Abstract
BACKGROUND
Adaptation of the maternal immune response to accommodate the semi-allogeneic fetus is necessary for pregnancy success, and disturbances in maternal tolerance are implicated in infertility and reproductive pathologies. T regulatory (Treg) cells are a recently discovered subset of T-lymphocytes with potent suppressive activity and pivotal roles in curtailing destructive immune responses and preventing autoimmune disease.
METHODS
A systematic review was undertaken of the published literature on Treg cells in the ovary, testes, uterus and gestational tissues in pregnancy, and their link with infertility, miscarriage and pathologies of pregnancy. An overview of current knowledge on the generation, activation and modes of action of Treg cells in controlling immune responses is provided, and strategies for manipulating regulatory T-cells for potential applications in reproductive medicine are discussed.
RESULTS
Studies in mouse models show that Treg cells are essential for maternal tolerance of the conceptus, and that expansion of the Treg cell pool through antigen-specific and antigen non-specific pathways allows their suppressive actions to be exerted in the critical peri-implantation phase of pregnancy. In women, Treg cells accumulate in the decidua and are elevated in maternal blood from early in the first trimester. Inadequate numbers of Treg cells or their functional deficiency are linked with infertility, miscarriage and pre-eclampsia.
CONCLUSIONS
The potency and wide-ranging involvement of Treg cells in immune homeostasis and disease pathology indicates the considerable potential of these cells as therapeutic agents, raising the prospect of their utility in novel treatments for reproductive pathologies.
Keywords: pregnancy, infertility, cytokines, regulatory T-cells, tolerance, immune suppression
Introduction
Pregnancy is a unique immunological challenge in which an antigenically distinct fetus and placenta develop in the uterus of the mother. The complex mechanisms by which the fetus avoids rejection, despite expression of paternal major histocompatibility (MHC) antigens, still remain incompletely understood (Billington, 2003). Over 50 years ago, Medawar first proposed the existence of regulatory mechanisms that suppress the maternal immune system (Medawar, 1953). After discovery of heterogeneity in T helper (Th) cell populations in the 1980s, for several years maternal tolerance towards fetal alloantigens was explored in the context of the Th1/Th2 paradigm, with Th2 cells and cytokines proposed to overrule the Th1 cellular immune response which can lead to fetal abortion (Wegmann et al., 1993; Raghupathy, 1997). However, this explanation is now insufficient and it has become clear that additional regulatory mechanisms involving both the innate and the adaptive compartments of the immune response play important roles (Sargent et al., 2006b; Trowsdale and Betz, 2006; Chaouat, 2007; Saito et al., 2007). Understanding the mechanisms responsible for tolerance of the male and female gametes poses a similar challenge, since these also express antigens perceived as foreign by the immune system, but are not rejected.
One emerging focus is the role of specialized populations of T-lymphocytes termed regulatory T-cells. These cells are potent suppressors of inflammatory immune responses, and are essential in preventing destructive immunity in all the tissues of the body. The physiological role of regulatory T-cells is 2-fold. Primarily, they act to control T-cells that react with ‘self’ antigens but have escaped negative selection from the thymus, and in addition, they limit the extent and duration of responses exerted by T-cells reactive with alloantigens and other exogenous antigens. Thus, regulatory T-cells can be viewed as guardians of tissue integrity, preventing harm that might otherwise be caused by aberrant or uncontrolled immune responses. This homeostatic regulation is pivotal in tissues containing endogenous physiological antigens that escape detection as ‘self’ due to their tissue-restricted expression, and in epithelial surfaces where tolerance of non-dangerous foreign antigens is essential to normal function. Their unique properties and behaviour, particularly their capacity to suppress responses to tissue-specific antigens and alloantigens, confer the capacity for regulatory T-cells to perform unique functions in the events of reproduction and pregnancy.
This review aims to examine the emerging importance of regulatory T-cells in suppressing immunological attack on the conceptus, spermatozoa and oocytes, and the promise for reproductive medicine of new drugs and technologies for manipulating these cells. The key take-home points relevant to regulatory T-cells in reproductive biology and medicine that emerge from this review are listed in Table I.
Table I.
Key features of regulatory T cells in regulating the immune response to pregnancy
| Treg cells are potent suppressors of autoimmunity and allograft rejection |
| Treg cells are implicated in immune tolerance of the conceptus tissues, oocytes and spermatozoa |
| Treg cells are increased in the blood, decidual tissue and lymph nodes draining the uterus in pregnancy |
| Deletion of these cells is incompatible with maintenance of allogeneic pregnancy |
| Unexplained infertility, miscarriage and pre-eclampsia are linked with numerical and functional Treg deficiency |
| Treg cell populations can be expanded in vitro or in vivo for therapeutic purposes |
| Dendritic cells controlling Treg cell populations can be targeted in vivo to enhance Treg cell numbers and function |
| Development of Treg cell therapies for treating infertility and reproductive pathologies will require knowledge of the antigens, cytokines and hormones regulating these cells |
Methods
Initially, we synthesized an overview of the current information on tissue origins and modes of action of regulatory T-cells, drawing mainly on seminal papers at the forefront of this specific field of immunology. We then undertook a systematic review of the published literature on regulatory T-cells in reproductive events spanning gametogenesis to embryo implantation and pregnancy. The papers cited were selected on the basis of relevance and quality from a list generated using combinations of the following search terms in Pubmed: ‘regulatory T-cells, Treg cells, Tr1 cells, Th3 cells, ovary, testes, uterus, decidua, placenta, pregnancy, infertility, miscarriage and pre-eclampsia’. Finally, we compiled information drawn from selected key papers on the manipulation and utility of regulatory T-cells for clinical applications in transplantation and autoimmune disease. On the basis of this information, we formulated a perspective on the future prospects for targeting regulatory T-cells in novel therepautic strategies for treatment of infertility and reproductive pathologies.
Regulatory T-cells and immune suppression
The discovery and classification of regulatory T-cells
The term ‘regulatory T-cells’ refers to a family of T-lymphocyte populations with suppressive/regulatory properties that are devoted to maintaining antigen-specific T-cell tolerance. At least three subsets of CD4+ regulatory T-cells with distinct suppressive mechanisms are distinguished by their phenotype, cytokine secretion and tissue origin (Jonuleit and Schmitt, 2003). These are type 1 regulatory T-cells (Tr1) cells, T-helper 3 (Th3) cells and CD4+CD25+ regulatory T-cells (Treg cells). Each of these populations has the characteristic capacity to actively inhibit the proliferation and effector function of other T-cells (Fukaura et al., 1996; Groux et al., 1997; Suri-Payer et al., 1998). CD8+ T-cells with regulatory properties have also been described, but less is known about their ontogeny, regulation and function (Smith and Kumar, 2008).
The history of regulatory cells/suppressor cells in the immunology literature dates back to the 1970s when T-lymphocytes that were capable of suppressing immune responses were first described and named ‘suppressor T-cells’ (Gershon et al., 1972). However with the lack of a definitive marker, questions regarding their authenticity were raised and attention shifted away from this cell population (Green and Webb, 1993), until Treg cells in their existing form were identified as a specialized T-cell subset in 1995 by Sakaguchi et al. (1995). Tr1 cells were initially characterized in mouse models of inflammatory bowel disease as potent suppressors of antigen-specific immune responses mediated by interleukin-10 (IL-10) synthesis (Groux et al., 1997). Th3 cells were discovered in mice as mediators of oral tolerance acting to inhibit induction of immunity through secretion of transforming growth factor-β (TGFβ) (Weiner, 2001). Of the three cell populations, Treg cells have fast become established as perhaps the most potent and widespread suppressive cell lineage in the immune system. Unlike Th3 and Tr1 cells which appear to represent altered differentiation states of conventional CD4+CD25− T-cells, Treg cells are believed to comprise a distinct and unique T-cell lineage (Weiner, 2001). They have now been implicated in critical protective functions in auto-immune disease (Sakaguchi, 2005), transplantation tolerance (Waldmann et al., 2004), gastro-intestinal homeostasis (Coombes et al., 2005) and inflammatory disease (Wahl et al., 2004b), and conversely, are a pivotal component of the pathophysiological immune tolerance induced by tumours (Munn and Mellor, 2006). Of the three cell subsets, Treg cells are distinguished by their apparently essential role in reproductive events. Although cells with features reminiscent of Tr1 cells and Th3 cells are present in the uterus (Robertson, 2000), any role for Tr1 cells appears to be redundant since allogenic pregnancy is not compromised in IL-10 null mutant mice (White et al., 2004). The necessity of Th3 cells remains to be tested, but this is more challenging since immunocompetent TGFβ null mutant mice do not survive to reproductive age and suffer non-immune-related reproductive disturbances (Ingman et al., 2006). The current review will therefore focus predominantly on the Treg cell subset of regulatory T cells.
Treg cells are a distinct T-lymphocyte subset
Treg cells are defined as a separate cellular subset on the basis of their surface phenotype as well as functional characteristics. Treg cells are one of the four major classes of CD4+ T-cells, together with Th1 cells, Th2 cells and Th17 cells (Zhu and Paul, 2008), distinguished from the other classes by their role in tolerance as opposed to immunity (Fig. 1). They comprise 1–3% of CD4+ T-cells in humans and 5–10% of CD4+ T-cells in rodents (Sakaguchi, 2000; Shevach, 2002). Despite the unique suppressive properties of Treg cells compared with other lymphocytes, their cellular features are less distinct. Treg cells are generally identified on the basis of their constitutive expression of surface markers including the interleukin-2 receptor CD25 (Sakaguchi et al., 1995), glucocorticoid-induced tumour necrosis factor receptor (GITR) (McHugh et al., 2002; Shimizu et al., 2002) cytotoxic T-lymphocyte associate protein 4 (CTLA-4) (Takahashi et al., 2000), together with high expression of CD95 and in humans, low expression of CD45RB and CD127 (Akbar et al., 2003; Liu et al., 2006b) (Table II). However, each of these markers can also be dynamically expressed on the surface of other cell populations (Damoiseaux, 2006) and there has been difficulty in identifying a definitive surface marker to distinguish Treg cells from related T-cells.
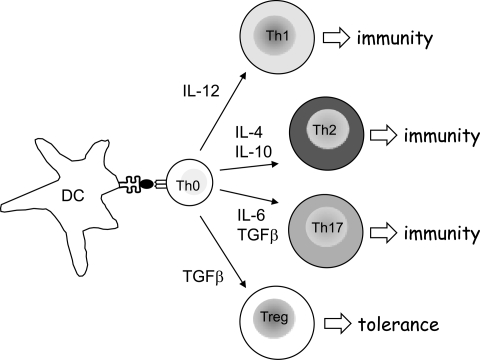
Figure 1.
The microenvironmental context in which naive CD4+ Th0 cells encounter their cognate antigen is a principal determinant of their differentiation fate and development into Treg cells as opposed to Th1, Th2 or Th17 cells.
Treg cells confer a tolerogenic immune response whereas Th1, Th2 and Th17 cells mediate protective immunity. Signals originating from the DC presenting antigen to the Th0 cell, as well as the relative concentrations of key cytokines in the immediate vicinity, are instrumental. DC, dendritic cell; IL, interleukin; Th1, Th2 and Th17, T-helper type 1, type 2 and interleukin 17-producing Th cell; TGF, transforming growth factor.
Table II.
Markers for Treg cells
| Marker | Location | Level of expression by Treg cells | Specificity for Treg cells | Expression by other cell lineages |
|---|---|---|---|---|
| CD25 | Surface | High | ++ | Effector/memory T cells |
| CD95 | Surface | High | ++ | Effector/memory T cells |
| GITR | Surface | High | ++ | Effector/memory T cells |
| CTLA-4 | Surface | High | ++ | Effector/memory T cells |
| CD45RB | Surface | Low | ++ | Effector/memory T cells |
| Foxp3 | Intra cellular | High | +++++ | Trophoblast giant cells |
| Nrp1 | Surface | High | +++ | Neurons |
| LAG-3 | Surface | High | +++ | B cells |
| CD127* | Surface | Low | ++++ | Newly activated T cells |
*Humans only.
The search for a specific marker for Treg cells was aided by the identification of a mutation in a gene that resulted in the fatal human autoimmune disease ‘immune dysregulation polyendocrinopathy, entropathy, X-linked’ (IPEX) and the analogous disease in a spontaneous mutant mouse known as the ‘scurfy’ mouse. The responsible mutation was located in the gene that encodes a transcription factor of the forkhead/winged-helix family, known as Forkhead Box P3 (FOXP3 or scurfin). Null mutation in this gene leads to a functional defect in the resultant protein and consequently the early onset of a severe lymphoproliferative/auto-immune disease (Brunkow et al., 2001). The link between FOXP3 expression and the development and function of the Treg cell was first made by Fontenot et al. who noted that FOXP3 mRNA was elevated in the suppressive CD4+CD25+ lymphocyte population, and went on to demonstrate that Foxp3 null mutant mice lacked Treg cells. Subsequently, it was shown that transfer of CD4+CD25+ lymphocytes rescued Foxp3 null mutant mice from autoimmune pathologies (Fontenot et al., 2003). The critical role of Foxp3 protein in the development, function and origins of Treg cells has been further explored in recent publications utilising a Foxp3gfp knock-in allele, which validated this gene as the ‘master-switch’ for Treg development (Fontenot et al., 2005a, b). Discovery of a definitive marker for Treg cells has allowed investigation of the origin and regulation of these cells, and has facilitated examination of their role in many disease states and physiological conditions.
Ontogeny of Treg cells
The precise origins and pathways of generation of Treg cells are active topics of research. It is becoming evident that there is heterogeneity in the ontogeny of Treg cells, with the processes through which Treg cells are generated, and the tissue in which they originate, being important factors in their suppressive function and target antigen repertoire as mature cells. At least two distinct pathways of Treg generation appear to exist. First, ‘natural’ Treg cells can originate via a selective process in the thymus based on the structure of their individual T-cell receptors (TCRs) (Itoh et al., 1999; Fontenot et al., 2005a). However, the thymus is not the sole source of Treg cells and there is now compelling evidence that the majority are ‘inducible’ Treg cells generated within peripheral tissues, particularly in later life when the thymus undergoes extensive involution (reviewed in Akbar et al., 2007). As a result, the gross pool of Treg cells at any one time is the sum of the cells selected for survival in the thymus and those cells generated in the periphery.
Treg cell generation in the thymus
The fate of T-cells differentiated in the thymus is ultimately determined by the varying avidities for self-antigens of the TCRs expressed on their surface. T-cell survival in the thymus is the result of a sequential selection process based on the interaction between naive T-cells and the thymic stromal epithelium. Depending on the avidity of the interaction between the TCR of an individual T-cell and the MHC/self-antigen peptide complex expressed by stromal cells, neglect, positive selection or negative selection can ensue (von Boehmer et al., 1989). Failure to interact with MHC molecules presenting self-antigen on the thymic epithelial cells leads to apoptosis of the T-cell through the lack of TCR signalling (neglect). Positive selection is the result of a TCR signal of sufficient avidity to signify a T-cell's ability to recognize self-MHC complexes, whereas a high avidity TCR/antigen interaction is indicative of excessive reactivity to self and hence a potentially pathological self-reactive T-cell, leading again to apoptosis of the T-cell (negative selection). In summary, ‘the thymus selects the useful, neglects the useless and destroys the harmful’ (von Boehmer et al., 1989).
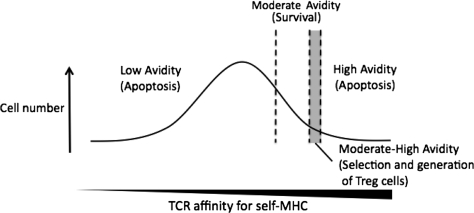
The generation of natural Treg cells in the thymus is believed to occur as the result of an altered negative selection process. Commitment of naive T-cells to Treg cell differentiation is thought to result when their TCR/antigen affinity is just weaker that that needed for negative selection, but at the extremity of the spectrum for positive selection (Jordan et al., 2001) (Fig. 2). In other words, Treg cells derived from the thymus are selected largely on the basis of their capacity to interact with self-antigens, and this interaction is implicit in their role for protection against pathological self-reactive immune responses. Thymic-generated Treg cells are thus thought to function primarily in protection from a range of autoimmune diseases (reviewed in Sakaguchi, 2005).
Figure 2.
Treg cells are selected in the thymus when the avidity of their TCR for self-MHC is lower than the threshold for negative selection by apoptosis, but higher than the threshold for positive selection of effector T cells.
