Abstract
Purpose
In this retrospective study we compared the efficacy of ultrasound and radiography for determining the position of the femoral head after closed or open reduction in DDH.
Materials and methods
The ultrasound was performed using the van Douveren technique by a transinguinal approach through a perineal window of the spica cast. Sixty-eight a.p. radiographs of the pelvis were correlated to 68 ultrasound images.
Results
Thirty-two radiographs were not useful for precisely determining the femoral head position, whereas the criteria described by van Douveren et al. could be identified in all ultrasound images. All ultrasound images in the study were useful and gave reliable information about the position of the femoral head.
Conclusion
Consequently, standard radiographic documentation is no longer used as a standard in our clinic. MRI and CT are reserved for special cases. We recommend transinguinal ultrasound as a standard diagnostic method to determine the position of the femoral head in hip spica casts safely and reliably.
Keywords: DDH, Ultrasound, Hip reduction, Hip dislocation, Spica cast treatment
Introduction
Developmental dysplasia of the hip is very common in newborns. The incidence of DDH in Europe ranges from 1 to 5% [1]. Higher incidences are reported in countries with ultrasound screening. In these countries, ultrasound evaluation of the infant hip and ultrasound classification of dysplasia led to the ultrasound diagnostic becoming the golden standard [2, 3]. To monitor treatment, particularly in cases with a hip spica cast, conventional radiographs, MRI and CT are still the recommended diagnostic procedures. In particular, CT is very widely used in English-speaking countries. Several methods have been described for determining the position of the femoral head after closed or open reduction; for instance, the determination of the position of the femoral head using Shenton’s line in CT [4]. CT results in a high radiation exposure. Therefore, others have recommended MRI as the imaging method of choice [5–8]. However, MRI is not immediately available in the operating room. X-ray is an acute diagnostic method in the operating room, but this method frequently fails to define the precise position of the reduced hip due to the transformation of a three-dimensional joint into a uniplanar image.
van Douveren et al. described a new ultrasound method in 2003 that was intended to reduce the radiation dose and to determine the position of the femoral head after the application of a spica cast more reliably [9] (Fig. 1). The purpose of this study was to compare the two diagnostic methods, radiography and ultrasound, with regard to accuracy during spica cast treatment.
Fig. 1.

Transinguinal ultrasound, landmarks: superior ramus of pubic bone, femoral head and femoral neck, acetabulum (left hip)
Materials and methods
DDH treatment is standardized according to Graf’s classification in our institution. Types IIb to IIc were treated by splinting using a Tübinger flexion brace; types D to IV were primarily treated with a Hoffmann–Daimler splint. If Hoffmann–Daimler splinting fails, a spica cast is applied in the human position. In this study, only cases with spica cast treatment are included.
Between 1 January 2004 and 30 July 2005, 25 patients with 33 affected hips were treated for DDH in a spica cast. According to Graf’s classification, there were 21 type IV, 8 type III, and 4 type D hips. Twenty-eight hips were treated by closed reduction under anesthesia, while five hips needed open reduction. Following reduction, the hips were immobilized in a spica cast with the legs in the human position. The casts were routinely changed every 4 weeks until the hip was stabilized at type IIc according to Graf’s classification [2]. Four attending surgeons were involved in the treatment. The treatment began as early as possible; the average was 6.5 weeks of age (ranging between 1 and 30 weeks of age). There were 23 girls and 2 boys. Six patients had previously undergone unsuccessful splinting treatment in another hospital.
Before 2003, reduction was controlled only by radiographs. In 2003 we introduced the transinguinal ultrasound method described by van Douveren et al. [9]. This ultrasound method is performed in the transverse plane with the superior ramus of the pubis, the acetabulum, the femoral head and the femoral neck all in one plane. Using transinguinal ultrasound, the reduction is complete when the pubic bone and the femoral neck lines are at the same level (Figs. 1, 4a, b). This means that the line drawn parallel to the pubic bone crosses the anteromedial aspect of the femoral metaphysis according to the modified Shenton’s line [4]. With the hip being dislocated, the femur lies behind the line of the pubic bone (Fig. 4c, d).
