% | 1859 | 11.9% | -- | 1858 | 12.0% | -- | 1595 | 10.5% | -- |
| Late AMD (%) | 2205 | 2.8% | 1895 | 1.3% | *** | 1891 | 1.3% | *** | 1618 | 0.9% | *** |
Definitions: AL=axial length; CR=radius of corneal curvature; ACD=anterior chamber depth; IOP=intraocular pressure; AMD=age-related macular degeneration.
Compare those in analysis to those not in analysis (age-adjusted).
- --=p value ≥ 0.10
- +=p value ≥ 0.05 and <0.10
- *=p value ≥ 0.01 and <0.05
- **=p value ≥ 0.001 and <0.01
- ***=p value <0.001
Statistical Methods
SAS version 9.129 was used for all analyses. Normality of each ocular biometry measure (AL, CR, and ACD) was assessed. Mean ocular dimensions were calculated for each eye separately and are reported for the right eye, as analyses for left eyes were similar (data not shown). However, both eyes were included in analysis of variance models with the generalized estimating equations (GEE) approach to adjust for correlation between the eyes. All adjustments were done for the continuous version of the variables. Models were assessed using appropriate contrast statements.
Results
The relationships of age and gender to the ocular dimensions and refractions are shown in Table 2. Men and younger persons had longer AL, greater (flatter) CR, and deeper ACD than women and older individuals. Persons who were < 65 years of age had a mean AL of 23.86 mm, a CR of 7.72 mm, and an ACD of 3.19 mm. Persons who were ≥ 75 years of age had a mean AL of 23.55 mm, a CR of 7.68 mm, and an ACD of 2.99 mm.
Table 2.
Age and Gender Distribution of Ocular Biometry (right eyes).
| Women | Men | Men vs Women |
All Persons | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (years) | N | Mean (SD) | P value | N | Mean (SD) | P value | P value | N | Mean (SD) | P value | |
| AL | <65 | 314 | 23.69 (1.25) | referent | 262 | 24.06 (1.06) | referent | 576 | 23.86 (1.18) | referent | |
| 65–74 | 447 | 23.49 (1.21) | .001 | 343 | 23.88 (1.14) | .06 | 790 | 23.66 (1.19) | <.001 | ||
| ≥ 75 | 366 | 23.37 (1.02) | <.001 | 235 | 23.83 (1.08) | .02 | 601 | 23.55 (1.06) | <.001 | ||
| Total | 1127 | 23.51 (1.17) | 840 | 23.92 (1.10) | <.001 | 1967 | 23.69 (1.16) | ||||
| CR | <65 | 313 | 7.67 (0.25) | referent | 263 | 7.77 (0.26) | referent | 576 | 7.72 (0.26) | referent | |
| 65–74 | 443 | 7.66 (0.25) | .36 | 343 | 7.77 (0.27) | .73 | 786 | 7.71 (0.26) | .55 | ||
| ≥ 75 | 365 | 7.63 (0.26) | .02 | 235 | 7.76 (0.27) | .58 | 600 | 7.68 (0.27) | .01 | ||
| Total | 1121 | 7.65 (0.25) | 841 | 7.77 (0.27) | <.001 | 1962 | 7.70 (0.26) | ||||
| ACD | <65 | 297 | 3.17 (0.32) | referent | 256 | 3.22 (0.36) | referent | 553 | 3.19 (0.34) | referent | |
| 65–74 | 397 | 3.11 (0.35) | .02 | 314 | 3.12 (0.38) | <.001 | 711 | 3.11 (0.36) | <.001 | ||
| ≥ 75 | 237 | 2.95 (0.37) | <.001 | 174 | 3.05 (0.40) | <.001 | 411 | 2.99 (0.39) | <.001 | ||
| Total | 931 | 3.09 (0.36) | 744 | 3.14 (0.38) | .004 | 1675 | 3.11 (0.37) | ||||
Definitions: SD=standard deviation; AL=axial length; CR=radius of corneal curvature; ACD=anterior chamber depth.
