Abstract
BACKGROUND
Upper abdominal exenteration (resection of the liver, stomach, spleen, pancreaticoduodenal complex, and part of the colon) for the treatment of otherwise unresectable tumors is one of the more radical operations in oncology. This study was done to analyze retrospectively a five-year experience with exenteration in 57 patients treated with variations of resectional and transplant reconstructive techniques.
STUDY DESIGN
Sixty-one transplantations were performed upon 57 patients. Three different organ replacement techniques were used: liver-pancreas-duodenum en bloc (original procedure), liver only (modified procedure), and liver plus pancreatic islets. The diagnoses were cholangiocarcinoma (20 patients), hepatocellular carcinoma (12 patients), endocrine neoplasms (14 patients), sarcoma (six patients), and adenocarcinoma of the pancreas (two patients), colon (two patients), or gallbladder (one patient). Analyses of survival and tumor recurrence were stratified by procedure variations, type and extent of tumor, and unmunosuppressive regimen.
RESULTS
The three month and one, two, three, and five year actuarial patient survival rates were 82, 56, 38, 33, and 30 percent, respectively. Eighteen (31.5 percent) of the 57 patients are alive after 425 15 (standard deviation) months (range of 17 to 61 months) and 12 patients are tumor free. The actuarial survival rates stratified by transplantation procedure, immunosuppression, and tumor diagnosis and extent showed no statistically significant differences beyond the three different transplantation groups. Endocrine tumors had a better three-year survival rate (64 percent) than sarcoma (44 percent), hepatocellular carcinoma (25 percent), cholangiocarcinoma (20 percent), and the other adenocarcinomas (20 percent). Twenty-three patients (40 percent) died as a result of tumor recurrence. Patients with combined factors of no lymph node involvement, absence of vascular invasion, and metastases to the liver only (11 patients) had the lowest incidence of recurrence (27 compared to 73.5 percent, p=0.006).
CONCLUSIONS
Patients with unresectable endocrine neoplasms, fibrolamellar hepatocellular carcinoma, and selected cholangiocarcinoma confined to the liver can benefit from this radical operative approach. Patients with sarcoma can achieve long survival periods but have a high recurrence rate.
Cluster exenteration has been used to treat patients with otherwise nonresectable malignancies of the upper abdominal tract. In most cases, the organs excised with this procedure were the liver, pancreas, spleen, stomach, duodenum, and variable amounts of the colon. Lately, two more conservative procedures have been used in some selected cases, with preservation of part of the stomach, or preservation of the body and the tail of the pancreas, or preservation of both (Whipple procedure), combined with a total hepatectomy. Three different organ replacement techniques have been used, all including the liver (1–3).
This is one of the more radical operations in oncology, for which reason it has been controversial. Ethics questions have concerned the survival of these patients, the possibility of controlling such advanced tumors, and the influence of original tumor diagnosis and extent on outcome. We have examined these and other issues in 57 consecutive patients who underwent exenteration one to almost five years ago.
METHODS
Case material
The 57 patients were treated between July 22, 1988 and June 4, 1992 and had follow-up evaluation to the end of 1993. Their ages ranged from eight to 59 years, with an equal distribution between genders. Before transplantation, 37 patients had normal liver function tests (LFT). Twenty patients had minor to moderate elevation of LFT but no hepatic failure or severe portal hypertension. Seventeen of the patients and two other patients with otherwise good hepatic function had jaundice at the time of the operation, with a mean total bilirubin level of 8.5 ± 4.3 (standard deviation) mg/dL. None of the patients were in renal failure before the transplant. One patient had diabetes mellitus.
Conventional operative treatment (including exploratory laparotomies) had been attempted in 30 patients; 19 patients had been treated with chemotherapy or radiation, or both. One patient previously treated for hepatocellular carcinoma (HCC) with hepatic transplantation underwent the cluster procedure when the malignancy recurred in the hepatic allograft. All of the patients were considered incurable by conventional medical treatment or operation at the time of the cluster operation.
Tumor pathology
There were 20 patients with cholangiocarcinoma (12 extrahepatic and eight intrahepatic) and 12 with HCC (Table I). Of special interest were three patients with fibrolamellar HCC, all with metastases to lymph nodes; two of the three had vascular invasion. The other patients had either endocrine neoplasms of pancreatic, enteric, or gastric origin (14 cases), gastrointestinal sarcoma (six cases), adenocarcinoma of the pancreas (two cases), adenocarcinoma of the study with a the colon (two cases), or adenocarcinoma of the gallbladder (one case). There were extensive hepatic metastases in all but three of the 57 cases.
TABLE I.
CASE MATERIAL
| No. of patients | |
|---|---|
| Disease categories | |
| Cholangiocarcinoma | 20 |
| Endocrine | 14 |
| Hepatocellular carcinoma | 12 |
| Sarcoma | 6 |
| Others | 5 |
| Type of cluster transplant | |
| Original | 21 |
| Modified | 25 |
| Islets and liver | 11 |
| Immunosuppression | |
| Cyclosporine | 32 |
| FK 506 | 25 |
There were 57 patients (33 males and 24 females) in mean age of 40±11 years (range of eight to 59 years).
No., Number.
Lymph nodes draining the liver, or other portions of the removed specimens, contained tumor in 31 of the 57 cases. Metastases to other whole organs (in addition to the hepatic involvement) were present in 18 patients. Macroscopic vascular invasion was found in 33 of the livers. Only 11 of the 57 patients had a triad of favorable findings consisting of negative nodes, absence of vascular invasion, and confinement of metastases to the liver. In two of the 11 patients, the hepatic parenchyma was free of metastases from a pancreatic endocrine tumor in one case and an adenocarcinoma of the pancreas in the other. In these two exceptions, extensive invasion of the extrahepatic biliary tree necessitated total hepatectomy.
