Abstract
Background
Observational studies suggest that moderate alcohol consumption may lower risk of myocardial infarction (MI) and coronary heart disease (CHD); yet, evidence for this comes almost entirely from Western populations.
Methods
We conducted a prospective cohort study in 64,597 Chinese men aged ≥40 years who were free of clinical CHD at baseline examination. Data on frequency and type of alcohol consumed were collected at the baseline examination in 1991 using a standard protocol. Follow-up evaluation was conducted in 1999–2000, with a response rate of 94%.
Results
Over 494,084 person-years of follow-up, we documented 725 (361 fatal) incident MI and 976 (588 fatal) incident CHD events. After stratification by province to account for multi-stage sampling design and adjustment for age, education, physical activity, cigarette smoking, body mass index, systolic blood pressure, urbanization (urban vs. rural), geographic variation (north vs. south) and history of diabetes, relative risk (95% confidence interval) of MI was 0.93 (0.70–1.24) for participants consuming 1 to 6 drinks/week, 0.66 (0.54–0.82) for those consuming 7 to 34 drinks/week, and 0.58 (0.41–0.81) for those consuming ≥35 drinks/week (P for linear trend <0.0001) compared to non-drinkers. The corresponding relative risks for CHD events were 0.99 (0.77–1.27), 0.67 (0.56–0.81), and 0.58 (0.44–0.78), respectively (P for linear trend <0.0001).
Conclusion
Alcohol consumption may be related to lower risk of MI and CHD in middle-aged and older Chinese men. However, heavy alcohol consumption may lead to increased mortality from other causes; therefore, the implications of these findings should be interpreted cautiously.
Keywords: Myocardial Infarction; Coronary Heart Disease; Alcohol Drinking, Risk Factor; Prospective Studies; Cohort Studies; Men
INTRODUCTION
Coronary heart disease (CHD) is the leading cause of death world-wide and the burden of heart disease has been growing among economically developing nations (1). In China, rapid economic development has significantly changed living conditions, nutrition, and health care. Age-standardized mortality rates for CHD were 93.3 and 76.4 per 100,000 person-years among Chinese men and women in a recent study (2). While low in comparison to CHD rates in some Western countries, these rates have been increasing rapidly in tandem with economic and lifestyle changes. Between the years 1990 and 2020, mortality from CHD in China is expected to increase by 81% in women and 110% in men (3).
Observational studies have suggested that moderate alcohol consumption may have a protective effect on the risk of CHD. Yet, evidence for this relationship comes primarily from studies of Western populations. Only one published case-control study and one prospective study confirmed this association among the Chinese, while another case-control study found no association (4–6). Moreover, a meta-analysis of 51 studies of alcohol consumption and risk of CHD found lesser protective effects and even harmful effects in men living in countries outside the Mediterranean area and where fatal events were used as the outcome (7). It is uncertain that the magnitude and direction of association observed among Western populations can be directly applied to the general Chinese population given their lower serum cholesterol levels, body mass index, and overall risk for CHD. In this study, we examined the relationship between alcohol consumption and risk of CHD among a nationally-representative cohort of middle-aged Chinese men.
METHODS
Study Population
In the 1991 China National Hypertension Survey, a multi-stage random cluster sampling design was used to select a representative sample of the general Chinese population aged 15 years or older from all 30 provinces in mainland China (8). In 1999, investigators from each province were invited to participate in the China National Hypertension Survey Epidemiology Follow-up Study. Of the 30 provinces, 13 were not included in the follow-up because study participants’ contact information was not available. However, the sampling process was conducted independently within each province in the 1991 China National Hypertension survey and the 17 provinces were included in the follow-up study were evenly distributed in different geographic regions representing various economic developing statuses in China (Figure 1). Overall, 83,533 men and 86,338 women who were aged 40 years or older at their baseline examination were eligible to participate in the follow-up study. Only men were included in this analysis because alcohol consumption was rare in women (2.8%). From these men, a total of 78,500 participants or their proxies were identified and interviewed as part of the follow-up study. There was little difference in response rates based on alcohol consumption. For example, among men who identified themselves as drinkers, 26,774 (93.9%) provided follow-up information, while among men who identified themselves as nondrinkers, 44,402 (93.2%) provided follow-up information. After excluding those with incomplete alcohol consumption information (2 provinces did not provide alcohol information, n=12,880), and those with a history of CHD at their baseline examination (n=1,023), data from 64,579 men across 15 provinces were included in this analysis. Participants included in the final analysis were not different from the overall eligible population. For example, the mean (standard deviation) of age is 55.5 (10.6) years, mean body mass index 22.4 (3.4) kg/m2, mean systolic blood pressure 126.2 (21.1) mm Hg, and percentage drinking alcohol 37.4% respectively, in the overall eligible population.
Figure 1.
Map of China with Participating Provinces Highlighted.
