Abstract
Multiple different types of anterior mediastinal masses may be encountered on computed tomography (CT) imaging, and many of these lesions are neoplastic in etiology. These include masses arising from the thymus, thyroid and parathyroid glands, as well as lymph nodes, pericardium, and vessels and nerves. Often, the CT attenuation of the mass can be helpful in narrowing down the differential diagnosis, and attenuation values suggesting fat, water or calcium may suggest certain diagnoses; significant enhancement of the mass with intravenous contrast may also be a helpful feature. Lesions with fatty attenuation include teratomas, thymolipomas and Morgagni hernias. Lesions that may manifest the attenuation of water include pericardial and thymic cysts, abscesses, and lymphangiomas, as well as neurogenic and germ cell tumors. Multiple types of lesions may contain calcium, including thyroid goiters and cancers, thymomas, thymic carcinomas and carcinoids, treated lymphoma, germ cell tumors, parathyroid adenomas, and lymph nodes involved with silicosis, sarcoid, tuberculosis, fungal diseases and pneumocystis. Contrast enhancement may be seen in lesions of vascular origin and in vascular neoplasms, such as parathyroid adenomas and Castleman's disease. In addition to CT attenuation values, the exact location and morphology of the mass in question, in conjunction with clinical features such as patient age, gender, signs, symptoms, and laboratory values, can usually lead to a short list of possible etiologies, thereby directing appropriate additional diagnostic procedures or therapeutic approaches.
Keywords: Thymic neoplasms, germ cell tumors, mediastinal neoplasms
Introduction
Anterior mediastinal masses are not uncommonly seen on imaging studies; many of these represent benign or malignant neoplasms. Often, the CT attenuation of the mass can be helpful in narrowing down the differential diagnosis, and attenuation values suggesting fat, water or calcium may suggest certain diagnoses; significant enhancement of the mass with intravenous contrast may also be a helpful feature. In addition, the exact location and morphology of the mass in question, in conjunction with clinical features such as patient age, gender, signs, symptoms, and laboratory values, can usually lead to a short list of possible etiologies, thereby directing appropriate additional imaging or other diagnostic procedures or therapeutic approaches.
Fat attenuation masses
There are only three major entities in the category of fat attenuation anterior mediastinal masses: teratoma, thymolipoma and Morgagni hernia.
Teratoma
Various different types of germ cell tumors may occur in the anterior mediastinum; these masses arise from primitive germ cell elements, and many are of mixed cell type. Mediastinal germ cell tumors are generally found in adolescents and young adults. Approximately 80% of such lesions are benign, and most of the benign lesions represent teratomas. Malignant germ cell tumors are seen much more commonly in males compared to females.
Teratomas are usually predominately cystic in nature, although they frequently have a soft tissue component, often showing a thin outer capsule. Fat and calcium are also common elements (Fig. 1). Fat/fluid levels are said to be a specific finding for teratomas; however they are rarely seen. Entirely solid teratomas are occasionally encountered; these lesions are usually malignant. Benign teratomas are usually encapsulated and well defined on computed tomography (CT) scan. However, they may hemorrhage, leading to a complicated CT appearance. Malignant teratomas are most often large, multinodular in appearance and poorly defined at CT. Both benign and malignant teratomas may grow and may rupture or fistulize with adjacent structures in the mediastinum or with lung, pleura or pericardium[1].
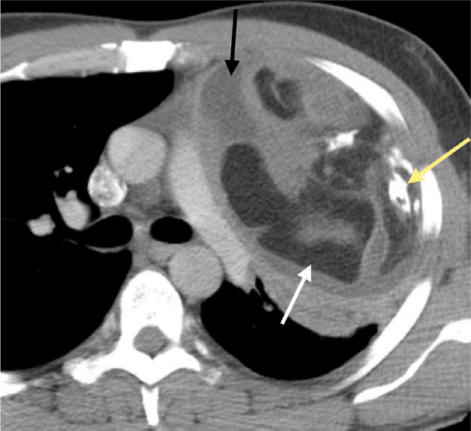
Figure 1.
Malignant teratoma showing areas of fat (white arrow), calcium (yellow arrow) and fluid attenuation (black arrow).
