Abstract
Sleep duration is associated with cardiovascular disease and diabetes risk factors, depression, automobile and workplace accidents, and prospective mortality. Little is known, however, about sleep patterns in the US population. The 2004–2007 National Health Interview Survey-Sample Adult Files provide nationally representative data for 110,441 noninstitutionalized US adults aged 18 years or older, and multinomial logistic regression examines whether variables in 5 domains—demographic, family structure, socioeconomic, health behavior, and health status—are associated with long or short sleep duration. Being older, non-Hispanic black, or a current or former smoker; having low levels of education, income, or few income sources; consuming few or numerous drinks in a week; or reporting cardiovascular disease, diabetes, depression, underweight, or activity limitations is associated with increased odds of both long and short sleep duration. Other variables are associated with shorter (e.g., living with young children, being unmarried, working long hours, more frequent binge drinking) or longer (e.g., being younger, Mexican American, pregnant, or having low levels of physical activity) sleep hours. The authors identify numerous risk factors for long and short sleep; many of those variables are potential confounders of the relation between sleep hours and other health outcomes.
Keywords: family, health behavior, health status disparities, life style, sleep, social class
Sleep durations that are longer or shorter than 7–8 hours in a 24-hour period are associated with cardiovascular disease and diabetes risk factors (1–5), depression (6, 7), automobile and workplace accidents (8–11), learning and memory problems (12), and excess mortality (13–19). Because we know little about the contours of sleep duration in the US population, our primary aim is to examine the relation between sleep duration and demographic, family structure, socioeconomic, health behavior, and health status variables in a nationally representative sample of US adults.
Short sleep duration is associated with demographic factors including being older (7, 20, 21) or female (22); being black is associated with both long and short sleep (23). Nativity has not been linked to sleep, but immigrants often have prosocial ties and cultural practices that promote health and reduce mortality (24, 25). Supportive marriages foster healthy behaviors and adequate sleep (19, 26–28). Pregnancy and parenting promote healthier lifestyles (29, 30), but caring for young children can disrupt sleep, and hormonal changes increase sleep among pregnant women (31). Low socioeconomic status limits the resources that foster health (25, 32) and is associated with long and short sleep (1, 7, 19, 33–35), but unemployment is associated with long sleep (28), and long work hours can limit the time available for sleep.
Smoking and alcohol consumption lead to reduced sleep, and physical inactivity is associated with both short and long sleep (19, 36–39). Health behaviors can increase (i.e., exercise, smoking) or depress (i.e., drinking) physiologic arousal or indicate lifestyles that interfere with good sleep hygiene. Subjective and objective measures of poor health and obesity are associated with reduced sleep (3–5, 13, 14, 16, 20, 37, 38), and cardiovascular disease and diabetes risk factors, as well as depression, are associated with both long and short sleep (1–7). Poor health can disturb sleep by increasing pain or discomfort (40), creating breathing problems (e.g., obesity, respiratory conditions) (5, 41), or increasing stress or impacting physiologic arousal (e.g., anxiety, depression) (6, 7, 23).
We extend prior research in 2 ways. First, we use a large, current, nationally representative sample of noninstitutionalized US adults with numerous covariates. Prior community-based studies are often limited by small, regional, or non-nationally representative data or by few social, behavioral, and health variables (1, 6, 7, 20, 22, 26–28, 33, 37, 42–49). Second, we allow our covariates to have different relations with long and short sleep. Many studies model sleep duration as a continuous variable (43, 44, 50), although both long and short sleep are associated with worse health (1–7, 13–17), and the determinants of long and short sleep may differ.
MATERIALS AND METHODS
We pooled the 2004–2007 waves of the National Health Interview Survey-Sample Adult Files (NHIS-SAF) to examine sleep duration in a large (N = 110,441), nationally representative survey of noninstitutionalized adults aged 18 years or older in the United States (51). These data come from annual, cross-sectional surveys that conducted in-person interviews in English or Spanish; asked detailed questions on sociodemographic, socioeconomic, and behavioral characteristics; and were designed to track the health of the US population. The response rate was 81%.
Variables
Self-reported sleep duration was ascertained with the question, “On average, how many hours of sleep do you get in a 24-hour period?” Respondents could report in only 1-hour increments; thus, they could report 7 hours or 8 hours but not 7 hours and 20 minutes. The item ranged from 0 to 23, with 99% of the cases falling between 4 and 12 hours. The variable was categorized as 5 or fewer hours, 6 hours, 7 hours, 8 hours, or 9 or more hours. We separated those who slept 7 and 8 hours, because those who sleep 7 hours have lower risks of death than those who sleep 8 hours (14, 16–18). We also examined whether different factors were associated with very short (5 or fewer hours) or moderately short (6 hours) sleep. Self-reported sleep duration is widely used in epidemiologic studies and is the basis of research on the relation between sleep duration and mortality (13–19).
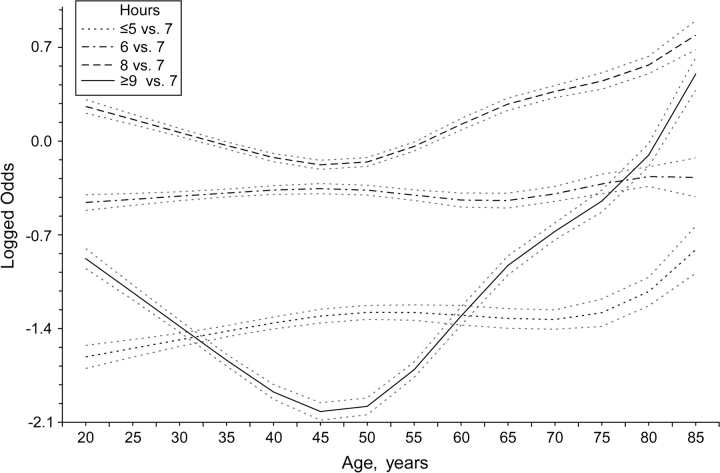
Cubic splines adjust for age (range, 18–85 years or older). We compared models with 1, 2, 3, and 4 knots, with 3 knots at ages 35, 50, and 65 years best fitting the data. Sex was coded as “1” for males and “0” for females. Race/ethnicity was coded categorically as non-Hispanic white, non-Hispanic black, other non-Hispanic, Mexican American, and other Hispanic. A dichotomous variable contrasted foreign-born and US-born respondents.
A categorical variable indicated respondents who live with 1 or more children aged from birth to less than 2 years, from 2 to less than 6 years, from 6 to less than 13 years, and from 13 to less than 18 years, or who were not living with children. Pregnancy status was coded as “1” if women aged 18–49 years reported that they were pregnant and as “0” otherwise. Marital status was coded as “1” if respondents were currently married and as “0” otherwise. Cohabiting individuals were assigned their legal marital status.
A categorical variable indicated whether respondents usually worked more than full-time (41 or more) hours, full-time (35–40) hours, or less than full-time (1–34) hours per week, or if they were not employed. Education was coded categorically as less than a high school degree, a high school degree, some college but less than a 4-year degree, and a 4-year degree or more. Family income was reported in 1 of 11 categories, ranging from $0–$4,500 to $75,000 or more. We took the midpoint of each interval that was less than $75,000 and estimated a median value for the open-ended interval to approximate a continuous variable (52), converted all values to 2007 dollars (53), adjusted for the purchasing power of differently sized families (54), divided the variable by 10,000, and took the log to account for the diminishing returns to health as income increases (25). The income portfolio ranged from 0 to 6 and measured the number of income sources, per family member, received from jobs, self-employment, Social Security retirement (not due to disability), interest-bearing accounts, dividends, and other income. The income portfolio is a proxy for wealth and captures the family's income diversification (55).
