Abstract
Rotating night shift work disrupts circadian rhythms and is associated with coronary heart disease. The relation between rotating night shift work and ischemic stroke is unclear. The Nurses’ Health Study, an ongoing cohort study of registered female nurses, assessed in 1988 the total number of years the nurses had worked rotating night shifts. The majority (69%) of stroke outcomes from 1988 to 2004 were confirmed by physician chart review. The authors used Cox proportional hazards models to assess the relation between years of rotating night shift work and ischemic stroke, adjusting for multiple vascular risk factors. Of 80,108 subjects available for analysis, 60% reported at least 1 year of rotating night shift work. There were 1,660 ischemic strokes. Rotating night shift work was associated with a 4% increased risk of ischemic stroke for every 5 years (hazard ratio = 1.04, 95% confidence interval: 1.01, 1.07; Ptrend = 0.01). This increase in risk was similar when limited to the 1,152 confirmed ischemic strokes (hazard ratio = 1.03, 95% confidence interval: 0.99, 1.07; Ptrend = 0.10) and may be confined to women with a history of 15 or more years of rotating shift work. Women appear to have a modestly increased risk of stroke after extended periods of rotating night shift work.
Keywords: risk factors; sleep disorders, circadian rhythm; stroke
Stroke is the third leading cause of death in the United States and the leading cause of adult disability (1). Because traditional risk factors do not account for stroke risk entirely, the study of novel stroke risk factors is important (2). There is growing evidence that perturbations in sleep influence stroke risk (3, 4). Shift work, a term that encompasses long-term night shift work, evening shifts, and rotating shift work, is known to disrupt circadian rhythms (5) and is associated with vascular disease risk factors (6–8) and increased catecholamine secretion (9). Several prospective studies have identified rotating night shift work as a risk factor for cardiovascular disease (10–12), with mixed findings regarding cardiovascular mortality (13–15). The association between shift work and cerebrovascular disease has not been well studied. One small case-control study from Europe has been reported, with no association identified (16).
In a previous analysis within the Nurses’ Health Study, rotating night shift work was found to be associated with a higher risk of developing coronary heart disease (10). Our objective was to assess the relation between rotating night shift work and incident ischemic stroke in this same cohort, furthering the understanding of the association between sleep and vascular disease and potentially identifying a novel, modifiable risk factor for stroke. We hypothesized that shift work would be positively associated with ischemic stroke risk and, further, that there would be a dose-response relation.
MATERIALS AND METHODS
Subjects/study population
The Nurses’ Health Study is a prospective, longitudinal cohort study in which married registered nurses aged 30–55 years were enrolled in 1976. A total of 121,701 nurses of the approximately 172,400 nurses who were mailed the baseline questionnaire responded. Every 2 years, cohort members receive a follow-up questionnaire with questions about diseases and other health-related topics. Deaths are identified through the National Death Index and supplemented by reports of next of kin or the postal system and are estimated as 98% complete (17). Detailed methods of the Nurses’ Health Study have been described (18). This project was approved by the Brigham and Women's Hospital Institutional Review Board in Boston, Massachusetts.
The current analysis included Nurses’ Health Study participants who responded to the shift work question in 1988 (n = 85,161). From this sample, women were excluded if they reported a history of stroke prior to ascertainment of shift work status (n = 648) or stroke at an unknown time point (n = 75). Because stroke risk differs significantly by race and ethnicity (19), with the overwhelming majority of Nurses’ Health Study participants Caucasian women (97%), minorities (non-Caucasian (n = 2,008) and Hispanic (n = 682) ethnicity) were excluded to eliminate confounding by race/ethnicity as the small numbers of these subgroups would preclude statistical adjustment. Another 1,640 women did not contribute to the analysis because they were missing data on at least 1 covariate in every questionnaire cycle. The remaining 80,108 women comprise the study population.
Ascertainment of rotating night shift work and covariates
“What is the total number of years during which you worked rotating night shifts (at least 3 nights/month in addition to days and evenings in that month)?” was queried at a single time point in 1988, with responses in 8 prespecified categories: never, 1–2, 3–5, 6–9, 10–14, 15–19, 20–29, and 30 or more years. For this analysis, baseline covariates were also measured by using data from the 1988 questionnaire. Covariates were updated through mailed questionnaires sent every other year and included the following: smoking status (never (referent), past, current); body mass index (<21, 21–<23, 23–<25 (referent), 25–<27, 27–<30, ≥30 kg/m2); alcohol consumption (0 (referent), >0–<5, 5–9.9, ≥10 g/day, updated every 4 years on food frequency questionnaires); fruit and vegetable intake (<3 (referent), 3–4.4, 4.5–5.9, 6–7.4, ≥7.5 servings/day); physical activity (<3 (referent), 3–8.9, 9–14.9, 15–23.9, ≥24 metabolic equivalent-hours/week); menopausal status (premenopausal, postmenopausal without hormone therapy, postmenopausal with past hormone therapy, postmenopausal with current hormone therapy (referent), or dubious status due to surgical menopause with at least 1 ovary remaining); regular use of at least 1 aspirin per week (never (referent), past, current); and dichotomously treated coronary heart disease (angina or reported myocardial infarction), high blood pressure, elevated lipids, and diabetes.
