Abstract
Background
Blount’s disease is a multi-planar deformity affecting the pediatric population which leads to varus alignment of the lower extremities. The Multi-Axial Correction (MAC) monolateral external fixation system (Biomet, Parsippany, NJ, USA) is a non-circular fixator that was developed as a response to the technical difficulty for both patients and physicians of placing, managing, and tolerating a circular fixator. The purpose of this study was to determine the efficacy of the MAC system for the treatment of pediatric patients with Blount’s disease.
Methods
A retrospective analysis of 17 consecutive patients with surgically corrected Blount’s disease using the MAC system with tibial and fibular osteotomies was identified. Patient charts and radiographs at three different time points (pre-operative, fixator removal, and final follow-up) were reviewed. The mechanical axis deviation (MAD), tibial–femoral angle (TFA), medial proximal tibial angle (MPTA), and posterior proximal tibial angle (PPTA) were measured in the MAC group at the three time points mentioned previously. The total wear time, total operative time, and post-operative complications were noted.
Results
The MAC system was able to correct the deformity of Blount’s disease as measured by a decrease in the MAD (40.2 ± 29.3 mm; P ≤ 0.001) and TFA (15.9 ± 13.7°; P ≤ 0.001), as well as an increase in the MPTA (15.7 ± 14.6°; P = 0.001) at the time of fixator removal. The correction was maintained for these parameters at the time of final follow-up (P ≤ 0.025). The absolute values obtained at final follow-up for MAD (20.5 ± 12.7 mm medial), TFA (8.0 ± 4.1° varus), and MPTA (83.7 ± 8.1°) after correction with the MAC system were close to what is considered as normal for these indices. The most common complications noted were superficial pin tract infections and/or cellulitis, with no patients having nerve palsy, compartment syndrome, non-union, or leg length discrepancies. The total time that the fixator was on the patients prior to removal was 130.6 days (standard deviation [SD] = 44.8). The mean operative time was 120.6 min (SD = 21.2).
Conclusions
Correction of Blount’s disease with osteotomy of the tibia and fibula as well as dynamic fixation with the MAC system achieved deformity correction as measured by radiographic indices with minimal intra- and post-operative complications. The ease of application and adjustment of the MAC system makes it an attractive option for Blount’s deformity correction.
Keywords: Blount’s disease, Tibia vara, Deformity correction, External fixation, Osteotomy
Introduction
Blount, in 1937 [1], described tibia vara as a developmental condition of the proximal tibia involving the epiphysis, physis, and metaphysis. Based on the age of onset and radiographic features, it is sub-classified into early-onset/infantile, juvenile, and adolescent varieties [2–4]. It is essentially a multi-planar deformity that leads to progressive varus and rotational malalignment of the proximal tibia, with the distal femur involved to a certain extent as well [5–8]. Mild cases may resolve, but in some untreated cases, the deformity may rapidly progress, leading to functional impairment, with early development of arthritis [9–11].
Management includes the restoration of limb alignment, joint congruency, limb length equalization, and careful follow-up to prevent recurrence, which can occur in up to 50% of patients [12–14]. Various surgical techniques, including osteotomies, can help to restore alignment of the leg. Reports include the use of circular Ilizarov external fixation [15–21], non-circular external fixation [22, 23], internal fixation [11, 24], hemiplateau elevation with/without epiphyseal distraction [25, 26], double elevating osteotomies [27], serrated W/M osteotomies [28], epiphyseal stapling [29], Taylor Spatial Frame correction [30], and hemiepiphysiodesis by guided growth [31]. All of these techniques vary in their ease of application/performance, achievement of (and time to) deformity correction (both clinically and radiographically), prevention of recurrence, and complications (i.e., nerve damage, infection, non-union, mal-union) [12, 14, 16, 17, 22–26, 28, 29, 32, 33].
The use of the Ilizarov circular fixator in combination with tibial osteotomy has been widely used for the correction of Blount’s disease [15–21]. Advantages of this method include early weight-bearing, early motion, and, most importantly, multi-planar deformity correction (including rotation, angulation, and translation) [17, 18]. Yet, the learning curve for circular fixator application can be very steep for clinicians, the total treatment time and rings may be cumbersome to patients, and there is, potentially, a high risk of complications. The Multi-Axial Correction (MAC) monolateral fixation system (Biomet, Parsippany, NJ, USA) was designed to overcome these issues. The MAC system achieves gradual or acute correction of single or multi-planar deformities, and can address angulational, translational, rotational, and length discrepancy issues in three planes.
