Abstract
Numerous studies document improvements in health status and health expectancies among older adults over time. However, most evidence is from developed nations and gender differences in health trends are often inconsistent. It remains unknown whether changes in health in developing countries resemble Western trends or whether patterns of health improvement are unique to the country’s epidemiologic transition and gender norms. Using two nationally representative samples of non-institutionalized adults in China ages 65 and older, this study investigates gender differences in the improvements in disability, chronic disease prevalence, and self-rated health from 1992 to 2002. Results from multivariate logistic regression models show that all three indicators of health improved over the 10-year period, with the largest improvement in self-rated health. With the exception of disability, the health of women improved more than men. Using Sullivan’s decomposition methods, we also show that active life expectancy, disease-free life expectancy, and healthy life expectancy increased over this decade and were patterned differently according to gender. Overall, the findings demonstrate that China experienced broad health-improvements during its early stages of the epidemiologic transition and that these changes were not uniform by gender. We discuss the public health implications of the findings in the context of China’s rapidly aging population.
Keywords: China, health expectancy, gender, life expectancy, daily activities, chronic disease, self-rated health, older adults
INTRODUCTION
Improvements in health and health expectancies (the average lifetime in different health states) among the elderly have recently attracted the attention of researchers and policymakers as longevity continues to increase. However, there are questions about whether declines in morbidity and disability will accompany the declines in mortality (Freedman, Martin, & Schoeni, 2002; Freedman et al., 2004; Robine et al., 2003). Studies show that improvements in health among the elderly are not universal and that the patterns of change are partly attributable to the stage of the epidemiologic transition in a given country (e.g., Myers, Lamb, & Agree, 2003; Robine & Michel, 2004). Another complication is that measures of health change often differ across studies and the evidence demonstrating a trend for one dimension of health (e.g., functional disability) may not accurately reflect changes in other dimensions of health (e.g., chronic disease) (Crimmins, 2004), both within and across nations. There are inconsistencies even among studies using data from the same country because of differences in sampling, survey methods, questionnaire wording (e.g., “getting help” vs. “having difficulty” with a task), and analytic strategies (Freedman et al., 2004; Hayward & Warner, 2005). With few exceptions (Jitapunkul & Chavovan, 2000; Saito, Qiao, & Jitapunkul, 2003; Tu & Chen, 1994; Zimmer, Martin, & Chang, 2002), most studies have not addressed health improvements among the elderly in developing countries or regions. Consequently, our current knowledge is primarily based on research from developed nations.
The purpose of this study is to document recent changes in health and health expectancies among older adults in mainland China (thereafter China). Our goals are fourfold. First, review the existing literature and empirical evidence of health changes in developed and developing countries as a basis for identifying and understanding recent trends in China. Second, using two large-scale national surveys from China, we examine a decade (1992 to 2002) of health change with measures of disability, morbidity, and self-rated health (SRH). Third, we focus on possible gender differentials in health improvements among the Chinese elderly. Finally, we estimate the relative impact of improvements in disability, morbidity, and SRH on the added number and proportion of years of health expectancies.
Changes in Health and Health Expectancies in Developed and Developing Countries
In low-mortality countries such as the United States, England, France, Finland, and the Netherlands, studies generally demonstrate increases in the prevalence of both fatal and non-fatal diseases among the elderly (Crimmins & Saito, 2000; Robine & Michel, 2004). Increases in the prevalence of chronic diseases are largely attributed to prolonged survival among those with fatal conditions rather than increases in disease incidence (Crimmins & Saito, 2000).
Despite similar trends of increasing disease prevalence, patterns of change in functional limitations and disabilities widely vary across Western nations. For example, evidence from cross-sectional and longitudinal studies show that the United States and France witnessed marked improvements in physical functioning (defined in terms of climbing stairs and walking a quarter of a mile) and performing instrumental activities of daily living (IADL) from the 1980s to the 1990s (see Robine & Michel, 2004). Conversely, Canada, Great Britain, Australia, New Zealand, and the Netherlands experienced declines in physical functioning and IADL performance in the 1990s; whereas little change occurred in these functional domains among the Dutch elderly in the 1990s (Robine & Michel, 2004). During the 1990s, severe disability – measured with activities of daily living (ADL) – declined in most European countries, leveled in the United States, and increased in Japan and Australia (see Robine & Michel, 2004). Interestingly, despite these dissimilar changes in functional limitations, studies also documented consistent improvements in SRH and healthy life expectancy (HLE) (defined as life expectancy with good SRH) in many developed nations during the 1980s and 1990s (Aromaa, Koskinen, & Huttunen, 1999; Doblhammer & Kytir, 2001; Zack et al., 2004).
In developing countries, data on health expectancies are primarily static (Robine et al., 2003) and studies seldom focus on changes in health status and the consequences of health expectancies. From what is known, research has shown significant improvements in SRH and HLE among the elderly in China and Thailand during the late 1980s (Jitapunkul & Chavovan, 2000; Saito et al., 2003). Similarly, in China and Taiwan, there are documented improvements in ADL functioning in the late 1980s (Saito et al., 2003; Tu & Chen, 1994). The evidence from these studies suggests that improvements in SRH and functioning occurred during periods of rapid economic development and an epidemiologic transition. However, other findings from Taiwan indicate that functional limitations (i.e., walking or climbing stairs) increased from 1993 to 1999 (Zimmer et al., 2002). There is some evidence to suggest that the worsening trend in Taiwan may be attributed to the implementation of universal health insurance in 1995 that influenced the reporting of limitations among elderly Taiwanese (Zimmer et al., 2002).
China experienced a similar pattern of economic growth and an epidemiologic transition in the 1990s as did Thailand and Taiwan in the 1980s (Yang et al., 2008). Therefore, we expect that the Chinese population would witness comparable improvements in health during the 1990s – particularly as older generations are becoming replaced by younger cohorts who had better conditions in earlier life and healthier lifestyles (Wu et al., 2004; Zhu & Xie, 2007). However, the pattern of improving health in China may be complicated by a couple of factors. First, health care reforms were implemented in China in the mid-1980s and led to reductions in access to health services into the 1990s. A second confounding factor is that cultural values and the family structure in China also began to shift during this period. As part of a Confucian dominant society, Chinese elders are traditionally bestowed the highest respect from family members and society (i.e., filial piety). Research has shown that Chinese elders who received such respect had significantly better rated physical and mental health than those with children who do not have a sense of filial piety (Yu et al., 1997). However, it is plausible that health perceptions change as these cultural norms and expectation are fading. For example, there are increasing numbers of older Chinese living alone due to modernization and the out-migration of children because of work or family preference. On one hand, these changes may negatively affect SRH and functional capacity due to the lack of support and caregiving resources in the household; on the other hand, more elders living alone may improve their daily functioning and sense of control (Gu, Dupre, & Liu, 2007; Gu & Zeng, 2004). Considering these various factors, it is unclear whether the health trends documented in many developed and some developing countries would be observed in China in the 1990s.
Explanations for Changes in Health and Health Expectancies
There are several hypotheses explaining how changes in health relate to health expectancies: compression of morbidity, expansion of morbidity, and dynamic equilibrium (Fries, 1980; Gurenberg, 1977; Manton, 1982). In the context of population aging, Robine and Michel (2004) proposed a general theory of healthy aging that includes four stages of progression related to morbidity, disability, and mortality. They argue that an expansion of morbidity occurs first as sick persons experience greater overall improvements in survival, followed by equilibrium between increased disability and reduced mortality due to greater control of disease progression. Cohort replacement gradually produces a compression of morbidity as mortality continues to decline and new cohorts have better profiles of health and risky behaviors. Finally, a re-expansion of morbidity is possible as new medical advancements improve the survival of increasingly old and frail populations. Similarly, some scholars maintain that patterns of disability change are associated with the epidemiologic transition and that patterns of health change may differ across stages of the transition (see Myers, Lamb, & Agree, 2003), which also may account for the various findings across time periods and countries.
However, a lingering concern is whether the observed changes in health represent actual improvements or declines or whether they simply reflect compositional shifts occurring in the population. Indeed, studies suggest that factors such as sociodemographic characteristics, health resources, and health behaviors significantly affect population rates of disability, morbidity, and self-rated health (e.g., Crimmins, 2004). Therefore, failing to account for several key covariates can produce biased estimates and erroneous conclusions about the apparent improvements in health and health expectancies (Freedman et al., 2004; Sazflarski & Cubbins, 2004).