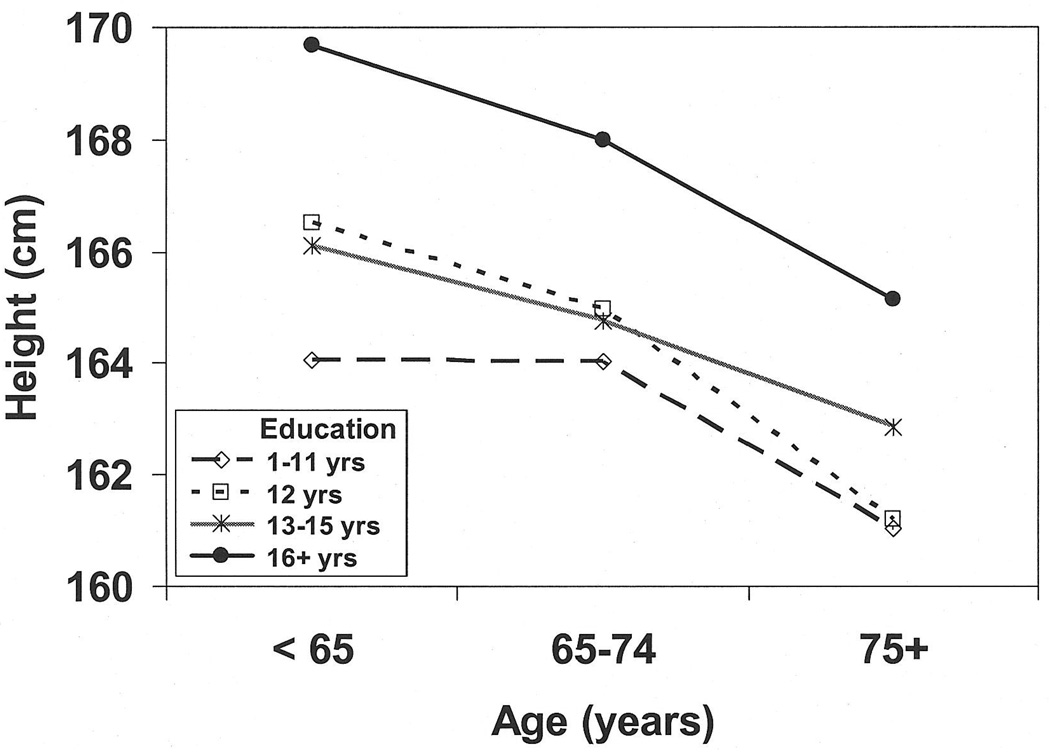
Both height and education decreased with increasing age. Persons younger than 65 years had a mean ± standard deviation height of 167.1 ± 9.9 cm (65.8 ± 3.9 inches) and had completed 13.6 ± 2.6 years of school. Persons ≥ 75 years were 162.0 ± 9.6 cm (63.8 ± 3.8 inches) tall and had completed 12.1 ± 2.9 years of school. The age trends were similar within genders and women were shorter (158.6 ± 6.6 cm vs 172.9 ± 7.2 cm; 62.5 ± 2.6 vs 68.1 ± 2.8 inches) and had completed less schooling (12.5 ± 2.3 vs 13.1 ± 3.2 years) than men. Within an age category, persons with more education were taller (Figure 1). The same trends were observed within each gender (data not shown).
Figure 1.
Distribution of height by age and education level.
Ocular dimensions varied with height and education and were similar in men and women (Table 3). Taller individuals generally had larger eyes. In the full population, AL increased from 23.36 mm in those < 158 cm (62 inches) tall to 24.20 mm in those > 178 cm (70 inches) tall (β = .31, P < .001 per 10 cm). Similarly, CR increased from 7.60 mm to 7.84 mm (β = .08, P < .001) and ACD increased from 3.04 mm to 3.21 mm (β = .05, P < .001). Persons with more education had longer AL (β = .08, P < .001 per year), greater (flatter) CR (β = .009 P < .001), and deeper ACD (β = .02, P < .001). When comparing CR by categories of education, only those with 16 or more years of education had significantly higher CR (versus those with 1–11 years). Additional adjustment for height attenuated the relationships, but they remained statistically significant (not shown).
Table 3.
