Abstract
The Diabetes Prevention Program (DPP) and Look AHEAD (Action for Health in Diabetes) trials are long-term randomized clinical trials that have the potential to direct diabetes care and medical nutrition therapy for obesity, prediabetes and type 2 diabetes now and in the future. This paper summarizes and compares the important evidence-based results of these diabetes and obesity clinical trials and reviews the similarities and differences in the lifestyle interventions that were designed for these trials. Although there were many similarities in the features of the DPP and Look AHEAD interventions, the Look AHEAD lifestyle intervention was more ambitious in several ways: higher individual weight loss goals, lower calorie and fat gram targets based on initial body weight, more intensive intervention frequency, combining closed group and individual session format, and use of more structured nutrition intervention strategies from the outset including meal replacements, structured menus and combined fat and calorie counting. The evidence, knowledge and insights gained from working on these clinical trials will be very important in determining the strategies, methods and approaches needed to make sure that the results of these trials will be fully applied in real-world practice settings for obesity, prediabetes and type 2 diabetes.
Keywords: lifestyle intervention, prediabetes, type 2 diabetes, obesity
The Diabetes Prevention Program (DPP) and its followup, the Diabetes Prevention Program Outcomes Study (DPPOS), and Look AHEAD (Action for Health in Diabetes), are long-term randomized clinical trials that have potential to direct diabetes care and medical nutrition therapy for obesity, prediabetes and type 2 diabetes (T2DM) now and in the future. The DPP results have provided practitioners and third party insurers with strong evidence regarding the beneficial impact of lifestyle intervention on development of diabetes. DPPOS is determining how long lifestyle changes can be sustained with minimal follow-up and how long diabetes and its complications can be prevented/ delayed in an ethnically diverse group of overweight patients with prediabetes. The Look AHEAD trial, in overweight people with T2DM, is designed to compare effects of a lifestyle intervention aimed at weight loss, and modeled after the DPP program, with a standardized program of diabetes education and support on cardiovascular outcomes. Similar to the impact DPP/ DPPOS has had on diabetes prevention, the 12-year Look AHEAD trial will define the role of lifestyle intervention and medical nutrition therapy in management of T2DM.
This paper will: (1) summarize and compare the design, population characteristics, and available results of the primary prevention DPP/DPPOS and secondary intervention Look AHEAD clinical trials; (2) review similarities and differences in their lifestyle interventions; and (3) discuss implications for implementing lifestyle intervention programs for obesity, pre-diabetes, and T2DM in real-world practice settings.
CLINICAL CHARACTERISTICS OF DPP AND LOOK AHEAD
DPP was designed to determine whether a lifestyle intervention directed at reducing body mass and increasing activity levels, or the medication metformin, would delay or prevent development of diabetes in a high-risk population. (1) The study was planned between 1994 and 1996 and recruitment began in 1996. The ongoing Look AHEAD study, planned between 1999 and 2001 and launched in 2001 after successful completion of DPP, is employing a similar lifestyle intervention, but instead of primary prevention, is examining effects of lifestyle intervention on occurrence of cardiovascular disease in persons with T2DM. (2) The eligibility criteria and resultant baseline characteristics of DPP and Look AHEAD have been described.(1–4) Each study recruited a population that would satisfy its particular goals. DPP recruited subjects who were representative of the pre-diabetic population and at high-risk for developing diabetes by virtue of being overweight, having impaired glucose tolerance (IGT) and fasting glucose levels that were generally above the median for IGT .(1,3). (Table 1) In addition, DPP aimed to enroll a population enriched with minority racial-ethnic groups (African-American, Hispanic-American, Asian-American and Pacific Islander, and American Indian) that had been identified as being at particularly high-risk for developing T2DM. The study projected a hazard rate of developing diabetes of 7.5% per year. In fact, the placebo treated group had a higher rate during the study (~11% per year) that contributed to the study’s early termination.
Table 1.
