Abstract
The timing and frequency of periconceptional multivitamin use may be related to the risk of preeclampsia. Women in the Danish National Birth Cohort (1997–2003) reported multivitamin or folate-only supplement use during a 12-week periconceptional period (from 4 weeks prior to 8 weeks after the last menstrual period). Preeclampsia cases were identified by using International Classification of Diseases, Tenth Revision, codes. Cox regression was used to estimate the association of frequency (weeks of use) and timing (preconception and postconception) of use with preeclampsia risk. Overall, there were 668 cases of preeclampsia (2.3%), and 18,551 women (65%) reported periconceptional multivitamin use. After adjustment, regular use (12 of 12 weeks) was related to a reduced risk of preeclampsia among normal-weight women. Compared with nonusers with a body mass index of 22 kg/m2, regular multivitamin users with the same body mass index had a 20% reduced risk of preeclampisa (hazard ratio = 0.78, 95% confidence interval: 0.60, 0.99). In addition, regular use in the postconception period only was associated with reduced risk, a relation that also appeared to be limited to women with a body mass index of <25 kg/m2 (hazard ratio = 0.63, 95% confidence interval: 0.42, 0.93). Folate-only supplement use was unrelated to preeclampsia risk. Regular periconceptional multivitamin use was associated with a reduced risk of preeclampsia among normal-weight women, and the immediate postconception period appeared to be the relevant exposure window.
Keywords: body mass index, dietary supplements, pre-eclampsia, pregnancy, vitamins, women
Preeclampsia is a leading cause of pregnancy-related morbidity and mortality among mothers and infants worldwide (1, 2). Nutrition is believed to play a role in the pathogenesis of adverse pregnancy outcomes, including preeclampsia. Several studies have reported a relation between prenatal vitamin and mineral supplementation and risk of preeclampsia, with equivocal findings (3–6). The periconceptional period, however, may be a particularly relevant exposure window given the critical role of implantation and placentation in the pathogenesis of preeclampsia (7).
We have recently reported that regular periconceptional multivitamin use was associated with reduced risk of preeclampsia among normal-weight women with a body mass index of <25 kg/m2 (8). These results, however, require replication in larger cohorts. We aimed to reexamine these results in the Danish National Birth Cohort, a large, well-characterized prospective cohort of pregnant women recruited early in gestation with reported multivitamin use during the period immediately before and after conception. If the relation between multivitamin use and a reduced risk of preeclampsia is corroborated, it raises the intriguing possibility that, similar to folate recommendations, micronutrient supplementation before or at the time of conception among well-nourished women living in developed countries may reduce risk for a leading cause of perinatal morbidity.
The objective of this study was to relate the frequency and timing of periconceptional multivitamin use to the risk of preeclampsia. We hypothesized that the effect of multivitamin supplementation would be strongest for women with regular use throughout the periconceptional period. We also considered that timing of use (preconception vs. postconception) may also be related to preeclampsia risk and hypothesized that regular use in both periods would be associated with a stronger effect. On the basis of previous reports, we also considered that an association between multivitamin use and preeclampsia may be limited to normal-weight women with a body mass index of <25 kg/m2. In addition, we hypothesized that any effect would be more pronounced for preterm (<37 weeks) versus term preeclampsia given the increased likelihood that preterm preeclampsia may involve a placental pathogenesis.
MATERIALS AND METHODS
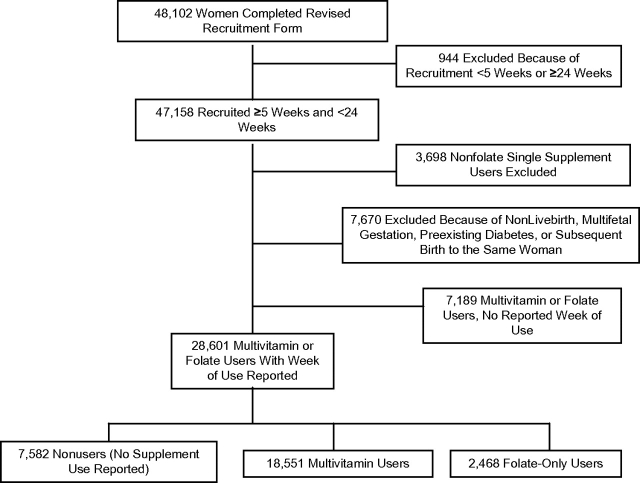
The Danish National Birth Cohort is a nationwide longitudinal study of pregnant women and their children that has been approved by the Danish National Ethics Board (9). Thirty percent of all pregnant women in Denmark were recruited between 1997 and 2003, and they are reasonably representative of the general Danish pregnant population (10). Of the 101,033 women in the Danish National Birth Cohort, 48,102 completed a revised version of the recruitment form used in the second wave of enrollment that allowed women to report each week their multivitamin use during the periconceptional period. Women with a questionable recruitment date or who joined the cohort at <5 weeks’ gestation or >24 weeks’ gestation were excluded (Figure 1). Women who reported only single supplement use (other than folate) were also excluded, as were women who did not report weeks of use and those with nonlivebirths, multifetal gestations, or preexisting diabetes. Only the first birth in the cohort was included. Of the remaining women, 7,582 reported no supplement use, 18,551 reported weekly information regarding multivitamin use, and 2,468 women reported folate supplementation alone. The final study population was 28,601.