Height and Education Relationship to Ocular Biometry (right eyes).
| Women | Men | All Persons | |||||
|---|---|---|---|---|---|---|---|
| N | Mean (SD) | N | Mean (SD) | N | Mean (SD) | ||
| AL | Height (cm) | ||||||
| ≤ 158 | 495 | 23.35 (1.18) | 15 | 23.57 (1.26) | 510 | 23.36 (1.18) | |
| 159–168 | 562 | 23.59 (1.12) | 189 | 23.66 (1.08) | 751 | 23.61 (1.11) | |
| 169–178 | 70 | 23.98 (1.27) | 453 | 23.93 (1.10) | 523 | 23.94 (1.13) | |
| >178 | 0 | - | 183 | 24.20 (1.03) | 183 | 24.20 (1.03) | |
| Education (years) | |||||||
| 1–11 | 153 | 23.23 (1.44) | 128 | 23.54 (0.85) | 281 | 23.37 (1.22) | |
| 12 | 593 | 23.47 (1.09) | 385 | 23.86 (1.15) | 978 | 23.62 (1.13) | |
| 13–15 | 214 | 23.61 (1.21) | 124 | 24.01 (1.03) | 338 | 23.76 (1.16) | |
| 16+ | 165 | 23.77 (1.00) | 200 | 24.25 (1.09) | 365 | 24.03 (1.07) | |
| CR | Height (cm) | ||||||
| ≤ 158* | 491 | 7.60 (0.25) | 15 | 7.65 (0.23) | 506 | 7.60 (0.25) | |
| 159–168 | 560 | 7.69 (0.24) | 189 | 7.69 (0.27) | 749 | 7.69 (0.25) | |
| 169–178 | 70 | 7.74 (0.27) | 454 | 7.78 (0.26) | 524 | 7.77 (0.26) | |
| >178 | 0 | - | 183 | 7.84 (0.26) | 183 | 7.84 (0.26) | |
| Education (years) | |||||||
| 1–11 | 150 | 7.63 (0.25) | 128 | 7.73 (0.25) | 278 | 7.68 (0.26) | |
| 12 | 591 | 7.64 (0.25) | 386 | 7.78 (0.27) | 977 | 7.70 (0.27) | |
| 13–15 | 213 | 7.66 (0.24) | 124 | 7.75 (0.24) | 337 | 7.69 (0.24) | |
| 16+ | 165 | 7.70 (0.25) | 200 | 7.79 (0.27) | 365 | 7.75 (0.27) | |
| ACD | Height (cm) | ||||||
| ≤ 158* | 392 | 3.04 (0.36) | 11 | 3.17 (0.42) | 403 | 3.04 (0.36) | |
| 159–168 | 479 | 3.11 (0.35) | 163 | 3.07 (0.38) | 642 | 3.10 (0.36) | |
| 169–178 | 60 | 3.22 (0.37) | 402 | 3.13 (0.38) | 462 | 3.15 (0.38) | |
| >178 | 0 | - | 168 | 3.21 (0.37) | 168 | 3.21 (0.37) | |
| Education (years) | |||||||
| 1–11 | 120 | 2.95 (0.35) | 109 | 3.00 (0.34) | 229 | 2.97 (0.34) | |
