Abstract
It is unknown whether caregivers who perform more caregiving tasks have a greater decline in health from higher stress or less decline because of better health, staying active, or psychological factors. This 1999−2004 US study examined caregiving intensity and 2-year change in performance-based functioning among 901 elderly women from the Caregiver-Study of Osteoporotic Fractures sample. Caregivers were categorized as high (n = 167) or low (n = 166) intensity based on how many activities of daily living they performed for the care recipient. Caregiving intensity status and physical performance score (sum of quartiles of walking pace, grip strength, and chair-stand speed; range, 0–9) were assessed at baseline and at 2 annual follow-up interviews. At baseline, high-intensity caregivers reported the most stress but had the best physical functioning; noncaregivers (n = 568) had the poorest physical functioning (adjusted scores = 5.09 vs. 4.54, P = 0.03). Low-intensity caregivers declined more than noncaregivers over 2 years, but high-intensity caregivers did not (adjusted difference = −0.33, P = 0.07 vs. 0.03, P = 0.89). Among respondents with the same caregiving status at baseline and 1-year interviews, high-intensity caregivers maintained the highest physical performance throughout follow-up. Higher levels of physical performance persisted over 2 years among high-intensity caregivers, which did not support the traditional stress hypothesis.
Keywords: activities of daily living, caregivers, disability evaluation
Caregivers consistently report higher levels of stress than noncaregivers do (1). According to theories of stress and health (2, 3), caregivers should have higher rates of health decline because of chronic stress. Furthermore, health decline should be greater among caregivers who perform more caregiving activities (i.e., high-intensity caregivers) because they are more stressed as a result of spending more time caregiving, caring for persons with more debilitating illnesses that require more care, or trying to balance caregiving and other responsibilities (4). However, studies provide inconsistent support for this theory: some studies found modestly elevated mortality rates among elderly caregivers (5, 6), but others found inconsistent or no associations (7, 8). Moreover, although high-intensity caregivers had a greater incidence of fatal and nonfatal coronary disease compared with noncaregivers in one study of middle-aged and elderly women (7), another study found inconsistent associations of high-intensity caregiving with mortality and incident mobility limitations in elderly adults (8).
These results may be explained by the “healthy caregiver” hypothesis. That is, elderly adults who become caregivers are healthier (9) and more physically active (10) than their peers. Caregivers may stay active through performing caregiving tasks, or they may maintain their health in order to continue assisting their care recipient. The current study tested both the stress hypothesis and the healthy caregiver hypothesis by evaluating the associations between caregiving status and change in physical-performance-based functioning over 2 years in a large, population-based sample of older women.
Performance-based functioning was selected as the outcome for several reasons. First, better functioning according to performance-based summary scales and individual performance-based measures has been associated with less stress (11, 12) and more physical activity (13–15). Thus, these measures are applicable to both the stress and the healthy caregiver hypotheses. Second, caregiving is dynamic: over a year, noncaregivers may start caregiving, or caregivers may cease caregiving or change their level of involvement in care-related activities. Change in performance-based functioning may be better than mortality or disease incidence at revealing short-term health effects of these transitions. Third, poorer performance-based functioning is a risk factor for health decline (16) and mortality (17). Therefore, it would be important to determine whether caregivers are more likely than noncaregivers to decline in performance-based functioning in order to prevent subsequent adverse health outcomes.
The current study (1999−2004) assessed caregiving intensity at 3 annual interviews, which enabled us to evaluate how change in functioning was influenced by caregiving intensity measured at various interview points: 1) baseline only, 2) baseline and the first follow-up interview among respondents whose level of caregiving intensity was the same at both interviews, and 3) baseline and first follow-up interviews according to the respondent's current caregiving status at these interviews. The third variation captured the dynamic aspect of caregiving by incorporating transition in caregiver status.
To test the stress hypothesis, we theorized that caregivers would decline more in functioning over 2 years than noncaregivers would and that high-intensity caregivers would decline the most. Alternatively, the healthy caregiver hypothesis would predict that caregivers would decline less in functioning than noncaregivers would and that high-intensity caregivers would decline the least, especially those who remained high-intensity caregivers.
MATERIALS AND METHODS
Sample
The participants in these analyses were enrolled in the Study of Osteoporotic Fractures (SOF) (18). The SOF sample included 9,704 women who were at least 65 years of age and were recruited between 1986 and 1988 from population-based listings in 4 areas of the United States: Baltimore, Maryland; Minneapolis, Minnesota; Portland, Oregon; and the Monongahela Valley, Pennsylvania. Women were excluded if they could not walk without help or had a history of bilateral hip replacement. Although African-American women were initially excluded because of their low incidence of hip fracture, 662 elderly African-American women with similar characteristics were enrolled in 1996–1997. Approximately every 2 years, SOF participants undergo a comprehensive clinical evaluation. Caregiver-SOF participants included members of the original and African-American SOF cohorts who participated in the sixth biennial examination that took place from 1997 to 1999.