Several covariates of interest were not available on the 1988 questionnaire. Atrial fibrillation was first queried in 2000 and updated every other year thereafter. Years of the nurses’ husbands’ education (in 5 categories: no high school, some high school, high school graduate (referent), college graduate, graduate school) were assessed in 1992 only, as an indicator of socioeconomic status. The number of hours of sleep per night (≤6, 7, 8 (referent), 9, ≥10 hours/night) and snoring (never (referent), occasional, regularly) were assessed in 1986. These 4 variables were included only in subanalyses. Their ability to confound the relation between shift work and stroke, defined by a ≥10% change in the point estimate for shift work, was assessed by building models with and without these variables limited to the subjects and time period after which the questions were asked.
Ascertainment of endpoints
The primary study endpoint was fatal or nonfatal ischemic stroke occurring between the return of the 1988 questionnaire and June 1, 2004. Hemorrhagic stroke was excluded, as there was no a priori hypothesis of an association for this stroke type with shift work given the different risk factors for hemorrhagic and ischemic vascular disease.
Between 1988 and 2004, 2,226 women in the study population self-reported a stroke. In addition, 284 fatal strokes were ascertained through the National Death Index or next of kin for a total of 2,510 identified strokes. A medical record or death certificate was sought for all reported strokes, and 1,897 (76%) were received and reviewed by a study physician. Strokes were classified according to established criteria (20), which required evidence of a neurologic deficit with sudden or rapid onset that persisted for more than 24 hours or until death. Computed tomography or magnetic resonance imaging reports were available for 91% of those with medical records. Cerebrovascular pathology due to infection, trauma, or malignancy was excluded, as were “silent” strokes discovered only by radiologic imaging. Of these 1,897 stroke reports, 1,503 (79%) were confirmed to be a stroke: 1,152 ischemic, 281 hemorrhagic, and 70 of unknown type. Of the 613 reported strokes for which a medical record or death certificate was unavailable, 438 were reconfirmed verbally or in writing by the participant after her original report. Because of the high confirmation rate for reported strokes (79%) and the overwhelming percentage of ischemic strokes among confirmed cases (77%), our primary outcome included confirmed ischemic stroke cases (n = 1,152), confirmed strokes of unknown type (n = 70), and unconfirmed strokes that were reconfirmed verbally or in writing by the participant (n = 438), for a total of 1,660 confirmed plus probable ischemic strokes (1,512 nonfatal and 148 fatal). The mean age at the time of stroke was 69 (standard deviation, 6.9) years.
Statistical analysis
Cox proportional hazards regression models were used to assess the relation between shift work and stroke risk. All models were stratified by age in months and questionnaire follow-up cycle. The time periods for which an individual's covariate status was unknown because of missing data did not contribute to the analysis (8% of person-time). As both age and questionnaire cycle are proxies for time, proportionality assumptions were tested by adding an interaction term for shift work × age and shift work × questionnaire cycle to models with shift work treated continuously and categorically.
To assess the overall association of shift work and stroke risk (adjusted for age and questionnaire cycle), we compared a model with shift work modeled categorically as a series of 7 dummy variables (referent was no shift work) with a model without the shift work variables using a likelihood ratio test (χ27). The association of shift work with stroke risk adjusted for potential confounders was then assessed after adding the covariates to the model (fully adjusted model) and again conducting a likelihood ratio test. To determine the most appropriate functional form for the shift work variable, we compared the fully adjusted model with the same model with shift work modeled as a grouped continuous variable (using midpoints from categories of years of shift work) using a likelihood ratio test (χ26). The results of this comparison failed to reject a departure from linearity and, therefore, the shift work variable was henceforth treated linearly. The hypothesis of a trend in stroke risk with increasing years of shift work was tested using a Wald χ2 test for trend in the fully adjusted model. The relation between shift work and stroke was summarized as the increase in risk of stroke for a 5-year increase in shift work. The above analyses were run by using confirmed plus probable cases and then repeated with only the confirmed ischemic strokes to determine the influence the probable cases had on the association between shift work and stroke risk.
Because hypertension, diabetes, and coronary heart disease may be in the causal pathway between shift work and stroke, models with and without these variables were run to assess their influence on the shift work–stroke association. Subanalyses with limited follow-up time were also conducted to explore potential confounding by socioeconomic status (husband's education), atrial fibrillation, snoring, and duration of sleep. These additional analyses were run using the primary endpoint of confirmed plus probable ischemic strokes.
In post hoc analyses, for the purpose of comparison with prior cardiac analyses in this study population, those who had worked 1 or more years of rotating night shift work were combined and compared with those who had never worked rotating night shift work in a fully adjusted model. After assessment of the hazard ratio in the 8-category analyses, the rotating night shift work variable was collapsed into never (referent), 1–14 years, and ≥15 years of shift work and assessed in fully adjusted models. All statistical analyses were performed on SAS, version 9, software (SAS Institute, Inc., Cary, North Carolina). All statistical tests were 2 sided.