Treg cell generation in peripheral tissues
Maintenance of Treg cell numbers over the human life span, despite the extensive and early involution of the thymus, indicates an alternate source of Treg cell generation independent of the thymus. Peripherally, there appears to be both de novo generation of inducible Treg cells and maintenance and expansion of the existing Treg cell pool (Seddon and Mason, 1999; Cozzo et al., 2005). The role of peripheral tissues in sustaining Treg cell populations was elegantly demonstrated by the observation that ablation of a tissue depletes the ability of donor Treg cells to prevent organ-specific autoimmune disease after adoptive transfer into intact recipients, compared with Treg cells from unmodified donors (Seddon and Mason, 1999). This shows that the presence of peripheral tissue antigens is essential for the de novo generation of antigen-specific regulatory T-cells from naive T-cell precursors (Seddon and Mason, 1999). The importance of tissue-specifc antigens for generation of Treg cells to protect against autoimmunity is also shown in other tissues, including the ovary (Samy et al., 2006) (see later). A similar conclusion is drawn from TCR transgenic mouse models, which show that with persistent low levels of antigenic stimulation, naive cells can be induced to express the hallmark Treg cell marker Foxp3 and take on a suppressive phenotype (Abbas et al., 2007).
A related explanation invokes a role for peripheral tissue antigens in providing a maintenance signal for existing Treg cells through promoting proliferation and survival after TCR engagement. Although it is widely reported that Treg cells are characteristically anergic following TCR stimulation in vitro, adoptive transfer experiments show that these cells can proliferate in vivo (Gavin et al., 2002; Fisson et al., 2003; Walker et al., 2003), suggesting their proliferation contributes to maintaining and expanding the in vivo Treg pool. Critically, proliferation is dependent on the presence of cognate antigen for the Treg TCR (Walker et al., 2003). The likely reality is that peripheral antigens are critical for both the generation of new Treg cells and the maintenance of pre-existing Treg cells.
Although the role of peripheral tissues in Treg cell generation is established in rodent models, a new understanding of human peripheral Treg cell generation is evolving. Recently, it has emerged that FOXP3 expression is a constitutive product of human (but not mouse) T-cell activation, although typically expression is transient and rapidly down-regulated (Wang et al., 2007). This has led to speculation that FOXP3 induction and subsequent suppression might be a default pathway in the activation of all human T-cells (Pillai and Karandikar, 2007); however, debate continues over the suppressive qualities of transiently FOXP3+ T-cells (Allan et al., 2007). Constitutive expression of FOXP3 during T-cell activation supports the plausibility of peripheral Treg cell generation being the predominant pathway in humans, but raises the question of how and why FOXP3 expression is extinguished in some cells but not others.
Importantly, the pathway of peripheral Treg cell generation provides a mechanism by which these cells might be generated with affinities for antigens not expressed in the thymus. Instead, peripherally generated Treg cells can express TCRs restricted to specific peripheral tissue antigens. This enables the immune system to regulate responses to exogenous antigens that are foreign to self, but against which aggressive responses are not appropriate, and equips the immune system with plasticity in the Treg cell repertoire facilitating dynamic change and adaptation to the environment. Importantly for reproductive events, this property allows the generation and expansion of Treg cell populations with affinities for reproductive antigens associated with the developing conceptus or expressed by sperm or oocytes, which are absent from the thymus.
Treg cell control by dendritic cells, co-stimulatory signals and indoleamine 2,3-dioxygenase
The microenvironmental context in which naive CD4+ Th0 cells encounter their cognate antigen is the principal determinant of their differentiation fate and development into Treg cells as opposed to Th1, Th2 or Th17 cells (Fig. 1) (Steinman et al., 2003; Rutella and Lemoli, 2004; Zhu and Paul, 2008). Dendritic cells (DCs) are professional antigen-presenting cells which exhibit considerable heterogeneity in their ontogeny, maturation status and accompanying functional phenotype, reflected in the combination of surface signalling molecules and cytokines they express (Morelli and Thomson, 2003). The dialogue between Treg cells and a specific class of DCs termed ‘tolerogenic DCs’ is pivotal in the activation and expansion of Treg cells (Steinman et al., 2003). Initially tolerogenic DCs were defined on the basis of their immature or semi-mature phenotype, altered expression of co-stimulatory molecules CD80 and CD86, and lack of expression of the Th1-inducing cytokine IL-12 (Steinman et al., 2003), but even mature DCs can drive Treg cell proliferation when differentiated appropriately (Yamazaki et al., 2003).
Certain co-stimulatory signals on DCs can down-regulate Treg-mediated suppression. Members of the tumour necrosis factor (TNF) receptor superfamily, including GITR, OX40, 4-1BB and RANK are expressed by Treg cells and their ligation can block suppression, increase proliferation, or both (Choi et al., 2004; Kanamaru et al., 2004; Valzasina et al., 2005).
The cytokine environment is critical in controlling DC phenotype and hence the signals sent to Treg cells. DCs differentiated in the presence of TGFβ, IL-10, granulocyte-macrophage colony-stimulating factor (GM-CSF) and IL-4 possess the immunotypic and functional features of immature DCs and reliably induce CD4+CD25+ Treg cells with immunosuppressive function (Sato et al., 2003).
Another important characteristic of tolerogenic DCs is expression of indoleamine 2,3-dioxygenase (IDO). In plasmacytoid DCs, IDO expression confers the ability to directly activate resting Tregs for potent suppressor activity, and is implicated in converting CD4+CD25+Foxp3+ Tregs from CD4+CD25− T-cells and maintaining Treg suppressive activity both in mice (Sharma et al., 2007) and in humans (Chen et al., 2008). This is additional to the ability of IDO-expressing DCs to dominantly inhibit T-cell activation by other non-suppressive DCs (Munn et al., 2004). Bi-directional signalling between Treg cells and tolerogenic DCs may be one means of infectious tolerance, since Treg cells can condition DCs to express IDO and thereby exert a suppressive influence over neighbouring T-cells (Grohmann et al., 2002; Munn et al., 2002). Induction of IDO may occur via ligation of the costimulatory molecule B7 (CD80/CD86) by CTLA-4, a molecule constitutively expressed on Treg cells, with this pathway ultimately also interfering with DC capacity to activate effector T-cell function (Grohmann et al., 2002).
Cytokines, prostaglandins and toll-like receptors in Treg cell generation
Like all T-cells, Treg cells require ligation of their TCR with cognate antigen and IL-2 in order to differentiate from naive CD4+ T-cell precursors. Studies in IL-2-deficient mice show that IL-2 is essential for Treg cell generation, and whereas high concentrations of IL-2 can block suppression, low levels of IL-2 modulate their development and maintenance (Scheffold et al., 2005). IL-15 can substitute for IL-2 in Treg generation, and potentiates Treg cells for further rounds of IL-15-induced proliferation (Koenen et al., 2003).
A crucial question is the nature of the cytokines and environmental signals that cause fate commitment to Treg cells, rather than Th1, Th2 or Th17 phenotypes. One key factor is TGFβ, a cytokine long recognized to have immune suppressive and anti-inflammatory properties (Gorelik and Flavell, 2002). There is evidence that TGFβ acts to override the default pathway that generates T-cells with no suppressive capabilities (Sakaguchi, 2000; Shevach, 2002). Naive CD4+CD25− T-cells differentiate into a suppressor T-cell phenotype and express Foxp3 when TGFβ is present at the time of TCR challenge (Chen et al., 2003). TGFβ is also implicated in proliferation of mature Treg cells through modifying the function and signalling capabilities of DCs (Ghiringhelli et al., 2005b). Prostaglandin E2 (PGE2) may synergize with TGFβ in this role, since in vitro experiments indicate that PGE2 can enhance the inhibitory capacity of human CD4+CD25+ Treg cells and induce a regulator phenotype in CD4+CD25− T-cells (Baratelli et al., 2005).
Additional cytokines, including several prominently expressed in the implantation site and gestational tissues, can modulate Treg cell proliferation and suppressive function (reviewed in Sutmuller et al., 2006b; Miyara and Sakaguchi, 2007). IL-4 and IL-7 are considered growth and survival factors, respectively (Thornton et al., 2004; Harnaha et al., 2006). IL-1 and IL-6 can release resting Treg cells from their anergic state and potentiate responsiveness to proliferative signals (Kubo et al., 2004), whereas IL-12 and IL-6 can reverse the suppressive function of Treg cells and rescue Th1 cells from Treg control (Pasare and Medzhitov, 2003; King and Segal, 2005).
An emerging area of central interest is the relationship between Treg cells and pro-inflammatory IL-17-producing T (Th17) cells which, like Th1 cells, are implicated in many autoimmune and inflammatory diseases (Zhu and Paul, 2008). Treg cells and Th17 cells appear to share a common lineage with their relative abundance influenced dramatically by the cytokine environment in which T-cell priming occurs, particularly the ratio of IL-6 to TGFβ (Bettelli et al., 2006). In the absence of IL-6, TGFβ1 simultaneously induces synthesis of both Foxp3 and the Th17 cell master switch, retinoic acid-related orphan receptor γt (RORγt). Foxp3 then directly interacts with RORγt to suppress the conversion of naive T-cells to Th17 cells (Ichiyama et al., 2008). However, in the presence of IL-6, Foxp3 expression is down-regulated, allowing RORγt to induce IL-17 synthesis and the conversion of naive T-cells to Th17 cells. IL-1 can also drive commitment to Th17 as opposed to Treg cells (Yang et al., 2008b). Existing Treg cells, in the absence of sufficient TGFβ1, can function as inducers of Th17 cells and themselves convert to Th17 cells (Xu et al., 2007). This mutual antagonism and plasticity between Treg and IL-17 cells illustrates the fine line between a suppressive or pro-inflammatory immune outcome, and the major importance of the cytokine environment not only at the outset but for the duration of the response.
Toll-like receptors (TLRs) are expressed by Treg cells and are emerging as key modulators of Treg cell proliferation and behaviour through conferring the ability to sense pathogens and either strengthen or reverse suppressive activity (reviewed by Sutmuller et al., 2006b). Ligation of these by pathogen-associated molecular patterns or other TLR ligands such as heat shock proteins leads to a range of different outcomes. Notably, TLR2 ligands increase Treg cell numbers through potentiating their release to antigen-stimulated activation (Sutmuller et al., 2006a). Proliferation of Treg cells exposed to TLR2 ligands is accompanied by loss of suppressive function, but withdrawal of the TLR2 stimulus results in immediate recovery of suppressive ability (Sutmuller et al., 2006a). Similarly, ligation of TLR8 abrogates Treg suppression (Peng et al., 2005), but in contrast, TLR5 ligation enhances suppressive capacity (Crellin et al., 2005). TLR9 ligands such as CpG oligodeoxynucleotides can promote Treg cell generation through stimulating plasmacytoid DCs to increase expression of costimulatory molecule B7, MHC class II and IDO (Chen et al., 2008).
Mechanisms of immune suppression by Treg cells
The mechanisms by which Treg cells exert their suppressive action are still being defined. Treg cells have an extensive and diverse target cell repertoire, and heterogeneous pathways operate depending on the tissue and the identity of the target cell against which suppression is directed. Initially, suppression of activation and proliferation of CD4+ T-cells was thought to comprise the principal function of Treg cells (Thornton and Shevach, 1998). However, Treg cells are now known to inhibit proliferation and cytokine production in both CD4+ and CD8+ T-cells (Piccirillo and Shevach, 2001), to suppress B-cell proliferation and immunoglobulin production (Lim et al., 2005), to inhibit cytotoxic function of natural killer (NK) cells (Ghiringhelli et al., 2005a) and inhibit maturation and function of antigen presenting cells including DCs and macrophages (Cederbom et al., 2000; Misra et al., 2004; Taams et al., 2005). Thus, Treg cells can target several stages of the adaptive immune response, spanning the events of lymphocyte activation and proliferation, through to effector function.
Like all T-cells, Treg cells require engagement of their TCR with cognate antigen to activate their full effector function (Thornton and Shevach, 1998). In this regard, Treg cell suppression is antigen-specific, with both pre-existing and newly generated Treg cells needing to encounter antigen in order to exert their suppressive effects. The presence of IL-2 or IL-4 is also critical for Treg cell activation and facilitates further rounds of antigen-driven Treg cell proliferation (Thornton et al., 2004). However, once activated, Treg cells are capable of targeting other cells in the vicinity and exerting suppression in an antigen non-specific manner (Thornton and Shevach, 2000; Karim et al., 2005).
A major obstacle hindering the definition of Treg cell suppressive action is their apparent multiple and redundant effector mechanisms (Miyara and Sakaguchi, 2007). The general consensus is that unlike other types of regulatory T-cells, Treg cells suppress largely in a contact-dependent manner (Annunziato et al., 2002). Their in vivo and in vitro activities may differ, with in vivo experiments implicating TGFβ and IL-10 in paracrine actions that augment their contact-dependent mechanism of suppression (reviewed in Wahl et al., 2004a).
Different suppressive mechanisms most likely operate synergistically. It has recently been shown that Treg cells can act as an IL-2 ‘sponge’, competitively depriving adjacent T-cells of autocrine IL-2, and thus preventing the IL-2-dependent processes of T-cell activation and proliferation (de la Rosa et al., 2004; Scheffold et al., 2005). Additional suppression is mediated by paracrine cytokine production or by cell-to-cell contact either directly between Treg cells and target/effector cells or via third-party cells such as antigen-presenting cells (Thornton and Shevach, 1998; Taams et al., 2005). Contact-mediated suppression results from ligation of a range of Treg surface molecules, namely CTLA-4, membrane-bound TGFβ and lymphocyte-activation gene 3 (Tivol et al., 1995; Gorelik and Flavell, 2000; Takahashi et al., 2000; Huang et al., 2004).
A unique property of Treg cells is their ability to transfer suppressive capabilities to other cellular subsets in a phenomenon known as bystander suppression (Jonuleit et al., 2002). This can be achieved through Treg cells conferring upon target cells the ability to inhibit downstream steps in the immune cascade. For example, Treg cells can modify the phenotype of DCs to become tolerogenic DCs, or induce T cell production of suppressive cytokines such as IL-10 (Hubert et al., 2002). This likely explains the notion of infectious tolerance, a process by which suppression to a third-party antigen can be induced via physical association of that antigen with a previously tolerated antigen (reviewed in Waldmann et al., 2006). This is illustrated when animals of strain A that are rendered tolerant to grafts from strain B demonstrate prolonged tolerance of subsequent grafts from (B×C) F1 animals, and eventually tolerate grafts from strain C animals (Davies et al., 1996; Waldmann et al., 2006). Such a process allows for a limited repertoire of antigens to induce a dominant tolerant state to a much larger range of antigens that may subsequently be encountered in the same tissue site. This characteristic feature might be of special relevance in reproductive tissues where a variety of antigens would be encountered in association with gametes and the developing gestational tissues. Mast cells, which are abundant in the uterus, have also been implicated as crucial intermediaries of Treg cell tolerance in allograft tissue, operating through secretion of IL-9 (Lu et al., 2006).
Regulatory T-cells in reproductive processes
The unique immunological challenges of reproduction are comparable with situations where mature peripheral tissues express physiological self-antigens that require tolerance, despite their absence of expression in the thymus. Both sperm and oocytes express a range of antigens such as late ontogeny lactate dehydrogenase c4 and the zona pellucida proteins, respectively, that can induce activity autoimmune orchitis and oophoritis when administered to naive recipients (Garza et al., 2000). Similarly, despite modulated expression of MHC antigens by placental cells (Trowsdale and Betz, 2006), the maternal system shows evidence of activation against paternal MHC and minor antigens during pregnancy in mice (Tafuri et al., 1995; Zhou and Mellor, 1998) and women (Bertrams et al., 1971). Peripheral tolerance mechanisms are clearly involved in preventing maternal immune rejection of the fetus in pregnancy (Trowsdale and Betz, 2006). The qualities and functions of regulatory T-cells make these cells perfectly suited to controlling the immune response to reproductive antigens, and there is now substantial evidence confirming their important roles in regulating tolerance to male and female gametes and to the conceptus.
Treg cells in the testes and ovary
The ovary has been informative in understanding the roles of Treg cells in protecting tissues expressing reproductive antigens from autoimmune destruction. In mice, removal of the thymus shortly after birth causes spontaneous ovarian autoimmune disease, but this can be prevented by passive transfer of T-lymphocytes from spleens of normal adult mice (Samy et al., 2006). The protection-conferring population is now known to be CD4+CD25+Foxp3+ Treg cells, and importantly, cells from females are intrinsically more potent suppressors than cells from males, particularly when retrieved from the lymph nodes draining the ovary (Samy et al., 2005). The gender-specific effect can be reversed if males are grafted with ovaries prior to recovery and transfer of Treg cells (Samy et al., 2006), showing the antigen-specific nature of the Treg suppressive activity and the necessity for persistent presence of the cognate tissue antigen in generating the ovary antigen-specific Treg cells. Autoimmune ovarian disease is believed to result from operational failure of the normal immune regulatory mechanisms required for normal tissue homeostasis (Alard et al., 2001).