Caregiver-SOF subsample
The study sample was identified in 2 phases, described elsewhere (19). The first phase consisted of administering a caregiver screening questionnaire to 5,952 SOF participants who had their sixth biennial examination at their home or a SOF clinic and were not cognitively impaired or living in long-term-care facilities. The second phase began in 1999 and consisted of readministering the screening questionnaire by telephone to all caregivers and a subset of noncaregivers who had been identified by the initial screening questionnaire. The questionnaire asked SOF participants if they currently helped a relative or friend with each of 7 instrumental activities of daily living (IADL) tasks (use the telephone, get to places out of walking distance, shop, prepare meals, manage medications, manage finances, do heavy housework (20)) and 7 basic activities of daily living (ADL) tasks (walk across a room, groom, transfer from bed to chair, eat, dress, bathe, use the toilet (21)) because that person was physically, cognitively, or mentally unable to do that task independently. Participants were categorized as caregivers if they helped one or more persons with at least one task, and as noncaregivers if they did not help anyone with these tasks.
In the telephone reevaluation phase, respondents who were currently caregiving were invited to participate in Caregiver-SOF; those who had stopped caregiving (n = 493) were excluded. For each caregiver participant, we matched 1 or 2 noncaregivers on SOF site, age, race, and US zip code. The resulting sample included 375 caregivers and 694 noncaregivers.
Data collection
Face-to-face interviews were conducted with the respondent at her home within 2 weeks of the telephone reevaluation (i.e., Caregiver-SOF baseline interview; 1999−2002) and at 2 annual follow-up interviews (2002−2004). This study was approved by the institutional review boards at each SOF site and the Boston University Medical Center (Massachusetts). All participants provided written informed consent.
Measures
Caregiving status.
Caregiver status was based on the respondent's report that she assisted someone with at least one IADL/ADL task, as described above. Caregiver status was assessed at each interview.
Caregiving intensity.
Caregiving intensity was determined by the number of IADL and ADL tasks the caregiver performed for the main care recipient. “High-intensity” caregivers helped with 6 or more IADL tasks or 2 or more ADL tasks. “Low-intensity” caregivers helped with 0–5 IADL tasks and 0–1 ADL tasks (but not 0 IADL and 0 ADL tasks). These cutpoints were chosen because they were the median values at baseline, thereby yielding equal baseline numbers of high- and low-intensity caregivers.
Physical-performance-based functioning.
Three performance-based measures were obtained at each interview: usual walking speed, grip strength, and chair-stand speed. Usual walking speed was calculated as the average of 2 timed walks over a 2-, 3-, or 6-m course at usual pace (meters/second). Maximum grip strength (kilograms) was measured by using a handheld dynamometer while the respondent was in a standing position (22). The average of 2 trials with each hand was obtained. Chair-stand speed was the number of seconds required to rise 5 times from a seated position on a straight-back chair without using one's arms. The sample-based distribution for each measure was categorized into quartiles. Respondents who could not perform the task were included in the lowest quartile. A summary score was created by summing the quartiles in which the respondent was categorized for each performance-based measure. Scores could range from 0 to 9 (9 being in the highest quartile for all 3 tasks). If one or more performance-based measures was missing at a given interview, no summary score was calculated.
Covariables.
Sociodemographic variables were based on the respondent's age at the Caregiver-SOF baseline interview and self-reported race (white or African American), highest level of education (dichotomized as high school graduate or higher vs. not graduated from high school), and current marital status (married vs. other). Limitations in IADLs and ADLs were based on the respondent's self-reported ability to independently perform each of the IADLs and ADLs listed above. Separate variables were constructed for the total number of IADL (0–7) and ADL (0–7) limitations. Body mass index (weight in kilograms divided by height in meters squared) at the Caregiver-SOF baseline and first follow-up interviews was based on the respondent's weight at that interview and her height, measured at her baseline SOF visit. Perceived stress was measured by the Perceived Stress Scale (23). This 14-item scale measures general stress experienced in the past month, with higher scores indicating more stress (possible range, 0–56). Perceived stress was used as a continuous variable in these analyses.
Caregiving characteristics.
Dichotomous variables indicated whether caregivers cared for a spouse versus another relative or friend, lived with the care recipient, and had scheduled time away from caregiving. Also assessed was whether the care recipient had dementia or a stroke.
Statistical methods
We compared baseline characteristics of high- and low-intensity caregivers and noncaregivers using analysis of variance for continuous variables and chi-square tests for categorical variables. We tested the hypotheses regarding change in physical-performance-based functioning score across the study period by fitting a linear mixed-effects model to the data. Baseline performance score was included as a covariate. Baseline caregiving intensity, time (to indicate follow-up interviews), and their interaction were included as fixed effects in the model. The covariance for each participant at different time points was modeled by a compound symmetry structure. Additional baseline variables were included as potential confounders if they were independently associated with caregiving intensity and performance score at baseline. All potential confounders were included in the initial model, and manual backward elimination was used to delete single variables if they were not statistically significant (P = 0.20) or their elimination did not meaningfully change the association between caregiving intensity and change in performance-based functioning. Changes in functioning between high- and low-intensity caregivers and noncaregivers were compared by computing the differences in least-square means for the performance-based functioning score at baseline versus the score at each follow-up interview.
