Abstract
In this paper, the authors report trends in hospitalized stroke rates among Minneapolis-St. Paul, Minnesota (population 2.6 million) metropolitan area residents aged 30–74 years from 1980 to 2000. Cases were identified from lists of discharge diagnoses provided by hospitals serving the target population. Age-adjusted, sex-specific stroke attack rates were computed for each survey year by using 5 different diagnostic definitions: 2 based purely on International Classification of Diseases, Ninth Revision (ICD-9) codes and 3 including clinical and neuroimaging criteria. Stroke rates, as measured by a highly specific clinical definition, remained stable from 1980 to 2000 for women. For men, these rates declined modestly from 1980 to 1990 and leveled off during 1990–2000. In contrast, use of stroke-related ICD-9 discharge codes declined significantly from 1980 to 2000: 35% among men and 16% among women. Neuroimaging use increased significantly from 75% of cases in 1980 to 98% in 2000. Short-term (28-day) stroke survival improved significantly, by 16% for women and 12% for men, from 1980 to 2000. The decline in stroke ICD-9 code usage reflects the influence of increased neuroimaging on discharge coding. The improved short-term survival in the face of stable, clinically defined stroke rates may imply treatment advances or ascertainment of less severe strokes, possibly masking a true decline in stroke rates.
Keywords: incidence, mortality, population surveillance, stroke
Trends in stroke rates represent a complex interaction between trends in population risk factors, improved preventive measures, and increasingly sensitive and specific case ascertainment. The prevalence of some vascular risk factors such as hypertension declined overall and treatment improved from the 1970s to 2000, while the prevalence of other factors, such as diabetes, increased (1, 2). Despite a decline in age-adjusted coronary heart disease incidence, improved survival after myocardial infarction, coupled with the aging US population, has likely increased the overall population burden of stroke risk. During the 1990s, numerous clinical trials identified therapies for optimal secondary prevention after stroke, and these therapies can be expected to reduce stroke event rates (3–5).
Parallel to trends in population characteristics and clinical practice are major changes in our ability to detect stroke events, driven by neuroimaging advances. The increasing availability and use of computed axial tomography in the 1980s and magnetic resonance imaging in the 1990s improved the overall accuracy (sensitivity and specificity) of stroke detection. A new magnetic resonance imaging sequence, diffusion weighted imaging, entered clinical use in 1997. Diffusion weighted imaging has a reported sensitivity of 88%–100% and specificity of 95%–100% for acute ischemia. The accuracy for detecting acute ischemic strokes is substantially improved by diffusion weighted imaging (95%–100%) compared with computed tomography (42%–75%) and standard magnetic resonance imaging (46%) (6). Medical record documentation has also improved over the last few decades, partly because of billing and reimbursement requirements, which also improved the completeness of stroke case ascertainment. These trends could increase stroke rates because of improved sensitivity of ascertainment or could lead to lower rates because of higher specificity (7).
We used a population-based stroke surveillance system, the Minnesota Stroke Survey, to examine trends in stroke rates. The Minnesota Stroke Survey is a multidecade study designed to examine trends in hospitalized stroke rates, stroke outcomes, risk factors, and treatment in the Minneapolis-St. Paul, Minnesota, metropolitan population. Data collection started in 1970, taking place typically at 5-year intervals. Results from the 1970, 1980, 1985, and 1990 surveys have been published previously (7–10).
Herein, we report results from the 1995 and 2000 surveys and examine trends in stroke rates spanning 2 decades, 1980–2000. Our goal was to peel away the effects of changes in case ascertainment sensitivity and specificity to study whether the observed stroke trends represent actual changes in population event rates or whether the true trends are masked by an overlay of improved case identification.
MATERIALS AND METHODS
Survey design
The Minnesota Stroke Survey, approved by the University of Minnesota Institutional Review Board, targeted all Minneapolis-St. Paul 7-county metropolitan area residents aged 30–74 years. Population sizes and interpolated intercensus year (1985, 1995) population estimates were obtained from the US Census Bureau.
Stroke cases were identified from lists of discharge diagnoses provided by all acute care hospitals serving the metropolitan area. The following acute cerebrovascular disease discharge codes from the International Classification of Diseases, Ninth Revision (ICD-9) were used to construct a sampling frame for each survey year: 431 (intracerebral hemorrhage), 432 (other and unspecified intracranial hemorrhage), 434 (occlusion of cerebral arteries), 436 (acute, but ill-defined cerebrovascular disease), and 437 (other and ill-defined cerebrovascular disease). Transient cerebral ischemia (ICD-9 code 435) and subarachnoid hemorrhage (ICD-9 code 430) were not included. For the 1980, 1985, 1990, and 1995 surveillance years, hospital records for 50% of cases in the sampling frame were randomly selected for detailed abstraction. In 2000, hospital records for 100% of cases were selected for detailed abstraction.
Data abstraction and quality control
Data were abstracted from hospital records by trained nurses using standardized forms and a manual. Abstractors recorded demographic information, medical history (including a history of prior stroke), relevant clinical information on stroke signs and symptoms, diagnostic procedures, and autopsy reports. Photocopied neuroimaging reports were independently abstracted by a trained physician reviewer using a manual and standardized data collection forms.
Data abstraction reliability was examined by reabstraction of randomly selected charts by an experienced “gold-standard” reference abstractor. An interrater reliability of greater than 95% was achieved for each of the demographic and clinical variables used to calculate stroke rates.