Eligibility Criteria and Baseline Characteristics of Recruited Cohort
| DPPa Eligibility Criteria | DPP Baseline Characteristics | Look:AHEAD Eligibility Criteria | Look:AHEAD Baseline Characteristics | |
|---|---|---|---|---|
| Number | 3000 | 3234 | 5000 | 5125 |
| Age (years) | ≥ 25 | 50.6 ± 10.7 b | 45–74c | 58.7 ± 6.8 b |
| Sex (% women) | 50 | 67.7 | 50 | 59.4 |
| Race (%) | ||||
| NHWd | 50 | 54.7 | <67 | 63.2 |
| African American |  |
19.9 | 15.6 | |
| Hispanic-American | 15.7 | 13.2 | ||
| Asian-American/ PIe | 4.4 | 1.0 | ||
| American Indian | 5.3 | 5.1 | ||
| BMI f (kg/m2) | ≥ 24g | 34 ± 6.7 b | ≥ 25h | 36.0 ± 6 b |
| Glucose levels (mg/dl) | ||||
| Fasting i | 95–125 | 107 ± 8.3 b | 153 ± 0.9j | |
| 2 hr- OGTT i | 140–199 | 165 ± 17 b | ||
| HbA1c (%) | 5.91 ± 0.5 b | ≤11 | 7.27 ± 0.2 b | |
DPP= Diabetes Prevention Program
Mean ± SD
Changed to 55–74 during 2nd year
NHW =Nonhispanic white
Pacific Islander
BMI =body mass index
≥ 22 in Asian-Americans
>27 if taking insulin.
To convert mg/dl glucose to mmol/L, multiply mg/dl by 0.05551.
Mean ± SE
Look AHEAD recruited a population of patients who had already developed T2DM to determine the putative benefits of a lifestyle intervention, similar to that implemented in DPP, on development of cardiovascular disease over time. (2) To enrich the rate of development of CVD events during the projected 12-year study, Look AHEAD included some patients who had already had a CVD event.
While these two studies, bound together through provision of a similar life-style intervention, had different specific goals, they both sought to delay the usual progression of dysglycemic states from pre-diabetes to diabetes and then to long-term complications. The lifestyle interventions addressed the underlying “environmental” factors, specifically overweight, obesity and sedentary lifestyle, that are widely accepted as central to increased risk of developing diabetes and, in turn, to its long-term complications. The studies were designed to address the metabolic continuum at different points in the pre-clinical and clinical course. In the US, pre-diabetes and diabetes affect as many as 60 million people (5).
The major recruitment criteria and profiles of the two study populations at baseline are shown (Table 1). The populations recruited represent two discrete slices of the pre-diabetes to diabetes continuum. Not surprisingly, the pre-diabetes cohort in DPP was approximately 8 years younger and slightly less overweight than the diabetic cohort in Look AHEAD.
LIFESTYLE INTERVENTION IN DPP AND LOOK:AHEAD: DESIGN
The major features of lifestyle interventions in DPP and Look AHEAD are summarized in Table 2. The DPP lifestyle intervention program has been previously described (6) and content and intervention materials are available at www.bsc.gwu./dpp/manuals.htmlvdoc Much of the content and materials used in Look AHEAD lifestyle intervention were adapted from DPP materials and then tailored for patients with T2DM (7). Intervention sessions in both trials focused on similar nutrition, behavioral and activity topics over the first year. In addition, both programs offered refresher programs and campaigns two to three times per year that were similar in content and duration (6,7).
Table 2.
Comparison of Lifestyle Intervention Features of DPP and Look AHEAD
| Diabetes Prevention Program (DPP) | Look AHEAD trial | |
|---|---|---|
| Weight loss goal | Study goal = 7% of initial wt Individual goal = 7% of initial wt |
Study goal = 7% of initial wt Individual goal = 10% of initial wt |
| Activity goal | 150 minutes per week | 175 minutes per week |
| Intervention format | Individual sessions | Group plus individual sessions |
| Frequency of follow up | 16 sessions in the 1st 6 months with minimum of one in-person follow up every 2 months thereafter | 24 sessions in the first 6 months; 18 sessions in months 7–12; minimum of monthly individual sessions years 2–4; |
| Refresher groups/ campaigns | 3 times/ year after 1st 6 months | 2–3 times/ year in years 2 and beyond |
| Supervised activity sessions | 2 times/ week throughout the trial | Periodically in refreshers or campaigns |
| Nutrition intervention | Fat gram counting with addition of calorie counting as needed; Self-selected diet | Calorie counting with inclusion of fat gram counting; Portion-controlled diet |
| Meal replacements | Recommended as a tool box or campaign strategy | Recommended as a regular part of the portion controlled diet and campaigns |
| Basic tool box strategies (to improve or maintain weight loss or physical activity) | Used throughout the intervention based on identification of barriers to achieving activity and weight loss goals: Problem solving strategies and no cost or low cost reinforcers for fulfilling behavioral contracts | Used in first 6 months for difficulty reaching weight loss and activity goals: Problem solving, motivational interviewing and behavioral contracts |
| Advanced tool box strategiesa | Higher cost items used to address barriers to weight loss and activity after first 6 months once no cost or low cost options had already been tried | Used after the first 6 months if participants did not meet activity goal or lose 5% of initial weight or regained 2% or more from lowest weight; includes use of higher cost items including weight loss medication |
Examples of advanced tool box strategies could be provision of frozen meals or exercise items.