Baseline Examination
Baseline data were collected at a single clinic visit by specially trained physicians and nurses using standardized methods with stringent levels of quality control (8). Data on demographic characteristics, medical history, and lifestyle risk factors were obtained using a standard questionnaire administered by trained staff. Work-related physical activity was assessed because leisure-time physical activity was uncommon at that time. Education was dichotomized as less than or at least some high school education. Cigarette smoking was defined as having smoked at least one cigarette per day for one or more years during the participant’s lifetime. Current cigarette smoking was defined as answering “yes” to the question, “Do you smoke now?”. Three blood pressure readings were obtained after the study participant had been seated quietly for 5 minutes. These blood pressure readings were averaged to obtain average systolic and diastolic blood pressures. Hypertension was defined as a mean systolic blood pressure of at least 140 mm Hg and/or a diastolic blood pressure of at least 90 mm Hg and/or use of antihypertensive medication. Body weight and height were measured in light indoor clothing without shoes, using a standard protocol. Body mass index was then calculated as weight in kilograms divided by height in square meters.
Alcohol use was assessed using an interviewer-administered questionnaire with six questions regarding the frequency, amount and type of alcoholic drinks consumed (8,9). Participants were initially asked whether or not they consumed alcohol. Participants who drank alcohol were then asked to specify: (1) the number of years during which they drank alcohol; and (2) the amounts of alcohol consumption per month for each of four types of alcohol: beer, liquor, wine (other than rice wine), and rice wine over the previous year. This quantity was then multiplied by the percent alcohol of each type of drink: for beer, 3.9%, for wine, 11.6%, for rice wine 13.6%, and for liquor, 53.3% (10). Grams of alcohol per month was then summed across the four types of beverages and divided by 12.5 grams to provide the number of standardized alcoholic drinks consumed per month. To obtain the number of standardized drinks per week, the latter number was divided by 4.33. To be consistent with literature on alcohol consumption in Western populations, 12.5 grams of pure alcohol was considered one standard drink (11). Those who reported never drinking or consumed less than 12 drinks per year were categorized as non-drinkers.
Follow-up Data Collection
The follow-up examination, which was conducted between 1999 and 2000, included tracking study participants or their proxies to a current address, performing in-depth interviews to ascertain disease status and vital information, and obtaining hospital records and death certificates. Information on alcohol use was not collected during follow-up. All CHD events reported during the in-person interview were verified by obtaining medical records or death certificates from the local hospital, public health department, or police department. If hospitalization occurred due to the event, participant’s hospital records, including medical history, physical examination findings, laboratory test results including cardiac enzymes, EKG, coronary angiography, discharge diagnosis, and/or autopsy reports were abstracted by trained staff using a standard form. In addition, photocopies of selected sections of the participant’s inpatient record, discharge summary, and pathology reports were obtained. An endpoint assessment committee within each province reviewed and confirmed (or rejected) the diagnosis of stroke based on the abstracted information using pre-established criteria. A study-wide endpoint assessment committee at the Chinese Academy of Medical Sciences in Beijing, China, reviewed all medical and death records and determined the final diagnosis or underlying cause of death. There was 88.6% ascertainment of medical records (specifically ECG, cardiac enzyme results, and/or coronary angiography) for persons reporting a diagnosis of acute myocardial infarction (MI) and 81.5% ascertainment of medical records for persons reporting a diagnosis of CHD. Death certificates were obtained for 99.9% of deceased participants. Two committee members independently verified the diagnosis or cause of death and discrepancies were adjudicated by discussion involving additional committee members. All members of the local and study-wide end point assessment committees were blinded to the participant’s baseline risk factor information.
This study was approved by the Tulane University Health Sciences Center Institutional Review Board and the Cardiovascular Institute and Fu Wai Hospital Ethics Committee. Written informed consent was obtained from all study participants at their follow-up visit.
Statistical Analysis
Study participants were grouped into 4 categories by alcohol consumption at the baseline examination (non-drinkers, 1 to 6 drinks/week, 7 to 34 drinks/week, more than 35 drinks/week). These categories were created to allow examination of the association between alcohol consumption and CHD without making a priori assumptions about the shape of the dose-response curve and to provide meaningful ranges of alcohol intake experienced by a general population. Category cut-offs were selected after a survey of national and international guidelines for moderate drinking (12). While no guidelines have been issued by the People’s Republic of China, the Hong Kong Department of Health has issued guidelines which state that alcohol consumption should not exceed 21 drinks/week for men (or 3 drinks per day), whereas the Central Authority of Catalonia recommends that alcohol consumption not exceed 35 drinks/week (or 5 drinks/day) (12). In order to avoid missing a possible J or U shape to the relationship, we divided drinkers into even quintiles and tested for a quadratic relationship as well as linear one. We also fitted restricted cubic splines to the dataset to test for nonlinear relationships in our time-to-event analysis (13). Person-years of follow-up were calculated from the date of baseline examination until the date of incident or fatal CHD event, death from other causes, or follow-up interview, whichever came first, for each study participant and grouped according to age in 5 year categories. Age standardized myocardial infarction (MI) and CHD incidence rates were calculated using the age distribution of the Chinese population from year 2000 census data.