Stroke case definitions
The Minnesota Stroke Survey has traditionally computed stroke rates based on multiple diagnostic definitions (8, 9). Several of these definitions are based entirely on ICD-9 codes, whereas other definitions considered clinical features. Having multiple diagnostic methods helps evaluate fluctuations in stroke rates induced by changes in coding or measurement technology. We used 4 diagnostic definitions from previous Minnesota Stroke Survey reports and introduced a fifth, neuroimaging-based definition in acknowledgment of advances in imaging technology.
The 5 stroke case definitions are as follows: 1) cases for whom at least 1 acute cerebrovascular disease ICD-9 code (431, 432, 434, 436, or 437) is listed among hospital discharge diagnoses; 2) cases for whom one of these codes was listed in the first position among discharge diagnoses; 3) cases initially identified by definition 1 and meeting the World Health Organization criteria for acute stroke (i.e., a new neurologic deficit of presumed vascular origin lasting at least 24 hours or until death if death occurred within 24 hours); 4) cases satisfying definition 3 and having specific documented neurologic deficits (listed below); and 5) cases satisfying definition 1 and identified as experiencing definite, probable, or possible acute strokes by neuroimaging.
These 5 case definitions are of increasing specificity. Definitions 2, 3, 4, and 5 are subsets of definition 1. Definition 4 (referred to as the Minnesota Stroke Survey definition of acute stroke) is a further subset of definition 3; it requires the presence of at least 1 major neurologic deficit or 2 minor neurologic deficits. Major deficits included aphasia, coma, visual field cut, and motor or sensory deficits in at least 2 of 3 (face, arm, leg) body parts. Minor deficits included dysarthria (slurred speech), motor or sensory deficits in 1 of 3 (face, arm, leg) body parts, apraxia, and abnormal plantar reflex. The Minnesota Stroke Survey and World Health Organization definitions excluded cases of obvious nonstroke etiology such as tumors and subdural hematomas. Stroke attack rates using definitions 1–4 were calculated by computerized algorithms in each survey year: 1980, 1985, 1990, 1995, and 2000. Definition 5 of stroke, the neuroimaging definition, was applied to survey years 1990, 1995, and 2000, when neuroimaging was used more frequently. Definition 5 strokes were divided into the subtypes ischemic and hemorrhagic. Cases of stroke without evidence of prior stroke history in hospital medical records were classified as incident events. Linkage to Minnesota Department of Health vital statistics data was used to identify poststroke deaths and date of deaths for all cases.
Statistical analysis
A small percentage of patients (5%–10%) had multiple stroke hospitalizations during a survey year. We counted only the first event in each survey year per person, therefore not missing incident strokes when both the incident and recurrent events occurred in the study sample. Event counts from survey years with 50% sampling were doubled to allow comparison to year 2000, when sampling was 100%. We computed sex-specific stroke attack rates as well as incident event rates. All rates were standardized by age adjustment to the 2000 US Census. Poisson regression (PROC GENMOD, LINK=LOG, DIST=POISSON; SAS version 9.1 software, SAS Institute, Inc., Cary, North Carolina), adjusting for age, was used to model event rates, test for an overall trend across survey years, and test the null hypotheses of no change in stroke rates between adjacent survey years (1980 vs. 1985, 1985 vs. 1990, 1990 vs. 1995, and 1995 vs. 2000).
Patient characteristics and practice issues, such as rates of neuroimaging and completeness of medical records, were tested for an overall trend across survey years. Median length of stay was calculated by excluding patients who died before hospital discharge. Distributions of categorical variables were compared by using the chi-square test. “Missing” was used as a possible value for stroke signs and symptoms, enabling comparison of medical record completeness. Continuous variables were examined by comparison of means using 1-way analysis of variance.
Sex-specific, age-adjusted, short-term (2-week, 4-week) and 1-year case fatality/survival poststroke was calculated for each survey year for cases identified by the Minnesota Stroke Survey stroke definition and was tested for an overall trend across the years.
RESULTS
More than 6,000 stroke events were sampled across the 5 survey years (Table 1). Of the events identified by definition 1 (ICD-9 discharge codes for acute cerebrovascular disease), as many as two-thirds (55%–70%) were validated as strokes by the World Health Organization criteria (definition 3), and less than half (36%–47%) were classified as strokes by the Minnesota Stroke Survey definition (definition 4). Some definition 1 cases were excluded from the World Health Organization and Minnesota Stroke Survey definitions; either they did not meet the criteria of deficits lasting at least 24 hours or the deficits were determined to have been caused by nonstroke etiologies (e.g., tumors). Nonstroke etiologies were found for 16% of definition 1 cases in 1980, and this fraction declined to 6% in 2000.
Table 1.