Gender Differences in Changes in Health and Health Expectancies
The gender paradox in health is widely recognized (e.g., Lamb, 1997). However, the reasons why women enjoy greater longevity but worse health are complex and are generally attributed to differences in socioeconomic status, genetic and acquired risks, immune-system responses, hormones, disease patterns and prevention, and health-reporting behaviors (Crimmins & Saito, 2000; Idler, 2003; Oksuzyan et al., 2008). For example, Crimmins and Saito (2000) showed that gender differences in disability and disability-free life expectancy was smaller among those with higher SES than those with lower SES. Other studies have shown that men are more likely than women to exhibit higher levels of muscle mass, bone mineral density, neuroendocrine, testosterone, and overall positive affect (Nolen-Hoeksema, Larson, & Grayson, 1999; Yates et al., 2007), which may delay the onset of disability or morbidity (Ostir, Ottenbacher, & Markides, 2004; Walston & Fried, 1999). Moreover, studies consistently find that men are more likely to die suddenly and women are more likely to experience a gradual progression of physical degeneration (Puts et al., 2005).
Inconsistencies are also reported with respect to gender differences in changes in health and health expectancies (Crimmins & Saito, 2000; Freedman et al., 2002). For instance, Crimmins and Saito (2000) found that elderly men in the U.S. experienced greater increases in chronic disease prevalence and no improvements in physical functioning or for several IADL tasks (e.g., preparing meals, managing money, light and heavy housework) from 1984 to 1994; however, elderly women had lesser increases in disease prevalence and significant improvements in physical functioning and IADL task performance. It also was shown that both elderly men and women had similar improvements in ADLs. Most other U.S. studies found that older women exhibited either the same or greater improvements in disability compared to older men from the 1980s to the 1990s (see Freedman, Martin, & Schoeni, 2002). Similar gendered patterns of improvement in disability are also found in Japan from the 1970s to 1990s (Saito et al., 2003; Schoeni et al., 2006) with the exception of the late 1980s when women’s bed disability-free life expectancy at age 65 worsened. In China, active life expectancy [(ALE) life expectancy without disability] was shown to improve for both sexes from 1987 to 1992 (Saito et al., 2003), although earlier research in Taiwan suggested that men had larger improvements in ALE and ADL functioning than women from 1986 to 1989 (Tu & Chen, 1994).
Sex-related changes in SRH and HLE over the past two decades have also been documented. In Austria, there are cross-sectional findings for the 1990s to suggest that elderly men and women reported similar improvements in very good, good, and fair SRH and HLE; women showed greater improvements when the categories were limited to very good and good (Doblhammer & Kytir, 2001). A study from the U.S. also demonstrated similar improvements in SRH among elderly men and women in the 1990s when good health was categorized as excellent, very good, and good (Zack et al., 2004). Using three categories of SRH (good, fair, not good), data from the U.K. showed that HLE among men increased more than women from 1981 to 2001 (U.K. National Statistics, 2006), and in China, improvements in SRH based on three categories were comparable for men and women in the late 1980s (Saito et al., 2003). Collectively, these findings indicate that gender differences in changes in SRH and HLE depend in part on the categorization of self-reported health.
DATA AND METHODS
Data
This study uses national data from the 1992 Old-Age Support Survey of the Chinese Elderly (OSSCE) and the 2002 Chinese Longitudinal Healthy Longevity Survey (CLHLS). The OSSCE was conducted in thirteen provinces/cities throughout mainland China to gather information on the elderly support system and to determine its policy implications by the China National Research Center on Aging (CNRCA). The OSSCE survey includes a multistage random sample of individuals selected according to (1) the economic, urbanization, and age strata of each province, and (2) the population of the city and the economic development of the county. Survey units are based on villages in rural areas (n = 47) and street blocks in urban areas (n = 49) in the thirteen provinces. Further details of the OSSCE sampling design and interview techniques are documented elsewhere and show that the data are of high quality (CNRCA, 1994).
The 2002 CLHLS is the third wave of data conducted in half of the randomly selected counties and cities in twenty-two provinces throughout China. The 2002 CLHLS is a national survey that included 48% newly interviewed persons aged 65 to 82 and 40% re-interviewed persons from the previous two waves of the CLHLS (1998 and 2000) who were aged 82 and older in 2002. Sampled individuals from the 1998 and 2000 waves who died or were lost to follow-up before 2002 (12%) were replenished with persons randomly selected from the same age and sex strata (refer to Zeng et al., 2008 for more sampling detail). All three subsamples of the 2002 CLHLS were randomly selected by age stratum and correspond nationally to the OSSCE survey. Much like the OSSCE, systematic assessments also indicate that the CLHLS data are of high quality (Zeng et al., 2008).
Data from the OSSCE and CLHLS were combined to provide two national datasets across a 10-year period. Studies show that combining data from multiple sources is appropriate for estimating health outcomes when the survey structures are sufficiently uniform and sampling weights are applied (Schenker & Raghunathan, 2007). Given the overall correspondence between the OSSCE and CLHLS datasets, we are confident that the weighted estimates from the two nationally representative samples are valid. Together, the two surveys cover twenty-three geographic areas across China and include interviews from both surveys in the following twelve major provinces: Beijing, Tianjin, Hebei, Heilongjiang, Shanghai, Jiangsu, Zhejiang, Hubei, Guangxi, Sichuan, Chongqing, and Shaanxi. Comparable data on the demographic characteristics, healthcare resources, and health conditions of participants were collected in both surveys. Among the twelve matching provinces, the 1992 OSSCE sample included 12,620 interviewed persons aged 65 and older (n = 6,590 women and 6,030 men). Of the 12,620 interviewees, 1,454 were ages 80 and over and 11,166 respondents were ages 65 to 79. The 1992 OSSCE did not collect data on institutionalized persons; therefore, institutionalized adults who were sampled in the 2002 CLHLS were excluded. Among the same provinces, the 2002 CLHLS included 9,583 interviewees (n = 5,493 women and n = 4,090 men), 6,544 aged 80 and over, and 3,039 aged 65 to 79. Thus, the combined analytic sample includes 22,203 respondents.
Measures
Health outcomes
Heath status was measured with three dichotomous outcomes: ADL disability, chronic conditions, and self-rated health (SRH). First, we used an abbreviated version of Katz’ ADL index based on compatible responses for the 1992 and 2002 surveys. Both datasets provided information on bathing, dressing, toileting, and eating (indoor transferring and continence are excluded in 1992). Results showed that bathing and eating ranked in the highest and lowest positions on the ADL functioning hierarchy, respectively, and suggested that the four items served as a valid approximation of the full ADL index. According to Freedman et al. (2004), the number of activities considered in the definition of disability is less important than the wording (“use help” vs. “have difficulty” vs. “use equipment”) and methodological techniques (e.g., age standardization). We tested the results based on three items – bathing, eating, and either toileting or dressing – and found that the results were almost the same with those based on four-items. The wording of the four ADL items in the two surveys was nearly identical (see Sagardui-Villamor et al. 2005 for a related analysis of these items). Persons with no ADL limitations were classified as ‘ADL active’ and those with one or more limitations were classified as ‘ADL disabled.’ Second, the OSSCE and CLHLS surveys collected the same information on various diseases (including hypertension, stroke, heart diseases, cerebrovascular disease, pneumonia, arthritis, etc.). For this analysis, we operationalized chronic disease as having at least one disease (coded 1) compared to no diseases. Comparisons of prevalence rates in the CLHLS with other external nation-wide surveys indicated that data on chronic conditions are valid and reliable (Zeng et al., 2008). Third, SRH in the 1992 OSSCE survey was based on three categories (good, so-so, and bad) with responses of “so-so” and “bad” being categorized as poor (coded 1) compared to good SRH. The 2002 CLHLS included five categories of SRH (very good, good, so-so, bad, and very bad) with responses of “so so,” “bad,” and “very bad” being categorized as poor health (coded 1). The patterns were approximately the same when combining “so-so” with “good” and “very good.”