Transplantation procedures
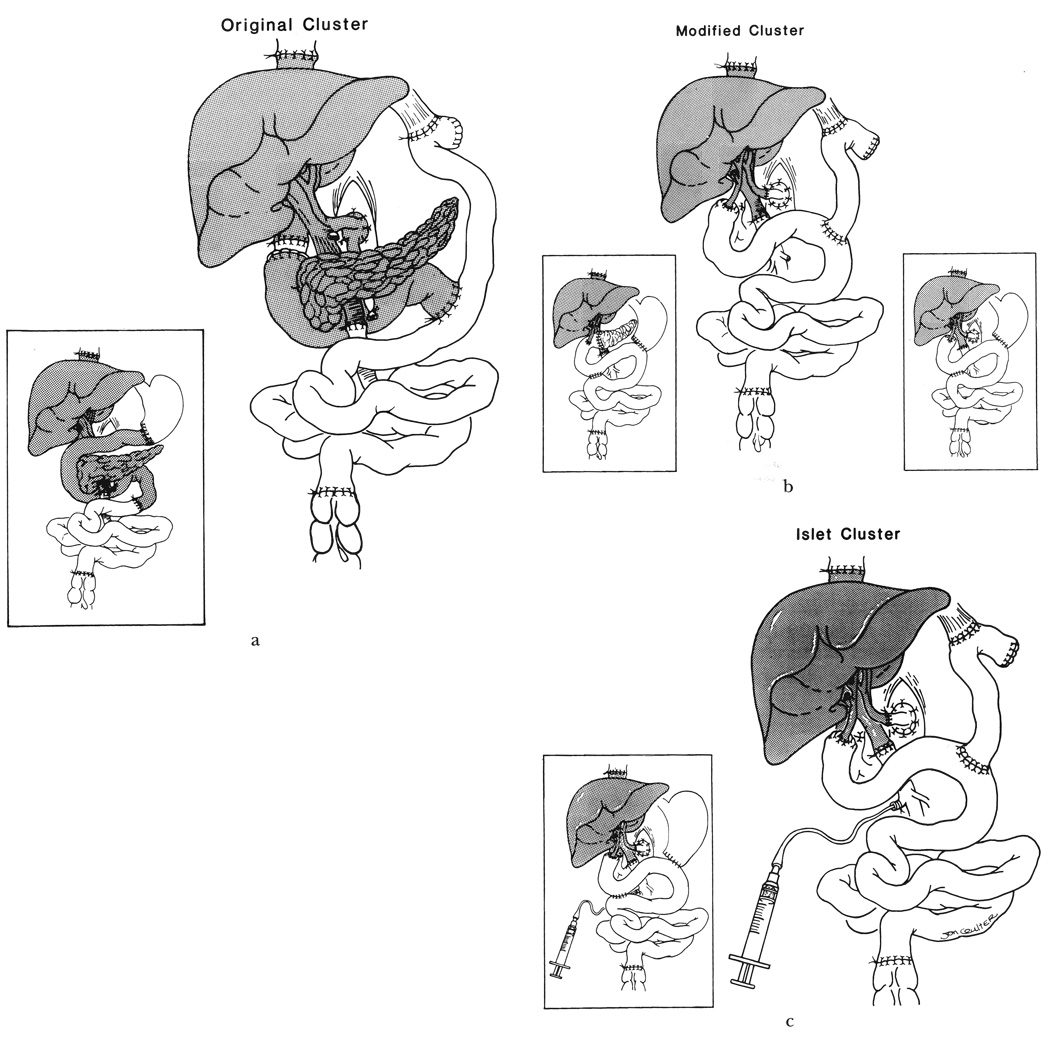
The 57 patients underwent 61 transplantations. The principles (1, 4) as well as details (1, 2, 5) of both the donor and recipient operations have been described elsewhere. The most common variation of the complete exenteration was preservation of part of the stomach in 12 patients (Fig. 1a, b, and c), of whom three also retained the body and the tail of the pancreas, as with the Whipple operation (Fig. 1b) . All but one of the 57 primary cadaveric donors were ABO blood group identical with the recipients, the only exception being an 0 to B combination for a patient too ill to wait for a matched graft. Similar degrees of urgency prompted the acceptance of nonidentical donorrecipient pairing (0 to A and 0 to B) for two of the four retransplantations. Human leukocyte antigen matching was random and uniformly poor. The lymphocytotoxic cross-match was positive in five of the 61 transplantations.
Fig. 1.
a, Original cluster procedure with transplantation of liver-pancreas-duodenum en bloc. In two cases, part of the stomach was preserved and the transplanted duodenum was placed in continuity with the stomach and jejunum of the patient (inset). b, Modified cluster procedure with transplantation of the liver only. In eight patients, one-third or more of the recipient stomach was preserved (inset, right), including three patients in whom the body and the tail of the pancreas also were retained (inset, left). c, Islet cluster procedure with transplantation of the liver and pancreatic islets injected into the portal vein of the transplanted liver. In two patients, part of the recipient stomach was preserved (inset).
The transplantation technique provided a basis for stratification of results:
Original cluster operation (1,6). Twenty-three composite grafts were transplanted to 21 patients. These consisted of the liver, pancreas, duodenum, and variable amounts of proximal jejunum (Fig. 1a). Two of these grafts were used for retransplantation four days after the primary procedure.
Modified cluster operation (2, 7). In 25 patients, the excised specimen was replaced with the liver only (n=27, including two retransplantations). The two retransplantations were one and 73 days, respectively, after the primary operation. In eight of the 25 cases, one-third or more of the recipient stomach was preserved (Fig. 1b), including three patients in whom the body and tail of the pancreas also were retained. All 22 recipients whose entire pancreas was excised became diabetic immediately.
Islet cluster. These 11 patients had islets prepared from the liver donor pancreas injected into the portal vein of the transplanted liver before the abdominal incision was closed (Fig. 1c). The details of islet preparation and the determination of islet viability and doses are given elsewhere (3).
Immunosuppression
Prophylaxis against graft-versus-host disease (GVHD) was attempted with donor pretreatment in eight of the first ten cases by infusion of 10 to 20 mg of OKT3 during or preceding organ procurement. The first 32 patients were treated with cyclosporine (CyA) and prednisone immunosuppression to which a prophylactic 10-to-14-day course of OKT3 was added perioperatively in the first 15 patients. Azathioprine was begun when and if the white blood count exceeded 5,000 mm3. These regimens have been described elsewhere (1). Several of these recipients were later changed to FK 506. FK 506 combined with prednisone was used in the last 25 patients, adjusting the dose on clinical grounds and by monitoring FK 506 plasma levels.
Statistical analysis
Survival curves were generated using the Kaplan-Meier (product limit) method and were compared using the generalized Wilcoxon’s (Breslow) test. The chi-square test of association was used to compare proportions. A p value of less than 0.05 was considered statistically significant.