Kaplan-Meier product limit methods were used to calculate the cumulative incidence and mortality of MI and CHD according to alcohol consumption categories (14) and Log-rank test was utilized to test the statistical significance of differences among these cumulative rates. Cox proportional hazards regression models were stratified by primary sampling unit (province) to account for the multi-stage sampling design, and adjusted for baseline age, cigarette smoking, physical activity (low, moderate, high), body mass index, systolic blood pressure (average of three measures), education (less than high school or high school graduate), geographic region (north vs. south), urbanization (urban vs. rural), and self-reported history of diabetes. History of diabetes was modeled as a time-dependent variable. Multivariate-adjusted relative risks were calculated using study participants who were non-drinkers as the reference group. The presence of a linear trend was tested using the medians of alcohol consumption in each group treated as a continuous variable. Subgroup analyses by age group, hypertension status, cigarette smoking, and body mass index were conducted for CHD and MI incidence. The sample sizes were too small to conduct subgroup analyses for CHD or MI mortality due to low event rates. All statistical analyses were conducted using SAS statistical software version 9.1 (SAS Institute Inc, Cary, NC).
RESULTS
Baseline characteristics of the study participants are presented according to alcohol consumption category in Table 1. On average, drinkers were younger than nondrinkers. Drinkers were more often smokers, tended to perform more physical activity in the course of their work, and were more often hypertensive than non-drinkers. On average, body mass index was slightly higher among drinkers than non-drinkers, with the exception of the heaviest drinkers. Men who drank alcohol were more often residents of rural areas and more often lived in Northern China than non-drinkers.
Table 1.
Baseline Characteristics according to Alcohol Consumption among N=64,597 Chinese Men.*
| Characteristics | Alcohol Consumption, Drinks/Week | |||
|---|---|---|---|---|
| Non-drinkers n=39,935 |
1 to 6 n=4,804 |
7 to 34 n=13,469 |
≥35 n=6,389 |
|
| Age (yr) | 56.4±10.7 | 54.0±9.9 | 54.8±10.0 | 54.7±9.6 |
| High-school graduate (%) | 49.8 | 54.9 | 46.8 | 34.5 |
| Current cigarette smoker (%) | 32.2 | 32.8 | 28.3 | 14.5 |
| Physical activity (%)† | ||||
| Low | 43.5 | 38.8 | 32.1 | 27.1 |
| High | 44.2 | 47.9 | 51.0 | 60.8 |
| Body Mass Index (kg/m2) | 22.3±3.4 | 22.5±3.3 | 22.5±3.3 | 21.7±3.1 |
| Blood pressure (mm Hg) | ||||
| Systolic | 126.3±21.1 | 124.8±19.9 | 127.2±20.9 | 129.0±22.1 |
| Diastolic | 78.2±11.9 | 78.7±11.7 | 79.5±12.1 | 79.7±12.7 |
| Hypertension (%) ‡ | 26.4 | 25.4 | 28.5 | 31.1 |
| Unemployed (%) | 26.3 | 17.6 | 20.7 | 21.9 |
| Living in Northern China (%) | 60.5 | 67.5 | 70.4 | 51.4 |
| Urban Residence (%) | 63.8 | 62.3 | 59.4 | 41.5 |
Plus-minus values are means ±SD.
Physical activity was assessed by categorizing the physical labor involved in a participant’s work at the time of the study. Those who did not work were assigned to the group with low physical activity. Percentages do not sum to 100 as data for the middle category are not shown.
Hypertension was defined as one or more of the following: a systolic blood pressure greater than or equal to 140 mm Hg, a diastolic blood pressure greater than or equal to 90 mm Hg, or the use of antihypertensive medications.
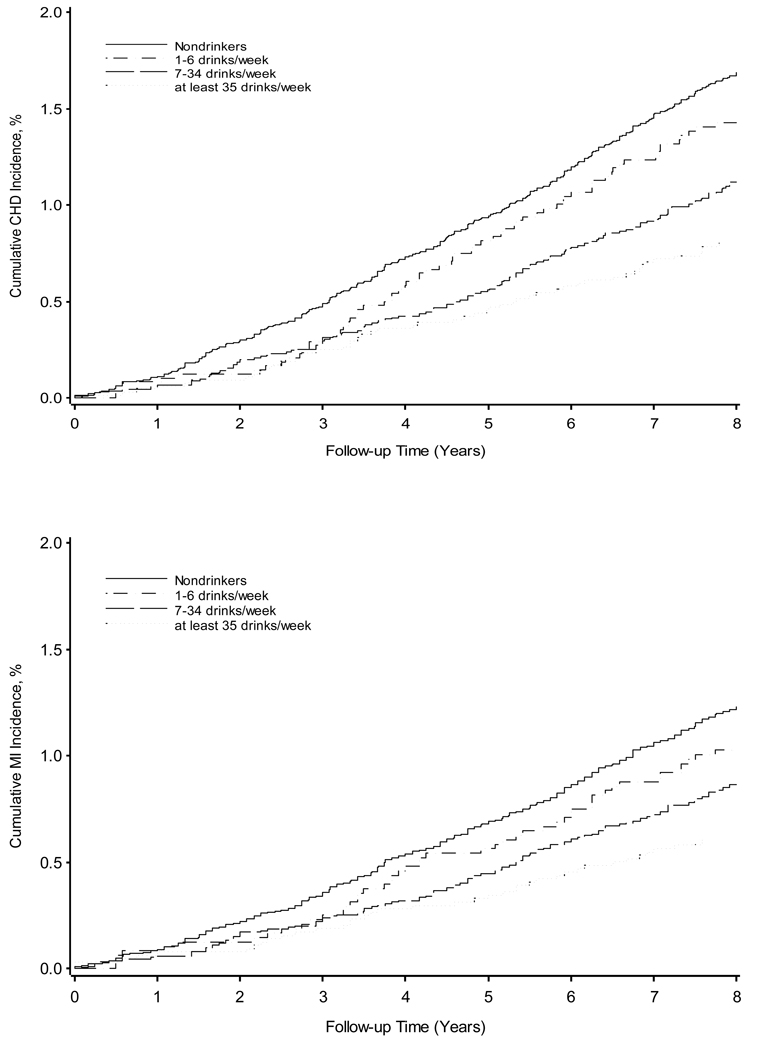
During an average follow-up of more than 8 years (494,084 person-years), 976 incident (588 fatal) CHD events, including 725 incident (361 fatal) MI events were documented. The age-standardized incidence rate per 100,000 person-years for MI among nondrinkers was 123.9; among those consuming 1 to 6 drinks/week the rate was 120.4; among those consuming 7 to 34 drinks/week, the rate was 92.9; and for those who consumed ≥35 drinks/week, the rate was 66.5. The age-standardized incidence rate per 100,000 person-years for CHD events among nondrinkers was 164.9; among those consuming 1 to 6 drinks/week the rate was 172.7; among those consuming 7 to 34 drinks/week, the rate was 122.7; and for those who consumed ≥35 drinks/week, the rate was 90.4. Kaplan-Meier product limit estimates for cumulative incidence of CHD and MI are presented in Figure 2. The cumulative incidence and mortality from MI and CHD were statistically significantly different by alcohol consumption (all log-rank p-values <0.0001).
