Abstract
Objective
National audit of informed choice in antenatal screening for thalassaemia.
Design
Audit from the UK Confidential Enquiry into Counselling for Genetic Disorders.
Setting
Thalassaemia module of the UK Confidential Enquiry into Counselling for Genetic Disorders.
Subjects
138 of 156 couples who had had a pregnancy affected by a major β thalassaemia from 1990 to 1994.
Main outcome measures
How and when genetic risk was identified for each couple, and whether and when prenatal diagnosis was offered.
Results
Risk was detected by screening before or during the first pregnancy in 49% (68/138) of couples and by diagnosis of an affected child in 28% (38/138) of couples. Prenatal diagnosis was offered in 69% (274/400) of pregnancies, ranging from 94% (122/130) for British Cypriots to 54% (80/149) for British Pakistanis and from 90% in the south east of England to 39% in the West Midlands. Uptake of prenatal diagnosis was 80% (216/274), ranging from 98% (117/120) among British Cypriots in either the first or second trimester to 73% (35/48) among British Pakistanis in the first trimester and 39% (11/28) in the second trimester. A demonstrable service failure occurred in 28% (110/400) of pregnancies, including 110 of 126 where prenatal diagnosis was not offered and 48 of 93 that ended with an affected liveborn infant.
Conclusion
Although antenatal screening and counselling for haemoglobin disorders are standard practices in the United Kingdom, they are delivered inadequately and inequitably. An explicit national policy is needed, aiming to make prenatal diagnosis in the first trimester available to all couples and including ongoing national audit.
Introduction
The UK National Confidential Enquiry into Counselling for Genetic Disorders aims to evaluate the quality of genetic counselling provided within general health services.1,2 Thalassaemia was selected as a pilot to audit population screening for recessively inherited disorders3 because antenatal screening for haemoglobin disorders is standard practice in the United Kingdom4 and cases could be identified through national registers.5,6 The objective of carrier screening is to permit couples who are at risk an informed choice among available options, including prenatal diagnosis in every pregnancy.7 The inquiry therefore focused on evaluating parents' access to information and choice.
When performed as recommended8 the “haemoglobinopathy screen” is an almost ideal screening test. It combines measurement of the red cell indices (to detect microcytosis typical of thalassaemias) and electrophoresis for abnormal haemoglobins. Sensitivity is 100% for common abnormal haemoglobins and over 96% for thalassaemias, and specificity is 100% for both. When a clear policy and multidisciplinary cooperation are in place it is possible to identify practically all couples at risk in their first pregnancy, but with present antenatal booking practice this is rarely achieved before the second trimester.9 Prenatal diagnosis in the first trimester, which has been feasible in all cases since 1990,10 should be offered in all subsequent pregnancies provided that the woman presents in time.4
With an appropriate service, utilisation of prenatal diagnosis (percentage of pregnancies at risk in which a prenatal diagnosis is actually performed) should approximate uptake (percentage of couples requesting prenatal diagnosis when it is offered). Although uptake of prenatal diagnosis for thalassaemia is over 80% in south east England,11 national audits conducted in 1985 and 1997 showed 50% utilisation and wide variations by region and ethnic group.12,5 In addition, a pilot confidential inquiry indicated that 60% of couples with a thalassaemic child born between 1980 and 1990 had not been informed of their risk during pregnancy.13 The Confidential Enquiry into Counselling for Genetic Disorders therefore undertook a formal study of the proportion of couples at risk who received timely risk detection and counselling during pregnancy.
The inquiry requested permission to review the clinical records of couples who had had a pregnancy affected by a major beta thalassaemia in the five year period from 1990 to 1994, identified through national registers.5,6 These couples provide a representative sample of the population at risk for haemoglobin disorders, as follows. Nationally every year there are at least 75 000 infants born to women in ethnic groups at risk of haemoglobin disorders (11% of the total)14,15: an essentially random 7120 of these women carry a haemoglobin disorder as do about 870 of their partners. A random 25% of these pregnancies at risk (about 218 a year) are affected and end either in an affected liveborn infant or in a termination of pregnancyafter prenatal diagnosis. About 20% of these have a major thalassaemia, and these can be almost completely ascertained through national registers. The method of case finding leads to overrepresentation of affected pregnancies among study couples (50% instead of 25%), but couples are unselected in terms of antenatal care provided, which is the subject of inquiry. The service these couples receive is therefore representative of that provided nationally.