At first glance, it’s clear that both DPP and Look AHEAD programs focused on the same process features: (1) goal setting for weight, activity, fat gram and calorie intake; (2) self-monitoring to achieve these goals; (3) frequent contact to provide accountability and sustain focus; (4) use of problem solving and other tool box strategies to address goals and potential barriers to achieving them; and (5) emphasis on managing individual high-risk situations. However, closer examination of these interventions reveals several differences that may help explain differences in weight loss results at 1 year and inform efforts to translate these programs and results into practice.
Goal setting
The DPP weight loss goal of losing 7% of initial body weight was based on results of previous weight loss trials, perceived feasibility of achieving the goal in a multicenter trial, and epidemiologic data supporting this level of weight loss as effective in reducing diabetes risk (6). While both DPP and Look AHEAD interventions set study-wide weight loss goals of 7% of initial body weight, Look AHEAD set individual weight loss goals of 10%, based on success of DPP, evidence that larger weight losses are generally associated with greater improvements in outcomes, and speculation whether DPP participants would have lost more weight if a higher goal had been set. (7)
To help achieve its weight loss goals, DPP set daily calorie goals that were 500 to 1000 calories below weight maintenance with the aim of achieving weight loss of 1 to 2 pounds per week. Fat gram goals were based on 25% of calories from fat. Four standard calorie levels were used based on initial body weights: 1200 kcal /day (33gm fat) for 120–170 lbs; 1500 kcal /day (42 gm fat) for 175–215 lbs; 1800 kcal /day (50 gm fat) for 220–245 lbs and 2000 kcal/day (55 gm fat) for >250 lbs (6). Look AHEAD calorie goals were more ambitious: 1200–1500 kcal /day (40–50 gm fat) for initial weights <250 lbs and 1500 to 1800 kcal/day (50–60 gm fat) for initial weights > 250 lbs. Look AHEAD fat gram goals were set at <30% of calories from fat (7).
The DPP activity goal of 150 minutes per week of moderate-intensity physical activity, similar to a brisk walk, was selected because evidence supported its feasibility and effectiveness, and it was consistent with public health recommendations and the Surgeon General’s Report on Physical Activity and Health (8). The 150-minute per week goal could include up to 75 minutes per week from strength training and would expend approximately 700 kilocalories. DPP lifestyle participants were encouraged to distribute their activity over at least 3 days per week with at least 10 minutes of physical activity per session. To support participants in achieving activity goals, each DPP center offered supervised activity sessions at least 2 times per week throughout the trial. (6)
Look AHEAD’s physical activity goal was set at 175 minutes per week, again based on the success of DPP, and on findings that higher levels of physical activity significantly improve weight loss maintenance and other health outcomes (7, 9). Look AHEAD’s activity program relies upon unsupervised (at-home) exercise.
Self-monitoring
DPP developed a fat and calorie counter booklet that addressed needs of a culturally diverse population and included foods commonly consumed by African-American, Hispanic-American, Asian-American, and American Indian subgroups. DPP self-monitoring booklets helped participants track food portions, fat gram and calorie intake and activity minutes. Look AHEAD used the same fat and calorie counter and food and activity diary. These resources are available at www.ndep.nih.gov as part of the National Diabetes Education Program (NDEP) “Small Steps Big Rewards Program: Prevent Type 2 Diabetes” toolkit that was developed based on DPP results.(10)
Intervention frequency and format
The DPP lifestyle intervention was delivered by individual lifestyle coaches. Participants received a 16-week core curriculum over the first 6 months (~ weekly contact) and then had at least one contact monthly for the remainder of the study (at least one in-person visit every 2 months with phone visits as needed to maintain once per month contact) (6). On average, lifestyle participants attended 23.6 + 7.1 individual sessions during year 1, 12.5 + 7.1 sessions during year 2 and 50.3 + 21.8 sessions over the entire trial (11).