The physical activity index was calculated as the sum of 3 items (α = 0.61) that indicated the number of times per week that individuals undertook leisure-time activity that caused heavy sweating or large increases in breathing or heart rate (item 1), caused light sweating or slight-to-moderate increases in breathing or heart rate (item 2), or was undertaken to improve strength (item 3). Each item was standardized to have a mean of 0 and a standard deviation of 1 to give it equal weight in the index, and we standardized the resulting index so we could interpret our results in standard deviation units. Current smokers were coded as the number of packs smoked per day (range, 0.05–4.5) and coded as “0” for former or never smokers. A dichotomous variable indicated former smokers, and never smokers were the referent when the variables for current packs smoked and former smoker were equal to 0.
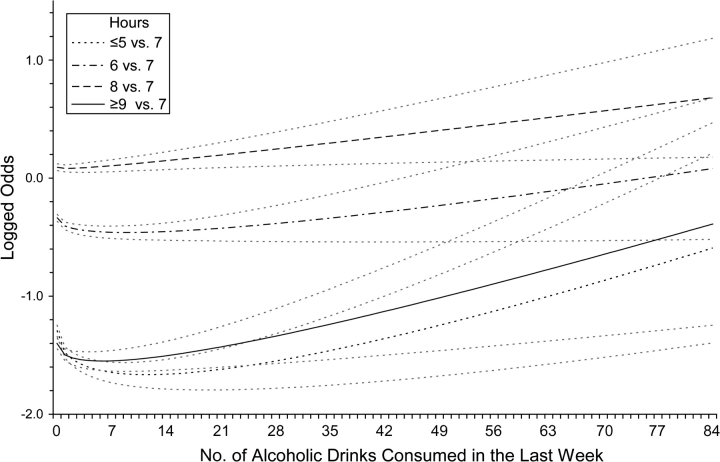
Weekly alcohol consumption (range, 0–84 drinks) was calculated by multiplying the number of days that respondents drank in the last 7 days by the number of drinks typically consumed on the days that they drank. We tested for a nonmonotonic relation with sleep by raising the drinking variable to all combinations of 2 of the following powers: 0.5, 1, 2, 3, and 4. The powers of 0.5 and 1 provided the best model fit. A variable for binge drinking indicated the number of days in the last year that respondents drank 5 or more drinks at a sitting (range, 0–365 days); adding 1 and taking the logarithm fit the data better than did linear or squared terms.
A dichotomous variable for cardiovascular disease indicated respondents who were ever told by a doctor that they had coronary heart disease, angina pectoris, hypertension, a heart attack, a stroke, or any other heart disease. Acute respiratory conditions were coded dichotomously and indicated whether respondents were diagnosed with bronchitis in the last 12 months or had a head or chest cold in the last 2 weeks. Chronic respiratory conditions were coded dichotomously and indicated whether respondents were ever diagnosed with emphysema or asthma. A dichotomous variable indicated respondents who were ever diagnosed with diabetes. A dichotomous variable indicated whether respondents had pain in their joints, back, head, or neck in the last 3 months.
Mental health was ascertained with the question, “During the past 30 days, how often did you feel [symptom]?” where the symptoms included “so sad that nothing could cheer you up,” “nervous,” “restless or fidgety,” “hopeless,” “that everything was an effort,” and “worthless.” Responses ranged from 0 (none of the time) to 4 (all of the time). Depression was measured as the sum of the symptoms of sadness, hopelessness, effort, and worthlessness (α = 0.84). Anxiety was measured as the sum of the symptoms of nervousness and restlessness (α = 0.77). Each index was standardized to have a mean of 0 and a standard deviation of 1. The mental health measures were validated with a 2-stage clinical reappraisal survey and strongly discriminate between community cases and noncases with Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), disorders (56).
Body mass index (BMI), based on self-reported heights and weights, was calculated as weight (kg)/height (m)2. Respondents were coded as underweight (BMI, <18.5), normal weight (BMI, 18.5–<25.0), overweight (BMI, 25.0–<30.0), or obese (BMI, ≥30.0) (57). Despite some misreporting in self-reported height and weight, the resulting body masses are associated with overall and cause-specific mortality in similar ways as objectively measured body mass (58). A dichotomous variable for functional limitations indicated respondents who were limited in their basic mobility or social activities.
Statistical analysis
Twenty-nine percent of the respondents had missing information on at least 1 of our variables. Multiple imputation preserved our sample size and relied on more plausible assumptions than other commonly used methods of dealing with missing data (59). Each of our 10 complete data sets drew different imputed values from the posterior predictive distribution that was estimated with over 75 variables from our data (60, 61). The variation across the data sets reflects our uncertainty about the imputed values and increases our standard errors accordingly (59, 60, 62).
Multinomial logistic regression models used 7 hours of sleep as the comparison group, because that sleep duration is associated with the lowest mortality risk (14, 16–18); this model allows the covariates to have different relations with short and long sleep. Four nested models explored the relations between our covariates and sleep duration; each model included additional variables that we considered increasingly proximate determinants of sleep. Model 1 examined baseline demographic differences in sleep before adjusting for additional variables. Model 2 further included the family structure and socioeconomic variables to establish their relations with sleep, regardless of whether they shaped sleep through health behaviors or health status. Model 3 further included the health behavior variables to examine their relations with sleep duration, regardless of whether they worked through health status. Model 4 further included the health status variables. The results were presented as odds ratios, and the “svy” commands in STATA, version 10, software (StataCorp LP, College Station, Texas) weighted our data to the US population and estimated Taylor linearized standard errors that accounted for the multistage sampling frame used by the NHIS-SAF (51, 63). We used the method described by Korn and Graubard (64) to adjust for changes in the survey design as recommended by the NHIS-SAF documentation (51).
RESULTS
The descriptive statistics in Table 1 show that short or long sleep is common: 28.3% of adults sleep 6 or fewer hours, 8.5% sleep 9 or more hours, and only 63.3% sleep 7 or 8 hours. Males and non-Hispanic whites were more likely to report 7 hours of sleep than were females or other race/ethnic groups. The presence of children aged 18 years or younger is associated with short sleep, and being pregnant is associated with long sleep.
Table 1.