Model with time-dependent covariates
To evaluate the association between current caregiving status and change in performance-based functioning over the next follow-up interval, we included current caregiver status at the baseline and first follow-up interviews in a mixed-effects model. In addition, we included variables from the first follow-up interview that were potential time-varying characteristics of the respondent and the caregiving situation. These variables were body mass index, Perceived Stress Scale score, number of IADL and ADL limitations of the respondent, and scheduled time away from caregiving.
All analyses were performed by using PROC MIXED in SAS 9.1 software (24).
RESULTS
The sample included 901 respondents who had performance-based functioning scores at 2 or 3 interviews. All respondents were women, 88% were white, and their mean age was 81.0 years (range, 70–94); 37% were caregivers. A total of 655 (73%) respondents completed all 3 performance measures at all interviews, while 57 (6%) and 189 (21%) respondents were missing one or more performance measures at the second and third interviews, respectively. Compared with the 168 participants excluded because they were missing performance-based measures at baseline (n = 67), had died before the first (n = 35) or second (n = 18) follow-up interview, or lacked performance-based measures at the first follow-up interview (n = 48), respondents included in these analyses were more likely to be younger, be married, and be better educated, and they had more stress and fewer ADL and IADL limitations but did not differ regarding race or body mass index. They were more likely to be caregivers at baseline (89% of caregivers vs. 82% of noncaregivers were included).
Caregivers were more likely than noncaregivers to be married and have fewer IADL limitations (Table 1). High-intensity caregivers reported more stress than other respondents did. Low-intensity caregivers had the best unadjusted performance-based functioning, whereas noncaregivers had the worst.
Table 1.
Baseline Characteristicsa of the Study Sample According to Baseline Caregiving Intensity Level Among 901 Caregiver-Study of Osteoporotic Fractures Participants, 1999–2002
| Characteristic | Caregiving Intensity Level |
P Value | ||
| Noncaregivers (n = 568) | Low-intensity Caregivers (n = 166) | High-intensity Caregivers (n = 167) | ||
| Demographic and health | ||||
| Age, years | 81.18 (3.60) | 80.84 (3.61) | 80.68 (3.31) | 0.219 |
| White race | 88.91 | 87.35 | 86.83 | 0.707 |
| Highest educational level: ≥high school | 52.11 | 58.43 | 58.08 | 0.202 |
| Marital status: married | 27.82 | 39.16 | 71.26 | <0.001 |
| Body mass index, kg/m2 | 27.26 (5.14) | 27.51 (5.13) | 26.84 (5.09) | 0.482 |
| No. of ADL limitations | 0.38 (0.67) | 0.30 (0.57) | 0.37 (0.63) | 0.344 |
| No. of IADL limitations | 0.70 (1.18) | 0.27 (0.59) | 0.39 (0.70) | <0.001 |
| Perceived Stress Scale score | 15.04 (6.91) | 15.96 (7.32) | 18.88 (7.91) | <0.001 |
| Caregiving | ||||
| Spouse of care recipient | 25.90 | 67.07 | <0.001 | |
| Lives with care recipient | 29.52 | 70.66 | <0.001 | |
| Care recipient has dementia | 16.27 | 37.72 | <0.001 | |
| Care recipient has stroke | 14.46 | 26.95 | 0.005 | |
| Has time away from caregiving | 81.33 | 72.46 | 0.055 | |
| Performance-based functioning score | ||||
| Time 1 | 4.53 (2.32) | 5.10 (2.21) | 4.95 (2.38) | 0.006 |
| Time 2 | 4.44 (2.44) | 5.03 (2.44) | 4.61 (2.43) | 0.028 |
| Time 3 | 4.47 (2.59) | 4.54 (2.43) | 4.76 (2.61) | 0.492 |
Abbreviations: ADL, activities of daily living; IADL, instrumental activities of daily living.
Values are expressed as mean (standard deviation) or %.
Most respondents remained at the same caregiving intensity level at the first 2 interviews: 70% of high-intensity caregivers, 58% of low-intensity caregivers, and 85% of noncaregivers (Table 2). Performance-based functioning declined over this period in all groups except for noncaregivers who became low-intensity caregivers and for low-intensity caregivers who became high-intensity caregivers (adjusted mean change = 0.12 and 0.20, respectively). High-intensity caregivers who stopped caregiving experienced the most decline (adjusted mean change = −0.69).
Table 2.