At our institution, patients with Blount’s disease who required surgical correction were traditionally treated with osteotomies of the tibia and fibula with application of an Ilizarov circular fixator. With the introduction and evolution of the MAC system, the technique of external fixation was changed. The purpose of this study was to determine the efficacy of the MAC system for the treatment of pediatric patients with Blount’s disease in regard to the correction of deformity, operative time, complications (intra-operative and post-operative), and treatment duration. We hypothesized that the MAC system would be able to correct the deformities associated with Blount’s disease, as measured by radiographic indices, with minimal complications.
Materials and methods
After obtaining institutional review board (IRB) approval, the surgical database of the senior authors at two institutions between 2003 and 2007 was reviewed to identify patients with surgically corrected Blount’s disease using the MAC system. This was a retrospective review. All patients were operated on by one of the two pediatric orthopedic fellowship-trained senior authors at their respective institutions, and were consecutive patients for each surgeon. Office charts and radiographs were reviewed.
Data parameters were standardized. All patients were clinically and radiographically followed. Patients were included in the study if the Blount’s disease was determined (by one of the senior surgeons) to be the sole cause of the patient’s deformity using radiographic criteria previously described for diagnosis [4]. All patients were treated with the MAC system, had unilateral or bilateral disease, were <20 years old at the time of surgery, and had adequate clinical and radiographic data in the chart review. Exclusion criteria included patients who had other etiologies as a cause of their varus deformity, other congenital/developmental/metabolic anomalies affecting the growth of the affected extremity, prior operations on the affected extremity, and prior trauma (i.e., fracture) to the affected extremity. In addition, patients who were receiving operative treatment for relapsed/recurrent Blount’s disease were also excluded.
Data collected included patient gender, unilateral/bilateral nature of disease, age at disease onset, age at time of operation, age at time of fixator removal, and age at final follow-up. The total procedure time was noted, as were any intra-operative/post-operative complications (defined as neurovascular deficit/injury, compartment syndrome, infection requiring antibiotics, over-correction of the deformity into severe valgus, under-correction with residual varus/recurrence, delayed union of the osteotomy, non-union of the osteotomy, and/or notable/clinically relevant leg length discrepancy).
Radiographs for each patient were performed at the time of pre-operative assessment, after fixator removal, and at final follow-up. All patients had a full-length weight-bearing anteroposterior (with both patella facing forward) views of both lower extremities. With these deformities being multi-planar, it is not always possible to obtain a lateral radiograph of the femur and proximal tibia in the same view and, additionally, the presence of an external fixator makes this cumbersome. Lateral radiographic views were, therefore, not routinely ordered by the senior surgeons. A small subset of the patients had adequate lateral radiographs and data from those were included in this review. Deformity was assessed based on principles outlined by Paley et al. [34, 35]. Patients had frontal plane analyses consisting of mechanical axis deviation (MAD), tibial–femoral angle (TFA), medial proximal tibial angle (MPTA), and posterior proximal tibial angle (PPTA) measured.
All patients with bilateral disease had each lower limb analyzed individually. The total number of days from the placement of the fixator to its removal and the total number of days from placement of the fixator to final follow-up were calculated. The mean change in MAD, TFA, MPTA, and PPTA between the pre-operative measurements and the time at which the fixator was taken off, as well as at the final follow-up visit, was calculated. Paired two-tailed Student’s t-tests were used to compare the mean change in the aforementioned radiographic parameters between the pre-operative measurements and the two other time points: fixator removal and final follow-up visit.
Statistical significance was defined as P < 0.05 and 95% confidence intervals were calculated. For patients whose radiographic measurements could not be calculated due to the availability or quality of the images, the patient was excluded only from the analysis related to that measurement at that specific time point (pre-operative, fixator removal, or final follow-up) analyzed in the study.
Based upon our power analysis (for a power of 0.08 and an alpha value of 0.05), utilizing a correction of 10° in the MPTA for the MAC system from pre-operative to fixator removal (utilizing a standard deviation of 15° in both groups), data for three patients was necessary, which we exceeded.
MAC system operative technique
The MAC system is a multi-axial correcting monolateral external fixation system (Figs. 1 and 2) with a central component consisting of two hinges and two translators at 90° to each other. The primary hinge (marked on the device) is capable of 80° of correction, while the secondary hinge is capable of 35–45° of correction, depending on the position of the primary hinge. The two translating screws are capable of 3 cm of correction at 90° to each other. As a component system, rings, arcs, rotating arcs, or linear compression/distraction devices can be attached to the MAC system, depending on its location on the extremities.
Fig. 1.

Multi-axial rotation ring used in the Multi-Axial Correction (MAC) system
Fig. 2.