RESULTS
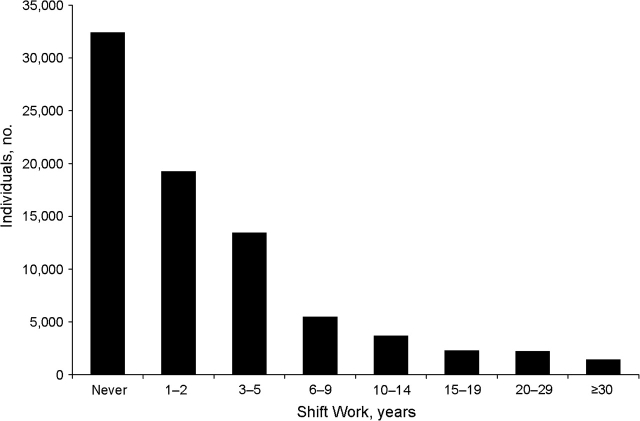
There were 80,108 subjects, contributing a total of 1,128,895 person-years, available for analysis. Baseline characteristics of the cohort are reported in Table 1. Women with more years spent in rotating night shift work were older; were less likely to use hormone therapy if postmenopausal or to have a husband who graduated from college; and were more likely to sleep 6 or less hours per night, to snore regularly, or to be diagnosed with coronary heart disease, diabetes, or hypertension. Of all women in the study population, 59.5% reported ever having engaged in 1 or more years of shift work (Figure 1), with only 7.4% reporting having worked rotating night shifts for 15 or more years. Interaction terms within the continuous shift work model (for age × shift work, P = 0.90; for questionnaire cycle × shift work, P = 0.97) and the categorical shift work model (for age × shift work, P = 0.49; for questionnaire × shift work, P = 0.53) were not significant, suggesting that proportionality assumptions were not violated.
Table 1.
Age-standardized Baseline Characteristics of the Study Populationa by Category of Years Spent in Rotating Night Shift Work, Nurses’ Health Study, 1988–2004
| Duration of Rotating Night Shift Work |
||||
| Never (n = 28,015) | 1–14 Years (n = 36,400) | 15–29 Years (n = 3,821) | ≥30 Years (n = 1,187) | |
| Mean (SD) | ||||
| Age, years | 54.5 (7.2) | 55.0 (7.1) | 56.3 (6.9) | 60.4 (4.5) |
| Physical activity, MET-hours/weekb | 13.7 (15.0) | 14.9 (15.9) | 14.7 (16.2) | 15.8 (15.1) |
| Body mass index, kg/m2 | 25.4 (4.8) | 25.6 (4.9) | 27.0 (5.4) | 26.8 (4.6) |
| Alcohol, g/day | 6.7 (10.6) | 6.7 (10.6) | 5.5 (9.9) | 6.1 (8.9) |
| Fruit, servings/day | 2.2 (1.3) | 2.3 (1.3) | 2.3 (1.3) | 2.5 (1.2) |
| Vegetables, servings/day | 3.0 (1.4) | 3.2 (1.5) | 3.1 (1.6) | 3.3 (1.4) |
| Percent | ||||
| Premenopausal | 29.0 | 28.6 | 26.0 | 6.4 |
| Postmenopausal | 64.5 | 64.6 | 66.1 | 85.1 |
| Dubious menopausal statusc | 6.6 | 6.8 | 7.9 | 8.5 |
| Current hormone therapy userd | 31.7 | 31.6 | 25.1 | 24.5 |
| Current smoker | 17.2 | 18.6 | 24.8 | 22.8 |
| Regular aspirin usere | 65.2 | 66.6 | 66.7 | 66.3 |
| Coronary heart disease | 5.1 | 5.8 | 8.3 | 11.0 |
| Diabetes | 3.9 | 4.2 | 6.8 | 6.5 |
| High blood pressure | 27.2 | 28.1 | 34.0 | 37.0 |
| High cholesterol | 24.5 | 25.0 | 26.6 | 29.6 |
| Atrial fibrillation | 6.7 | 7.0 | 7.4 | 6.5 |
| Husband's education | ||||
| Less than high school | 6.0 | 5.9 | 9.1 | 11.8 |
| High school graduate | 40.0 | 39.2 | 49.2 | 46.9 |
| College or more | 54.0 | 54.9 | 41.6 | 41.3 |
| Sleep, hours/night | ||||
| ≤6 | 26.5 | 29.8 | 42.5 | 40.1 |
| 7 | 43.1 | 42.1 | 35.4 | 31.6 |
| 8 | 25.3 | 23.5 | 17.9 | 23.9 |
| ≥9 | 5.0 | 4.6 | 4.2 | 4.4 |
| Snore regularly | 8.8 | 9.6 | 12.8 | 13.6 |
Abbreviations: MET, metabolic equivalent; SD, standard deviation.
Baseline was 1988 for all variables except husband's education, hours of sleep, snoring, and atrial fibrillation, where the baseline was 1992, 1986, 1986, and 2000, respectively. Values are standardized to the age distribution of the study population at baseline. The baseline study population is smaller than the total number as some nurses did not contribute data in 1988.
MET-hours/week of recreational or leisure-time activity; 3 MET-hours/week is equivalent to walking at an average pace for 1 hour each week.