Methods
The thalassaemia module
The thalassaemia module of the UK Confidential Enquiry into Counselling for Genetic Disorders was initiated in 1997. Cases for the module were found through the UK register of prenatal diagnosis for haemoglobin disorders and the UK thalassaemia (patient) register, which are both over 95% complete.5,6 Because of the lag time in diagnosing and registering patients the patient register was then up to date to 1995, so the inquiry focused on pregnancies affected by a major β thalassaemia in the five years from 1990 to 1994. The team identified 172 affected pregnancies in 156 women. A wide range of records was made available, but the formal protocol required review of obstetric notes. In 34 cases the responsible obstetrician could not be identified, did not respond, or could not locate the notes, so the inquiry reported on 137 pregnancies in 124 women (80% of those identified).3
Audit
To audit the service provided to couples we examined all available records and obtained the full obstetric history of 138 of the 156 women identified (86%). Multiple information sources were used for most cases. Primary sources were: obstetric notes (91 women), notes from specialist prenatal diagnosis centres (33), a national register for prenatal diagnosis (10), general practitioners' notes (3), and correspondence (1). Information on whether and how risk was recognised was available for all cases through pathology reports, notes about a previous affected child or previous recognition of risk, records of couples' choices, and correspondence. Records of information and counselling varied from none to detailed correspondence among general practitioners, haematologists, obstetricians, and counsellors.
For each couple we extracted data onethnic group, region of residence, and how and when risk was detected. For each viable pregnancy with antenatal care in the United Kingdom we extracted data on offer and uptake of prenatal diagnosis and outcome.
Results
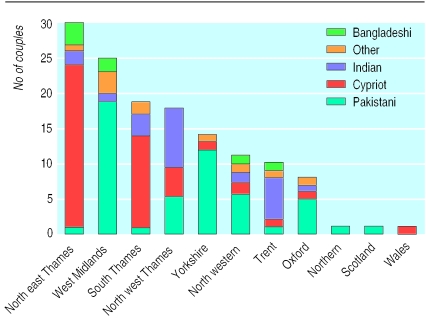
The 138 women had had 485 pregnancies. Eighty five pregnancies were ineligible (38 miscarriages, 12 social abortions, 3 ectopics, 2 hydatidiform moles, 6 with another partner, 10 live births abroad, and 14 before 1980 when prenatal diagnosis became established), leaving 400 study pregnancies. Figure 1 shows the regional and ethnic distribution of the couples.
Figure 1.
Distribution and ethnic group of 138 study couples by 1991 regional health authority or country. Other=Italian or other Mediterranean, Chinese or other South East Asian, African-Caribbean, and Middle Eastern
Risk recognition and offer of prenatal diagnosis
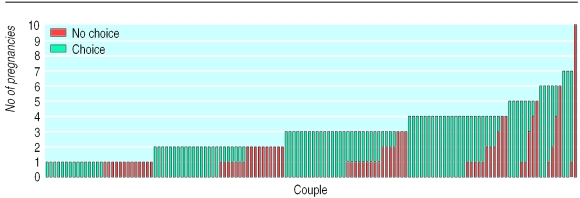
Events in the first pregnancy are the best indicator of screening practice as risk should normally be recognised at this stage. Table 1 and figure 2 show that only 49% of couples were informed and offered prenatal diagnosis in their first pregnancy. By the third pregnancy the proportion had risen to over 80%, but the main reason for the increase was that 38 couples (28% of those at risk) were identified through the diagnosis of an affected child. Risk was recognised in 43% of first pregnancies occurring before 1990 (27 of 63) and in 55% since 1990 (41 of 74). Figure 2 shows that most couples whose risk was recognised in the first pregnancy had an informed choice in every pregnancy, whereas many of those “missed” in the first pregnancy were missed again, indicating systematic differences in service provision.
Table 1.