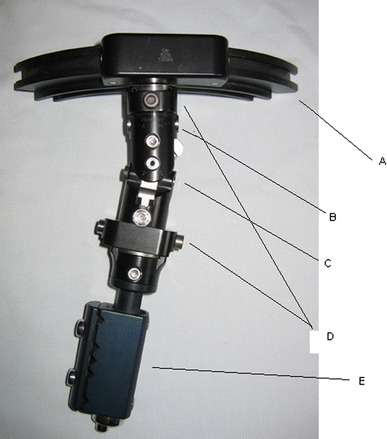
MAC system with multiple labeled components. A Multi-axial rotation ring (also shown in Fig. 1). B Primary hinge (80° of correction). C Secondary hinge (35°–45° of correction). D Translation component in two separate planes (3 cm of correction each). E Lengthening component
For the correction of the tibia vara deformity in this series, the primary hinge was centered on the center of rotation of angulation (CORA), and was also angulated to match the tibial (Blount’s) deformity. A rotational arc capable of at least 80° of rotational correction was attached to the MAC device proximally and lined up with the proximal tibial joint line. A compression/distraction clamp (capable of 5 cm of lengthening) was applied to the MAC device distally and lined up with the tibial diaphysis. This construct of the MAC system was lined up with the tibial deformity and centered on the CORA. Two to three bicortical hydroxyapatite-coated cortical screws were placed proximally (one medial to the MAC and one laterally, so as not to block lateral rotation of the distal tibia). These screws do not have to be perpendicular to the tibia. If the arc is proximal to the metaphysis, these screws can be angulated to fit between the physis and the planned osteotomy. Three distal screws are then inserted into the medial face of the tibia. The MAC device allows medial translation and rotation to align the distal component with the medial face of the tibia.
The tibial osteotomy is then placed distally to the CORA, which is usually positioned between the physis and the insertion of the patellar tendon to avoid damage to the physis and distal displacement of the patella during lengthening. A local zig-zag displacement is, therefore, a desired effect of angular correction with the hinge at the CORA but the osteotomy distal to the CORA. This restores the mechanical axis. A Gigli saw is used to make the tibial osteotomy. A fibular osteotomy is then performed at the middle or distal thirds of the fibula, with care not to injure the sensory branch of the peroneal nerve. A power saw is used to remove an angled cylindrical shape of bone (Figs. 3–7). Anterior and lateral subcutaneous fasciotomies are then performed through the incisions for the osteotomies of the tibia and fibula, respectively.
Fig. 4.

Anteroposterior and lateral pre-operative X-rays of a patient with Blount’s disease prior to deformity correction
Fig. 5.
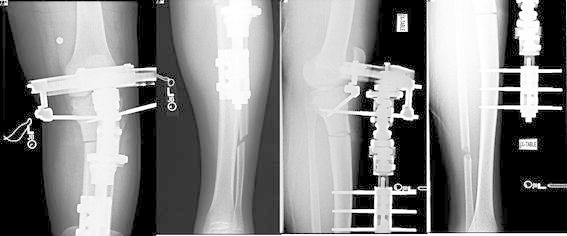
Anteroposterior and lateral post-operative X-rays of the same patient with Blount’s disease (from Fig. 4) after placement of the MAC system after deformity correction
Fig. 6.

Anteroposterior and lateral post-operative X-rays of the same patient with Blount’s disease (from Fig. 4) after removal of the MAC system
Fig. 3.

MAC system with tibial osteotomy performed on sawbones
Fig. 7.

Anterior view of the patient with the MAC system placed for Blount’s disease
No corrections are performed acutely, avoiding peroneal nerve stretch injury. In the first post-operative week, the patients are taught how to do range of motion exercises for the hip, knee, and ankle on the operated side, and to walk on crutches at 10 lb partial weight-bearing. During the second week, the patients are taught to turn the compression/distraction mechanism 90° four times a day (1 mm per day) in the direction of the marked arrow for distraction of the osteotomized tibial bone ends for 7 days or about 7 mm. Additional lengthening at a rate of 1 mm per day is accomplished, depending on what was needed based on pre-operative planning. While most patients require lengthening, any over-correction is eliminated after realignment by compressing at a rate of about 1 mm per day. At the beginning of the third week or after lengthening has been accomplished, angular correction is begun at a rate of 1° four times a day (turning the primary angulation screw 90° four times a day) until realignment has been achieved.
After lengthening and biplanar angular deformities are corrected, rotation (at 2° or a 90° turn of the key four times per day), translation, and any residual angular deformities are corrected. Weekly X-rays are obtained until the deformities are corrected, usually in 2–3 weeks. Then, monthly X-rays are obtained until consolidation. The device is removed after radiographic evidence of consolidation. Weight-bearing is increased as tolerated to full weight-bearing once consolidation is observed. Sports are not permitted until at least 6 weeks after removal of the fixator. Contact sports are not permitted for 6 months. Local zig-zag deformity should be seen on the X-ray, confirming proper axial alignment.