Fig. 4.
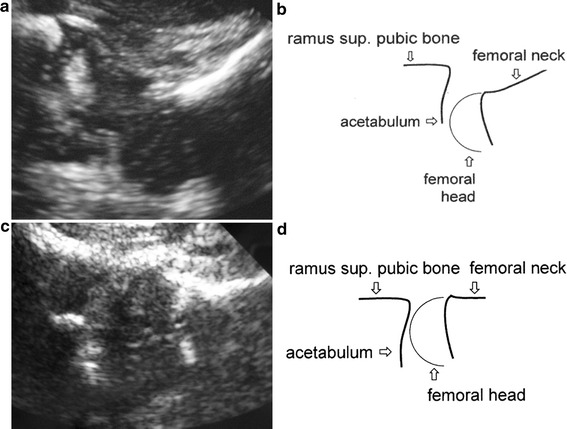
Ultrasound images (a,c) for dislocated (b) and reduced (d) hip (left hip)
In 2004 and 2005 both ultrasound and radiography were used at the same time to determine the position of the femoral head after reduction and application of the cast. The use of radiography and/or ultrasound depended on the preference of the attending surgeon.
An ultrasound examination was performed by the radiologist immediately after the completion of the cast in the operating room using a portable Sonosite “Titan” machine with a 8 MHz mini-convex probe (Figs. 2, 3). Radiographs were performed as standard a.p. views of the pelvis in the operating room by the radiologist.
Fig. 2.

Intraoperative positioning and ultrasound investigation; reduction maneuver under ultrasound evaluation
Fig. 3.

Positioning of the ultrasound probe through the perineal opening after spica cast application
In the cases in which both methods were utilized, both methods were compared.
The determination of the femoral head position on radiographs in children between three and 12 months old is indirect; lines and distances are used to evaluate the immature hip. Reference to the femoral head position in the immature hip on radiographs are symmetrical or asymmetrical aspects of distances and lines.
The radiographic evaluation in our study comprised the measurement of the distance between the end of the femur to the acetabulum and the end of the femur to the teardrop figure. The position of the femur in relation to the acetabulum was compared.
Ultrasound images were checked for the landmarks given by van Douveren, which are the superior ramus of the pubis, the femoral neck, and the femoral head. The image was usable if all landmarks could be identified.
Radiographs and ultrasound images were evaluated by the first author (orthopedic surgeon) and the third author (radiologist) of this study.
Results
Nineteen out of the 25 patients were treated for 12 weeks in a hip spica with subsequent abduction splinting. One patient needed 4 weeks, three patients 8 weeks, and two patients 16 weeks of spica cast treatment. The mean treatment time for the 25 patients was 5.5 months to develop into a Graf type I hip. In one case of open reduction, we had an avascular necrosis of the femoral head and redislocation. In one case, we had persistent dysplasia after treatment for 8 months. Using an abduction walking brace, the hip normalized after 6 months of further treatment.
In 68 casts, the surgeon applying the cast used X-ray and ultrasound. Thus, ultrasound images could be compared with radiographic images in 68 cases. The landmarks of the transinguinal ultrasound could be identified in all 68 examinations (Table 1). In two cases, the ultrasound images showed a dislocation of the hip after application of the cast (conservative treatment) and the modified Shenton’s line crossed the femoral neck. The radiographic image showed no dislocation, while the MRI confirmed the results of the ultrasound examination (Fig. 5a–c). In three cases, there was intracapsular soft tissue in the acetabulum shown by the ultrasound images.
Table 1.
Ultrasound evaluation after cast application
| Transinguinal ultrasound | Identification of all landmarks | Intracapsular soft tissue | Images with reduction | Images with dislocation |
|---|---|---|---|---|
| Ultrasound images | N = 68 | N = 3 | N = 66 | N = 2 |
Fig. 5.