Caregiver Intensity Level at the Baseline and First Follow-up Interviews, and Adjusted Change in Performance-based Functioning Among Caregiver-Study of Osteoporotic Fractures Participants, 1999–2004
| Level at the Baseline Interview | Level at the First Follow-up Interviewa | Baseline Respondents at Each Level at the First Follow-up Interview |
Adjustedb Change in Performance Score From Baseline to the First Follow-up Interview, Mean (SE) | |
| No. | % | |||
| Noncaregiver (n = 563) | Noncaregiver | 521 | 85.27 | −0.28 (0.08)c |
| Low-intensity caregiver | 37 | 26.81 | 0.12 (0.27) | |
| High-intensity caregiver | 5 | 3.42 | −0.58 (0.78) | |
| Low-intensity caregiver (n = 166) | Noncaregiver | 47 | 7.69 | −0.10 (0.24) |
| Low-intensity caregiver | 80 | 57.97 | −0.16 (0.18) | |
| High-intensity caregiver | 39 | 26.71 | 0.20 (0.27) | |
| High-intensity caregiver (n = 166) | Noncaregiver | 43 | 7.04 | −0.63 (0.26)c |
| Low-intensity caregiver | 21 | 15.22 | −0.03 (0.35) | |
| High-intensity caregiver | 102 | 69.86 | −0.09 (0.20) | |
Abbreviation: SE, standard error.
For 6 participants (5 noncaregivers and 1 high-intensity caregiver), information on caregiver status at the first follow-up interview was missing.
Adjusted for baseline performance score, instrumental activities of daily living limitations, caregiver lives with care recipient, and has time away from caregiving.
Significant at 0.05.
Table 3 presents the adjusted change in physical functioning from baseline to each follow-up interview for the 3 random-effects models. Model A was based on baseline caregiving intensity status only; model B included 182 caregivers and 512 noncaregivers whose caregiving intensity status remained the same for the first 2 interviews; and model C incorporated current caregiving intensity status at the first follow-up interview as a time-varying covariate. At baseline, both high- and low-intensity caregivers had slightly better performance-based functioning than noncaregivers did: adjusted scores were 4.53 for noncaregivers, 4.93 for low-intensity caregivers (P = 0.047), and 5.09 for high-intensity caregivers (P = 0.03).
Table 3.
Adjusted Difference in Mean Change in Performance-based Functioning From Baseline to the First and Second Follow-up Interviews in High- and Low-intensity Caregivers Versus Noncaregivers Among 901 Caregiver-Study of Osteoporotic Fractures Participants, 1999–2004
| Model Aa |
Model Bb |
Model Cc |
||||
| Estimate (SE) | P Value | Estimate (SE) | P Value | Estimate (SE) | P Value | |
| Independent variables | ||||||
| Baseline to the first follow-up interview | ||||||
| Intercept | 4.22 (1.42) | 0.00 | 4.53 (1.65) | 0.00 | 3.89 (1.39) | 0.00 |
| High-intensity caregiver vs. noncaregiver | −0.05 (0.21) | 0.81 | 0.28 (0.31) | 0.36 | −0.22 (0.16) | 0.19 |
| Low-intensity caregiver vs. noncaregiver | 0.14 (0.17) | 0.40 | 0.20 (0.22) | 0.36 | 0.12 (0.16) | 0.46 |
| Baseline to the second follow-up interview | ||||||
| Intercept | 4.20 (1.42) | 0.00 | 4.50 (1.65) | 0.00 | 3.98 (1.38) | 0.00 |
| High-intensity caregiver vs. noncaregiver | 0.03 (0.21) | 0.89 | 0.38 (0.31) | 0.23 | −0.02 (0.18) | 0.91 |
| Low-intensity caregiver vs. noncaregiver | −0.33 (0.18) | 0.07 | −0.59 (0.24) | 0.01 | −0.53 (0.20) | 0.01 |
| Covariables | ||||||
| Performance at baseline | −0.29 (0.02) | <0.0001 | −0.30 (0.03) | <0.0001 | −0.28 (0.02) | <0.0001 |
| Age at baseline | −0.03 (0.02) | 0.07 | −0.03 (0.02) | 0.07 | −0.03 (0.02) | 0.06 |
| African-American race | −0.33 (0.17) | 0.06 | −0.29 (0.20) | 0.15 | −0.32 (0.17) | 0.06 |
| Education: ≥high school graduate | −0.17 (0.10) | 0.10 | −0.20 (0.12) | 0.09 | −0.16 (0.10) | 0.12 |
| No. of IADL limitationsd | −0.26 (0.06) | <0.0001 | −0.27 (0.06) | <0.0001 | −0.20 (0.05) | <0.0001 |
| Caregiver lives with care recipient | −0.29 (0.19) | 0.13 | −0.46 (0.29) | 0.12 | ||
| Caregiver has time away from caregivingd | −0.43 (0.21) | 0.04 | −0.32 (0.18) | 0.08 | ||
Abbreviations: IADL, instrumental activities of daily living; SE, standard error.
Caregiving intensity status at the baseline interview only.
