Abstract
The association of psychosocial stress with weight gain may have important implications for clinical practice and workplace and public health interventions. To determine whether multiple domains of psychosocial stress were associated with weight gain from 1995 to 2004, the authors analyzed a nationally representative longitudinal cohort of 1,355 men and women in the United States. Change in body mass index was assessed for multiple domains of psychosocial stress related to work, personal relationships, life constraints, and finances, controlling for other factors associated with weight gain. All analyses were stratified by sex and weighted to account for the complex survey design. Among men with high baseline body mass index, weight gain was associated with increasing levels of psychosocial stress related to job-related demands (P < 0.001 for interaction with baseline body mass index), lack of skill discretion (P = 0.014), lack of decision authority (P = 0.026), and difficulty paying bills (P = 0.004). Among women with high baseline body mass index, weight gain was associated with job-related demands (P < 0.001 for interaction with baseline body mass index), perceived constraints in life (P < 0.001), strain in relations with family (P = 0.016), and difficulty paying bills (P = 0.010). Interventions to address psychosocial stress may limit weight gain among overweight and obese men and women.
Keywords: body mass index; longitudinal studies; obesity; overweight; stress, psychological; weight gain
Psychosocial stress has been implicated as a risk factor for high blood pressure, cardiovascular disease, and cancer (1–7). The association between stress and long-term weight gain is less clear. Stress may contribute to changes in dietary behaviors that lead to weight change, with various effects related to sex (8–10), baseline body mass index (11), or cortisol reactivity in response to stress (12, 13). These factors may cause some people to gain more weight under stressful circumstances, while others may gain less weight or even lose weight when stressed.
Cross-sectional studies have reported only weak associations between psychosocial stress and body mass index (14). Three longitudinal cohort studies conducted in populations outside the United States have produced mixed results. Kivimaki et al. (11) used the Whitehall study, a prospective cohort of British civil servants, to analyze the prospective association between work stress and weight change over 5 years. They found that greater job strain and lesser job control at baseline were associated with weight gain among men who were overweight or obese at baseline, but a similar association was not observed among women. Brunner et al. (15) completed an additional analysis of the same cohort after further follow-up. They reported that men with chronic job strain, coupled with low social support among co-workers, were more likely to develop obesity (body mass index, ≥30 kg/m2) and central obesity (waist circumference, >102 cm in men and >88 cm in women) than those who had no job strain. In a Dutch cohort, Van Strien et al. (16) showed that men who were “emotional eaters” experienced weight gain over the 6 months after a negative life event, such as death of a family member, divorce or separation from a spouse, or financial difficulties. Korkeila et al. (17) found an association between neuroticism and weight gain among women over 6 years in a cohort of Finnish twins, but this effect subsided after 15 years of follow-up.
Based on this prior research, the objective of the current study was to assess the association of weight gain with numerous types of psychosocial stress related to work, personal relationships, life constraints, and finances over approximately 9 years in a nationally representative cohort of adults in the United States. We hypothesized, on the basis of prior research (11), that baseline body mass index would be an effect modifier of the relation between psychosocial stress and weight gain, and we tested for this effect in all statistical models.
MATERIALS AND METHODS
Study population
The Midlife in the United States (MIDUS) study enrolled a nationally representative cohort of noninstitutionalized adults between the ages of 25 and 74 years in 1995 (www.midus.wisc.edu). This study was designed to assess psychosocial factors that influence physical and mental health for adults in midlife. At enrollment, participants responded to a telephone survey and self-administered questionnaire. Households with telephones were sampled in the coterminous United States by random digit dialing. One English-speaking adult was chosen at random in each participating household, with oversampling of older adults and men.
The combined response rate at enrollment to telephone and written questionnaires was 60.8% (70.0% of those who were contacted and eligible for the telephone survey responded, and 86.8% of telephone respondents completed the written questionnaire) (18). A similar telephone survey and self-administered questionnaire were administered to surviving participants in 2004. The study protocol was approved by the human studies committees of Harvard Medical School and the University of Wisconsin, and all subjects provided informed consent for participation in this study.
The analysis was restricted to 2,570 respondents <65 years of age at baseline because of limited weight change in those aged ≥65 years. In this cohort, the response rate to the follow-up survey was 60% (n = 1,552) among surviving adults. Nonrespondents to the follow-up survey had a similar baseline mean body mass index when compared with respondents (26.75 vs. 26.80 kg/m2; P = 0.83). They also had similar levels of baseline psychosocial stress, though nonrespondents had slightly higher levels of perceived constraint in life (scale score, 2.76 vs. 2.64; P = 0.020) and strain in relations with spouse/partner (scale score, 2.31 vs. 2.23; P = 0.009). Nonrespondents also were younger (P < 0.001); more likely to be male (P < 0.001), unmarried (P = 0.015), or nonwhite (P < 0.001); more likely to smoke (P < 0.001); and had lower incomes (P < 0.001) and worse self-rated health (P < 0.001). All respondents undergoing cancer treatment (n = 42) and female respondents who were pregnant (n = 28) at baseline or follow-up were excluded because of fluctuations in weight related to these conditions. Another 127 subjects who were missing a baseline or follow-up body mass index measurement were excluded, yielding a final study cohort of 1,355 adults who completed the follow-up survey an average of 9.2 years after the baseline survey.
Study variables
The change in body mass index from 1995 to 2004 was our outcome measure. Body mass index was calculated from self-reported height and weight. A subset of 464 subjects in our sample (34%) also had height and weight measured objectively in 2004. The Pearson correlation coefficients between the self-reported and measured values of body mass index for these subjects in 2004 were 0.93 in men and 0.92 in women.
Our primary predictor variables were psychosocial stress scales measured at baseline that assessed stress related to work, personal relationships, life constraints, and finances (Appendix). Three well-validated stress scales captured work experiences related to skill discretion (3 items), decision authority (6 items), and job-related demands (5 items) (19, 20). These scales each had strong internal reliability, with a Cronbach coefficient alpha ranging from 0.68 to 0.85 in our cohort. Other scales captured strain in relations with spouse/partner (6 items: Cronbach alpha = 0.81), friends (4 items: alpha = 0.79), or family (4 items: alpha = 0.80) (21). To evaluate stress from general life experiences, we used a scale that evaluated perceived constraints in life (8 items: alpha = 0.86) (22, 23). Financial stress was assessed with a single question about difficulty paying bills.
Clinical and demographic covariates, selected a priori from the baseline survey, included baseline body mass index, medical conditions and health status (diabetes, smoking, self-rated health, and relative self-rated health compared with others the same age), self-reported race/ethnicity, income, age, and psychiatric conditions (depression, generalized anxiety, and panic disorder as defined according to psychiatric scales derived from the Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Appendix) (24, 25). Race/ethnicity was included in the analysis because of previously described racial and ethnic differences in body mass index in the United States (26). An indicator variable for quitting smoking during the follow-up period controlled for the likely associated weight gain. All variables were entered into models as presented in Table 1 except for baseline body mass index, which was included in the models after being centered on sex-specific mean body mass index. The covariates had no missing data; psychosocial stress scales had less than 1% missing except for work-related stress scales, which had 6.7% missing. Subjects with missing predictors were excluded from the models assessing those predictors.
Table 1.