Figure 1.
Study population, Danish National Birth Cohort, 1997–2003.
The Danish National Birth Cohort recruitment form was completed at a mean gestational age of 10.8 (standard deviation, 3.6) weeks and provided a table on which women were asked to check a box indicating in which weeks they took a supplement (11). In this tabular format, women reported weekly supplement type and frequency from 4 weeks prior to the last menstrual period (LMP) through 14 weeks after the LMP. For the purposes of this study, the periconceptional period was defined as the LMP − 4 through the LMP + 8, and this period was further categorized as preconception (LMP − 4 through LMP + 2) and postconception (LMP + 3 through LMP + 8). Multivitamin supplementation was evaluated as any use in each of the 12 weeks comprising the periconceptional period, and the contents of the most commonly used multivitamin are provided in Table 1. For the 4,547 women who were recruited during gestation weeks 5, 6, and 7, we imputed supplement use for the remainder of the periconceptional period on the basis of the use reported during the week of enrollment. Frequency of use was calculated as the ratio of the reported number of weeks of multivitamin use relative to the 12 weeks comprising the periconceptional period, and it could range from 0 for nonusers to 1 for regular users (12 of 12 weeks). Similarly, regular use in the preconception period was defined as 6 of 6 weeks of use. Regular use in the postconception period was defined as at least 4 of 6 weeks of use to capture women with regular use that began around the time a pregnancy would be detected. Thus, the dominant multivitamin usage patterns of women in the periconceptional period (regular use, use initiated immediately after a pregnancy was detected, no use) comprised our main analysis. The group with folate-only supplement use was analyzed in the same way as multivitamin use and was evaluated to determine if the effect appeared to be different in this group compared with multivitamin users. We selected this single supplement given the current worldwide recommendations that women considering pregnancy consume 400 μg/day.
Table 1.
Contents of the Most Commonly Used Multivitamin Supplement, Danish National Birth Cohort, 1997–2003
| Nutrient | Unit |
|
| μg | mg | |
| Vitamin A | 800 | |
| Thiamin (B1) | 1.4 | |
| Riboflavin (B12) | 1.6 | |
| Vitamin B6 | 2 | |
| Vitamin B12 | 1 | |
| Folic acid | 200 | |
| Niacin | 18 | |
| Pantothenic acid | 6 | |
| Vitamin C | 60 | |
| Vitamin D | 5 | |
| Vitamin E | 10 | |
| Iron | 14 | |
| Zinc | 15 | |
| Copper | 2 | |
| Iodine | 150 | |
| Manganese | 2.5 | |
| Chromium | 50 | |
| Selenium | 50 | |
| Molybdenum | 150 | |
Women with preeclampsia (n = 668) were identified via International Classification of Diseases, Tenth Revision, codes O14–O15. Danish guidelines define preeclampsia as gestational hypertension after 20 weeks’ gestation (blood pressure, >140/90 mm Hg) that resolves postpartum, in combination with proteinuria of ≥0.3 g/L. Use of the hospital registry to identify cases of preeclampsia has been validated (69% sensitivity and 99% specificity), and any misclassification is expected to be nondifferential (12). The preeclampsia group was further categorized into those delivered at term (≥37 weeks) or preterm (<37 weeks) to describe severity based on gestational age. Gestational age was based on the best clinical estimate at birth, which in more than 90% of cases was checked and adjusted according to early ultrasound (13).
The covariates included maternal age at delivery, self-reported smoking status at the first interview, self-reported height and prepregnancy weight that were used to calculate body mass index (weight (kg)/height (m)2), physical exercise (total time spent in exercise per week during early pregnancy, in minutes), parity, alcohol intake in the first part of pregnancy (drinks/week), mother's country of origin, and sociooccupational status that was based on a woman's job classification or education. High status included women in management or those with jobs requiring more than 4 years of education beyond high school. Office, service, or skilled manual workers and women in the military were classified in the middle category; unskilled workers or unemployed women were classified in the low category. Women were categorized with chronic hypertension if they reported at the first interview that they were diagnosed prior to pregnancy and also reported use of antihypertensive medication or indicated that the hypertension persisted (14). A long waiting time to pregnancy was characterized as ≥12 months among women who reported that their pregnancies were planned (89%); unplanned pregnancies or those with a time to pregnancy of <12 months were the referent. Dietary data were collected via a food frequency questionnaire in midpregnancy from a subset of women enrolled in the Danish National Birth Cohort, and diet was characterized as Western (high-fat dairy and red meat), health conscious (intake of fruits and vegetables, poultry, and fish), and intermediate as previously reported (15). Briefly, this approach utilizes factor analysis to identify patterns in dietary intakes assessed via a validated food frequency questionnaire. Diet patterns are able to account for many intake characteristics, may be more informative than individual nutrient analysis, and account for the fact that single nutrient intakes are often correlated.