RESULTS
Overall patient survival
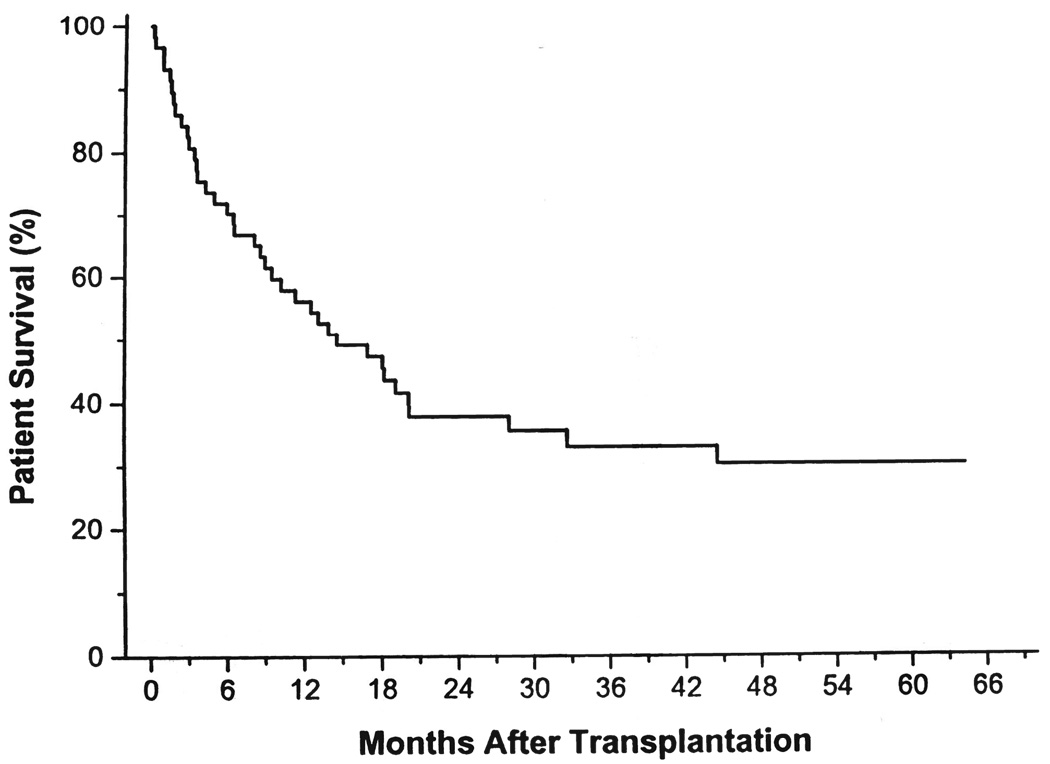
All patients survived the operation, although four required retransplantation one, four, four, and 73 days later, respectively. At three months, the patient survival rate was 82 percent. The one, two, three, and five year actuarial patient survival rate was 56, 38, 33, and 30 percent, respectively (Fig. 2). Eighteen (31.5 percent) of the 57 patients are alive after 42 ± 15 months (range of 17 to 61 months). Only two patients have less than two years of follow-up evaluation. Six of the 18 survivors have recurrent tumor.
Fig. 2.
The overall actuarial patient survival rate curve.
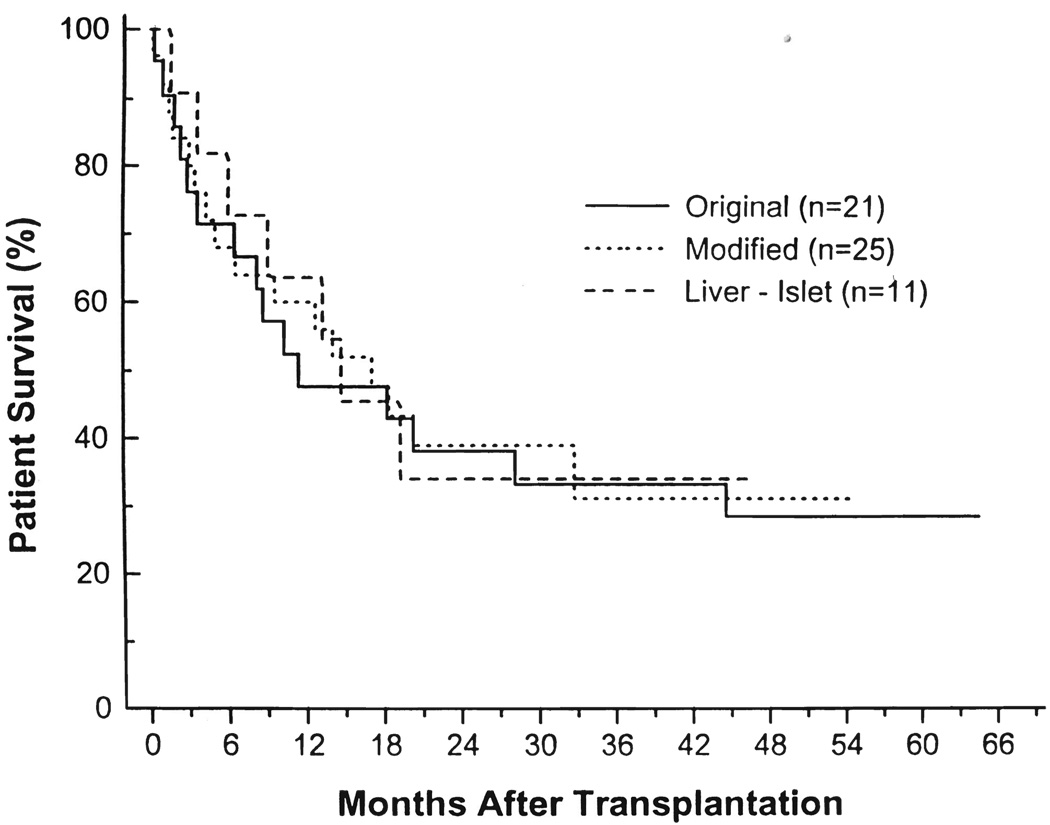
Stratified patient survival
By transplantation procedure.— The actuarial survival rates for the three cohorts of patients that underwent original, modified, or islet cluster transplantation are illustrated in Figure 3. The actuarial one, two, and three year survival rates were 48, 38, and 33 percent in the original cluster group; 60, 39, and 31 percent in the modified cluster group; and 63, 34, and 34 percent in the islet cluster group. The differences were not significant.
Fig. 3.
The actuarial patient survival rate stratified by transplantation procedure: original cluster (liver-pancreas-duodenum), modified cluster (liver only), and liver plus pancreatic islets.