Baseline Characteristics of the US Study Cohort in 1995a
| Variable | Percent |
|
| Men (N = 633) | Women (N = 722) | |
| Age, years | ||
| <35 | 23.3 | 26.7 |
| 35–44 | 35.3 | 30.6 |
| 45–54 | 27.4 | 23.2 |
| 55–64 | 14.0 | 19.5 |
| Race | ||
| White | 87.7 | 83.1 |
| Black | 5.1 | 10.3 |
| Hispanic | 3.3 | 3.9 |
| Other race | 3.9 | 2.7 |
| Income, $ | ||
| <25,000 | 15.9 | 24.8 |
| 25,000–44,999 | 25.0 | 32.9 |
| 45,000–69,999 | 29.9 | 21.0 |
| ≥70,000 | 29.2 | 21.4 |
| Baseline weight classification | ||
| Normal weight | 27.4 | 50.1 |
| Overweight | 49.3 | 28.9 |
| Obese | 23.3 | 21.0 |
| Depressionb | 9.7 | 18.5 |
| Generalized anxiety disorderb | 2.0 | 6.1 |
| Panic disorderc | 3.5 | 9.6 |
| Smoking | 23.7 | 22.7 |
| Quit smokingd | 7.7 | 6.8 |
| Diabetes | 3.6 | 2.8 |
| General health status, % fair/poor | 8.6 | 14.3 |
| Relative health status, % somewhat worse/much worse | 4.6 | 7.6 |
| Working | 93.9 | 78.5 |
| Married or living with partner | 81.5 | 75.2 |
Variables are weighted to account for the complex survey design and to approximate the distribution of US adults aged 25–64 years by region, residence in a metropolitan area, sex, race, age, education, and marital status.
Designation based on self-reported responses to the World Health Organization's Composite International Diagnostic Interview scale (21).
Designation based on self-reported responses to a scale derived from Diagnostic and Statistical Manual of Mental Disorders, Third Edition, criteria (20).
Not a baseline measure; defined as someone smoking in 1995 who was no longer smoking in 2004.
Statistical analysis
The psychosocial stress scales were constructed by calculating the mean for all responses to items in a scale, coded so that higher values represented greater psychosocial stress. Analyses of work-related stress included only respondents who were working at baseline. Analysis of spouse- or partner-related stress included only respondents who were married or living with a partner. All analyses were stratified by sex, because of prior studies demonstrating that the relation between stress and eating behaviors or weight differs between men and women (8–11, 15–17, 27).
Data were weighted to adjust for probabilities of reaching households within each telephone exchange, sampling subjects within each household, and obtaining completed telephone interviews and questionnaires from designated subjects (28). Poststratification weights were calculated so the cohort that completed both the baseline telephone interview and written questionnaire approximated the distribution of US adults aged 25–64 years by region, residence in a metropolitan area, sex, race, age, education, and marital status from the October 1995 Current Population Survey (29).
Change in body mass index was regressed on each psychosocial stress variable, controlling for the clinical and demographic covariates listed above and for interactions between baseline body mass index as a continuous variable and the psychosocial stress scales as continuous variables. These interactions assessed potential effect modification of the association between psychosocial stress and weight gain related to baseline body mass index. All beta coefficients are unit dependent with units of kg/m2. To graphically present the interaction effects for those variables found to have significant interactions, trend lines were graphed to represent predictions from the fitted model for specified baseline body mass index values, set to the mean for the body mass index categories of normal weight (<25 kg/m2), overweight (25–29.9 kg/m2), and obesity (≥30 kg/m2). We report other covariates if they were significantly associated with a change in body mass index in more than half of the final sex-stratified models.
All analyses were conducted with SAS, version 9.1, statistical software (SAS Institute, Inc., Cary, North Carolina) to account for the complex survey design. Two-tailed P values are reported for all analyses.
RESULTS
Weighted descriptive characteristics of the study cohort at baseline are presented in Table 1. Women had higher levels of baseline psychosocial stress than men in several domains: less skill discretion (P = 0.004), less decision authority (P < 0.001), more perceived constraints in life (P < 0.001), and more strain in relationships with family (P < 0.001) (Table 2). Psychosocial stress levels measured at baseline and follow-up were moderately correlated for each stress scale (Pearson correlations: 0.43–0.55 for men and 0.41–0.57 for women). Women had lower mean baseline body mass index than men (26.29 vs. 27.49 kg/m2; P < 0.001). The change in body mass index over the mean follow-up period of 9.2 years was similar in women and men (1.57 vs. 1.37 kg/m2; P = 0.33).
Table 2.
Mean Body Mass Index and Baseline Psychosocial Stress of US Men and Women in 1995 and Test of Difference Between Men and Womena
| Variable | Mean (SE) |
P Value | |
| Men (N = 633) | Women (N = 722) | ||
| Baseline body mass index, kg/m2 | 27.49 (0.19) | 26.29 (0.27) | <0.001 |
| Follow-up body mass index, kg/m2b | 28.86 (0.22) | 27.86 (0.29) | 0.007 |
| Body mass index change, kg/m2 | 1.37 (0.12) | 1.57 (0.17) | 0.33 |
| Lack of skill discretion (scale range, 1–5) | 2.38 (0.03) | 2.52 (0.04) | 0.004 |
| Lack of decision authority (scale range, 1–5) | 2.23 (0.04) | 2.45 (0.04) | <0.001 |
| Job-related demands (scale range, 1–5) | 3.06 (0.03) | 3.07 (0.03) | 0.85 |
| Perceived constraints in life (scale range, 1–7) | 2.53 (0.05) | 2.79 (0.05) | <0.001 |
| Strain in relations with family (scale range, 1–4) | 2.10 (0.03) | 2.23 (0.03) | <0.001 |
| Strain in relations with friends (scale range, 1–4) | 1.98 (0.02) | 1.94 (0.02) | 0.24 |
| Strain in relations with spouse/partner (scale range, 1–4) | 2.21 (0.03) | 2.28 (0.03) | 0.10 |
| Difficulty paying bills (scale range, 1–4) | 2.20 (0.04) | 2.26 (0.04) | 0.28 |
Abbreviation: SE, standard error.
Variables are weighted to account for the complex survey design and to approximate the distribution of US adults aged 25–64 years by region, residence in a metropolitan area, sex, race, age, education, and marital status.
Mean follow-up in sample was 9.2 years.
In multivariable models including all covariates and an interaction term between baseline body mass index and each respective psychosocial stress scale, numerous significant associations for psychosocial stress emerged (Table 3). When interactions were significant, greater psychosocial stress was associated with greater weight gain as baseline body mass index increased (P < 0.05 for interaction term). This effect was evident for financial stress for both men and women, for all work-related stress variables (less skill discretion, less decision authority, and higher job-related demands) for men, and for job-related demands, perceived constraints in life, and strain in relationships with family for women. Figures 1–4 portray the significant relations between psychosocial stress and change in body mass index for selected baseline body mass indexes that correspond to the mean body mass index of 3 weight categories (normal weight, overweight, and obesity).
Table 3.