Women whose periods had ceased because of surgery but still have at least 1 ovary remaining.
Use of hormone therapy was calculated among 44,850 postmenopausal women.
Regular use of 1 or more aspirin tablets per week.
Figure 1.
Distribution of rotating night shift work reported among 80,108 baseline participants, Nurses’ Health Study, 1988–2004.
Using the confirmed plus probable ischemic stroke cases, we found that there was an overall association between years of rotating night shift work (modeled categorically) and stroke (χ27 = 21.2; P = 0.004) adjusted for age and questionnaire follow-up cycle (“time-adjusted” model); women who worked longer durations of shift work (≥15 years) had an elevated risk of ischemic stroke compared with women who never worked any rotating shifts (Table 2). After adjustment for confounders (fully adjusted model), the overall association between years of shift work (modeled categorically) and stroke was no longer significant (χ27 = 8.0; P = 0.33), and only ≥30 years of shift work remained marginally significant (hazard ratio (HR) = 1.32, 95% confidence interval (CI): 1.00, 1.73) (Table 2). When restricting to confirmed ischemic stroke cases only, we found that the association between shift work and ischemic stroke was significant only in the 15- to 19-year category in both the time-adjusted (HR = 1.65, 95% CI: 1.24, 2.20) and fully adjusted (HR = 1.42, 95% CI: 1.07, 1.89) models (Table 2).
Table 2.
Hazard Ratio of Ischemic Stroke by Years of Working Rotating Night Shifts, Nurses’ Health Study, 1988–2004
| Type of Ischemic Stroke | Duration of Rotating Night Shift Workab |
Hazard Ratio/5 Years of Shift Work | Ptrend | |||||||
| Never | 1–2 Years | 3–5 Years | 6–9 Years | 10–14 Years | 15–19 Years | 20–29 Years | ≥30 Years | |||
| Confirmed + probable | ||||||||||
| No. of cases | 622 | 343 | 287 | 130 | 88 | 68 | 63 | 59 | ||
| Time-adjustedc hazard ratio | 1.00 | 0.96 | 1.01 | 1.16 | 1.11 | 1.43 | 1.34 | 1.47 | 1.07 | <0.001 |
| 95% confidence interval | 0.84, 1.09 | 0.88, 1.16 | 0.96, 1.40 | 0.89, 1.40 | 1.11, 1.84 | 1.03, 1.74 | 1.12, 1.92 | 1.04, 1.10 | ||
| Fully adjustedd hazard ratio | 1.00 | 0.99 | 1.00 | 1.10 | 0.99 | 1.24 | 1.17 | 1.32 | 1.04 | 0.01 |
| 95% confidence interval | 0.87, 1.13 | 0.87, 1.15 | 0.91, 1.33 | 0.79, 1.24 | 0.96, 1.59 | 0.90, 1.52 | 1.00, 1.73 | 1.01, 1.07 | ||
| Confirmed only | ||||||||||
| No. of cases | 437 | 237 | 197 | 92 | 57 | 54 | 43 | 35 | ||
| Time-adjustedc hazard ratio | 1.00 | 0.94 | 0.98 | 1.16 | 1.05 | 1.65 | 1.29 | 1.22 | 1.06 | 0.002 |
| 95% confidence interval | 0.80, 1.10 | 0.83, 1.16 | 0.92, 1.45 | 0.79, 1.38 | 1.24, 2.20 | 0.94, 1.77 | 0.86, 1.73 | 1.02, 1.10 | ||
| Fully adjustedd hazard ratio | 1.00 | 0.96 | 0.96 | 1.09 | 0.94 | 1.42 | 1.13 | 1.11 | 1.03 | 0.10 |
| 95% confidence interval | 0.82, 1.13 | 0.81, 1.14 | 0.87, 1.36 | 0.71, 1.24 | 1.07, 1.89 | 0.82, 1.55 | 0.78, 1.57 | 0.99, 1.07 | ||
At least 3 nights per month of night shift work in addition to days or evenings in that month.
Never (458,880 person-years of follow-up); 1–2 years (274,665 person-years); 3–5 years (188,648 person-years); 6–9 years (76,393 person-years); 10–14 years (51,029 person-years); 15–19 years (30,882 person-years); 20–29 years (29,846 person-years), and ≥30 years (18,702 person-years).
Adjusted for age and questionnaire cycle.
Adjusted for age, questionnaire cycle, hypertension, coronary heart disease, diabetes, elevated cholesterol, aspirin use, body mass index, smoking, alcohol consumption, fruit and vegetable consumption, physical activity, menopausal status, and use of hormone replacement therapy.
No significant deviation from linearity was found (χ26 = 1.9; P = 0.93) when comparing the fully adjusted models with shift work modeled categorically and as a grouped continuous variable, suggesting that the grouped continuous variable was the appropriate functional form of the shift work variable. In the fully adjusted model with confirmed plus probable cases and shift work modeled as a grouped continuous variable, each 5-year increment of rotating shift work increased the risk of ischemic stroke by 4% (HR = 1.04, 95% CI: 1.01, 1.07) (Table 2). The Wald χ2 test for trend was significant (Ptrend = 0.01). Restricting to confirmed ischemic stroke cases resulted in little change in the association between shift work and stroke (HR = 1.03, 95% CI: 0.99, 1.07), but the test for trend was no longer significant (Ptrend = 0.10).