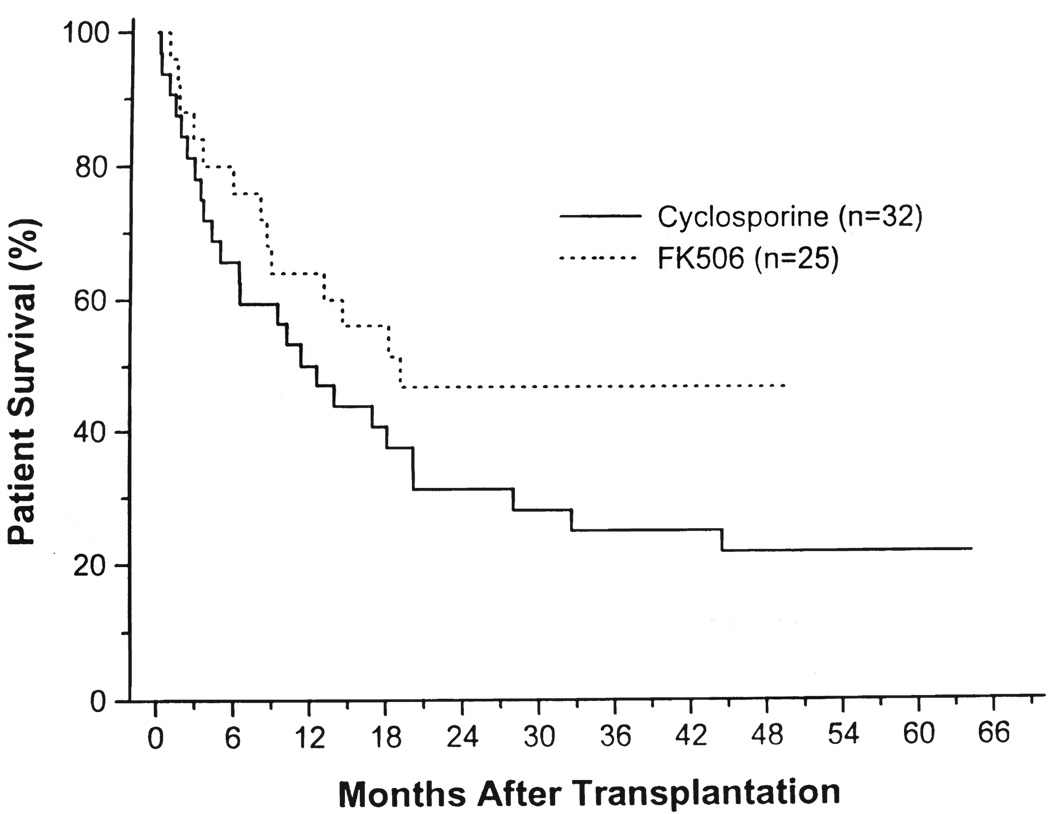
By immunosuppression.—There is a trend of better survival in the FK 506 cohort (Fig. 4). However, the cyclosporine and FK 506 cohorts were not statistically comparable because they were consecutive and there were differences in neoplastic disease and type of transplantation procedure.
Fig. 4.
The actuarial patient survival rate stratified by immunosuppression with cyclosporine or FK 506.
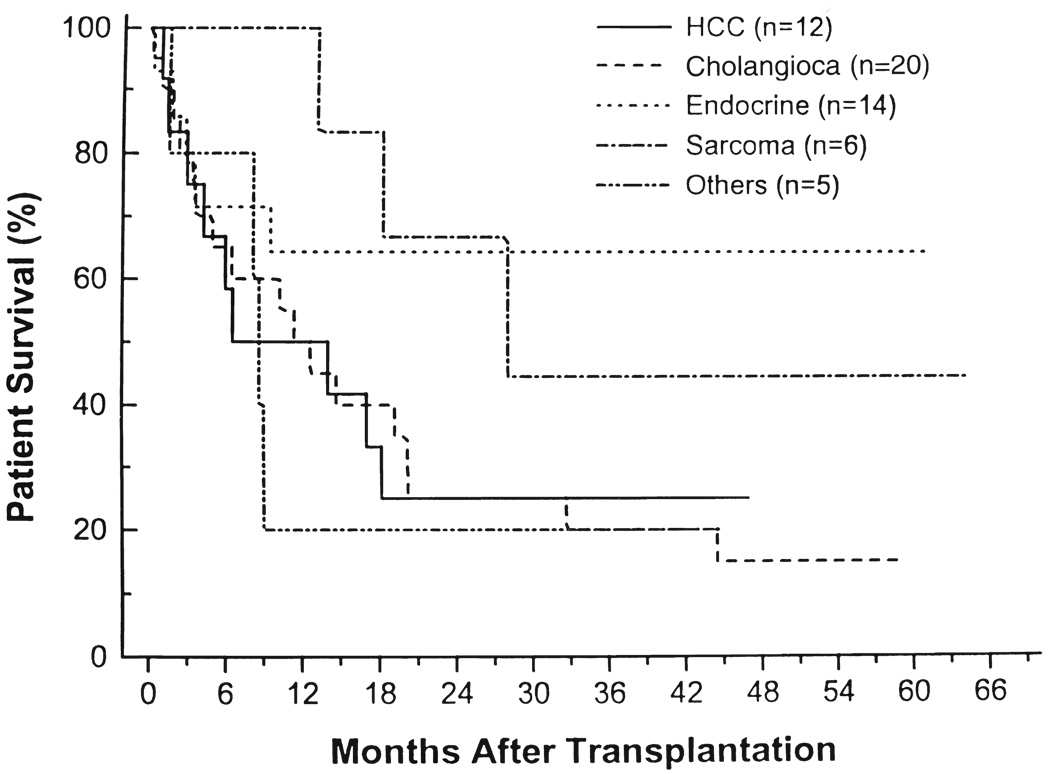
By tumor histology.—The actuarial survival rates of the five groups were not significantly different (Fig. 5). However, patients with endocrine and sarcoma neoplasms had a better survival rate when compared with the others. At three years, the survival rate was 64 percent for patients with endocrine tumors, 44 percent for those with sarcoma, and 20 to 25 percent in the other three tumor groups.
Fig. 5.
The actuarial patient survival rate stratified by histologic diagnosis. HCC, Hepatocellular carcinoma, and Cholangioca, cholangiocarcinoma.
By tumor extent.—Patients with metastases to local and regional lymph nodes had almost the same one, two, and three year survival rates (52, 38, and 33 percent, respectively) as those with negative nodes (62, 37, and 33 percent, respectively). The survival rate for one, two, and three years was better in patients without tumor vascular invasion than with this finding, but the differences were not significant (data not shown). Patients with metastases in other whole organs in addition to the liver had survival rates at one, two, and three years of 50, 38, and 20 percent, respectively, while those with tumor confined to the liver had survival rates at these times of 59,38, and 38 percent, respectively (data not shown).