Caregiving intensity status at the first interview; includes only those participants whose status did not change from the first to the second interview.
Current caregiving intensity status at the first and second interview.
Time-dependent predictors in model C.
All groups declined in functioning over the study period. Decline in caregivers and noncaregivers did not differ significantly from baseline to the first follow-up interview. However, between baseline and the second follow-up interview, low-intensity caregivers declined more than noncaregivers according to all models: the difference in adjusted performance scores between these 2 groups ranged from −0.33 (P = 0.07) in model A to −0.59 (P = 0.01) in model B. As shown in model C, current caregiving intensity at baseline and the first follow-up interview had different influences on change in functioning over the subsequent follow-up period (i.e., there was a statistically significant interaction between time and caregiving intensity, P = 0.005).
The associations that were most affected by the method of modeling caregiving intensity were found among high-intensity caregivers (Figure 1). When caregiving intensity was modeled according to baseline status alone (model A) or current status (model C), high-intensity caregivers declined over the first year of follow-up (adjusted mean change = −0.31, P = 0.07 and −0.46, P = 0.001, respectively) yet had virtually no change over the second year of follow-up in model A and a nonsignificant trend toward improved functioning in model C. In contrast, when analyses were restricted to respondents who were in the same intensity category at baseline and the first follow-up interview (model B), high-intensity caregivers exhibited no perceptible change over the entire study period. By comparison, low-intensity caregivers showed little change over the first year of follow-up but declined more than the other groups over the second year of follow-up in all 3 models (adjusted mean change ranged from −0.57, P < 0.001 in model A to −0.92, P < 0.001 in model B). Likewise, noncaregivers had a small, but significant decline between baseline and the first follow-up interview and a smaller decline over the next follow-up interval in all models (adjusted mean change ranged from −0.24, P = 0.002 in model C to −0.31, P < 0.001 in model B).
Figure 1.
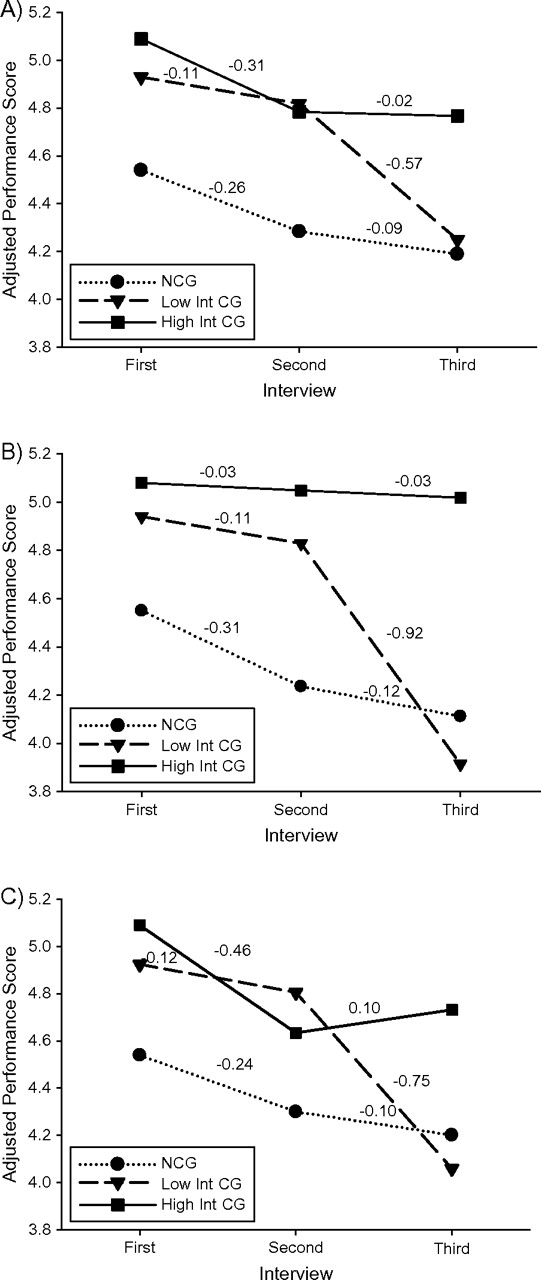
Adjusted means and change in performance score over 2 years among elderly US women in the Caregiver-Study of Osteoporotic Fractures, 1999–2004. Predicting change in performance score from the first interview to the second and third interviews as a function of caregiving intensity status at the first interview. A): Model A, caregiving intensity status at the first interview. B): Model B, caregiving intensity status at the first interview; only those participants whose status did not change from the first to the second interview were included. C): Model C, current caregiving intensity status at the first and second interviews; participants’ caregiving status at baseline and caregiving status at the first follow-up interview. The numbers on the lines represent adjusted mean changes in performance score estimated by the model. NCG, noncaregivers; Low Int CG, low-intensity caregivers; High Int CG, high-intensity caregivers.