Figure 2.
Cumulative Incidence of Myocardial Infarction and Coronary Heart Disease among 64,597 Chinese Men by Alcohol Consumption.
Relative risks (RR) and 95% confidence intervals (95% CI) for MI and CHD incidence and mortality in relation to alcohol consumption are presented in Table 2. In age-adjusted Cox proportional hazards models, there was a statistically significant inverse relationship between alcohol consumption and both incidence and mortality of MI and CHD events (p-value for linear trend <.0001 for all outcomes). These relationships were not attenuated after additional adjustment for established risk factors for CHD such as cigarette smoking, physical activity, body mass index, systolic blood pressure, education, geographic region, urbanization, and self-reported history of diabetes.
Table 2.
Relative Risk and 95% CI of Myocardial Infarction and Coronary Heart Disease according to Baseline Alcohol Consumption among N=64,597 Chinese Men.
| Alcohol consumption, Drinks/Week | P for Linear Trend |
||||
|---|---|---|---|---|---|
| Non-drinkers | 1 to 6 | 7 to 34 | ≥35 | ||
| Person years | 303,016 | 37,483 | 104,463 | 49,122 | |
| MI Incidence | |||||
| No. of Events | 513 | 52 | 121 | 39 | |
| Age-adjusted relative risk | 1.00 | 0.94 (0.70, 1.25) | 0.69 (0.56, 0.84)†† | 0.60 (0.43, 0.84) †† | <.000 |
| Multivariate-adjusted relative risk* | 1.00 | 0.93 (0.70, 1.24) | 0.66 (0.54, 0.82) †† | 0.58 (0.41, 0.81) †† | <.000 |
| MI Mortality | |||||
| No. of Events | 263 | 27 | 53 | 18 | |
| Age-adjusted relative risk | 1.00 | 1.07 (0.72, 1.59) | 0.63 (0.47, 0.85) ‡ | 0.53 (0.32, 0.87) † | 0.0003 |
| Multivariate-adjusted relative risk* | 1.00 | 1.05 (0.70, 1.57) | 0.58 (0.42, 0.79) †† | 0.46 (0.28, 0.76) ‡ | <.0001 |
| CHD Incidence | |||||
| No. of Events | 694 | 71 | 159 | 52 | |
| Age-adjusted relative risk | 1.00 | 0.99 (0.78, 1.28) | 0.70 (0.59, 0.83) †† | 0.61 (0.46, 0.82) †† | <.000 |
| Multivariate-adjusted relative risk* | 1.00 | 0.99 (0.77, 1.27) | 0.67 (0.56, 0.81) †† | 0.58 (0.44, 0.78) †† | <.000 |
| CHD Mortality | |||||
| No. of Events | 426 | 48 | 84 | 30 | |
| Age-adjusted relative risk | 1.00 | 1.21 (0.90, 1.63) | 0.64 (0.50, 0.81) †† | 0.60 (0.41, 0.88) ‡ | <.000 |
| Multivariate-adjusted relative risk* | 1.00 | 1.20 (0.88, 1.62) | 0.59 (0.46, 0.75) †† | 0.53 (0.36, 0.78) ‡ | <.000 |
| CVD Mortality | |||||
| No. of Events | 2,916 | 249 | 746 | 366 | |
| Age-adjusted relative risk | 1.00 | 0.89 (0.79, 1.02) | 0.88 (0.81, 0.96) | 1.02 (0.91, 1.14) | 0.08 |
| Multivariate-adjusted relative risk* | 1.00 | 0.88 (0.77, 1.01) | 0.79 (0.73, 0.86) | 0.86 (0.77, 0.96) | <.0001 |
| Non-CVD Mortality | |||||
| No. of Events | 3,391 | 290 | 956 | 572 | |
| Age-adjusted relative risk | 1.00 | 0.86 (0.76, 0.97) | 0.95 (0.89, 1.03) | 1.18 (1.08, 1.29) | 0.11 |
| Multivariate-adjusted relative risk* | 1.00 | 0.84 (0.74, 0.95) | 0.87 (0.81, 0.94) | 1.05 (0.95, 1.15) | 0.14 |
stratified by province and adjusted for age, body-mass index, average systolic blood pressure, physical activity, cigarette smoking, diabetes education, urban or rural residence, and living in North China;
p<0.05;
p<0.01;
p<0.001
We conducted subgroup analyses to further examine the relationship between alcohol consumption and MI and CHD incidence among men with selected characteristics such as age, hypertension, cigarette smoking, and overweight (Table 3). Relationships were generally consistent for alcohol consumption and risk of MI and CHD events across categories. Those consuming more drinks per week had lower risks of MI and CHD compared to other groups. Tests for effect modification of covariables (including body mass index) on the relationship between alcohol consumption and risk of MI and CHD were significant but ordinal in character.