At risk pregnancies, risk recognition, and ethnic group. Values are numbers (percentages) of couples
| Ethnic group | First pregnancy
|
All pregnancies
|
|||
|---|---|---|---|---|---|
| Total No | No (%) offered prenatal diagnosis | Total No | No (%) offered prenatal diagnosis | ||
| Cypriot* | 42 | 34 (81) | 130 | 119 (92) | |
| Indian | 26 | 13 (50) | 73 | 46 (63) | |
| Other† | 10 | 4 (40) | 28 | 17 (61) | |
| Pakistani* | 52 | 15 (29) | 149 | 76 (51) | |
| Bangladeshi | 8 | 2 (25) | 20 | 7 (35) | |
| Total | 138 | 68 (49) | 400 | 268 (67) | |
Difference between proportion of Cypriot and Pakistani couples whose risk was detected in first pregnancy is highly significant, χ2=62.9, P<0.0001).
Italian or other Mediterranean, Chinese or other South East Asian, African-Caribbean, Middle Eastern.
Figure 2.
Availability of information and choice to 138 couples at risk of a thalassaemic pregnancy, from national inquiry into genetic counselling, ranked in order of total number of pregnancies. Each column represents one woman, and shows all viable pregnancies at risk since 1980 with antenatal care in the United Kingdom
Overall, risk was recognised before 24 weeks' gestation in 271 of 400 pregnancies. There was evidence of service failure in 100 of the remaining 129 pregnancies (table 2).
Table 2.
Reasons for failure to offer prenatal diagnosis in 126 pregnancies
| Reason | No (%) of couples | Notes |
|---|---|---|
| Unavoidable | 10 (8) | 3 atypical indices, 3 partners unavailable, 2 late presentations of pregnancy, 2 wrong dates |
| Woman not screened | 35 (28) | No Hb A2 estimation or electrophoresis |
| Partner not tested | 29 (23) | No indices, Hb A2 estimation, or electrophoresis for partner |
| Laboratory error | 15 (12) | 1 inappropriate test, 3 false low Hb A2, 3 borderline indices, 3 clerical or communication errors, 3 false risk assessments, 2 “knock on” errors* |
| Undue delay in screening | 13 (10) | Late detection of risk |
| Failed communication | 5 (4) | 4 general practitioner reported risk when referring, no action 1 carrier father given “non-carrier” card |
| Manifest risk not recognised | 5 (4) | Previous history (existing affected child or known risk) noted, no action |
| Not counselled | 4 (3) | Carrier state detected in both partners, no action |
| Risk “lost” | 4 (3) | No record in obstetric notes or laboratory of a risk already detected in a previous pregnancy |
| Unknown | 6 (5) | |
| Total | 126 (100) |
Failure to recognise risk or retest during a pregnancy because of false negative result in earlier pregnancy.
Risk was recognised later than 24 weeks' gestation in 23 pregnancies. This was not owing to late presentation as 10 available referral letters from doctors showed that six women presented in the first trimester and four in the second. Two had a late prenatal diagnosis, one affected pregnancy was terminated at 27 weeks, and 10 liveborn infants were affected.
Ethnic variations—The proportion of pregnancies where prenatal diagnosis was offered ranged from 81% of first pregnancies and 92% of all pregnancies in British Cypriots, to 29% of first pregnancies and 51% of all pregnancies in British Pakistanis.
Prenatal diagnosis in the first trimester, feasible in all cases since 1990, was offered to 87% of British Cypriots and 50% of British Pakistanis with eligible pregnancies and to 62% (8 of 13) of British Cypriot couples and 9% (3 of 32) of British Pakistani couples with eligible first pregnancies.
Regional variations—In south east England prenatal diagnosis was offered in 79% (25 of 30) of first pregnancies and 92% (83 of 90) of all pregnancies. In the West Midlands and Anglia and Oxford prenatal diagnosis was offered in 20% of first pregnancies (5 of 25 and 1 of 8 respectively) and 39% of all pregnancies (23 of 59 and 9 of 23 respectively).