Control variables
To minimize confounding bias in the estimates of health change from 1992 to 2002, we adjusted for individual differences in demographic characteristics, socioeconomic status (SES), and healthcare resources. Demographic variables included age (in years), residence (urban vs. rural), and ethnicity (Han vs. non-Han minorities). Measures of SES included categorical levels of education (no formal schooling, 1–6 years, and 7+ years) and a dichotomous indicator of economic well-being (coded 1 if respondent reports sufficient financial resources in daily life). Variables indicating healthcare resources included current married status (yes/no), living alone (yes/no), the number of living children (0, 1–2, 3–4, and 5+), and whether the respondent was covered by free public medical services at the time of the survey (yes/no). All control variables were previously shown to be associated with the three health outcomes (Stuck et al., 1999; Szaflarski & Cubbins, 2004). Table 1 presents the sample distributions of the study variables by health outcome for the 1992 and 2002 surveys.
Table 1.
Sample distributions of covariates by health status in the 1992 and 2002 surveys
| 1992 OSSCE survey |
2002 CLHLS survey |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sample size | ADL disabled | Chronic disease | Poor self-rated health | Sample size | ADL disabled | Chronic disease | Poor self-rated health | |||
| #a | %a | %b | %b | %b | #a | %a | %b | %b | %b | |
| Total | 12,620 | 100.00 | 7.91 | 66.66 | 65.60 | 9,583 | 100.00 | 7.27 | 60.39 | 50.59 |
| Age | ||||||||||
| 65–79 | 11,166 | 88.48 | 5.59 | 66.76 | 64.56 | 3,039 | 31.71 | 5.18 | 59.77 | 49.76 |
| 80+ | 1,454 | 11.52 | 21.53 | 66.09 | 71.69 | 6,544 | 68.29 | 19.42 | 64.00 | 55.39 |
| Sex | ||||||||||
| Women | 6,590 | 52.22 | 8.95 | 68.72 | 69.83 | 5,493 | 57.32 | 8.61 | 61.94 | 53.11 |
| Men | 6,030 | 47.78 | 6.75 | 64.36 | 60.88 | 4,090 | 42.68 | 5.78 | 58.66 | 47.77 |
| Residence | ||||||||||
| Rural | 6,391 | 50.64 | 6.05 | 60.06 | 63.56 | 4,987 | 52.04 | 6.15 | 54.69 | 50.32 |
| Urban | 6,229 | 49.36 | 10.91 | 77.33 | 68.89 | 4,596 | 47.96 | 9.07 | 69.59 | 51.02 |
| Ethnicity | ||||||||||
| Minorities | 543 | 4.30 | 5.99 | 60.53 | 68.50 | 701 | 7.32 | 4.52 | 44.81 | 49.20 |
| Han | 12,077 | 95.70 | 8.01 | 66.97 | 65.45 | 8,882 | 92.68 | 7.38 | 61.03 | 50.65 |
| Education | ||||||||||
| No schooling | 7,141 | 56.58 | 7.93 | 65.49 | 68.44 | 5,812 | 60.65 | 8.78 | 59.29 | 53.84 |
| 1–6 years | 3,960 | 31.38 | 7.54 | 66.60 | 61.88 | 2,735 | 28.54 | 5.28 | 59.18 | 47.98 |
| 7+ years | 1,519 | 12.04 | 8.85 | 73.62 | 59.92 | 1,036 | 10.81 | 6.79 | 67.03 | 45.58 |
| Economic well-being | ||||||||||
| No | 3,621 | 28.69 | 9.87 | 71.60 | 77.89 | 1,924 | 20.08 | 7.81 | 67.96 | 69.80 |
| Yes | 8,999 | 71.31 | 6.99 | 64.34 | 59.83 | 7,657 | 79.90 | 7.14 | 58.55 | 45.92 |
| Marital status | ||||||||||
| Not married | 5,129 | 40.64 | 9.67 | 66.47 | 67.48 | 6,396 | 66.74 | 10.48 | 59.96 | 54.40 |
| Currently Married | 7,491 | 59.36 | 6.54 | 66.81 | 64.14 | 3,187 | 33.26 | 5.23 | 60.66 | 48.17 |
| Living alone | ||||||||||
| No | 10,762 | 85.28 | 8.48 | 66.48 | 65.19 | 8,222 | 85.80 | 7.74 | 60.48 | 48.91 |
| Yes | 1,858 | 14.72 | 4.70 | 67.66 | 67.95 | 1,361 | 14.20 | 4.11 | 59.80 | 61.93 |
| Number of living children | ||||||||||
| 0 | 334 | 2.65 | 9.04 | 68.16 | 74.09 | 940 | 9.81 | 10.58 | 55.00 | 59.03 |
| 1–2 | 3,019 | 23.92 | 9.65 | 68.43 | 68.22 | 2,544 | 26.55 | 6.97 | 60.82 | 49.17 |
| 3–4 | 4,425 | 35.06 | 7.23 | 66.43 | 64.47 | 3,360 | 35.06 | 7.13 | 61.46 | 50.79 |
| 5+ | 4,842 | 38.37 | 7.32 | 65.58 | 64.28 | 2,739 | 28.58 | 7.18 | 59.66 | 50.07 |
| Covered by free public medical services | ||||||||||
| No | 8,627 | 68.36 | 7.88 | 61.67 | 64.40 | 8,308 | 86.70 | 7.12 | 58.12 | 51.28 |
| Yes | 3,993 | 31.64 | 8.01 | 82.27 | 69.35 | 1,275 | 13.30 | 8.08 | 72.36 | 46.95 |
Note: unweighted
weighted
Analytic Strategy
Standardization
Studies suggest that variations in survey design and individual heterogeneity introduce bias when comparing health change across time (Freedman et al., 2004). Therefore, standardization by sex (e.g., Freedman et al., 2002) and urban/rural residence (e.g., Gu & Zeng, 2004; Laditka, 2005) is essential. Due to the unique designs of the OSSCE and CLHLS surveys, we first applied separate weights to match the total age-sex-urban/rural and living arrangements distributions in the twelve overlapping provinces in 1992 and 2002 surveys as estimated from the 1990 and 2000 censuses, respectively. The weighted samples match the age-sex-urban/rural specific distributions according to living arrangements in the 12 provinces estimated from the 1990 and 2000 censuses. We then standardized the age-sex-urban/rural compositions of the two datasets as previously shown in the literature (Freedman et al., 2004) and the new weight was used for all analyses to adjust for major structural compositions of the two sampled populations.
Logistic regression
We used multiple logistic regression models to examine how improvements in health status are mediated by several covariates. The following model and delta method were used to estimate the annual change of health status (Waidmann & Liu, 2000): , where p is the probability of being in a given category (or event), βixi is the product of explanatory variable xi and the unknown βicoefficient. Note that t distinguishes the year of the survey (i.e., 1992 or 2002) and is added to the regression model to estimate the change between survey intervals. γ is an unknown coefficient. All models are run separately by sex because previous research has shown that elderly men and women have different trajectories of morbidity and disability (e.g., Lamb, 1997). There is evidence in our data that also support this analytical strategy. For instance, after adjustments for age, socioeconomic status, and health care resources, men were 20–28% (p<.001) less likely to be ADL disabled, have a chronic disease, and poor health compared to women. Furthermore, men were about 55% (p<.001) less likely than women to have ADL disability from 1992 to 2000, whereas men were 15% (p=.009) and 13% (p=.033) more likely to experience respective declines in self-rated health and chronic conditions compared to women.
We estimated three sequential models to examine how various covariates influenced changes in health. Model I tested the annual rate of change for each of the three health outcomes adjusting for age, residence, and ethnicity. Preliminary analyses showed no significant effects for an age-squared term and an interaction between age and survey year and were excluded from the final models. Based on established research, the initial model (Model I) established the baseline estimates for the standardized results. Model II then tested how the annual rate of change for each health outcome was influenced by the SES variables. Model III further tested the rate of health change by including the variables for healthcare resources. The purpose of using sequential model was to demonstrate how compositional differences in SES and healthcare resources related to changes in ADL disability, chronic disease, and SRH from 1992 to 2002. Because disease is often the precursor to disability (Verbrugge & Jette, 1994), an additional model for ADL disability (Model IV) was included to control for chronic disease. Likewise, because ADLs and chronic disease largely influence perceptions of health (Bosworth et al., 1999; Tobiasz-Adamczyk & Brzyski, 2005), an additional model for SRH (Model IV) included controls for these two objective health indicators.