Results
Seventeen patients (age 10.7 ± 2.7 years) with Blount’s tibia vara were treated with the MAC system. Sixteen of the patients had unilateral disease, while one patient had bilateral disease. The full demographic data are displayed in Table 1. The total time that the fixator was on the patients prior to removal was 130.6 days (standard deviation [SD] = 44.8). The mean operative time was 120.6 min (SD = 21.2). The most common complication noted post-operatively was pin site infections and/or cellulitis requiring antibiotics (Table 2).
Table 1.
Demographic data
| Variable | MAC |
|---|---|
| Number of patients | 17 |
| Number of limbs | 18 |
| Male:female | 10:7 |
| Blount’s classification (early-onset:late-onset) | 9:8 |
| Age in years at time of operation | 10.7 (2.7) |
| Total follow-up time in days | 625.3 (325.0) |
Standard deviation (SD) in parentheses
Table 2.
Percentage of surgical complications
| Complication | Percentage |
|---|---|
| Any complication per limb | 70.5 (12) |
| Pin tract infection and/or cellulitis requiring antibiotics | 50.0 (9) |
| Over-correction or under-correction or recurrence of deformity | 17.6 (3) |
| Delayed union/non-union | 0 (0) |
| Nerve palsy | 0 (0) |
| Leg length discrepancy | 0 (0) |
| Compartment syndrome | 0 (0) |
Raw number in parentheses
The mean values for the radiographic parameters measured (MAD, TFA, MPTA, and PPTA) are shown in Table 3. The MAC system was able to correct the Blount’s deformity as measured by a decrease in the MAD (P ≤ 0.001) and TFA (from varus; P ≤ 0.001), as well as an increase in the MPTA (P = 0.001) at the time of fixator removal (Table 4). The correction was still maintained at the time of final follow-up (Table 4). The MAC system did not change the PPTA at both the time when the fixator was taken off (P = 0.24) and at the final follow-up (P = 0.56).
Table 3.
Multi-Axial Correction (MAC) system radiographic data for mechanical axis deviation (MAD), tibial–femoral angle (TFA), medial proximal tibial angle (MPTA), and posterior proximal tibial angle (PPTA) measured at pre-operative, fixator removal, and final follow-up visits
| Parameter | Pre-operative | Fixator removal | Final follow-up |
|---|---|---|---|
| Mechanical axis deviation (mm) | 75.5a (29.2); 95% CI (60.98–90.02) | 31.8a (19.1); 95% CI (20.3–43.3) | 20.5a (12.7); 95% CI (7.2–33.8) |
| Tibial–femoral angle (degree) | 21.2b (8.3); 95% CI (17.1–25.3) | 5.9b (10.7); 95% CI (0.36–11.4) | 8.0b (4.1); 95% CI (4.2–11.8) |
| Medial proximal tibial angle (degree) | 68.8 (13.5); 95% CI (62.1–75.5) | 83.8 (11.8); 95% CI (77.3–90.3) | 83.7 (8.1); 95% CI (75.2–92.2) |
| Posterior proximal tibial angle (degree) | 78.6 (8.0); 95% CI (72.4–84.7) | 71.8 (8.8); 95% CI (65.5–78.0) | 72.3 (3.9); 95% CI (66.0–78.5) |
SD in parentheses
aMedial
bVarus
Table 4.
Correction of Blount’s disease achieved by the MAC system radiographically (MAD, TFA, MPTA, and PPTA)
| Radiographic parameter | Mean change (pre-operative to fixator removal) | P value | Mean change (pre-operative to final follow-up) | P value |
|---|---|---|---|---|
| Mechanical axis deviation (mm) | −40.2 (29.3); 95% CI (−22.5 to −58.0) | ≤0.001* | −54.3 (30.7); 95% CI (−22.1 to −86.6) | 0.025* |
| Tibial–femoral angle (degree) | 15.9a (13.7); 95% CI (9.1–22.7) | ≤0.001* | 13.8a (9.6); 95% CI (3.7–23.9) | 0.01* |
| Medial proximal tibial angle (degree) | 15.7 (14.6); 95% CI (8.0–23.4) | 0.001* | 19.8 (12.6); 95% CI (6.6–33.0) | 0.01* |
| Posterior proximal tibial angle (degree) | −6.7 (14.8); 95% CI (−19.0 to 5.7) | 0.24 | −3.7 (18.0); 95% CI (−48.4 to 41.1) | 0.56 |
SD in parentheses
* Statistically significant
aDecrease in varus angulation
Discussion
The circular external fixation system was initially described by Ilizarov in 1951 as a novel modality of external fixation with a circular frame that would help control angulation, rotation, translation, and axial motion (distraction/compression) in a triplane fashion [36]. The MAC system was developed as a possible alternative to the Ilizarov circular fixator. The surgical treatment of Blount’s disease has centered around the use of tibial osteotomies with varying forms of internal or external fixation [11, 14–29]. Due to the fact that the two institutions involved in this study are large referral centers for Blount’s disease, we felt that choosing to analyze this deformity (with its combination of angulation, rotation, and medial column shortening) would be the ideal manner to analyze the MAC system [5–8]. In support of our hypothesis, we found that the MAC system was able to correct the radiographic deformities of Blount’s disease with minimal complication.