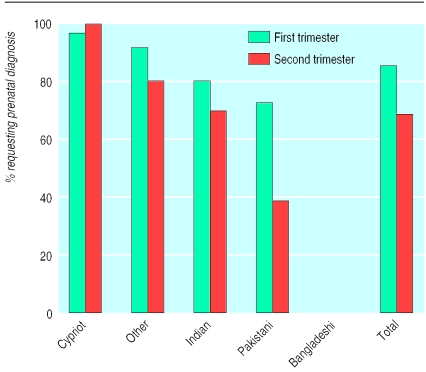
Uptake of prenatal diagnosis when offered was 80% (214 of 266) but varied with ethnic origin and gestation (fig 3). For example, uptake by British Pakistanis was 73% (35 of 48) in the first trimester, with 11 of 12 affected pregnancies being terminated, and 39% (11 of 28) in the second trimester, with four of seven affected pregnancies being terminated.
Figure 3.
Uptake of prenatal diagnosis by ethnic group and gestation at counselling. Fisher's exact test for British Pakistanis showed a significant difference (P=0.004) in proportion requesting prenatal diagnosis in first versus second trimester
Couples' uptake of prenatal diagnosis was not always consistent. Nine of 10 couples who declined and had an affected child requested prenatal diagnosis in subsequent pregnancies. Seven who declined and had an unaffected child declined again. Six couples who had had a prenatal diagnosis, later declined: one couple after an intrauterine death associated with the procedure, three after a mid-trimester abortion, one after a first trimester abortion, and one after continuing a known affected pregnancy and having a mildly affected child.
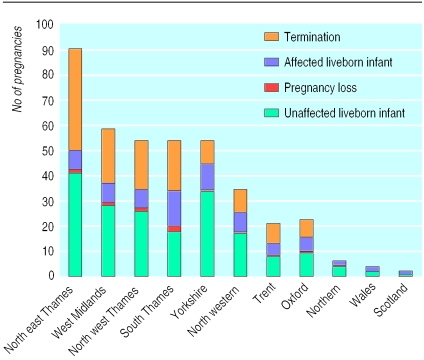
Affected liveborn infants—Overall, 93 of the 201 affected pregnancies ended in a liveborn infant (fig 4). This could not be foreseen in six cases (atypical carrier, partner abroad) and followed parental choice in 37 (33 declined prenatal diagnosis, 4 continued an affected pregnancy). Service failure occurred in 48 (52%) cases (risk not detected, detected after 24 weeks' gestation, lost, or couple not counselled). Circumstances were unclear in one case. More than two thirds of affected liveborn infants were to British Pakistani or Bangladeshi parents, and more than two thirds occurred in the midlands and the north.
Figure 4.
Outcome of 403 conceptions at risk (400 pregnancies) by region. Regional differences are highly significant (χ2 test on 8 df=96.87, P<0.001)
Discussion
Screening and counselling for genetic disorders
In the United Kingdom haemoglobin disorders are two thirds as common as cystic fibrosis,14,15 and antenatal carrier screening is standard practice.4 Eighty per cent of couples at risk of a serious haemoglobin disorder are at risk of a sickle cell disorder. Detailed study of the screening process is feasible for the 20% subset at risk of thalassaemia, because national registers exist. The UK Confidential Enquiry into Counselling for Genetic Disorders therefore conducted a national audit of informed choice for risk of thalassaemia from 1990 to 1994. The offer of prenatal diagnosis, which is a precondition for choice, was the principal indicator. Only half the couples at risk received a service that allowed them an informed choice in every pregnancy, ranging from 86% of British Cypriots to 33% of British Pakistanis and from 83% of residents in the south east to 16% of of those in the West Midlands. Almost one third of couples (mostly British Pakistanis) first discovered their risk through the diagnosis of an affected child, and over half of all affected liveborn infants were associated with a service failure. There was little change in service quality between 1980 and 1995, and there is limited evidence of subsequent change.