The Look AHEAD intervention is delivered in a group plus individual format by intervention teams that include registered dietitians, behavioral psychologists and exercise specialists. Participants are offered weekly sessions with three group sessions and one individual session per month in the first six months and two group sessions and one individual session per month during months 7 –12, a total of 42 sessions the first year. In years 2–4, participants are offered a minimum of monthly individual sessions and one additional contact by group, phone, mail or e-mail (7).
Individual sessions in DPP and Look AHEAD ranged from 20–60 minutes and included private weigh-in, review of self-monitoring records, presentation of a new topic, ongoing identification of personal barriers to weight loss and activity and development of action plans/goals for the next session (6, 7). Group sessions in Look AHEAD include the same 10–20 participants for the first year (closed groups) and range from 60–75 minutes. The group format includes the same private weigh-in, group check-ins to self report on progress with weight, self-monitoring and goal setting, presentation of a new topic, discussion and problem solving of ongoing barriers and identification of action plans and homework for next session (7).
Nutrition Intervention Strategy
The main focus of the nutrition intervention strategy in DPP started with a self-discovery process through self-monitoring of food intake and fat gram intake. Participants learned that there were three ways to eat less fat: choose high fat foods less often, eat smaller portions of high fat foods, or substitute lower fat foods. For the first seven sessions, participants focused only on fat gram counting. Then, if they were not on track for a 7% weight loss at session 7 they would also receive a calorie goal to enhance progress with weight loss on their self-selected diet. Meal replacements and structured menus or meals were optional tool-box items that coaches could use with participants to enhance weight loss (7).
In Look AHEAD, the nutrition intervention strategy focused on calorie counting with fat gram goals and use of meal replacements as part of the intervention for all participants from the outset. For the first 4 to 16 weeks, participants were encouraged to use two meal replacements and two snack replacements per day, and structured menus for their main meal. After that, they were encouraged to transition to one meal replacement and one snack replacement per day and continue with structured menus and meals and a portion controlled diet for the remainder of the day (7). Look AHEAD nutrition intervention strategies were chosen based on evidence that combining fat and calorie counting vs. calorie or fat gram counting alone, and using meal replacements vs. a self-selected diet from the outset resulted in significantly greater weight losses. (7, 12, 13)
Tool box approaches
Throughout DPP, coaches worked with each participant individually to identify personal barriers to achieving the activity and weight loss goals. They could use a variety of “tool-box” approaches to help participants deal with barriers. Tool-box approaches were used in hierarchical fashion such that low cost or no cost approaches (in terms of both staff time and money) were used first and higher cost approaches were used after low cost approaches were tried. The most common tool-box approaches used were problem solving and use of reinforcers for fulfilling behavioral contracts. Examples of higher cost items might be the purchase of walking shoes, a cookbook, frozen dinners, or enrollment in a community class (6, 14).
In Look AHEAD, basic and more advanced tool-box approaches were designed with specific criteria for use. Basic tool-box strategies, such as problem solving, motivational interviewing and behavioral contracts, were used for participants who had difficulty adhering to diet and exercise recommendations or who were losing <1% of weight per month. Advanced tool-box approaches were used after the first six months for participants who failed to lose 5% of initial weight or who had regained 2% or more from their lowest weight. (7)
In Look AHEAD, advanced tool-box items could include provision of frozen meals, community classes, exercise items or use of weight loss medication. Thus far, orlistat has been the only weight loss medication in the tool-box and it is only offered as an option to those who lost <5% of initial weight or regain > 2% from their lowest weight. Participants who lose and maintain > 10% of initial weight are not eligible for the weight loss medication; however, those who lose 5–9.9% of initial weight can request it (4,7).
In summary, although there were many similarities in features of DPP and Look AHEAD lifestyle interventions, Look AHEAD’s lifestyle intervention was more ambitious in several ways: higher individual weight loss goals; lower calorie and fat gram targets based on initial body weight; more intensive intervention frequency capitalizing on advantages of both closed group and individual formats; and more structured nutrition intervention strategies that combined fat and calorie counting and incorporated use of meal replacements from the outset. Look AHEAD’s lifestyle intervention was planned to be more ambitious because people with T2DM enrolled in weight loss programs have traditionally lost less weight than their non-diabetic counterparts and because of the need to produce weight loss over 12 years to answer the primary study question.
LIFESTYLE INTERVENTION IN DPP AND LOOK AHEAD: RESULTS
DPP completed its major clinical trial phase in 2001, after approximately 3 years mean study duration and one year sooner than its planned duration. Look AHEAD is ongoing and is approximately half-way through its anticipated 12-year duration. The currently available data allow comparison of weight loss results at 1 year for DPP and Look AHEAD.