Paley et al. have outlined the radiographic measurements for the evaluation of Blount’s disease [34, 35]. A decrease in the MAD and TFA with concurrent increases in MPTA and PPTA are indicative of correction. We recognize that, with nearly all external fixators, anatomic alignment can be achieved. In order to compare the results of the MAC (in a quantifiable and reproducible manner) to that of other fixators in the literature, we have included the multiple measurements to aid in comparison. Prior studies have attempted to outline the following range of values as suggestive of Blount’s disease: MAD (70–108 mm medial), TFA (19–28° of varus), MPTA (68–75°), and PPTA (64–71°) [5, 8, 17, 20, 37]. Normal values for these measurements are as follows: MAD (10.0 mm medial; range 3–17 mm), TFA (1.3° of varus; range 1° of valgus to 4° of varus), MPTA (87°; range 85–89°), and PPTA (80°; range 77–84°) [5, 15, 34, 35, 37].
The pre-operative values for the patients in the MAC group in our series were consistent with the range of Blount’s measurements previously cited in the literature [5, 8, 15, 17, 20, 37], with a mean MAD of 75.5 mm, TFA of 21.2° varus, and MPTA of 68.8°. Furthermore, the MAC system was able to achieve the goals of radiographic Blount deformity correction by achieving statistically significant decreases in MAD and TFA (decreased varus), as well as an increase in MPTA. The PPTA did not significantly change after treatment, and can be likely explained by the fact that the pre-operative PPTA in our patient population (78.6°) was much closer to what has been cited as a normal value (81°) after correction [35]. Further study with a larger number of patients may also allow for a determination of the MAC device’s effect on the PPTA.
Critically speaking, the radiographic changes achieved by the MAC system would be of little clinical significance if the absolute change produced in these parameters did not lead to values considered as normal. In our series, the MAC system did achieve a large absolute amount of deformity correction (40.2 mm decrease in MAD, 15.9° varus decrease in TFA, 15.7° increase in MPTA) such that the post-operative values approached those considered as normal [5, 34, 35]. Given the preceding data, the question naturally arises: How does the MAC system compare to other methods of Blount’s correction, particularly the Ilizarov circular frame?
Utilizing the Ilizarov fixator as the ‘gold standard’ in the treatment of Blount’s disease [15–21], there have been several studies that have investigated correction using this method. This allows for a comparison between the results obtained with the MAC system and those of the Ilizarov fixator in terms of radiographic correction, wear time, operative time, and complications. First, looking at radiographic correction, Gordon et al. examined 15 patients with late-onset tibia vara who were corrected using tibial osteotomy and an Ilizarov circular fixator [15]. Their pre-operative MAD (108 mm) was more severe than our patient population, yet, their pre-operative MPTA (71°) was similar to the pre-operative MPTA (68.8°) in our patient population. Their method was able to achieve a mean decrease of 107 mm in the MAD and a 17° increase in the MPTA (mean 88.0°). This is similar to the correction achieved by the MAC system in our series at final follow-up with a 54.3-mm decrease in the MAD (mean 20.5 mm) and 19.8° increase in the MPTA (mean 83.7°). Therefore, the Ilizarov fixator improved the MAD slightly better than the MAC system, whereas the MAC system improved the MPTA slightly more than the Ilizarov fixator.
Second, the total time that the fixator was on prior to removal can be compared between the Ilizarov fixator and the MAC system. In Gordon et al.’s study, the mean fixator wear time was approximately 150 days, which is approximately 20 days longer than the wear time in our study (130.6 days). This may be related to the differing speeds with which an efficacious result can be obtained between the two fixators due to fixator design or could possibly be related to differing rates of correction, post-operative protocols, and/or specific osteotomies. Yet, examining the work of Gordon et al. in the context of the results of our study, it can be postulated that the MAC system achieves results similar to that of the traditional Ilizarov circular fixator in terms of deformity correction of Blount’s disease with less mean wear time, the clinical significance of which is largely based on the clinical application of the fixator (i.e., specific osteotomies utilized and post-operative protocols) and the specific patient and his/her surgeon.