Weighted Means and Percentages of Covariates by Self-reported Sleep Hours in a Usual 24-Hour Period, US Adults Aged 18 Years or Older, 2004–2007a
| Self-reported Sleep Hours |
P Valueb | |||||
| ≤5 | 6 | 7 | 8 | ≥9 | ||
| Total, % | 7.8 | 20.5 | 30.8 | 32.5 | 8.5 | |
| Demographic status | ||||||
| Age, mean years | 46.8 | 45.4 | 45.2 | 46.2 | 49.7 | <0.001 |
| Sex, % | <0.001 | |||||
| Female | 7.9 | 19.9 | 29.8 | 33.3 | 9.2 | |
| Male | 7.6 | 21.1 | 31.9 | 31.6 | 7.8 | |
| Race/ethnicity, % | <0.001 | |||||
| Non-Hispanic white | 7.4 | 20.1 | 32.1 | 32.1 | 8.3 | |
| Non-Hispanic black | 11.0 | 23.8 | 25.0 | 30.2 | 10.1 | |
| Other non-Hispanic | 7.9 | 22.1 | 31.3 | 31.5 | 7.2 | |
| Mexican American | 5.4 | 17.1 | 27.9 | 40.1 | 9.5 | |
| Other Hispanic | 9.0 | 21.2 | 31.0 | 32.3 | 6.6 | |
| Foreign born, % | <0.001 | |||||
| No | 8.0 | 20.7 | 30.7 | 31.9 | 8.7 | |
| Yes | 6.6 | 19.2 | 31.3 | 35.8 | 7.2 | |
| Family structure | ||||||
| Any children, % | <0.001 | |||||
| No children | 7.4 | 19.2 | 29.7 | 34.0 | 9.8 | |
| >0–<2 years | 9.2 | 25.1 | 31.2 | 28.3 | 6.2 | |
| 2–<6 years | 8.2 | 22.9 | 32.5 | 30.2 | 6.2 | |
| 6–<13 years | 8.5 | 22.7 | 33.8 | 29.3 | 5.8 | |
| 13–<18 years | 9.2 | 23.3 | 33.8 | 28.8 | 4.9 | |
| Currently pregnant, % | <0.001 | |||||
| No | 7.8 | 20.6 | 30.9 | 32.4 | 8.4 | |
| Yes | 4.1 | 11.4 | 21.4 | 42.6 | 20.6 | |
| Currently married, % | <0.001 | |||||
| No | 8.8 | 20.8 | 28.2 | 32.1 | 10.2 | |
| Yes | 7.0 | 20.2 | 32.8 | 32.8 | 7.2 | |
| Socioeconomic status | ||||||
| Hours worked per week, % | <0.001 | |||||
| ≥41 | 9.7 | 27.0 | 35.6 | 24.4 | 3.3 | |
| 35–40 | 6.3 | 21.2 | 35.2 | 32.6 | 4.7 | |
| 1–34 | 6.9 | 18.9 | 30.4 | 35.0 | 8.9 | |
| Not working | 8.5 | 16.7 | 23.9 | 35.9 | 15.0 | |
| Education, % | <0.001 | |||||
| Less than high school degree | 10.1 | 19.0 | 23.8 | 34.2 | 12.9 | |
| High school degree | 7.7 | 20.1 | 28.5 | 34.2 | 9.6 | |
| Some college | 8.6 | 22.0 | 31.0 | 30.8 | 7.6 | |
| College degree or higher | 5.1 | 20.2 | 38.2 | 31.4 | 5.1 | |
| Family income, mean $ | 36,819 | 43,869 | 48,065 | 42,907 | 34,883 | <0.001 |
| Family income portfolio, mean score | 1.01 | 1.11 | 1.20 | 1.15 | 1.15 | <0.001 |
| Health behaviors | ||||||
| Physical activity index, mean | −0.01 | 0.05 | 0.12 | 0.02 | −0.15 | <0.001 |
| Smoking status | <0.001 | |||||
| Current smoker, mean packs smoked/day | 0.25 | 0.17 | 0.12 | 0.12 | 0.16 | |
| Former smoker, % | 7.2 | 20.5 | 30.5 | 32.0 | 9.9 | |
| Never smoker, % | 6.6 | 19.5 | 32.3 | 34.0 | 7.6 | |
| Drinks consumed last week, mean | 2.72 | 2.53 | 2.38 | 2.27 | 2.37 | 0.042 |
| Days binge drank last year, mean | 10.6 | 8.5 | 6.9 | 7.0 | 8.5 | 0.005 |
| Health status | ||||||
| Cardiovascular disease, % | <0.001 | |||||
| No | 6.6 | 20.1 | 32.7 | 33.5 | 7.2 | |
| Yes | 10.4 | 21.2 | 26.8 | 30.4 | 11.3 | |
| Acute respiratory condition, % | <0.001 | |||||
| No | 7.1 | 20.0 | 31.4 | 33.2 | 8.3 | |
| Yes | 11.7 | 22.9 | 27.2 | 28.7 | 9.6 | |
| Chronic respiratory condition, % | <0.001 | |||||
| No | 7.2 | 20.2 | 31.4 | 33.1 | 8.2 | |
| Yes | 12.3 | 22.2 | 26.8 | 28.1 | 10.6 | |
| Diabetes, % | <0.001 | |||||
| No | 7.4 | 20.5 | 31.5 | 32.6 | 8.0 | |
| Yes | 11.4 | 20.5 | 23.5 | 31.2 | 13.4 | |
| Pain, % | <0.001 | |||||
| No | 5.2 | 18.5 | 32.5 | 35.7 | 8.0 | |
| Yes | 11.9 | 23.7 | 28.0 | 27.2 | 9.3 | |
| Depression index, mean | 0.5 | 0.0 | −0.2 | −0.2 | 0.3 | <0.001 |
| Anxiety index, mean | 0.5 | 0.1 | −0.1 | −0.2 | 0.1 | <0.001 |
| Body mass, % | <0.001 | |||||
| Obese | 10.6 | 23.5 | 28.1 | 29.0 | 8.9 | |
| Overweight | 7.6 | 20.2 | 31.9 | 32.7 | 7.8 | |
| Normal weight | 6.1 | 18.8 | 32.1 | 34.5 | 8.6 | |
| Underweight | 7.7 | 17.7 | 23.5 | 36.7 | 14.5 | |
| Activity limitations, % | <0.001 | |||||
| No | 6.6 | 20.8 | 32.9 | 33.2 | 6.6 | |
| Yes | 14.2 | 18.8 | 19.2 | 28.8 | 19.1 | |
Unweighted N = 110,441.
Significant P values indicate that the distribution of a given covariate differs across sleep duration. The authors used Wald tests that account for the complex sampling frame used by the National Health Interview Survey.
Working 41 or more hours is associated with short sleep, and not working is associated with long sleep. Higher levels of education, family income, and the family income portfolio are associated with midrange sleep hours. Respondents who sleep 7 hours per night have high levels of physical activity and low levels of current smoking, consumed 2.4 drinks in the prior week, and binge drank on 6.9 days in the last year. Those who report any of the medical conditions, higher levels of depression or anxiety, being obese or underweight, or activity limitations are more likely to report long or short sleep.
Model 1 (Table 2) presents odds ratios for the demographic variables and shows that males have reduced odds of sleeping 5 or fewer hours or 8 or more hours. Relative to non-Hispanic whites, non-Hispanic blacks are more likely to report both short and long sleep hours, but Mexican Americans have similar odds of sleeping 5 or fewer hours and higher odds of sleeping 8 or more hours. Foreign-born individuals have reduced odds of sleeping 6 or fewer hours or 9 or more hours.
Table 2.