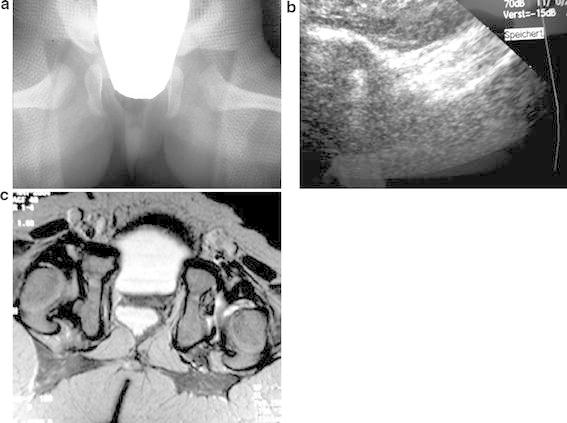
a Inaccurate asymmetric radiograph; exact determination of the femoral head position is not possible. Posterior dislocation is missed on the left side.b Ultrasound image with posterior dislocation of femoral head; line of the femoral neck is behind the pubic bone line.cMRI confirmed the posterior dislocation
Twenty-one X-rays out of 68 showed an asymmetrical pelvis. In these radiographs, there was a difference between the left and the right ileum, and a difference in the prominence of the left and the right spina ischiadica caused by asymmetrical positioning during the radiographic examination.
Twenty-nine X-rays showed differences between the right and left side upon measuring the distance of the end of femur to the acetabulum, and 19 X-rays showed differences upon measuring the distance of the end of femur to the teardrop figure.
The position of the neck of the femur in relation to the acetabulum was asymmetrical in twelve radiographs. These twelve images had a dubious relation of the neck of the femur to the triradiate cartilage which gave unreliable information concerning hip reduction.
Regarding all measurements, distances and lines used to indirectly determine the femoral head in the immature hip in our study, 32 of the X-rays were retrospectively found to be insufficient for exactly determining the femoral head position (Table 2).
Table 2.
Radiographic measurements with respect to symmetry/asymmetry of pelvis a.p. view radiographs
| Distances and lines for evaluating radiographs | Distance femur–acetabulum | Distance femur–teardrop figure | Relation femur neck–acetabulum |
|---|---|---|---|
| Symmetrical | N = 38 | N = 48 | N = 56 |
| Asymmetrical | N = 29 | N = 19 | N = 12 |
| Distances and lines for evaluating ultrasound images | Distance femur–acetabulum | Relation femur neck–pubic bone |
|---|---|---|
| Symmetrical | N = 65 | N = 66 |
| Asymmetrical | N = 3 | N = 2 |
In two cases we performed a MRI because radiographs showed a symmetrical aspect resulting in the interpretation of a reduced hip, whereas the ultrasound showed a posterior dislocation. The MRI confirmed the ultrasound findings.
The evaluations of the radiologist were the same as the ultrasound findings. Sixty-eight static ultrasound images showed the landmarks of femoral head, pubic bone and femoral neck. Sixty-five ultrasound evaluations were symmetrical. An asymmetrical situation was found on three occasions, a dislocation of the hip with intracapsular soft tissue twices, and intracapsular soft tissue without posterior dislocation once. The radiologist considered 35 of the X-rays to be insufficient to determine the position of the femoral head.
Discussion
Ultrasound is the gold standard in early diagnosis of DDH. CT, MRI and radiography used to be the diagnostic methods of choice for monitoring hip position after closed or open reduction and the application of a spica cast [1–4, 7, 10, 11].