The survival rates were 64, 45, and 45 percent at one, two, and three years, respectively, for the 11 patients who had all three of the presumed favorable conditions of no lymph node metastases, absence of vascular invasion, and confinement of metastases to the liver. For the other 46 patients, the survival rates at one, two, and three years were 54, 36, and 29 percent, respectively. These differences were not statistically significant because of the low number of patients in the first group (data not shown).
Analysis of deaths
Nontumor related.—Ten patients died perioperatively or during the first three months postoperatively, eight as a result of disseminated bacterial, viral, or fungal infections. The two other early deaths were a result of intra-abdominal hemorrhage and multiorgan lymphoproliferative disease. Of the eight patients who were septic, one had recurrence at the time of death. This recipient had tumor in the resected margin of the upper vena cava of the multivisceral specimen.
Five more deaths occurred as a result of delayed technical or other nontumor complications and consequent fatal sepsis by the end of the first year. An example was a patient with a duct cell carcinoma who died from rupture of a mycotic aneurysm of the celiac Carrel patch after 345 days. Hepatic artery thrombosis in another patient resulted in death after an unsuccessful retransplantation. In the second postoperative year, a woman with renal failure, who was noncompliant, committed suicide at 19 months after ceasing medications and refusing further treatment, including dialysis. All but one of the six patients who died after the first three months were tumor free at the time of death. In the one exception, micrometastases of cholangiocarcinoma were an incidental finding at autopsy.
The number of patients who died as a result of causes not related to tumor recurrence was 16 (28 percent). The incidence of the nontumor-related mortality in the different transplantation procedure groups was 33 percent in the original cluster, 24 percent in the modified cluster, and 27 percent in the islet cluster groups. The differences were not significant statistically. The special group of 11 patients with only hepatic metastases had a 36 percent incidence of nontumor-related mortality, compared with 26 percent for the other population. The groups did not differ significantly.
No differences were seen between the CyA and the FK 506 groups, but a trend of more frequent fatal sepsis was present in the CyA group (25 versus 16 percent). Lymphoproliferative disease accounted for the death of a patient who was FK 506 immunosuppressed.
Tumor related.—Twenty-three patients (40 percent) died as a result of tumor recurrence after a mean survival period of 515 ± 430 days (range of 91 to 1,948 days). In the special group of 11 patients with hepatic metastases only, the incidence of death from recurrence was 27 percent, while in the other 46 patients, the incidence was 44 percent.
There was only one example (7 percent) of a lethal recurrence of an endocrine tumor (carcinoid of the pancreas) causing death after 289 days. The incidence and median time of tumor-related mortality was 45 percent for cholangiocarcinoma (562 days), 50 percent for HCC (327 days), 60 percent for adenocarcinoma of the pancreas, colon, or gallbladder (259 days), and 66.6 percent for sarcoma (938 days). The latest tumor-related death was a 31-year-old woman whose diagnosis was sarcoma of the duodenum with massive hepatic metastases. After four years, metastases to the brain were noted on a computer tomographic scan and the patient died as a result of disseminated tumor recurrence after five years and four months.
The different transplantation techniques had no influence on the incidence of tumor-related mortality, which was 43, 40, and 36 percent in the original, modified, and islet cluster procedure groups, respectively. The incidence of death from recurrence was higher in the CyA group (50 percent) than in the FK 506 group (28 percent), but this difference was not significant.
Analysis of recurrence
To better define the real incidence of and the influence of the different procedures on recurrence, the ten patients who died within the first three months as a result of technical or nontumor complications were excluded, as well as two others who died later in whom gross tumor was left at the resection margin. The two patients who were excluded who died as a result of recurrence after three months (197 and 304 days) were omitted from the analysis because there was roentgenographic and other evidence in both of extension of the cholangiocarcinomas beyond the surgical boundaries at the time of operation.
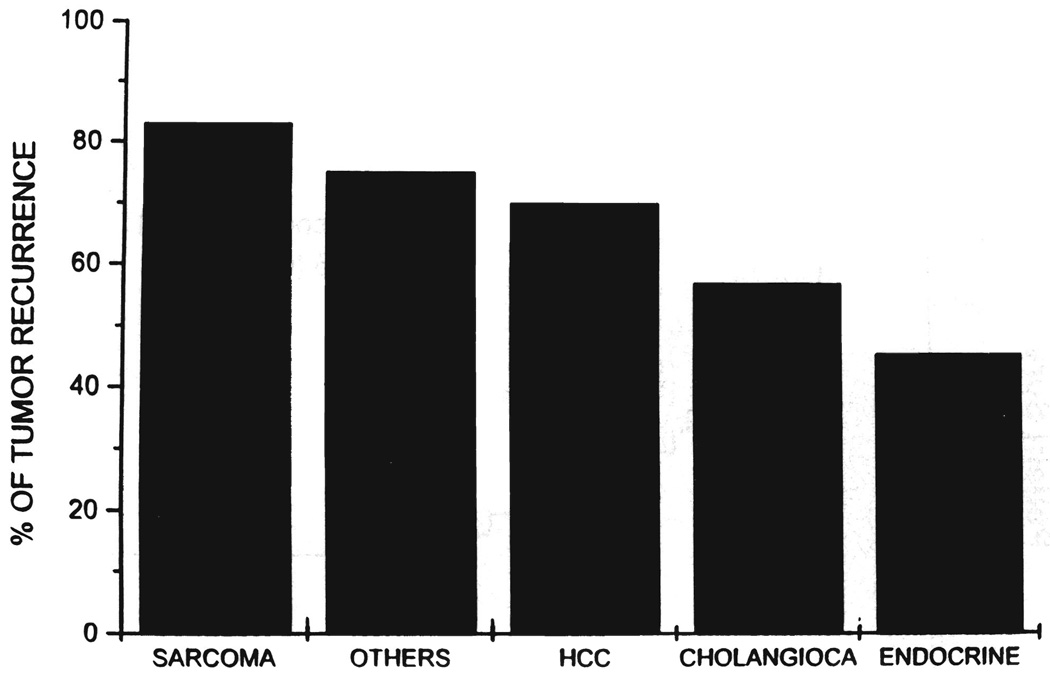
The remaining 45 patients who had at least three months of follow-up evaluation had a 62 percent incidence of tumor recurrence. Sarcoma was the highest (83 percent), followed by the mixed group of adenocarcinoma of the pancreas, colon, and gallbladder (75 percent), HCC (70 percent), cholangiocarcinoma (57 percent), and endocrine tumor (45.5 percent) (Fig. 6). The differences within these five groups were not statistically significant.