Life tables
In many cases the effects of health improvements on increases in health expectancies are more informative than absolute changes in health status. Age-sex-specific mortality in 1992 was interpolated based on published census data for the twelve provinces in 1990 and 2000. Mortality schedules for 2002 were extrapolated from the 1990 and 2000 Chinese censuses. Prevalence rates of age-specific disability, chronic disease, and self-rated health were estimated with sequential models for men and women. Based on previous research (refer to Robine et al., 2003; Hayward & Warner, 2005), we employed Sullivan’s method to estimate disability-free life expectancy (a.k.a. ALE), disease-free life expectancy (DFLE), and healthy life expectancy (HLE) in 1992 and 2002. The common formula to calculate a health expectancy is (see Lamb & Siegel, 2004), or in continuous form , where HEx represent health expectancy; lx is the number of living persons in the life table at age x; Lx is person-years lived at age x; hx is the prevalence of the healthy state (e.g., ADL active) at age x; is person-years lived in a healthy state at age x. Using the Sullivan method, expected years in disability-free, disease-free, and good SRH states were calculated by applying the corresponding cross-sectional age-sex-specific prevalence rates to the person-years lived in different age categories derived from period life tables in 1992 and 2002, respectively.
Decompositions
Improvements in health expectancies from 1992 to 2002 could be due to either improvements in health status or mortality. The following method was used to decompose improvements in health expectancies:
where is the change in health expectancy at age x between time t1 and time t2; and are the health expectancies at age x for time t1 and time t2 respectively; and are the prevalence rates of health status (referring to ADL active, no diseases, or good self-rated health) at age x for times t1 and t2 respectively; and are the number of living individuals in the life table at age x (in relative terms it is the survival probability from birth to age x ) for time t1 and time t2, respectively. The first part of the right-side equation estimates the change in health expectancy due to the change in prevalence rate of a specific health outcome and the second part of the equation estimates the change in health expectancy due to survival probability (i.e., mortality). In doing so, we estimated the proportion of the contribution in changed health expectancy due to changes in either health status or mortality by dividing the right side of the equation over the total change of . Because we differentiated how changes in health status were impacted by various covariates in the logistic analyses, we likewise investigated how the association between changes in health status and health expectancies was influenced by the addition of the control variables. However, we were unable to examine how differences in survival probabilities were affected by the various covariates because the data are cross-sectional and the only officially released life tables are age-sex-specific. Therefore, we applied different sets of age-sex-specific prevalence rates of disability, morbidity, or poor SRH to survival probabilities in 1992 and 2002, respectively. In other words, we assumed that each age-gender-specific person experienced the same rate of improvement in survival from 1992 to 2002, which may be unrealistic; however, this is an inherent deficiency of the Sullivan method.
RESULTS
Improvements in Health Status
Table 2 presents the results from the weighted logistic models of the annual change in the rates of the health outcomes from 1992 to 2002. Overall, the demographic-adjusted results show significant improvements in chronic disease and SRH over the 10-year period. The results for ADL disability are not statistically significant in any of the models; however, it is noteworthy that the annual decline for older men is much larger than for older women. We find that improvements in SRH are largest among the three health outcomes and the improvements appear to be independent of disability and disease. The annual decline in SRH was 2.4% for men and 2.7% for women and the rates of change fluctuated by 1.4–1.9% for men and by approximately 2.4% for women depending on the covariates included in the analyses (Models II-IV).
Table 2.
Average annual percentage change (95% CI) in prevalence rates of ADL disability, chronic disease, and poor self-rated health from 1992 to 2002 among adults aged 65+ in China Model I
| Model I | Model II | Model III | Model IV | |
|---|---|---|---|---|
| Men | ||||
| ADL disabled | −1.72 (−4.14, 0.67) | −1.37 (−3.83, 1.06) | −0.81 (−3.34, 1.73) | −0.18 (−3.05, 2.85) |
| Having 1+ chronic diseases | −0.96 (−1.51, −0.44)*** | −0.82 (−1.38, −0.31)* | −0.62 (−1.28, −0.03)* | NA |
| Poor self-rated health | −2.43 (−3.10, −1.79)*** | −1.87 (−2.53, −1.25)*** | −1.44 (−2.22, −0.73)*** | −1.39 (−2.26, −0.61)*** |
| Women | ||||
| ADL disabled | −0.50 (−2.40, 1.36) | −0.22 (−2.14, 1.68) | −0.42 (−2.39, 1.53) | 0.65 (−1.51, 2.96) |
| Having 1+ chronic diseases | −1.06 (−1.55, −0.61)*** | −0.90 (−1.38, −0.05)*** | −0.82 (−1.31, −0.37)*** | NA |
| Poor self-rated health | −2.74 (−3.33, −2.19)*** | −2.35 (−2.92, −1.81)*** | −2.37 (−2.96, −1.83)*** | −2.39 (−3.02, −1.79)*** |
Note: (1) Model I controls for age, residence, and ethnicity. Model II further adjusts for education and economic well-being. Model III further adjusts for marital status, living arrangement, number of living children, and access to free public medical service. Model IV further adjusts for chronic disease for the ADL disability rates and adjusts for chronic disease and ADL disability for the SRH rates.
(2) NA, not applicable.
(3) *, p<0.05; **, p<0.01; ***, p<0.001.
Increased Health Expectancies
Table 3 reports the age-sex-specific ALE, DFLE, and HLE results and their corresponding proportions of total life expectancy (TLE) for 1992 and 2002 after adjusting for urban/rural residence and ethnicity. Although women enjoy longer life expectancy and health expectancies in both 1992 and 2002, men exhibit higher proportions of healthy lives. Table 3 and Table 4 further show that from 1992 to 2002 women gained more in both the absolute number of years and relative proportions in TLE, DFLE, and HLE compared to men. However, these gains are reduced for both sexes after controlling for covariates.
Table 3.
Comparisons of total and healthy life expectancies between 1992 and 2002 among adults aged 65+ in China
| Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|
| Sex and age | TLE | ALE | DFLE | HLE | TLE | ALE | DFLE | HLE |
| 1992 (in years) | ||||||||
| 65 | 12.86 | 11.89 | 4.48 | 4.93 | 15.11 | 13.56 | 4.60 | 4.48 |
| 70 | 9.90 | 8.93 | 3.33 | 3.57 | 11.89 | 10.30 | 3.52 | 3.37 |
| 75 | 7.46 | 6.50 | 2.42 | 2.52 | 9.14 | 7.52 | 2.64 | 2.47 |
| 80 | 5.51 | 4.55 | 1.72 | 1.73 | 6.88 | 5.23 | 1.93 | 1.77 |
| 85 | 4.07 | 3.11 | 1.22 | 1.18 | 5.14 | 3.47 | 1.40 | 1.25 |
| 90 | 3.02 | 2.06 | 0.87 | 0.80 | 3.83 | 2.17 | 1.01 | 0.88 |
| 95 | 2.32 | 1.34 | 0.63 | 0.56 | 2.89 | 1.28 | 0.73 | 0.62 |
| 100 | 1.85 | 0.86 | 0.48 | 0.41 | 2.24 | 0.71 | 0.55 | 0.45 |
| 2002 (in years) | ||||||||
| 65 | 14.05 | 13.08 | 5.69 | 7.17 | 16.85 | 15.03 | 6.27 | 7.74 |
| 70 | 10.84 | 9.88 | 4.26 | 5.28 | 13.22 | 11.39 | 4.81 | 5.87 |
| 75 | 8.23 | 7.28 | 3.14 | 3.81 | 10.15 | 8.32 | 3.60 | 4.35 |
| 80 | 6.05 | 5.10 | 2.22 | 2.64 | 7.55 | 5.73 | 2.61 | 3.11 |
| 85 | 4.60 | 3.63 | 1.63 | 1.88 | 5.74 | 3.87 | 1.93 | 2.26 |
| 90 | 3.39 | 2.41 | 1.15 | 1.29 | 4.32 | 2.46 | 1.41 | 1.63 |
| 95 | 2.62 | 1.62 | 0.85 | 0.92 | 3.28 | 1.46 | 1.03 | 1.17 |
| 100 | 2.09 | 1.06 | 0.65 | 0.67 | 2.52 | 0.82 | 0.77 | 0.85 |
| 1992 (% of TLE) | ||||||||
| 65 | 100.00 | 92.46 | 34.84 | 38.38 | 100.00 | 89.72 | 30.44 | 29.67 |
| 70 | 100.00 | 90.26 | 33.69 | 36.11 | 100.00 | 86.68 | 29.65 | 28.37 |
| 75 | 100.00 | 87.12 | 32.50 | 33.79 | 100.00 | 82.30 | 28.84 | 27.04 |
| 80 | 100.00 | 82.64 | 31.26 | 31.41 | 100.00 | 76.05 | 28.00 | 25.68 |
| 85 | 100.00 | 76.42 | 29.98 | 28.99 | 100.00 | 67.47 | 27.13 | 24.30 |
| 90 | 100.00 | 68.16 | 28.66 | 26.57 | 100.00 | 56.54 | 26.23 | 22.89 |
| 95 | 100.00 | 57.95 | 27.32 | 24.17 | 100.00 | 44.08 | 25.30 | 21.48 |
| 100 | 100.00 | 46.51 | 25.97 | 21.85 | 100.00 | 31.74 | 24.34 | 20.07 |
| 2002 (% of TLE) | ||||||||
| 65 | 100.00 | 93.11 | 40.54 | 51.06 | 100.00 | 89.19 | 37.20 | 45.93 |
| 70 | 100.00 | 91.17 | 39.34 | 48.72 | 100.00 | 86.23 | 36.37 | 44.43 |
| 75 | 100.00 | 88.41 | 38.10 | 46.24 | 100.00 | 81.98 | 35.49 | 42.87 |
| 80 | 100.00 | 84.43 | 36.78 | 43.60 | 100.00 | 75.88 | 34.57 | 41.20 |
| 85 | 100.00 | 78.82 | 35.40 | 40.85 | 100.00 | 67.49 | 33.60 | 39.45 |
| 90 | 100.00 | 71.29 | 33.99 | 38.02 | 100.00 | 56.81 | 32.59 | 37.63 |
| 95 | 100.00 | 61.65 | 32.52 | 35.11 | 100.00 | 44.60 | 31.55 | 35.76 |
| 100 | 100.00 | 50.52 | 31.03 | 32.21 | 100.00 | 32.40 | 30.45 | 33.82 |
Note: (1) Estimates based on Model I in Table 2.