During spica cast treatment, it is often difficult to determine whether a successful reduction has been achieved. The casting material can veil the bony structures, and radiographic imaging frequently fails to define the precise position of the reduced hip due to the transformation of the three-dimensional joint into a uniplanar image. These disadvantages of radiography necessitated the use of other diagnostic methods, such as MRI or CT. A CT scan gives an excellent image of the infant hip. Several anatomic landmarks and relations have been described for postreduction CT scans. The modified Shenton’s line is an accurate and safe measurement method for determining the femoral head position [4]. However, CT leads to a high radiation dose.
MRI, a diagnostic tool that does not necessitate exposure to radiation, gives an excellent overview of anatomical structures of infant hips [5, 12]. The accuracy with which it can determine hip reduction is clearly demonstrated in the literature [5, 8, 12, 13]. However, MRI is expensive and, like CT, not usually immediately available in the operating room. Further, logistical problems en route between the operation theater and MRI can prolong the anesthesia.
Ultrasound has been described as a method for monitoring hip position during harness treatment and a standard assessment for clarifying hip position in the spica cast [14]. Keller and Weiss [15] demonstrated the possibility of postreduction ultrasound after the application of a spica cast in a case report. Van Douveren et al. [9] developed an ultrasound method for the determination of the femoral head position during spica cast treatment (Figs. 1, 2, 3, 4). In a prospective study they evaluated the accuracy of the transinguinal ultrasound method in comparison with CT. In 16 cases they found that similar interpretations were obtained from both CT and ultrasound images. In both CT and ultrasound, reduction was determined according to the modified Shenton’s line. In our study we compared 68 radiographs to 68 transinguinal ultrasound images. Determination of reduction on ultrasound followed the criteria given by van Douveren et al. using the modified Shenton’s line [9]. The accuracy of the ultrasound technique was excellent. All images reliably showed the head of the femur and its position in relation to the acetabulum. In all ultrasound images, all of the landmarks—superior ramus of the pubis, acetabulum, femoral head, and femoral neck—could be identified. In contrast, nearly half of the radiographs were unsuitable. The femoral head position is determined only indirectly from radiographs of children between three and 12 months old, using lines and distances to evaluate the immature hip. Thirty-two radiographs yielded unreliable measurements concerning the indirect determination of the femoral head in the immature hip, and were retrospectively found to be inaccurate for the precise determination of hip reduction. A posterior dislocation was missed in the radiographs in two cases (Fig. 5). The ultrasound images clearly showed posterior dislocation. MRI gave the same results as the ultrasound images.
We performed the transinguinal ultrasound investigations with a mini-convex probe of 8 MHz. Using dual-mode imaging it is possible to compare the left and right sides for dislocation and reduction in unilateral or bilateral DDH cases. The results of reduction are immediately visible in the operating room using a portable system. This is an enormous advantage over MRI or CT. The transfer of the child under general anesthesia from the operating room to the radiological institute is not necessary. The reduction or dislocation is seen in the operating room immediately after the application of the cast, and the treatment can be adapted to the results of the transinguinal ultrasound.
An arthrogram is used in our clinic in selected cases only after failed conservative treatment. In the evaluated cohort, no arthrograms were needed to access the medialization of the hip. Before spica cast application, a lateral ultrasound view provides reliable information on reduction and medialization, and transinguinal ultrasound provides reliable information on the reduction or posterior dislocation.
This study showed that transinguinal ultrasound is better than radiographic imaging at determining the femoral head position after application of the spica cast. The limitation of the study lies in the study design, since it only involved retrospective analysis of the images. Both the orthopedic surgeon and radiologist were experienced in DDH treatment and ultrasound examination. The study gives no information on the intra-observer reliability of transiguinal ultrasound.
Nevertheless, this study underlines the efficacy of transinguinal ultrasound for determining the femoral head position after hip reduction. Ultrasound imaging is easy to use and can be rapidly performed in the operating room. The transinguinal ultrasound method uses the same landmarks as CT scans. The identifiable anatomic structures are the ramus superior os pubis, the femoral head, and the neck of the femur.