Numbers of Hospitalized Acute Stroke Events Sampled in the Minneapolis-St. Paul, Minnesota, Metropolitan Area Across Survey Years for Cases Aged 30–74 Yearsa
| 1980 |
1985 |
1990 |
1995 |
2000b |
||||||
| No. | % | No. | % | No. | % | No. | % | No. | % | |
| ICD-9 code 431, 432, 434, 436, or 437 | 1,040 | 100c | 899 | 100 | 1,000 | 100 | 1,024 | 100 | 2,069 | 100 |
| First ICD-9 code 431, 432, 434, 436, or 437 | 602 | 58 | 604 | 67 | 649 | 65 | 686 | 67 | 1,255 | 61 |
| WHO stroke definition | 567 | 55 | 602 | 67 | 695 | 70 | 660 | 65 | 1,249 | 60 |
| MSS stroke definition | 372 | 36 | 405 | 47 | 410 | 41 | 463 | 45 | 915 | 44 |
| Neuroimaging stroke definition | 489 | 49 | 457 | 45 | 1,210 | 59 | ||||
| Ischemic stroke | 397 | 81d | 360 | 79 | 910 | 75 | ||||
| Hemorrhagic stroke | 92 | 19 | 97 | 21 | 300 | 25 | ||||
| Incident WHO stroke | 448 | 504 | 473 | 887 | ||||||
| Incident MSS stroke | 301 | 297 | 342 | 691 | ||||||
Abbreviations: ICD-9, International Classification of Diseases, Ninth Revision; MSS, Minnesota Stroke Survey; WHO, World Health Organization.
Refer to the Materials and Methods section of the text for stroke measure definitions.
Fifty percent of eligible acute stroke hospitalizations were sampled in 1980–1995, and 100% of eligible acute stroke hospitalizations were sampled in 2000, hence the substantially larger number of events in 2000 compared with prior cohort years.
Percentage of the most comprehensive definition.
Percentage of cases undergoing neuroimaging.
Only half (49%–58%) of the events identified by definition 1 were classified as strokes by the neuroimaging definition (definition 5). Some neuroimaging strokes did not meet the World Health Organization (and Minnesota Stroke Survey) time duration criterion of neurologic deficits lasting at least 24 hours. This fraction increased from 13% in 1990 to 18% in 2000.
Table 2 summarizes trends in stroke case characteristics across survey years for those meeting the World Health Organization stroke definition. The percentage of patients identified as white declined, with an increase in those identified as black or Asian. Prevalence of a prior history of stroke, transient ischemic attack, and atrial fibrillation fluctuated across the cohort years, without clear rising or declining trends. Prior history of myocardial infarction declined beginning in 1985. We found a rising trend in prestroke hypertension history. Neuroimaging use increased significantly, with almost all World Health Organization cases undergoing some neuroimaging from 1990 onward. Use of brain magnetic resonance imaging also increased significantly, from 18% in 1990 to 60% in 2000. Diffusion weighted imaging was used for 35% of cases in 2000. Length of hospital stay declined substantially, largely between 1980 and 1985. The proportion of cases unconscious at admission or presenting with a major neurologic deficit declined in the 2000 cohort, especially when compared with cohorts a decade or more prior.
Table 2.
Patient Population Characteristics Across Survey Years for WHO Stroke Cases Aged 30–74 Years in the Minneapolis-St. Paul, Minnesota, Metropolitan Area
| Characteristic | 1980 (n = 567) | 1985 (n = 602) | 1990 (n = 695) | 1995 (n = 660) | 2000 (n = 1,249) | P-trend |
| Sex, % female | 44 | 46 | 47 | 45 | 47 | NS |
| Mean age, years | 64 | 64 | 64 | 63 | 62 | 0.0002 |
| Race, % | ||||||
| White | 87 | 92 | 91 | 82 | 69 | <0.0001 |
| Black | 5 | 3 | 5 | 9 | 7 | |
| Asian | 0 | 1 | 1 | 3 | 5 | |
| Hispanic | 1 | 0 | 0 | 0 | 1 | |
| Native American/other | 1 | 1 | 1 | 1 | 1 | |
| Missing | 5 | 3 | 1 | 5 | 17 | |
| Preadmission history, % | ||||||
| History of stroke | 21 | 25 | 27 | 28 | 25 | 0.02 |
| History of transient ischemic attack | 10 | 15 | 10 | 18 | 10 | NS |
| History of myocardial infarction | 20 | 19 | 16 | 16 | 0.006 | |
| History of atrial fibrillation | 14 | 15 | 19 | 17 | 14 | NS |
| History of hypertension | 53 | 58 | 63 | 67 | 68 | <0.0001 |
| History of diabetes mellitus | 31 | 32 | 28 | NS | ||
| Clinical variables, % | ||||||
| Level of consciousness | ||||||
| Unconscious | 16 | 14 | 17 | 13 | 10 | 0.0007 |
| Conscious | 79 | 85 | 81 | 86 | 90 | |
| Missing | 5 | 1 | 2 | 1 | 0 | |
| Neurologic deficit | ||||||
| Major | 78 | 81 | 77 | 73 | 72 | <0.0001 |
| Two minor | 7 | 8 | 11 | 10 | 7 | |
| Other | 15 | 11 | 12 | 17 | 21 | |
| Aphasiaa | ||||||
| Yes | 33 | 31 | 29 | 26 | 29 | 0.03 |
| No | 42 | 56 | 57 | 57 | 59 | |
| Missing | 25 | 13 | 14 | 17 | 12 | |
| Visual field cuta | ||||||
| Yes | 16 | 25 | 21 | 17 | 17 | NS |
| No | 41 | 50 | 44 | 46 | 64 | |
| Missing | 43 | 25 | 35 | 37 | 19 | |
| Median length of hospital stay, days | 12 | 8 | 7 | 5 | 5 | <0.0001 |
| Neuroimaging present (includes MRI and CT), % | 75 | 88 | 96 | 98 | 98 | <0.0001 |
| MRI present, % | 18 | 30 | 60 | <0.0001 | ||
| Diffusion weighted imaging present, % | 35 |
Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging; NS, not significant; WHO, World Health Organization.