DISCUSSION
This study found that low-intensity, but not high-intensity, caregivers declined more in performance-based functioning than noncaregivers did over a 2-year period. This excess decline was concentrated in the second year. Functional decline did not differ significantly between high-intensity caregivers and noncaregivers when we evaluated baseline caregiving status only or adjusted for current caregiving status at the first follow-up interview. However, in analyses restricted to respondents who maintained the same caregiving intensity level at the baseline and first follow-up interviews, performance-based functioning remained high among high-intensity caregivers throughout the follow-up period, while it declined among other respondents. Thus, caregiving intensity was associated with different trajectories of decline, although the absolute change in functional performance for each group was relatively small. These results support the healthy caregiver hypothesis more than the caregiver-stress hypothesis; the caregiver-stress hypothesis may be more appropriate for psychological outcomes rather than physical health outcomes.
The healthy caregiver hypothesis may be viewed as a variation of models of health benefits of physical activity. This hypothesis is based on observations that older adults who become caregivers are physically healthier than other older adults (9) and that older caregivers are more active than noncaregivers (8, 10). The rationale is that caregivers who are healthier are able to undertake more caregiving tasks and that helping with more caregiving tasks reflects higher physical activity (either as a result of caregiving activities or in general). Accordingly, our results are consistent with studies finding that physically active elderly adults experienced less functional decline than their counterparts (15, 25, 26) and, particularly, those who remained physically active experienced the least mobility decline (15).
By contrast, the results of prospective studies on caregiving and physical health decline have been inconsistent (1). Some studies support a caregiving stress hypothesis. For example, higher mortality rates were found for spouse caregivers strained by caregiving tasks but not for those not stressed by these activities (6). However, this study also found that caregivers who helped a spouse with more ADL/IADL tasks reported fewer health risk behaviors over 1 year but did not exhibit changes in perceived health (27). To our knowledge, only one study evaluated respondents’ physical health at more than 2 time points and used analytic techniques similar to those in our study (28). That study found that self-reported physical symptoms increased more over 2 years in caregivers to a relative with dementia than in noncaregivers. Our results may have differed for several reasons: we used a performance-based measure rather than self-report, separated high- and low-intensity caregivers, and adjusted for health and other covariables. In addition, our sample was older, was restricted to women, and included caregivers to persons with dementia and nondementia diagnoses. It is also possible that older caregivers may develop more physical symptoms than noncaregivers do but maintain their physical functioning in order to meet their caregiving responsibilities.
The better functioning experienced by the high-intensity caregivers who continued at that level may be explained by several factors. These women may have had healthier constitutions, since better physical health predisposes elderly adults to become caregivers and remain as caregivers (9). Likewise, they may have stayed healthier through the physical activity of caregiving or intentionally stayed fit to continue helping their care recipient. Also, their greater involvement in caregiving may have given them more satisfaction, resulting in health benefits (29).
This study had several potential limitations. The caregiving-intensity variable was based on the median number of IADL and ADL tasks performed. Thus, each caregiving-intensity group included respondents who performed different types of tasks, reflecting different intensities. For example, helping with one ADL task, such as toileting, may be more time-consuming, physically difficult, and stressful than helping with one IADL task, such as managing finances. Moreover, although high-intensity caregivers reported the most stress, some high-intensity caregivers may have been less stressed by caregiving than some low-intensity caregivers. This variable did not account for number of hours per week that respondents performed these tasks, which also reflects caregiving intensity, and was assessed in previous studies (7, 8). Given the lack of a standard definition of caregiving intensity, number of caregiving tasks provides a more quantifiable, objective measure than asking respondents to rate the intensity of their caregiving involvement. Furthermore, performing more caregiving tasks has been correlated with more daily hours of caregiving (30) and with higher stress in this study and others (31).
Another potential limitation is that noncaregivers were not matched to caregivers on health status, and a third were enrolled 6 months after the caregiver was. We adjusted for baseline health and IADL limitations. Yet, it is unlikely that this lag time, or residual confounding by unmeasured factors (e.g., physical activity, psychological resilience), would have totally explained differences in functioning between caregivers and noncaregivers.
Loss to follow-up from mortality did not differ between caregivers and noncaregivers (4.7% vs. 5.3%, P = 0.65). However, noncaregivers were more likely to lack follow-up performance-based functioning measures. Since poorer health was a reason for lacking these measures, our results most likely underestimated the true differences in decline between caregivers and noncaregivers.
Additionally, the sample comprised elderly women who were mainly white and high functioning, thus limiting generalizability of the results. However, these results apply to the majority of caregivers in the United States, who are elderly women (32). It is unlikely that the mechanisms linking caregiving intensity to performance-based functioning would differ in other groups of older adults. Although the study design enabled us to observe yearly change in functioning over 3 time points, having more follow-up points would reveal more complex trends.