Fig. 6.
Incidence of recurrence within each tumor diagnosis group. Patients who died within the first three months from technical or nontumor complications (ten cases), as well as those in whom gross tumor remained (two cases) were excluded from this analysis. HCC, Hepatocellular carcinoma, and cholangioca, cholangiocarcinoma.
All of the 11 patients with no lymph node metastases, no vascular invasion, and absence of metastases to whole organs other than the liver were among the culled 45 patients. Their recurrence rate was 27 percent compared with 73.5 percent in the remaining 34 patients (p=0.006).
Analysis of the surviving patients
Of the 18 patients alive, 12 are tumor free after 42 ± 15 months (range of 17 to 61 months). Interestingly, two of the three patients with fibrolamellar HCC are well at 28 and 47 months, respectively. Of these two patients, the one surviving the longest period, a 21-year-old woman, was operated upon and treated with adjuvant chemotherapy for a right mandibular recurrence two years after the exenteration. Although she is clinically well at 47 months, a recent cervical lymph node biopsy revealed recurrent tumor. The other patient with the fibrolamellar variant has no evidence of recurrence. The third living patient of the HCC group is a 52-year-old physician who presented preoperatively with two HCC nodules in the cirrhotic liver, one in the right lobe and the other in the caudate lobe, with portal vein invasion and direct invasion of the contiguous pancreas. After three courses of pretransplant intra-arterial local and regional chemotherapy, modified cluster exenteration was performed with preservation of part of the stomach and of the distal portion of the pancreas. After 29 months, the patient has no evidence of recurrence.
Three patients with cholangiocarcinoma who are alive without recurrence at 52, 54, and 59 months, respectively, belonged to the special group of 11 patients with hepatic metastases only. The primary lesion in these three patients was in the extrahepatic ducts, which was thought to preclude hepatic transplantation alone. Another patient with adenocarcinoma of the pancreas has no evidence of recurrence at 44 months.
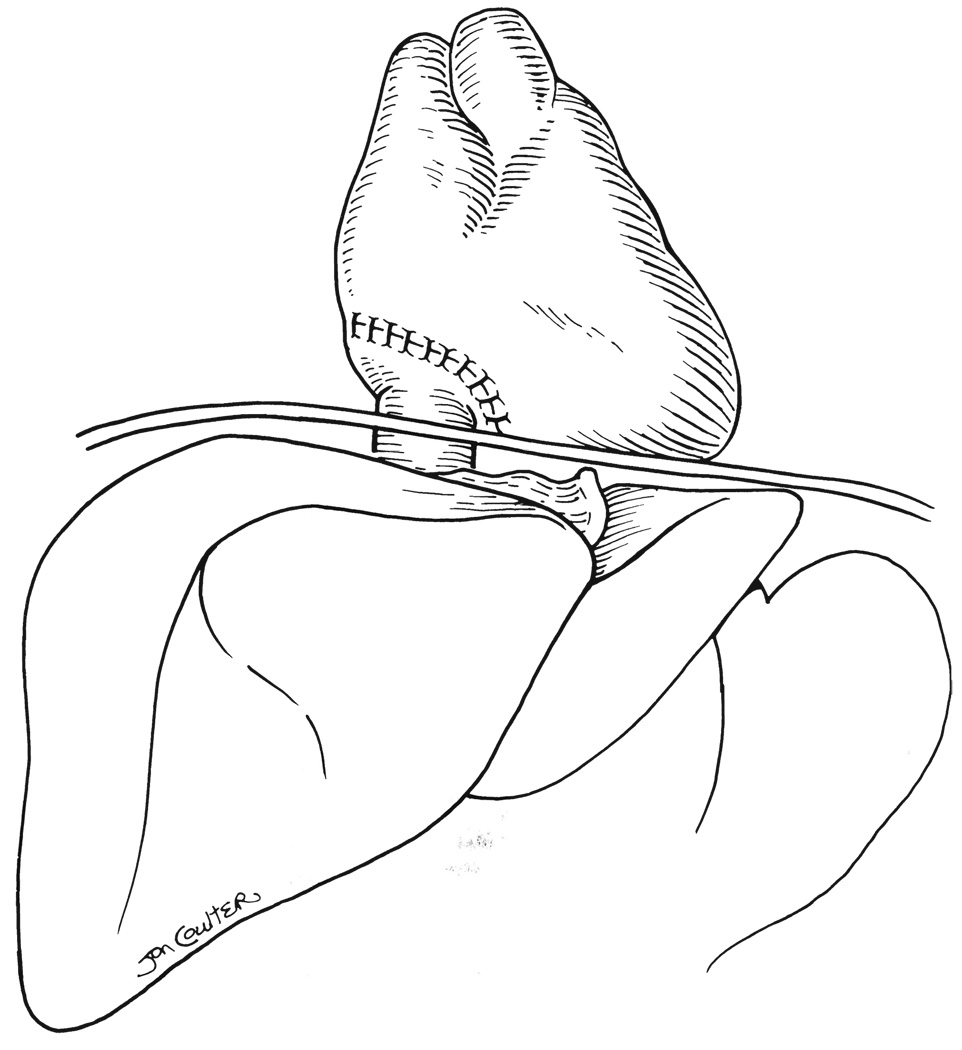
One of the two patients with sarcoma is alive at 19 months with recurrence, and the other patient is tumor free at 49 months. Three patients are alive at 33, 50, and 56 months, respectively, with recurrent endocrine tumor. A fourth patient with endocrine tumor diagnosis is alive at 18 months, but with a biopsy-proved primary adenocarcinoma of the lung, which was diagnosed after eight months. Five patients with pretransplant diagnosis of endocrine tumor are alive without evidence of disease at 17, 27, 32, 54, and 61 months, respectively. Of these, the patient who is alive at 32 months presented a difficult technical problem because the tumor (a gastrinoma) was found inside the upper vena cava, invading the right atrium. During the exenteration, the diaphragm was opened and the entire upper vena cava and part of the wall of the right atrium were excised and replaced with both donor structures (Fig. 7). This patient, who also had an infusion of donor pancreatic islets, now has a normal life.
Fig. 7.
Transplantation technique in a patient with gastrinoma invading the upper vena cava and the right atrium. The entire upper vena cava and part of the wall of the right atrium were excised and replaced with both donor structures. This patient, whose entire pancreas was removed, had donor pancreatic islets infused into the portal vein and is insulin free after four years.