Excludes cases who were unconscious at the first examination (n = 498).
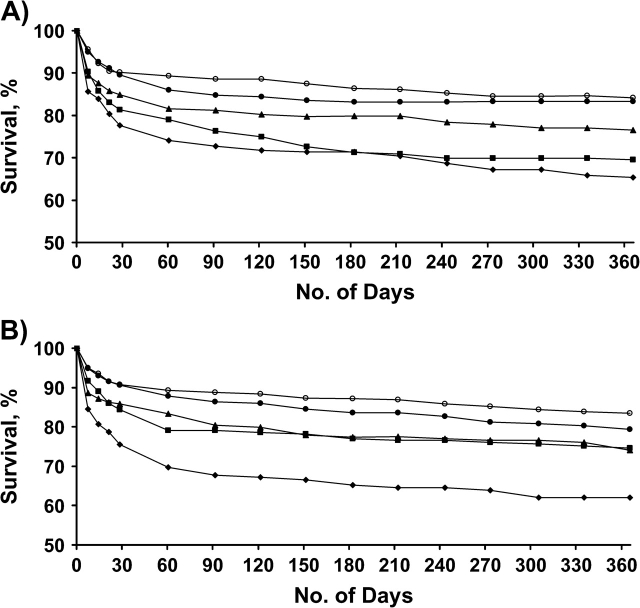
For each survey year, age-adjusted, hospitalized stroke rates by various metrics were calculated separately for men (Table 3, Figure 1A) and for women (Table 4, Figure 1B). For men, the highly specific Minnesota Stroke Survey–based measure declined significantly over the 2 decades (P < 0.0001), with most of the decline occurring in the first decade, and plateaued between 1990 and 2000. The neuroimaging-based rates also plateaued between 1990 and 2000. Rates computed by metrics based purely on ICD-9 codes (definitions 1 and 2) and the World Health Organization definition (definition 3) showed an overall significant decline (P < 0.0001), with the stroke rates falling across all survey periods. Rates measured by the least specific measure (definition 1) showed the most decline (35%), although other metrics (definitions 2 and 3) also showed rates declining by 27%–31%.
Table 3.
Age-adjusted Stroke Rates per 100,000, by Various Stroke Measures, Among Men Aged 30–74 Years in the Minneapolis-St. Paul, Minnesota, Metropolitan Area From 1980 to 2000
| Stroke Measurea | 1980 |
1985 |
1990 |
1995 |
2000 |
P-Trend | |||||
| Rate | 95% CI | Rate | 95% CI | Rate | 95% CI | Rate | 95% CI | Rate | 95% CI | ||
| Definition 1 | 307 | 272, 345 | 245b | 215, 278 | 242 | 214, 273 | 231 | 205, 260 | 199c | 182, 216 | <0.0001 |
| Definition 2 | 177 | 150, 206 | 168 | 143, 195 | 158 | 135, 183 | 154 | 132, 177 | 121 | 108, 134 | <0.0001 |
| Definition 3 | 170 | 144, 198 | 160 | 136, 187 | 166 | 143, 192 | 149 | 127, 172 | 124d | 111, 138 | <0.0001 |
| Definition 4 | 116 | 95, 140 | 108 | 88, 130 | 96 | 78, 115 | 101 | 84, 120 | 91 | 80, 103 | <0.0001 |
| Definition 5 | 120 | 101, 142 | 103 | 85, 122 | 116 | 102, 129 | NS | ||||
| Ischemic | 102 | 84, 122 | 82 | 66, 99 | 94 | 82, 106 | NS | ||||
| Hemorrhagic | 18 | 11, 28 | 21 | 14, 30 | 22 | 17, 28 | |||||
| Definition 3 incident events | 115 | 95, 137 | 120 | 100, 142 | 106 | 88, 126 | 91 | 80, 103 | <0.0001 | ||
| Definition 4 incident events | 77 | 60, 95 | 68 | 53, 85 | 74 | 59, 90 | 68 | 58, 78 | 0.02 | ||
Abbreviations: CI, confidence interval; NS, not significant.
Definition 1: International Classification of Diseases, Ninth Revision (ICD-9) codes 431, 432, 434, 436, 437; definition 2: first-position ICD-9 codes 431, 432, 434, 436, 437; definition 3: World Health Organization stroke; definition 4: Minnesota Stroke Survey stroke; definition 5: neuroimaging stroke. Refer to the Materials and Methods section of the text for stroke measure definitions.
P = 0.0003 for comparison between 1985 and 1980.
P = 0.02 for comparison between 2000 and 1995.
P = 0.03 for comparison between 2000 and 1995.
Figure 1.
Trends in stroke attack rates among men (A) and women (B) aged 30–74 years in the Minneapolis-St. Paul metropolitan area population from 1980 to 2000, by various stroke metrics in the Minnesota Stroke Survey. Square: International Classification of Diseases, Ninth Revision (ICD-9) code 431, 432, 434, 436, 437; dark circle: first-position ICD-9 code 431, 432, 434, 436, 437; diamond: World Health Organization stroke; open circle: Minnesota Stroke Survey stroke metric; star: neuroimaging stroke. Refer to the Materials and Methods section of the text for definitions of the various metrics.
Table 4.