With regard to analysis, we assessed maternal characteristics according to periconceptional multivitamin use versus nonuse. The risk of preeclampsia associated with multivitamin use was estimated as hazard ratios with 95% confidence intervals by using Cox regression with gestational days as the underlying time variable. Follow-up started at gestational day 140 and ended at the date of delivery. The absolute risk associated with frequency of use during the 12-week periconceptional period (1–4 weeks, 5–8 weeks, 9–12 weeks) was described. In addition, weeks of multivitamin use were analyzed as a continuous variable to evaluate a dose effect (number of weeks of use divided by 12 weeks; regular users were those with multivitamin use during 12 of 12 weeks). Regular use during both the preconception period and the postconception period (12 of 12 weeks) versus regular use during the postconception period only (at least 4 of 6 weeks) was evaluated; partial use in either period (1–3 weeks) was also characterized in these models. Nonusers were the referent for all models. Given the evidence that the effect of vitamin supplementation during pregnancy differs by body mass index (8, 16–18) and that the relation between body mass index and preeclampsia is linear (14, 19), we modeled the relation between multivitamin use (continuous) and body mass index (continuous) with an interaction term. Nonusers with a body mass index of 22 kg/m2, the median body mass index for the entire study population, were the referent. Results were also stratified by overweight status (body mass index, ≥25 kg/m2). In the above models, the differential effects for term versus preterm preeclampsia were examined by testing for interaction between regular pre- or postconception multivitamin use and gestational age at delivery, as well as a dichotomized time variable (<37 weeks vs. ≥37 weeks).
Potential confounders were retained in the models if they changed the effect of multivitamin exposure by >10%. The variables evaluated included maternal age, smoking status, body mass index, parity, marital status, country of origin, and chronic hypertension given the association between these factors and preeclampsia risk. Additional covariates were evaluated (gestational age at recruitment, sociooccupational status, physical activity, and alcohol consumption) that may account for confounding by health-promoting behaviors that are likely also associated with multivitamin use. Multivitamin use may be casually related to a long waiting time to pregnancy, and there is evidence that a long time to pregnancy is associated with increased risk of preeclampsia (20). We therefore explored the relation among multivitamin use, time to pregnancy, and preeclampsia by first including and then excluding women with time to pregnancy >12 months from the analysis to determine if the effect remained unchanged. SAS, version 9.1, software (SAS Institute, Inc., Cary, North Carolina) and STATA, version 10.0, software (StataCorp LP, College Station, Texas) were used for analyses, and results were considered significant with a 2-sided P < 0.05.
RESULTS
Overall, 18,551 women (65%) reported any multivitamin use in the periconceptional period (Table 2). Multivitamin users versus nonusers were more likely to be >25 years of age, to have a body mass index of <25 kg/m2, to be nulliparous, to engage in physical exercise, to report a midpregnancy diet that was classified as health conscious, and to report >12 months’ waiting time to pregnancy. They were also less likely to smoke and less likely to report a lower sociooccupational status. Folate-only supplement users were similar to multivitamin users. Overall, there were 668 cases of preeclampsia (2.3%), and the frequency of multivitamin or folate-only supplement use was associated with modestly reduced rates of preeclampsia (Figure 2).
Table 2.