Adjusted Association of Psychosocial Stress and Psychiatric Conditions in 1995 With Change in Body Mass Index From Baseline in 1995 to Follow-up in 2004, by Gender, With Interaction Between Baseline Body Mass Index and Stress, United Statesab
| Stress Variables and Effects | Men |
Women |
||
| β (SE) | P Value | β (SE) | P Value | |
| Lack of skill discretionc | ||||
| Main effect | 0.06 (0.16) | 0.72 | −0.05 (0.23) | 0.84 |
| Interaction | 0.08 (0.03) | 0.014 | −0.02 (0.04) | 0.64 |
| Lack of decision authorityc | ||||
| Main effect | 0.03 (0.15) | 0.83 | 0.23 (0.22) | 0.30 |
| Interaction | 0.07 (0.03) | 0.026 | 0.006 (0.03) | 0.83 |
| Job-related demandsc | ||||
| Main effect | 0.18 (0.18) | 0.30 | 0.38 (0.26) | 0.15 |
| Interaction | 0.16 (0.04) | <0.001 | 0.18 (0.05) | <0.001 |
| Perceived constraint in life | ||||
| Main effect | 0.18 (0.10) | 0.076 | 0.16 (0.13) | 0.21 |
| Interaction | −0.001 (0.02) | 0.96 | 0.06 (0.02) | <0.001 |
| Strain in relations with friends | ||||
| Main effect | −0.11 (0.22) | 0.60 | −0.28 (0.28) | 0.31 |
| Interaction | 0.02 (0.05) | 0.68 | −0.06 (0.04) | 0.16 |
| Strain in relations with family | ||||
| Main effect | 0.15 (0.19) | 0.44 | 0.07 (0.24) | 0.77 |
| Interaction | 0.04 (0.04) | 0.34 | 0.08 (0.03) | 0.016 |
| Strain in relations with spouse/partnerd | ||||
| Main effect | −0.02 (0.20) | 0.90 | 0.34 (0.28) | 0.22 |
| Interaction | 0.003 (0.04) | 0.94 | −0.02 (0.05) | 0.74 |
| Difficulty paying bills | ||||
| Main effect | 0.18 (0.14) | 0.18 | 0.47 (0.17) | 0.007 |
| Interaction | 0.08 (0.03) | 0.004 | 0.06 (0.02) | 0.010 |
| Depression | ||||
| Main effect | −0.04 (0.38) | 0.92 | 0.10 (0.41) | 0.81 |
| Interaction | 0.11 (0.06) | 0.051 | 0.12 (0.06) | 0.035 |
| Generalized anxiety | ||||
| Main effect | 2.65 (0.80) | <0.001 | 0.64 (0.66) | 0.33 |
| Interaction | 0.49 (0.13) | <0.001 | 0.32 (0.09) | <0.001 |
| Panic disorder | ||||
| Main effect | −0.54 (0.59) | 0.36 | 0.80 (0.53) | 0.13 |
| Interaction | 0.08 (0.10) | 0.42 | 0.11 (0.08) | 0.17 |
Abbreviation: SE, standard error.
All β coefficients are unit dependent with units of kg/m2.
All models were adjusted for baseline body mass index centered on mean body mass index; age; race; income; presence of generalized anxiety disorder, panic attack, or depression; smoking status; whether quit smoking by 2004; presence of diabetes; self-rated health; and self-rated relative health. The main effects presented are from the models that included interaction terms.
Includes only respondents who were employed at the initial survey in 1995.
Includes only respondents who were married or had a partner at the initial survey in 1995.
Figure 1.
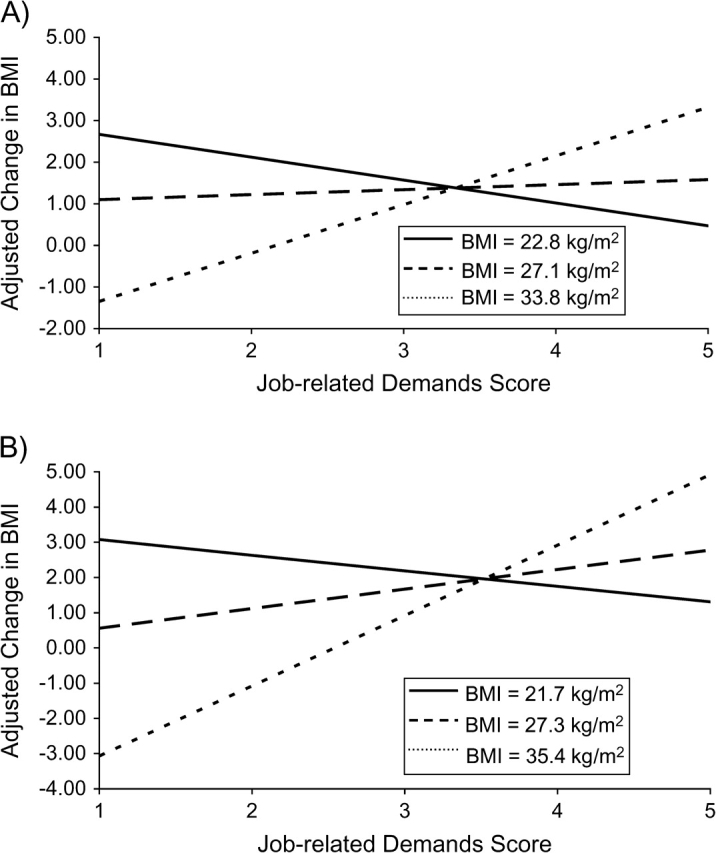
Adjusted change in body mass index from 1995 to 2004 for job-related demands among US men and women. Increasing job-related demands were associated with increasing weight gain among obese men (A) and women (B) and less weight gain among normal weight men and women. Results were adjusted for baseline body mass index (BMI); age; race; income; presence of generalized anxiety disorder, panic attack, or depression; smoking status; quitting smoking; presence of diabetes; self-rated health; and self-rated relative health. Trend lines represent predictions from the fitted model for specified body mass index values, set to the body mass index mean for each baseline body mass index category. In A, mean body mass index values are 22.8 (normal weight), 27.1 (overweight), and 33.8 (obese) kg/m2. In B, mean body mass index values are 21.7 (normal weight), 27.3 (overweight), and 35.4 (obese) kg/m2.
Figure 2.
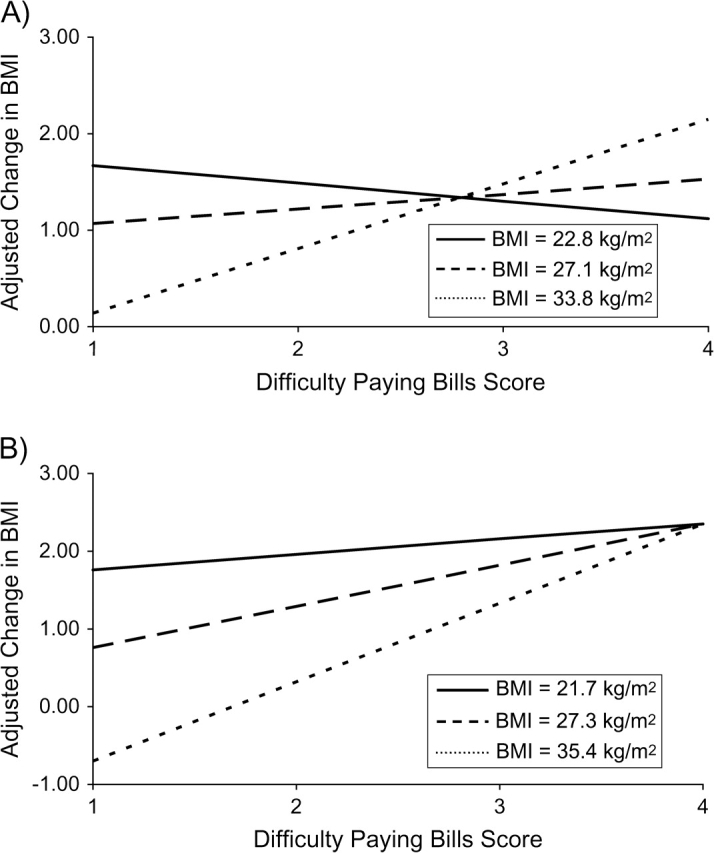
Adjusted change in body mass index from 1995 to 2004 for difficulty paying bills among US men and women. Increasing difficulty paying bills was associated with a steeper gradient of weight gain among obese men (A) and women (B) than for normal weight men and women. Results were adjusted for baseline body mass index; age; race; income; presence of generalized anxiety disorder, panic attack, or depression; smoking status; quitting smoking; presence of diabetes; self-rated health; and self-rated relative health. Trend lines represent predictions from the fitted model for specified body mass index (BMI) values, set to the body mass index mean for each baseline body mass index category. In A, mean body mass index values for men are 22.8 (normal weight), 27.1 (overweight), and 33.8 (obese) kg/m2. In B, mean body mass index values for women are 21.7 (normal weight), 27.3 (overweight), and 35.4 (obese) kg/m2.