Life-style changes- intermediate outcomes
The Look AHEAD lifestyle intervention borrowed extensively from DPP’s protocol; therefore, similar results in the two studies with regard to weight loss and activity levels would not be surprising. However, differences in study populations reviewed above, potential impact of diabetes medications on weight change in Look AHEAD, implementation of lifestyle interventions individually in DPP but in groups in Look AHEAD, and the differences, albeit modest, in lifestyle goals between the two studies might have resulted in different outcomes. In fact, the intermediate outcomes of the lifestyle interventions in the two studies were remarkably more similar than not (Table 3).
Table 3.
Lifestyle Goals and Results after One Year of Lifestyle Interventions
Major study outcomes
In DPP, lifestyle intervention was highly effective in delaying the onset of diabetes, reducing the cumulative incidence by 58% compared with placebo. Similar results were achieved with lifestyle intervention in the Finnish Diabetes Prevention study.(15) Of note, secondary analyses of DPP revealed that weight loss appeared to be the major mediator of diabetes prevention, with physical activity levels playing a “supporting role” by helping to maintain weight loss.(16) Look AHEAD has not reported any interim outcome results of its lifestyle intervention, other than the intermediate weight loss noted above, and CVD risk factors reviewed below.
In addition to the salutary effect of lifestyle intervention on diabetes prevention, reduction in diabetes complications, including cardiovascular disease (CVD), is an important goal of the ongoing follow-up to DPP, the DPP Outcomes Study. Reduction in CVD outcomes is the primary goal of Look AHEAD. Both studies will require more years of follow-up to demonstrate the putative effects of lifestyle intervention on CVD; however, a beneficial effect of lifestyle intervention on CVD risk factors has been demonstrated after three years and one year of follow-up in DPP and Look AHEAD studies, respectively.(4,17) (Table 4) Lifestyle intervention in pre-diabetes and diabetes results in improvements in blood pressure and lipids, in addition to weight-loss and physical conditioning. In addition, DPP lifestyle intervention significantly reduced levels of nontraditional risk factors, including CRP and fibrinogen relative to placebo and to a lesser degree relative to metformin.(18) Comparable analyses have not yet been reported in Look AHEAD.
Table 4.
Effects of Lifestyle Interventions on Glycemia and CVD Risk Factors
| DPPa (n = 1079) | Look:AHEADb (n = 2496) | |
|---|---|---|
| HbA1c (%) | N/Ac | −0.64 ± 0.02d |
| Fasting plasma glucose (mg/dl) | N/A c | −21.5 ± 0.9d |
| Blood Pressure (mmHg) | ||
| Systolic | −3.3 ± 0.5d | −6.8 ± 0.4d |
| Diastolic | −3.8 ± 0.3d | −3.0 ± 0.2d |
| LDL-cholesterol (mg/dl) | NS | −5.2 ± 0.6 |
| HDL-cholesterol (mg/dl) | +1.0d | +3.4 ± 0.2d |
| Triglycerides (mg/dl) | −25.4d | −30.3 ± 2.0d |
N/A= specific results not available, however for approximate results, see figure 3 (ref 3)
< 0.001 compared with control group; To convert mg/dl glucose to mmol/L, multiply mg/dl by 0.05551; To convert mg/dl LDL or HDL to mmol/L, multiply by 0.02586; To convert mg/dl triglycerides to mmol/L, multiply by 0.0112.
TRANSLATING EVIDENCE-BASED LIFESTYLE INTERVENTIONS INTO COMMUNITY RESEARCH AND CLINICAL PRACTICE
Since Look AHEAD is still in progress, studies investigating means of translating its results into community practice have not yet been conducted. However, an increasing number of studies are investigating translating DPP results. (19–26). These DPP translational research studies have demonstrated that DPP lifestyle intervention can be successfully implemented in various settings; a diabetes education center and medical fitness facility (19), primary care settings (20), urban underserved communities (19,21,22), YMCAs (21), Latino communities (22), and employee worksites (24,25).
As a result of United States Congressional direction, Indian Health Service (IHS) established the SDPI Diabetes Prevention Project to fund activities based on DPP including (1) diabetes screening, (2) recruitment of individuals with “prediabetes” into programs (approximately 50 per year for three years), (3) implementation of group classes providing the DPP’s 16-session education curriculum, and (4) individual lifestyle coaching sessions, exercise programs, cooking and shopping demonstrations, and follow-up support to reinforce the curriculum program. Currently 36 Tribal, IHS, and Urban Indian programs nationwide participate in the program (Personal communication, Tammy L. Brown, MPH, RD, Nutrition Consultant, IHS Division of Diabetes Treatment and Prevention, July 16, 2007).