Role of inadequate or absent screening policies
The wide range of problems identified by the inquiry underlines the multidisciplinary nature of antenatal genetic screening and shows the need for explicit policies, good communication, and a clear line of responsibility. Clustering of problems in some regions identifies inadequate local screening policies as the principal reason for uneven service delivery. Many districts, predominantly in south east England, developed an explicit policy in the early 1980s when prenatal diagnosis became available, and they provide a consistent high quality service. Recruitment of other districts has been slow despite the increasing numbers and changing regional distribution of ethnic groups at risk.6,14,15 In a 1999 postal survey of clinical directors and heads of midwifery, 104 units (65%) were reported to have neither local nor regional written policies for screening for haemoglobin disorders (unpublished data). The problems identified must also apply for sickle cell disorders because the same screening and counselling approach applies for all haemoglobin disorders.5
Importance of early detection of risk, and counselling
The choices of British Pakistanis highlight the importance of the timingof offering prenatal diagnosis. In this group, uptake of prenatal diagnosis in the first trimester is over 70% and over 90% of affected pregnancies are terminated, whereas uptake of diagnosis in the second trimester is 40% and half of the affected pregnancies are terminated. The same preference applies for couples of any ethnic origin but is often masked by higher acceptance of late abortion. Informed choice clearly requires the offer of diagnosis in the first trimester whenever possible, which will require increased involvement of primary care teams.16 With truly informed choice there would be 75%-80% national utilisation of prenatal diagnosis for thalassaemia.
Role of ethnic stereotyping
Equity in medical services requires facilities for crossing social, educational, language, and cultural barriers. British Cypriots are highly aware of thalassaemia and have high expectations; many “beat the system” by asking their doctor for prepregnancy screening and so obtain prenatal diagnosis in the first trimester of their first pregnancy. By contrast, most British Pakistanis depend on health workers for information and screening and few know that prenatal diagnosis in the first trimester is available with religious agreement in Pakistan and Iran.17 We show here that British Pakistanis' low utilisation of prenatal diagnosis reflects inadequate risk detection, lack of awareness, poor communication, and a strong preference for early testing. It is, however, often taken to support a view (documented in several notes) that Muslims “do not want” prenatal diagnosis. This leads to half hearted screening and self confirming results, so the population that needs the best service obtains the worst.
What is already known on this topic
The aim of antenatal screening for haemoglobin disorders is to allow couples at risk an informed choice, including the option of prenatal diagnosis, in every pregnancy
The observed utilisation of prenatal diagnosis is lower than predicted, and the extent to which this reflects couples' informed choices versus problems in service delivery was unclear
What this paper adds
The UK confidential inquiry into antenatal screening for thalassaemia has shown that: only half of all couples at risk obtain full access to information and choice; over half of all affected liveborn infants are associated with a demonstrable service failure; the service is not provided to many British Pakistanis and Bangladeshis because of ethnic stereoptyping; and prenatal diagnosis is highly acceptable to all ethnic groups at risk, especially when offered in the first trimester
A national policy on screening for haemoglobin disorders is needed, as the main cause of service failures is inadequate policy development at the district level
The eight British Bangladeshi couples studied encountered most problems. There was no evidence of any counselling for four couples, no couple was counselled in their mother tongue, and two couples at risk of haemoglobin E/β thalassaemia were not offered prenatal diagnosis because their risk was incorrectly assessed.3 Although two haemoglobinopathy counsellors with appropriate language skills are in post in the United Kingdom, they are geographically inaccessible to most British Bangladeshis.18 A distance interpreting or counselling service could help to overcome such problems.19
Conclusion
The UK Confidential Enquiry into Counselling for Genetic Disorders shows the need for a national policy on screening for haemoglobin disorders, aiming to offer prenatal diagnosis in the first trimester in all pregnancies at risk, and including ongoing audit. To maintain the audit initiated by the inquiry the UK thalassaemia register now collects information about the circumstances of each new affected birth.
Acknowledgments
We thank Paula Williamson and Mark Griffin for statistical advice.
Footnotes
Funding: The UK Confidential Enquiry into Counselling for Genetic Disorders was sponsored by the Royal College of Physicians and supported by the UK Department of Health. BM is supported by the Wellcome Trust as a prinical research fellow.
Competing interests: None declared.