Figure 3.
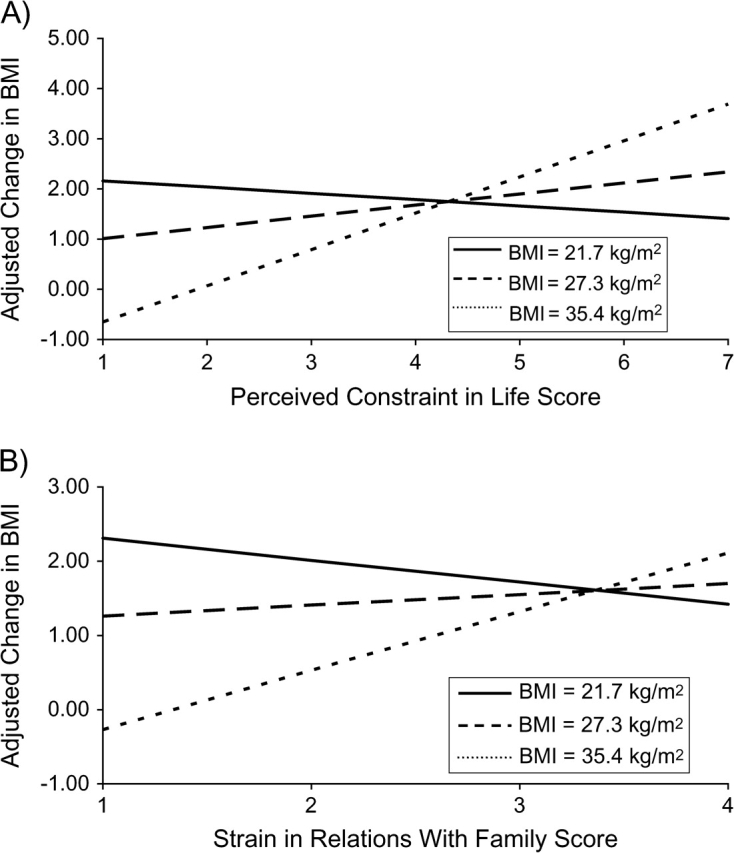
Adjusted change in body mass index from 1995 to 2004 for perceived constraint in life and strain in relations with family among US women. Increasing perceived constraint in life (A) and increasing strain in relations with family (B) were associated with increasing weight gain among obese women and less weight gain among normal weight women. Results were adjusted for baseline body mass index; age; race; income; presence of generalized anxiety disorder, panic attack, or depression; smoking status; quitting smoking; presence of diabetes; self-rated health; and self-rated relative health. Trend lines represent predictions from the fitted model for specified body mass index (BMI) values, set to the body mass index mean for each baseline body mass index category: 21.7 (normal weight), 27.3 (overweight), and 35.4 (obese) kg/m2.
Figure 4.
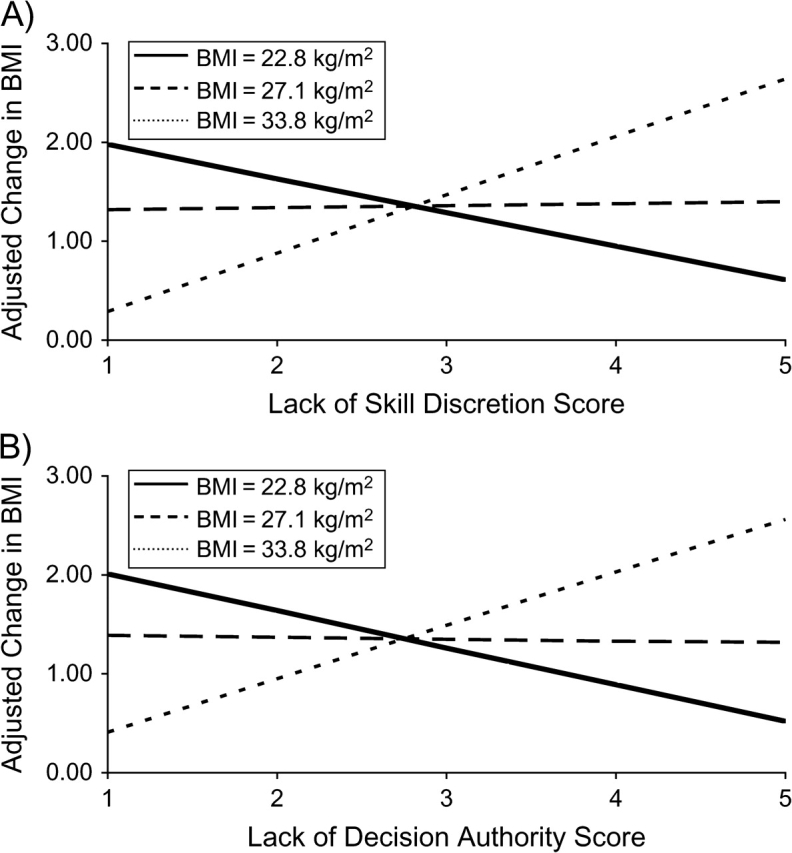
Adjusted change in body mass index from 1995 to 2004 for lack of skill discretion and lack of decision authority among US men. Lower levels of job-related skill discretion (A) and lower levels of decision authority (B) were associated with increasing weight gain among obese men and less weight gain among normal weight men. Results were adjusted for baseline body mass index; age; race; income; presence of generalized anxiety disorder, panic attack, or depression; smoking status; quitting smoking; presence of diabetes; self-rated health; and self-rated relative health. Trend lines represent predictions from the fitted model for specified body mass index (BMI) values, set to the body mass index mean for each baseline body mass index category: 22.8 (normal weight), 27.1 (overweight), and 33.8 (obese) kg/m2.
Several other covariates also significantly predicted a change in body mass index in at least half of the sex-stratified models. Men and women who were aged 55–64 years at enrollment experienced less weight gain compared with the youngest age group. Among women, increasing baseline body mass index was associated with less weight gain, and quitting smoking was associated with more weight gain. Generalized anxiety and an income between $25,000 and $44,999 were associated with more weight gain for men.
Because generalized anxiety was a significant predictor of more weight gain for men in the base models, we fitted additional models without the psychosocial stress scales and included interaction terms between the presence of each psychiatric condition and baseline body mass index (in 3 separate models for depression, generalized anxiety disorder, and panic disorder for both men and women). Depression and generalized anxiety were highly correlated within each sex (P < 0.01), and both conditions were significantly associated with more weight gain among women and men at higher levels of baseline body mass index. There was no significant association of panic disorder with change in body mass index for either men or women.