Odds Ratios and 95% Confidence Intervals From Multinomial Logistic Regression for the Relation Between the Covariates and Self-reported Sleep Hours in a Usual 24-Hour Period, US Adults Aged 18 Years or Older, 2004–2007a
| Self-reported Sleep Hours |
P Valueb | ||||||||
| ≤5 vs. 7 |
6 vs. 7 |
8 vs. 7 |
≥9 vs. 7 |
||||||
| Odds Ratio | 95% Confidence Interval | Odds Ratio | 95% Confidence Interval | Odds Ratio | 95% Confidence Interval | Odds Ratio | 95% Confidence Interval | ||
| Model 1: demographic status variablesc | |||||||||
| Demographic status | |||||||||
| Male | 0.93** | 0.88, 0.98 | 1.00 | 0.96, 1.04 | 0.90*** | 0.86, 0.93 | 0.84*** | 0.79, 0.89 | <0.001 |
| Race/ethnicity | <0.001 | ||||||||
| Non-Hispanic white | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| Non-Hispanic black | 2.00*** | 1.84, 2.17 | 1.54*** | 1.44, 1.65 | 1.23*** | 1.16, 1.31 | 1.72*** | 1.59, 1.87 | |
| Other non-Hispanic | 1.39*** | 1.19, 1.63 | 1.27*** | 1.15, 1.42 | 1.03 | 0.92, 1.15 | 1.15 | 0.97, 1.37 | |
| Mexican American | 1.09 | 0.97, 1.23 | 1.10* | 1.00, 1.20 | 1.48*** | 1.38, 1.58 | 1.70*** | 1.52, 1.89 | |
| Other Hispanic | 1.63*** | 1.42, 1.87 | 1.24*** | 1.12, 1.38 | 1.06 | 0.97, 1.16 | 1.07 | 0.92, 1.24 | |
| Foreign born | 0.70*** | 0.63, 0.78 | 0.82*** | 0.77, 0.89 | 1.02 | 0.96, 1.09 | 0.78*** | 0.70, 0.87 | <0.001 |
| Model 2: family structure and socioeconomic status, adjusted for demographic status variablesc | |||||||||
| Family structure | |||||||||
| Any children | <0.001 | ||||||||
| No children | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| >0–<2 years | 1.34*** | 1.18, 1.51 | 1.28*** | 1.18, 1.39 | 0.80*** | 0.73, 0.87 | 0.72*** | 0.63, 0.82 | |
| 2–<6 years | 1.06 | 0.96, 1.18 | 1.07 | 0.99, 1.15 | 0.87*** | 0.82, 0.93 | 0.76*** | 0.68, 0.85 | |
| 6–<13 years | 0.95 | 0.87, 1.03 | 0.97 | 0.91, 1.03 | 0.86*** | 0.81, 0.90 | 0.85** | 0.77, 0.94 | |
| 13–<18 years | 1.00 | 0.91, 1.10 | 1.00 | 0.93, 1.06 | 0.90*** | 0.84, 0.95 | 0.78*** | 0.70, 0.88 | |
| Currently pregnant | 0.94 | 0.66, 1.34 | 0.88 | 0.69, 1.11 | 1.77*** | 1.49, 2.10 | 3.65*** | 2.96, 4.49 | <0.001 |
| Currently married | 0.76*** | 0.71, 0.81 | 0.86*** | 0.82, 0.90 | 1.07** | 1.02, 1.11 | 0.94 | 0.88, 1.00 | <0.001 |
| Socioeconomic status | |||||||||
| Hours worked per week | <0.001 | ||||||||
| ≥41 | 1.40*** | 1.24, 1.58 | 1.31*** | 1.20, 1.42 | 0.66*** | 0.61, 0.71 | 0.41*** | 0.36, 0.47 | |
| 35–40 | 0.81*** | 0.72, 0.90 | 0.97 | 0.90, 1.05 | 0.83*** | 0.78, 0.89 | 0.53*** | 0.47, 0.59 | |
| 1–34 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| Not working | 1.33*** | 1.19, 1.48 | 1.02 | 0.94, 1.11 | 1.19*** | 1.10, 1.27 | 1.74*** | 1.58, 1.93 | |
| Education | <0.001 | ||||||||
| Less than high school degree | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| High school degree | 0.71*** | 0.65, 0.77 | 0.90** | 0.84, 0.96 | 0.95 | 0.89, 1.01 | 0.79*** | 0.73, 0.86 | |
| Some college | 0.78*** | 0.71, 0.85 | 0.92* | 0.86, 0.99 | 0.81*** | 0.76, 0.86 | 0.62*** | 0.56, 0.68 | |
| College degree or higher | 0.43*** | 0.38, 0.48 | 0.72*** | 0.66, 0.77 | 0.76*** | 0.71, 0.81 | 0.46*** | 0.41, 0.51 | |
| Ln(family income/10,000) | 0.77*** | 0.73, 0.80 | 0.91*** | 0.88, 0.95 | 0.97 | 0.94, 1.00 | 0.90*** | 0.86, 0.94 | <0.001 |
| Family income portfolio | 0.88*** | 0.85, 0.92 | 0.93*** | 0.90, 0.96 | 0.94*** | 0.92, 0.97 | 0.96* | 0.92, 0.99 | <0.001 |
| Model 3: health behaviors, adjusted for demographic status, family structure, and socioeconomic status variablescd | |||||||||
| Health behaviors | |||||||||
| Physical activity index | 1.01 | 0.98, 1.05 | 0.98 | 0.96, 1.00 | 0.96*** | 0.94, 0.98 | 0.86*** | 0.83, 0.89 | <0.001 |
| Smoking status | <0.001 | ||||||||
| Current packs smoked | 1.74*** | 1.60, 1.89 | 1.34*** | 1.26, 1.43 | 0.99 | 0.94, 1.06 | 1.45*** | 1.32, 1.59 | |
| Former smoker | 1.09* | 1.01, 1.18 | 1.12*** | 1.06, 1.18 | 0.99 | 0.94, 1.04 | 1.26*** | 1.17, 1.35 | |
| Never smoker | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| Ln(≥1 days that binge drank) | 1.09*** | 1.05, 1.14 | 1.04** | 1.02, 1.07 | 0.97 | 0.94, 1.00 | 1.02 | 0.98, 1.06 | 0.003 |
| Model 4: health status, adjusted for demographic status, family structure, socioeconomic status, and health behavior variablescd | |||||||||
| Health status | |||||||||
| Cardiovascular disease | 1.24*** | 1.16, 1.33 | 1.11*** | 1.05, 1.17 | 0.98 | 0.94, 1.03 | 1.11* | 1.03, 1.19 | <0.001 |
| Acute respiratory condition | 1.21*** | 1.12, 1.30 | 1.11** | 1.05, 1.18 | 1.02 | 0.97, 1.08 | 1.05 | 0.97, 1.14 | <0.001 |
| Chronic respiratory condition | 1.25*** | 1.14, 1.36 | 1.08 | 1.00, 1.16 | 0.98 | 0.92, 1.04 | 1.05 | 0.96, 1.15 | <0.001 |
| Diabetes | 1.19** | 1.07, 1.33 | 1.09* | 1.01, 1.19 | 1.12** | 1.03, 1.20 | 1.25*** | 1.13, 1.38 | 0.002 |
| Pain | 1.69*** | 1.57, 1.81 | 1.29*** | 1.22, 1.35 | 0.89*** | 0.85, 0.93 | 0.97 | 0.90, 1.04 | <0.001 |
| Depression index | 1.23*** | 1.18, 1.27 | 1.09*** | 1.06, 1.13 | 1.03 | 1.00, 1.06 | 1.30*** | 1.25, 1.35 | <0.001 |
| Anxiety index | 1.22*** | 1.18, 1.27 | 1.10*** | 1.07, 1.13 | 0.89*** | 0.87, 0.92 | 0.93** | 0.89, 0.97 | <0.001 |
| Body mass | <0.001 | ||||||||
| Obese | 1.39*** | 1.29, 1.51 | 1.23*** | 1.16, 1.30 | 0.96 | 0.91, 1.02 | 1.07 | 0.99, 1.16 | |
| Overweight | 1.18*** | 1.10, 1.27 | 1.04 | 0.99, 1.10 | 0.99 | 0.95, 1.03 | 1.00 | 0.93, 1.08 | |
| Normal weight | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| Underweight | 1.37* | 1.03, 1.84 | 1.19 | 0.98, 1.45 | 1.29** | 1.11, 1.50 | 1.51*** | 1.24, 1.84 | |
| Activity limitations | 1.59*** | 1.46, 1.73 | 1.13** | 1.05, 1.21 | 1.21*** | 1.13, 1.29 | 2.22*** | 2.04, 2.42 | <0.001 |
* P < 0.05; **P < 0.01; ***P < 0.001 (2-tailed tests).
Unweighted N = 110,441.
P values come from Wald tests of the joint significance of the coefficients across all categories of the dependent variable.
All models use cubic splines to adjust for age in years, with knots at ages 35, 50, and 65 (refer to Figure 1).
All models that include the health behaviors also adjust for the number of drinks consumed in the last week, raised to the powers of 0.5 and 1 (refer to Figure 2).
Figure 1 shows the relation between age and sleep duration from model 1 while holding the other covariates at their means; 7 hours of sleep is the baseline category with the logged odds of 0. The logged odds of sleeping 6 or fewer hours increase in early adulthood, level off in midlife, and then increase at the older ages. However, the logged odds of sleeping 8 or more hours are highest among the youngest and oldest individuals and lowest among those aged 45 years.
Figure 1.
Logged odds and 95% confidence intervals for the relation between age and sleep hours, from model 1, Table 2, holding all other covariates at their means, US adults aged 18 years or older, 2004–2007.
Model 2 (Table 2) shows odds ratios for the family structure and socioeconomic variables, after adjustment for demographic status. Compared with those not living with children, parents of children aged from birth to less than 2 years have 34% higher odds of sleeping 5 or fewer hours and 28% lower odds of sleeping 9 or more hours. Living with children aged from 2 to less than 18 years is also associated with lower odds of long sleep. Because women are coded as “0” on the variable for sex, the odds ratio for pregnancy status contrasts pregnant women with nonpregnant women. Compared with nonpregnant women, pregnant women are 77% more likely to sleep 8 hours and 3.7 times as likely to sleep 9 or more hours. Married individuals have lower odds of short sleep.