Nutritional status
The nutritional complications of the cluster operations have been previously reported (1, 7). Malabsorption, diarrhea, and weight loss occurred in all patients, but the explanation was frequently difficult to sort out because of the frequent technical complications in early stages and tumor recurrence later. Consequently, we separately analyzed the 12 patients who are alive without evidence of tumor.
During the first three months, these patients lost 15 ± 8 percent of their preoperative body weight. Later, they maintained this level with only an additional 5 percent loss during the first two years. At three years or at the latest follow-up evaluation (42 ± 15 months), or both, the weight remained stable. Two patients still require occasional home parenteral nutrition support at night to maintain a regular weight. In the only surviving patient with nonfibrolamellar HCC, the current weight after 29 months is higher than before operation.
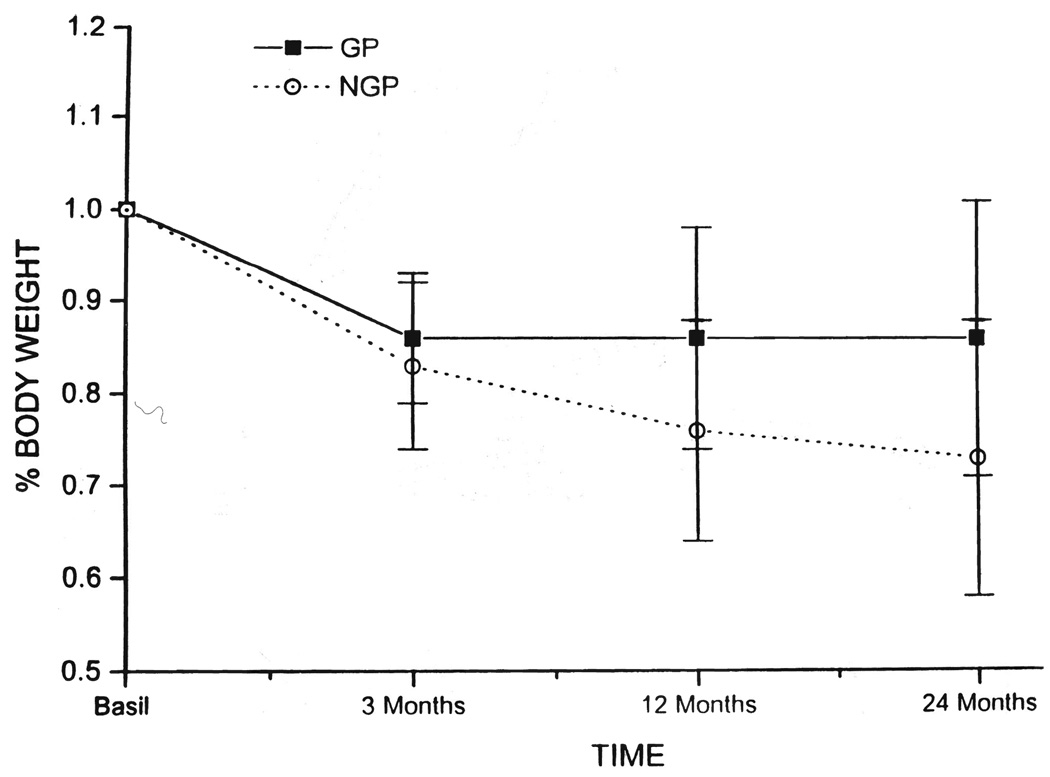
In the group of 12 patients, there were seven patients with retention of a significant gastric remnant and five without this advantage (Fig. 8). Patients with a gastric remnant had minor weight loss that was limited to the first three months compared to the other cohort. However, the weight of those with total gastrectomy stabilized after one year.
Fig. 8.
The mean percent of weight loss in the surviving are tumor free who had part of the stomach preserved (GP=7 cases) and those in whom total gastrectomy was performed (NGP=5 cases). GP, Gastric preservation, and NGP, nongastric preservation.
Four of the 12 patients received pancreatic islet allografts in addition to the liver (3) after complete recipient pancreas removal. Two patients are insulin free at 44 and 47 months, respectively, while the other two require daily insulin injections.
DISCUSSION
One purpose of this follow-up study was to define the patient populations that might be helped by the radical cluster operations, considering histopathologic criteria and degree of metastatic extension. Grouping all tumor types together, the results were favorably influenced by the triad of negative lymph nodes, involvement of no more than one whole organ, and absence of vascular invasion by tumor. The greatest benefit was in patients with endocrine tumors, and the least was in those with adenocarcinoma of colon, pancreas, or gallbladder. Patients with sarcoma survived for long periods, although they eventually had a high recurrence rate. Patients with cholangiocarcinoma had no significant benefit from this procedure unless the primary tumor was confined to the liver and bile ducts.
The prognosis was poor for patients with HCC, but as suspected from previous investigations (8), the fibrolamellar variant may be an exception. McMaster and co-workers (9) have argued that there is no legitimate place for the cluster procedure in the treatment of this disease, believing that conventionally unresectable hepatoma should either be treated by hepatic transplantation alone or not at all. Our experience, particularly with the fibrolamellar variant, does not support this position, although it has verified the poor outlook with advanced disease. All of the patients in our study with the diagnosis of HCC had tumor beyond the confines of an extended total hepatectomy, such as that described by McMaster and associates (9), including 30 percent who had gross metastases in other whole organs. Two of three patients in our study with fibrolamellar HCC benefitted from treatment, compared with only one in nine with the more common HCC in which the presence of multiple organ involvement or metastases in any of the lymph nodes was an ominous prognostic sign.
Aside from survival, the nutritional morbidity caused by cluster operation was an observation end point. This seemed to be related to a balance between the extent of extirpation and the degree of organ replacement. The loss of the entire stomach was disabling, whereas weight loss and diarrhea were reduced in patients with a significant gastric remnant. However, there may be no alternative to total gastrectomy if gross tumor is to be removed, and in such cases, variations of the multivisceral operation in which the hollow gastrointestinal organs are transplanted in continuity with the liver, may be an option. These so-called multivisceral operations, including the transplantation of the entire intra-abdominal gastrointestinal tract, have permitted restoration of a good quality of life for as many as three years in most patients with non-neoplastic disease (10–12).
Despite the high morbidity and mortality rates in these otherwise incurable patients, it is appropriate to consider that nearly one of every three patients who entered the series is alive or expected to be alive at five years. Most of the surviving patients are functional in society (some completely normally), although two of them require overnight parenteral feedings to maintain their weight. Whether or not the benefit is judged to be sufficient to warrant further trials may become moot because of the organ shortage that began during the case accrual of this study and evolved to crisis proportions by its conclusion. Few would debate the propriety of heroic efforts at carcinoma therapy resulting in a significant survival rate if there were an unlimited organ supply. However, with the logic that organs can be more efficiently invested to patients without carcinoma, it may be that the cluster or multivisceral operations will have to wait the development of xenotransplantation for a full evaluation.