Third, the mean operative time can be compared between the two fixators. Coogan et al. retrospectively reviewed their treatment of eight patients (12 limbs) with adolescent tibia vara with distraction osteogenesis by using an Ilizarov circular external fixation device [21]. Their average operative time was noted to be 180 min. In Stanitski et al.’s series, their mean operative time was 150 min [20]. Both of these series of patients treated with the Ilizarov fixator had higher mean operative times than the 120.6 min of operative time for the MAC system. As with the mean wear time, the decreased operative time of the MAC system may be due to the ease with which the MAC system can be applied in a unilateral (non-circular) nature compared to the technically demanding Ilizarov application. Yet, this time difference may not be fully attributable to the above fact, as differing osteotomies and surgeon experience may account for some of the variations in operative time. Yet, it can be postulated that the unilateral (non-circular) nature in which the MAC system can be applied decreases the operative time of the procedure.
Finally, post-operative complications between the two fixators can be compared. Stanitski et al. examined 17 patients who underwent correction of Blount’s disease with an Ilizarov circular fixator [20]. The incidence of complications was slightly higher in the series of Stanitski et al. compared to those of the MAC system with eight patients with pin tract infections; one delayed union, one premature consolidation, and two limb length discrepancies. This is in line with other studies which have shown the Ilizarov technique to be susceptible to both major and minor complications. Velazquez et al. examined 40 patients who were treated with the Ilizarov technique for the correction of various limb deformities [38]. They had a total of 88 complications, with 38 defined as major (a complication that required an additional operative procedure or caused lasting sequelae, such as mal-union, bone deformation, joint contracture, nerve palsy, etc.) and 50 defined as minor (a complication that required non-operative treatment such as pin tract infection or paresthesias). Even with increasing surgeon experience, the rate of minor complications was not found to decrease in their study group. As a result, we believe that the MAC system may be applied with less risk of operative complications with theoretically equivocal radiographic correction, less mean wear time, and less operative time than the Ilizarov fixator.
There are several limitations in this study. First, our study was retrospective in nature, with no control group. A prospective trial in which patients with Blount’s disease are randomly assigned to either the MAC system or another form of fixation (i.e., Ilizarov frame) would have been ideal. Second, due to the retrospective nature of the study, complete anteroposterior and lateral radiographs of the patients at the three time points examined in the study were not available at all time points for all patients. Although full radiographic analysis was not available, the parameter which was more fully examined (MPTA) can be considered as one of the key radiographic parameters in Blount deformity analysis and is utilized in most studies examining Blount’s disease [5, 8, 14, 15, 22, 34, 35, 37]. Another limitation of our study is that we did not assess the femoral involvement of Blount’s disease (i.e., lateral distal femoral angle). We do agree that this is necessary in future studies to not only better understand the disease, but determine if primary correction in the tibia can affect secondary changes in the femur. This can help us better understand the etiology of the femoral deformity in Blount’s disease as either primary or secondary. Furthermore, limitations due to the retrospective nature of our study include the lack of measurements in regards to rotation correction, leg length discrepancy/lengthening, knee stability, knee range of motion, and gait. Further prospectively designed studies which attempt to seek this information from the onset of study initiation will be able to provide insight into these values. Finally, an assessment of the clinical outcomes of these patients (function, patient satisfaction, etc.) was not performed. This was difficult since our patients have a wide referral base and there is a reasonable reluctance for individuals who live a great distance (out of state and/or country) and are now fully corrected and asymptomatic to come back for follow-up.
In conclusion, the results of our study indicate that the MAC system is able to achieve correction of Blount’s deformity, as measured radiographically, with minimal complications. These results should be considered as preliminary, as the follow-up is in the 1- to 2-year time period. The MAC system can be considered to be comparable to the traditional circular external fixator (Ilizarov frame) in its ability to correct the multiple deformity components of Blount’s disease, as measured by radiographic indices, with perhaps less wear time and less risk of major complications. Deformity correction, particularly in Blount’s disease, can be achieved in multiple, different fashions. Clinicians should utilize whatever technique they are most comfortable with and which they believe they can achieve the most reliable and reproducible deformity correction with minimal complications. The MAC system is another option that the surgeon has at their disposal for deformity correction. For individuals not familiar with circular frame application or those currently in training, the ease of application (as measured by decreased operative time and relative familiarity with similar external fixation techniques utilized in trauma) of the MAC system makes it an excellent choice for the surgical correction of Blount’s disease.
Acknowledgment
We would like to thank Richard S. Davidson, M.D., for providing the description of the surgical technique in this paper.