DISCUSSION
In this nationally representative cohort of US adults followed longitudinally over 9 years, psychosocial stress was associated with greater weight gain among both men and women with higher baseline body mass indexes if they experienced job-related demands, had difficulty paying bills, or had depression or generalized anxiety disorder. Among women with higher baseline body mass indexes, perceived constraints in life and strain in relations with family also were associated with greater weight gain. Among men with higher baseline body mass indexes, lack of skill discretion or decision authority at work was associated with greater weight gain.
These findings extend prior cross-sectional and longitudinal research by providing an expanded view of associations between psychosocial stress and weight gain in a nationally representative cohort of adults in the United States. Several studies have demonstrated heterogeneity in eating behaviors in response to stress; some people eat more when stressed while others eat less (30–32). Laboratory and observational studies of stress and eating behavior have shown inconsistent results when stratified by baseline weight (27). In our study, with a long follow-up period and diverse measures of psychosocial stress, subjects with higher body mass indexes at baseline who reported greater psychosocial stress gained more weight, whereas this pattern was not evident for those with lower baseline body mass indexes.
Our results also highlight apparent sex differences in the influence of stress on weight gain. Some stressors outside of work or finances, including general life constraints and strain in relationships with family, were associated with weight gain among women but not among men, suggesting effects on weight from a broader range of life domains in women. Prior cross-sectional studies have shown some differential effects by sex. These studies assessed fewer measures of stress than our study evaluated and provided only limited information about specific types of stressors that might differentially influence weight gain (14, 33, 34).
Analyses from the 3 prior longitudinal studies were stratified by sex. In the Whitehall study of British civil servants, Kivimaki et al. (11) found that men with higher baseline body mass indexes gained weight over 5 years if they experienced higher levels of work stress, but men with lower body mass indexes were more likely to lose weight under stressful job circumstances. Among women, weight gain was associated with higher job demands in main effect models, but the association was no longer significant when an interaction with baseline body mass index was included. In the subsequent analysis of the same cohort, men with chronically elevated levels of job strain and low social support at work were more likely to become obese and to develop a high waist circumference than those with no job strain (15); these associations were not significant among women.
Van Strien et al. (16) prospectively evaluated the influence of negative life events in a cohort in the Netherlands. Men classified as highly “emotional eaters” gained weight for up to 2 years after the occurrence of a negative life event. No correlation was observed for women. In a large cohort study of monozygotic and same-sex dizygotic Finnish twins, Korkeila et al. (17) assessed associations of stress and personality type at baseline with weight gain of greater than 10 kg after follow-up of 6 years and 15 years. The only significant adjusted associations were between neuroticism and weight gain after 6 years among older women and between extroversion and less weight gain among younger men.
Stress appears to influence eating behaviors differently by sex as well. In a study of high school students aged 15–19 years, caloric consumption increased on days with stressful events for girls but not for boys (though boys did increase their fat intake) (9). Similarly, among college students, women consumed more calories than men when exposed to a stressful film (8).
Our study found an association between baseline depression and anxiety and weight gain among men and women with higher baseline body mass indexes. Prior evidence has linked depression with the development of obesity, specifically among children and adolescents (35–38). Investigations of the relation between anxiety and weight gain have shown mixed results. Some studies have shown associations between anxiety at baseline and weight gain among men (39) and women (38), yet another study found a trend toward decreased likelihood of becoming overweight among men and women with anxiety at baseline (40). None of these studies of depression and anxiety have assessed the effect modification of baseline body mass index.
Several pathways have been explored in animal models to assess how psychosocial stress may influence weight gain. Social subordination in several species of primates induces chronically elevated cortisol levels, and high cortisol levels are associated with abdominal obesity in both nonhuman primates and humans (41–43). As a result, social subordination has been examined as a model for stress-induced eating and weight gain. Female monkeys who are socially subordinate have higher levels of abdominal obesity than socially dominant females (44). In an observational study of macaques, Wilson et al. (45) found that socially subordinate females consumed more calories and fed more frequently than socially dominant females. The subordinate females also demonstrated more anxious behavior and had alternations of the hypothalamic-pituitary axis with less negative feedback from elevated glucocorticoid levels. Laboratory studies in rats have shown that mild stress (e.g., tail pinching or restraint) can lead to weight gain if highly palatable foods are provided, but not with regular diets (46–48).
Based in large part on animal models, a complex interplay of hormones such as glucocorticoids and ghrelin (that increase appetite) and corticotrophin-releasing hormone and leptin (that decrease appetite) has been proposed by other researchers (48–51) to be involved in the physiologic pathways between stress and weight gain. Endogenous opiates induced by eating might also serve a role in limiting the dysphoric effects of stress (52). These pathways suggest a “comfort food” or “emotional eating” paradigm that has been proposed to explain stress-induced eating and weight gain (53, 54). The influence of stress on weight gain, therefore, may depend on the intensity and duration of stress and the types of food that are available for consumption.
Few mechanistic studies have assessed hormonal pathways that could link stress and weight in humans. Normal-weight women with major depression had more than twice the cortisol level and intraabdominal fat as those without depression (55). In a laboratory experiment with postmenopausal women subjected to a stress-inducing protocol, Epel et al. (56) discovered that women with high waist/hip ratios, regardless of body mass index, were more likely to display higher stress-induced cortisol levels. Women with high waist/hip ratios also felt more threatened under stress, and controlling for this high threat appraisal partially attenuated the association between waist/hip ratio and cortisol. Additional studies have documented higher snack food consumption in women with high stress-induced cortisol levels (12, 13).
Our study had several potential limitations. First, there was only 1 follow-up measure of body mass index over a mean of 9.2 years. Psychosocial stress could change over this time period, though there was a moderately high degree of correlation between baseline and follow-up psychosocial stress. Second, although our study cohort was representative of US adults, the response rate to the follow-up survey in our sample was 60%, and nonrespondents differed from respondents on several demographic and health characteristics. However, models were adjusted for the variables that differed between respondents and nonrespondents, and further bias would only arise if the relation of stress and weight change also differed for these 2 groups. Third, certain medications can be associated with weight gain (57). However, the MIDUS survey did not collect specific drug names, so we could not control for active use of these medications. Nonetheless, in all models, we controlled for diabetes, generalized anxiety disorder, and depression, conditions which are commonly treated with medications that are associated with weight gain. The most commonly used medications for depression and generalized anxiety disorder, selective serotonin reuptake inhibitors, have mixed effects on weight, so the net effect of these medications on weight gain may be limited (57). Fourth, causality cannot be established in our data despite the temporal ordering of baseline stress and subsequent weight gain. Fifth, weight and height were self-reported in this study and thus could be biased. Other studies have reported a high correlation between self-reported weight and height and measured body mass index (17, 58–60), and the prevalence of obesity and overweight in our sample was consistent with reported national estimates (26). Furthermore, in the subset of 464 subjects in our sample who had height and weight objectively measured at follow-up, the correlation between self-reported and measured body mass index in 2004 exceeded 0.92 for both men and women. Finally, the number of significant interactions found (12 of 22 tested at the 0.05 level, all in the same direction) exceeded what would be expected by chance, and the pattern was consistent with prior evidence.
In this nationally representative cohort, several domains of psychosocial stress as well as anxiety and depression were associated with weight gain among men and women with higher body mass indexes. Awareness of these associations may enable clinicians to help their overweight and obese patients avoid gaining further weight during stressful periods. Stress reduction may also be an important component of weight-loss interventions in worksites and in clinical and public health programs (61–65).