Thymolipoma
Thymolipomas are benign lesions that arise from the thymus gland and may grow slowly over time. Despite their usually large size, they are generally asymptomatic; occasionally, however, they may compress or displace adjacent structures, leading to symptoms. On CT scanning, they may clearly lie within the thymus. Frequently, however, they are pedunculated, filling a large portion of one hemithorax; in these cases, it may be difficult to discern the thymic origin of the mass. These tumors are usually predominately fatty in attenuation, with a variable component of soft tissue elements (Fig. 2)[2]. Surgical excision is curative.
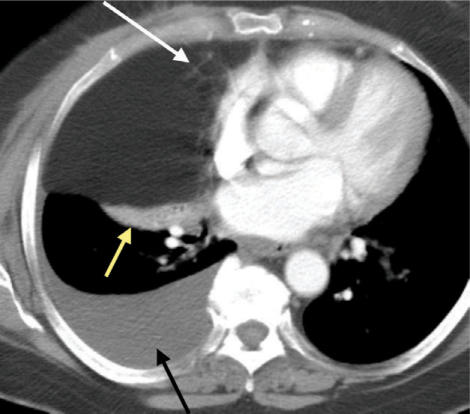
Figure 2.
Thymolipoma composed mostly of fat, with minor, strandy soft tissue elements (white arrow). Yellow arrow denotes atelectasis and black arrow indicates a pleural effusion related to metastatic breast cancer.
Morgagni hernia
The major entity in the differential diagnosis of a thymolipoma is a Morgagni hernia. These hernias contain omental fat that has herniated from the abdomen into the thorax via the foramen of Morgagni; the fat lies in a retrosternal or parasternal location, usually on the right side[3]. Occasionally Morgagni hernias also contain small or large bowel or portions of the liver. On CT, a Morgagni hernia appears as a fat containing mass in the lower, anterior mediastinum, usually large in size. The key to the diagnosis on CT is the detection of linear-appearing soft tissue opacities in the fat which represent omental vessels; with close scrutiny, the vessels can be traced down into the upper abdomen.
Water attenuation masses
There are several entities in the category of water attenuation anterior mediastinal masses, including cysts arising from thymus or pericardium, foregut duplication cysts, neurogenic tumors, abscesses and lymphangiomas (particularly in children); many of these lesions may be neoplastic in nature[4].
Thymic cyst
Thymic cysts may be congenital in nature, arising from remnants of the thymophargyngeal duct. Such lesions may occur anywhere along the course of thymic descent from the neck during development; however, they often occur in the anterior mediastinum. Acquired thymic cysts are much more common than congenital cysts, and may arise in association with neoplasms such as thymomas, lymphomas or germ cell tumors. Although teratomas are the most common type of germ cell tumor to develop cystic areas, other cell types may contain cysts (Figs. 1 and 3). Thymic cysts may also be seen in the anterior mediastinum after radiation therapy for Hodgkin's disease, and occasionally multilocular thymic cysts are seen in patients with AIDS, particularly in children[5]. Sometimes acquired cysts are unassociated with neoplasms, likely related to an inflammatory process (Fig. 4)[6]. Such lesions may contain cellular debris, cholesterol crystals and/or hemorrhage, leading to a complicated appearance at CT and magnetic resonance imaging (MRI). The cystic material may leak into the surrounding mediastinal tissues, inciting an inflammatory response.
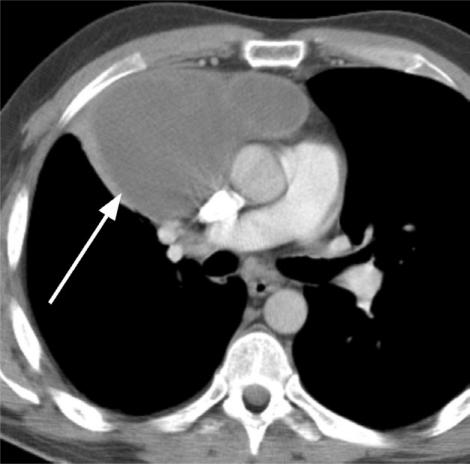
Figure 3.
Mixed, malignant germ cell tumor with necrotic/cystic components (arrow) after treatment with chemotherapy.