The association between shift work and confirmed plus probable ischemic stroke remained virtually unchanged in adjusted models without hypertension (HR = 1.04, 95% CI: 1.01, 1.07), diabetes (HR = 1.05, 95% CI: 1.01, 1.08), or coronary heart disease (HR = 1.04, 95% CI: 1.01, 1.07) compared with the fully adjusted results.
Subanalyses
The relation between shift work and stroke did not differ in analyses with (per 5 years of shift work, HR = 1.04, 95% CI: 1.01, 1.08) or without (HR = 1.04, 95% CI: 1.01, 1.08) adjustment for husbands’ education (n = 61,653; strokes = 1,181). Similarly, there was no difference in the association between shift work and stroke, with (HR = 1.05, 95% CI: 1.00, 1.11) or without (HR = 1.06, 95% CI: 1.00, 1.11) (n = 69,241; strokes = 317) adjustment for atrial fibrillation. Furthermore, there was no difference in the association between shift work and stroke (n = 70,312; strokes = 1,494) with (HR = 1.03, 95% CI: 0.99, 1.06) or without (HR = 1.03, 95% CI: 0.99, 1.06) adjustment for sleep duration or with (HR = 1.03, 95% CI: 0.99, 1.06) or without (HR = 1.03, 95% CI: 0.99, 1.06) adjustment for snoring.
Post hoc analyses
Those who worked ≥1 years of shift work did not have a higher risk of confirmed plus probable (HR = 1.04, 95% CI: 0.94, 1.15) or confirmed ischemic stroke only (HR = 1.02, 95% CI: 0.90, 1.14) compared with those who had never worked rotating night shifts. The lack of a significant association when using this crude measure of shift work probably resulted from the loss of information in the shift work variable due to dichotomization. Although those who worked 1–14 years of rotating night shift work did not have a higher risk for either confirmed plus probable (HR = 1.01, 95% CI: 0.91, 1.12) or confirmed ischemic stroke only (HR = 0.98, 95% CI: 0.86, 1.11), those with ≥15 years of rotating night shift work did have a higher risk of both confirmed plus probable (HR = 1.41, 95% CI: 1.19, 1.66) and confirmed ischemic stroke only (HR = 1.23, 95% CI: 1.01, 1.50) compared with those who had never worked rotating night shifts.
DISCUSSION
The current analyses demonstrate an independent association between rotating night shift work and ischemic stroke risk in a cohort of non-Hispanic white female nurses. A linear trend between the number of years of rotating night shift work and ischemic stroke risk was observed, with a 4% increase in ischemic stroke risk for each 5 years of shift work. Despite the linear trend identified, a threshold effect may exist, as risk was only significantly increased in categorical models for women who worked 15 or more years of rotating night shift work. The only other prospective study to date addressing a similar question reported no association between shift work and risk of incident ischemic stroke (16). However, this study was limited by methodological issues including small size, limited follow-up, and exposure misclassification. Two other unadjusted studies from Europe failed to demonstrate a clear relation between rotating night shift work and stroke mortality (14, 15).
Our analysis adds to the expanding body of work evaluating the influence of sleep disorders on stroke risk. Both sleep apnea and longer sleep durations have been described as risk factors for stroke (3, 4, 21, 22), although whether sleep apnea is more prevalent in shift workers remains unknown. The mechanism by which rotating shift work may affect stroke risk is unclear. One possibility is that sleep deprivation in shift workers may worsen existing sleep apnea, although this is not well substantiated (23). Another possibility is that the effect may be mediated through melatonin. It is generally well accepted that exposure to light during the night decreases melatonin synthesis (24). Nighttime workers are therefore at risk for lower melatonin exposure (25), a finding that has been substantiated by lower urinary 6-sulfatoxymelatonin excretion in rotating and fixed night workers (26). There are several ways by which lowered melatonin production may increase stroke risk (27). First, it may promote atherosclerosis, as melatonin is known to be a direct radical scavenger and to have other antioxidant effects (28). Second, it may result in a relatively hypercoagulable state, as melatonin administration may reduce coagulability (29). Third, exogenous melatonin has been shown to lower blood pressure in small studies (30, 31). Given the suggested threshold effect in the current study, the effect on coagulability is a less likely explanation given that this should not require over a decade to take effect.
Alternatively, rotating shift work may affect the risk of ischemic stroke indirectly through its effects on other stroke risk factors. In addition to hypertension, shift work has also been associated with diabetes, heart disease, smoking, and obesity, but results have been variable (6–8, 32–34). Evening work and night shift work have also been found to be associated with nondipping blood pressure status (lack of blood pressure decrease during sleep), which is an emerging stroke risk factor (35). The current analysis accounted for traditional stroke risk factors and showed an independent association between rotating night shift work and ischemic stroke risk. We were unable to adjust for atrial fibrillation and socioeconomic status in the main models, but in a more limited follow-up period, neither appeared to be a significant confounder. Given the importance of hypertension, diabetes, and coronary heart disease as risk factors for ischemic stroke, we considered their mediating effects by comparing models with and without these covariates. The association of rotating night shift work was similar in these models, suggesting that these factors are not the main biologic mediators of the observed increased risk. The mediating effects of vascular risk factors on the association between rotating night shift work and stroke risk require further study.