Maternal Characteristics According to Periconceptional Multivitamin and Folate-only Supplement Use, Danish National Birth Cohort, 1997–2003
| Nonusers (n = 7,582) |
Multivitamin Users (n = 18,551) |
Folate-only Supplement Users (n = 2,468) |
||||
| No. | % | No. | % | No. | % | |
| Maternal age, years | ||||||
| <21 | 199 | 2.6 | 148 | 0.8 | 15 | 0.6 |
| 21–25 | 1,251 | 16.5 | 2,337 | 12.6 | 310 | 12.6 |
| 26–30 | 3,021 | 39.8 | 8,481 | 45.7 | 1,070 | 43.4 |
| 31–35 | 2,241 | 29.6 | 5,686 | 30.7 | 802 | 32.5 |
| ≥36 | 870 | 11.5 | 1,899 | 10.2 | 271 | 11.0 |
| Body mass index, kg/m2 | ||||||
| <18.5 | 324 | 4.3 | 801 | 4.3 | 106 | 4.3 |
| 18.5–24.9 | 4,734 | 62.4 | 12,621 | 68.0 | 1,675 | 67.9 |
| 25–29.9 | 1,677 | 22.1 | 3,544 | 19.1 | 467 | 18.9 |
| ≥30 | 847 | 11.2 | 1,585 | 8.6 | 220 | 8.9 |
| Smoking during pregnancy, cigarettes/day | ||||||
| 1–10 | 1,198 | 15.8 | 1,930 | 10.4 | 239 | 9.7 |
| >10 | 454 | 6.0 | 501 | 2.7 | 52 | 2.1 |
| Physical exercise, minutes/week | ||||||
| 0 | 5,108 | 67.5 | 11,467 | 61.9 | 1,544 | 62.6 |
| 1–180 | 1,911 | 25.3 | 5,673 | 30.6 | 738 | 29.9 |
| >180 | 547 | 7.2 | 1,392 | 7.5 | 184 | 7.5 |
| Alcohol consumption, drinks/week | ||||||
| 0 | 4,262 | 56.2 | 10,443 | 56.3 | 1,377 | 55.8 |
| 0.5–3 | 3,099 | 40.9 | 7,736 | 41.7 | 1,052 | 42.6 |
| >3 | 217 | 2.9 | 368 | 2.0 | 38 | 1.5 |
| Maternal diet patterna | ||||||
| Western | 674 | 20.9 | 1,004 | 13.8 | 149 | 16.4 |
| Intermediate | 2,114 | 65.5 | 4,752 | 65.5 | 579 | 63.7 |
| Health conscious | 440 | 13.6 | 1,497 | 20.6 | 181 | 19.9 |
| Maternal country of origin | ||||||
| Denmark or other Nordic countries | 7,313 | 96.6 | 17,900 | 96.6 | 2,354 | 95.5 |
| Greenland and Faroe Islands | 49 | 0.7 | 175 | 0.9 | 35 | 1.4 |
| Other | 212 | 2.8 | 456 | 2.5 | 76 | 3.1 |
| Low sociooccupational status | 517 | 6.8 | 596 | 3.2 | 94 | 3.8 |
| Time to pregnancy, >12 months | 833 | 11.0 | 2,506 | 13.5 | 413 | 16.7 |
| Multiparous | 4,299 | 57.7 | 8,719 | 47.0 | 1,084 | 43.9 |
| Chronic hypertension | 120 | 1.6 | 265 | 1.4 | 28 | 1.1 |
| Mean gestational age at recruitment, weeks (standard deviation) | 11.2 (3.8) | 10.9 (3.5) | 10.8 (3.4) | |||
Available for 10,481 women.
Figure 2.
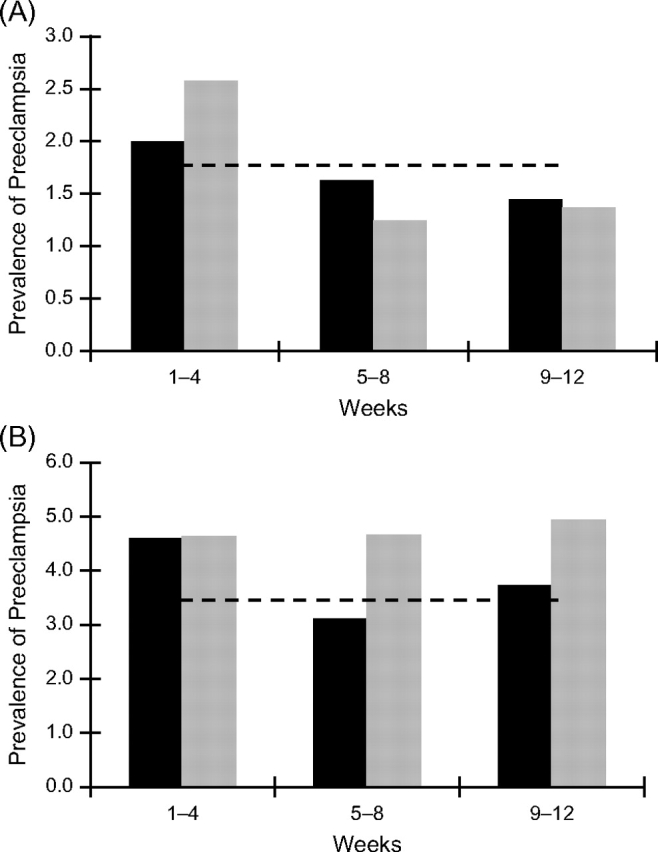
Preeclampsia prevalence according to weeks of periconceptional multivitamin or folate-only supplementation among normal-weight (body mass index, <25 kg/m2; n = 20,261) (A) and overweight (body mass index, ≥25 kg/m2; n = 8,340) (B) women, Danish National Birth Cohort, 1997–2003. The black bar represents preeclampsia prevalence among multivitamin users, the gray bar represents prevalence among folate-only supplement users, and the dashed line represents prevalence among nonusers.