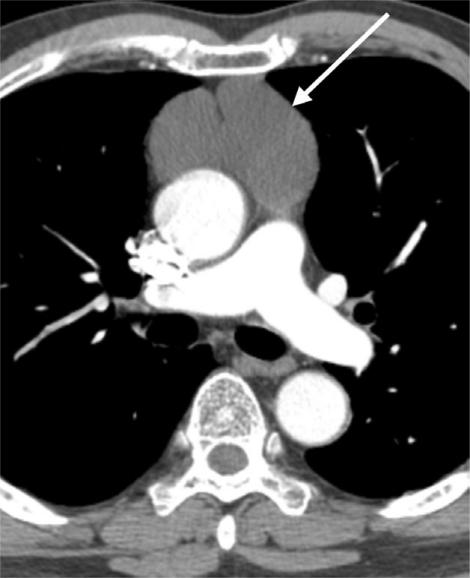
Figure 4.
Cystic, septated benign thymic cyst (arrow).
Pericardial cyst
Pericardial cysts may occasionally mimic thymic cysts. However, the former are usually simple in appearance at CT, unlike the latter which often have associated soft tissue. Moreover, pericardial cysts are generally located more inferiorly in the anterior mediastinum compared to thymic cysts: approximately 90% are tucked down between the heart and the hemidiaphragm, usually on the right side[7]. Pericardial cysts may change in shape on follow-up imaging studies. These lesions are benign, and they are thought to be congenital in nature.
Foregut duplication cysts
Foregut duplication cysts are uncommon congenital abnormalities of enteric origin[8]. Most duplication cysts occur in the middle or posterior mediastinum; however, bronchogenic cysts may occasionally be seen in the anterior mediastinum. These lesions may appear as simple, water attenuation lesions, or they may be complicated, showing soft tissue attenuation and heterogeneity due to mucus, proteinaceous or cellular debris and/or hemorrhage[9].
Neurogenic tumor
Neurogenic tumors may occasionally occur in or adjacent to the anterior mediastinum. Lipid-like material in the tumors leads to their low attenuation appearance, mimicking a fluid-containing lesion. Such lesions are often easily diagnosed if they are elongated in shape and occur in the characteristic location of the phrenic nerve; the diagnosis is clinched if there are bilateral lesions in a patient with known neurofibromatosis (Fig. 5).
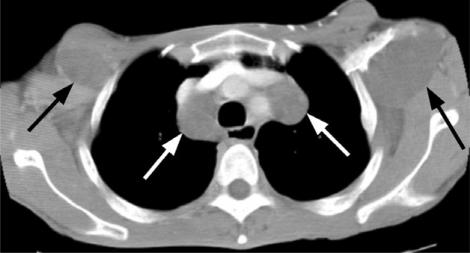
Figure 5.
Bilateral, low attenuation mediastinal (white arrows) and axillary (black arrows) neurofibromas in a patient with neurofibromatosis.
Calcified masses
There are a multitude of entities in the category of calcified anterior mediastinal masses, including lesions arising from the thyroid, thymus or parathyroid glands, germ cell tumors, treated lymphoma, and lymph nodes involved with diseases such as silicosis, sarcoidosis, tuberculosis, histoplasmosis or pneumocystis.
Thyroid masses
Both benign and malignant thyroid masses, including goiters, thyroiditis, and thyroid neoplasms, may calcify and contain areas of heterogeneity due to hemorrhage, fibrosis or cysts (Figs. 6 and 7). Goiters tend to be well marginated. A lesion with ill-defined margins and nearby lymph node enlargement suggests the diagnosis of thyroid cancer; invasion of an adjacent structure, such as the trachea, is diagnostic for a neoplasm. The finding of multiple concomitant small lung nodules is suspicious for metastatic disease from thyroid cancer. Occasionally goiters and thyroid cancers coexist in the same gland: carcinoma may be found in up to 10% of resected goiters[10,11]. The key to diagnosing an anterior mediastinal mass as a thyroid lesion is to follow the lesion up into the neck and look for evidence of thyroid lobe involvement (Figs. 6 and 7). Most commonly goiters are bilateral and cancers are unilateral, but this rule is not absolute.