Age-adjusted Stroke Rates per 100,000, by Various Stroke Measures, Among Women Aged 30–74 Years in the Minneapolis-St. Paul, Minnesota, Metropolitan Area From 1980 to 2000
| Stroke Measurea | 1980 |
1985 |
1990 |
1995 |
2000 |
P-Trend | |||||
| Rate | 95% CI | Rate | 95% CI | Rate | 95% CI | Rate | 95% CI | Rate | 95% CI | ||
| Definition 1 | 195 | 171, 222 | 160b | 138, 183 | 172 | 151, 196 | 160 | 140, 182 | 163 | 149, 177 | <0.0001 |
| Definition 2 | 116 | 97, 137 | 104 | 87, 124 | 112 | 94, 131 | 108 | 91, 126 | 98 | 87, 110 | 0.002 |
| Definition 3 | 106 | 88, 126 | 110 | 92, 129 | 122 | 104, 142 | 105 | 89, 123 | 97 | 86, 108 | 0.007 |
| Definition 4 | 66 | 52, 82 | 74 | 60, 90 | 74 | 60, 90 | 77 | 63, 92 | 71 | 62, 81 | NS |
| Definition 5 | 83 | 68, 99 | 71 | 58, 86 | 94 | 84, 106 | NS | ||||
| Ischemic | 63 | 50, 78 | 56 | 44, 69 | 67 | 58, 77 | NS | ||||
| Hemorrhagic | 19 | 13, 28 | 15 | 10, 23 | 27 | 22, 33 | |||||
| Definition 3 incident events | 85 | 69, 102 | 89 | 74, 106 | 74 | 60, 89 | 72 | 63, 82 | 0.009 | ||
| Definition 4 incident events | 58 | 45, 72 | 55 | 43, 69 | 57 | 45, 70 | 53 | 45, 62 | NS | ||
Abbreviations: CI, confidence interval; NS, not significant.
Definition 1: International Classification of Diseases, Ninth Revision (ICD-9) codes 431, 432, 434, 436, 437; definition 2: first-position ICD-9 codes 431, 432, 434, 436, 437; definition 3: World Health Organization stroke; definition 4: Minnesota Stroke Survey stroke; definition 5: neuroimaging stroke. Refer to the Materials and Methods section of the text for stroke measure definitions.
P = 0.02 for comparison between 1985 and 1980.
The age-adjusted rates for women were substantially lower than those for men according to all stroke measures. In contrast to those for men, rates as measured by the specific Minnesota Stroke Survey definition of stroke remained stable over the 2 decades, 1980–2000. Neuroimaging-based rates were also flat between 1990 and 2000, similar to those for men. While rates measured by definitions 1–3 declined significantly from 1980 to 2000, the magnitude of decline (9%–16%) was more modest than those for men.
For both women and men, incident stroke rates paralleled the attack rate trends but were 23%–29% lower. Hemorrhages constituted 19%–25% of all strokes validated by neuroimaging in our population, with no significant change in the relative proportion of ischemic versus hemorrhagic strokes from 1990 to 2000 (Tables 3 and 4).
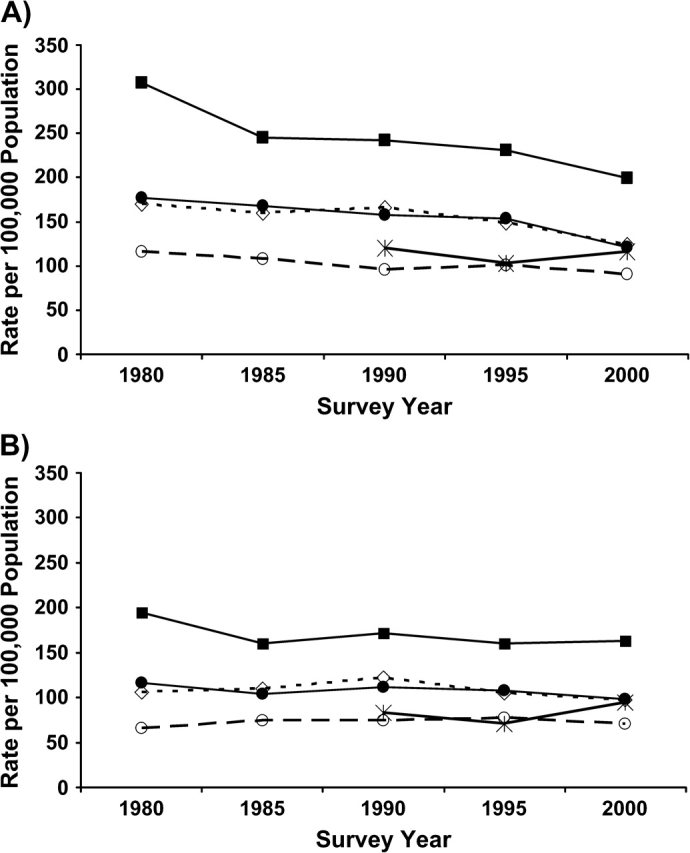
For cases meeting the Minnesota Stroke Survey stroke definition, age-adjusted 14-day and 28-day poststroke case fatality declined significantly from 1980 to 2000 (P < 0.0001) in both sexes (Figures 2A and 2B, Table 5). Most of the decline occurred from 1980 to 1995, with minimal changes between 1995 and 2000. One-year case fatality showed similar significant declining trends. One-year case-fatality gains among those who survived for 28 days were more modest than improvements in 28-day fatality.