Regular periconceptional multivitamin use throughout the entire period (12 of 12 weeks; n = 6,374) showed a modest association with reduced risk of preeclampsia (crude hazard ratio (HR) = 0.83, 95% confidence interval (CI): 0.68, 1.02). Adjustment for body mass index, smoking, parity, gestational age at recruitment, and chronic hypertension (covariates that met our a priori requirements) attenuated this finding (HR = 0.88, 95% CI: 0.71, 1.08).
There was marginal evidence that this association differed by prepregnancy body mass index (Pinteraction = 0.09). Compared with a referent of nonusers with a body mass index of 22 kg/m2, women with the same body mass index and 12 weeks of periconceptional multivitamin use had about a 20% reduced risk of preeclampsia compared with nonusers (HR = 0.78, 95% CI: 0.60, 0.99) (Table 3). When compared with the same referent, regular multivitamin users with a body mass index of 20 had a 35% reduced risk of preeclampsia, whereas nonusers had only a 13% reduced risk (HR = 0.64, 95% CI: 0.48, 0.84 vs. HR = 0.87, 95% CI: 0.84, 0.90). In contrast, multivitamin users and nonusers with a body mass index of 30 had similar preeclampsia risks of 1.73 and 1.74, respectively.
Table 3.
Association Between Preeclampsia and Body Mass Index Among Regular Users (12 of 12 weeks) and Nonusers of Periconceptional Multivitamins, Danish National Birth Cohort, 1997–2003
| Body Mass Index, kg/m2 | Nonuser |
Multivitamin User in the Entire Period (12 of 12 weeks) |
||
| Adjusted Hazard Ratioa | 95% Confidence Interval | Adjusted Hazard Ratioa | 95% Confidence Interval | |
| 18 | 0.76 | 0.70, 0.82 | 0.52 | 0.38, 0.71 |
| 20 | 0.87 | 0.84, 0.90 | 0.64 | 0.48, 0.84 |
| 22 | 1.00 | Referent | 0.78 | 0.60, 0.99 |
| 24 | 1.15 | 1.11, 1.19 | 0.95 | 0.75, 1.19 |
| 26 | 1.32 | 1.22, 1.43 | 1.16 | 0.93, 1.44 |
| 28 | 1.52 | 1.35, 1.70 | 1.41 | 1.13, 1.77 |
| 30 | 1.74 | 1.49, 2.03 | 1.73 | 1.36, 2.18 |
Model adjusted for smoking, parity, chronic hypertension, and gestational age at recruitment.
When evaluated according to frequency and timing, 6,655 women reported regular multivitamin use in both the preconception (LMP − 4 through LMP + 2) and postconception (LMP + 3 through LMP + 8) periods. A total of 3,666 women reported regular use in the postconception period only (Table 4). Consistent with our earlier result, regular multivitamin use in both periods was associated with a reduced risk for preeclampsia among women with a body mass index of <25 kg/m2 (HR = 0.78, 95% CI: 0.57, 1.06). However, normal-weight women with regular multivitamin use in the postconception-only period also showed a reduced risk (HR = 0.63, 95% CI: 0.42, 0.93). There did not appear to be a relation between postconception use and preeclampsia risk among overweight women (body mass index of ≥25, HR = 0.88, 95% CI: 0.59, 1.30).
Table 4.
Adjusted Hazard Ratios for Preeclampsia Related to Regular Multivitamin Use in the Preconception and Postconception Periods, Danish National Birth Cohort, 1997–2003
| Preconception Multivitamin Usea | Postconception Multivitamin Useb | Total (n = 26,133) |
Body Mass Index, <25 (n = 18,479) |
Body Mass Index, ≥25 (n = 7,653) |
||||
| No. | Adjusted Hazard Ratioc | 95% Confidence Interval | Adjusted Hazard Ratioc | 95% Confidence Interval | Adjusted Hazard Ratioc | 95% Confidence Interval | ||
| None | None | 7,582 | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| Regular | Regular | 6,655 | 0.88 | 0.70, 1.10 | 0.78 | 0.57, 1.06 | 0.98 | 0.71, 1.36 |
| None | Regular | 3,666 | 0.74 | 0.56, 0.98 | 0.63 | 0.42, 0.93 | 0.88 | 0.59, 1.30 |
Preconception use was from 4 weeks prior to the last menstrual period (LMP − 4) to 2 weeks after the last menstrual period (LMP + 2); regular use was for 6 of 6 weeks.
Postconception use was from 3 weeks (LMP + 3) to 8 weeks (LMP + 8) after the last menstrual period. (Regular use for 4 or more weeks every 6 weeks included women who initiated use at the time of a detected pregnancy).
Adjusted for body mass index, smoking, parity, chronic hypertension, gestational age at recruitment, and partial multivitamin use.