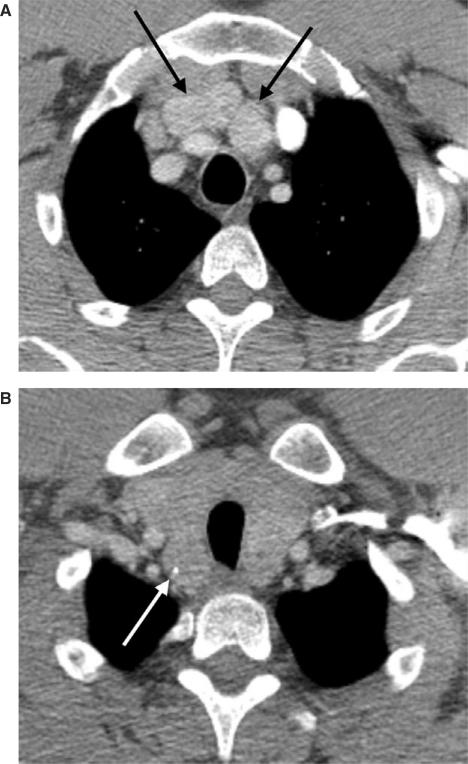
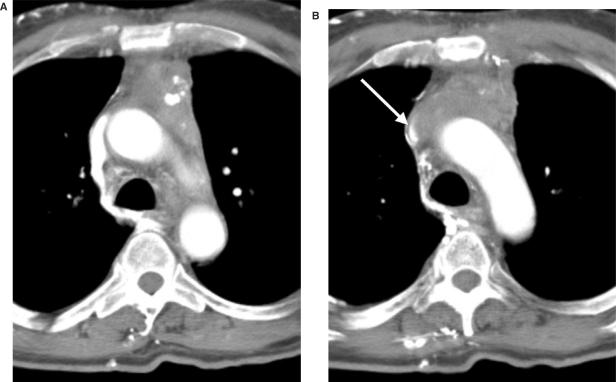
Figure 6.
Lobulated anterior mediastinal mass (black arrows) (A) is arising from the thyroid more superiorly (B). Thyroid enlargement is due to thyroiditis; white arrow in (B) indicates calcification.
Figure 7.
Heterogeneous anterior mediastinal mass (black arrow) with areas of calcification and cysts (A) is arising from the thyroid more superiorly (white arrow) (B). The mass represents a unilateral goiter.
Thymic masses
Thymomas
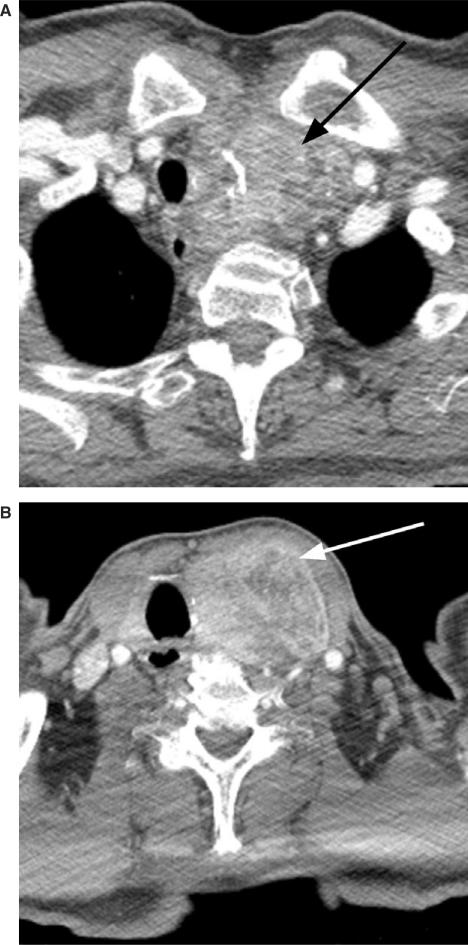
Thymomas are common tumors of the anterior mediastinum, generally showing a slow growth pattern. They manifest as soft tissue density masses at CT, although they often have areas of cysts, hemorrhage, necrosis and/or coarse clumps of calcification (Fig. 8). These lesions are usually asymmetric, commonly draping along one side of the heart. Rarely thymomas may occur in the neck, along the lines of thymic descent during development. Thymomas are the most common type of thymic neoplasm, usually occurring in patients between the ages of 45 and 60, and rarely below the age of 20[12]. Approximately half to a third of patients with this tumor either have or will develop myasthenia gravis. On the other hand, only approximately 10% of patients with myasthenia gravis develop a thymoma. Thymomas are occasionally seen in association with other disorders such as hypogammaglobulinemia, red cell aplasia, connective tissue diseases, and paraneoplastic syndromes. Approximately 20% of patients with thymoma have a malignant neoplasm such as lymphoma, lung cancer or thyroid cancer.
Figure 8.
Invasive thymoma with calcifications (black arrow) and enlarged paratracheal lymph nodes (white arrow) (A). Pleural tumor deposit is seen in (B) (arrow); elevated left hemidiaphragm is due to left phrenic nerve invasion by the mediastinal tumor. (C) Tumor has crossed over the left hemidiaphragm into the retroperitoneum (arrows).