Table 3.
Multivariate Adjusted Relative Risk and 95% CI for CHD Incidence and Mortality by Specific Characteristics among Chinese Men*.
| Alcohol consumption, Drinks/Week | P for Linear Trend | ||||
|---|---|---|---|---|---|
| Non-drinkers | 1 to 6 | 7 to 34 | ≥35 | ||
| CHD Incidence | |||||
| Age, years | |||||
| >60 (n=20,954) | 1.00 | 0.92 (0.66, 1.28) | 0.58 (0.45, 0.74) †† | 0.60 (0.40, 0.88) † | <.0001 |
| ≤60 (n=43,295) | 1.00 | 0.99 (0.69, 1.43) | 0.82 (0.63, 1.06) | 0.60 (0.39, 0.93) † | 0.01 |
| Hypertension | |||||
| Yes (n=17,505) | 1.00 | 1.07 (0.77, 1.47) | 0.57 (0.44, 0.75) †† | 0.63 (0.43, 0.92) † | <.0001 |
| No (n=46,744) | 1.00 | 0.83 (0.57, 1.20) | 0.80 (0.63, 1.02) | 0.55, (0.35, 0.87) † | 0.003 |
| Current Smoker | |||||
| Yes (n=39,037) | 1.00 | 1.02 (0.75, 1.37) | 0.72 (0.58, 0.89) †† | 0.61 (0.44, 0.85) ‡ | <.0001 |
| No (n=25,212) | 1.00 | 0.83 (0.53, 1.28) | 0.64 (0.46, 0.88) ‡ | 0.61 (0.33, 1.16) | 0.002 |
| Body Mass Index | |||||
| ≥25 (n=13,057) | 1.00 | 1.07 (0.79, 1.75) | 0.77 (0.57, 1.06) | 0.75 (0.43, 1.29) | 0.09 |
| <25 (n=51,192) | 1.00 | 0.83 (0.61, 1.14) | 0.65 (0.52, 0.81) †† | 0.57 (0.41, 0.81) ‡ | <.0001 |
| MI Incidence | |||||
| Age, years | |||||
| >60 (n=20,954) | 1.00 | 0.73 (0.47, 1.14) | 0.55 (0.40, 0.75) †† | 0.63 (0.40, 1.01) | <.0001 |
| ≤60 (n=43,295) | 1.00 | 1.04 (0.71, 1.52) | 0.79 (0.60, 1.05) | 0.54 (0.33, 0.87) † | 0.004 |
| Hypertension | |||||
| Yes (n=17,505) | 1.00 | 0.96 (0.65, 1.43) | 0.57 (0.42, 0.78) †† | 0.58 (0.37, 0.91) † | <.0001 |
| No (n=46,744) | 1.00 | 0.81 (0.53, 1.24) | 0.78 (0.59, 1.03) | 0.61 (0.38, 0.99) † | 0.01 |
| Current Smoker | |||||
| Yes (n=39,037) | 1.00 | 0.96 (0.68, 1.36) | 0.67 (0.52, 0.86) †† | 0.60 (0.42, 0.87) ‡ | 0.0002 |
| No (n=25,212) | 1.00 | 0.73 (0.42, 1.24) | 0.71 (0.49, 1.01) | 0.59 (0.28, 1.26) | 0.02 |
| Body Mass Index | |||||
| ≥25 (n=13,057) | 1.00 | 1.24 (0.81, 1.92) | 0.75 (0.53, 1.07) | 0.79 (0.43, 1.44) | 0.15 |
| <25 (n=51,192) | 1.00 | 0.70 (0.47, 1.03) | 0.64 (0.50, 0.82) †† | 0.54 (0.37, 0.81) ‡ | <.0001 |
N=64,249 with complete covariate information; adjusted for age, body-mass index, average systolic blood pressure, physical activity, cigarette smoking, diabetes education, urban or rural residence, and living in North China;
p<0.05;
p<0.01;
p<0.001
Mortality from non-CVD causes was not linearly increased among drinkers as compared to non-drinkers in this cohort. A statistically significant J-shaped association was identified where, compared to non-drinkers, the relative risks of non-CVD mortality (RR; 95% CI) were significantly lower for men who drank 1 to 6 drinks/week (0.84; 0.74 to 0.95), 7–34 drinks/week (0.87; 0.81 to 0.94), and not significantly different from non-drinkers for persons consuming ≥35 drinks/week (1.05; 0.95–1.15).