The converse situation occurs with male reproductive antigens, where spleen cells from normal male donors are more effective in suppressing epididymitis and orchitis than the Treg cells from female or neonatally orchidectomized donors (Taguchi and Nishizuka, 1981), indicating that native testicular tissue is required to generate suppressive cells specifically targeted to antigens in that tissue. The testes appear to have particular physical properties that confer a bias towards generation of Treg cells rather than memory T-cells compared with other sites such as the kidney capsule (Nasr et al., 2005), an observation that at least partly explains the long-recognized concept of testicular immune privilege. Interestingly, Sertoli cells may be instrumental in activating testicular Treg cell responses due to their expression of the immune-regulatory co-stimulatory molecule programmed death ligand 1 (PDL1, also known as CD274 or B7-H1) which binds programmed death 1 (PD1) expressed by Treg cells and inhibits proliferation of CD8+ T-cells (Dal Secco et al., 2008).
Treg cells in rodent models of pregnancy
The first report implicating Treg cells in pregnancy appeared in 2004, when it was shown that CD4+CD25+ cells increase in number in the blood and lymph nodes of pregnant mice (Aluvihare et al., 2004). An expanded Treg cell pool is detectable in lymph nodes draining the uterus from as early as 2 days after mating, whereas elevated blood levels do not become evident until after implantation (Aluvihare et al., 2004). The increase in Treg cells is associated with accumulation of Foxp3+ cells and Foxp3 mRNA expression in the uterus, as well as elevated lymphocyte suppressive function in the spleen and lymph nodes. The systemic expansion in Treg cell populations occurs independently of fetal alloantigens, since Treg cell numbers are elevated over non-pregnant levels in both syngeneic and allogeneic pregnancies, suggesting involvement of factors such as pregnancy hormones (Aluvihare et al., 2004). However, conceptus alloantigen leads to a greater increase in Treg cell numbers, and is associated with specific suppression of anti-paternal alloantigen reactivity (Zhao et al., 2007). The early increase in Treg cell numbers even prior to embryo implantation was confirmed in another study (Thuere et al., 2007). Interestingly, the increase in Treg cells is not sustained throughout pregnancy but progressively declines from mid-gestation to return to non-pregnant levels by fetal delivery at term (Zhao et al., 2007). CD8+ regulatory cells have also been implicated in suppression of fetal immune rejection from early pregnancy in mice (Clark et al., 1994; Blois et al., 2004a).
The physiological necessity of Treg cells for pregnancy was elegantly demonstrated using an adoptive transfer model, wherein complete T-cell populations or populations depleted of CD4+CD25+ Treg cells were transferred into pregnant T-cell-deficient mice (Aluvihare et al., 2004). In the absence of Treg cells, allogeneic fetuses were uniformly rejected, whereas syngeneic fetuses were unaffected (Aluvihare et al., 2004). These findings were confirmed in another approach using passive transfer of CD25-reactive PC61 monoclonal antibody to deplete CD25+ cells in vivo (Darrasse-Jeze et al., 2006). When mice mated with allogeneic or syngeneic males were administered PC61 on the day of mating, activated CD8+ and CD4+ cell populations were expanded in the lymph nodes draining the uterus and fewer allogeneic fetuses survived to term, whereas no effect on syngeneic pregnancies was observed (Darrasse-Jeze et al., 2006). Collectively, these studies support the notion that Treg cells are required to suppress maternal immune responses targeted against fetal alloantigens, rather than male-specific or trophoblast-specific minor histocompatibility antigens.
In a further demonstration of the importance of Treg cells for maternal–fetal tolerance, fewer CD4+CD25+ cells associated with elevated Th1 cell activity were found in the decidual tissues of abortion-prone CBA/J mice mated with DBA/2J males. Adoptive transfer of Treg cells, purified from normal pregnant mice, elevated decidual Foxp3 mRNA levels and prevented fetal loss (Zenclussen et al., 2005). Interestingly, transfer of Treg cells from non-pregnant normal mice to the abortion prone mice was ineffective, and transfer of Treg cells on or after day 4 of pregnancy did not prevent abortion (Zenclussen et al., 2005). Consistent with this, depletion of Treg cells using PC61 during the first 2 days of pregnancy led to implantation failure (Zenclussen et al., 2005). Together, these findings show that Treg cells are essential during the first days of pregnancy, even prior to the time of embryo implantation.
Transfer of exogenous Treg to abortion-prone mice was associated with elevated expression of leukaemia inhibitory factor, TGFβ and heme oxygenase-1 at the maternal–fetal interface, whereas IDO as well as Th1 cytokines interferon-γ (IFNγ) and TNFα were unchanged (Zenclussen et al., 2006). These data suggest molecular mechanisms of Treg cell operation are not necessarily restricted to limiting Th1 cells or pro-inflammatory cytokine expression. An interaction between PDL1-expressing decidual cells and PD1 on Treg cells is also essential for Treg-mediated protection of alloantigenic fetuses, since adoptive transfer of Treg cells from wild-type mice reversed the high incidence of alloantigen-expressing fetal death in PDL1 null mutant mice (Habicht et al., 2007).
Treg cells in human pregnancy
Several studies have examined the dynamics of lymphocyte subpopulations during pregnancy in women. An increased expression of CD25 on decidual lymphocytes compared with peripheral blood lymphocytes was described in 1992 (Saito et al., 1992). Later, decreased CD25 expression in decidual tissue of normal pregnancies compared with luteal phase tissue was reported (Chao et al., 2002). However, these studies examined CD25+ cells, without regard to markers definitively identifying Treg cells.
The first observations on CD4+CD25+ cells in human pregnancy described an increase in this subset in early pregnancy decidual tissue (Sasaki et al., 2003). Other reports demonstrated an increase in circulating CD4+CD25+ cells during early pregnancy with a peak phase at the second trimester and a decline post-partum to levels slightly higher than pre-pregnancy levels (Heikkinen et al., 2004; Somerset et al., 2004). The elevation during the first and second trimesters has been confirmed in studies more precisely identifying Treg cells as CD25high cells (Sasaki et al., 2004; Saito et al., 2005; Tilburgs et al., 2006; Zhao et al., 2007), and a clear decline in CD4+CD25high Treg cells occurs during the weeks just prior to delivery (Zhao et al., 2007). The CD4+CD25+ T-cells comprising the expanded pool in pregnancy are highly enriched for FOXP3 and exert suppressive function in vitro (Somerset et al., 2004). Furthermore, cells expressing the Treg cell activation marker CTLA-4 are more prevalent in peripheral blood and term deciduas of normal healthy pregnant women compared with non-pregnant women (Heikkinen et al., 2004). Several studies report that Treg cells accumulate in decidual tissue at densities greater than in peripheral blood (Sasaki et al., 2004; Tilburgs et al., 2006). Treg cells from peripheral blood of pregnant and non-pregnant women suppress anti-alloantigen responses in vitro, with differential capacity to suppress anti-paternal as opposed to irrelevant alloantigen responses (Mjosberg et al., 2007).
As in mice, Treg cell numbers in women decline as term approaches. The percentage of CD3+ lymphocytes that express CD4 and CD25 are significantly decreased in deciduas in spontaneous vaginal delivery compared with elective Caesarean section (Sindram-Trujillo et al., 2004). These findings were recently confirmed by a study showing a sharp decrease in CD4+CD25high Treg cells towards the end of pregnancy and an increase in CD4+CD25low T-cells (Zhao et al., 2007). This implies a potential role for Treg cells in the immunological changes preceding labour, and prompts speculation that their decline might be a causal factor in fetal expulsion from the maternal tissues. However, studies using more specific markers and animal models are needed to address the possibility of any active role of Treg cells in parturition.
Treg cells in infertility, miscarriage and pregnancy complications
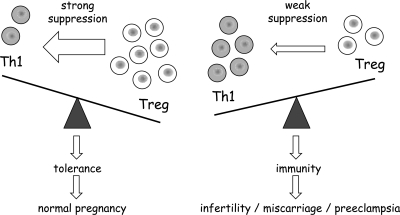
Several studies report an association between Treg cell paucity and complications of pregnancy (Fig. 3), particularly pre-eclampsia. There is abundant evidence that immunological factors are crucial for the development of this common disease, which in developed countries is responsible for ∼15–20% of maternal mortality (Sargent et al., 2006a). In pre-eclampsia, Th1 dominance develops together with an increased inflammatory response towards the fetus (Saito and Sakai, 2003; Sargent et al., 2006a), raising the question of whether this might be secondary to impaired function or decreased numbers of Treg cells.
Figure 3.
Deficiency in Treg cell numbers and/or suppressive function are associated with infertility, recurrent spontaneous abortion and pre-eclampsia in women.
Studies in mouse models show that in normal pregnancy, adequate Treg cell function acts to suppress Th1-mediated maternal attack of the semi-allogeneic conceptus, but Treg cell depletion leads to insufficient suppression and Th1-mediated fetal loss.
Initially, it was reported that the number of CD3+CD25+ lymphocytes is decreased in peripheral blood of women with gestational-induced hypertension and especially in the event of pre-eclampsia (Mahmoud et al., 2003); however, no Treg cell specific markers were used to confirm this. Although another study found no association between pre-eclampsia and changes in peripheral blood Treg cell levels (Paeschke et al., 2005), several subsequent studies have reported that CD4+CD25high T-cells are significantly reduced in both the peripheral blood and decidual tissue of pre-eclamptic patients compared with normal pregnant women (Darmochwal-Kolarz et al., 2007; Sasaki et al., 2007). Observations that the tryptophan catabolizing enzyme IDO is decreased in pregnancies complicated by pre-eclampsia is consistent with diminished Treg cell activity in pregnancy (Santoso et al., 2002; Nishizawa et al., 2007), with decreased IDO potentially caused by, and contributing to, insufficient Treg cell activity (Grohmann et al., 2002). A preliminary report suggests a possible bias towards Th17 cells over Treg cells in women suffering third trimester pre-eclampsia (Santner-Nanan et al., 2008).
Recurrent spontaneous miscarriage has also been associated with a mal-adaptation in the maternal immune system (Laird et al., 2003). Several studies report increased numbers of CD3+CD25+ cells in the decidua at the time of spontaneous abortion compared with decidua recovered at therapeutic abortion (Vassiliadou et al., 1999; Quack et al., 2001). However, the proportion of Treg cells among these cells is evidently reduced, since both decidual and peripheral blood CD4+CD25high T-cells are lower in tissues recovered after spontaneous abortion compared with induced abortions and non-pregnant women (Sasaki et al., 2004; Yang et al., 2008a). Reduced responsiveness to pregnancy-associated expansion of Treg cell populations, due to numerically fewer Treg cells as well as Treg functional deficiency, may underpin a reduced immunosuppressive capability and cause predisposition to miscarriage. In a comprehensive study, women experiencing repeated miscarriage were shown to have a reduced frequency of Treg cells within the peripheral blood CD4+ pool, and reduced suppressive capacity, compared with normal fertile women (Arruvito et al., 2007).
Primary unexplained infertility has also been associated with reduced expression of FOXP3 mRNA in endometrial tissue (Jasper et al., 2006), suggesting that impaired recruitment of Treg cells, or insufficient differentiation of uterine T-cells into Treg cells even prior to conception may affect the capacity to establish pregnancy in women.
Origin and antigen specificity of Treg cells in pregnancy
Defining the pathways of Treg generation and the consequences for specific functional roles is critical for understanding how Treg cells operate in reproductive processes, and for designing possible interventions to exploit these cells to improve fertility and pregnancy outcomes. We have only incomplete knowledge of the tissue origins of decidual Treg cells and the roles of conceptus antigens and other factors including cytokines and hormones in driving their expansion in early pregnancy, but there is sufficient emerging information to build a working model (Fig. 4).
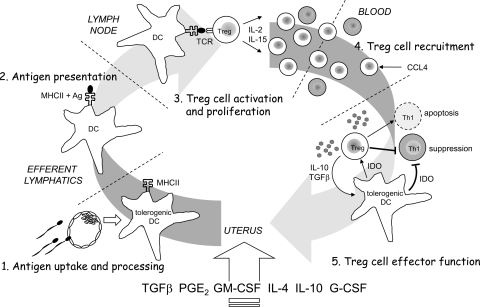
Figure 4.
A working model of the key steps in the induction and effector pathways of Treg cell activation, expansion and suppressive function to mediate maternal–fetal tolerance.
The sequence of events includes (1) antigen uptake and processing within tolerogenic DCs; (2) trafficking of DCs to draining lymph nodes and presentation of antigen fragments on the surface of the DC in association with MHC molecules; (3) interaction between the DC and Treg cells expressing cognate TCRs in the presence of IL-2 and/or IL-15 to elicit their activation and proliferation; (4) recruitment of Treg cell populations from the maternal circulation into the decidual tissue mediated by CCL4 and (5) exertion of specific effector functions, including secretion of IL-10 and TGFβ, and inducing IDO expression in target DCs to further activate and maintain suppressive function in Treg cells, inhibit Th1 cell proliferation and induce Th1 cell apoptosis. Specific cytokines including TGFβ, GM-CSF, IL-4, IL-10, G-CSF and prostaglandin E known to predominate the uterine cytokine milieu are identified as regulators of tolerogenic DCs. Ag, antigen; CCL4, chemokine (C–C motif) ligand 4; DC, dendritic cell; G-CSF, granulocyte colony-stimulating factor; GM-CSF, granulocyte-macrophage colony-stimulating factor; IDO, indoleamine 2,3-dioxygenase; IL, interleukin; MHC, major histocompatibility complex; TGF, transforming growth factor.
In both mice and women, there is evidence of ovarian hormone-regulated fluctuations in uterine Treg cell populations. In mice, administration of 17-β-estradiol (E2) to ovariectomized mice causes elevation in Treg cell numbers and Foxp3 mRNA expression, and in vitro experiments using CD4+CD25− cells show direct induction of Foxp3 by E2 (Polanczyk et al., 2004). Treg cells accumulate in the uterus during the estrus phase of the reproductive cycle as evidenced by elevated Foxp3 mRNA expression, potentially in response to estrogen-induced expression of several chemokines that target the CCR5 chemokine receptor expressed by Treg cells (Kallikourdis and Betz, 2007). In women, a comparable expansion in CD4+CD25+FOXP3+ Treg cells occurs in the peripheral blood during the late follicular phase of the menstrual cycle, when cell abundance tightly correlates with serum E2 levels, and then is followed by a dramatic decline at the luteal phase (Arruvito et al., 2007). Direct actions of E2 on Treg proliferation and suppressive function may contribute to these cycle-related fluctuations (Prieto and Rosenstein, 2006). Thus, each reproductive cycle elicits a relative expansion of Treg cell populations. However, it is important to note that since Treg cells require exposure to antigen to exert their full suppressive function, estrogen alone would be insufficient to activate Treg cells for pregnancy, and instead can be viewed as potentiating Treg cells in preparation for stimulation by pregnancy-associated antigens.
The Treg cell pool is further expanded during early pregnancy in mice and humans and several observations suggest that they have a key protective role when the maternal tissues first come into contact with conceptus antigens associated with invading placental trophoblast cells. Both antigen-associated and antigen-independent mechanisms are likely to contribute to the further expansion in Treg cell populations observed in early pregnancy. The thymus appears not to be the origin of the elevated numbers of Treg cells in pregnancy (Zhao et al., 2007), so by default a peripheral tissue pathway of generation must occur, in line with studies implicating the uterus draining lymph nodes as the predominant site of Treg pool expansion (Zhao et al., 2007). The relatively elevated numbers of Treg cells in tissues of mice bearing allogeneic pregnancies (Kallikourdis et al., 2007; Zhao et al., 2007) suggest fetal alloantigens act to drive Treg cell proliferation. Non-MHC antigens and non-classical MHC molecules expressed by placental trophoblast cells are implicated, and indeed a population of CD8+ T cells with regulatory properties that is activated in response to co-stimulation by the carcinoembryonic antigen family present on trophoblast cells has been described in women (Shao et al., 2005). Heat shock protein-60 (HSP-60) is another candidate trophoblast protein for T-cell recognition (Heyborne et al., 1994) and is identified as a target antigen for Treg cells in atherosclerosis (Yang et al., 2006). Since antigen presenting cells expressing human leukocyte antigen-G (HLA-G) preferentially induce suppressive activity in CD4+ T-cells (LeMaoult et al., 2004), it is possible that trophoblast cell HLA-G also acts to influence the number of Treg cells in the implantation site. Furthermore, PDL1 is strongly expressed by human placental trophoblast cells and a role in influencing cytokine expression by decidual regulatory T-cells is indicated (Taglauer et al., 2008).