Apart from the question of their practical clinical application, the cluster procedures have contributed lessons in biology and transplantation immunology. In supporting animal research, it was discovered by Murase and colleagues (13), and was confirmed by Iwaki and associates (14) in humans, that partial or complete multivisceral grafts became hematolymphopoietic chimeras within a short time after their transplantation with donor specific retention of the epithelial components, while the leukocyte constituency is replaced with a recipient population. This important discovery resulted directly in a realization that the interstitial donor white cells departing the grafts migrated ubiquitously in the recipient and survived, creating the systemic microchimerism that we postulate to be the basis for acceptance of all kinds of grafts (15).
Furthermore, the elucidation of this bidirectional traffic has clarified much of the mystery about the feared complication of GVHD, including the reason for its lack of appearance after the transplantation of lymphoid-rich organs, such as those in the composite cluster grafts (16). This paradigm of transplantation immunology has contained a warning (4, 16) against not only host preconditioning with immunosuppression, but equally against the kind of graft preconditioning with lymphoid depletion that was attempted with OKT3 in the first eight patients in our study. We have ascribed the high rate of lymphoproliferative tumors (B-cell lymphomas) in the early attempts at multivisceral transplantation (17, 18) to the lymphoid depletion procedures (16). Fortunately, there was only one example of this complication in the 57 cases of the present series. Reversible GVHD was seen in only two patients, as noted elsewhere (16).
It is also noteworthy that two of the 11 patients who had replacement of the liver combined with free pancreatic islet allografts remain alive in an insulin-free state after 44 and 47 months. Because these were the first patients in the world to undergo successful pancreatic islet transplantation (3), they established the feasibility of this procedure after total pancreatectomy using a single donor source, and stimulated other successful trials elsewhere in patients with type I diabetes mellitus.
Acknowledgments
This study was supported, in part , by Project Grant No DK 29961 from the National Institutes of Health, Bethesda, MD.
REFERENCES
- 1.Starzl TE, Todo S, Tzakis A, et al. Abdominal organ cluster transplantation for the treatment of upper abdominal malignancies. Ann. Surg. 1989;210:374–386. doi: 10.1097/00000658-198909000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tzakis AG, Todo S, Starzl TE. Upper abdominal exenteration with liver replacement: a modification of the cluster procedure. Transplant. Proc. 1990;22:273–274. [PMC free article] [PubMed] [Google Scholar]
- 3.Tzakis AG, Ricordi C, Alejandro R, et al. Pancreatic islet transplantation after upper abdominal exenteration and liver replacement. Lancet. 1990;336:402–405. doi: 10.1016/0140-6736(90)91946-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Starzl TE, Todo S, Tzakis A, et al. The many faces of multivisceral transplantation. Surg. Gynecol. Obstet. 1991;172:335–344. [PMC free article] [PubMed] [Google Scholar]
- 5.Casavilla A, Selby R, Abu-Elmagd K, et al. Donor selection and surgical technique for en bloc liver-small bowel graft procurement. Transplant. Proc. 1993;25:2638–2639. [PMC free article] [PubMed] [Google Scholar]
- 6.Mieles L, Todo S, Tzakis A, Starzl TE. The treatment of upper abdominal malignancies with organ cluster procedure. Clin. Transplant. 1990;4:63–67. [PMC free article] [PubMed] [Google Scholar]
- 7.Tzakis AG, Todo S, Madariaga J, et al. Upper abdominal exenteration in transplantation for extensive malignancies of the upper abdomen: an update. Transplantation. 1991;51:727–728. doi: 10.1097/00007890-199103000-00035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Starzl TE, Iwatsuki S, Shaw BW, Jr., et al. Treatment of fibrolamellar hepatoma with partial or total hepatectomy transplantation of the liver. Surg. Gynecol. Obstet. 1986;162:145–148. [PMC free article] [PubMed] [Google Scholar]
- 9.McMaster P, Mirza D, Harrison JD. Surgical options for primary hepatocellular carcinoma. Br. J. Surg. 1993;80:1365–1367. doi: 10.1002/bjs.1800801103. [DOI] [PubMed] [Google Scholar]
- 10.Abu-Elmagd K, Todo S, Tzakis A, et al. Three years clinical experience with intestinal transplantation. J. Am. Coll. Surg. 1994;179:385–400. [PMC free article] [PubMed] [Google Scholar]
- 11.Todo S, Tzakis AG, Abu-Elmagd K, et al. Intestinal transplantation in composite visceral grafts or alone. Ann. Surg. 1992;216:223–234. doi: 10.1097/00000658-199209000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tzakis AG, Todo S, Reyes J, et al. Intestinal transplantation in children under FK506 immunosuppression. J. Pediatr. Surg. 1993;8:1040–1043. doi: 10.1016/0022-3468(93)90514-l. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murase N, Demetris AJ, Matsuzaki T, et al. Long survival in rats after multivisceral versus isolated small bowel allotransplantation under FK 506. Surgery. 1991;110:87–98. [PMC free article] [PubMed] [Google Scholar]
- 14.Iwaki Y, Starzl TE, Yagihashi A, et al. Replacement of donor lymphoid tissue in human small bowel transplants under FK 506 immunosuppression. Lancet. 1991;337:818–819. doi: 10.1016/0140-6736(91)92517-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Starzl TE, Demetris AJ, Murase N, et al. Donor cell chimerism permitted by immunosuppressive drugs: a new view of organ transplantation. Immunol. Today. 1993;14:326–332. doi: 10.1016/0167-5699(93)90054-o. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Starzl TE, Demetris AJ, Trucco M, et al. Cell migration and chimerism after whole organ transplantation: the basis of graft acceptance. Hepatology. 1993;17:1127–1152. [PMC free article] [PubMed] [Google Scholar]
- 17.Starzl TE, Rowe M, Todo S, et al. Transplantation of multiple abdominal viscera. J. A. M. A. 1989;261:1449–1457. [PMC free article] [PubMed] [Google Scholar]
- 18.Williams JW, Sankary HN, Foster PF, et al. Splanchnic transplantation: an approach to the infant dependent on parenteral nutrition who develops irreversible liver disease. J. A. M. A. 1989;261:1458–1462. doi: 10.1001/jama.261.10.1458. [DOI] [PubMed] [Google Scholar]