This study also had many strengths. The Caregiver-SOF sample comes from a large, multisite, community-based study of elderly women. Caregivers and noncaregivers were derived from the same source population, thus reducing possible biases related to recruiting caregivers from patient registries and noncaregivers from another source. The inclusion criteria required that caregivers were helping the care recipient with at least one IADL/ADL, thereby minimizing likelihood of misclassification of caregiver status and allowing categorization of high- and low-intensity caregivers by using criteria that can be replicated in other studies. Sensitivity analyses, in which we randomly recategorized 133 caregivers whose intensity values were near the cutpoint for high- and low-intensity and reran model A, showed that our results were robust to misclassification. Reassessment of caregiving intensity status at each annual interview provided insight into the impact of caregiving transitions versus continuation at the same intensity level. Finally, quantification of performance-based functioning was based on measures from previous studies (16, 26).
In conclusion, these results suggest that factors other than psychological stress influence performance-based functioning in older, high-intensity caregivers. Given that this study and others (1) found that caregiving is stressful, future studies should explore the healthy caregiver hypothesis to better understand how caregiving affects physical health in older adults.
Acknowledgments
Author affiliations: Department of Epidemiology, Boston University School of Public Health, Boston, Massachusetts (Lisa Fredman); Department of Biostatistics, Boston University School of Public Health, Boston, Massachusetts (Gheorghe Doros); Department of Medicine and Division of Epidemiology, University of Minnesota, Minneapolis, Minnesota (Kristine E. Ensrud); Division of Rheumatology and Clinical Immunology, Department of Medicine, University of Maryland School of Medicine, Baltimore, Maryland (Marc C. Hochberg); and Department of Epidemiology, University of Pittsburgh, Pittsburgh, Pennsylvania (Jane A. Cauley).
This work was supported by grants and contracts from the National Institutes of Health (AG18037 to L. F.; AG05407, AR35582, AG05394, AR35584, and AR35583 to K. E. E., M. C. H., and J. A. C.).
Conflict of interest: none declared.
Glossary
Abbreviations
- ADL
activities of daily living
- IADL
instrumental activities of daily living
- SOF
Study of Osteoporotic Fractures
References
- 1.Pinquart M, Sörensen S. Differences between caregivers and noncaregivers in psychological health and physical health: a meta-analysis. Psychol Aging. 2003;18(2):250–267. doi: 10.1037/0882-7974.18.2.250. [DOI] [PubMed] [Google Scholar]
- 2.Pearlin LI, Mullan JT, Semple SJ, et al. Caregiving and the stress process: an overview of concepts and their measures. Gerontologist. 1990;30(5):583–594. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- 3.Selye H. The Stress of Life. New York, NY: McGraw-Hill; 1956. [Google Scholar]
- 4.Navaie-Waliser M, Spriggs A, Feldman PH. Informal caregiving: differential experiences by gender. Med Care. 2002;40(12):1249–1259. doi: 10.1097/01.MLR.0000036408.76220.1F. [DOI] [PubMed] [Google Scholar]
- 5.Christakis NA, Allison PD. Mortality after the hospitalization of a spouse. N Engl J Med. 2006;354(7):719–730. doi: 10.1056/NEJMsa050196. [DOI] [PubMed] [Google Scholar]
- 6.Schulz R, Beach SR. Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. JAMA. 1999;282(23):2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- 7.Lee S, Colditz GA, Berkman LF, et al. Caregiving and risk of coronary heart disease in U.S. women, a prospective study. Am J Prev Med. 2003;24(2):113–119. doi: 10.1016/s0749-3797(02)00582-2. [DOI] [PubMed] [Google Scholar]
- 8.Fredman L, Cauley JA, Satterfield S, et al. Caregiving, mortality, and mobility decline: the Health, Aging, and Body Composition (Health ABC) Study. Arch Intern Med. 2008;168(19):2154–2162. doi: 10.1001/archinte.168.19.2154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McCann JJ, Hebert LE, Bienias JL, et al. Predictors of beginning and ending caregiving during a 3-year period in a biracial community population of older adults. Am J Public Health. 2004;94(10):1800–1806. doi: 10.2105/ajph.94.10.1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fredman L, Bertrand RM, Martire LM, et al. Leisure-time exercise and overall physical activity in older women caregivers and non-caregivers from the Caregiver-SOF Study. Prev Med. 2006;43(3):226–229. doi: 10.1016/j.ypmed.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 11.King AC, Baumann K, O'Sullivan P, et al. Effects of moderate-intensity exercise on physiological, behavioral, and emotional responses to family caregiving: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2002;57(1):M26–M36. doi: 10.1093/gerona/57.1.m26. [DOI] [PubMed] [Google Scholar]