DISCUSSION
In this prospective cohort study of 64,597 Chinese men free of CHD at baseline, we identified a strong and statistically significant inverse relationship between alcohol consumption and risk of MI and CHD incidence and mortality, which remained after adjustment for age, body mass index, average systolic blood pressure, physical activity, urbanization (urban vs. rural), geographic region (north vs. south), cigarette smoking, history of diabetes, and education. Men consuming more alcoholic drinks per week appeared to be at a lower risk for incident and fatal MI and CHD events than their counterparts who drank less or did not drink at all. Alcohol consumption in relation to all-cause mortality was examined in a separate manuscript (15). There was a J-shaped relationship between non-CVD mortality and alcohol consumption in this cohort. The most common non-CVD causes of mortality were malignant neoplasm, cirrhosis, accidents, and other causes.
Our results are consistent with those of Yuan and colleagues who examined cardiovascular and all-cause mortality among a cohort of 18,244 middle-age men in Shanghai, China (6). Compared to lifelong non-drinkers, they found a 36% lower mortality from ischemic heart disease (RR, 0.64; 95% CI, 0.41 to 0.99) among those who consumed 1 to 28 drinks/week, after adjustment for age, education, and cigarette smoking. Yuan and colleagues did not examine non-fatal coronary events in their study. In a case-control study of alcohol consumption and non-fatal CHD among Hong-Kong Chinese, Lam and colleagues examined the characteristics of 598 CHD hospital cases and 1,100 community controls (5). They found a significant protective effect for all drinking frequencies examined (four categories ranging from less than monthly to >3 days/week) and for all types of drink preferences (beer, spirits, others, no preference). In contrast, Donnan and colleagues did not find a relationship between alcohol consumption and risk of MI in a case-control study conducted in southern Chinese population (4).
A small number of studies conducted among the Japanese are also available for comparison. In a study of 8,476 middle-aged, working Japanese men, Kitamura and colleagues identified 83 new CHD events over an average of 8.8 years of follow-up (12). After adjustment for major CHD risk factors, RR (95% CI) of CHD was 0.83 (0.24–2.86) in ex-drinkers, 0.69 (0.37–1.29) in drinkers consuming less than 2 drinks/day, 0.55 (0.29–1.05) in drinkers consuming 2 to 4 drinks/day, 0.41 (0.19–0.88) in drinkers of 4 to 5.5 drinks/day, and 0.59 (0.23–1.51) in drinkers of more than 5.5 drinks per day, as compared to non-drinkers. In a 5 year 10 prospective study of 2,890 middle-aged Japanese men, Iso and colleagues identified 34 CHD events (13). They found no significant relationship between consumption of alcohol and CHD events. Our results greatly expand the present literature by demonstrating a significant inverse association between alcohol consumption and risk of MI and CHD among a nationally representative sample of the Chinese male population.
This study has several strengths which lend support to our findings. Foremost are its large sample size and high follow-up rate, which allows us to examine the relationship between alcohol consumption and risk of CHD with precision. Second, our study was conducted among a nationally representative sample of men in the general Chinese population, which allows the study findings to apply to a large population. Finally, the association between alcohol consumption and relative risk of CHD was consistent among subgroups by age, hypertension status, smoking, and body mass index.
There are also some potential limitations to our study. Data on dietary patterns, leisure-time physical activity, medications for lipid lowering, prophylactic aspirin use, and serum lipid levels were not available at baseline. Therefore, the potential confounding effect of these factors on MI and CHD incidence and mortality could not be controlled. However, leisure time physical activity, prophylactic aspirin use, and lipid-lowering medication use were rare in China during the decade of the 1990s (14–16). In addition, studies in Chinese populations have shown that alcohol intake is associated with higher levels of total and HDL cholesterol in a dose-response fashion (17,18). This is likely to be an important part of the mechanism by which alcohol may decrease risk of coronary heart disease and therefore should not be adjusted in the epidemiologic analyses of alcohol consumption and CHD. Other studies have demonstrated that among U.S. adults, nondrinkers were more likely to have sociodemographic and behavioral characteristics associated with increased CVD mortality than moderate drinkers (19). To reduce the potential for this type of confounding, we controlled for smoking status, physical activity, education level, as well as urbanization in our analysis. Moreover, medical record ascertainment did not differ by drinking status. For nondrinkers in our population, medical record ascertainment was 89.5% for reported diagnoses of MI and 80.3% for reported diagnoses of CHD. For the heaviest drinkers in our population, the corresponding percentages were 87.2% and 82.7%. We did not collect dietary data in the current study. However, we adjusted for urbanization (urban vs. rural) and geographic region (north vs. south), the two most important factors which affected dietary habits in China. Alcohol intake was assessed at baseline examination and may have changed over the course of follow-up. Nevertheless, little change was observed in alcohol consumption over 6 years of follow up in a recent assessment of alcohol intake and risk of CHD among men with hypertension in the Health Professional’s Follow-up Study (20). Diagnosis of diabetes was self-reported in our study and so likely underestimates the actual number of diabetics in the study population. Finally, the possibility that many nondrinkers may be former drinkers who have experienced adverse health events which may lead to a higher risk of CHD mortality must also be addressed. While we do not have information on former drinking in our study, other studies have shown that the presence of “sick quitters” does not explain the apparent benefits of alcohol consumption on the risk of CHD (21).