(2) TLE, total life expectancy; ALE, active life expectancy; DFLE, Disease-free life expectancy; HLE, Healthy life expectancy.
Table 4.
Proportion of years gained in life expectancy from 1992 to 2002 among adults aged 65+ in China
| Men (%) |
Women (%) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Ages | TLE | ALE | DFLE | HLE | TLE | ALE | DFLE | HLE |
| Model I | ||||||||
| 65 | 9.27 | 10.04 | 27.16 | 45.38 | 11.53 | 10.86 | 36.32 | 72.63 |
| 70 | 9.48 | 10.60 | 27.87 | 47.69 | 11.17 | 10.59 | 36.35 | 74.12 |
| 80 | 9.79 | 12.16 | 29.17 | 52.43 | 9.75 | 9.51 | 35.49 | 76.06 |
| 85 | 12.87 | 16.42 | 33.30 | 59.05 | 11.55 | 11.59 | 38.16 | 81.12 |
| 90 | 11.99 | 17.13 | 32.80 | 60.26 | 12.73 | 13.27 | 40.09 | 85.31 |
| 95 | 13.14 | 20.37 | 34.68 | 64.33 | 13.16 | 14.48 | 14.12 | 88.39 |
| 100 | 12.93 | 22.66 | 34.94 | 66.46 | 12.49 | 14.80 | 40.72 | 89.59 |
| Model IV a | ||||||||
| 65 | 9.27 | 8.94 | 20.74 | 30.99 | 11.53 | 9.81 | 30.19 | 65.82 |
| 70 | 9.48 | 9.11 | 21.35 | 31.81 | 11.17 | 9.13 | 30.36 | 66.16 |
| 75 | 10.40 | 10.00 | 22.75 | 33.51 | 10.99 | 8.51 | 30.71 | 66.77 |
| 80 | 9.79 | 9.29 | 22.43 | 33.37 | 9.75 | 6.62 | 29.79 | 65.80 |
| 85 | 12.87 | 12.36 | 26.25 | 37.75 | 11.55 | 7.54 | 32.44 | 69.46 |
| 90 | 11.99 | 11.48 | 25.70 | 37.36 | 12.73 | 7.68 | 34.39 | 72.23 |
| 95 | 13.14 | 12.64 | 27.37 | 39.44 | 13.16 | 7.09 | 35.49 | 73.92 |
| 100 | 12.93 | 12.56 | 27.52 | 39.85 | 12.49 | 5.55 | 35.21 | 73.86 |
Note: (1) TLE, total life expectancy; ALE, active life expectancy; DFLE, Disease-free life expectancy; HLE, Healthy life expectancy.
(2) Estimates for DFLE are from Model III in Table 2.
(3) Proportion of year gained for TLE is the difference in TLE between 1992 and 2002 divided by TLE in 1992 for each sex and age group. Proportions for ALE, DFLE, and HLE are also calculated accordingly.
In relative terms, both men and women exhibited a greater increase in DFLE and HLE, along with TLE. Interestingly, the oldest-old adults (ages 80+) gained relatively more DFLE and HLE compared to elderly men and women aged 65 to 79. With respect to improvements in ALE, elderly women gained more absolute years in ALE before age 80 than elderly men (Table 3). Yet, in relative terms (Table 4), men gained more years in ALE for all ages above 65 compared to women; however the gains for both men and women were reduced after adjusting for covariates (results from Models II and III, not shown). Furthermore, when controlling for all covariates, the relative age patterning for ALE for men increases monotonically regardless of the adjustments, whereas women exhibit a similar pattern only in the absence of covariates. The gendered patterns of improvements in chronic disease and SRH are consistent in both absolute and relative terms.
Decomposition of Increased Health Expectancies
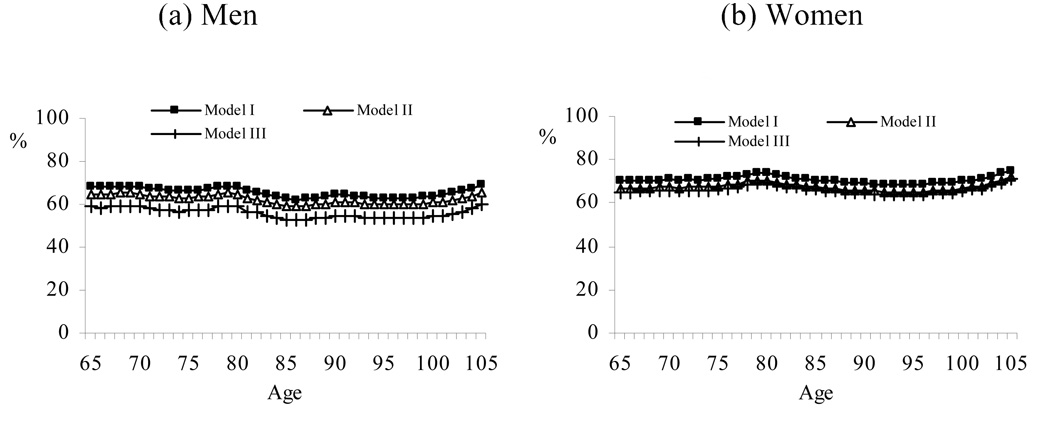
Our analysis cannot address whether reductions in mortality are associated with the differential characteristics of the population. Therefore, we assume that each age-sex-specific individual experiences similar improvements in mortality from 1992 to 2002. Under this assumption, we examine how improvements in health status contribute to increases in health expectancies. Figure 1 illustrates the percentages in increased ALE due to improvements in disability by sex for each covariate-adjusted model. In all cases, increases in ALE from 1992 to 2002 due to improvements in ADL disability are larger among elderly men than women. For instance, Model I shows that the decline in disability contributes 15% of the increase in active life expectancy (ALE) for men age 65 compared to 5% for women at the same age. That is, much of the increase in ALE at age 65 for men and women is attributed to reductions in mortality.
Figure 1.
Relative impact of disability prevalence on active life expectancy, China (1992–2002)
Note: * Model IV is not presented because ALE declined from 1992 to 2002. %, the shared proportion of increased ALE attributable to improved ADL functioning from 1992 to 2002.
The contribution of declines in disability to ALE increases with advancing age and is more pronounced in elderly men than women. However, the contribution related to improved ADL functioning disappears for men and becomes negative for women once disease conditions are included with only controls for SES and health resources (see Figure 1). This finding suggests that increases in male and female ALE from 1992 to 2002 are primarily due to improvements in chronic diseases and other associated factors. More interestingly, Table 2 shows that ADL disability among women increased slightly from 1992 to 2002 given the same levels of disease prevalence and other covariates. Indeed, the proportion of ALE out of TLE is slightly lower (though not statistically significant) in 2002 compared to 1992 without adjustments for SES, healthcare resources, and chronic diseases.