Antigen-driven proliferation of Treg cells is evident in lymph nodes draining the uterus, and might also occur within the decidual tissue, where abundant populations of mature myeloid DCs capable of presenting trophoblast cell antigens are present (Blois et al., 2004c). These DCs express markers indicative of a tolerogenic phenotype (Blois et al., 2007b) which is likely to be maintained by the GM-CSF, IL-10 and IL-4-dominated cytokine environment of the decidual tissue (Robertson, 2000). A notable role for an immunoregulatory glycan binding protein, galectin-1 in inducing tolerogenic DCs and supporting their capacity to generate decidual Tr1 cells is shown by loss of allogeneic pregnancies in mice deficient in galectin-1 (Blois et al., 2007a).
The mechanisms for recruitment of Treg cells in the decidual tissue after embryo implantation are likely to be modified compared with the non-pregnant state. Expression of chemokine (C–C motif) receptor 5 (CCR5) may facilitate accumulation and retention of antigen-activated effector Treg cells in the implantation site since Treg cells in the gravid uterus are predominantly CCR5+. This marker is associated with a highly suppressive phenotype and may be a marker for those cells that have been activated by paternal alloantigen (Kallikourdis et al., 2007). One CCR5 ligand in particular, chemokine (C–C motif) ligand 4 (CCL4), is intensely expressed in the gravid uterus and may mediate the further selective accumulation of these cells in pregnancy (Kallikourdis and Betz, 2007). The Treg cells that accumulate in the decidual tissue in pregnancy show specificity in their suppressive function for fetus alloantigens, indicating there is preferential recruitment from maternal peripheral blood, or possibly local expansion of Treg cells reactive with conceptus tissue (Tilburgs et al., 2008).
Consistent with a possible role for normal embryonic development in regulating Treg numbers, CD25+CD3+ cells are decreased in the decidual tissues of women with ectopic pregnancies, compared to tissues from women with normal pregnancies, while numbers in the peripheral blood were unchanged (Ho et al., 1996). However, interpretation of this study is limited by lack of utilization of a specific marker for Treg cells. Conversely, Treg cells were more abundant in implantation sites in partial and complete molar pregnancies, where Treg cell numbers positively correlated with CD8+ cytotoxic T-cells (Nagymanyoki et al., 2007). An intact conceptus may therefore not be required for recruitment of Treg cells, but a role for trophoblast antigens or immunoregulatory agents seems likely.
Role of seminal fluid in activating Treg cells for pregnancy
Exposure to paternal alloantigen occurs in two waves in the reproductive process—initially during transmission of seminal fluid at coitus (Robertson and Sharkey, 2001), and secondly when placental trophoblast cells invade maternal tissues after embryo implantation (Redline and Lu, 1989; Jaffe et al., 1991). This raises the possibility that male alloantigens present in seminal fluid may contribute to activating and expanding the antigen-specific Treg cell pool prior to conceptus antigen encounter. CD4+CD25+ Treg cell abundance increases within days after mating in mice (Aluvihare et al., 2004) and there is evidence of antigen specificity in the Treg cell response even before embryo implantation (Kallikourdis et al., 2007; Zhao et al., 2007). In both mice and women, seminal fluid elicits an inflammation-like response in the female reproductive tract associated with recruitment of DCs into the endometrial and cervical tissues (Robertson et al., 1996; Robertson, 2005, 2007; Sharkey et al., 2007). These DCs are capable of processing male antigens in seminal fluid and activating T-cells in draining lymph nodes (Johansson et al., 2004). Recent observations in mice exposed to seminal fluid in the absence of conception support a role for seminal fluid in driving Treg cell activation and proliferation, resulting in which promotes tolerance of paternal alloantigens at the time of embryo implantation (Robertson et al., 2009). The high levels of TGFβ and prostaglandin E in seminal fluid (Robertson et al., 2002) are likely to be important in skewing the T-cell response towards the Treg cell phenotype.
Such a process would explain epidemiological observations that exposure of the mother to the conceiving partners semen reduces the rate of pre-eclampsia (Marti and Herrmann, 1977; Robillard et al., 1994). Seminal fluid shares many of the same paternal antigens later expressed by the conceptus; however, the nature of Treg cells would not necessitate that the full repertoire of conceptus antigens should be present at the site of initial Treg cell priming. When applied in the context of pregnancy, the notion of bystander tolerance conferred by Treg cells might explain why repeated exposure of the female reproductive tract to a limited panel of paternal antigens in seminal fluid, or alternatively prolonged exposure to a small number of trophoblast antigens early in pregnancy, may be sufficient to prime the maternal immune system to tolerate a wider repertoire of additional antigens expressed later in gestational tissues.
Therapeutic potential of regulatory T-cells in reproductive medicine
The pivotal role of Treg cells in pregnancy and the clear association between their deficiency and pregnancy pathologies raise the enticing prospect of exploiting Treg cells in new therapeutic options for pregnancy complications where insufficient immune tolerance is implicated. Although to date there are no reports of efforts to manipulate Treg cell numbers to assist pregnancy, therapeutic interventions for allograft tolerance and auto-immune disease treatment are under development (Cobbold et al., 2003; Allan et al., 2008) and these might reasonably be extrapolated as candidate treatments for pregnancy disorders. In particular, the potential exploitation of Treg cells to promote tolerance for alloantigens in tissue transplantation is driving extensive efforts to increase Treg cell numbers and/or their suppressive capacity by a variety of strategies (Fig. 5). Emerging insights on the mechanistic basis of tumour-induced tolerance via Treg cell induction (Munn and Mellor, 2006) and studies in animals showing that in vivo depletion of Treg cells can drive regression of syngeneic tumours (Shimizu et al., 1999) have prompted development of therapies to deplete Treg cells for treatment of cancers where tumour-mediated elevation of Treg cells is evident (Gallimore and Godkin, 2008). The current state of investigation targeting Treg cells in human diseases is summarized below, highlighting features that might be relevant to applications in the reproductive domain.
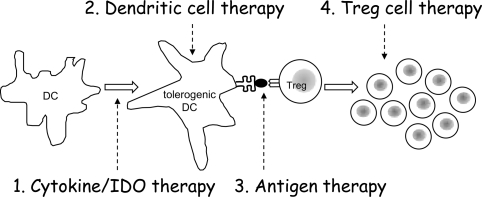
Figure 5.
Several strategies for increasing Treg cell activity are in development as novel tissue transplantation therapies or treatments for autoimmune disease, and analogous approaches might have applications in reproductive medicine.
These include (1) administration of IDO-inducing agents or cytokines (such as G-CSF) to expand the pool of tolerogenic DCs; (2) delivery of tolerogenic DCs after pulsing with specific antigen; (3) delivery of antigen in a form such as apoptotic cellular material known to stimulate Treg proliferation and (4) delivery of antigen-specific Treg cells after recovery and ex vivo expansion. DC, dendritic cell.
Harvesting and expanding Treg cell populations in vitro
A range of strategies is under investigation to expand Treg cell numbers, in both an antigen-specific and a non-specific manner. Current approaches typically involve cell-based therapies using either adoptive transfer of ex vivo manipulated Treg cells or induction of FOXP3 expression in naive lymphocytes (Verbsky, 2007). However, several hurdles need to be overcome before either of these strategies can be implemented. The attractive approach of increasing Treg cell numbers by recovery and expansion of an individual patient's Treg cells ex vivo (Masteller et al., 2006) is currently limited by the ability to isolate Treg cells from human samples with high purity. The intracellular nature of FOXP3 means it cannot be utilized for cell purification.
Typical isolation protocols use magnetic beads that purify cells based on the expression of surface markers such as CD4, using positive selection for these cell types or elimination of non-CD4+ cells, followed by multiple rounds of selection for CD25+ cells (Hoffmann et al., 2006; Bresatz et al., 2007). However, this approach fails to yield sufficient purity as CD25 also isolates activated T-cells and fails to discriminate between the CD25high cell population, which includes the majority of human Treg cells, and CD25intermediate cells that largely comprise non-regulatory T-cells. Consequently, when the isolated cells are expanded in vitro, the anergic nature of Treg cells means that any contaminating T-cell subsets expand faster and result in a low percentage of the desired suppressive populations (Baecher-Allan et al., 2005). Adoptive transfer of preparations that contain activated/reactive T-cells could, in opposition to the desired effect, adversely affect tolerance.
Another protocol for isolating Treg cells uses multiple surface markers in combination including CD4, CD25, CTLA4 and CD127, followed by fluorescent-activated cell sorting (Hoffmann et al., 2004; Hartigan-O'Connor et al., 2007). Although this technique can produce a highly purified population, the quantity of cells generated is substantially lower than with magnetic bead protocols, and as a result, significant levels of in vitro expansion are required. This problem has largely been overcome in the past few years. Although traditional protocols expand cell numbers ∼40-fold (Bresatz et al., 2007; Chai et al., 2008), some current protocols can routinely yield ∼13 000-fold increase in Treg cell numbers in a period of 3–4 weeks (Hoffmann et al., 2004). Importantly, these expanded Treg cells maintain their suppressive capacity and in some cases show increased suppressive ability (Chai et al., 2008). A better understanding of the requirement of signalling and co-stimulatory factors in Treg cell proliferation and homeostasis will allow more efficient expansion protocols. For example, blockade of phospholipase D signalling using primary alcohols in ex vivo cultures selectively expands Treg cells over effector T-cells (Singh et al., 2006). The major limiting factor in implementing in vitro cell-based therapies is now the lengthy time and cost of such labour intensive procedures. Additionally, standardized procedures and good manufacturing practice in cell-based therapies are yet to be implemented.
Promoting development of Treg cells in vivo and in vitro
Alternative strategies for augmenting Treg cell activity involve the manipulation of naive CD4+ T-cells to induce FOXP3 expression. There is a growing body of evidence that FOXP3+ cells can be generated from naive T-cells in the periphery through stimulation with low levels of antigen (Apostolou and von Boehmer, 2004) or by delivering antigens in association with DCs (Cobbold et al., 2003; Kretschmer et al., 2005). The efficacy of this approach both in vitro and in vivo is improved when DCs are conditioned into a tolerogenic phenotype by addition of exogenous cytokines or by transfection with immunosuppressive cytokine genes (Rutella and Lemoli, 2004). The challenge of this approach is the necessity for pulsing DCs with the appropriate antigen, to ensure that sufficient T-cells expressing cognate TCRs respond.
Ectopic lenti-viral-induced expression of FOXP3 is another proposed technique for conversion of naive T-cells into suppressive cells. However, whether FOXP3 transformed cells represent a true regulatory phenotype is still in question (Gavin et al., 2006). Furthermore, the amount of in vitro manipulation involved in this approach outweighs that required for purification and expansion of pre-existing Treg cells.
The ability to generate new Treg cells in vivo without the need for prior isolation and in vitro manipulation would circumvent many of the problems and cost involved in the aforementioned approaches. With the incomplete knowledge of the factors driving the generation and maintenance of Treg cells in vivo, the ability to expand these cells within an individual is yet to be exploited to its full potential. Currently, few strategies exist to artificially augment Treg cell numbers without the need for in vitro manipulation. One current approach involves the concurrent injection of IL-2 and the anti-IL-2 antibody JES6-1. When administered, these form a complex that has high affinity for IL-2Rα (CD25), which is constitutively expressed at high levels on Treg cells, leading to an ∼4-fold selective expansion of CD4+CD25+ cells (Boyman et al., 2006).
Another alternative for driving endogenous regulatory T-cell production might be administration of granulocyte colony-stimulating factor (G-CSF). This cytokine, which is conventionally utilized in treatment of severe chronic neutropenia or in bone marrow transplant patients, has been shown to be efficacious in Treg cell generation (Rutella et al., 2002; Rutella and Lemoli, 2004). G-CSF treatment is reported to induce development of tolerogenic DCs, which in turn elicit potently suppressive regulatory T-cells reminiscent of Tr1 cells (Rutella et al., 2002). However, an important pitfall of this approach is the possibility of phenotype reversion in G-CSF-induced DCs, leading to the opposite effect of inducing immunity.
Exploiting the IDO pathway provides additional novel opportunities for manipulating Treg cells in vivo. IDO can now be considered a physiological Treg cell activator, and therapeutic treatments to induce IDO expression or augment IDO enzymatic activity in DCs seem feasible options for inducing Treg cells, analogous to mechanisms utilized by tumour cells (Curti et al., 2007). Over-expressing IDO utilizing adenovirus or transposon-mediated gene therapy in lung tissue has been shown to have potent effects on persistence of allogeneic lung transplants, associated with suppression of allo-reactive T-cells (Swanson et al., 2004; Liu et al., 2006a). An FDA-approved treatment for the rheumatoid arthritis utilizes CTLA-4-Ig to promote tolerance by targeting the IDO pathway. In several animal models, CTLA-4-Ig treatment has been shown to increase allogeneic graft survival and reduce clonal T-cell expansion linked with elevated IDO expression in DCs (Grohmann et al., 2002; Mellor et al., 2003). Importantly, suppression was abrogated by the IDO inhibiting agent 1-methyl tryptophan, implicating IDO as a critical factor in the treatment effect.
Prospects for utilizing Treg cells in treatments for infertility and subfertility
The efforts to devise Treg therapies for tissue transplantation show exciting promise and the lessons learnt will be valuable for developing analogous therapies for reproductive disorders. It seems reasonable that boosting the number and/or activity of Treg cells reactive with appropriate conceptus antigens should confer stronger immune tolerance in women prone to unexplained infertility, miscarriage or pre-eclampsia due to intrinsic tolerance deficiency. Animal studies that support this concept are beginning to appear in the literature, with recent reports of elevated Treg cells protecting against fetal loss in the abortion-prone CBA/J x DBA/2J mouse model (Zenclussen et al., 2005), and exogenous TGFβ delivered at conception boosting vaginal Treg cell numbers and also reducing fetal loss in the CBA/J x DBA/2J model (Clark et al., 2008). Interestingly, the peri-conceptual timing of these successful interventions suggests that in women, Treg cell boosting might be efficacious if achieved even prior to the index pregnancy.
The first reported clinical study targeting the regulatory T-cell nexus has utilized G-CSF treatments in women experiencing recurrent miscarriage. Administration of Filgrastim (G-CSF) for the first 30 days of pregnancy showed promise in a small pilot study in reducing the incidence of subsequent miscarriage (Scarparelli and Sbracia, 2004). As expected, G-CSF treatment appears to be associated with an increase in circulating CD4+CD25+ Treg cells and DCs (Scarparelli and Sbracia, 2007). Despite these encouraging initial results and the established safety of this drug (Dale et al., 2003), it is somewhat concerning that pre-clinical animal studies to investigate the effects of G-CSF therapy on fetal and post-natal parameters have not been reported, particularly in view of mounting evidence for cytokine effects on fetal programming (Sjoblom et al., 2005).
Another strategy worthy of clinical evaluation would involve recovery and in vitro priming of DCs with male partner MHC antigen, in an approach analogous to treatments under development for allogeneic graft rejection (Rutella and Lemoli, 2004), utilizing cytokines to condition DCs into a tolerogenic phenotype prior to transfer (Sato et al., 2003). A simpler possibility might involve transferring male partner-derived MHC+ apoptotic cells, which would then be processed by recipient DCs in vivo (Morelli and Thomson, 2003). The validity of these strategies is supported by an experiment in CBA/J x DBA/2J mice where paternal alloantigen-pulsed DCs elicited a short-lived reduction in abortion rates, although whether the effect was mediated through increased Treg cells was not examined (Blois et al., 2004b).
Investigation of IDO-inducing reagents such as CTLA4-Ig that are currently in use as immunosuppressants for other clinical applicants also seems worthwhile in the reproductive setting. The benefit of these agents is their generic, antigen-independent nature; however, there may be pitfalls associated with the lack of specific targeting of tissue-specific Treg cell populations.
However, it is important to caution that any attempts in women to alter Treg cell number or function during or prior to pregnancy must be based in a sound biological rationale, informed by knowledge of the antigens against which pregnancy-associated Tregs are normally targeted, and taking into account the natural ontogeny, timing of activation and regulators governing these cells. Compelling pre-clinical animal data will be essential to provide proof-of-concept and to justify any clinical attempt to boost Treg cells in women. Although there are differences in the detail of the precise mechanisms mediating maternal immune tolerance in rodents and humans, the data available to date support the reasonable likelihood of a comparable role for Treg cells in both species. As well as the abortion-prone mouse model, genetic mouse models that allow fine manipulation of Treg cell numbers, such as the DEREG mouse where low-dose diphtheria toxin can be utilized to selectively and acutely deplete Treg cells (Lahl et al., 2007), will be valuable tools for more fully defining Treg cell functions in pregnancy.