| 12 | 493 | 3.09 (0.36) | 336 | 3.13 (0.37) | 829 | 3.11 (0.36) | |
| 13–15 | 178 | 3.11 (0.33) | 112 | 3.14 (0.38) | 290 | 3.12 (0.35) | |
| 16+ | 138 | 3.16 (0.36) | 185 | 3.22 (0.41) | 323 | 3.20 (0.39) | |
Abbreviations: SD=standard deviation; AL=axial length; CR=radius of corneal curvature; ACD=anterior chamber depth
- ≤ 158 cm = ≤ 62 inches
- 159–168 cm = 63–66.00 inches
- 169–178 cm = 67–70 inches
- >178 cm = > 70.1 inches
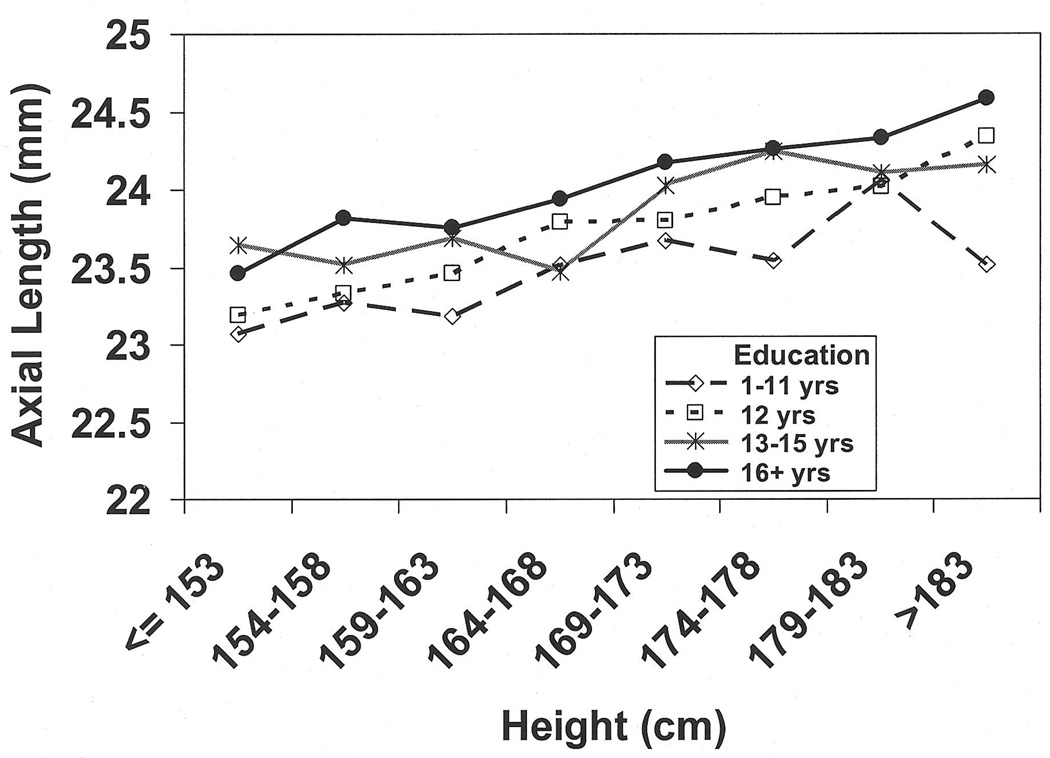
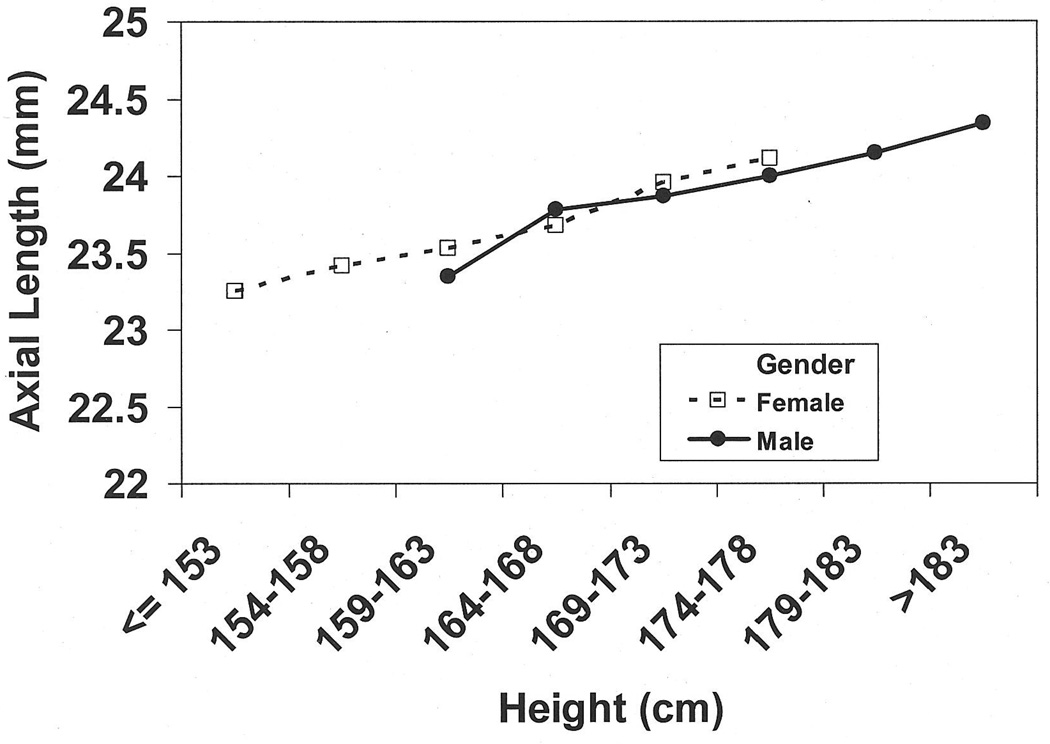
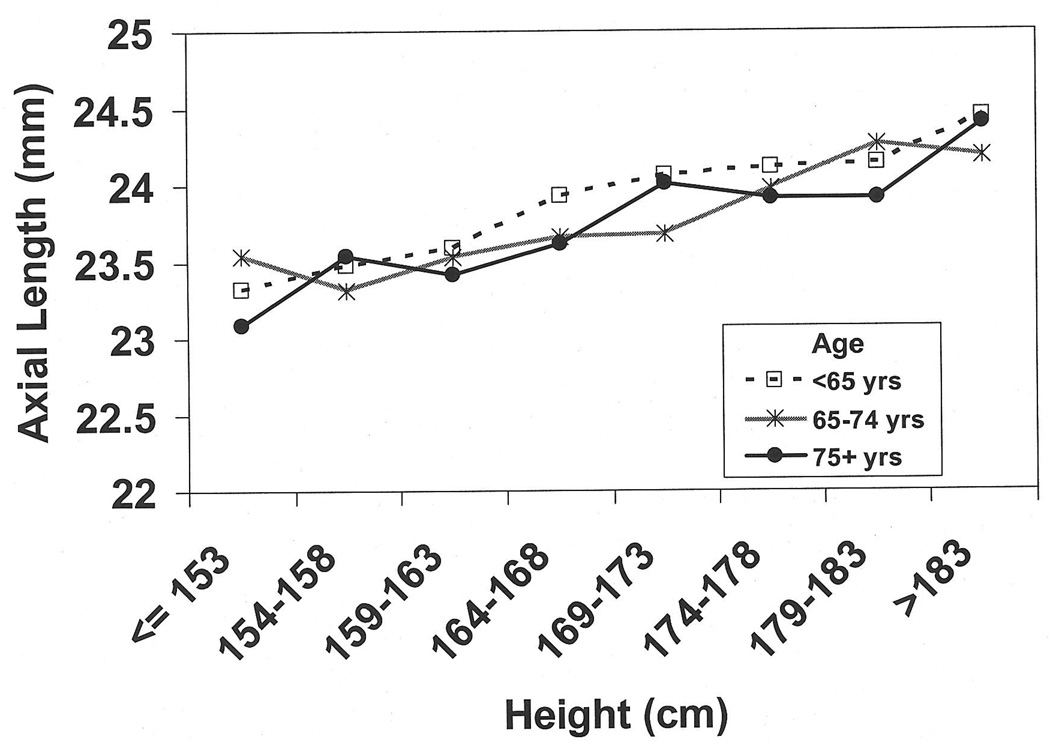
To further explore whether height differences may explain the age, gender, and education relationships to the biometry measures, we plotted AL by height for age (Figure 2a), gender (Figure 2b), and education (Figure 2c) categories. For persons of the same height, those younger than 65 years and those with more education appeared to have longer AL. Similar figures for CR and ACD (not shown) also suggested that among persons with the same height, younger persons had deeper ACD and those with ≥ 16years of education had greater (flatter) CR and deeper ACD.
Figure 2.
Distribution of axial length (right eyes) by height and a) age, b) gender, and c) education in the Beaver Dam Eye Study.
In models adjusting for height and education (Table 4), the age and gender relationships to the ocular components were attenuated. Importantly, the age relationship to AL was non-significant after adjustment for both height and education (P = .06). The age relationship to CR was no longer significant after adjustment for height. Education did not add information beyond height for CR. Both height and education add to the model for ACD and the age relationship remained significant. The gender relationships to AL, ACD, and CR were no longer significant after adjustment for height.
Table 4.