Figure 2.
Short-term and long-term survival trends after stroke in men (A) and women (B) aged 30–74 years in the Minneapolis-St. Paul metropolitan area population from 1980 to 2000 for cases determined according to the clinical Minnesota Stroke Survey definition of stroke. Refer to the Materials and Methods section of the text for a definition of this metric. Diamond: 1980; square: 1985; triangle: 1990; dark circle: 1995; open circle: 2000. Case fatality data are shown in Table 5.
Table 5.
Age-adjusted Mortality (Case Fatality) for Stroke Defined by the Minnesota Stroke Survey (Clinical) Definition Among Men and Women Aged 30–74 Years in the Minneapolis-St. Paul Metropolitan Area From 1980 to 2000a
| Age-adjusted Mortality, % |
P-Trend | |||||
| 1980 | 1985 | 1990 | 1995 | 2000 | ||
| Men | ||||||
| 14-day | 16.1 | 14.2 | 12.4 | 7.4 | 7.7 | <0.0001 |
| 28-day | 22.4 | 18.7 | 15.1 | 10.5 | 9.9 | <0.0001 |
| 1-year | 34.6 | 30.5 | 23.5 | 16.8 | 15.9 | <0.0001 |
| 1-year among 28-day survivors | 15.9 | 14.5 | 9.8 | 7.0 | 6.6 | <0.0001 |
| Women | ||||||
| 14-day | 19.3 | 11.0 | 12.8 | 7.0 | 6.5 | <0.0001 |
| 28-day | 24.5 | 15.6 | 14.2 | 9.4 | 9.2 | <0.0001 |
| 1-year | 38.0 | 25.4 | 25.9 | 20.6 | 16.6 | <0.0001 |
| 1-year among 28-day survivors | 17.9 | 11.7 | 13.6 | 12.5 | 8.0 | 0.0112 |
Survival data are shown in Figure 2.
DISCUSSION
Observed stroke attack rates, as measured by a highly specific clinical definition, remained stable from 1980 to 2000 for women, confirmed from 1990 to 2000 by a sensitive and specific neuroimaging definition. For men, rates measured by the same definitions also plateaued from 1990 to 2000 while declining modestly from 1980 to 1990. Consistent with national statistics, incident events constituted three-quarters of all strokes, and trends in incident event rates were parallel to attack rate trends (1). Comparable to our findings, the Greater Cincinnati/Northern Kentucky Stroke Study reported unchanged stroke incidence when comparing 1993–1994 with 1999 (11). Two studies using vital statistics databases reported flat rates of hospitalized stroke, declining length of stay, and decreased case fatality in the 1990s, results similar to ours (12, 13). Brown et al. (14) also reported a plateauing of stroke rates from 1980 to 1989 in Rochester, Minnesota.
Measured stroke rates varied widely by case definition. Furthermore, although the most specific measures of stroke (Minnesota Stroke Survey and neuroimaging definitions) suggest stable trends, rates as measured by ICD-9–based metrics declined substantially among men and, to a lesser extent, women. We argue that this decline is a consequence of increased neuroimaging use leading to improvement in discharge coding; that is, stroke-related ICD-9 codes have become more specific for stroke. Supporting evidence for this argument is the recent convergence of definitions based purely on ICD-9 coding with the neuroimaging definition (Figure 1). The decline in the proportion of patients presenting with unconsciousness also supports the influence of neuroimaging on discharge coding (Table 2). Unconsciousness at presentation is often not due to stroke, and neuroimaging in recent surveys has likely helped clarify the diagnosis.
We also draw attention to the substantial decline (16% in 1980 to 6% in 2000) in the proportion of definition 1 cases found to have nonstroke etiologies of stroke. We therefore infer that the ICD-9 codes in early surveys contained many misdiagnoses and that most or all of the decline in stroke rates, as measured by definitions based purely on ICD-9 codes, is artifactual and due to the influence of neuroimaging on diagnosis and consequent discharge coding.
While rates assessed by the specific stroke measures appear to be static since 1980 for women and since 1990 for men, a key question remains: have stroke rates genuinely plateaued despite advances in medical therapy, or is the flat trend the result of a true decline masked by a countercurrent of more sensitive case ascertainment due to better diagnostic tools? The following are relevant observations from our data.
Neuroimaging improves the accuracy (sensitivity and specificity) of stroke diagnosis. Across every survey period, imaging use rates either increased substantially (1980 to 1990) or a more technologically advanced modality began to be used. While overall imaging rates were flat from 1990 to 2000, magnetic resonance imaging use increased substantially from 1990 to 2000, and diffusion weighted imaging was introduced only in the 2000 survey.
Have imaging trends changed Minnesota Stroke Survey case ascertainment by detecting smaller strokes or led to reclassification of transient ischemic attacks as strokes? The Minnesota Stroke Survey definition uses specific clinical variables abstracted from medical records that do not depend on imaging findings, although retrospective clinician documentation of stroke signs could be influenced by imaging results. A fraction of transient ischemic attacks with imaging correlates will be coded as strokes on hospital discharge. These cases will not meet the 24-hour requirement for clinical deficit duration required by the Minnesota Stroke Survey definition. Cases with acute strokes on imaging but such short-lived deficits increased from 13% in 1990 to 18% in 2000, reflecting perhaps the high sensitivity of diffusion weighted imaging. The Minnesota Stroke Survey definition excludes cases with alternate explanations for focal symptoms and has therefore always been specific, although it is conceivable that imaging has increased the ease of detection of nonstroke etiologies. Thus, even the Minnesota Stroke Survey definition may have become more specific over time.