The long controversy surrounding the use of paternal allo-immunization as a treatment for miscarriage patients resulted from incomplete understanding of the relevant biological mechanisms and failure to engage the correct path to clinical translation (Porter et al., 2006). It is essential that new and promising reproductive immunology therapies do not suffer the same fate. In view of our emerging knowledge on the mechanisms controlling induction of tolerance versus immunity, it seems likely that administration of paternal antigen without appropriate tolerance-inducing agents might in some women aggravate Th1 or Th17-mediated immunity, rather than induce Treg cells.
Comprehensive clinical trials will be essential to ensure that no adverse effects result from manipulating Treg cells. The risk–benefit analysis of experimental treatments in otherwise healthy, reproductive aged women is ethically challenging compared with patients suffering terminal illness or a debilitating autoimmune condition. Relevant concerns might include inadvertently exacerbating an inappropriate immune response, whereas an overly robust maternal Treg response could cause diminished ability to reject chromosomally abnormal embryos, and/or predispose to aggressive placental invasion of maternal tissues (placenta accreta). Increasing susceptibility to choriocarcinoma, gynaecological or unrelated tumours through artificially expanding Treg cell populations is a further serious risk, needing careful and thorough evaluation. Finally, since reproductive pathologies result from multiple aetiologies, robust and practical diagnostics for defining individual women or couples at risk of Treg cell-deficient pregnancy will need to be developed.
Conclusions and future perspectives
Collectively, the emerging literature provides a compelling case that Treg cells have an important role in successful pregnancy. That several studies show a peak of Treg cells in the first trimester of pregnancy implies a particularly important role for Treg cells in implantation and the initial wave of placental invasion of the maternal tissues during early pregnancy. Insufficient Treg cell numbers and/or function appear to be associated with several complications of pregnancy; however, the underlying mechanisms governing Treg cell numbers and function in the implantation site, and the reasons for their deficiency in some reproductive pathologies, are not clear.
To understand the function and dynamics of Treg cells during pregnancy, more basic research is needed. In particular, the origin and nature of the eliciting antigens and the roles of cytokines, IDO, TLR ligands and other regulatory factors driving activation and expansion of conceptus antigen-reactive Treg cell populations in early pregnancy, as well as the chemokine signals regulating their recruitment and retention in the uterus, have to be defined. The utility of many existing studies is limited by their use of CD25 as a Treg cell marker, underscoring the need for consistent use of Foxp3 and other specific surface markers to definitively identify Treg cells. Defining the nature and significance of Treg cell interactions with other uterine leukocyte populations, notably DCs, NK cells and mast cells, should also be a research priority.
There is no doubt that Treg cells offer an attractive target for treatment of disease and hold great promise for reproductive applications; however, ultimately the science of manipulation of Treg cell numbers is still in its infancy. As our understanding of the origins and factors controlling Treg cells expands, their utility as therapeutic agents will begin to be actualized through clinical trial evaluation. Any treatment will need to meet the requirements of safety, efficacy and ease of administration that govern the development of all pharmaceutical agents. Once this is achieved, and with their distinct importance in reproduction, it is highly likely that they will become a powerful new tool for the treatment of fertility pathologies stemming from disturbances in immune tolerance.
Funding
The authors’ research is supported by Fellowship and Program Grant funding from the National Health and Medical Research Council of Australia (S.A.R.).
References
- Abbas AK, Lohr J, Knoechel B. Balancing autoaggressive and protective T cell responses. J Autoimmun. 2007;28:59–61. doi: 10.1016/j.jaut.2007.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akbar AN, Taams LS, Salmon M, Vukmanovic-Stejic M. The peripheral generation of CD4+CD25+ regulatory T cells. Immunology. 2003;109:319–325. doi: 10.1046/j.1365-2567.2003.01678.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akbar AN, Vukmanovic-Stejic M, Taams LS, Macallan DC. The dynamic co-evolution of memory and regulatory CD4+ T cells in the periphery. Nat Rev Immunol. 2007;7:231–237. doi: 10.1038/nri2037. [DOI] [PubMed] [Google Scholar]
- Alard P, Thompson C, Agersborg SS, Thatte J, Setiady Y, Samy E, Tung KS. Endogenous oocyte antigens are required for rapid induction and progression of autoimmune ovarian disease following day-3 thymectomy. J Immunol. 2001;166:4363–4369. doi: 10.4049/jimmunol.166.7.4363. [DOI] [PubMed] [Google Scholar]
- Allan SE, Crome SQ, Crellin NK, Passerini L, Steiner TS, Bacchetta R, Roncarolo MG, Levings MK. Activation-induced FOXP3 in human T effector cells does not suppress proliferation or cytokine production. Int Immunol. 2007;19:345–354. doi: 10.1093/intimm/dxm014. [DOI] [PubMed] [Google Scholar]
- Allan SE, Broady R, Gregori S, Himmel ME, Locke N, Roncarolo MG, Bacchetta R, Levings MK. CD4+ T-regulatory cells: toward therapy for human diseases. Immunol Rev. 2008;223:391–421. doi: 10.1111/j.1600-065X.2008.00634.x. [DOI] [PubMed] [Google Scholar]
- Aluvihare VR, Kallikourdis M, Betz AG. Regulatory T cells mediate maternal tolerance to the fetus. Nat Immunol. 2004;5:266–271. doi: 10.1038/ni1037. [DOI] [PubMed] [Google Scholar]
- Annunziato F, Cosmi L, Liotta F, Lazzeri E, Manetti R, Vanini V, Romagnani P, Maggi E, Romagnani S. Phenotype, localization, and mechanism of suppression of CD4(+)CD25(+) human thymocytes. J Exp Med. 2002;196:379–387. doi: 10.1084/jem.20020110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apostolou I, von Boehmer H. In vivo instruction of suppressor commitment in naive T cells. J Exp Med. 2004;199:1401–1408. doi: 10.1084/jem.20040249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arruvito L, Sanz M, Banham AH, Fainboim L. Expansion of CD4+CD25+ and FOXP3+ regulatory T cells during the follicular phase of the menstrual cycle: implications for human reproduction. J Immunol. 2007;178:2572–2578. doi: 10.4049/jimmunol.178.4.2572. [DOI] [PubMed] [Google Scholar]
- Baecher-Allan C, Wolf E, Hafler DA. Functional analysis of highly defined, FACS-isolated populations of human regulatory CD4+ CD25+ T cells. Clin Immunol. 2005;115:10–18. doi: 10.1016/j.clim.2005.02.018. [DOI] [PubMed] [Google Scholar]
- Baratelli F, Krysan K, Heuze-Vourc'h N, Zhu L, Escuadro B, Sharma S, Reckamp K, Dohadwala M, Dubinett SM. PGE2 confers survivin-dependent apoptosis resistance in human monocyte-derived dendritic cells. J Leukoc Biol. 2005;78:555–564. doi: 10.1189/jlb.1004569. [DOI] [PubMed] [Google Scholar]
- Bertrams J, Kuwert E, Lohmeyer HH. The specificity of leukocyte antibodies in histocompatibility testing of serum from prima- and multiparas. Bibl Haematol. 1971;37:98–106. [PubMed] [Google Scholar]
- Bettelli E, Carrier Y, Gao W, Korn T, Strom TB, Oukka M, Weiner HL, Kuchroo VK. Reciprocal developmental pathways for the generation of pathogenic effector TH17 and regulatory T cells. Nature. 2006;441:235–238. doi: 10.1038/nature04753. [DOI] [PubMed] [Google Scholar]
- Billington WD. The immunological problem of pregnancy: 50 years with the hope of progress. A tribute to Peter Medawar. J Reprod Immunol. 2003;60:1–11. doi: 10.1016/s0165-0378(03)00083-4. [DOI] [PubMed] [Google Scholar]
- Blois SM, Joachim R, Kandil J, Margni R, Tometten M, Klapp BF, Arck PC. Depletion of CD8+ cells abolishes the pregnancy protective effect of progesterone substitution with dydrogesterone in mice by altering the Th1/Th2 cytokine profile. J Immunol. 2004a;172:5893–5899. doi: 10.4049/jimmunol.172.10.5893. [DOI] [PubMed] [Google Scholar]
- Blois S, Alba Soto CD, Olmos S, Chuluyan E, Gentile T, Arck PC, Margni RA. Therapy with dendritic cells influences the spontaneous resorption rate in the CBA/J x DBA/2J mouse model. Am J Reprod Immunol. 2004b;51:40–48. doi: 10.1046/j.8755-8920.2003.00120.x. [DOI] [PubMed] [Google Scholar]
- Blois SM, Alba Soto CD, Tometten M, Klapp BF, Margni RA, Arck PC. Lineage, maturity, and phenotype of uterine murine dendritic cells throughout gestation indicate a protective role in maintaining pregnancy. Biol Reprod. 2004c;70:1018–1023. doi: 10.1095/biolreprod.103.022640. [DOI] [PubMed] [Google Scholar]
- Blois SM, Ilarregui JM, Tometten M, Garcia M, Orsal AS, Cordo-Russo R, Toscano MA, Bianco GA, Kobelt P, Handjiski B, et al. A pivotal role for galectin-1 in fetomaternal tolerance. Nat Med. 2007a;13:1450–1457. doi: 10.1038/nm1680. [DOI] [PubMed] [Google Scholar]
- Blois SM, Kammerer U, Alba Soto C, Tometten MC, Shaikly V, Barrientos G, Jurd R, Rukavina D, Thomson AW, Klapp BF, et al. Dendritic cells: key to fetal tolerance? Biol Reprod. 2007b;77:590–598. doi: 10.1095/biolreprod.107.060632. [DOI] [PubMed] [Google Scholar]
- Boyman O, Kovar M, Rubinstein MP, Surh CD, Sprent J. Selective stimulation of T cell subsets with antibody–cytokine immune complexes. Science. 2006;311:1924–1927. doi: 10.1126/science.1122927. [DOI] [PubMed] [Google Scholar]
- Bresatz S, Sadlon T, Millard D, Zola H, Barry SC. Isolation, propagation and characterization of cord blood derived CD4+ CD25+ regulatory T cells. J Immunol Methods. 2007;327:53–62. doi: 10.1016/j.jim.2007.06.006. [DOI] [PubMed] [Google Scholar]
- Brunkow ME, Jeffery EW, Hjerrild KA, Paeper B, Clark LB, Yasayko S-A, Wilkinson JE, Galas D, Ziegler SF, Ramsdell F. Disruption of a new forkhead/winged-helix protein, scurfin, results in the fatal lymphoproliferative disorder of the scurfy mouse. Nat Genet. 2001;27:68–73. doi: 10.1038/83784. [DOI] [PubMed] [Google Scholar]
- Cederbom L, Hall H, Ivars F. CD4+CD25+ regulatory T cells down-regulate co-stimulatory molecules on antigen-presenting cells. Eur J Immunol. 2000;30:1538–1543. doi: 10.1002/1521-4141(200006)30:6<1538::AID-IMMU1538>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- Chai JG, Coe D, Chen D, Simpson E, Dyson J, Scott D. In vitro expansion improves in vivo regulation by CD4+CD25+ regulatory T cells. J Immunol. 2008;180:858–869. doi: 10.4049/jimmunol.180.2.858. [DOI] [PubMed] [Google Scholar]
- Chao KH, Wu MY, Yang JH, Chen SU, Yang YS, Ho HN. Expression of the interleukin-2 receptor alpha (CD25) is selectively decreased on decidual CD4+ and CD8+ T lymphocytes in normal pregnancies. Mol Hum Reprod. 2002;8:667–673. doi: 10.1093/molehr/8.7.667. [DOI] [PubMed] [Google Scholar]
- Chaouat G. The Th1/Th2 paradigm: still important in pregnancy? Semin Immunopathol. 2007;29:95–113. doi: 10.1007/s00281-007-0069-0. [DOI] [PubMed] [Google Scholar]
- Chen W, Jin W, Hardegen N, Lei KJ, Li L, Marinos N, McGrady G, Wahl SM. Conversion of peripheral CD4+CD25− naive T cells to CD4+CD25+ regulatory T cells by TGF-beta induction of transcription factor Foxp3. J Exp Med. 2003;198:1875–1886. doi: 10.1084/jem.20030152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W, Liang X, Peterson AJ, Munn DH, Blazar BR. The indoleamine 2,3-dioxygenase pathway is essential for human plasmacytoid dendritic cell-induced adaptive T regulatory cell generation. J Immunol. 2008;181:5396–5404. doi: 10.4049/jimmunol.181.8.5396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi BK, Bae JS, Choi EM, Kang WJ, Sakaguchi S, Vinay DS, Kwon BS. 4-1BB-dependent inhibition of immunosuppression by activated CD4+CD25+ T cells. J Leukoc Biol. 2004;75:785–791. doi: 10.1189/jlb.1003491. [DOI] [PubMed] [Google Scholar]
- Clark DA, Chaouat G, Mogil R, Wegmann TG. Prevention of spontaneous abortion in DBA/2-mated CBA/J mice by GM-CSF involves CD8+ T cell-dependent suppression of natural effector cell cytotoxicity against trophoblast target cells. Cell Immunol. 1994;154:143–152. doi: 10.1006/cimm.1994.1064. [DOI] [PubMed] [Google Scholar]
- Clark DA, Fernandes J, Banwatt D. Prevention of spontaneous abortion in the CBA x DBA/2 mouse model by intravaginal TGF-beta and local recruitment of CD4+8+ FOXP3+ cells. Am J Reprod Immunol. 2008;59:525–534. doi: 10.1111/j.1600-0897.2008.00582.x. [DOI] [PubMed] [Google Scholar]
- Cobbold SP, Nolan KF, Graca L, Castejon R, Moine AL, Frewin M, Humm S, Adams E, Thompson S, Zelenika D, et al. Regulatory T cells and dendritic cells in transplantation tolerance: molecular markers and mechanisms. Immunol Rev. 2003;196:109–124. doi: 10.1046/j.1600-065x.2003.00078.x. [DOI] [PubMed] [Google Scholar]
- Coombes JL, Robinson NJ, Maloy KJ, Uhlig HH, Powrie F. Regulatory T cells and intestinal homeostasis. Immunol Rev. 2005;204:184–194. doi: 10.1111/j.0105-2896.2005.00250.x. [DOI] [PubMed] [Google Scholar]
- Cozzo C, Lerman MA, Boesteanu A, Larkin J, 3rd, Jordan MS, Caton AJ. Selection of CD4+CD25+ regulatory T cells by self-peptides. Curr Top Microbiol Immunol. 2005;293:3–23. [PubMed] [Google Scholar]
- Crellin NK, Garcia RV, Hadisfar O, Allan SE, Steiner TS, Levings MK. Human CD4+ T cells express TLR5 and its ligand flagellin enhances the suppressive capacity and expression of FOXP3 in CD4+CD25+ T regulatory cells. J Immunol. 2005;175:8051–8059. doi: 10.4049/jimmunol.175.12.8051. [DOI] [PubMed] [Google Scholar]
- Curti A, Pandolfi S, Valzasina B, Aluigi M, Isidori A, Ferri E, Salvestrini V, Bonanno G, Rutella S, Durelli I, et al. Modulation of tryptophan catabolism by human leukemic cells results in the conversion of CD25− into CD25+ T regulatory cells. Blood. 2007;109:2871–2877. doi: 10.1182/blood-2006-07-036863. [DOI] [PubMed] [Google Scholar]