Generalized Estimating Equation Models for Ocular Dimensions with Age, Gender, Height, and Education.
| Model 1a | Model 2b | ||||
|---|---|---|---|---|---|
| β (95% CI) | P valuec | β (95% CI) | P valuec | ||
| AL | Male vs Female | 0.41 (0.32, 0.50) | <.001 | 0.02 (−0.13, 0.16) | .80 |
| Age (per 5 years) | −0.08 (−0.11, −0.05) | <.001 | −0.03 (−0.07, 0.001) | .06 | |
| Height (per 10 cm) | - | - | 0.20 (0.14, 0.26) | <.001 | |
| Education (per 4 years) | - | - | 0.24 (0.16, 0.31) | <.001 | |
| CR | Male vs Female | 0.12 (0.10, 0.14) | <.001 | 0.002 (−0.03, 0.04) | .88 |
| Age (per 5 years) | −0.01 (−0.02, −0.003) | .005 | 0.001 (−0.01, 0.01) | .74 | |
| Height (per 10 cm) | - | - | 0.06 (0.05, 0.08) | <.001 | |
| Education (per 4 years) | - | - | 0.01 (0.00, 0.03) | .11 | |
| ACD | Male vs Female | 0.04 (0.01, 0.08) | .01 | −0.01 (−0.06, 0.04) | .69 |
| Age (per 5 years) | −0.06 (−0.07, −0.05) | <.001 | −0.05 (−0.06, −0.04) | <.001 | |
| Height (per 10 cm) | - | - | 0.03 (0.01, 0.05) | 0.01 | |
| Education (per 4 years) | - | - | 0.06 (0.03, 0.08) | <.001 | |
Abbreviations: β=estimate of slope; CI=confidence interval; AL=axial length; CR=radius of corneal curvature; ACD=anterior chamber depth
Model 1 adjusted for age and gender
Model 2 adjusted for age, gender, height, and education
P value analogous to type III sums of squares
Discussion
In this study, we report on the distribution of ocular biometry measures in an older Caucasian population. We found that younger people, men, taller and more educated people had generally longer AL and larger eyes. We found that height explained most of the variations in the measures between men and women as well as the variation in CR between younger and older people. Adjustment for education in addition to height explained some of the variation in AL between younger and older people.