We examined improved medical record documentation and its effect on case ascertainment. Table 2 shows fewer missing data for 3 key clinical variables (level of consciousness, aphasia, and visual field cut). This improvement is due to increased documentation of the absence (vs. presence) of stroke signs and symptoms. For example, missing documentation on results of visual field testing declined from 43% in 1980 to 19% in 2000 and documentation of its absence of abnormality increased from 41% to 64%, whereas documentation of its presence remained unchanged. Improved documentation did not necessarily translate into identification of more cases in our study.
Several markers of stroke severity declined from 1980 to 2000. Median length of stay declined, with the largest drop between 1980 and 1985 coinciding with introduction of diagnosis-related group-based reimbursement in the early 1980s (15). The proportion of cases with major neurologic deficits declined. Short-term (14-day, 28-day) survival, a reasonable surrogate for stroke severity, improved substantially. While this improvement may be in part have been due to improved acute care, detection of less severe events likely played a role.
The observations described above emphasize that the Minnesota Stroke Survey case definition is by design highly specific and reasonably impervious to technologic advances such as the availability of more accurate neuroimaging. Nevertheless, we cannot dismiss improvements in various markers of stroke severity possibly due to improved detection of smaller strokes. Hence, while the observed Minnesota Stroke Survey rates appear flat, a true decline may be masked.
We also draw attention to the changing risk factor profile of stroke cases (Table 2). The distribution of race in the stroke population mirrors the distribution in the general population. Prestroke history of myocardial infarction decreased across survey years, reflecting the declining incidence of coronary heart disease in the general population. There was no significant trend in prestroke atrial fibrillation history. Thus, we do not have evidence to suggest that advances in coronary care and improved post–myocardial infarction survival have led to increased rates of stroke in our population aged 30–74 years. It is possible that increased stroke rates due to improved post–myocardial infarction survival are actually occurring in those aged 75 years or older.
The rising prevalence of diabetes mellitus in the US population is not reflected in our stroke population. Prestroke history of hypertension increased significantly across the survey years, from 53% in 1980 to 68% in 2000. The Minnesota Heart Survey (16), a parallel study to the Minnesota Stroke Survey, found declining hypertension from the 1980s to 2000–2002 in the general Minneapolis-St. Paul population. During this same time frame, increases were observed in the proportion of hypertensive patients aware of their diagnosis of hypertension. These results parallel those from the National Health and Nutrition Examination Survey, which found increased hypertension awareness, detection, and treatment at a national level (17). On the basis of Minnesota Heart Survey results, we argue that the increased prevalence of prestroke history of hypertension in Minnesota Stroke Survey patients reflects population trends in increased awareness and detection of hypertension. Although improved hypertension detection and treatment have not apparently led to a decline in stroke rates, it is consistent with our view that stroke rates may have actually declined and that this decline may be masked by increased identification of less severe strokes.
We noted that our data show declining poststroke case fatality (Table 5), with most of the gains occurring between 1980 and 1995, although 1-year case fatality continued to decline among women between 1995 and 2000 as well. These observations are consistent with national trends that have shown a rapid decline in mortality in the 1970s and 1980s and a leveling off or slowed decline in the 1990s despite advances in therapies (18).
Strengths of our study include the large population base under observation, the longitudinal nature of our data, and the use of multiple measures of stroke rates. A criticism of our study is that it examined rates of stroke hospitalizations only. Hence, acute strokes treated in an outpatient setting or nursing home were not captured. However, data from the Northern Manhattan Stroke Study suggest that hospital surveillance captured 94% of acute strokes and that only an additional 6%–7% of strokes can be identified by community surveillance efforts (19). The Northern Manhattan Stroke Study conducted its surveillance from 1993 to 1996. It is possible that the proportion of stroke patients hospitalized for acute stroke changed over the 2-decade span of our study because of increased public awareness or changing practice due to the availability of acute treatments such as recombinant tissue-type plasminogen activator.
In conclusion, despite a significant decline in the use of stroke-related ICD-9 codes in the Minneapolis-St. Paul metropolitan area, rates, as measured by highly specific clinical criteria, remained stable among women between 1980 and 2000 and among men between 1990 and 2000. Short-term survival after stroke improved substantially from 1980 to 2000 for both men and women. Although our study used clinical criteria specifically designed to be robust to changing technology such as neuroimaging advances and the improved short-term survival is likely partly explained by improved stroke treatment, there is a strong possibility that less severe strokes are being ascertained, masking a true decline in strokes rates.
Acknowledgments
Author affiliations: Department of Neurology, School of Medicine, University of Minnesota, Minneapolis, Minnesota (Kamakshi Lakshminarayan, David C. Anderson); and Division of Epidemiology, School of Public Health, University of Minnesota, Minneapolis, Minnesota (David R. Jacobs, Jr., Cheryl A. Barber, Russell V. Luepker).
This research was supported by the National Institute of Neurological Disorders and Stroke (NINDS)/National Institutes of Health (NIH) (grant R01NS39028). K. L. was supported by an NINDS/NIH career development award (grant K23NS051377) and a National Center for Research Resources/NIH K12 award (grant 5K12RR023247) during this work.