Acknowledgments
Author affiliations: Harvard Center for Population and Development Studies, Harvard School of Public Health, Boston, Massachusetts (Jason P. Block); Division of General Internal Medicine, Brigham and Women's Hospital, Boston, Massachusetts (Jason P. Block, John Z. Ayanian); and Department of Health Care Policy, Harvard Medical School, Boston, Massachusetts (Yulei He, Alan M. Zaslavsky, Lin Ding, John Z. Ayanian).
This research was supported by a grant from the National Institute on Aging (P01-AG020166) to conduct a longitudinal follow-up of the MIDUS investigation. The original study was supported by the John D. and Catherine T. MacArthur Foundation Research Network on Successful Midlife Development. Dr. Block was supported by the Robert Wood Johnson Foundation Health and Society Scholars Program.
The authors are grateful for helpful comments on an earlier draft of the manuscript provided by Dr. Mark Friedberg and Dr. J. Michael McWilliams.
An abstract of this study was presented at the 31st Annual Meeting of the Society of General Internal Medicine in Pittsburgh, Pennsylvania, April 11, 2008.
Conflict of interest: none declared.
Glossary
Abbreviation
- MIDUS
Midlife in the United States
APPENDIX
Survey Measures of Psychosocial Stress and Psychiatric Conditions
PSYCHOSOCIAL STRESS
Job characteristics
“Please indicate how often each of the following is true of your job” or “how often has each of the following occurred at your job.”
Skill discretion (5 response categories from “never” to “all the time”).
“How often do you learn new things at work?”
“How often does your work demand a high level of skill or expertise?”
“How often does your job provide you with a variety of things that interest you?”
Decision authority (5 response categories from “never” to “all the time”).
“On your job, how often do you have to initiate things—such as coming up with your own ideas, or figuring out on your own what needs to be done?”
“How often do you have a choice in deciding how you do your tasks at work?”
“How often do you have a choice in deciding what tasks you do at work?”
“How often do you have a say in decisions about your work?”
“How often do you have a say in planning your work environment—that is, how your workplace is arranged or how things are organized?”
“(How often) you control the amount of time you spend on tasks.”
Demands (5 response categories from “never” to “all the time”).
“How often do you have to work very intensively—that is, you are very busy trying to get things done?”
“How often do different people or groups at work demand things from you that you think are hard to combine?”
“(How often) you have too many demands made on you.”
“(How often) you have enough time to get everything done.”
“(How often) you have a lot of interruption.”
Perceived constraints
“Please indicate how strongly you agree or disagree with each of the following statements,” choosing from among 7 response categories from “strongly agree” to “strongly disagree.”
“There is little I can do to change the important things in my life.”
“I often feel helpless in dealing with the problems of life.”
“Other people determine most of what I can and cannot do.”
“What happens in my life is often beyond my control.”
“There are many things that interfere with what I want to do.”
“I have little control over the things that happen to me.”
“There is really no way I can solve the problems I have.”
“I sometimes feel I am being pushed around in my life.”
Family strain
Please choose from among 4 response categories from “often” to “never.”
“Not including your spouse or partner, how often do members of your family make too many demands on you?”
“How often do they criticize you?”
“How often do they let you down when you are counting on them?”
“How often do they get on your nerves?”
Friend strain
Please choose from among 4 response categories from “often” to “never.”
“How often do your friends make too many demands on you?”
“How often do they criticize you?”
“How often do they let you down when you are counting on them?”
“How often do they get on your nerves?”
Spouse/partner strain
Please choose from among 4 response categories from “often” to “never.”
“How often does your spouse or partner make too many demands on you?”
“How often does he or she argue with you?”
“How often does he or she make you feel tense?”
“How often does he or she criticize you?”
“How often does he or she let you down when you are counting on him or her?”
“How often does he or she get on your nerves?”
Financial strain
This was queried as a single question rather than on a scale.
- “How difficult is it for you (and your family) to pay your monthly bills?”
- a. Very difficult
- b. Somewhat difficult
- c. Not very difficult
- d. Not at all difficult
DEPRESSION
A person was considered depressed if he/she reported having at least 4 of the listed symptoms under depressed mood or anhedonia and indicated that these symptoms were present “all day long” or “most of the day” and if the symptoms were present “every day” or “almost every day.”
Depressed affect
“During two weeks in past 12 months, when you felt sad, blue, or depressed, did you
Lose interest in most things?
Feel more tired out or low on energy than is usual?
Lose your appetite?
Have more trouble falling asleep than usual?
Have a lot more trouble concentrating than usual?
Feel down on yourself, no good, or worthless?
Think a lot about death?”
Anhedonia
“During two weeks in past 12 months, when you lost interest in most things, did you
Feel more tired out or low on energy than is usual?
Lose your appetite?
Have more trouble falling asleep than usual?
Have a lot more trouble concentrating than usual?
Feel down on yourself, no good, or worthless?
Think a lot about death?”
GENERALIZED ANXIETY DISORDER
A person was considered to have generalized anxiety disorder if he/she reported having at least 3 of the listed symptoms on most days and reported worrying “a lot more” than most people, worrying “every day, just about every day, or most days,” and worrying about “more than one thing” or having different worries “at the same time.”
“How often—over the past 12 months—you
Were restless because of your worry?
Were keyed up, on edge, or had a lot of nervous energy?
Were irritable because of your worry?
Had trouble falling asleep?
Had trouble staying asleep because of your worry?
Had trouble keeping your mind on what you were doing?
Had trouble remembering things because of your worry?
Were low on energy?
Tired easily because of your worry?
Had sore or arching muscles because of tension?”
PANIC ATTACK (PANIC DISORDER)
A person was considered to have panic attack (panic disorder) if he/she reported having at least 3 of the listed symptoms, an “attack happened when a respondent was not in danger or the center of attention,” and either “had a spell or an attack when they felt frightened” or “had a spell or an attack for no reason.”
“When you have attacks
Your heart pounds?
You have tightness, pain, or discomfort in your chest or stomach?
You sweat?
You tremble or shake?
You have hot flashes or chills?
You or things around you seem unreal?”
Documentation of scales for the MIDUS study can be found online at http://www.midus.wisc.edu/midus1/documentationofscales.pdf.