As in previous studies in Asian and Hispanic populations, we found that younger persons had longer AL, greater (flatter) CR, and deeper ACD than older persons. In a separate analysis in which we used age groups similar to those used in the other studies,1,2 our Caucasian population had, on average, longer AL and greater CR than the Asian and Hispanic populations (K. Lee, unpublished data 2007). In 60–69 year old women, the mean AL was 23.7 mm in BDES, 22.7 mm in Tanjong Pagar, 23.2 mm in Mongolia, and 23.1 mm in Los Angeles Latino Eye Study. These differences may be influenced by differing methods (IOL master compared to ultra sound) used to obtain biometry measures. Additionally our population is slightly older, taller, had more years of education, and had a spherical equivalent between the Asian and Hispanic population.1,2
The age and gender differences observed for AL, CR, and ACD may be related to the fact that older persons and women have smaller stature and thus smaller eyes. In our population, height decreased by 1.3 cm (0.5 inches) for every 5 year increase in age and women were on average 14 cm (5 inches) shorter than men. In addition, shorter persons had significantly shorter AL, shorter CR, and shallower ACD which is consistent with observations in Asian populations.5,6 Height was not related to the ratio of AL to CR (K. Lee, unpublished data 2007), supporting the notion that the AL and CR remained in similar proportions for taller and shorter persons. Adjustment for height attenuated the age and gender relationships to the ocular biometry measures. The gender differences for all measures were no longer significant after height adjustment. However, despite some attenuation, older individuals still had shorter AL and shallower ACD, but there were no significant differences in CR after adjustment for height. The AL/CR ratio was larger in younger persons (K. Lee, unpublished data 2007), even after adjustment for height, suggesting that these persons have proportionately longer AL given the CR than older persons.
The relationship between education and AL has not been widely studied.30 It may reflect excessive AL growth associated with near work (“use-abuse” theory)13 as supported by data from studies of medical students or microscopists that show an increase in AL with adult-onset myopia.10,11,31 It may also reflect larger stature resulting from a higher socio-economic status and better nutrition associated with more educated groups. Indeed, we found that among persons the same age, persons with more education tended to be taller. We also observed that among persons the same height, those with more education had longer AL. We found that more education was significantly associated with longer AL, greater (flatter) CR, and deeper ACD. With the exception of CR, these relationships remained despite adjustment for age and height (data not shown). Thus, height differences associated with education do not explain the longer AL in persons with more education.
The major limitation in this and other reported population-based studies is that they were cross-sectional, which does not allow evaluation of change of these measures with age. To investigate a real effect of aging as opposed to a cohort effect, longitudinal data are needed. While such data are lacking for axial length, data on myopia suggest that the aging process may explain age-related declines in myopia observed in many cross-sectional studies.32 It is possible that some of these results may be affected by differential survival, where survivors may be more educated and taller. However, we did not observe large differences in baseline height or education level among participants in this analysis compared to all participants in the baseline examination phase.
An important observation in our study was that adjustment for both education and height attenuated the relationship between age and axial length. Younger persons had more education and were taller. Among persons with a similar height, those with ≥ 16 years of education had longer AL. Our finding that age variations in axial length, a key determinant of refraction, is largely explained by height and education may partially explain the “cohort” effect of more myopic refractions at younger ages that is now recognized in many different populations with diverse racial/ethnic groups.