References
- 1.Blount WP. Tibia vara osteochondritis deformans tibiae. J Bone Joint Surg. 1937;19:1–29. [Google Scholar]
- 2.Thompson GH, Carter JR. Late-onset tibia vara (Blount’s disease). Current concepts. Clin Orthop Relat Res. 1990;255:24–35. [PubMed] [Google Scholar]
- 3.Langenskiöld A. Tibia vara. A critical review. Clin Orthop Relat Res. 1989;246:195–207. [PubMed] [Google Scholar]
- 4.Langenskiöld A, Riska EB. Tibia vara (osteochondrosis deformans tibiae): a survey of seventy-one cases. J Bone Joint Surg Am. 1964;46:1405–1420. [PubMed] [Google Scholar]
- 5.Sabharwal S, Lee J, Jr, Zhao C. Multiplanar deformity analysis of untreated Blount disease. J Pediatr Orthop. 2007;27:260–265. doi: 10.1097/BPO.0b013e31803433c3. [DOI] [PubMed] [Google Scholar]
- 6.Hosalkar HS, Jones S, Hartley J, et al. Three-dimensional tomography of relapsed infantile Blount’s disease. Clin Orthop Relat Res. 2005;431:176–180. doi: 10.1097/01.blo.0000150463.79616.48. [DOI] [PubMed] [Google Scholar]
- 7.Kline SC, Bostrum M, Griffin PP. Femoral varus: an important component in late-onset Blount’s disease. J Pediatr Orthop. 1992;12:197–206. doi: 10.1097/01241398-199203000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Myers TG, Fishman MK, McCarthy JJ, et al. Incidence of distal femoral and distal tibial deformities in infantile and adolescent Blount disease. J Pediatr Orthop. 2005;25:215–218. doi: 10.1097/01.bpo.0000149858.04659.d8. [DOI] [PubMed] [Google Scholar]
- 9.Ingvarsson T, Hägglund G, Ramgren B, et al. Long-term results after adolescent Blount’s disease. J Pediatr Orthop B. 1997;6:153–156. doi: 10.1097/01202412-199704000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Ingvarsson T, Hägglund G, Ramgren B, et al. Long-term results after infantile Blount’s disease. J Pediatr Orthop B. 1998;7:226–229. doi: 10.1097/01202412-199807000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Schoenecker PL, Meade WC, Pierron RL, et al. Blount’s disease: a retrospective review and recommendations for treatment. J Pediatr Orthop. 1985;5:181–186. doi: 10.1097/01241398-198505020-00012. [DOI] [PubMed] [Google Scholar]
- 12.Accadbled F, Laville JM, Harper L. One-step treatment for evolved Blount’s disease: four cases and review of the literature. J Pediatr Orthop. 2003;23:747–752. doi: 10.1097/01241398-200311000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Loder RT, Johnston CE., 2nd Infantile tibia vara. J Pediatr Orthop. 1987;7:639–646. doi: 10.1097/01241398-198707060-00002. [DOI] [PubMed] [Google Scholar]
- 14.Jones S, Hosalkar HS, Hill RA, et al. Relapsed infantile Blount’s disease treated by hemiplateau elevation using the Ilizarov frame. J Bone Joint Surg Br. 2003;85:565–571. doi: 10.1302/0301-620X.85B4.13602. [DOI] [PubMed] [Google Scholar]
- 15.Gordon JE, Heidenreich FP, Carpenter CJ, et al. Comprehensive treatment of late-onset tibia vara. J Bone Joint Surg Am. 2005;87:1561–1570. doi: 10.2106/JBJS.02276. [DOI] [PubMed] [Google Scholar]
- 16.Rajacich N, Bell DF, Armstrong PF. Pediatric applications of the Ilizarov method. Clin Orthop Relat Res. 1992;280:72–80. [PubMed] [Google Scholar]
- 17.Alekberov C, Shevtsov VI, Karatosun V, et al. Treatment of tibia vara by the Ilizarov method. Clin Orthop Relat Res. 2003;409:199–208. doi: 10.1097/01.blo.0000052937.71325.a2. [DOI] [PubMed] [Google Scholar]
- 18.Hefny H, Shalaby H, El-Kawy S, et al. A new double elevating osteotomy in management of severe neglected infantile tibia vara using the Ilizarov technique. J Pediatr Orthop. 2006;26:233–237. doi: 10.1097/01.bpo.0000218530.59233.ab. [DOI] [PubMed] [Google Scholar]
- 19.Laville JM, Chau E, Willemen L, et al. Blount’s disease: classification and treatment. J Pediatr Orthop B. 1999;8:19–25. [PubMed] [Google Scholar]
- 20.Stanitski DF, Dahl M, Louie K, et al. Management of late-onset tibia vara in the obese patient by using circular external fixation. J Pediatr Orthop. 1997;17:691–694. doi: 10.1097/01241398-199709000-00021. [DOI] [PubMed] [Google Scholar]