Shift work appears to have deleterious effects on multiple vascular systems. Prior studies have shown an increased risk of cardiac disease, deaths from ischemic heart disease, and hospitalization for other vascular diseases (10–12, 14, 36). A prior analysis within the Nurses’ Health Study cohort showed a positive association, as well as a dose-response relation, between rotating night shift work and coronary heart disease (10). This study adds rotating night shift work to the list of shared risk factors for ischemic heart and cerebrovascular disease, although the apparent threshold appears lower (approximately 6 years) for cardiovascular outcomes than the longer ≥15 years identified in the current study for stroke.
This study has several limitations. This analysis was limited to Caucasian women, thereby limiting the generalizability to males or to other race/ethnic groups. Most, but not all, stroke cases were confirmed by study physicians through review of medical and death records. However, the effect size for shift work and stroke was similar using the confirmed or confirmed plus probable stroke cases in the continuous models for this group of health professionals. Shift work was also quantified at 1 time point only; therefore, subsequent shift work could not be taken into account. This measurement error would be likely to lead to an underestimation of the association. We also assessed only rotating night shift work and thus cannot determine whether there is an association with stable night shift work and stroke. Misinterpretation of the shift work question could have resulted in inclusion of stable night shift work, which would likely have resulted in a bias toward the null. As with all longitudinal studies, there were some missing data. Because some data may not have been missing completely at random, excluding time periods with missing data could have contributed to bias, although the magnitude of missing data was not large. As with other studies assessing shift work as a risk factor for cardiovascular disease (10, 33, 37), unmeasured confounding remains a potential limitation. However, covariate information was extensively measured in the Nurses’ Health Study making this unlikely. Further, the use of a nursing cohort helps to reduce confounding by socioeconomic status, an important stroke risk factor (38, 39). Moreover, subanalyses including atrial fibrillation and husband's education as a surrogate for socioeconomic status suggest that these factors were not confounders and, therefore, unlikely that they explain the observed association between rotating night shift work and ischemic stroke. Nonetheless, there may be other confounders that we were not able to take into account. For instance, 1 could postulate an unhealthy shift worker effect in which less healthy individuals with more comorbidities select rotating night shift work rather than daytime work. Of course, the opposite or no effect could be true (40). The categorical analysis showed significant associations with stroke only for the higher shift work categories. It is therefore possible that these higher shift work year categories with fewer subjects may have been overly influential on the test for trend.
The current study identified rotating night shift work as an independent risk factor for ischemic stroke. Although the potential biologic explanations support either a threshold or a linear effect, the data suggest that this association may be present only in the highest years of shift work. More research is needed to confirm this finding in other cohorts and to evaluate underlying mechanisms. Given that up to 14.8% of the US workforce work alternate shift schedules (41), ultimately, ways to reduce stroke risk in occupations requiring nighttime workers may be needed.
Acknowledgments
Author affiliations: Stroke Program, University of Michigan Health System, Ann Arbor, Michigan (Devin L. Brown, Lynda D. Lisabeth); Channing Laboratory, Department of Medicine, Brigham and Women's Hospital and Harvard Medical School, Boston, Massachusetts (Diane Feskanich, Eva S. Schernhammer); Department of Biostatistics, University of Michigan School of Public Health, Ann Arbor, Michigan (Brisa N. Sánchez); Division of Preventive Medicine, Brigham and Women's Hospital, Boston, Massachusetts (Kathryn M. Rexrode); and Department of Epidemiology, University of Michigan School of Public Health, Ann Arbor, Michigan (Lynda D. Lisabeth).
The project was supported by grants HL34594, CA87969, and HL088521, as well as by a grant from the Office of the Vice President for Research, University of Michigan. L. D. L. is supported by a career development award (K23 NS050161) from the National Institute of Neurological Disorders and Stroke, and D. L. B. is supported by a career development award (K23 NS051202) from the National Institute of Neurological Disorders and Stroke.
Conflict of interest: none declared.