Results were unchanged when the 3,339 women with a waiting time to pregnancy of >12 months were excluded (data not shown). In addition, there was no evidence of effect measure modification by the presence of chronic hypertension (P = 0.70), and results were unchanged after excluding the 385 women with chronic hypertension. Similarly, results were unaffected when the analysis was replicated by using robust standard errors to allow 2,880 women to contribute more than 1 birth. Although precision was compromised when the analysis was limited to women with diet data available (n = 10,481), additional adjustment for this covariate did not affect the magnitude of the hazard ratio associated with postconception regular multivitamin use (HR = 0.73, 95% CI: 0.47, 1.14). In addition, there was no effect of folate-only supplementation in the pre- and postconception periods (HR = 0.98, 95% CI: 0.50, 1.92) or the postconception-only period (HR = 0.95, 95% CI: 0.55, 1.66) on risk of preeclampsia among all women or among normal-weight women (HR = 0.80, 95% CI: 0.51, 1.26).
There was no evidence that the associations between regular pre- or postconception multivitamin use and preeclampsia risk differed in cases of preterm versus term preeclampsia (Pinteraction = 0.56 with regular pre- and postconception use).
DISCUSSION
Our results indicated that regular multivitamin use in the periconceptional period was associated with reduced risk of preeclampsia among normal-weight women. If causal, multivitamin use immediately after conception appeared to be the relevant exposure window. No effect measure modification was seen with gestational age at birth, and there did not appear to be a relation between folate-only supplement use and preeclampsia.
Our previous observational studies of periconceptional multivitamin use, preeclampsia (8), and small-for-gestational-age births (18) also reported associations that were limited to normal-weight women, as did earlier reports of zinc and folate supplementation effects on fetal growth and malformations (16, 17). We can only speculate on the mechanisms underlying the various effects of multivitamin use by body mass index status. Overweight women may have higher nutrient requirements than do lean women. Perhaps the metabolic dysregulation in obese women (21) is so vast that any positive changes in micronutrient intake may be blunted or nullified. Alternatively, the recommended doses of nutrients contained in multivitamins may be too low to overcome the metabolic disturbances characteristic of the obese or overweight state. It is also possible that these metabolic or physiologic factors might directly or indirectly alter the absorption, transport, or storage of nutrients in an overweight individual. In addition, different mechanisms may be involved in the pathogenesis of preeclampsia among normal versus overweight women. For example, lack of micronutrients may be relevant in the setting of oxidative stress among normal-weight women, while different mechanisms may be involved in the development of preeclampsia in overweight women. Further research in this area is needed, given the excess risk of preeclampsia associated with overweight and obese status.
Normal-weight women with regular pre- and postconception multivitamin use had a reduced risk for preeclampsia in our data. So did women with postconception-only use, suggesting that multivitamin use after conception was perhaps more strongly related to preeclampsia risk. This possibility is biologically plausible given the importance of micronutrients to the vascular remodeling and rapid cell division that characterizes placentation. Folate and B12 deficiencies have been linked to defects in the placental vascular bed (22), and other nutrients may be equally important (23). In addition, the more robust effect of postconception multivitamin use may be related to the higher doses of folate and other micronutrients in prenatal versus standard multivitamin.
The association between multivitamin use and preeclampsia was more modest in the Danish National Birth Cohort compared with previous reports (8), but given the relatively homogenous nature of the Danish population, this more modest effect may more accurately reflect the independent contribution of supplementation. Alternatively, Danish women may be less nutritionally deficient and, thus, the effect of supplementation may be reduced. Wen et al. (24) have reported a markedly reduced preeclampsia risk among a Canadian cohort of folate users. The majority of users in that study, however, achieved their folate supplementation via multivitamin use, and therefore a folate-only effect could not be isolated. In contrast to our results, their study reported no differential effect among women who initiated supplementation use before versus after conception. Only 34% of this Canadian cohort was recruited before 12 weeks’ gestation; thus, the precision of the reported timing of initiation may be compromised. In our much larger cohort, 73% were recruited at ≤12 weeks, and we limited analysis to women who reported weekly use in a tabular format. Although we cannot directly compare our data collection method with those of the study by Wen et al., we are confident that earlier reporting in a systematic fashion provides the most precise assessment of multivitamin use.
Our results should be considered in light of limitations. Although the Danish National Birth Cohort is a large, well-characterized population cohort, it consists predominantly of Caucasian women, and therefore our results may not be generalizable to other ethnicities. As mentioned above, the exposure contrast may be low among this population if lack of multivitamin intake is compensated for by an adequate diet. The homogeneity of the Danish population, however, also helps to reduce residual confounding by social and lifestyle factors, and therefore our observational results may more accurately identify a true multivitamin effect. We relied on the Danish Hospital Register to identify cases of preeclampsia, but this method has been validated (12). We were unable to specifically study the content of each multivitamin supplement used in the Danish National Birth Cohort. The most commonly reported product, however, contains less folic acid (200 μg) than currently recommended doses for women considering pregnancy (400 μg). Folate supplementation was, however, the most common single supplement used in this cohort (in addition to multivitamin use or used alone), and our analysis did not suggest that folate was related to preeclampsia risk.