Compared with those who work 1–34 hours, those who work 41 or more hours are 40% more likely to sleep 5 or fewer hours and 59% less likely to sleep 9 or more hours. Yet, those who are not working have increased odds of both short and long sleep. High levels of education or income or additional sources of income per family member are associated with lower odds of short or long sleep.
Model 3 shows odds ratios for the health behaviors, after adjustment for demographic, family structure, and socioeconomic variables. A 1-standard-deviation increase in the physical activity index is associated with 14% lower odds of sleeping 9 or more hours. Compared with never smokers, current smokers had, for each additional pack smoked, 74% higher odds of sleeping 5 or fewer hours and 45% higher odds of sleeping 9 or more hours. Former smokers also have increased odds of short and long sleep. Binge drinking more days per year is associated with higher odds of sleeping 6 or fewer hours.
Figure 2 graphs the logged odds for the number of drinks consumed in the last week, from model 2, holding all other covariates at their means. The wide confidence intervals at high levels of alcohol consumption result from the relatively few respondents who drink that much. Alcohol consumption has a J-shaped relation with the logged odds of sleeping 6 or fewer hours, or 9 or more hours, with the lowest logged odds among those who consume 6–12 drinks per week. The logged odds of sleeping 8 hours increase fairly linearly with increasing alcohol consumption.
Figure 2.
Logged odds and 95% confidence intervals for the relation between the number of drinks consumed and sleep hours, from model 3, Table 2, holding all other covariates at their means, US adults aged 18 years or older, 2004–2007.
Model 4 shows that cardiovascular disease, acute or chronic respiratory conditions, diabetes, pain, anxiety, depression, obesity, overweight, underweight, and activity limitations are associated with increased odds of short sleep, after adjustment for demographic, family structure, socioeconomic, and health behavior variables. Cardiovascular disease, diabetes, depression, underweight, and activity limitations are positively associated with long sleep, but high levels of anxiety are associated with lower odds of long sleep.
Table 3 presents the full results from model 4 (Table 2). In the fully adjusted model, race/ethnic differences remain substantial, but sex differences are no longer significant and foreign-born respondents no longer have reduced odds of sleeping 5 or fewer hours (compare with Table 2). Consistent with the notion that family structure and socioeconomic variables may shape sleep through health behaviors and health status, nonworking individuals no longer have increased odds of short sleep, and the odds ratios for education, family income, and the family income portfolio are closer to 0 after adjustment for health behaviors and health status. Further, after adjustment for health status, low levels of exercise are positively associated with short sleep, the odds ratios for current or former smoking are closer to 0, and binge drinking is no longer jointly significant across the sleep hours at the P ≤ 0.05 level.
Table 3.
Odds Ratios and 95% Confidence Intervals From Multinomial Logistic Regression for the Relation Between the Covariates and Self-reported Sleep Hours in a Usual 24-Hour Period, US Adults Aged 18 Years or Older, 2004–2007ab
| Self-reported Sleep Hours |
P Valuec | ||||||||
| ≤5 vs. 7 |
6 vs. 7 |
8 vs. 7 |
≥9 vs. 7 |
||||||
| Odds Ratio | 95% Confidence Interval | Odds Ratio | 95% Confidence Interval | Odds Ratio | 95% Confidence Interval | Odds Ratio | 95% Confidence Interval | ||
| Demographic status | |||||||||
| Male | 1.03 | 0.96, 1.10 | 1.00 | 0.95, 1.04 | 0.96 | 0.92, 1.01 | 1.00 | 0.94, 1.07 | 0.357 |
| Race/ethnicity | <0.001 | ||||||||
| Non-Hispanic white | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| Non-Hispanic black | 1.78*** | 1.62, 1.96 | 1.47*** | 1.37, 1.59 | 1.12** | 1.05, 1.19 | 1.46*** | 1.33, 1.59 | |
| Other non-Hispanic | 1.54*** | 1.30, 1.82 | 1.37*** | 1.23, 1.52 | 0.99 | 0.88, 1.10 | 1.13 | 0.95, 1.34 | |
| Mexican American | 0.86* | 0.76, 0.98 | 1.00 | 0.91, 1.11 | 1.31*** | 1.22, 1.41 | 1.42*** | 1.27, 1.60 | |
| Other Hispanic | 1.31*** | 1.13, 1.52 | 1.15* | 1.03, 1.29 | 0.98 | 0.90, 1.08 | 0.91 | 0.78, 1.07 | |
| Foreign born | 0.91 | 0.82, 1.01 | 0.92* | 0.85, 0.99 | 0.98 | 0.91, 1.05 | 0.85** | 0.76, 0.95 | 0.023 |
| Family structure | |||||||||
| Any children | <0.001 | ||||||||
| No children | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| >0–<2 years | 1.41*** | 1.24, 1.60 | 1.29*** | 1.18, 1.40 | 0.79*** | 0.73, 0.86 | 0.73*** | 0.64, 0.84 | |
| 2–<6 years | 1.12* | 1.01, 1.23 | 1.08 | 1.00, 1.16 | 0.87*** | 0.82, 0.93 | 0.80*** | 0.72, 0.89 | |
| 6–<13 years | 1.00 | 0.92, 1.09 | 0.98 | 0.92, 1.04 | 0.86*** | 0.82, 0.91 | 0.90 | 0.82, 1.00 | |
| 13–<18 years | 1.06 | 0.96, 1.16 | 1.01 | 0.94, 1.08 | 0.90** | 0.85, 0.96 | 0.83** | 0.74, 0.93 | |
| Currently pregnant | 0.95 | 0.66, 1.36 | 0.85 | 0.68, 1.08 | 1.76*** | 1.48, 2.09 | 3.48*** | 2.83, 4.28 | <0.001 |
| Currently married | 0.84*** | 0.79, 0.90 | 0.89*** | 0.85, 0.93 | 1.07** | 1.02, 1.12 | 1.03 | 0.97, 1.10 | <0.001 |
| Socioeconomic status | |||||||||
| Hours worked per week | <0.001 | ||||||||
| ≥41 | 1.52*** | 1.34, 1.72 | 1.32*** | 1.21, 1.43 | 0.66*** | 0.61, 0.71 | 0.45*** | 0.39, 0.51 | |
| 35–40 | 0.93 | 0.83, 1.04 | 1.01 | 0.94, 1.09 | 0.82*** | 0.77, 0.88 | 0.57*** | 0.51, 0.63 | |
| 1–34 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| Not working | 1.02 | 0.91, 1.14 | 0.94 | 0.87, 1.03 | 1.17*** | 1.09, 1.26 | 1.49*** | 1.34, 1.65 | |
| Education | <0.001 | ||||||||
| Less than high school degree | |||||||||
| High school degree | 0.87** | 0.79, 0.95 | 0.97 | 0.91, 1.04 | 0.95 | 0.89, 1.01 | 0.88** | 0.81, 0.96 | |
| Some college | 0.93 | 0.84, 1.02 | 1.00 | 0.93, 1.07 | 0.82*** | 0.77, 0.87 | 0.71*** | 0.65, 0.78 | |
| College degree or higher | 0.60*** | 0.53, 0.68 | 0.84*** | 0.77, 0.91 | 0.76*** | 0.71, 0.82 | 0.58*** | 0.52, 0.65 | |
| Ln(family income/10,000) | 0.89*** | 0.85, 0.93 | 0.97 | 0.93, 1.00 | 0.98 | 0.95, 1.01 | 0.99 | 0.94, 1.03 | <0.001 |
| Family income portfolio | 0.91*** | 0.87, 0.95 | 0.93*** | 0.90, 0.96 | 0.96** | 0.93, 0.98 | 1.01 | 0.97, 1.05 | <0.001 |
| Health behaviors | |||||||||
| Physical activity index | 1.05** | 1.02, 1.09 | 0.99 | 0.97, 1.02 | 0.96*** | 0.94, 0.98 | 0.90*** | 0.87, 0.93 | <0.001 |
| Smoking status | <0.001 | ||||||||
| Current packs smoked | 1.46*** | 1.34, 1.59 | 1.25*** | 1.17, 1.34 | 1.02 | 0.96, 1.08 | 1.32*** | 1.20, 1.45 | |
| Former smoker | 0.93 | 0.85, 1.00 | 1.05 | 0.99, 1.11 | 1.01 | 0.96, 1.06 | 1.17*** | 1.09, 1.25 | |
| Never smoker | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| Ln(≥1 days that binge drank) | 1.05* | 1.01, 1.09 | 1.02 | 1.00, 1.05 | 0.98 | 0.95, 1.01 | 1.01 | 0.97, 1.05 | 0.052 |
| Health status | |||||||||
| Cardiovascular disease | 1.24*** | 1.16, 1.33 | 1.11*** | 1.05, 1.17 | 0.98 | 0.94, 1.03 | 1.11* | 1.03, 1.19 | <0.001 |