Thymomas are classified as low-risk or high-risk tumors, based on histological features, and as non-invasive or invasive, based on whether the capsule of the gland has been transgressed; approximately 30% of thymomas are invasive. Once the tumor has breached the capsule, it commonly invades adjacent structures such as lung, phrenic nerve, central airways, chest wall, superior vena cava, and great vessels. Elevation of a hemidiaphragm at imaging is highly suggestive of phrenic nerve involvement (Fig. 8). Thymomas typically spread along pleural and pericardial surfaces, leaving behind discrete tumor droplets which are visible at CT as small nodules, masses or plaque-like lesions (Fig. 8). Tumor may cross into the abdomen either directly across a hemidiaphragm or via the retrocrural space (Fig. 8). Thymomas may spread to mediastinal, supraclavicular and cervical lymph nodes, leading to lymph node enlargement in these regions (Fig. 8); however, hematogenous metastases are exceedingly rare.
Thymic carcinomas
Whereas thymomas cannot be classified as benign or malignant at histopathology, thymic carcinomas are histopathologically malignant, occurring with various different cell types. These lesions tend to very aggressive biologically, with a strong tendency to metastasize to distant locations such as lungs, liver, brain and bone. Patients have a very poor prognosis, even after surgical resection. Thymic carcinomas generally show a similar appearance to thymomas at CT and MR, including frequent tumor spread along the pleural and pericardial surfaces. However, if there are findings suggestive of distant metastases, for example lung nodules, then the diagnosis of carcinoma should be entertained, and irregular contour, necrotic or cystic component, heterogeneous enhancement, lymphadenopathy, and/or great vessel invasion are also more common in thymic carcinomas compared to thymomas (Fig. 9)[13]. Preliminary data suggest that fluorodeoxyglucose (FDG)-positron emission tomography (PET) scanning may help in distinguishing thymomas from thymic carcinomas based on standardized uptake values (SUV)[14].
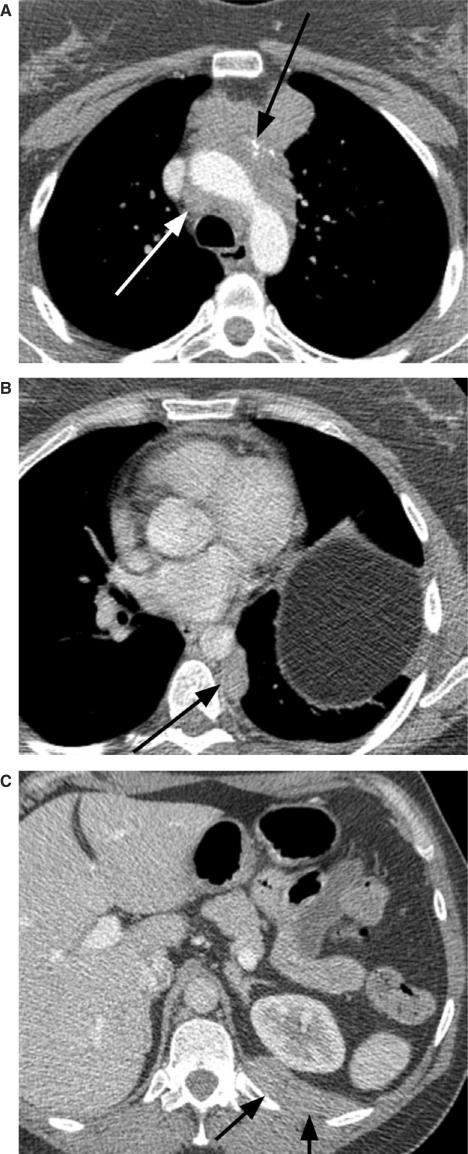
Figure 9.
Thymic carcinoma manifesting as an anterior mediastinal mass with calcifications (A). There is invasion, with near obliteration, of the superior vena cava (B arrow) and multiple venous collaterals are present.
Thymic carcinoids
Thymic carcinoids arise from cells of neural crest origin, i.e. amine precursor uptake and decarboxylation (APUD) cells. Approximately one-half of thymic carcinoids are hormonally active, usually secreting adrenocorticotropic hormone (ACTH) which may lead to Cushing's syndrome[15]. Occasionally patients may present with syndrome of inappropriate antidiuretic hormone secretion (SIADH), although they do not show carcinoid syndrome. Approximately 20% of patients with a thymic carcinoid have underlying MEN I or MEN II disease[16,17].