Although we attempted to account for unmeasured residual confounding by accounting for diet pattern in the subgroup of women who completed the food frequency questionnaire, we cannot rule out the possibility that women who take a multivitamin supplement may also eat a diet that is more importantly related to preeclampsia risk. However, multivitamin users in our study were very similar to those that reported folate-only supplement intake, and in this group of women we did not identify an association with reduced risk of preeclampsia. This provides some reassurance that our findings are not entirely due to residual confounding by diet. Regrettably, more detailed analysis of the specific micronutrients consumed in food was not feasible in our current study, because diet data were collected after 25 weeks’ gestation, well beyond the periconceptional period.
Our results indicate that regular periconceptional multivitamin use is associated with a reduced risk of preeclampsia among normal-weight women. If causal, multivitamin use immediately after conception may be the relevant exposure window. Similar to folate supplementation recommendations, multivitamin supplementation around the time of conception may be worth considering as a preeclampsia prevention strategy.
Acknowledgments
Author affiliations: Department of Obstetrics, Gynecology, and Reproductive Sciences, University of Pittsburgh, Pittsburgh, Pennsylvania (Janet M. Catov, Lisa M. Bodnar); Department of Epidemiology, University of Pittsburgh, Pittsburgh, Pennsylvania (Janet M. Catov, Lisa M. Bodnar); Department of Epidemiology, Institute of Public Health, University of Aarhus, Aarhus, Denmark (Ellen A. Nohr, Jorn Olsen); Danish Epidemiology Science Centre, Statens Serum Institut, Copenhagen, Denmark (Vibeke K. Knudsen, Sjurdur F. Olsen); and Department Epidemiology, School of Public Health, University of California at Los Angeles, Los Angeles, California (Jorn Olsen).
The Danish National Research Foundation has established the Danish Epidemiology Science Centre that initiated and created the Danish National Birth Cohort. The cohort is furthermore a result of a major grant from this Foundation. Additional support for the Danish National Birth Cohort was obtained from the Pharmacy Foundation, the Egmont Foundation, the March of Dimes Birth Defects Foundation, the Augustinus Foundation, and the Health Foundation. Dr. Catov is supported by the BIRCWH-K12HD043441-06.
Conflict of interest: none declared.
Glossary
Abbreviations
- CI
confidence interval
- HR
hazard ratio
- LMP
last menstrual period
References
- 1.Chang J, Elam-Evans LD, Berg CJ, et al. Pregnancy-related mortality surveillance—United States 1991–1999. MMWR Surveill Summ. 2003;52(2):1–8. [PubMed] [Google Scholar]
- 2.Roberts JM, Pearson G, Cutler J, et al. Summary of the NHLBI Working Group on Research on Hypertension During Pregnancy. Hypertension. 2003;41(3):437–445. doi: 10.1161/01.HYP.0000054981.03589.E9. [DOI] [PubMed] [Google Scholar]
- 3.Rumbold AR, Crowther CA, Haslam RR, et al. Vitamins C and E and the risks of preeclampsia and perinatal complications. N Engl J Med. 2006;354(17):1796–1806. doi: 10.1056/NEJMoa054186. [DOI] [PubMed] [Google Scholar]
- 4.Merchant AT, Msamanga G, Villamor E, et al. Multivitamin supplementation of HIV-positive women during pregnancy reduces hypertension. J. Nutr. 2005;135(7):1776–1781. doi: 10.1093/jn/135.7.1776. [DOI] [PubMed] [Google Scholar]
- 5.Poston L, Briley AL, Seed PT, et al. Vitamin C and vitamin E in pregnant women at risk for pre-eclampsia (VIP trial): randomised placebo-controlled trial. Lancet. 2006;367(9517):1145–1154. doi: 10.1016/S0140-6736(06)68433-X. [DOI] [PubMed] [Google Scholar]
- 6.Olsen SF, Secher NJ. A possible preventive effect of low-dose fish oil on early delivery and pre-eclampsia: indications from a 50-year-old controlled trial. Br J Nutr. 1990;64(3):599–609. doi: 10.1079/bjn19900063. [DOI] [PubMed] [Google Scholar]