References
- 1.Landsbergis PA, Schnall PL, Pickering TG, et al. Life-course exposure to job strain and ambulatory blood pressure in men. Am J Epidemiol. 2003;157(11):998–1006. doi: 10.1093/aje/kwg095. [DOI] [PubMed] [Google Scholar]
- 2.Nielsen NR, Kristensen TS, Schnohr P, et al. Perceived stress and cause-specific mortality among men and women: results from a prospective cohort study. Am J Epidemiol. 2008;168(5):481–491. doi: 10.1093/aje/kwn157. discussion 492–496. [DOI] [PubMed] [Google Scholar]
- 3.Aboa-Eboulé C, Brisson C, Maunsell E, et al. Job strain and risk of acute recurrent coronary heart disease events. JAMA. 2007;298(14):1652–1660. doi: 10.1001/jama.298.14.1652. [DOI] [PubMed] [Google Scholar]
- 4.Bosma H, Marmot MG, Hemingway H, et al. Low job control and risk of coronary heart disease in Whitehall II (prospective cohort) study. BMJ. 1997;314(7080):558–565. doi: 10.1136/bmj.314.7080.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Bacquer D, Pelfrene E, Clays E, et al. Perceived job stress and incidence of coronary events: 3-year follow-up of the Belgian Job Stress Project cohort. Am J Epidemiol. 2005;161(5):434–441. doi: 10.1093/aje/kwi040. [DOI] [PubMed] [Google Scholar]
- 6.Lillberg K, Verkasalo PK, Kaprio J, et al. Stressful life events and risk of breast cancer in 10,808 women: a cohort study. Am J Epidemiol. 2003;157(5):415–423. doi: 10.1093/aje/kwg002. [DOI] [PubMed] [Google Scholar]
- 7.Chida Y, Hamer M, Wardle J, et al. Do stress-related psychosocial factors contribute to cancer incidence and survival? Nat Clin Pract Oncol. 2008;5(8):466–475. doi: 10.1038/ncponc1134. [DOI] [PubMed] [Google Scholar]
- 8.Grunberg NE, Straub RO. The role of gender and taste class in the effects of stress on eating. Health Psychol. 1992;11(2):97–100. doi: 10.1037//0278-6133.11.2.97. [DOI] [PubMed] [Google Scholar]
- 9.Michaud C, Kahn JP, Musse N, et al. Relationships between a critical life event and eating behaviour in high-school students. Stress Med. 1990;6(1):57–64. [Google Scholar]
- 10.Wardle J, Steptoe A, Oliver G, et al. Stress, dietary restraint and food intake. J Psychosom Res. 2000;48(2):195–202. doi: 10.1016/s0022-3999(00)00076-3. [DOI] [PubMed] [Google Scholar]
- 11.Kivimäki M, Head J, Ferrie JE, et al. Work stress, weight gain and weight loss: evidence for bidirectional effects of job strain on body mass index in the Whitehall II study. Int J Obes (Lond) 2006;30(6):982–987. doi: 10.1038/sj.ijo.0803229. [DOI] [PubMed] [Google Scholar]
- 12.Epel E, Lapidus R, McEwen B, et al. Stress may add bite to appetite in women: a laboratory study of stress-induced cortisol and eating behavior. Psychoneuroendocrinology. 2001;26(1):37–49. doi: 10.1016/s0306-4530(00)00035-4. [DOI] [PubMed] [Google Scholar]
- 13.Newman E, O'Connor DB, Conner M. Daily hassles and eating behaviour: the role of cortisol reactivity status. Psychoneuroendocrinology. 2007;32(2):125–132. doi: 10.1016/j.psyneuen.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 14.Overgaard D, Gyntelberg F, Heitmann BL. Psychological workload and body weight: is there an association? A review of the literature. Occup Med (Lond) 2004;54(1):35–41. doi: 10.1093/occmed/kqg135. [DOI] [PubMed] [Google Scholar]
- 15.Brunner EJ, Chandola T, Marmot MG. Prospective effect of job strain on general and central obesity in the Whitehall II study. Am J Epidemiol. 2007;165(7):828–837. doi: 10.1093/aje/kwk058. [DOI] [PubMed] [Google Scholar]
- 16.Van Strien T, Rookus MA, Bergers GP, et al. Life events, emotional eating and change in body mass index. Int J Obes. 1986;10(1):29–35. [PubMed] [Google Scholar]
- 17.Korkeila M, Kaprio J, Rissanen A, et al. Predictors of major weight gain in adult Finns: stress, life satisfaction and personality traits. Int J Obes Relat Metab Disord. 1998;22(10):949–957. doi: 10.1038/sj.ijo.0800694. [DOI] [PubMed] [Google Scholar]
- 18.The Technical Report on the Methodology of the MIDUS Survey. Ann Arbor, MI: Inter-university Consortium for Political and Social Research; 1999. ( http://midmac.med.harvard.edu/tech.html). (Accessed March 30, 2009) [Google Scholar]
- 19.Karasek R, Baker D, Marxer F, et al. Job decision latitude, job demands, and cardiovascular disease: a prospective study of Swedish men. Am J Public Health. 1981;71(7):694–705. doi: 10.2105/ajph.71.7.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schwartz JE, Pieper CF, Karasek RA. A procedure for linking psychosocial job characteristics data to health surveys. Am J Public Health. 1988;78(8):904–909. doi: 10.2105/ajph.78.8.904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schuster TL, Kessler RC, Aseltine RH., Jr Supportive interactions, negative interactions, and depressed mood. Am J Community Psychol. 1990;18(3):423–438. doi: 10.1007/BF00938116. [DOI] [PubMed] [Google Scholar]
- 22.Lachman ME, Weaver SL. The sense of control as a moderator of social class differences in health and well-being. J Pers Soc Psychol. 1998;74(3):763–773. doi: 10.1037//0022-3514.74.3.763. [DOI] [PubMed] [Google Scholar]
- 23.Pearlin LI, Schooler C. The structure of coping. J Health Soc Behav. 1978;19(1):2–21. [PubMed] [Google Scholar]
- 24.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd ed. Washington, DC: American Psychiatric Association; 1987. [Google Scholar]
- 25.World Health Organization. Composite International Diagnostic Interview, CIDI, Version 10. Geneva, Switzerland: World Health Organization; 1990. [Google Scholar]
- 26.Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 27.Greeno CG, Wing RR. Stress-induced eating. Psychol Bull. 1994;115(3):444–464. doi: 10.1037/0033-2909.115.3.444. [DOI] [PubMed] [Google Scholar]
- 28.Levy PS, Lemeshow S. Sampling of Populations: Methods and Applications. New York, NY: John Wiley & Sons, Inc; 1991. [Google Scholar]
- 29.Current Population Survey: Basic Monthly CPS. Washington, DC: US Bureau of Labor Statistics and US Bureau of the Census; 1995. ( http://www.bls.census.gov/cps_ftp.html#4). (Accessed March 30, 2009) [Google Scholar]
- 30.Kandiah J, Yake M, Jones J, et al. Stress influences appetite and comfort food preferences in college women. Nutr Res. 2006;26(3):118–123. [Google Scholar]
- 31.Stone A, Brownell K. The stress–eating paradox: multiple daily measurements in adult males and females. Psychol Health. 1994;9:425–436. [Google Scholar]
- 32.Epel E, Jimenez S, Brownell K, et al. Are stress eaters at risk for the metabolic syndrome? Ann N Y Acad Sci. 2004;1032:208–210. doi: 10.1196/annals.1314.022. [DOI] [PubMed] [Google Scholar]
- 33.Serlachius A, Hamer M, Wardle J. Stress and weight change in university students in the United Kingdom. Physiol Behav. 2007;92(4):548–553. doi: 10.1016/j.physbeh.2007.04.032. [DOI] [PubMed] [Google Scholar]
- 34.Thurston RC, Kubzansky LD. Multiple sources of psychosocial disadvantage and risk of coronary heart disease. Psychosom Med. 2007;69(8):748–755. doi: 10.1097/PSY.0b013e31815772a3. [DOI] [PubMed] [Google Scholar]