| Acute respiratory condition | 1.21*** | 1.12, 1.30 | 1.11** | 1.05, 1.18 | 1.02 | 0.97, 1.08 | 1.05 | 0.97, 1.14 | <0.001 |
| Chronic respiratory condition | 1.25*** | 1.14, 1.36 | 1.08 | 1.00, 1.16 | 0.98 | 0.92, 1.04 | 1.05 | 0.96, 1.15 | <0.001 |
| Diabetes | 1.19** | 1.07, 1.33 | 1.09* | 1.01, 1.19 | 1.12** | 1.03, 1.20 | 1.25*** | 1.13, 1.38 | 0.002 |
| Pain | 1.69*** | 1.57, 1.81 | 1.29*** | 1.22, 1.35 | 0.89*** | 0.85, 0.93 | 0.97 | 0.90, 1.04 | <0.001 |
| Depression index | 1.23*** | 1.18, 1.27 | 1.09*** | 1.06, 1.13 | 1.03 | 1.00, 1.06 | 1.30*** | 1.25, 1.35 | <0.001 |
| Anxiety index | 1.22*** | 1.18, 1.27 | 1.10*** | 1.07, 1.13 | 0.89*** | 0.87, 0.92 | 0.93** | 0.89, 0.97 | <0.001 |
| Body mass | <0.001 | ||||||||
| Obese | 1.39*** | 1.29, 1.51 | 1.23*** | 1.16, 1.30 | 0.96 | 0.91, 1.02 | 1.07 | 0.99, 1.16 | |
| Overweight | 1.18*** | 1.10, 1.27 | 1.04 | 0.99, 1.10 | 0.99 | 0.95, 1.03 | 1.00 | 0.93, 1.08 | |
| Normal weight | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| Underweight | 1.37* | 1.03, 1.84 | 1.19 | 0.98, 1.45 | 1.29** | 1.11, 1.50 | 1.51*** | 1.24, 1.84 | |
| Activity limitations | 1.59*** | 1.46, 1.73 | 1.13** | 1.05, 1.21 | 1.21*** | 1.13, 1.29 | 2.22*** | 2.04, 2.42 | <0.001 |
* P < 0.05; **P < 0.01; ***P < 0.001 (2-tailed tests).
Unweighted N = 110,441.
This model used cubic splines to adjust for age in years, with knots at ages 35, 50, and 65. This model also adjusts for the number of drinks consumed in the last week, raised to the powers of 0.5 and 1.
P values come from Wald tests of the joint significance of the coefficients across all categories of the dependent variable.
DISCUSSION
Long or short sleep is common: 28.3% of adults sleep 6 or fewer hours, and 8.5% sleep 9 or more hours. Table 2 shows strong and persistent relations between sleep duration and demographic, family structure, socioeconomic, health behavior, and health status variables. The physical and mental health variables are associated with sleep duration in a sample of noninstitutionalized (and thus relatively healthy) adults, but Table 3 demonstrates that poor health does not account for the relation between sleep and the other variables.
We find important differences in the predictors of short and long sleep, a finding that could not have emerged from research that models sleep duration as a continuous variable (43, 44, 50) or that combines those with short and long sleep (17, 20). Consistent with prior research findings, our results show that non-Hispanic black race/ethnicity (23), low levels of socioeconomic status (7, 35), depression (6, 7), and cardiovascular disease and diabetes (1, 2) are associated with both long and short sleep duration. Older ages (7, 20, 21), current smoking and former smoking, and alcohol consumption (19, 36, 38, 39) are associated with short sleep in prior work, but they are also associated with long sleep in our data, as are US-born status, underweight, and activity limitations. Young children, being unmarried (19, 26), working long hours (11, 27, 28), overweight and obesity (3–5), and measures of poor health (13, 14, 16, 20, 37, 38, 40) including acute and chronic respiratory conditions, pain, and anxiety increase the odds of short sleep and have a null or inverse association with long sleep. Conversely, some variables are associated with increased odds of long sleep and have null or inverse relations with short sleep, including being younger, Mexican American (23), or pregnant (31). Contrary to prior research, our research did not find that women report shorter sleep than men do (22) after adjustment for other variables.
Many of our covariates have established relations with the risk of death (25, 65) and might account for the relation between sleep duration and mortality (13–18). Prior studies have shown that those who sleep 8 hours have 12%–35% increased risks of death compared with those who sleep 7 hours (14, 16–18), findings that might result from differences in race/ethnicity, the presence of children, pregnancy status, work hours, education, physical activity, alcohol consumption, or health status variables that differ among those sleeping 7 or 8 hours in our data but that prior research has not been able to include. Working 35–40 hours, chronic respiratory conditions, or being overweight or underweight is associated with the odds of sleeping 5 or fewer hours but not of sleeping 6 hours. Thus, the possible confounders of the sleep-mortality relation may differ across very short, short, and long sleep.
Our analyses have 3 major strengths. First, we use a large, current, nationally representative, population-based sample of noninstitutionalized US adults. Second, we extend the findings from prior community-based studies (1, 6, 7, 20, 22, 23, 26–28, 33, 37, 42–49), by examining a detailed measure of sleep duration, presenting results from a richer array of social, economic, and behavioral variables, and allowing our covariates to have different relations with long and short sleep hours. Third, we use multiple imputation methods that rely on more plausible assumptions than do other methods of dealing with missing data (59, 62).
Three limitations warrant mention. First, our data ask only about self-reported sleep duration and provide no information on daytime sleepiness or difficulty with falling or staying asleep. Some surveys collect objective sleep data (43), but those measures are unavailable for large, nationally representative samples. Further, self-reported sleep duration reliably predicts prospective mortality and other health outcomes (1–7, 13–18). Second, our data do not provide clinical measures of mental health or medical conditions or information on shift work, caffeine consumption, or medication usage, although our measures of mental health were validated previously (56), and we include conditions that may prompt respondents to visit their doctors and that are easily assessed in clinical settings. Given the numerous medications used by US adults and their myriad effects on sleep (66, 67), it is difficult to speculate about how our lack of information on medication usage might bias our results. Third, although there are sound theoretical reasons for treating our covariates as potential determinants of sleep duration and, thus, as potential confounders of the sleep-mortality relation, our cross-sectional data preclude the identification of causal relations.
Despite the high prevalence of long and short sleep durations and the established relation between sleep hours and adverse health outcomes, prior research has offered little insight into sleep patterns in the US population. There is substantial research on pharmaceutical treatments for short or disturbed sleep, but our findings suggest that numerous demographic, family structure, socioeconomic, and health behavior factors might also shape sleep duration, even in the noninstitutionalized and relatively healthy US population, and after adjustment for physical and mental health. Our results suggest the need for research that more completely adjusts for social, economic, and behavioral factors when modeling the relation between sleep and other health or mortality outcomes.