- 21.Coogan PG, Fox JA, Fitch RD. Treatment of adolescent Blount disease with the circular external fixation device and distraction osteogenesis. J Pediatr Orthop. 1996;16:450–454. doi: 10.1097/01241398-199607000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Wilson NA, Scherl SA, Cramer KE. Complications of high tibial osteotomy with external fixation in adolescent Blount’s disease. Orthopedics. 2007;30:848–852. doi: 10.3928/01477447-20071001-04. [DOI] [PubMed] [Google Scholar]
- 23.Price CT, Scott DS, Greenberg DA. Dynamic axial external fixation in the surgical treatment of tibia vara. J Pediatr Orthop. 1995;15:236–243. doi: 10.1097/01241398-199503000-00021. [DOI] [PubMed] [Google Scholar]
- 24.Laurencin CT, Ferriter PJ, Millis MB. Oblique proximal tibial osteotomy for the correction of tibia vara in the young. Clin Orthop Relat Res. 1996;327:218–224. doi: 10.1097/00003086-199606000-00027. [DOI] [PubMed] [Google Scholar]
- 25.Storen H. Operative elevation of the medial tibial joint surface in Blount’s disease. One case observed for 18 years after operation. Acta Orthop Scand. 1969;40:788–796. doi: 10.3109/17453676908989543. [DOI] [PubMed] [Google Scholar]
- 26.Janoyer M, Jabbari H, Rouvillain JL, et al. Infantile Blount’s disease treated by hemiplateau elevation and epiphyseal distraction using a specific external fixator: preliminary report. J Pediatr Orthop B. 2007;16:273–280. doi: 10.1097/01.bpb.0000210591.35652.84. [DOI] [PubMed] [Google Scholar]
- 27.van Huyssteen AL, Hastings CJ, Olesak M, et al. Double-elevating osteotomy for late-presenting infantile Blount’s disease: the importance of concomitant lateral epiphysiodesis. J Bone Joint Surg Br. 2005;87:710–715. doi: 10.1302/0301-620X.87B5.15473. [DOI] [PubMed] [Google Scholar]
- 28.Hayek S, Segev E, Ezra E, et al. Serrated W/M osteotomy. Results using a new technique for the correction of infantile tibia vara. J Bone Joint Surg Br. 2000;82:1026–1029. doi: 10.1302/0301-620X.82B7.10507. [DOI] [PubMed] [Google Scholar]
- 29.Bardier M, Senie JN, Fabre J, et al. Temporary epiphyseal stapling of the lower limbs in children suffering from Blount’s disease. An experimental study based on a hundred and sixty cases. Ann Chir. 1982;36:396–401. [PubMed] [Google Scholar]
- 30.Feldman DS, Madan SS, Koval KJ, et al. Correction of tibia vara with six-axis deformity analysis and the Taylor Spatial Frame. J Pediatr Orthop. 2003;23:387–391. [PubMed] [Google Scholar]
- 31.Stevens PM. Guided growth for angular correction: a preliminary series using a tension band plate. J Pediatr Orthop. 2007;27:253–259. doi: 10.1097/BPO.0b013e31803433a1. [DOI] [PubMed] [Google Scholar]
- 32.Stanitski DF, Srivastava P, Stanitski CL. Correction of proximal tibial deformities in adolescents with the T-Garches external fixator. J Pediatr Orthop. 1998;18:512–517. [PubMed] [Google Scholar]
- 33.Zayer M. Hemicondylar tibial osteotomy in Blount’s disease. A report of 2 cases. Acta Orthop Scand. 1992;63:350–352. doi: 10.3109/17453679209154801. [DOI] [PubMed] [Google Scholar]
- 34.Paley D. Principles of deformity correction. 1. New York: Springer; 2002. [Google Scholar]
- 35.Paley D, Herzenberg JE, Tetsworth K, et al. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am. 1994;25:425–465. [PubMed] [Google Scholar]
- 36.Paul GW. The history of external fixation. Clin Podiatr Med Surg. 2003;20:1–8. doi: 10.1016/S0891-8422(02)00050-2. [DOI] [PubMed] [Google Scholar]
- 37.Gordon JE, King DJ, Luhmann SJ, et al. Femoral deformity in tibia vara. J Bone Joint Surg Am. 2006;88:380–386. doi: 10.2106/JBJS.C.01518. [DOI] [PubMed] [Google Scholar]
- 38.Velazquez RJ, Bell DF, Armstrong PF, et al. Complications of use of the Ilizarov technique in the correction of limb deformities in children. J Bone Joint Surg Am. 1993;75:1148–1156. doi: 10.2106/00004623-199308000-00004. [DOI] [PubMed] [Google Scholar]