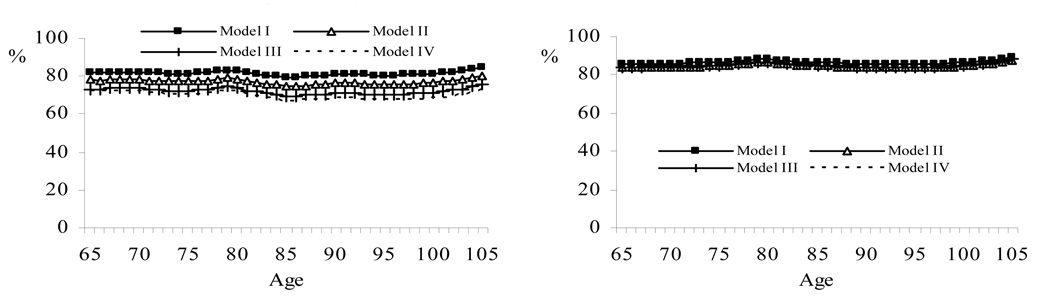
Figure 2 illustrates the relative contributions to DFLE due to chronic disease prevalence by sex and for each of the covariate-adjusted models. Assuming 1992 and 2002 share the same demographic and SES characteristics, the increases in DFLE over the 10 years due to a decline in disease prevalence are approximately 60 to 70% for men and women. Further assuming comparable healthcare resources in 1992 and 2002, the contribution to DFLE is a marginal decline for men and a slight increase for women. Unlike the age patterning observed for ALE, the contribution of lower disease rates to DFLE for all models is constant across age. Therefore, 30–40% of the improvement in DEFL during this period can be attributed to declines in mortality.
Figure 2.
Relative impact of chronic disease prevalence on disease-free life expectancy, China (1992–2002)
Note: %, the shared proportion of increased DFLE attributable to reduced disease prevalence from 1992 to 2002.
Results in Figure 3 suggest that the contributions of improved perceived health (SRH) and increased HLE are nearly identical across all ages for women despite the covariate adjustments (~80–85%). For men, approximately 80% of increased HLE is due to improved SRH after controlling for demographic characteristics and SES factors. Controlling for healthcare resources, disability, and disease decreases the contribution to 70%, although remaining the key factor for increases in HLE. These results suggest that increases in HLE from 1992 to 2002 were mainly attributable to improvements in SRH and not to the compositional changes in the population. The decline in mortality only attributed to increases in HLE by less than 20% in women and by 20–30% in men.
Figure 3.
Relative impact of self-rated health on healthy life expectancy, China (1992–2002)
Note: %, the shared proportion of increased HLE attributable to improved SRH from 1992 to 2002.
DISCUSSION
The present study is unique because it investigates changing health and health expectancies using two large national datasets from China, a rapidly developing country with the world’s largest elderly population. The results showed that elderly men and women in China exhibited significant improvements in chronic disease and SRH from 1992 to 2002, although improvements in ADL functioning were not statistically significant. Health expectancies measured as ALE, DFLE, and HLE increased during this period and were patterned differently according to sex and changes in disease prevalence, mortality decline, and individual health assessments. Overall, our findings support the compression of morbidity hypothesis for older adults in China from 1992 to 2002. However, the general improvements we identified in these major health indicators do not concur with most studies in developed nations (Robine & Michel, 2004).
Results from multivariate models adjusted for SES and healthcare resources showed that improvements in ADL functioning accounted for a portion of the relative contributions to increases in ALE from 1992 to 2002 for both sexes. However, there was almost no contribution attributed to ADL functioning for men after further controlling for disease prevalence. For women, ADL functioning declined when adjusting for chronic disease and thus its contribution to ALE was instead negative. These findings suggest that advances in ALE for men and women were primarily due to reductions in disease prevalence and supports the argument that disability rates remain relatively stable when the progression of disease is controlled (Robine & Michel, 2004). Such findings may reflect medical and technical advances in the treatments, devices, and accommodations for persons to help them achieve better functioning in their environments (Freedman et al., 2004). Indeed, recent research has shown that home-care facilities improved greatly in China during the 1990s (Yu, 2006). If this is the case, ADL improvements between 1992 and 2002 in China may be overestimated without information on the use of medical equipment and other apparatus that may conceal an underlying trend in unassisted functioning. However, more research is needed to validate this argument.
The findings also showed that the relative contribution of reduced chronic disease to increases in DFLE was approximately 60–70% for men and women and the contribution of improved SRH to increases in HLE was 70%85% for men and 80–85% for women. Overall, we found that SRH improved at a greater rate than disability and chronic disease. It is plausible that these findings reflect in part the general improvements in socioeconomic conditions of older adults in China between 1992 and 2002. Recent Chinese censuses showed that illiteracy rates among Chinese adults aged 60 and older declined dramatically from 70% in 1990 to 42% in 2000 and that per capita family income doubled during the same period (National Statistics of China, 2003). These factors corroborate evidence showing that SES is positively associated with SRH (Liu & Zhang, 2004; Popham & Mitchell, 2007). Alternatively, improvements in SRH could reflect possible changes in disease detection and subjective reports of health problems following health care reforms in China that limited access to health services during the 10-year period (Yip & Hsiao, 2008). It is also possible that measurement biases due to subjective reporting and the different number of categories for SRH in the two surveys. For these reasons we remain guarded in our interpretations of the improvements in SRH and HLE from 1992 to 2002.
One striking finding is the gender difference in health-change over time. We found that elderly men had larger annual declines in rates of disability and greater increases in relative ALE compared to elderly women. This finding is consistent with previous studies showing that women are at greater risk of disability and living longer with disabilities at older ages as the epidemiologic transition progresses (Myers, Lamb, & Agree, 2003; Tu & Chen, 1994). We further showed that elderly women experienced greater annual improvements in rates of chronic disease and SRH from 1992 to 2002 compared to men, with greater relative gains in DFLE and HLE. The finding that women had greater improvements in SRH than men is consistent with previous research and suggests that women have greater symptom recognitions and knowledge of disease history which may influence their reported SRH (Chen & Wu, 2008; Doblhammer & Kytir, 2001). Although the gender differences in chronic disease reductions from 1992 to 2002 may be a reflection of changes in the disablement process (Verbrugge & Jette, 1994), it also may be due to more undiagnosed conditions among older women due to their lesser accessibility to healthcare facilities in this period (Gao, Raven, & Tang, 2007).
Another noteworthy finding is that men and women exhibited a significant age-graded increase in ALE, but not for DFLE or HLE. We found that increases in ALE were greatest among oldest-old men and women and there was an upward trend across age with respect to the contribution of disability decline to improvements in ALE. Decomposition analyses showed no age differences in the relative contribution of less chronic disease to increases in DFLE and improved SRH to increases in HLE. To our knowledge, these patterns have not been documented and suggest that improvements in DFLE and HLE were universal across age from 1992 to 2002 in China.
We suspect that the uniform health-improvements in China reflect the distinct stage(s) in the epidemiologic transition that differentiate(s) many Western nations from developing nations like China. As noted earlier, China initiated its epidemiologic transition in the 1980s and it is thought that Chinese elders began to manifest improvements in the major health domains in the 1990s. This finding supports the argument that advances in public health knowledge, improved health behaviors, and new diagnostic and medical technology in the initial stage of the epidemiologic transition promotes greater awareness of health and illness that helps reduce disability and morbidity before increases in longevity are achieved (Myers et al., 2003; Robine & Michel, 2004). A key contribution of the present study is that it is the first to document changes in three major health indicators from a developing country in an epidemiologically important period.
We recognize several limitations of this study. First, the results may not be fully generalizable to the population because the institutionalized elderly were not included in the 1992 survey. However, such bias is presumably small given the low rates of institutionalization (< 2%) and that health differences between the institutionalized and community-dwelling elderly is much smaller in China than most Western countries (Gu et al., 2007). Second, as previously noted, our reliance on cross-sectional data precluded examinations of the relationships between various covariates and survival. This limitation prohibited us from knowing how improvements in mortality are associated with improvements in health status. Consequently, we had to assume no differences in improved mortality across individuals and could not determine differences in the contributions of the three health statuses to their corresponding health expectancies. Our analyses focused exclusively on the prevalence of health conditions with cross-sectional data. However, longitudinal research shows that changes in the onset, recovery, and deaths related to health conditions (i.e., incidence and duration) are also important dimensions of health patterns across age and time (Dupre, 2007). Multi-wave data over longer periods are necessary to disentangle these issues and, unfortunately, are lacking in most developing countries (Hayward & Warner, 2005). Third, the study was limited to an overall classification of chronic disease during the 1990s. We encourage future studies to differentiate fatal and non-fatal diseases to determine if the health trends reported here are generalizable or disease-specific, as others have shown (e.g., Crimmins & Saito, 2000; Robine & Michel, 2004).