- Dal Secco V, Riccioli A, Padula F, Ziparo E, Filippini A. Mouse Sertoli cells display phenotypical and functional traits of antigen-presenting cells in response to interferon gamma. Biol Reprod. 2008;78:234–242. doi: 10.1095/biolreprod.107.063578. [DOI] [PubMed] [Google Scholar]
- Dale DC, Cottle TE, Fier CJ, Bolyard AA, Bonilla MA, Boxer LA, Cham B, Freedman MH, Kannourakis G, Kinsey SE, et al. Severe chronic neutropenia: treatment and follow-up of patients in the Severe Chronic Neutropenia International Registry. Am J Hematol. 2003;72:82–93. doi: 10.1002/ajh.10255. [DOI] [PubMed] [Google Scholar]
- Damoiseaux J. Regulatory T cells: back to the future. Neth J Med. 2006;64:4–9. [PubMed] [Google Scholar]
- Darmochwal-Kolarz D, Saito S, Rolinski J, Tabarkiewicz J, Kolarz B, Leszczynska-Gorzelak B, Oleszczuk J. Activated T lymphocytes in pre-eclampsia. Am J Reprod Immunol. 2007;58:39–45. doi: 10.1111/j.1600-0897.2007.00489.x. [DOI] [PubMed] [Google Scholar]
- Darrasse-Jeze G, Klatzmann D, Charlotte F, Salomon BL, Cohen JL. CD4+CD25+ regulatory/suppressor T cells prevent allogeneic fetus rejection in mice. Immunol Lett. 2006;102:106–109. doi: 10.1016/j.imlet.2005.07.002. [DOI] [PubMed] [Google Scholar]
- Davies JD, Leong LY, Mellor A, Cobbold SP, Waldmann H. T cell suppression in transplantation tolerance through linked recognition. J Immunol. 1996;156:3602–3607. [PubMed] [Google Scholar]
- de la Rosa M, Rutz S, Dorninger H, Scheffold A. Interleukin-2 is essential for CD4+CD25+ regulatory T cell function. Eur J Immunol. 2004;34:2480–2488. doi: 10.1002/eji.200425274. [DOI] [PubMed] [Google Scholar]
- Fisson S, Darrasse-Jeze G, Litvinova E, Septier F, Klatzmann D, Liblau R, Salomon BL. Continuous activation of autoreactive CD4+ CD25+ regulatory T cells in the steady state. J Exp Med. 2003;198:737–746. doi: 10.1084/jem.20030686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontenot JD, Gavin MA, Rudensky AY. Foxp3 programs the development and function of CD4+CD25+ regulatory T cells. Nat Immunol. 2003;4:330–336. doi: 10.1038/ni904. [DOI] [PubMed] [Google Scholar]
- Fontenot JD, Dooley JL, Farr AG, Rudensky AY. Developmental regulation of Foxp3 expression during ontogeny. J Exp Med. 2005a;202:901–906. doi: 10.1084/jem.20050784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontenot JD, Rasmussen JP, Williams LM, Dooley JL, Farr AG, Rudensky AY. Regulatory T cell lineage specification by the forkhead transcription factor foxp3. Immunity. 2005b;22:329–341. doi: 10.1016/j.immuni.2005.01.016. [DOI] [PubMed] [Google Scholar]
- Fukaura H, Kent SC, Pietrusewicz MJ, Khoury SJ, Weiner HL, Hafler DA. Induction of circulating myelin basic protein and proteolipid protein-specific transforming growth factor-beta 1 secreting Th3 T cells by oral administration of myelin in multiple sclerosis patients. J Clin Invest. 1996;98:70–77. doi: 10.1172/JCI118779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallimore A, Godkin A. Regulatory T cells and tumour immunity—observations in mice and men. Immunology. 2008;123:157–163. doi: 10.1111/j.1365-2567.2007.02748.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garza KM, Agersborg SS, Baker E, Tung KS. Persistence of physiological self antigen is required for the regulation of self tolerance. J Immunol. 2000;164:3982–3989. doi: 10.4049/jimmunol.164.8.3982. [DOI] [PubMed] [Google Scholar]
- Gavin MA, Clarke SR, Negrou E, Gallegos A, Rudensky A. Homeostasis and anergy of CD4(+)CD25(+) suppressor T cells in vivo. Nat Immunol. 2002;3:33–41. doi: 10.1038/ni743. [DOI] [PubMed] [Google Scholar]
- Gavin MA, Torgerson TR, Houston E, deRoos P, Ho WY, Stray-Pedersen A, Ocheltree EL, Greenberg PD, Ochs HD, Rudensky AY. Single-cell analysis of normal and FOXP3-mutant human T cells: FOXP3 expression without regulatory T cell development. Proc Natl Acad Sci. 2006;103:6659–6664. doi: 10.1073/pnas.0509484103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gershon RK, Cohen P, Hencin R, Liebhaber SA. Suppressor T Cells. J Immunol. 1972;108:586–590. [PubMed] [Google Scholar]
- Ghiringhelli F, Menard C, Terme M, Flament C, Taieb J, Chaput N, Puig PE, Novault S, Escudier B, Vivier E, et al. CD4+CD25+ regulatory T cells inhibit natural killer cell functions in a transforming growth factor-beta-dependent manner. J Exp Med. 2005a;202:1075–1085. doi: 10.1084/jem.20051511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghiringhelli F, Puig PE, Roux S, Parcellier A, Schmitt E, Solary E, Kroemer G, Martin F, Chauffert B, Zitvogel L. Tumor cells convert immature myeloid dendritic cells into TGF-beta-secreting cells inducing CD4+CD25+ regulatory T cell proliferation. J Exp Med. 2005b;202:919–929. doi: 10.1084/jem.20050463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorelik L, Flavell RA. Abrogation of TGFbeta signaling in T cells leads to spontaneous T cell differentiation and autoimmune disease. Immunity. 2000;12:171–181. doi: 10.1016/s1074-7613(00)80170-3. [DOI] [PubMed] [Google Scholar]
- Gorelik L, Flavell RA. Transforming growth factor-beta in T-cell biology. Nat Rev Immunol. 2002;2:46–53. doi: 10.1038/nri704. [DOI] [PubMed] [Google Scholar]
- Green DR, Webb DR. Saying the ‘S’ word in public. Immunol Today. 1993;14:523–525. doi: 10.1016/0167-5699(93)90180-S. [DOI] [PubMed] [Google Scholar]
- Grohmann U, Orabona C, Fallarino F, Vacca C, Calcinaro F, Falorni A, Candeloro P, Belladonna ML, Bianchi R, Fioretti MC, et al. CTLA-4-Ig regulates tryptophan catabolism in vivo. Nat Immunol. 2002;3:1097–1101. doi: 10.1038/ni846. [DOI] [PubMed] [Google Scholar]
- Groux H, O'Garra A, Bigler M, Rouleau M, Antonenko S, de Vries JE, Roncarolo MG. A CD4+ T-cell subset inhibits antigen-specific T-cell responses and prevents colitis. Nature. 1997;389:737–742. doi: 10.1038/39614. [DOI] [PubMed] [Google Scholar]
- Habicht A, Dada S, Jurewicz M, Fife BT, Yagita H, Azuma M, Sayegh MH, Guleria I. A link between PDL1 and T regulatory cells in fetomaternal tolerance. J Immunol. 2007;179:5211–5219. doi: 10.4049/jimmunol.179.8.5211. [DOI] [PubMed] [Google Scholar]
- Harnaha J, Machen J, Wright M, Lakomy R, Styche A, Trucco M, Makaroun S, Giannoukakis N. Interleukin-7 is a survival factor for CD4+ CD25+ T-cells and is expressed by diabetes-suppressive dendritic cells. Diabetes. 2006;55:158–170. [PubMed] [Google Scholar]
- Hartigan-O'Connor DJ, Poon C, Sinclair E, McCune JM. Human CD4+ regulatory T cells express lower levels of the IL-7 receptor alpha chain (CD127), allowing consistent identification and sorting of live cells. J Immunol Methods. 2007;319:41–52. doi: 10.1016/j.jim.2006.10.008. [DOI] [PubMed] [Google Scholar]
- Heikkinen J, Mottonen M, Alanen A, Lassila O. Phenotypic characterization of regulatory T cells in the human decidua. Clin Exp Immunol. 2004;136:373–378. doi: 10.1111/j.1365-2249.2004.02441.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heyborne K, Fu YX, Nelson A, Farr A, O'Brien R, Born W. Recognition of trophoblasts by gamma delta T cells. J Immunol. 1994;153:2918–2926. [PubMed] [Google Scholar]
- Ho HN, Chao KH, Chen CK, Yang YS, Huang SC. Activation status of T and NK cells in the endometrium throughout menstrual cycle and normal and abnormal early pregnancy. Hum Immunol. 1996;49:130–136. doi: 10.1016/0198-8859(96)00120-6. [DOI] [PubMed] [Google Scholar]
- Hoffmann P, Eder R, Kunz-Schughart LA, Andreesen R, Edinger M. Large-scale in vitro expansion of polyclonal human CD4+CD25 high regulatory T cells. Transplantion. 2004;104:895–903. doi: 10.1182/blood-2004-01-0086. [DOI] [PubMed] [Google Scholar]
- Hoffmann P, Boeld TJ, Eder R, Albrecht J, Doser K, Piseshka B, Dada A, Niemand C, Assenmacher M, Orso E, et al. Isolation of CD4+CD25+ regulatory T cells for clinical trials. Biol Blood Marrow Transplant. 2006;12:267–274. doi: 10.1016/j.bbmt.2006.01.005. [DOI] [PubMed] [Google Scholar]
- Huang C-T, Workman CJ, Flies D, Pan X, Marson AL, Zhou G, Hipkiss EL, Ravi S, Kowalski J, Levitsky HI. Role of LAG-3 in regulatory T cells. Immunity. 2004;21:503–513. doi: 10.1016/j.immuni.2004.08.010. [DOI] [PubMed] [Google Scholar]
- Hubert P, Jacobs N, Caberg J-H, Boniver J, Delvenne P. The cross-talk between dendritic and regulatory T cells: good or evil? J Leukoc Biol. 2007;82:781–794. doi: 10.1189/jlb.1106694. [DOI] [PubMed] [Google Scholar]
- Ichiyama K, Yoshida H, Wakabayashi Y, Chinen T, Saeki K, Nakaya M, Takaesu G, Hori S, Yoshimura A, Kobayashi T. Foxp3 inhibits RORgammat-mediated IL-17A mRNA transcription through direct interaction with RORgammat. J Biol Chem. 2008;283:17003–17008. doi: 10.1074/jbc.M801286200. [DOI] [PubMed] [Google Scholar]
- Ingman WV, Robker RL, Woittiez K, Robertson SA. Null mutation in transforming growth factor beta1 disrupts ovarian function and causes oocyte incompetence and early embryo arrest. Endocrinol. 2006;147:835–845. doi: 10.1210/en.2005-1189. [DOI] [PubMed] [Google Scholar]
- Itoh M, Takahashi T, Sakaguchi N, Kuniyasu Y, Shimizu J, Otsuka F, Sakaguchi S. Thymus and autoimmunity: production of CD25+CD4+ naturally anergic and suppressive T cells as a key function of the thymus in maintaining immunologic self-tolerance. J Immunol. 1999;162:5317–5326. [PubMed] [Google Scholar]
- Jaffe L, Robertson EJ, Bikoff EK. Distinct patterns of expression of MHC class I and beta 2-microglobulin transcripts at early stages of mouse development. J Immunol. 1991;147:2740–2749. [PubMed] [Google Scholar]
- Jasper MJ, Tremellen KP, Robertson SA. Primary unexplained infertility is associated with reduced expression of the T-regulatory cell transcription factor Foxp3 in endometrial tissue. Mol Hum Reprod. 2006;12:301–308. doi: 10.1093/molehr/gal032. [DOI] [PubMed] [Google Scholar]
- Johansson M, Bromfield JJ, Jasper MJ, Robertson SA. Semen activates the female immune response during early pregnancy in mice. Immunology. 2004;112:290–300. doi: 10.1111/j.1365-2567.2004.01876.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonuleit H, Schmitt E. The regulatory T cell family: distinct subsets and their interrelations. J Immunol. 2003;171:6323–6327. doi: 10.4049/jimmunol.171.12.6323. [DOI] [PubMed] [Google Scholar]
- Jonuleit H, Schmitt E, Kakirman H, Stassen M, Knop J, Enk AH. Infectious tolerance: human CD25(+) regulatory T cells convey suppressor activity to conventional CD4(+) T helper cells. J Exp Med. 2002;196:255–260. doi: 10.1084/jem.20020394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan MS, Boesteanu A, Reed AJ, Petrone AL, Holenbeck AE, Lerman MA, Naji A, Caton AJ. Thymic selection of CD4+CD25+ regulatory T cells induced by an agonist self-peptide. Nat Immunol. 2001;2:301–306. doi: 10.1038/86302. [DOI] [PubMed] [Google Scholar]
- Kallikourdis M, Betz AG. Periodic accumulation of regulatory T cells in the uterus: preparation for the implantation of a semi-allogeneic fetus? PLoS ONE. 2007;2:e382. doi: 10.1371/journal.pone.0000382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kallikourdis M, Andersen KG, Welch KA, Betz AG. Alloantigen-enhanced accumulation of CCR5+ ‘effector’ regulatory T cells in the gravid uterus. Proc Natl Acad Sci USA. 2007;104:594–599. doi: 10.1073/pnas.0604268104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanamaru F, Youngnak P, Hashiguchi M, Nishioka T, Takahashi T, Sakaguchi S, Ishikawa I, Azuma M. Costimulation via glucocorticoid-induced TNF receptor in both conventional and CD25+ regulatory CD4+ T cells. J Immunol. 2004;172:7306–7314. doi: 10.4049/jimmunol.172.12.7306. [DOI] [PubMed] [Google Scholar]
- Karim M, Feng G, Wood KJ, Bushell AR. CD25+CD4+ regulatory T cells generated by exposure to a model protein antigen prevent allograft rejection: antigen-specific reactivation in vivo is critical for bystander regulation. Blood. 2005;105:4871–4877. doi: 10.1182/blood-2004-10-3888. [DOI] [PubMed] [Google Scholar]
- King IL, Segal BM. Cutting edge: IL-12 induces CD4+CD25− T cell activation in the presence of T regulatory cells. J Immunol. 2005;175:641–645. doi: 10.4049/jimmunol.175.2.641. [DOI] [PubMed] [Google Scholar]
- Koenen HJ, Fasse E, Joosten I. IL-15 and cognate antigen successfully expand de novo-induced human antigen-specific regulatory CD4+ T cells that require antigen-specific activation for suppression. J Immunol. 2003;171:6431–6441. doi: 10.4049/jimmunol.171.12.6431. [DOI] [PubMed] [Google Scholar]
- Kretschmer K, Apostolou I, Hawiger D, Khazaie K, Nussenzweig MC, von Boehmer H. Inducing and expanding regulatory T cell populations by foreign antigen. Nat Immunol. 2005;6:1219–1227. doi: 10.1038/ni1265. [DOI] [PubMed] [Google Scholar]
- Kubo T, Hatton RD, Oliver J, Liu X, Elson CO, Weaver CT. Regulatory T cell suppression and anergy are differentially regulated by proinflammatory cytokines produced by TLR-activated dendritic cells. J Immunol. 2004;173:7249–7258. doi: 10.4049/jimmunol.173.12.7249. [DOI] [PubMed] [Google Scholar]
- Lahl K, Loddenkemper C, Drouin C, Freyer J, Arnason J, Eberl G, Hamann A, Wagner H, Huehn J, Sparwasser T. Selective depletion of Foxp3+ regulatory T cells induces a scurfy-like disease. J Exp Med. 2007;204:57–63. doi: 10.1084/jem.20061852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laird SM, Tuckerman EM, Cork BA, Linjawi S, Blakemore AI, Li TC. A review of immune cells and molecules in women with recurrent miscarriage. Hum Reprod Update. 2003;9:163–174. doi: 10.1093/humupd/dmg013. [DOI] [PubMed] [Google Scholar]
- LeMaoult J, Krawice-Radanne I, Dausset J, Carosella ED. HLA-G1-expressing antigen-presenting cells induce immunosuppressive CD4+ T cells. Proc Natl Acad Sci USA. 2004;101:7064–7069. doi: 10.1073/pnas.0401922101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim HW, Hillsamer P, Banham AH, Kim CH. Cutting edge: direct suppression of B cells by CD4+ CD25+ regulatory T cells. J Immunol. 2005;175:4180–4183. doi: 10.4049/jimmunol.175.7.4180. [DOI] [PubMed] [Google Scholar]
- Liu H, Liu L, Fletcher BS, Visner GA. Sleeping beauty-based gene therapy with indoleamine 2,3-dioxygenase inhibits lung allograft fibrosis. FASEB J. 2006a;20:2384–2386. doi: 10.1096/fj.06-6228fje. [DOI] [PubMed] [Google Scholar]