Glossary
Abbreviations
- CI
confidence interval
- HR
hazard ratio
References
- 1.American Heart Association. Heart Disease and Stroke Statistics—2006 Update. Dallas, TX: American Heart Association; 2006. [Google Scholar]
- 2.Lumley T, Kronmal RA, Cushman M, et al. A stroke prediction score in the elderly: validation and Web-based application. J Clin Epidemiol. 2002;55(2):129–136. doi: 10.1016/s0895-4356(01)00434-6. [DOI] [PubMed] [Google Scholar]
- 3.Munoz R, Duran-Cantolla J, Martínez-Vila E, et al. Severe sleep apnea and risk of ischemic stroke in the elderly. Stroke. 2006;37(9):2317–2321. doi: 10.1161/01.STR.0000236560.15735.0f. [DOI] [PubMed] [Google Scholar]
- 4.Qureshi AI, Giles WH, Croft JB, et al. Habitual sleep patterns and risk for stroke and coronary heart disease: a 10-year follow-up from NHANES I. Neurology. 1997;48(4):904–911. doi: 10.1212/wnl.48.4.904. [DOI] [PubMed] [Google Scholar]
- 5.Pilcher JJ, Lambert BJ, Huffcutt AI. Differential effects of permanent and rotating shifts on self-report sleep length: a meta-analytic review. Sleep. 2000;23(2):155–163. [PubMed] [Google Scholar]
- 6.van Amelsvoort LG, Jansen NW, Kant I. Smoking among shift workers: more than a confounding factor. Chronobiol Int. 2006;23(6):1105–1113. doi: 10.1080/07420520601089539. [DOI] [PubMed] [Google Scholar]
- 7.Ghiasvand M, Heshmat R, Golpira R, et al. Shift working and risk of lipid disorders: a cross-sectional study [electronic article] Lipids Health Dis. 2006;5:9. doi: 10.1186/1476-511X-5-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oishi M, Suwazono Y, Sakata K, et al. A longitudinal study on the relationship between shift work and the progression of hypertension in male Japanese workers. J Hypertens. 2005;23(12):2173–2178. doi: 10.1097/01.hjh.0000189870.55914.b3. [DOI] [PubMed] [Google Scholar]
- 9.Costa G, Bertoldi A, Kovacic M, et al. Hormonal secretion of nurses engaged in fast-rotating shift systems. Int J Occup Environ Health. 1997;3(supp 2):S35–S39. [PubMed] [Google Scholar]
- 10.Kawachi I, Colditz GA, Stampfer MJ, et al. Prospective study of shift work and risk of coronary heart disease in women. Circulation. 1995;92(11):3178–3182. doi: 10.1161/01.cir.92.11.3178. [DOI] [PubMed] [Google Scholar]
- 11.Fujino Y, Iso H, Tamakoshi A, et al. A prospective cohort study of shift work and risk of ischemic heart disease in Japanese male workers. Am J Epidemiol. 2006;164(2):128–135. doi: 10.1093/aje/kwj185. [DOI] [PubMed] [Google Scholar]
- 12.Knutsson A, Akerstedt T, Jonsson BG, et al. Increased risk of ischaemic heart disease in shift workers. Lancet. 1986;2(8498):89–92. doi: 10.1016/s0140-6736(86)91619-3. [DOI] [PubMed] [Google Scholar]
- 13.Taylor PJ, Pocock SJ. Mortality of shift and day workers 1956–68. Br J Ind Med. 1972;29(2):201–207. doi: 10.1136/oem.29.2.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Karlsson B, Alfredsson L, Knutsson A, et al. Total mortality and cause-specific mortality of Swedish shift- and dayworkers in the pulp and paper industry in 1952–2001. Scand J Work Environ Health. 2005;31(1):30–35. doi: 10.5271/sjweh.845. [DOI] [PubMed] [Google Scholar]
- 15.Virtanen SV, Notkola V. Socioeconomic inequalities in cardiovascular mortality and the role of work: a register study of Finnish men. Int J Epidemiol. 2002;31(3):614–621. doi: 10.1093/ije/31.3.614. [DOI] [PubMed] [Google Scholar]
- 16.Hermansson J, Gillander Gådin K, Karlsson B, et al. Ischemic stroke and shift work. Scand J Work Environ Health. 2007;33(6):435–439. doi: 10.5271/sjweh.1165. [DOI] [PubMed] [Google Scholar]
- 17.Stampfer MJ, Willett WC, Speizer FE, et al. Test of the National Death Index. Am J Epidemiol. 1984;119(5):837–839. doi: 10.1093/oxfordjournals.aje.a113804. [DOI] [PubMed] [Google Scholar]
- 18.Stampfer MJ, Willett WC, Colditz GA, et al. A prospective study of postmenopausal estrogen therapy and coronary heart disease. N Engl J Med. 1985;313(17):1044–1049. doi: 10.1056/NEJM198510243131703. [DOI] [PubMed] [Google Scholar]
- 19.Sacco RL, Boden-Albala B, Gan R, et al. Stroke incidence among white, black, and Hispanic residents of an urban community: the Northern Manhattan Stroke Study. Am J Epidemiol. 1998;147(3):259–268. doi: 10.1093/oxfordjournals.aje.a009445. [DOI] [PubMed] [Google Scholar]
- 20.Walker AE, Robins M, Weinfeld FD. The National Survey of Stroke. Clinical findings. Stroke. 1981;12(2 pt 2 suppl 1):I13–I44. [PubMed] [Google Scholar]
- 21.Yaggi HK, Concato J, Kernan WN, et al. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353(19):2034–2041. doi: 10.1056/NEJMoa043104. [DOI] [PubMed] [Google Scholar]