Another limitation is that we were unable to examine whether changes in the social and economic forces influence the prevention and treatment of health conditions. It is likely that social and economic factors led to changes in health-related behaviors, technology, and self–monitoring (i.e., check-ups and/or seeking treatment). We had to assume that health awareness, reports, and were constant from 1992 to 2002 and may have biased our results upward by showing greater improvements in health conditions than what may be the case. Lastly, we used a global measure of chronic disease and did not consider disease-specific prevalence and disease-specific free life-expectancy. We encourage future research to investigate these relationships to enhance policies and health interventions that are often disease-specific.
Despite these limitations, the findings of our study may have important policy implications. It is well known that the number of older adults in China will increase dramatically over the next few decades and most Chinese families practice filial piety. The number of the Chinese elderly population (aged 65+) reached 13 million at the 2000 census and these numbers are projected to be 236 million and 334 million by the years 2030 and 2050, respectively. The corresponding figures for the oldest-old (aged 80+) are 42 million and 103 million persons by 2030 and 2050 (Population Division, U.N., 2007). In a society marked by a culture of filial piety and family care, it is plausible that if future cohorts of Chinese elderly continue to achieve greater active, disease-free, and healthy life-expectancy, there may be a considerable reduction in medical expenditures and long-term care needs. Such improvements also may facilitate China’s development given a concurrent demographic structure that is expected to maintain a large working-age population before the year 2030 (Population Division, U.N., 2007).
Acknowledgments
The data used in this study were from the Old-Age Support Survey of the Chinese Elderly in 1992 and the Chinese Longitudinal Healthy Longevity Survey in 2002. The latter survey was funded by the National Institute on Aging (R01 AG023627, Principle Investigator: Zeng Yi), the China Natural Science Foundation, China Social Science Foundation, UNFPA, and Hong Kong Research Grant Council. Danan Gu's work was supported by NIA grant R01 AG023627 (Duke University) and Provost Internationalization Mini-Grant at Portland State University. Zeng Yi's work was supported by NIA grant R01 AG023627.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Danan Gu, Email: gudanan@yahoo.com, Portland State University Portland, OR UNITED STATES.
Matthew E Dupre, Department of Sociology/Center for the Study of Aging and Human Development, Duke University
David F Warner, Department of Sociology, Case Western Reserve University
Yi Zeng, Center for the Study of Aging and Human Development, Duke University/China Center for Economic Research, Peking University
REFERENCES
- Aromaa A, Koskinen S, Huttunen J. Health in Finland. Helsinki: National Public Health Institute; 1999. [Google Scholar]
- Bosworth HB, Siegler IC, Brummett BH, Barefoot JC, Williams RB, Vitaliano PP, Clapp-Channing N, Lytle BL, Mark DB. The Relationship between Self-Rated Health and Health Status among Coronary Artery Patients. Journal of Aging and Health. 1999;11(4):565–584. doi: 10.1177/089826439901100405. [DOI] [PubMed] [Google Scholar]
- China National Research Center on Aging (CNRCA) Data book of Old-age Support Survey on Chinese Elderly. Beijing: Hualin Press; 1994. [Google Scholar]
- China National Research Center on Aging (CNRCA) Data analysis of the Sampling of Survey of the Aged Population in China. Beijing: China Standard Press; 2003. [Google Scholar]
- Chen J, Wu Z. Gender differences in the effects of self-rated health status on mortality among the oldest-old in China. In: Zeng Y, Poston D, Vlosky DA, Gu D, editors. Healthy longevity in China: Demographic, socioeconomic, and psychological dimensions. Dordrecht, The Netherlands: Springer Publisher; 2008. pp. 397–418. [Google Scholar]
- Crimmins EM. Trends in the health of the elderly. Annual Review of Public Health. 2004;25:79–98. doi: 10.1146/annurev.publhealth.25.102802.124401. [DOI] [PubMed] [Google Scholar]
- Crimmins EM, Saito Y. Change in the prevalence of diseases among older Americans: 1984–1994. Demographic Research. 2000;3(online) Artic. 9. [Google Scholar]
- Crimmins EM, Saito Y. Trends in healthy life expectancy in the United States 1970–1990: Gender, racial, and educational differences. Social Science and Medicine. 2001;52:1629–1641. doi: 10.1016/s0277-9536(00)00273-2. [DOI] [PubMed] [Google Scholar]
- Doblhammer G, Kytir J. Compression or expansion of morbidity? Trends in healthy-life expectancy in the elderly Austrian population between 1978 and 1998. Social Science & Medicine. 2001;52:385–391. doi: 10.1016/s0277-9536(00)00141-6. [DOI] [PubMed] [Google Scholar]
- Dupre ME. Educational differences in age-related patterns of disease: Reconsidering cumulative disadvantage and age-as-leveler. Journal of Health and Social Behavior. 2007;48(1):1–15. doi: 10.1177/002214650704800101. [DOI] [PubMed] [Google Scholar]
- Freedman VA, Crimmins EM, Schoeni RF, Spillman BC, Aykan H, Kramarow E, Land KC, Lubitz J, Manton KG, Martin LG, Shinberg D, Waidmann T. Resolving inconsistencies in trends in old-age disability: Report from a technical working group. Demography. 2004;41(3):417–441. doi: 10.1353/dem.2004.0022. [DOI] [PubMed] [Google Scholar]
- Freedman VA, Martin LG, Schoeni RF. Recent trends in disability and functioning among older adults in the United States: A systematic review. Journal of the American Medical Association. 2002;288(24):3137–3146. doi: 10.1001/jama.288.24.3137. [DOI] [PubMed] [Google Scholar]
- Fries JF. Aging, natural death, and the compression of morbidity. New England Journal of Medicine. 1980;303:130–135. doi: 10.1056/NEJM198007173030304. [DOI] [PubMed] [Google Scholar]
- Gao J, Raven JH, Tang S. Hospitalisation among the elderly in urban China. Health Policy. 2007;84:210–219. doi: 10.1016/j.healthpol.2007.03.007. [DOI] [PubMed] [Google Scholar]
- Gu D, Dupre ME, Liu G. Characteristics of the institutionalized and community-residing oldest-old in China. Social Science and Medicine. 2007;64:871–883. doi: 10.1016/j.socscimed.2006.10.026. [DOI] [PubMed] [Google Scholar]
- Gu D, Zeng Y. Sociodemographic effects on onset and recovery of ADL disability among Chinese oldest-old. Demographic Research. 2004;11:1–42. [Google Scholar]
- Gurenberg EM. The failure of success. Milbank memorial Fund Quarterly/Health and Society. 1977;55:3–24. [PubMed] [Google Scholar]
- Hayward MD, Warner DF. The demography of population health. In: Poston DL, Micklin M, editors. The handbook of population. New York: Springer; 2005. pp. 809–825. [Google Scholar]
- Idler EL. Discussion: Gender differences in self-rated health, in mortality, and in the relationship between the two. The Gerontologist. 2003;43:372–375. [Google Scholar]
- Jitapunkul S, Chavovan N. Healthy life expectancy of Thai elderly: Did it improve during the soap-bubble economic period? Journal of Medical Association of Thailand. 2000;83(8):861–864. [PubMed] [Google Scholar]
- Laditka S. Healthy life expectancy among older Americans in rural and urban areas; Beijing. Paper presented at REVES 2005 Conference on Population Health and Health Expectancy-Policy Implications.; 18–20 May 2005.2005. [Google Scholar]
- Lamb VL. Gender differences in correlates of disablement among the elderly in Egypt. Social Science and Medicine. 1997;45(1):127–136. doi: 10.1016/s0277-9536(96)00326-7. [DOI] [PubMed] [Google Scholar]