Thymic carcinoids are usually malignant, and patients tend to have locally invasive disease, distant metastases and a poor prognosis[18]. The tumors often recur locally after surgical resection. Thymic carcinoids are generally indistinguishable from thymomas and thymic carcinomas at CT. If a thymic carcinoid is clinically suspected, somatostatin receptor scintigraphy, for example with [111In]diethylene triamine pentaacetic acid (DTPA) (Octreotide) or [99mTc]EDDA/HYNIC-octreotate, may be performed to confirm the diagnosis[19].
Masses showing significant contrast enhancement
Anterior mediastinal lesions showing significant contrast enhancement include those that arise from vessels, such as aneurysms or pseudoaneurysms, and vascular neoplasms, such as parathyroid adenomas and Castleman's disease[20].
Parathyroid adenomas
Parathyroid adenomas usually occur immediately lateral to the thyroid gland; occasionally, however, they may be seen in ectopic locations such as within the thymus, the tracheoesophageal groove, retroesophageal region or posterosuperior mediastinum. They tend to be small, oval, well-defined soft tissue attenuation structures that enhance strongly with intravenous contrast material and may contain calcifications at CT[21]. Sestamibi scanning or ultrasonography of the neck are often the first imaging modalities used to search for a parathyroid adenoma in a patient with primary hyperparathyroidism[22]; if these studies are inconclusive, then CT or MR may be performed to look for an ectopic focus in the mediastinum.
Conclusion
The attenuation of an anterior mediastinal mass at CT is helpful in narrowing down the differential diagnosis, and evidence of fat, water or calcium may suggest certain diagnoses; significant enhancement of the mass with intravenous contrast may also be a helpful feature. In addition, the exact location and morphology of the mass in question, in conjunction with clinical features, can usually lead to a short list of possible etiologies, thereby directing appropriate additional imaging or other diagnostic procedures or therapeutic approaches.
References
- 1.Sasaka K, Kurihara Y, Nakajima Y, et al. Spontaneous rupture: a complication of benign mature teratomas of the mediastinum. Am J Roentgenol. 1998;170:323–8. doi: 10.2214/ajr.170.2.9456938. [DOI] [PubMed] [Google Scholar]
- 2.Gamanagatti S, Sharma R, Hatimota P, Guleria R, Arvind S. Giant thymolipoma. AJR Am J Roentgenol. 2005;185:283–4. doi: 10.2214/ajr.185.1.01850283a. [DOI] [PubMed] [Google Scholar]
- 3.Sirmali M, Turut H, Gezer S, et al. Clinical and radiologic evaluation of foramen of Morgagni hernias and the transthoracic approach. World J Surg. 2005;29:1520–4. doi: 10.1007/s00268-005-0055-4. [DOI] [PubMed] [Google Scholar]
- 4.Kim JH, Goo JM, Lee HJ, et al. Cystic tumors in the anterior mediastinum. Radiologic-pathological correlation. J Comput Assist Tomogr. 2003;27:714–23. doi: 10.1097/00004728-200309000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Leonidas JC, Berdon WE, Valderrama E, et al. Human immunodeficiency virus infection and multilocular thymic cysts. Radiology. 1996;198:377–9. doi: 10.1148/radiology.198.2.8596835. [DOI] [PubMed] [Google Scholar]
- 6.Choi YW, McAdams HP, Jeon SC, et al. Idiopathic multilocular thymic cyst: CT features with clinical and histopathologic correlation. Am J Roentgenol. 2001;177:881–5. doi: 10.2214/ajr.177.4.1770881. [DOI] [PubMed] [Google Scholar]
- 7.Wang ZJ, Reddy GP, Gotway MB, Yeh BM, Hetts SW, Higgins CB. CT and MR imaging of pericardial disease. Radiographics. 2003;23:S167–80. doi: 10.1148/rg.23si035504. [DOI] [PubMed] [Google Scholar]