- 35.Goodman E, Whitaker RC. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics. 2002;110(3):497–504. doi: 10.1542/peds.110.3.497. [DOI] [PubMed] [Google Scholar]
- 36.Pine DS, Goldstein RB, Wolk S, et al. The association between childhood depression and adulthood body mass index. Pediatrics. 2001;107(5):1049–1056. doi: 10.1542/peds.107.5.1049. [DOI] [PubMed] [Google Scholar]
- 37.Richardson LP, Davis R, Poulton R, et al. A longitudinal evaluation of adolescent depression and adult obesity. Arch Pediatr Adolesc Med. 2003;157(8):739–745. doi: 10.1001/archpedi.157.8.739. [DOI] [PubMed] [Google Scholar]
- 38.Anderson SE, Cohen P, Naumova EN, et al. Association of depression and anxiety disorders with weight change in a prospective community-based study of children followed up into adulthood. Arch Pediatr Adolesc Med. 2006;160(3):285–291. doi: 10.1001/archpedi.160.3.285. [DOI] [PubMed] [Google Scholar]
- 39.Chiriboga DE, Ma Y, Li W, et al. Gender differences in predictors of body weight and body weight change in healthy adults. Obesity (Silver Spring) 2008;16(1):137–145. doi: 10.1038/oby.2007.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hasler G, Pine DS, Gamma A, et al. The associations between psychopathology and being overweight: a 20-year prospective study. Psychol Med. 2004;34(6):1047–1057. doi: 10.1017/s0033291703001697. [DOI] [PubMed] [Google Scholar]
- 41.Abbott DH, Keverne EB, Bercovitch FB, et al. Are subordinates always stressed? A comparative analysis of rank differences in cortisol levels among primates. Horm Behav. 2003;43(1):67–82. doi: 10.1016/s0018-506x(02)00037-5. [DOI] [PubMed] [Google Scholar]
- 42.Sapolsky RM. The influence of social hierarchy on primate health. Science. 2005;308(5722):648–652. doi: 10.1126/science.1106477. [DOI] [PubMed] [Google Scholar]
- 43.Pasquali R, Vicennati V, Cacciari M, et al. The hypothalamic-pituitary-adrenal axis activity in obesity and the metabolic syndrome. Ann N Y Acad Sci. 2006;1083:111–128. doi: 10.1196/annals.1367.009. [DOI] [PubMed] [Google Scholar]
- 44.Shively CA, Clarkson TB. Regional obesity and coronary artery atherosclerosis in females: a non-human primate model. Acta Med Scand Suppl. 1988;723:71–78. doi: 10.1111/j.0954-6820.1987.tb05930.x. [DOI] [PubMed] [Google Scholar]
- 45.Wilson ME, Fisher J, Fischer A, et al. Quantifying food intake in socially housed monkeys: social status effects on caloric consumption. Physiol Behav. 2008;94(4):586–594. doi: 10.1016/j.physbeh.2008.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Levine AS, Morley JE. Stress-induced eating in rats. Am J Physiol. 1981;241(1):R72–R76. doi: 10.1152/ajpregu.1981.241.1.R72. [DOI] [PubMed] [Google Scholar]
- 47.Rowland NE, Antelman SM. Stress-induced hyperphagia and obesity in rats: a possible model for understanding human obesity. Science. 1976;191(4224):310–312. doi: 10.1126/science.1246617. [DOI] [PubMed] [Google Scholar]
- 48.Michel C, Levin BE, Dunn-Meynell AA. Stress facilitates body weight gain in genetically predisposed rats on medium-fat diet. Am J Physiol Regul Integr Comp Physiol. 2003;285(4):R791–R799. doi: 10.1152/ajpregu.00072.2003. [DOI] [PubMed] [Google Scholar]
- 49.Lutter M, Sakata I, Osborne-Lawrence S, et al. The orexigenic hormone ghrelin defends against depressive symptoms of chronic stress. Nat Neurosci. 2008;11(7):752–753. doi: 10.1038/nn.2139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Levin BE, Richard D, Michel C, et al. Differential stress responsivity in diet-induced obese and resistant rats. Am J Physiol Regul Integr Comp Physiol. 2000;279(4):R1357–R1364. doi: 10.1152/ajpregu.2000.279.4.R1357. [DOI] [PubMed] [Google Scholar]
- 51.Torres SJ, Nowson CA. Relationship between stress, eating behavior, and obesity. Nutrition. 2007;23(11–12):887–894. doi: 10.1016/j.nut.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 52.Adam TC, Epel ES. Stress, eating and the reward system. Physiol Behav. 2007;91(4):449–458. doi: 10.1016/j.physbeh.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 53.Ganley RM. Emotion and eating in obesity: a review of the literature. Int J Eat Disord. 1989;8(3):343–361. [Google Scholar]
- 54.Dallman MF, Pecoraro N, Akana SF, et al. Chronic stress and obesity: a new view of “comfort food. Proc Natl Acad Sci U S A. 2003;100(20):11696–11701. doi: 10.1073/pnas.1934666100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Thakore JH, Richards PJ, Reznek RH, et al. Increased intra-abdominal fat deposition in patients with major depressive illness as measured by computed tomography. Biol Psychiatry. 1997;41(11):1140–1142. doi: 10.1016/S0006-3223(97)85394-2. [DOI] [PubMed] [Google Scholar]
- 56.Epel ES, McEwen B, Seeman T, et al. Stress and body shape: stress-induced cortisol secretion is consistently greater among women with central fat. Psychosom Med. 2000;62(5):623–632. doi: 10.1097/00006842-200009000-00005. [DOI] [PubMed] [Google Scholar]
- 57.Malone M. Medications associated with weight gain. Ann Pharmacother. 2005;39(12):2046–2055. doi: 10.1345/aph.1G333. [DOI] [PubMed] [Google Scholar]
- 58.Field AE, Aneja P, Rosner B. The validity of self-reported weight change among adolescents and young adults. Obesity (Silver Spring) 2007;15(9):2357–2364. doi: 10.1038/oby.2007.279. [DOI] [PubMed] [Google Scholar]
- 59.Nyholm M, Gullberg B, Merlo J, et al. The validity of obesity based on self-reported weight and height: implications for population studies. Obesity (Silver Spring) 2007;15(1):197–208. doi: 10.1038/oby.2007.536. [DOI] [PubMed] [Google Scholar]
- 60.White MA, Masheb RM, Burke-Martindale C, et al. Accuracy of self-reported weight among bariatric surgery candidates: the influence of race and weight cycling. Obesity (Silver Spring) 2007;15(11):2761–2768. doi: 10.1038/oby.2007.328. [DOI] [PubMed] [Google Scholar]
- 61.Ornish D, Brown SE, Scherwitz LW, et al. Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. Lancet. 1990;336(8708):129–133. doi: 10.1016/0140-6736(90)91656-u. [DOI] [PubMed] [Google Scholar]
- 62.Ornish D, Scherwitz LW, Billings JH, et al. Intensive lifestyle changes for reversal of coronary heart disease. JAMA. 1998;280(23):2001–2007. doi: 10.1001/jama.280.23.2001. [DOI] [PubMed] [Google Scholar]
- 63.Nilsson PM, Klasson EB, Nyberg P. Life-style intervention at the worksite—reduction of cardiovascular risk factors in a randomized study. Scand J Work Environ Health. 2001;27(1):57–62. doi: 10.5271/sjweh.587. [DOI] [PubMed] [Google Scholar]
- 64.Rahe RH, Taylor CB, Tolles RL, et al. A novel stress and coping workplace program reduces illness and healthcare utilization. Psychosom Med. 2002;64(2):278–286. doi: 10.1097/00006842-200203000-00011. [DOI] [PubMed] [Google Scholar]
- 65.Petterson IL, Arnetz BB. Psychosocial stressors and well-being in health care workers. The impact of an intervention program. Soc Sci Med. 1998;47(11):1763–1772. doi: 10.1016/s0277-9536(98)00245-7. [DOI] [PubMed] [Google Scholar]