Conclusion
Transinguinal ultrasound is an excellent method for determining the femoral head position in a hip spica cast during treatment for DDH. It gives much better visualization of the head position than radiographic imaging. Unlike CT, no radiation exposure is necessary. Also, in contrast to MRI, portable ultrasound devices are rapidly accessible in the operating room. Consequently, standard radiographic documentation is no longer used as standard in our clinic. We recommend transinguinal ultrasound as a standard diagnostic method for the determination of the femoral head position in hip spica casts. In our institution, MRI and CT are reserved for special questions.
References
- 1.Graf R (2000) Sonographie der Säuglingshuefte und therapeutische Konsequenzen. Georg Thieme, Stuttgart
- 2.Graf R. Fundamentals of sonographic diagnosis in infant hip dysplasia. J Pediatr Orthop. 1984;4:735–740. doi: 10.1097/01241398-198411000-00015. [DOI] [PubMed] [Google Scholar]
- 3.Hensinger RN. The changing role of the ultrasound in the management of developmental dysplasia of the hip. J Pediatr Orthop. 1995;15:723–724. doi: 10.1097/01241398-199511000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Smith BG, Kasser JR, Hey L et al (1997) Postreduction tomography in developmental dislocation of the hip: part I: analysis of measurement reliability. J Pediatr Orthop 17:626–630 [DOI] [PubMed]
- 5.Bos CF, Bloem JL, Obermann WR et al (1988) Magnetic resonance imaging in congenital dislocation of the hip. J Bone Joint Surg 70:174–178 [DOI] [PubMed]
- 6.Bos CF, Bloem JL. Treatment of dislocation of the hip, detected in early childhood, based on magnetic resonance imaging. J Bone Joint Surg. 1989;71:1523–1529. [PubMed] [Google Scholar]
- 7.Mc Nally EG, Tasker A, Benson MK. MRI after reduction for developmental dysplasia of the hip. J Bone Joint Surg. 1997;7:724–726. doi: 10.1302/0301-620X.79B5.7772. [DOI] [PubMed] [Google Scholar]
- 8.Westhoff B, Wild A, Seller K et al (2003) Magnetic resonance imaging after reduction for congenital dislocation of the hip. Arch Orthop Trauma Surg 123:289–292 [DOI] [PubMed]
- 9.van Douveren F, Pruijs H, Sakkers R et al (2003) Ultrasound in the management of the position of the femoral head during spica cast after reduction of the hip dislocation in developmental dyslasia of the hip. J Bone Joint Surg 85-B:117–120 [DOI] [PubMed]
- 10.Mandel DM, Loder RT, Hensinger RN. The predictive value of computed tomograpy in the treatment of developmental dysplasia of the hip. J Pediatr Orthop. 1998;18:794–798. [PubMed] [Google Scholar]
- 11.Stanton RP, Capecci R. Computed tomography for the early evaluation of developmental dysplasia of the hip. J Pediatr Orthop. 1992;12:727–730. doi: 10.1097/01241398-199211000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Wirth T, Haake M, Hahn-Rinne R et al (1998) Magnetic resonance imaging in diagnostics and therapy control of patients with congenital dysplasia and dislocation of the hip. Z Orthop 136:210–214 [DOI] [PubMed]
- 13.Tennant S, Kinmont C, Lamb G et al (1999) The use of dynamic interventional MRI in developmental dysplasia of the hip. J Bone Joint Surg 81:392–397 [DOI] [PubMed]
- 14.Donaldson JS, Feinstein KA. Imaging of developmental dysplasia of the hip. Pedatr Clin North Am. 1997;44:591–614. doi: 10.1016/S0031-3955(05)70495-8. [DOI] [PubMed] [Google Scholar]
- 15.Keller MS, Weiss AA. Sonographic guidance for infant hip reduction under anaesthesia. Pediatr Radiol. 1988;18:174–175. doi: 10.1007/BF02387568. [DOI] [PubMed] [Google Scholar]