The Diabetes Primary Prevention Initiative (DPPI), funded by Centers for Disease Control and Prevention’s Division of Diabetes Translation (DDT), has funded five Diabetes Prevention and Control Programs to design and implement pilot interventions adapted from DPP in California, Massachusetts, Michigan, Minnesota, and Washington State. These programs focus on interventions, surveillance, and systems dynamics modeling and are targeting health care organizations, local worksites, educators, primary care practices, community-based lifestyle intervention resources, YMCA programs, and clinic and community events to conduct diabetes screenings.
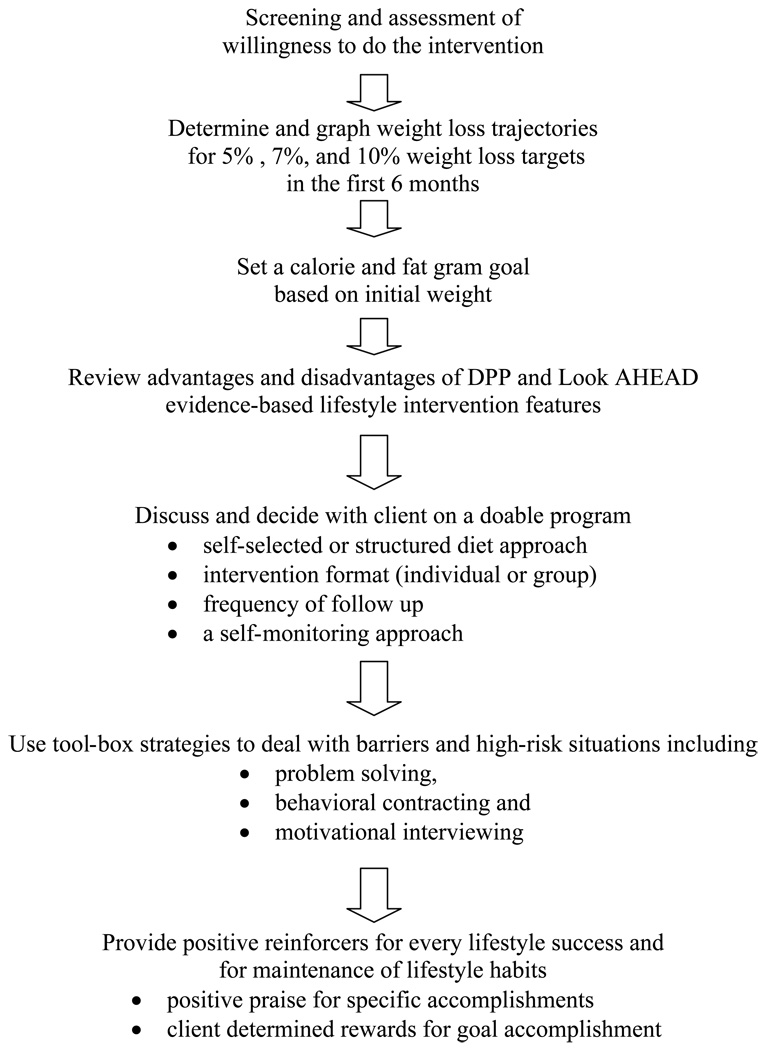
More full-scale translational research trials are planned and dietitians need to consider how they might translate these evidence-based interventions into practice. Figure 1 represents a conceptual model for evidence-based translation of DPP and Look AHEAD into clinical practice using individual, group or combined group and individual formats. This process starts with helping patients determine through a behavioral screening interview process whether or not they are ready to commit to lifestyle change and what type of program is best suited for them. Once readiness is established, then dietitians can review various weight loss trajectories that would be considered safe, realistic, efficacious and successful over 6 months. Since calorie and fat gram goals for DPP and Look AHEAD were somewhat different, dietitians can review these distinctions with clients and help them choose fat and calorie goals that are achievable based on assessment of motivation and usual eating habits. Since both self-selected and structured diet approaches have been shown to be effective, dietitians can review advantages and disadvantages of each, offer patients a menu approach to selecting a nutrition intervention strategy and then agree upon calorie and fat gram goals, an individual, group or combined individual and group format, type of self-monitoring (related to weight, food, activity) and frequency of follow-up needed to support goal achievement. Every step of the process described in Figure 1 helps patients establish realistic goals that are achievable, receive positive reinforcement for those achievements, and learn self-monitoring skills, problem solving skills and self-motivational strategies that contribute to increased self-efficacy and satisfactory results.