- Liu W, Putnam AL, Xu-yu Z, Szot GL, Lee MR, Zhu S, Gottlieb PA, Kapranov P, Gingeras TR, de St Groth BF, et al. CD127 expression inversely correlates with FoxP3 and suppressive function of human CD4+ T reg cells. J Exp Med. 2006b;203:1701–1711. doi: 10.1084/jem.20060772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu L-F, Lind EF, Gondek DC, Bennett KA, Gleeson MW, Pino-Lagos K, Scott ZA, Coyle AJ, Reed JL, Van Snick J, et al. Mast cells are essential intermediaries in regulatory T-cell tolerance. Nature. 2006;442:997–1002. doi: 10.1038/nature05010. [DOI] [PubMed] [Google Scholar]
- Mahmoud F, Omu A, Abul H, El-Rayes S, Haines D. Lymphocyte subpopulations in pregnancy complicated by hypertension. J Obstet Gynaecol. 2003;23:20–26. doi: 10.1080/0144361021000043163. [DOI] [PubMed] [Google Scholar]
- Marti JJ, Herrmann U. Immunogestosis: a new etiologic concept of ‘essential’ EPH gestosis, with special consideration of the primigravid patient; preliminary report of a clinical study. Am J Obstet Gynecol. 1977;128:489–493. doi: 10.1016/0002-9378(77)90030-8. [DOI] [PubMed] [Google Scholar]
- Masteller EL, Tang Q, Bluestone JA. Antigen-specific regulatory T cells—ex vivo expansion and therapeutic potential. Semin Immunol. 2006;18:103–110. doi: 10.1016/j.smim.2006.01.004. [DOI] [PubMed] [Google Scholar]
- McHugh RS, Whitters MJ, Piccirillo CA, Young DA, Shevach EM, Collins M, Byrne MC. CD4+CD25+ immunoregulatory T Cells: gene expression analysis reveals a functional role for the glucocorticoid-induced TNF receptor. Immunity. 2002;16:311–323. doi: 10.1016/s1074-7613(02)00280-7. [DOI] [PubMed] [Google Scholar]
- Medawar PB. Some immunological and endocrinological problems raised by the evolution of viviparity in vertebrates. Symp Soc Exp Biol. 1953;7:320–338. [Google Scholar]
- Mellor AL, Baban B, Chandler P, Marshall B, Jhaver K, Hansen A, Koni PA, Iwashima M, Munn DH. Cutting edge: induced indoleamine 2,3 dioxygenase expression in dendritic cell subsets suppresses T cell clonal expansion. J Immunol. 2003;171:1652–1655. doi: 10.4049/jimmunol.171.4.1652. [DOI] [PubMed] [Google Scholar]
- Misra N, Bayry J, Lacroix-Desmazes S, Kazatchkine MD, Kaveri SV. Cutting edge: human CD4+CD25+ T cells restrain the maturation and antigen-presenting function of dendritic cells. J Immunol. 2004;172:4676–4680. doi: 10.4049/jimmunol.172.8.4676. [DOI] [PubMed] [Google Scholar]
- Miyara M, Sakaguchi S. Natural regulatory T cells: mechanisms of suppression. Trends Mol Med. 2007;13:108–116. doi: 10.1016/j.molmed.2007.01.003. [DOI] [PubMed] [Google Scholar]
- Mjosberg J, Berg G, Ernerudh J, Ekerfelt C. CD4+CD25+ regulatory T cells in human pregnancy: development of a Treg-MLC-ELISPOT suppression assay and indications of paternal specific Tregs. Immunology. 2007;120:456–466. doi: 10.1111/j.1365-2567.2006.02529.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morelli AE, Thomson AW. Dendritic cells under the spell of prostaglandins. Trends Immunol. 2003;24:108–111. doi: 10.1016/s1471-4906(03)00023-1. [DOI] [PubMed] [Google Scholar]
- Munn DH, Mellor AL. The tumor-draining lymph node as an immune-privileged site. Immunol Rev. 2006;213:146–158. doi: 10.1111/j.1600-065X.2006.00444.x. [DOI] [PubMed] [Google Scholar]
- Munn DH, Sharma MD, Lee JR, Jhaver KG, Johnson TS, Keskin DB, Marshall B, Chandler P, Antonia SJ, Burgess R, et al. Potential regulatory function of human dendritic cells expressing indoleamine 2,3-dioxygenase. Science. 2002;297:1867–1870. doi: 10.1126/science.1073514. [DOI] [PubMed] [Google Scholar]
- Munn DH, Sharma MD, Hou D, Baban B, Lee JR, Antonia SJ, Messina JL, Chandler P, Koni PA, Mellor AL. Expression of indoleamine 2,3-dioxygenase by plasmacytoid dendritic cells in tumor-draining lymph nodes. J Clin Invest. 2004;114:280–290. doi: 10.1172/JCI21583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagymanyoki Z, Callahan MJ, Parast MM, Fulop V, Mok SC, Berkowitz RS. Immune cell profiling in normal pregnancy, partial and complete molar pregnancy. Gynecol Oncol. 2007;107:292–297. doi: 10.1016/j.ygyno.2007.06.028. [DOI] [PubMed] [Google Scholar]
- Nasr IW, Wang Y, Gao G, Deng S, Diggs L, Rothstein DM, Tellides G, Lakkis FG, Dai Z. Testicular immune privilege promotes transplantation tolerance by altering the balance between memory and regulatory T cells. J Immunol. 2005;174:6161–6168. doi: 10.4049/jimmunol.174.10.6161. [DOI] [PubMed] [Google Scholar]
- Nishizawa H, Hasegawa K, Suzuki M, Kamoshida S, Kato T, Saito K, Tsutsumi Y, Kurahashi H, Udagawa Y. The etiological role of allogeneic fetal rejection in pre-eclampsia. Am J Reprod Immunol. 2007;58:11–20. doi: 10.1111/j.1600-0897.2007.00484.x. [DOI] [PubMed] [Google Scholar]
- Paeschke S, Chen F, Horn N, Fotopoulou C, Zambon-Bertoja A, Sollwedel A, Zenclussen ML, Casalis PA, Dudenhausen JW, Volk HD, et al. Pre-eclampsia is not associated with changes in the levels of regulatory T cells in peripheral blood. Am J Reprod Immunol. 2005;54:384–389. doi: 10.1111/j.1600-0897.2005.00334.x. [DOI] [PubMed] [Google Scholar]
- Pasare C, Medzhitov R. Toll pathway-dependent blockade of CD4+CD25+ T cell-mediated suppression by dendritic cells. Science. 2003;299:1033–1036. doi: 10.1126/science.1078231. [DOI] [PubMed] [Google Scholar]
- Peng G, Guo Z, Kiniwa Y, Voo KS, Peng W, Fu T, Wang DY, Li Y, Wang HY, Wang RF. Toll-like receptor 8-mediated reversal of CD4+ regulatory T cell function. Science. 2005;309:1380–1384. doi: 10.1126/science.1113401. [DOI] [PubMed] [Google Scholar]
- Piccirillo CA, Shevach EM. Cutting edge: control of CD8+ T cell activation by CD4+CD25+ immunoregulatory cells. J Immunol. 2001;167:1137–1140. doi: 10.4049/jimmunol.167.3.1137. [DOI] [PubMed] [Google Scholar]
- Pillai V, Karandikar NJ. Human regulatory T cells: a unique, stable thymic subset or a reversible peripheral state of differentiation? Immunol Lett. 2007;114:9–15. doi: 10.1016/j.imlet.2007.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polanczyk MJ, Carson BD, Subramanian S, Afentoulis M, Vandenbark AA, Ziegler SF, Offner H. Cutting edge: estrogen drives expansion of the CD4+CD25+ regulatory T cell compartment. J Immunol. 2004;173:2227–2230. doi: 10.4049/jimmunol.173.4.2227. [DOI] [PubMed] [Google Scholar]
- Porter TF, LaCoursiere Y, Scott JR. Immunotherapy for recurrent miscarriage. Cochrane Database Syst Rev. 2006:CD000112. doi: 10.1002/14651858.CD000112.pub2. [DOI] [PubMed] [Google Scholar]
- Prieto GA, Rosenstein Y. Oestradiol potentiates the suppressive function of human CD4+CD25+ regulatory T cells by promoting their proliferation. Immunology. 2006;118:58–65. doi: 10.1111/j.1365-2567.2006.02339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quack KC, Vassiliadou N, Pudney J, Anderson DJ, Hill JA. Leukocyte activation in the decidua of chromosomally normal and abnormal fetuses from women with recurrent abortion. Hum Reprod. 2001;16:949–955. doi: 10.1093/humrep/16.5.949. [DOI] [PubMed] [Google Scholar]
- Raghupathy R. Th1-type immunity is incompatible with successful pregnancy. Immunol Today. 1997;18:478–482. doi: 10.1016/s0167-5699(97)01127-4. [DOI] [PubMed] [Google Scholar]
- Redline RW, Lu CY. Localization of fetal major histocompatibility complex antigens and maternal leukocytes in murine placenta. Implications for maternal–fetal immunological relationship. Lab Invest. 1989;61:27–36. [PubMed] [Google Scholar]
- Robertson SA. Control of the immunological environment of the uterus. Rev Reprod. 2000;5:164–174. doi: 10.1530/ror.0.0050164. [DOI] [PubMed] [Google Scholar]
- Robertson SA. Seminal plasma and male factor signalling in the female reproductive tract. Cell Tissue Res. 2005;322:43–52. doi: 10.1007/s00441-005-1127-3. [DOI] [PubMed] [Google Scholar]
- Robertson SA. Seminal fluid signaling in the female reproductive tract: lessons from rodents and pigs. J Anim Sci. 2007;85:E36–E44. doi: 10.2527/jas.2006-578. [DOI] [PubMed] [Google Scholar]
- Robertson SA, Mau VJ, Tremellen KP, Seamark RF. Role of high molecular weight seminal vesicle proteins in eliciting the uterine inflammatory response to semen in mice. J Reprod Fertil. 1996;107:265–277. doi: 10.1530/jrf.0.1070265. [DOI] [PubMed] [Google Scholar]
- Robertson SA, Sharkey DJ. The role of semen in induction of maternal immune tolerance to pregnancy. Semin Immunol. 2001;13:243–254. doi: 10.1006/smim.2000.0320. [DOI] [PubMed] [Google Scholar]
- Robertson SA, Ingman WV, O'Leary S, Sharkey DJ, Tremellen KP. Transforming growth factor beta—a mediator of immune deviation in seminal plasma. J Reprod Immunol. 2002;57:109–128. doi: 10.1016/s0165-0378(02)00015-3. [DOI] [PubMed] [Google Scholar]
- Robertson SA, Guerin LR, Bromfield JJ, Branson KM, Ahlstrom AC, Care AS. Seminal fluid drives expansion of the CD4+CD25+ T regulatory cell pool and induces tolerance to paternal alloantigens in mice. Biol Reprod. 2009 doi: 10.1095/biolreprod.108.074658. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robillard PY, Hulsey TC, Perianin J, Janky E, Miri EH, Papiernik E. Association of pregnancy-induced hypertension with duration of sexual cohabitation before conception. Lancet. 1994;344:973–975. doi: 10.1016/s0140-6736(94)91638-1. [DOI] [PubMed] [Google Scholar]
- Rutella S, Lemoli RM. Regulatory T cells and tolerogenic dendritic cells: from basic biology to clinical applications. Immunol Lett. 2004;94:11–26. doi: 10.1016/j.imlet.2004.04.015. [DOI] [PubMed] [Google Scholar]
- Rutella S, Pierelli L, Bonanno G, Sica S, Ameglio F, Capoluongo E, Mariotti A, Scambia G, d'Onofrio G, Leone G. Role for granulocyte colony-stimulating factor in the generation of human T regulatory type 1 cells. Blood. 2002;100:2562–2571. doi: 10.1182/blood-2001-12-0291. [DOI] [PubMed] [Google Scholar]
- Saito S, Sakai M. Th1/Th2 balance in preeclampsia. J Reprod Immunol. 2003;59:161–173. doi: 10.1016/s0165-0378(03)00045-7. [DOI] [PubMed] [Google Scholar]
- Saito S, Nishikawa K, Morii T, Narita N, Enomoto M, Ichijo M. Expression of activation antigens CD69, HLA-DR, interleukin-2 receptor-alpha (IL-2R alpha) and IL-2R beta on T cells of human decidua at an early stage of pregnancy. Immunology. 1992;75:710–712. [PMC free article] [PubMed] [Google Scholar]
- Saito S, Sasaki Y, Sakai M. CD4+CD25 high regulatory T cells in human pregnancy. J Reprod Immunol. 2005;65:111–120. doi: 10.1016/j.jri.2005.01.004. [DOI] [PubMed] [Google Scholar]
- Saito S, Shiozaki A, Sasaki Y, Nakashima A, Shima T, Ito M. Regulatory T cells and regulatory natural killer (NK) cells play important roles in feto-maternal tolerance. Semin Immunopathol. 2007;29:115–122. doi: 10.1007/s00281-007-0067-2. [DOI] [PubMed] [Google Scholar]
- Sakaguchi S. Regulatory T cells: key controllers of immunologic self-tolerance. Cell. 2000;101:455–458. doi: 10.1016/s0092-8674(00)80856-9. [DOI] [PubMed] [Google Scholar]
- Sakaguchi S. Naturally arising Foxp3-expressing CD25+CD4+ regulatory T cells in immunological tolerance to self and non-self. Nat Immunol. 2005;6:345–352. doi: 10.1038/ni1178. [DOI] [PubMed] [Google Scholar]
- Sakaguchi S, Sakaguchi N, Asano M, Itoh M, Toda M. Immunologic self-tolerance maintained by activated T cells expressing IL-2 receptor alpha-chains (CD25). Breakdown of a single mechanism of self-tolerance causes various autoimmune diseases. J Immunol. 1995;155:1151–1164. [PubMed] [Google Scholar]
- Samy ET, Parker LA, Sharp CP, Tung KSK. Continuous control of autoimmune disease by antigen-dependent polyclonal CD4+CD25+ regulatory T cells in the regional lymph node. J Exp Med. 2005;202:771–781. doi: 10.1084/jem.20041033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samy ET, Setiady YY, Ohno K, Pramoonjago P, Sharp C, Tung KS. The role of physiological self-antigen in the acquisition and maintenance of regulatory T-cell function. Immunol Rev. 2006;212:170–184. doi: 10.1111/j.0105-2896.2006.00404.x. [DOI] [PubMed] [Google Scholar]
- Santner-Nanan B, Peek MJ, Khanam R, Richarts L, Zhu E, Fazekas De st. Groth B, Nanan RK. Increased Th17 cells and decreased CD4+Foxp3+ T regulatory cells in third trimester pregnancies with pre-eclampsia. 38th Annual Australasian Society of Immunology; Canberra, Australia. 2008. Abstract 65. [Google Scholar]
- Santoso DI, Rogers P, Wallace EM, Manuelpillai U, Walker D, Subakir SB. Localization of indoleamine 2,3-dioxygenase and 4-hydroxynonenal in normal and pre-eclamptic placentae. Placenta. 2002;23:373–379. doi: 10.1053/plac.2002.0818. [DOI] [PubMed] [Google Scholar]
- Sargent IL, Borzychowski AM, Redman CW. Immunoregulation in normal pregnancy and pre-eclampsia: an overview. Reprod Biomed Online. 2006a;13:680–686. doi: 10.1016/s1472-6483(10)60659-1. [DOI] [PubMed] [Google Scholar]
- Sargent IL, Borzychowski AM, Redman CW. NK cells and human pregnancy—an inflammatory view. Trends Immunol. 2006b;27:399–404. doi: 10.1016/j.it.2006.06.009. [DOI] [PubMed] [Google Scholar]
- Sasaki Y, Satomi M, Miyazaki J, Sakai M, Saito S. CD4+CD25+ regulatory T cells are increased in the human early pregnancy decidua and have immunosuppressive activity. Am J Reprod Immunol. 2003;49:356. [Google Scholar]
- Sasaki Y, Sakai M, Miyazaki S, Higuma S, Shiozaki A, Saito S. Decidual and peripheral blood CD4+CD25+ regulatory T cells in early pregnancy subjects and spontaneous abortion cases. Mol Hum Reprod. 2004;10:347–353. doi: 10.1093/molehr/gah044. [DOI] [PubMed] [Google Scholar]
- Sasaki Y, Darmochwal-Kolarz D, Suzuki D, Sakai M, Ito M, Shima T, Shiozaki A, Rolinski J, Saito S. Proportion of peripheral blood and decidual CD4(+) CD25(bright) regulatory T cells in pre-eclampsia. Clin Exp Immunol. 2007;149:139–145. doi: 10.1111/j.1365-2249.2007.03397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato K, Yamashita N, Baba M, Matsuyama T. Modified myeloid dendritic cells act as regulatory dendritic cells to induce anergic and regulatory T cells. Blood. 2003;101:3581–3589. doi: 10.1182/blood-2002-09-2712. [DOI] [PubMed] [Google Scholar]