- Lamb VL, Siegel JS. Health demography. In: Siegel JS, Sawnson DA, editors. The methods and materials of demography. San Diego, CA: Elsevier Academic Press; 2004. pp. 341–370. [Google Scholar]
- Liu G, Zhang Z. Sociodemographic differentials of the self-rated health of the oldest-old Chinese. Population Research and Policy Review. 2004;23:117–133. [Google Scholar]
- Manton KG. Changing concepts of morbidity and mortality in the elderly population. Milbank Memorial Fund Quarterly/Health and Society. 1982;60:183–244. [PubMed] [Google Scholar]
- Manton KG, Stallard E, Corder L. Changes in morbidity and chronic disability in the U.S. elderly population: Evidence from the 1982, 1984, and 1989 National Long Term Care Surveys. Journal of gerontology: Psychology Sciences and Social Sciences. 1995;50:S194–S204. doi: 10.1093/geronb/50b.4.s194. [DOI] [PubMed] [Google Scholar]
- Myers GC, Lamb VL, Agree EM. Patterns of disability change associated with the epidemiologic transition. In: Robine J-M, Jagger C, Materhs CD, Crimmins EM, Suzman RM, editors. Determining health expectancies. West Sussex, England: John Wiley & Sons Ltd; 2003. pp. 59–74. [Google Scholar]
- National Statistics of China. Statistical yearbook of China, 2002. Beijing: China Statistics Press; 2003. [Google Scholar]
- Nolen-Hoeksema S, Larson J, Grayson C. Explaining the gender difference in depressive symptoms. Journal of Personality and Social Psychology. 1999;77:1061–1072. doi: 10.1037//0022-3514.77.5.1061. [DOI] [PubMed] [Google Scholar]
- Oksuzyan A, Juel K, Vaupel JW, Christensen K. Men: Good health and high mortality-Sex differences in health and aging. Aging Clinical and Experimental Research. 2008;20(2):91–102. doi: 10.1007/bf03324754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostir GV, Ottenbacher KJ, Markides KS. Onset of frailty in older adults and the protective role of positive affect. Psychology and Aging. 2004;19(3):402–408. doi: 10.1037/0882-7974.19.3.402. [DOI] [PubMed] [Google Scholar]
- Popham F, Mitchell R. Self-rated life expectancy and lifetime socio-economic position: cross-sectional analysis of the British household panel survey. International Journal of Epidemiology. 2007;36:58–65. doi: 10.1093/ije/dyl241. [DOI] [PubMed] [Google Scholar]
- Puts MT, Lips P, Deeg DJ. Sex differences in the risk of frailty for mortality independent of disability and chronic diseases. Journal of the American Geriatrics Society. 2005;53:40–47. doi: 10.1111/j.1532-5415.2005.53008.x. [DOI] [PubMed] [Google Scholar]
- Robine JM, Jagger C, Mathers CD, Crimmins EM, Suzman RM. Determining health expectancies. West Sussex, England: John Wiley & Sons Ltd; 2003. [Google Scholar]
- Robine JM, Michel J-P. Looking forward to a general theory on population. Journal of Gerontology: Medical Sciences. 2004;59(A):590–597. doi: 10.1093/gerona/59.6.m590. [DOI] [PubMed] [Google Scholar]
- Sagardui-Villamor J, Guallar-Castillón P, García-Ferruelo M, Banegas JR, Rodríguez-Artalejo F. Trends in disability and disability-free expectancy among elderly people Spain: 1986–1999. Journal of Gerontology: Medical Science. 2005;60A(8):1028–1034. doi: 10.1093/gerona/60.8.1028. [DOI] [PubMed] [Google Scholar]
- Saito Y, Qiao X, Jitapunkul S. Health expectancies in Asian countries. In: Robine JM, Jagger C, Mathers CD, Crimmins EM, Suzman RM, editors. Determining health expectancies. West Sussex, England: John Wiley & Sons Ltd; 2003. pp. 289–317. [Google Scholar]
- Schenker N, Raghunathan TE. Combining information from multiple surveys to enhance estimation of measures of health. Statistics in Medicine. 2007;26:1802–1811. doi: 10.1002/sim.2801. [DOI] [PubMed] [Google Scholar]
- Schoenil RF, Liang J, Bennett J, Sugisawa H, Fukaya T, Kobayashi E. Trends in old-age functioning and disability in Japan, 1993–2002. Population Studies. 2006;60(1):39–53. doi: 10.1080/00324720500462280. [DOI] [PubMed] [Google Scholar]
- Stuck AE, Egger M, Hammer A, Minder CE, Beck JC. Home visits to prevent nursing home admission and functional decline in elderly people: Systematic review and meta-regression analysis. Journal of the American Medical Association. 2002;287(4):1022–1028. doi: 10.1001/jama.287.8.1022. [DOI] [PubMed] [Google Scholar]
- Szaflarski M, Cubbins LA. Self-reported health in Poland and the United States: A comparative analysis of demographic, family and socioeconomic influences. Health. 2004;8(1):5–31. doi: 10.1177/1363459304038793. [DOI] [PubMed] [Google Scholar]
- Tobiasz-Adamczyk B, Brzyski P. Factors determining changes in self-rated health in the Polish community-dwelling elderly. Central European Journal of Public Health. 2005;13(3):117–124. [PubMed] [Google Scholar]
- Tu E, J-C, Chen K. Changes in active life expectancy in Taiwan: Compression or expansion? Social Science & Medicine. 1994;39(12):1657–1665. doi: 10.1016/0277-9536(94)90080-9. [DOI] [PubMed] [Google Scholar]
- UK National Statistics. [Access on December 22, 2008];Health expectancy: living longer, more years in poor health. 2006 http://www.statistics.gov.uk/cci/nugget.asp?id=918).
- United Nations Population Division. World population prospects: The 2006 revision. New York: United Nations; 2007. [Accessed on March 18, 2007]. http://esa.un.org/unpp. [Google Scholar]
- Verbrugge LM, Jette A. The disablement process. Social Science & Medicine. 1994;39:1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- Waidmann T, Liu K. Disability trends among the elderly and implications for the future. Journal of Gerontology: Psychology and Social Sciences. 2000;56(B):S298–S307. doi: 10.1093/geronb/55.5.s298. [DOI] [PubMed] [Google Scholar]
- Walston J, Fried LP. Frailty and the older man. The Medical Clinics of North America. 1999;3:1173–1194. doi: 10.1016/s0025-7125(05)70157-7. [DOI] [PubMed] [Google Scholar]
- Yang G, Kong L, Zhao W, Wan X, Zhai Y, Chen LC, Koplan JP. Emergence of chronic non-communicable diseases in China. Lancet. 2008;372:1697–1705. doi: 10.1016/S0140-6736(08)61366-5. [DOI] [PubMed] [Google Scholar]
- Yates LB, Karasik D, Beck TJ, Cupples LA, Kiel DP. Hip Structural geometry in old and old-old age: Similarities and differences between men and women. Bone. 2007;41(4):722–732. doi: 10.1016/j.bone.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yip W, Hsiao WC. The Chinese health system at a crossroads: A new infusion of government funds has sparked debate in China about how best to transform money into effective services. Health Affairs. 2008;27(2):460–468. doi: 10.1377/hlthaff.27.2.460. [DOI] [PubMed] [Google Scholar]
- Yu LC, Zhang AY, Draper P, Kassab C, Miles T. Cultural correlates of self perceived health status among Chinese elderly. Journal of Cross-Cultural Gerontology. 1997;12:73–89. doi: 10.1023/a:1006545521022. [DOI] [PubMed] [Google Scholar]
- Yu Z. Heterogeneity and dynamics in China's emerging urban housing market: Two sides of a success story from the late 1990s. Habitat International. 2006;30(2):277–304. [Google Scholar]
- Zack MM, Moriaarty DG, Ford ES, Mokdad AH. Worsening trends in adult health-rated quality of life and self-rated health- United States, 1993–2001. Public Health Report. 2004;119:493–505. doi: 10.1016/j.phr.2004.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng Y, Poston DL, Vlosky DA, Gu D. Healthy longevity in China: Demographic, socioeconomic, and psychological dimensions. Dordrecht, The Netherlands: Springer Publisher; 2008. [Google Scholar]
- Zhu H, Xie Y. Socioeconomic differentials in mortality among the oldest-old in China. Research on Aging. 2007;29(2):125–143. [Google Scholar]
- Zimmer Z, Martin LG, Chang MC. Changes in functional limitations and survival among the elderly in Taiwan: 1993, 1996, and 1999. Population Studies. 2002;56:265–276. doi: 10.1080/00324720215931. [DOI] [PubMed] [Google Scholar]