Figure 1.
Translating Lifestyle interventions to Clinical Practice Settings
As researchers and practitioners, dietitians are in key roles to make sure the evidence, knowledge and insights gained from working in clinical trials are translated and fully applied in both community-based research and practice. Dietitians in DPP and Look AHEAD received annual trainings focused on effective delivery of lifestyle intervention sessions, extensive use of case presentations, role playing and clinical practice skills such as reflective listening, motivational interviewing and empowerment strategies. Most centers also had a part-time behavioral psychologist who could help dietitians address chronic behavioral barriers to diet and exercise adherence (6,7). Dietitians should seek opportunities to refine their skills, and identify what roles they might play in establishing or participating in community programs and translational research so they are positioned to effectively apply lessons learned in DPP and Look AHEAD and help combat the dual epidemics of obesity and T2DM.
Contributor Information
Linda M Delahanty, Chief Dietitian and Director of Nutrition and Behavioral Research, MGH Diabetes Center, Massachusetts General Hospital, 50 Staniford St Suite 340, Boston, MA 02114, Phone: 617-724-9727, Fax: 617-726-1871, ldelahanty@partners.org.
David M Nathan, Director, MGH Diabetes Center Massachusetts General Hospital, 50 Staniford St Suite 340, Boston, MA 02114, Phone: 617-726-2875, Fax: 617-726-1871, dnathan@partners.org.
References
- 1.Diabetes Prevention Program Research Group. The Diabetes Prevention Program: Design and methods for a clinical trial in the prevention of type 2 diabetes. Diabetes Care. 1999;22:623–634. doi: 10.2337/diacare.22.4.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Look AHEAD Research Group. Look AHEAD (Action for Health in Diabetes): design and methods for a clinical trial of weight loss for the prevention of cardiovascular disease in type 2 diabetes. Con Clin Trials. 2003;24:610–628. doi: 10.1016/s0197-2456(03)00064-3. [DOI] [PubMed] [Google Scholar]
- 3.Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Look AHEAD Research Group. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes. Diabetes Care. 2007;30:1374–1383. doi: 10.2337/dc07-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Atlanta: National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention; National Diabetes Surveillance System: Data and Trends. Accessed at http://www.cdc.gov/diabetes/statistics/index.htm on 24 July 2007.
- 6.The Diabetes Prevention Program Research Group. The Diabetes Prevention Program (DPP): Description of lifestyle intervention. Diabetes Care. 2002 Dec;25(12):2165–2171. doi: 10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wadden TA, Smith WestD, Delahanty LM, Jakicic JM, Rejeski J, Berkowitz RI, Williamson DA, Kelley DE, Kumanyika SK, Hill JO Tomchee CM and the Look AHEAD Research Group. The Look AHEAD study: A description of the lifestyle intervention and the evidence supporting it. Obesity. 2006;14(5):737–752. doi: 10.1038/oby.2006.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Physical Activity and Health: A report of the Surgeon General. Washington, DC: U.S. Department of Health and Human Services, President’s Council on Fitness and Sports; 1996. National Center for Chronic Disease Prevention and Health Promotion. [Google Scholar]
- 9.Jeffrey RW, Wing RR, Sherwood NE, Tate DF. Physical activity and weight loss: Does prescribing higher physical activity goals improve outcome? Am J Clin Nutr. 2003;78:684–689. doi: 10.1093/ajcn/78.4.684. [DOI] [PubMed] [Google Scholar]
- 10.Delahanty LM, Nathan DM. Research Navigating the Course of Clinical Practice in Diabetes. Am Diet Assoc. 2004;104:1846–1853. doi: 10.1016/j.jada.2004.09.028. [DOI] [PubMed] [Google Scholar]