Support for the protective effects of alcohol consumption on incidence and mortality from MI and CHD comes from many studies. Moderate alcohol consumption increases high-density lipoprotein cholesterol levels and fibrinolytic activity, while decreasing platelet aggregation (22,23). In addition, alcohol consumption decreases gluconeogenesis and so may contribute to the maintenance of normoglycemia (24,25). A recent nested case-control study conducted among 747 women enrolled in the Nurses’ Health Study and 798 men enrolled in the Health Professionals’ Follow-up Study found that the association between alcohol and risk of MI was almost entirely attributable to the relationship of alcohol with HDL cholesterol, fibrinogen, and hemoglobin A1C levels (26).
In summary, we found a significant inverse relationship between alcohol consumption and risk of MI and CHD among a large and nationally representative sample of Chinese men aged 40 years or older. However, these results must be viewed in the context of the potential harm of alcohol consumption as well as its benefits. In middle-aged and older men, alcohol consumption might reduce risk of CHD. However, this effect might not directly apply to a younger age group. Any advice regarding the consumption of alcohol should be tailored to the individual patient's risks and potential benefits.
ACKNOWLEDGEMENTS
This study was supported by a national Grant-in-Aid (9750612N) from the American Heart Association, Dallas, TX, and partially supported by a grant (R01 HL68057) from the National Heart, Lung, and Blood Institute of the National Institutes of Health, Bethesda, MD, and by a grant (1999-272) from the Chinese Ministry of Health, Beijing, China and by the Chinese Academy of Medical Sciences, Beijing, China. Dr. Bazzano was supported by a Building Interdisciplinary Research Careers in Women’s Health Scholarship (K12-HD43451) co-funded by the Office of Research on Women’s Health (ORWH) and the Office of Dietary Supplements (ODS), of the National Institutes of Health, Bethesda, MD. Dr. Reynolds was partially supported by grant number (P20-RR17659) from the National Center for Research Resources, of the National Institutes of Health, Bethesda, MD. Dr. Bazzano had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Grant Support: This study was supported by a national Grant-in-Aid (9750612N) from the American Heart Association, Dallas, TX, and partially supported by a grant (U01 HL072507) from the National Heart, Lung, and Blood Institute of the National Institutes of Health, Bethesda, MD, and by a grant (1999-272) from the Chinese Ministry of Health, Beijing, China and by the Chinese Academy of Medical Sciences, Beijing, China. Dr. Bazzano was supported by a Building Interdisciplinary Research Careers in Women’s Health Scholarship (K12-HD43451) co-funded by the Office of Research on Women’s Health (ORWH) and the Office of Dietary Supplements (ODS), of the National Institutes of Health, Bethesda, MD. Dr. Reynolds was partially supported by grant number (P20-RR17659) from the National Center for Research Resources, of the National Institutes of Health, Bethesda, MD.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease Study. Lancet. 1997;349:1498–1504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 2.He J, Gu D, Wu X, et al. Major causes of death among men and women in China. N Engl J Med. 2005;353:1124–1134. doi: 10.1056/NEJMsa050467. [DOI] [PubMed] [Google Scholar]
- 3.Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation. 2001;104:2746–2753. doi: 10.1161/hc4601.099487. [DOI] [PubMed] [Google Scholar]
- 4.Donnan SP, Ho SC, Woo J, et al. Risk factors for acute myocardial infarction in a southern Chinese population. Ann Epidemiol. 1994;4:46–58. doi: 10.1016/1047-2797(94)90042-6. [DOI] [PubMed] [Google Scholar]
- 5.Lam TH, Chung SF, Janus ED, et al. Smoking, alcohol drinking and non-fatal coronary heart disease in Hong Kong Chinese. Ann Epidemiol. 2002;12:560–567. doi: 10.1016/s1047-2797(01)00294-0. [DOI] [PubMed] [Google Scholar]
- 6.Yuan JM, Ross RK, Gao YT, Henderson BE, Yu MC. Follow up study of moderate alcohol intake and mortality among middle aged men in Shanghai, China. BMJ. 1997;314:18–23. doi: 10.1136/bmj.314.7073.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Corrao G, Rubbiati L, Bagnardi V, Zambon A, Poikolainen K. Alcohol and coronary heart disease: a meta-analysis. Addiction. 2000;95:1505–1523. doi: 10.1046/j.1360-0443.2000.951015056.x. [DOI] [PubMed] [Google Scholar]