- 7.Roberts JM, Cooper DW. Pathogenesis and genetics of preeclampsia. Lancet. 2001;357(9249):53–56. doi: 10.1016/s0140-6736(00)03577-7. [DOI] [PubMed] [Google Scholar]
- 8.Bodnar LM, Tang G, Ness RB, et al. Periconceptional multivitamin use reduces the risk of preeclampsia. Am J Epidemiol. 2006;164(5):470–477. doi: 10.1093/aje/kwj218. [DOI] [PubMed] [Google Scholar]
- 9.Olsen J, Melbye M, Olsen SF, et al. The Danish National Birth Cohort—its background, structure and aim. Scand J Public Health. 2001;29(4):300–307. doi: 10.1177/14034948010290040201. [DOI] [PubMed] [Google Scholar]
- 10.Nohr EA, Frydenberg M, Henriksen TB, et al. Does low participation in cohort studies induce bias? Epidemiology. 2006;17(4):413–418. doi: 10.1097/01.ede.0000220549.14177.60. [DOI] [PubMed] [Google Scholar]
- 11.Olsen SF, Mikkelsen TB, Knudsen VK, et al. Data collected on maternal dietary exposures in the Danish National Birth Cohort. Paediatr Perinat Epidemiol. 2007;21(1):76–87. doi: 10.1111/j.1365-3016.2007.00777.x. [DOI] [PubMed] [Google Scholar]
- 12.Klemmensen AK, Olsen SF, Osterdal ML, et al. Validity of preeclampsia-related diagnoses recorded in a national hospital registry and in a postpartum interview of the women. Am J Epidemiol. 2007;166(2):117–124. doi: 10.1093/aje/kwm139. [DOI] [PubMed] [Google Scholar]
- 13.Nohr EA, Bech BH, Davies MJ, et al. Prepregnancy obesity and fetal death: a study within the Danish National Birth Cohort. Obstet Gynecol. 2005;106(2):250–259. doi: 10.1097/01.AOG.0000172422.81496.57. [DOI] [PubMed] [Google Scholar]
- 14.Catov JM, Ness RB, Kip KE, et al. Risk of early or severe pre-eclampsia related to pre-existing conditions. Int J Epidemiol. 2007;36(2):412–419. doi: 10.1093/ije/dyl271. [DOI] [PubMed] [Google Scholar]
- 15.Knudsen VK, Orozova-Bekkevold IM, Mikkelsen TB, et al. Major dietary patterns in pregnancy and fetal growth. Eur J Clin Nutr. 2008;62(4):463–470. doi: 10.1038/sj.ejcn.1602745. [DOI] [PubMed] [Google Scholar]
- 16.Shaw GM, Velie EM, Schaffer D. Risk of neural tube defect-affected pregnancies among obese women. JAMA. 1996;275(14):1093–1096. doi: 10.1001/jama.1996.03530380035028. [DOI] [PubMed] [Google Scholar]
- 17.Goldenberg RL, Tamura T, Neggers Y, et al. The effect of zinc supplementation on pregnancy outcome. JAMA. 1995;274(6):463–468. doi: 10.1001/jama.1995.03530060037030. [DOI] [PubMed] [Google Scholar]
- 18.Catov JM, Bodnar LM, Ness RB, et al. Association of periconceptional multivitamin use is associated with reduced risk of preterm or small for gestational age births. Am J Epidemiol. 2007;166(3):296–303. doi: 10.1093/aje/kwm071. [DOI] [PubMed] [Google Scholar]
- 19.Bodnar LM, Ness RB, Markovic N, et al. The risk of preeclampsia rises with increasing prepregnancy body mass index. Ann Epidemiol. 2005;15(7):475–482. doi: 10.1016/j.annepidem.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 20.Basso O, Weinberg CR, Baird DD, et al. Subfecundity as a correlate of preeclampsia: a study within the Danish National Birth Cohort. Am J Epidemiol. 2003;157(3):195–202. doi: 10.1093/aje/kwf194. [DOI] [PubMed] [Google Scholar]
- 21.Ramsay JE, Ferrell WR, Crawford L, et al. Maternal obesity is associated with dysregulation of metabolic, vascular, and inflammatory pathways. J Clin Endocrinol Metab. 2002;87(9):4231–4237. doi: 10.1210/jc.2002-020311. [DOI] [PubMed] [Google Scholar]
- 22.Ray JG, Laskin CA. Folic acid and homocyst(e)ine metabolic defects and the risk of placental abruption, pre-eclampsia and spontaneous pregnancy loss: a systematic review. Placenta. 1999;20(7):519–529. doi: 10.1053/plac.1999.0417. [DOI] [PubMed] [Google Scholar]
- 23.Jauniaux E, Watson AL, Hempstock J, et al. Onset of maternal arterial blood flow and placental oxidative stress. Am J Pathol. 2000;157(6):2111–2122. doi: 10.1016/S0002-9440(10)64849-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wen SW, Chen XK, Rodger M, et al. Folic acid supplementation in early second trimester and the risk of preeclampsia. Am J Obstet Gynecol. 2008;198(1):45. doi: 10.1016/j.ajog.2007.06.067. e1–45.e7. [DOI] [PubMed] [Google Scholar]