Acknowledgement
Supported by the National Institutes of Health grant EY06594 (R Klein, BEK Klein) and, in part, by the Research to Prevent Blindness (R and BEK Klein, Senior Scientific Investigator Awards), New York, NY.
Reference List
- 1.Wong TY, Foster PJ, Ng TP, Tielsch JM, Johnson GJ, Seah SK. Variations in ocular biometry in an adult Chinese population in Singapore: the Tanjong Pagar Survey. Invest Ophthalmol Vis Sci. 2001;42:73–80. [PubMed] [Google Scholar]
- 2.Shufelt C, Fraser-Bell S, Ying-Lai M, Torres M, Varma R. Refractive error, ocular biometry, and lens opalescence in an adult population: the Los Angeles Latino Eye Study. Invest Ophthalmol Vis Sci. 2005;46:4450–4460. doi: 10.1167/iovs.05-0435. [DOI] [PubMed] [Google Scholar]
- 3.Grosvenor T. Reduction in axial length with age: an emmetropizing mechanism for the adult eye? Am J Optom Physiol Opt. 1987;64:657–663. [PubMed] [Google Scholar]
- 4.Ip JM, Huynh SC, Kifley A, et al. Variation of the contribution from axial length and other oculometric parameters to refraction by age and ethnicity. Invest Ophthalmol Vis Sci. 2007;48:4846–4853. doi: 10.1167/iovs.07-0101. [DOI] [PubMed] [Google Scholar]
- 5.Saw SM, Chua WH, Hong CY, et al. Height and its relationship to refraction and biometry parameters in Singapore Chinese children. Invest Ophthalmol Vis Sci. 2002;43:1408–1413. [PubMed] [Google Scholar]
- 6.Wong TY, Foster PJ, Johnson GJ, Klein BE, Seah SK. The relationship between ocular dimensions and refraction with adult stature: the Tanjong Pagar Survey. Invest Ophthalmol Vis Sci. 2001;42:1237–1242. [PubMed] [Google Scholar]
- 7.Eysteinsson T, Jonasson F, Arnarsson A, Sasaki H, Sasaki K. Relationships between ocular dimensions and adult stature among participants in the Reykjavik Eye Study. Acta Ophthalmol Scand. 2005;83:734–738. doi: 10.1111/j.1600-0420.2005.00540.x. [DOI] [PubMed] [Google Scholar]
- 8.Ojaimi E, Morgan IG, Robaei D, et al. Effect of stature and other anthropometric parameters on eye size and refraction in a population-based study of Australian children. Invest Ophthalmol Vis Sci. 2005;46:4424–4429. doi: 10.1167/iovs.05-0077. [DOI] [PubMed] [Google Scholar]
- 9.Uranchimeg D, Yip JL, Lee PS, et al. Cross-sectional differences in axial length of young adults living in urban and rural communities in Mongolia. Asian J Ophthalmol. 2005;7:133–139. [Google Scholar]
- 10.Lin LL, Shih YF, Lee YC, Hung PT, Hou PK. Changes in ocular refraction and its components among medical students-- a 5-year longitudinal study. Optom Vis Sci. 1996;73:495–498. doi: 10.1097/00006324-199607000-00007. [DOI] [PubMed] [Google Scholar]
- 11.McBrien NA, Adams DW. A longitudinal investigation of adult-onset and adult progression of myopia in an occupational group. Refractive and biometric findings. Invest Ophthalmol Vis Sci. 1997;38:321–333. [PubMed] [Google Scholar]
- 12.Olsen T, Arnarsson A, Sasaki H, Sasaki K, Jonasson F. On the ocular refractive components: the Reykjavik Eye Study. Acta Ophthalmol Scand. 2007;85:361–366. doi: 10.1111/j.1600-0420.2006.00847.x. [DOI] [PubMed] [Google Scholar]
- 13.Saw SM, Katz J, Schein OD, Chew SJ, Chan TK. Epidemiology of myopia. Epidemiol Rev. 1996;18:175–187. doi: 10.1093/oxfordjournals.epirev.a017924. [DOI] [PubMed] [Google Scholar]
- 14.Familial aggregation and prevalence of myopia in the Framingham Offspring Eye Study.The Framingham Offspring Eye Study Group. Arch Ophthalmol. 1996;114:326–332. doi: 10.1001/archopht.1996.01100130322017. [DOI] [PubMed] [Google Scholar]