The authors thank Dr. Anne Marie Weber-Main for her critical review and editing of manuscript drafts. The authors also thank Drs. Henry Blackburn and Aaron Folsom for feedback on manuscript drafts.
Conflict of interest: none declared.
Glossary
Abbreviation
- ICD-9
International Classification of Diseases, Ninth Revision
References
- 1.Rosamond W, Flegal K, Furie K, et al. Heart disease and stroke statistics—2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008;117(4):e25–e146. doi: 10.1161/CIRCULATIONAHA.107.187998. [DOI] [PubMed] [Google Scholar]
- 2.Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289(1):76–79. doi: 10.1001/jama.289.1.76. [DOI] [PubMed] [Google Scholar]
- 3.Clinical alert: benefit of carotid endarterectomy for patients with high-grade stenosis of the internal carotid artery. National Institute of Neurological Disorders and Stroke Stroke and Trauma Division. North American Symptomatic Carotid Endarterectomy Trial (NASCET) investigators. Stroke. 1991;22(6):816–817. doi: 10.1161/01.str.22.6.816. [DOI] [PubMed] [Google Scholar]
- 4.Stroke Prevention in Atrial Fibrillation Study. Final results. Circulation. 1991;84(2):527–539. doi: 10.1161/01.cir.84.2.527. [DOI] [PubMed] [Google Scholar]
- 5.The International Stroke Trial (IST): a randomised trial of aspirin, subcutaneous heparin, both, or neither among 19435 patients with acute ischaemic stroke. International Stroke Trial Collaborative Group. Lancet. 1997;349(9065):1569–1581. [PubMed] [Google Scholar]
- 6.Kidwell CS, Saver J, Ovbiagele B, et al. Brain imaging in stroke. In: Adams HP Jr, editor. Handbook of Cerebrovascular Diseases. 2nd ed. New York, NY: Marcel Dekker; 2005. p. 81. [Google Scholar]
- 7.McGovern PG, Shahar E, Sprafka JM, et al. The role of stroke attack rate and case fatality in the decline of stroke mortality. The Minnesota Heart Survey. Ann Epidemiol. 1993;3(5):483–487. doi: 10.1016/1047-2797(93)90101-9. [DOI] [PubMed] [Google Scholar]
- 8.Shahar E, McGovern PG, Sprafka JM, et al. Improved survival of stroke patients during the 1980s. The Minnesota Stroke Survey. Stroke. 1995;26(1):1–6. doi: 10.1161/01.str.26.1.1. [DOI] [PubMed] [Google Scholar]
- 9.Shahar E, McGovern PG, Pankow JS, et al. Stroke rates during the 1980s. The Minnesota Stroke Survey. Stroke. 1997;28(2):275–279. doi: 10.1161/01.str.28.2.275. [DOI] [PubMed] [Google Scholar]
- 10.McGovern PG, Pankow JS, Burke GL, et al. Trends in survival of hospitalized stroke patients between 1970 and 1985. The Minnesota Heart Survey. Stroke. 1993;24(11):1640–1648. doi: 10.1161/01.str.24.11.1640. [DOI] [PubMed] [Google Scholar]
- 11.Kleindorfer D, Broderick J, Khoury J, et al. The unchanging incidence and case-fatality of stroke in the 1990s: a population-based study. Stroke. 2006;37(10):2473–2478. doi: 10.1161/01.STR.0000242766.65550.92. [DOI] [PubMed] [Google Scholar]
- 12.Sturgeon JD, Folsom AR. Trends in hospitalization rate, hospital case fatality, and mortality rate of stroke by subtype in Minneapolis-St. Paul, 1980–2002. Neuroepidemiology. 2007;28(1):39–45. doi: 10.1159/000097855. [DOI] [PubMed] [Google Scholar]
- 13.Fang J, Alderman MH. Trend of stroke hospitalization, United States, 1988–1997. Stroke. 2001;32(10):2221–2226. doi: 10.1161/hs1001.096193. [DOI] [PubMed] [Google Scholar]
- 14.Brown RD, Whisnant JP, Sicks JD, et al. Stroke incidence, prevalence, and survival: secular trends in Rochester, Minnesota, through 1989. Stroke. 1996;27(3):373–380. [PubMed] [Google Scholar]
- 15.Diagnosis Related Groups (DRGs) and the Medicare Program: Implications for Medical Technology: A Technical Memorandum. Washington, DC: US Congress, Office of Technology Assessment; 1983. (Publication OTA-TM-H-17) [Google Scholar]
- 16.Luepker RV, Arnett DK, Jacobs DR, Jr, et al. Trends in blood pressure, hypertension control, and stroke mortality: the Minnesota Heart Survey. Am J Med. 2006;119(1):42–49. doi: 10.1016/j.amjmed.2005.08.051. [DOI] [PubMed] [Google Scholar]
- 17.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003;290(22):199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 18.National Center for Health Statistics. Age-adjusted Death Rates for Selected Causes. Hyattsville, MD: National Center for Health Statistics; ( http://www.cdc.gov/nchs/data/mortab/aadr7998s.pdf). (Accessed December 22, 2008) [Google Scholar]
- 19.Sacco RL, Boden-Albala B, Gan R, et al. Stroke incidence among white, black, and Hispanic residents of an urban community: the Northern Manhattan Stroke Study. Am J Epidemiol. 1998;147(3):259–268. doi: 10.1093/oxfordjournals.aje.a009445. [DOI] [PubMed] [Google Scholar]