- 8.Rattan KN, Magu S, Rohilla S. Mediastinal foregut duplication cysts. Indian J Pediatr. 2004;71:103–5. doi: 10.1007/BF02725668. [DOI] [PubMed] [Google Scholar]
- 9.McAdams HP, Kirejczyk WM, Rosado-de-Christenson ML, Matsumoto S. Bronchogenic cyst: imaging features with clinical and histopathologic correlation. Radiology. 2000;217:441–6. doi: 10.1148/radiology.217.2.r00nv19441. [DOI] [PubMed] [Google Scholar]
- 10.Cakir M, Arici C, Alakus H, Altunbas H, Balci MK, Karayalcin U. Incidental thyroid carcinoma in thyrotoxic patients treated by surgery. Horm Res. 2007;67:96–9. doi: 10.1159/000096357. [DOI] [PubMed] [Google Scholar]
- 11.Miccoli P, Minuto MN, Galleri D, et al. Incidental thyroid carcinoma in a large series of consecutive patients operated on for benign thyroid disease. ANZ J Surg. 2006;76:123–6. doi: 10.1111/j.1445-2197.2006.03667.x. [DOI] [PubMed] [Google Scholar]
- 12.Strollo DC, Rosado-de-Christenson ML. Tumors of the thymus. J Thorac Imaging. 1999;14:152–71. doi: 10.1097/00005382-199907000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Sadohara J, Fujimoto K, Muller NL, et al. Thymic epithelial tumors: comparison of CT and MR imaging findings of low-risk thymomas, high-risk thymomas, and thymic carcinomas. Eur J Radiol. 2006;60:70–9. doi: 10.1016/j.ejrad.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 14.Sung YM, Lee KS, Kim B-T, Choi JY, Shim YM, Yi CA. 18F-FDG PET/CT of thymic epithelial tumors: usefulness for distinguishing and staging tumor subgroups. J Nucl Med. 2006;47:1628–34. [PubMed] [Google Scholar]
- 15.Wang WQ, Ye L, Bi YF, et al. Six cases of ectopic ACTH syndrome caused by thymic carcinoid. J Endocrinol Invest. 2006;29:293–7. doi: 10.1007/BF03344098. [DOI] [PubMed] [Google Scholar]
- 16.Ferolla P, Falchetti A, Filosso P, et al. Thymic neuroendocrine carcinoma (carcinoid) in multiple endocrine neoplasia type 1 syndrome: the Italian series. J Clin Endocrinol Metab. 2005;90:2603–9. doi: 10.1210/jc.2004-1155. [DOI] [PubMed] [Google Scholar]
- 17.Gibril F, Chen YJ, Schrump DS, et al. Prospective study of thymic carcinoids in patients with multiple endocrine neoplasia type 1. J Clin Endocrinol Metab. 2003;88:1066–81. doi: 10.1210/jc.2002-021314. [DOI] [PubMed] [Google Scholar]
- 18.Moran CA, Suster S. Neuroendocrine carcinomas (carcinoid tumor) of the thymus. A clinicopathologic analysis of 80 cases. Am J Clin Pathol. 2000;114:100–10. doi: 10.1309/3PDN-PMT5-EQTM-H0CD. [DOI] [PubMed] [Google Scholar]
- 19.Hubalewska-Dydejczyk A, Fross-Baron K, Mikolajczak R, et al. 99mTc-EDDA/HYNIC-octreotate scintigraphy, an efficient method for the detection and staging of carcinoid tumours: results of 3 years’ experience. Eur J Nucl Med Mol Imaging. 2006;33:1123–33. doi: 10.1007/s00259-006-0113-7. [DOI] [PubMed] [Google Scholar]
- 20.McAdams HP, Rosado-de-Christenson M, Fishback NF, Templeton PA. Castleman disease of the thorax: radiologic features with clinical and histopathologic correlation. Radiology. 1998;209:221–8. doi: 10.1148/radiology.209.1.9769835. [DOI] [PubMed] [Google Scholar]
- 21.Rodger SE, Hunter GJ, Homberg LM, et al. Improved preoperative planning for directed parathyroidectomy with 4-dimensional computed tomography. Surgery. 2006;140:932–40 (. doi: 10.1016/j.surg.2006.07.028. discussion 940–1. [DOI] [PubMed] [Google Scholar]
- 22.Lo C-Y, Lang BH, Chan WF, Kung AWC, Lam KSL. A prospective evaluation of preoperative localization by technetium-99m sestamibi scintigraphy and ultrasonography in primary hyperparathyroidism. Am J Surg. 2007;193:155–9. doi: 10.1016/j.amjsurg.2006.04.020. [DOI] [PubMed] [Google Scholar]