References
- 1.Harris R. How well do we manage families with genetic problems? A national confidential enquiry into counselling for genetic disorders should tell us. BMJ. 1991;303:1412–1413. doi: 10.1136/bmj.303.6815.1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harris R, Lane B, Harris HJ, Williamson P, Dodge J, Modell B, et al. National confidential enquiry into counselling for genetic disorders by non-geneticists: general recommendations and specific standards for improving care. Brit J Obst Gynaecol. 1999;106:658–663. doi: 10.1111/j.1471-0528.1999.tb08364.x. [DOI] [PubMed] [Google Scholar]
- 3.National confidential enquiry into counselling for genetic disorders. Homozygous beta thalassaemias, Great Britain 1990-94. Report to the Department of Health from the steering committee. 1998. [Google Scholar]
- 4.Sickle cell, thalassaemia and other haemoglobinopathies. Report of a working party of the Standing Medical Advisory Committee. London: HMSO; 1994. [Google Scholar]
- 5.Modell B, Petrou M, Layton M, Varnavides L, Slater C, Ward RHT, et al. Audit of prenatal diagnosis for haemoglobin disorders in the United Kingdom: the first 20 years. BMJ. 1997;315:779–784. doi: 10.1136/bmj.315.7111.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Modell B, Khan M, Darlison M. Survival in beta thalassaemia major in the United Kingdom: data from the UK thalassaemia register. Lancet 2000 (in press). [DOI] [PubMed]
- 7.Nuffield Council on Bioethics. Genetic screening, ethical issues. London: Nuffield Council on Bioethics.
- 8.Working party of the General Haematology Task Force of the British Committee for Standards in Haematology. Guideline. The laboratory diagnosis of haemoglobinopathies. Brit J Haematol. 1998;101:783–792. [Google Scholar]
- 9.Neuenschwander H, Modell B. The process of antenatal sickle cell screening at a north London hospital. BMJ. 1997;315:784–785. doi: 10.1136/bmj.315.7111.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Old JM, Varawalla NY, Weatherall DJ. Rapid detection and prenatal diagnosis of beta-thalassaemia: studies in Indian and Cypriot populations in the UK. Lancet. 1990;336:834–837. doi: 10.1016/0140-6736(90)92338-i. [DOI] [PubMed] [Google Scholar]
- 11.Modell B, Ward RHT, Fairweather DVI. Effect of introducing antenatal diagnosis on the reproductive behaviour of families at risk for thalassaemia major. BMJ. 1980;2:737–740. doi: 10.1136/bmj.280.6228.1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Modell B, Petrou M, Ward RHT, Fairweather DVI, Rodeck C, Varnavides LA, et al. Effect of fetal diagnostic testing on the birth-rate of thalassaemia in Britain. Lancet. 1985;2:1383–1386. doi: 10.1016/s0140-6736(84)92070-1. [DOI] [PubMed] [Google Scholar]
- 13.Modell B. EC concerted action on developing patient registers as a tool for improving service delivery for haemoglobin disorders. In: Fracchia GN, Theophilatou M, editors. Health services research. Amsterdam: IOS Press; 1993. [Google Scholar]
- 14.Health Education Authority. Sickle cell and thalassaemia: achieving health gain. Guidance for commissioners and providers. London: HEA; 1998. [Google Scholar]
- 15.Hickman M, Modell B, Greengross P, Chapman C, Layton M, Gill M, et al. Mapping the prevalence of sickle cell and β thalassaemia in England: recommended rates for local service planning. Brit J Haematol. 1999;104:860–867. doi: 10.1046/j.1365-2141.1999.01275.x. [DOI] [PubMed] [Google Scholar]
- 16.Modell M, Wonke B, Anionwu E, Khan M, See Tai S, Lloyd M, et al. A multidisciplinary approach for improving services in primary care: the example of screening for haemoglobin disorders. BMJ. 1998;7161:788–791. doi: 10.1136/bmj.317.7161.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anionwu EN. Ethnic origin of sickle and thalassaemia counsellors; does it matter? In: Kelleher D, Hillier D, editors. Research in cultural differences in health. Routledge: London; 1996. [Google Scholar]
- 18.Petrou M, Modell B. Prenatal screening for haemoglobin disorders. Prenat Diag. 1995;15:1275–1295. doi: 10.1002/pd.1970151308. [DOI] [PubMed] [Google Scholar]
- 19.Jones D, Gill P. Breaking down language barriers: the provision of accessible interpreting services for all. BMJ. 1998;316:1476. doi: 10.1136/bmj.316.7143.1476. [DOI] [PMC free article] [PubMed] [Google Scholar]