- 8.Wu X, Duan X, Gu D, Hao J, Tao S, Fan D. Prevalence of hypertension and its trends in Chinese populations. Int J Cardiol. 1995;52:39–44. doi: 10.1016/0167-5273(95)02443-z. [DOI] [PubMed] [Google Scholar]
- 9.Rose GA, Blackburn H, Gillum RF, Prineas RJ. Cardiovascular survey methods. 2nd ed. Geneva: World Health Organization; 1982. [PubMed] [Google Scholar]
- 10.Nutrition NIo. Chinese Food Composition Table. Beijing: People's Health Press; 1986. [Google Scholar]
- 11.Turner C. How much alcohol is in a 'standard drink'? An analysis of 125 studies. Br J Addict. 1990;85:1171–1175. doi: 10.1111/j.1360-0443.1990.tb03442.x. [DOI] [PubMed] [Google Scholar]
- 12.Kitamura A, Iso H, Sankai T, et al. Alcohol intake and premature coronary heart disease in urban Japanese men. Am J Epidemiol. 1998;147:59–65. doi: 10.1093/oxfordjournals.aje.a009367. [DOI] [PubMed] [Google Scholar]
- 13.Iso H, Kitamura A, Shimamoto T, et al. Alcohol intake and the risk of cardiovascular disease in middle-aged Japanese men. Stroke. 1995;26:767–773. doi: 10.1161/01.str.26.5.767. [DOI] [PubMed] [Google Scholar]
- 14.Critchley J, Liu J, Zhao D, Wei W, Capewell S. Explaining the increase in coronary heart disease mortality in Beijing between 1984 and 1999. Circulation. 2004;110:1236–1244. doi: 10.1161/01.CIR.0000140668.91896.AE. [DOI] [PubMed] [Google Scholar]
- 15.Muntner P, Gu D, Wildman RP, et al. Prevalence of physical activity among Chinese adults: results from the International Collaborative Study of Cardiovascular Disease in Asia. Am J Public Health. 2005;95:1631–1636. doi: 10.2105/AJPH.2004.044743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Muntner P, Gu D, Reynolds RF, et al. Therapeutic lifestyle changes and drug treatment for high blood cholesterol in China and application of the Adult Treatment Panel III guidelines. Am J Cardiol. 2005;96:1260–1265. doi: 10.1016/j.amjcard.2005.06.068. [DOI] [PubMed] [Google Scholar]
- 17.Yin R, Chen Y, Pan S, et al. Comparison of lipid levels, hyperlipidemia prevalence and its risk factors between Guangxi Hei Yi Zhuang and Han populations. Arch Med Res. 2006;37:787–793. doi: 10.1016/j.arcmed.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 18.Chen Z, Peto R, Collins R, MacMahon S, Lu J, Li W. Serum cholesterol concentration and coronary heart disease in population with low cholesterol concentrations. BMJ. 1991;303:276–282. doi: 10.1136/bmj.303.6797.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Naimi TS, Brown DW, Brewer RD, et al. Cardiovascular risk factors and confounders among nondrinking and moderate-drinking U.S. adults. Am J Prev Med. 2005;28:369–373. doi: 10.1016/j.amepre.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 20.Beulens JW, Rimm EB, Ascherio A, Spiegelman D, Hendriks HF, Mukamal KJ. Alcohol consumption and risk for coronary heart disease among men with hypertension. Ann Intern Med. 2007;146:10–19. doi: 10.7326/0003-4819-146-1-200701020-00004. [DOI] [PubMed] [Google Scholar]
- 21.Mukamal KJ, Rimm EB. Alcohol's effects on the risk for coronary heart disease. Alcohol Res Health. 2001;25:255–261. [PMC free article] [PubMed] [Google Scholar]
- 22.Salem RO, Laposata M. Effects of alcohol on hemostasis. Am J Clin Pathol. 2005;123 Suppl:S96–S105. doi: 10.1309/113N8EUFXYUECCNA. [DOI] [PubMed] [Google Scholar]
- 23.Zakhari S. Alcohol and the cardiovascular system: molecular mechanisms for beneficial and harmful action. Alcohol Health Res World. 1997;21:21–29. [PMC free article] [PubMed] [Google Scholar]
- 24.Avogaro A, Valerio A, Miola M, et al. Ethanol impairs insulin-mediated glucose uptake by an indirect mechanism. J Clin Endocrinol Metab. 1996;81:2285–2290. doi: 10.1210/jcem.81.6.8964865. [DOI] [PubMed] [Google Scholar]
- 25.Siler SQ, Neese RA, Christiansen MP, Hellerstein MK. The inhibition of gluconeogenesis following alcohol in humans. Am J Physiol. 1998;275:E897–E907. doi: 10.1152/ajpendo.1998.275.5.E897. [DOI] [PubMed] [Google Scholar]
- 26.Mukamal KJ, Jensen MK, Gronbaek M, et al. Drinking frequency, mediating biomarkers, and risk of myocardial infarction in women and men. Circulation. 2005;112:1406–1413. doi: 10.1161/CIRCULATIONAHA.105.537704. [DOI] [PubMed] [Google Scholar]