- 15.Attebo K, Ivers RQ, Mitchell P. Refractive errors in an older population: the Blue Mountains Eye Study. Ophthalmology. 1999;106:1066–1072. doi: 10.1016/S0161-6420(99)90251-8. [DOI] [PubMed] [Google Scholar]
- 16.Katz J, Tielsch JM, Sommer A. Prevalence and risk factors for refractive errors in an adult inner city population. Invest Ophthalmol Vis Sci. 1997;38:334–340. [PubMed] [Google Scholar]
- 17.Wang Q, Klein BE, Klein R, Moss SE. Refractive status in the Beaver Dam Eye Study. Invest Ophthalmol Vis Sci. 1994;35:4344–4347. [PubMed] [Google Scholar]
- 18.Wensor M, McCarty CA, Taylor HR. Prevalence and risk factors of myopia in Victoria, Australia. Arch Ophthalmol. 1999;117:658–663. doi: 10.1001/archopht.117.5.658. [DOI] [PubMed] [Google Scholar]
- 19.Wong TY, Foster PJ, Hee J, et al. Prevalence and risk factors for refractive errors in adult Chinese in Singapore. Invest Ophthalmol Vis Sci. 2000;41:2486–2494. [PubMed] [Google Scholar]
- 20.Gardiner PA. Physical growth and the progress of myopia. Lancet. 1955;269:952–953. doi: 10.1016/s0140-6736(55)92792-6. [DOI] [PubMed] [Google Scholar]
- 21.Gardiner PA. The relation of myopia to growth. Lancet. 1954;266:476–479. doi: 10.1016/s0140-6736(54)91187-3. [DOI] [PubMed] [Google Scholar]
- 22.Goldschmidt E. Myopia and height. Acta Ophthalmol. 1966;44:751–761. [Google Scholar]
- 23.Klein R, Klein BE, Lee KE, Cruickshanks KJ, Gangnon RE. Changes in visual acuity in a population over a 15-year period: the Beaver Dam Eye Study. Am J Ophthalmol. 2006;142:539–549. doi: 10.1016/j.ajo.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 24.Klein R, Klein BE, Lee KE, Cruickshanks KJ, Chappell RJ. Changes in visual acuity in a population over a 10-year period : The Beaver Dam Eye Study. Ophthalmology. 2001;108:1757–1766. doi: 10.1016/s0161-6420(01)00769-2. [DOI] [PubMed] [Google Scholar]
- 25.Klein R, Klein BE, Lee KE. Changes in visual acuity in a population. The Beaver Dam Eye Study. Ophthalmology. 1996;103:1169–1178. doi: 10.1016/s0161-6420(96)30526-5. [DOI] [PubMed] [Google Scholar]
- 26.Klein R, Klein BE, Linton KL, De Mets DL. The Beaver Dam Eye Study: visual acuity. Ophthalmology. 1991;98:1310–1315. doi: 10.1016/s0161-6420(91)32137-7. [DOI] [PubMed] [Google Scholar]
- 27.Lee KE, Klein BE, Klein R, Wong TY. Changes in refraction over 10 years in an adult population: the Beaver Dam Eye study. Invest Ophthalmol Vis Sci. 2002;43:2566–2571. [PubMed] [Google Scholar]
- 28.Klein BE, Klein R, Linton KL. Prevalence of age-related lens opacities in a population. The Beaver Dam Eye Study. Ophthalmology. 1992;99:546–552. doi: 10.1016/s0161-6420(92)31934-7. [DOI] [PubMed] [Google Scholar]
- 29.SAS Institute Inc. SAS/STAT User’s Guide, Version 9.1. Cary, NC: SAS Institute Inc; 2004. [Google Scholar]
- 30.Wong TY, Foster PJ, Johnson GJ, Seah SK. Education, socioeconomic status, and ocular dimensions in Chinese adults: the Tanjong Pagar Survey. Br J Ophthalmol. 2002;86:963–968. doi: 10.1136/bjo.86.9.963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kinge B, Midelfart A, Jacobsen G, Rystad J. Biometric changes in the eyes of Norwegian university students--a three- year longitudinal study. Acta Ophthalmol Scand. 1999;77:648–652. doi: 10.1034/j.1600-0420.1999.770608.x. [DOI] [PubMed] [Google Scholar]
- 32.Mutti DO, Zadnik K. Age-related decreases in the prevalence of myopia: longitudinal change or cohort effect? Invest Ophthalmol Vis Sci. 2000;41:2103–2107. [PubMed] [Google Scholar]