- Scarparelli F, Sbracia M. Effectiveness of GM-CSF 1 in the treatment of habitual abortion in a controlled study (Abstract 6.7) Am J Reprod Immunol. 2004;51:433–434. [Google Scholar]
- Scarparelli F, Sbracia M. G-CSF treatment in unexplained recurrent spontaneous abortion mobilized different lymphocytes and dendritic cells in peripheral blood (Abstract 1171570850) Am J Reprod Immunol. 2007;57:327. [Google Scholar]
- Scheffold A, Huhn J, Hofer T. Regulation of CD4+CD25+ regulatory T cell activity: it takes (IL-) two to tango. Eur J Immunol. 2005;35:1336–1341. doi: 10.1002/eji.200425887. [DOI] [PubMed] [Google Scholar]
- Seddon B, Mason D. Peripheral autoantigen induces regulatory T cells that prevent autoimmunity. J Exp Med. 1999;189:877–882. doi: 10.1084/jem.189.5.877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shao L, Jacobs AR, Johnson VV, Mayer L. Activation of CD8+ regulatory T cells by human placental trophoblasts. J Immunol. 2005;174:7539–7547. doi: 10.4049/jimmunol.174.12.7539. [DOI] [PubMed] [Google Scholar]
- Sharkey DJ, Macpherson AM, Tremellen KP, Robertson SA. Seminal plasma differentially regulates inflammatory cytokine gene expression in human cervical and vaginal epithelial cells. Mol Hum Reprod. 2007;13:491–501. doi: 10.1093/molehr/gam028. [DOI] [PubMed] [Google Scholar]
- Sharma MD, Baban B, Chandler P, Hou DY, Singh N, Yagita H, Azuma M, Blazar BR, Mellor AL, Munn DH. Plasmacytoid dendritic cells from mouse tumor-draining lymph nodes directly activate mature Tregs via indoleamine 2,3-dioxygenase. J Clin Invest. 2007;117:2570–2582. doi: 10.1172/JCI31911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shevach EM. CD4+ CD25+ suppressor T cells: more questions than answers. Nat Rev Immunol. 2002;2:389–400. doi: 10.1038/nri821. [DOI] [PubMed] [Google Scholar]
- Shimizu J, Yamazaki S, Sakaguchi S. Induction of tumor immunity by removing CD25+CD4+ T cells: a common basis between tumor immunity and autoimmunity. J Immunol. 1999;163:5211–5218. [PubMed] [Google Scholar]
- Shimizu J, Yamazaki S, Takahashi T, Ishida Y, Sakaguchi S. Stimulation of CD25+CD4+ regulatory T cells through GITR breaks immunological self-tolerance. Nat Immunol. 2002;3:135–142. doi: 10.1038/ni759. [DOI] [PubMed] [Google Scholar]
- Sindram-Trujillo AP, Scherjon SA, van Hulst-van Miert PP, Kanhai HH, Roelen DL, Claas FH. Comparison of decidual leukocytes following spontaneous vaginal delivery and elective cesarean section in uncomplicated human term pregnancy. J Reprod Immunol. 2004;62:125–137. doi: 10.1016/j.jri.2003.11.007. [DOI] [PubMed] [Google Scholar]
- Singh N, Seki Y, Takami M, Baban B, Chandler PR, Khosravi D, Zheng X, Takezaki M, Lee JR, Mellor AL, et al. Enrichment of regulatory CD4(+)CD25(+) T cells by inhibition of phospholipase D signaling. Nat Methods. 2006;3:629–636. doi: 10.1038/nmeth903. [DOI] [PubMed] [Google Scholar]
- Sjoblom C, Roberts CT, Wikland M, Robertson SA. Granulocyte-macrophage colony-stimulating factor alleviates adverse consequences of embryo culture on fetal growth trajectory and placental morphogenesis. Endocrinology. 2005;146:2142–2153. doi: 10.1210/en.2004-1260. [DOI] [PubMed] [Google Scholar]
- Smith TR, Kumar V. Revival of CD8+ Treg-mediated suppression. Trends Immunol. 2008;29:337–342. doi: 10.1016/j.it.2008.04.002. [DOI] [PubMed] [Google Scholar]
- Somerset DA, Zheng Y, Kilby MD, Sansom DM, Drayson MT. Normal human pregnancy is associated with an elevation in the immune suppressive CD25+ CD4+ regulatory T-cell subset. Immunology. 2004;112:38–43. doi: 10.1111/j.1365-2567.2004.01869.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinman RM, Hawiger D, Nussenzweig MC. Tolerogenic dendritic cells. Annu Rev Immunol. 2003;21:685–711. doi: 10.1146/annurev.immunol.21.120601.141040. [DOI] [PubMed] [Google Scholar]
- Suri-Payer E, Amar AZ, Thornton AM, Shevach EM. CD4+CD25+ T cells inhibit both the induction and effector function of autoreactive T cells and represent a unique lineage of immunoregulatory cells. J Immunol. 1998;160:1212–1218. [PubMed] [Google Scholar]
- Sutmuller RP, den Brok MH, Kramer M, Bennink EJ, Toonen LW, Kullberg BJ, Joosten LA, Akira S, Netea MG, Adema GJ. Toll-like receptor 2 controls expansion and function of regulatory T cells. J Clin Invest. 2006a;116:485–494. doi: 10.1172/JCI25439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutmuller RP, Morgan ME, Netea MG, Grauer O, Adema GJ. Toll-like receptors on regulatory T cells: expanding immune regulation. Trends Immunol. 2006b;27:387–393. doi: 10.1016/j.it.2006.06.005. [DOI] [PubMed] [Google Scholar]
- Swanson KA, Zheng Y, Heidler KM, Mizobuchi T, Wilkes DS. CDllc+ cells modulate pulmonary immune responses by production of indoleamine 2,3-dioxygenase. Am J Respir Cell Mol Biol. 2004;30:311–318. doi: 10.1165/rcmb.2003-0268OC. [DOI] [PubMed] [Google Scholar]
- Taams LS, van Amelsfort JMR, Tiemessen MM, Jacobs KMG, de Jong EC, Akbar AN, Bijlsma JWJ, Lafeber FPJG. Modulation of monocyte/macrophage function by human CD4+CD25+ regulatory T cells. Human Immunol. 2005;66:222–230. doi: 10.1016/j.humimm.2004.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tafuri A, Alferink J, Moller P, Hammerling GJ, Arnold B. T cell awareness of paternal alloantigens during pregnancy. Science. 1995;270:630–633. doi: 10.1126/science.270.5236.630. [DOI] [PubMed] [Google Scholar]
- Taglauer ES, Trikhacheva AS, Slusser JG, Petroff MG. Expression and function of PDCD1 at the human maternal–fetal interface. Biol Reprod. 2008;79:562–569. doi: 10.1095/biolreprod.107.066324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taguchi O, Nishizuka Y. Experimental autoimmune orchitis after neonatal thymectomy in the mouse. Clin Exp Immunol. 1981;46:425–434. [PMC free article] [PubMed] [Google Scholar]
- Takahashi T, Tagami T, Yamazaki S, Uede T, Shimizu J, Sakaguchi N, Mak TW, Sakaguchi S. Immunologic self-tolerance maintained by CD25(+)CD4(+) regulatory T cells constitutively expressing cytotoxic T lymphocyte-associated antigen 4. J Exp Med. 2000;192:303–310. doi: 10.1084/jem.192.2.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornton AM, Shevach EM. CD4+CD25+ immunoregulatory T cells suppress polyclonal T cell activation in vitro by inhibiting interleukin 2 production. J Exp Med. 1998;188:287–296. doi: 10.1084/jem.188.2.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornton AM, Shevach EM. Suppressor effector function of CD4+CD25+ immunoregulatory T cells is antigen nonspecific. J Immunol. 2000;164:183–190. doi: 10.4049/jimmunol.164.1.183. [DOI] [PubMed] [Google Scholar]
- Thornton AM, Piccirillo CA, Shevach EM. Activation requirements for the induction of CD4+CD25+ T cell suppressor function. Eur J Immunol. 2004;34:366–376. doi: 10.1002/eji.200324455. [DOI] [PubMed] [Google Scholar]
- Thuere C, Zenclussen ML, Schumacher A, Langwisch S, Schulte-Wrede U, Teles A, Paeschke S, Volk HD, Zenclussen AC. Kinetics of regulatory T cells during murine pregnancy. Am J Reprod Immunol. 2007;58:514–523. doi: 10.1111/j.1600-0897.2007.00538.x. [DOI] [PubMed] [Google Scholar]
- Tilburgs T, Roelen DL, van der Mast BJ, van Schip JJ, Kleijburg C, de Groot-Swings GM, Kanhai HH, Claas FH, Scherjon SA. Differential distribution of CD4(+)CD25(bright) and CD8(+)CD28(-) T-cells in decidua and maternal blood during human pregnancy. Placenta. 2006;27(Suppl A):S47–S53. doi: 10.1016/j.placenta.2005.11.008. [DOI] [PubMed] [Google Scholar]
- Tilburgs T, Roelen DL, van der Mast BJ, de Groot-Swings GM, Kleijburg C, Scherjon SA, Claas FH. Evidence for a selective migration of fetus-specific CD4+CD25bright regulatory T cells from the peripheral blood to the decidua in human pregnancy. J Immunol. 2008;180:5737–5745. doi: 10.4049/jimmunol.180.8.5737. [DOI] [PubMed] [Google Scholar]
- Tivol EA, Borriello F, Schweitzer AN, Lynch WP, Bluestone JA, Sharpe AH. Loss of CTLA-4 leads to massive lymphoproliferation and fatal multiorgan tissue destruction, revealing a critical negative regulatory role of CTLA-4. Immunity. 1995;3:541–547. doi: 10.1016/1074-7613(95)90125-6. [DOI] [PubMed] [Google Scholar]
- Trowsdale J, Betz AG. Mother's little helpers: mechanisms of maternal–fetal tolerance. Nat Immunol. 2006;7:241–246. doi: 10.1038/ni1317. [DOI] [PubMed] [Google Scholar]
- Valzasina B, Guiducci C, Dislich H, Killeen N, Weinberg AD, Colombo MP. Triggering of OX40 (CD134) on CD4(+)CD25+ T cells blocks their inhibitory activity: a novel regulatory role for OX40 and its comparison with GITR. Blood. 2005;105:2845–2851. doi: 10.1182/blood-2004-07-2959. [DOI] [PubMed] [Google Scholar]
- Vassiliadou N, Searle RF, Bulmer JN. Elevated expression of activation molecules by decidual lymphocytes in women suffering spontaneous early pregnancy loss. Hum Reprod. 1999;14:1194–1200. doi: 10.1093/humrep/14.5.1194. [DOI] [PubMed] [Google Scholar]
- Verbsky JW. Therapeutic use of T regulatory cells. Curr Opin Rheumatol. 2007;19:252–258. doi: 10.1097/BOR.0b013e3280ad46bb. [DOI] [PubMed] [Google Scholar]
- von Boehmer H, Teh HS, Kisielow P. The thymus selects the useful, neglects the useless and destroys the harmful. Immunol Today. 1989;10:57–61. doi: 10.1016/0167-5699(89)90307-1. [DOI] [PubMed] [Google Scholar]
- Wahl SM, Swisher J, McCartney-Francis N, Chen W. TGF-beta: the perpetrator of immune suppression by regulatory T cells and suicidal T cells. J Leukoc Biol. 2004a;76:15–24. doi: 10.1189/jlb.1103539. [DOI] [PubMed] [Google Scholar]
- Wahl SM, Vazquez N, Chen W. Regulatory T cells and transcription factors: gatekeepers in allergic inflammation. Curr Opin Immunol. 2004b;16:768–774. doi: 10.1016/j.coi.2004.09.006. [DOI] [PubMed] [Google Scholar]
- Waldmann H, Graca L, Cobbold S, Adams E, Tone M, Tone Y. Regulatory T cells and organ transplantation. Semin Immunol. 2004;16:119–126. doi: 10.1016/j.smim.2003.12.007. [DOI] [PubMed] [Google Scholar]
- Waldmann H, Adams E, Fairchild P, Cobbold S. Infectious tolerance and the long-term acceptance of transplanted tissue. Immunol Rev. 2006;212:301–313. doi: 10.1111/j.0105-2896.2006.00406.x. [DOI] [PubMed] [Google Scholar]
- Walker LSK, Chodos A, Eggena M, Dooms H, Abbas AK. Antigen-dependent proliferation of CD4+ CD25+ regulatory T cells in vivo. J Exp Med. 2003;198:249–258. doi: 10.1084/jem.20030315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, Ioan-Facsinay A, van der Voort EI, Huizinga TW, Toes RE. Transient expression of FOXP3 in human activated nonregulatory CD4+ T cells. Eur J Immunol. 2007;37:129–138. doi: 10.1002/eji.200636435. [DOI] [PubMed] [Google Scholar]
- Wegmann TG, Lin H, Guilbert L, Mosmann TR. Bidirectional cytokine interactions in the maternal–fetal relationship: is successful pregnancy a TH2 phenomenon? Immunol Today. 1993;14:353–356. doi: 10.1016/0167-5699(93)90235-D. [DOI] [PubMed] [Google Scholar]
- Weiner HL. Induction and mechanism of action of transforming growth factor-beta-secreting Th3 regulatory cells. Immunol Rev. 2001;182:207–214. doi: 10.1034/j.1600-065x.2001.1820117.x. [DOI] [PubMed] [Google Scholar]
- White CA, Johansson M, Roberts CT, Ramsay AJ, Robertson SA. Effect of interleukin-10 null mutation on maternal immune response and reproductive outcome in mice. Biol Reprod. 2004;70:123–131. doi: 10.1095/biolreprod.103.018754. [DOI] [PubMed] [Google Scholar]
- Xu L, Kitani A, Fuss I, Strober W. Cutting edge: regulatory T cells induce CD4+CD25-Foxp3- T cells or are self-induced to become Th17 cells in the absence of exogenous TGF-beta. J Immunol. 2007;178:6725–6729. doi: 10.4049/jimmunol.178.11.6725. [DOI] [PubMed] [Google Scholar]
- Yamazaki S, Iyoda T, Tarbell K, Olson K, Velinzon K, Inaba K, Steinman RM. Direct expansion of functional CD25+ CD4+ regulatory T cells by antigen-processing dendritic cells. J Exp Med. 2003;198:235–247. doi: 10.1084/jem.20030422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang K, Li D, Luo M, Hu Y. Generation of HSP60-specific regulatory T cell and effect on atherosclerosis. Cell Immunol. 2006;243:90–95. doi: 10.1016/j.cellimm.2007.01.002. [DOI] [PubMed] [Google Scholar]
- Yang H, Qiu L, Chen G, Ye Z, Lu C, Lin Q. Proportional change of CD4+CD25+ regulatory T cells in decidua and peripheral blood in unexplained recurrent spontaneous abortion patients. Fertil Steril. 2008a;89:656–661. doi: 10.1016/j.fertnstert.2007.03.037. [DOI] [PubMed] [Google Scholar]
- Yang XO, Nurieva R, Martinez GJ, Kang HS, Chung Y, Pappu BP, Shah B, Chang SH, Schluns KS, Watowich SS, et al. Molecular antagonism and plasticity of regulatory and inflammatory T cell programs. Immunity. 2008b;29:44–56. doi: 10.1016/j.immuni.2008.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zenclussen AC, Gerlof K, Zenclussen ML, Sollwedel A, Bertoja AZ, Ritter T, Kotsch K, Leber J, Volk HD. Abnormal T-cell reactivity against paternal antigens in spontaneous abortion: adoptive transfer of pregnancy-induced CD4+CD25+ T regulatory cells prevents fetal rejection in a murine abortion model. Am J Pathol. 2005;166:811–822. doi: 10.1016/S0002-9440(10)62302-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zenclussen AC, Gerlof K, Zenclussen ML, Ritschel S, Zambon Bertoja A, Fest S, Hontsu S, Ueha S, Matsushima K, Leber J, et al. Regulatory T cells induce a privileged tolerant microenvironment at the fetal–maternal interface. Eur J Immunol. 2006;36:82–94. doi: 10.1002/eji.200535428. [DOI] [PubMed] [Google Scholar]
- Zhao JX, Zeng YY, Liu Y. Fetal alloantigen is responsible for the expansion of the CD4+CD25+ regulatory T cell pool during pregnancy. J Reprod Immunol. 2007;75:71–81. doi: 10.1016/j.jri.2007.06.052. [DOI] [PubMed] [Google Scholar]
- Zhou M, Mellor AL. Expanded cohorts of maternal CD8+ T-cells specific for paternal MHC class I accumulate during pregnancy. J Reprod Immunol. 1998;40:47–62. doi: 10.1016/s0165-0378(98)00030-8. [DOI] [PubMed] [Google Scholar]
- Zhu J, Paul WE. CD4 T cells: fates, functions, and faults. Blood. 2008;112:1557–1569. doi: 10.1182/blood-2008-05-078154. [DOI] [PMC free article] [PubMed] [Google Scholar]