Acknowledgments
Author affiliations: School of Public Health, University of Texas, Houston, Texas (Patrick M. Krueger); Population Research Center, University of Texas, Austin, Texas (Patrick M. Krueger); Leonard Davis Institute of Health Economics, University of Pennsylvania, Philadelphia, Pennsylvania (Patrick M. Krueger); Population Program, University of Colorado, Boulder, Colorado (Patrick M. Krueger); Institute on Aging, University of Wisconsin, Madison, Wisconsin (Elliot M. Friedman); and Department of Population Health Sciences, University of Wisconsin, Madison, Wisconsin (Elliot M. Friedman).
The authors acknowledge administrative support from the Robert Wood Johnson Foundation Health & Society Scholars Program at the University of Pennsylvania (P. M. K.) and the University of Wisconsin (E. M. F.); the University of Texas Population Research Center (The Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) grant R24 HD42849); and the University of Colorado Population Program (NICHD grant R21 HD51146). The National Institute on Aging provided research support (grant 1K01-AG29381-01A1 to E. M. F.).
The authors thank Dr. Richard G. Rogers for insightful comments on an earlier version of this paper. They also received many helpful suggestions when presenting an earlier version of this work to the 2008 meeting of the Robert Wood Johnson Foundation Health & Society Scholars in San Antonio, Texas.
Conflict of interest: none declared.
Glossary
Abbreviations
- BMI
body mass index
- NHIS-SAF
National Health Interview Survey-Sample Adult Files
References
- 1.Gottlieb DJ, Redline S, Nieto FJ, et al. Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep. 2006;29(8):1009–1014. doi: 10.1093/sleep/29.8.1009. [DOI] [PubMed] [Google Scholar]
- 2.Gottlieb DJ, Punjabi NM, Newman AB, et al. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med. 2005;165(8):863–867. doi: 10.1001/archinte.165.8.863. [DOI] [PubMed] [Google Scholar]
- 3.Gangwisch JE, Malaspina D, Boden-Albala B, et al. Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep. 2005;28(10):1289–1296. doi: 10.1093/sleep/28.10.1289. [DOI] [PubMed] [Google Scholar]
- 4.Hasler G, Buysse DJ, Klaghofer R, et al. The association between short sleep duration and obesity in young adults: a 13-year prospective study. Sleep. 2004;27(4):661–666. doi: 10.1093/sleep/27.4.661. [DOI] [PubMed] [Google Scholar]
- 5.Singh M, Drake CL, Roehrs T, et al. The association between obesity and short sleep duration: a population-based study. J Clin Sleep Med. 2005;1(4):357–363. [PubMed] [Google Scholar]
- 6.Newman AB, Enright PL, Manolio TA, et al. Sleep disturbance, psychosocial correlates, and cardiovascular disease in 5201 older adults: the Cardiovascular Health Study. J Am Geriatr Soc. 1997;45(1):1–7. doi: 10.1111/j.1532-5415.1997.tb00970.x. [DOI] [PubMed] [Google Scholar]
- 7.Patel SR, Malhotra A, Gottlieb DJ, et al. Correlates of long sleep duration. Sleep. 2006;29(7):881–889. doi: 10.1093/sleep/29.7.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pack AI, Maislin G, Staley B, et al. Impaired performance in commercial drivers: role of sleep apnea and short sleep duration. Am J Respir Crit Care Med. 2006;174(4):446–454. doi: 10.1164/rccm.200408-1146OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Terán-Santos J, Jiménex-Gómez A, Cordero-Guevara J. The association between sleep apnea and the risk of traffic accidents. N Engl J Med. 1999;340(11):847–851. doi: 10.1056/NEJM199903183401104. [DOI] [PubMed] [Google Scholar]
- 10.Connor J, Norton R, Ameratunga S, et al. Driver sleepiness and risk of serious injury to car occupants: population based control study. BMJ. 2002;324(7346):1125–1130. doi: 10.1136/bmj.324.7346.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lockley SW, Cronin JW, Evans EE, et al. Effect of reducing intern's weekly work hours on sleep and attentional failures. N Engl J Med. 2004;351(18):1829–1837. doi: 10.1056/NEJMoa041404. [DOI] [PubMed] [Google Scholar]
- 12.Stickgold R, Hobson JA, Fosse R, et al. Sleep, learning, dreams: off-line memory reprocessing. Science. 2001;294(5544):1052–1057. doi: 10.1126/science.1063530. [DOI] [PubMed] [Google Scholar]
- 13.Kojima M, Wakai K, Kawamura T, et al. Sleep patterns and total mortality: a 12-year follow-up study in Japan. J Epidemiol. 2000;10(2):87–93. doi: 10.2188/jea.10.87. [DOI] [PubMed] [Google Scholar]
- 14.Kripke DF, Garfinkel L, Wingard DL, et al. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59(2):131–136. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 15.Sekine M, Chandola T, Martikainen P, et al. Explaining social inequalities in health by sleep: the Japanese civil servants study. J Public Health (Oxf) 2006;28(1):63–70. doi: 10.1093/pubmed/fdi067. [DOI] [PubMed] [Google Scholar]
- 16.Tamakoshi A, Ohno Y. Self-reported sleep duration as a predictor of all-cause mortality: results from the JACC study, Japan. Sleep. 2004;27(1):51–54. [PubMed] [Google Scholar]
- 17.Wingard DL, Berkman LF. Mortality risk associated with sleeping patterns among adults. Sleep. 1983;6(2):102–107. doi: 10.1093/sleep/6.2.102. [DOI] [PubMed] [Google Scholar]
- 18.Patel SR, Ayas NT, Malhotra MR, et al. A prospective study of sleep duration and mortality risk in women. Sleep. 2004;27(3):440–444. doi: 10.1093/sleep/27.3.440. [DOI] [PubMed] [Google Scholar]
- 19.Ferrie JE, Shipley MJ, Cappuccio FP, et al. A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Sleep. 2007;30(12):1659–1666. doi: 10.1093/sleep/30.12.1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Adams J. Socioeconomic position and sleep quantity in UK adults. J Epidemiol Community Health. 2006;60(3):267–269. doi: 10.1136/jech.2005.039552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hale L. Who has time to sleep? J Public Health (Oxf) 2005;27(2):205–211. doi: 10.1093/pubmed/fdi004. [DOI] [PubMed] [Google Scholar]
- 22.Moore PJ, Adler NE, Williams DR, et al. Socioeconomic status and health: the role of sleep. Psychosom Med. 2002;64(2):337–344. doi: 10.1097/00006842-200203000-00018. [DOI] [PubMed] [Google Scholar]
- 23.Hale L, Phuong Do D. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30(9):1096–1103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Antecol H, Bedard K. Unhealthy assimilation: why do immigrants converge to American health status levels? Demography. 2006;43(2):337–360. doi: 10.1353/dem.2006.0011. [DOI] [PubMed] [Google Scholar]
- 25.Rogers RG, Hummer RA, Nam C. Living and Dying in the USA: Behavioral, Health, and Social Differentials of Adult Mortality. San Diego, CA: Academic Press; 2000. [Google Scholar]
- 26.Friedman EM, Hayney MS, Love GD, et al. Social relationships, sleep quality, and interleukin-6 in aging women. Proc Natl Acad Sci U S A. 2005;102(51):18757–18762. doi: 10.1073/pnas.0509281102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Takahashi M, Nakata A, Haratani T, et al. Psychosocial work characteristics predicting daytime sleepiness in day and shift workers. Chronobiol Int. 2006;23(6):1409–1422. doi: 10.1080/07420520601100963. [DOI] [PubMed] [Google Scholar]