- 22.Chen JC, Brunner RL, Ren H, et al. Sleep duration and risk of ischemic stroke in postmenopausal women. Stroke. 2008;39(12):3185–3192. doi: 10.1161/STROKEAHA.108.521773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Desai AV, Marks G, Grunstein R. Does sleep deprivation worsen mild obstructive sleep apnea? Sleep. 2003;26(8):1038–1041. doi: 10.1093/sleep/26.8.1038. [DOI] [PubMed] [Google Scholar]
- 24.Brainard GC, Kavet R, Kheifets LI. The relationship between electromagnetic field and light exposures to melatonin and breast cancer risk: a review of the relevant literature. J Pineal Res. 1999;26(2):65–100. doi: 10.1111/j.1600-079x.1999.tb00568.x. [DOI] [PubMed] [Google Scholar]
- 25.Schernhammer ES, Rosner B, Willett WC, et al. Epidemiology of urinary melatonin in women and its relation to other hormones and night work. Cancer Epidemiol Biomarkers Prev. 2004;13(6):936–943. [PubMed] [Google Scholar]
- 26.Hansen AM, Garde AH, Hansen J. Diurnal urinary 6-sulfatoxymelatonin levels among healthy Danish nurses during work and leisure time. Chronobiol Int. 2006;23(6):1203–1215. doi: 10.1080/07420520601100955. [DOI] [PubMed] [Google Scholar]
- 27.Tengattini S, Reiter RJ, Tan DX, et al. Cardiovascular diseases: protective effects of melatonin. J Pineal Res. 2008;44(1):16–25. doi: 10.1111/j.1600-079X.2007.00518.x. [DOI] [PubMed] [Google Scholar]
- 28.Reiter RJ, Tan DX, Osuna C, et al. Actions of melatonin in the reduction of oxidative stress. A review. J Biomed Sci. 2000;7(6):444–458. doi: 10.1007/BF02253360. [DOI] [PubMed] [Google Scholar]
- 29.Wirtz PH, Spillmann M, Bärtschi C, et al. Oral melatonin reduces blood coagulation activity: a placebo-controlled study in healthy young men. J Pineal Res. 2008;44(2):127–133. doi: 10.1111/j.1600-079X.2007.00499.x. [DOI] [PubMed] [Google Scholar]
- 30.Scheer FA, Van Montfrans GA, van Someren EJ, et al. Daily nighttime melatonin reduces blood pressure in male patients with essential hypertension. Hypertension. 2004;43(2):192–197. doi: 10.1161/01.HYP.0000113293.15186.3b. [DOI] [PubMed] [Google Scholar]
- 31.Grossman E, Laudon M, Yalcin R, et al. Melatonin reduces night blood pressure in patients with nocturnal hypertension. Am J Med. 2006;119(10):898–902. doi: 10.1016/j.amjmed.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 32.Ha M, Park J. Shiftwork and metabolic risk factors of cardiovascular disease. J Occup Health. 2005;47(2):89–96. doi: 10.1539/joh.47.89. [DOI] [PubMed] [Google Scholar]
- 33.Di Lorenzo L, De Pergola G, Zocchetti C, et al. Effect of shift work on body mass index: results of a study performed in 319 glucose-tolerant men working in a southern Italian industry. Int J Obes Relat Metab Disord. 2003;27(11):1353–1358. doi: 10.1038/sj.ijo.0802419. [DOI] [PubMed] [Google Scholar]
- 34.Hannerz H, Albertsen K, Nielsen ML, et al. Occupational factors and 5-year weight change among men in a Danish national cohort. Health Psychol. 2004;23(3):283–288. doi: 10.1037/0278-6133.23.3.283. [DOI] [PubMed] [Google Scholar]
- 35.Yamasaki F, Schwartz JE, Gerber LM, et al. Impact of shift work and race/ethnicity on the diurnal rhythm of blood pressure and catecholamines. Hypertension. 1998;32(3):417–423. doi: 10.1161/01.hyp.32.3.417. [DOI] [PubMed] [Google Scholar]
- 36.Tuchsen F, Hannerz H, Burr H. A 12 year prospective study of circulatory disease among Danish shift workers. Occup Environ Med. 2006;63(7):451–455. doi: 10.1136/oem.2006.026716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ellingsen T, Bener A, Gehani AA. Study of shift work and risk of coronary events. J R Soc Health. 2007;127(6):265–267. doi: 10.1177/1466424007083702. [DOI] [PubMed] [Google Scholar]
- 38.Avendano M, Kawachi I, Van Lenthe F, et al. Socioeconomic status and stroke incidence in the US elderly: the role of risk factors in the EPESE Study. Stroke. 2006;37(6):1368–1373. doi: 10.1161/01.STR.0000221702.75002.66. [DOI] [PubMed] [Google Scholar]
- 39.Cox AM, McKevitt C, Rudd AG, et al. Socioeconomic status and stroke. Lancet Neurol. 2006;5(2):181–188. doi: 10.1016/S1474-4422(06)70351-9. [DOI] [PubMed] [Google Scholar]
- 40.Yadegarfar G, McNamee R. Shift work, confounding and death from ischaemic heart disease. Occup Environ Med. 2008;65(3):158–163. doi: 10.1136/oem.2006.030627. [DOI] [PubMed] [Google Scholar]
- 41.Washington, DC: US Department of Labor; 2005. Workers on flexible and shift schedules in May 2004. ( http://www.bls.gov/news.release/History/flex.txt). (Accessed April 7, 2008) [Google Scholar]