- 11.Wing RR, Hamman RF, Bray GA, Delahanty L, Edelstein SL, Hill JO, Horton ES, Hoskin MA, Kriska A, Lachin J, Mayer-Davis EJ, Pi-Sunyer X, Regensteiner JG, Venditti E. Wylie-Rosett J and Diabetes Prevention program Research Group Achieving weight and activity goals among Diabetes Prevention Program lifestyle participants. Obes Res. 2004;12:1426–1434. doi: 10.1038/oby.2004.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ditschuneit HH, Fletchner-Mors M, Johnson TD, Adler G. Metabolic and weight loss effects of long-term dietary intervention in obese subjects. AmJ Clin Nutr. 1999;69:198–204. doi: 10.1093/ajcn/69.2.198. [DOI] [PubMed] [Google Scholar]
- 13.Pascale RW, Wing RR, Butler BA, Mullen M, Bononi P. Effects of a behavioral weight loss program stressing calorie restrictions versus calorie plus fat restriction in obese individuals with NIDDM or a family history of diabetes. Diabetes Care. 1995;18:1241–1248. doi: 10.2337/diacare.18.9.1241. [DOI] [PubMed] [Google Scholar]
- 14.Wylie-Rosett J, Delahanty L The Diabetes Prevention Program Research Group. An integral role of the dietitian: Implications of the Diabetes Prevention Program. J Am Diet Assoc. 2002 Aug;102(8) doi: 10.1016/s0002-8223(02)90241-5. 1065-8.mi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P, Keinanen-Kiukaanniemi S, Laakso M, Louheranta A, Rastas M, Salminen V. Uusitupa M and the Finnish Diabetes Prevention Study Group Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;34:1342–1350. doi: 10.1056/NEJM200105033441801. [DOI] [PubMed] [Google Scholar]
- 16.Hamman RF, Wing RR, Edelstein SL, Lachin JM, Bray GA, Delahanty L, Hoskin M, Kriska AM, Mayer-Davis EJ, Pi-Sunyer X, Regensteiner J, Venditti B. Wylie-Rosett J, for the Diabetes Prevention Program Research Group. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care. 2006 Sep;29(9):2102–2107. doi: 10.2337/dc06-0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Diabetes Prevention Program Research Group. Impact of intensive lifestyle and metformin therapy on cardiovascular disease risk factors in the Diabetes Prevention Program. Diabetes Care. 2005;28:888–894. doi: 10.2337/diacare.28.4.888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Diabetes Prevention Program Research Group. Intensive lifestyle intervention or metformin on inflammation and coagulation in participants with impaired glucose tolerance. Diabetes. 2005;54:1566–1572. doi: 10.2337/diabetes.54.5.1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Seidel MC, Powell RO, Piatt GA. Translating the diabetes prevention program in an urban underserved community: long term sustainability of positive clinical outcomes. Diabetes. 2007;56 Supp:A42. [Google Scholar]
- 20.Kramer MK, Miller R, Venditti E, Orchard TJ. Group Lifestyle Intervention for Diabetes Prevention in Those with Metabolic Syndrome in Primary Care Practice. Diabetes. 2006 June;55 Supp:A517. [Google Scholar]
- 21.Ackermann RT, Marrero D, Honghong Z, Brizendin EJ. Translating the Diabetes prevention Program into the community: The YMCA model. Diabetes. 2007;56 Supp:A43. [Google Scholar]
- 22.Ruggiero L, Rodriguez-Sanchez M, Oros S. Translating the Diabetes Prevention Program’s (DPP) lifestyle intervention to the community: Making the connection latino pilot study. Diabetes. 2007;56 Supp:A226. [Google Scholar]
- 23.Janetski JH, Lisowski C. Living on the Edge of Diabetes: A study using the Diabetes Prevention Program in a community setting. Diabetes. 2007;56 Supp:A229. [Google Scholar]
- 24.Aldana S, Barlow M, Smith R, Yanowitz F, Adams T, Loveday L, Arbuckle J, LaMonte M. The Diabetes Prevention Program: A Worksite Experience. Association of Occupational Health Nurses Journal. 2005;53:499–507. [PubMed] [Google Scholar]
- 25.Aldana S, Barlow M, Smith R, Yanowitz F, Adams T, Loveday L, Merrill RM. A worksite diabetes prevention program: two-year impact on employee health. American Association of Occupational Health Nurses Journal. 2006;54(9):389–395. doi: 10.1177/216507990605400902. [DOI] [PubMed] [Google Scholar]
- 26.McBride PE, Einerson JA, Grant H, Sargent C, Underbakke G, Vitcenda M, Zeller L, Stein JH. Putting the Diabetes Prevention Program into practice: A program for weight loss and cardiovascular risk reduction for patients with metabolic syndrome or type 2 diabetes mellitus. Journal of Nutrition, Aging and Health. doi: 10.1007/BF03028624. (in press). [DOI] [PubMed] [Google Scholar]