- 28.Scott LD, Hwang WT, Rogers AE, et al. The relationship between nurse work schedules, sleep duration, and drowsy driving. Sleep. 2007;30(12):1801–1807. doi: 10.1093/sleep/30.12.1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Umberson D. Family status and health behaviors: social control as a dimension of social integration. J Health Soc Behav. 1987;28(3):306–319. [PubMed] [Google Scholar]
- 30.Armstrong EM. Conceiving Risk, Bearing Responsibility: Fetal Alcohol Syndrome and the Diagnosis of Moral Disorder. Baltimore, MD: Johns Hopkins University Press; 2003. [Google Scholar]
- 31.Lee KA, Zaffke ME, McEnany G. Parity and sleep patterns during and after pregnancy. Obstet Gynecol. 2000;95(1):14–18. doi: 10.1016/s0029-7844(99)00486-x. [DOI] [PubMed] [Google Scholar]
- 32.Mirowsky J, Ross CE. Education, Social Status, and Health. Hawthorne, NY: Aldine De Gruyter; 2003. [Google Scholar]
- 33.Bjorvatn B, Sagen IM, Oyane N, et al. The association between sleep duration, body mass index and metabolic measures in the Hordaland Health Study. J Sleep Res. 2007;16(1):66–76. doi: 10.1111/j.1365-2869.2007.00569.x. [DOI] [PubMed] [Google Scholar]
- 34.Hale L, Do DP. Re: “Objectively measured sleep characteristics among early-middle-aged adults: the CARDIA Study” [letter] Am J Epidemiol. 2007;165(2):231–232. doi: 10.1093/aje/kwk080. [DOI] [PubMed] [Google Scholar]
- 35.Van Cauter E, Spiegel K. Sleep as a mediator of the relationship between socioeconomic status and health: a hypothesis. Ann N Y Acad Sci. 1999;896:254–261. doi: 10.1111/j.1749-6632.1999.tb08120.x. [DOI] [PubMed] [Google Scholar]
- 36.Ohayon MM. Interactions between sleep normative data and sociocultural characteristics in the elderly. J Psychosom Res. 2004;56(5):479–486. doi: 10.1016/j.psychores.2004.04.365. [DOI] [PubMed] [Google Scholar]
- 37.Ohayon MM, Vecchierini MF. Normative sleep data, cognitive function and daily living activities in older adults in the community. Sleep. 2005;28(8):981–989. [PubMed] [Google Scholar]
- 38.Roehrs T, Roth T. Sleep, sleepiness, sleep disorders and alcohol use and abuse. Sleep Med Rev. 2001;5(4):287–297. doi: 10.1053/smrv.2001.0162. [DOI] [PubMed] [Google Scholar]
- 39.Stein MD, Friedmann PD. Disturbed sleep and its relationship to alcohol use. Subst Abus. 2005;26(1):1–13. doi: 10.1300/j465v26n01_01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Roehrs T, Roth T. Sleep and pain: interaction of two vital functions. Semin Neurol. 2005;25(1):106–116. doi: 10.1055/s-2005-867079. [DOI] [PubMed] [Google Scholar]
- 41.Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165(9):1217–1239. doi: 10.1164/rccm.2109080. [DOI] [PubMed] [Google Scholar]
- 42.Foley DJ, Monjan AA, Brown SL, et al. Sleep complaints among elderly persons: an epidemiologic study of three communities. Sleep. 1995;18(6):425–432. doi: 10.1093/sleep/18.6.425. [DOI] [PubMed] [Google Scholar]
- 43.Lauderdale DS, Knutson KL, Yan LL, et al. Objectively measured sleep characteristics among early-middle-aged adults: the CARDIA Study. Am J Epidemiol. 2006;164(1):5–16. doi: 10.1093/aje/kwj199. [DOI] [PubMed] [Google Scholar]
- 44.Ursin R, Bjorvatn B, Holsten F. Sleep duration, subjective sleep need, and sleep habits of 40- to 45-year-olds in the Hordaland Health Study. Sleep. 2005;28(10):1260–1269. doi: 10.1093/sleep/28.10.1260. [DOI] [PubMed] [Google Scholar]
- 45.Phillips BA, Danner FJ. Cigarette smoking and sleep disturbance. Arch Intern Med. 1995;155(7):734–737. [PubMed] [Google Scholar]
- 46.Jefferson CD, Drake CL, Scofield HM, et al. Sleep hygiene practices in a population-based sample of insomniacs. Sleep. 2005;28(5):611–615. doi: 10.1093/sleep/28.5.611. [DOI] [PubMed] [Google Scholar]
- 47.Steptoe A, Peacey V, Wardle J. Sleep duration and health in young adults. Arch Intern Med. 2006;166(16):1689–1692. doi: 10.1001/archinte.166.16.1689. [DOI] [PubMed] [Google Scholar]
- 48.Ayas NT, White DP, Manson JE, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163(2):205–209. doi: 10.1001/archinte.163.2.205. [DOI] [PubMed] [Google Scholar]
- 49.Stranges S, Dorn JM, Shipley MJ, et al. Correlates of short and long sleep duration: a cross-cultural comparison between the United Kingdom and the United States. Am J Epidemiol. 2008;168(12):1353–1364. doi: 10.1093/aje/kwn337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ohayon MM, Carskadon MA, Guilleminault C, et al. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27(7):1255–1273. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- 51.National Center for Health Statistics. Data File Documentation, National Health Interview Survey, 2002–2004 (Machine Readable Data File and Documentation) Hyattsville, MD: National Center for Health Statistics/Centers for Disease Control and Prevention; pp. 2003–2005. [Google Scholar]
- 52.Parker RN, Fenwick R. The Pareto curve and its utility for open-ended income distributions in survey research. Soc Forces. 1983;61(3):873–885. [Google Scholar]
- 53.US Census Bureau. Statistical Abstract of the United States: 2008. 127th ed. Washington, DC: Government Printing Office; 2008. [Google Scholar]
- 54.Van der Gaag J, Smolensky E. True household equivalence scales and characteristics of the poor in the United States. Rev Income Wealth. 1982;28(1):17–28. [Google Scholar]
- 55.Krueger PM, Rogers RG, Hummer RA, et al. Socioeconomic status and age: the effect of income sources and portfolios on adult mortality in the United States. Sociol Forum. 2003;18(3):465–482. [Google Scholar]
- 56.Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 57.Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 1995;854:1–452. [PubMed] [Google Scholar]
- 58.Rogers RG, Hummer RA, Krueger PM. The effect of obesity on overall, circulatory disease, and diabetes-specific mortality. J Biosoc Sci. 2003;35(1):107–129. [PubMed] [Google Scholar]
- 59.Schafer JL. Analysis of Incomplete Multivariate Data. London, United Kingdom: Chapman and Hall; 1997. [Google Scholar]
- 60.Allison PD. Missing Data. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- 61.Royston PM. Multiple imputation of missing values: update. Stata J. 2005;5(2):188–201. [Google Scholar]
- 62.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York, NY: John Wiley & Sons, Inc; 1987. [Google Scholar]
- 63.StataCorp LP. Stata Statistical Software: Release 10.0. College Station, TX: Stata Press; 2007. [Google Scholar]
- 64.Korn EL, Graubard BI. Analysis of Health Surveys. New York, NY: John Wiley & Sons, Inc; 1999. [Google Scholar]
- 65.Berkman LF, Kawachi I. Social Epidemiology. New York, NY: Oxford University Press; 2000. [Google Scholar]
- 66.Ensrud KE, Blackwell TL, Ancoli-Israel S, et al. Use of selective serotonin reuptake inhibitors and sleep disturbances in community-dwelling older women. J Am Geriatr Soc. 2006;54(10):1508–1515. doi: 10.1111/j.1532-5415.2006.00880.x. [DOI] [PubMed] [Google Scholar]
- 67.Hall MH, Muldoon MF, Jennings R, et al. Self-reported sleep duration is associated with the metabolic syndrome in midlife adults. Sleep Med Rev. 2008;31(5):635–643. doi: 10.1093/sleep/31.5.635. [DOI] [PMC free article] [PubMed] [Google Scholar]