- 12.Schnohr P, Kristensen TS, Prescott E, et al. Stress and life dissatisfaction are inversely associated with jogging and other types of physical activity in leisure time—the Copenhagen City Heart Study. Scand J Med Sci Sports. 2005;15(2):107–112. doi: 10.1111/j.1600-0838.2004.00394.x. [DOI] [PubMed] [Google Scholar]
- 13.Newman AB, Haggerty CL, Kritchevsky SB, et al. Walking performance and cardiovascular response: associations with age and morbidity—the Health, Aging and Body Composition Study. J Gerontol A Biol Sci Med Sci. 2003;58(8):715–720. doi: 10.1093/gerona/58.8.m715. [DOI] [PubMed] [Google Scholar]
- 14.King AC, Pruitt LA, Phillips W, et al. Comparative effects of two physical activity programs on measured and perceived physical functioning and other health-related quality of life outcomes in older adults. J Gerontol A Biol Sci Med Sci. 2000;55(2):M74–M83. doi: 10.1093/gerona/55.2.m74. [DOI] [PubMed] [Google Scholar]
- 15.Visser M, Pluijm SM, Stel VS, et al. Physical activity as a determinant of change in mobility performance: the Longitudinal Aging Study Amsterdam. J Am Geriatr Soc. 2002;50(11):1774–1781. doi: 10.1046/j.1532-5415.2002.50504.x. [DOI] [PubMed] [Google Scholar]
- 16.Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55(4):M221–M231. doi: 10.1093/gerona/55.4.m221. [DOI] [PubMed] [Google Scholar]
- 17.Newman AB, Simonsick EM, Naydeck BL, et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA. 2006;295(17):2018–2026. doi: 10.1001/jama.295.17.2018. [DOI] [PubMed] [Google Scholar]
- 18.Cummings SR, Black DM, Nevitt MC, et al. Appendicular bone density and age predict hip fracture in women. The Study of Osteoporotic Fractures Research Group. JAMA. 1990;263(5):665–668. [PubMed] [Google Scholar]
- 19.Fredman L, Tennstedt S, Smyth KA, et al. Pragmatic and internal validity issues in sampling in caregiver studies: a comparison of population-based, registry-based, and ancillary studies. J Aging Health. 2004;16(2):175–203. doi: 10.1177/0898264303262639. [DOI] [PubMed] [Google Scholar]
- 20.Multidimensional Functional Assessment: The OARS Methodology. Durham, NC: Duke University Center for the Study of Aging and Human Development; 1978. [Google Scholar]
- 21.Katz S, Ford AB, Moskowitz RW, et al. Studies on illness in the aged. The Index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 22.Ensrud KE, Nevitt MC, Yunis C, et al. Correlates of impaired function in older women. J Am Geriatr Soc. 1994;42(5):481–489. doi: 10.1111/j.1532-5415.1994.tb04968.x. [DOI] [PubMed] [Google Scholar]
- 23.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 24.SAS Institute, Inc. SAS version 9.1. Cary, NC: SAS Institute, Inc;; 2002–2003. [Google Scholar]
- 25.Buchman AS, Wilson RS, Boyle PA, et al. Physical activity and leg strength predict decline in mobility performance in older persons. J Am Geriatr Soc. 2007;55(10):1618–1623. doi: 10.1111/j.1532-5415.2007.01359.x. [DOI] [PubMed] [Google Scholar]
- 26.Seeman T, Chen X. Risk and protective factors for physical functioning in older adults with and without chronic conditions: MacArthur Studies of Successful Aging. J Gerontol B Psychol Sci Soc Sci. 2002;57(3):S135–S144. doi: 10.1093/geronb/57.3.s135. [DOI] [PubMed] [Google Scholar]
- 27.Beach SR, Schulz R, Yee JL, et al. Negative and positive health effects of caring for a disabled spouse: longitudinal findings from the caregiver health effects study. Psychol Aging. 2000;15(2):259–271. doi: 10.1037//0882-7974.15.2.259. [DOI] [PubMed] [Google Scholar]
- 28.Roth DL, Haley WE, Owen JE, et al. Latent growth models of the longitudinal effects of dementia caregiving: a comparison of African American and White family caregivers. Psychol Aging. 2001;16(3):427–436. [PubMed] [Google Scholar]
- 29.Gruenewald TL, Karlamangla AS, Greendale GA, et al. Feelings of usefulness to others, disability, and mortality in older adults: the MacArthur Study of Successful Aging. J Gerontol B Psychol Sci Soc Sci. 2007;62(1):P28–P37. doi: 10.1093/geronb/62.1.p28. [DOI] [PubMed] [Google Scholar]
- 30.Desbiens NA, Mueller-Rizner N, Virnig B, et al. Stress in caregivers of hospitalized oldest-old patients. J Gerontol A Biol Sci Med Sci. 2001;56(4):M231–M235. doi: 10.1093/gerona/56.4.m231. [DOI] [PubMed] [Google Scholar]
- 31.Pinquart M, Sörensen S. Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: a meta-analysis. J Gerontol B Psychol Sci Soc Sci. 2003;58(2):P112–P128. doi: 10.1093/geronb/58.2.p112. [DOI] [PubMed] [Google Scholar]
- 32.Caregiving in the U.S. Bethesda, MD: National Alliance for Caregiving and AARP; 2004. [Google Scholar]


