Abstract
Objective
To determine if, and at what point, glaucoma affects spoken reading speed.
Methods
Data were collected from the Salisbury Eye Evaluation, a population-based evaluation of visual function and disability in the elderly. Non-scrolling text was displayed on a screen and the rate words were read aloud was measured. Subjects reading slower than 90 words/minute were defined as impaired. Glaucoma status was determined using optic disc appearance and visual field testing.
Results
1,154 subjects completed evaluations of spoken reading speed and glaucoma status. Univariate analysis demonstrated reading impairment in 16.0% of non-glaucoma subjects, 21.1% of unilateral glaucoma subjects (p=0.25) and 28.4% of bilateral glaucoma subjects (p=0.006). Multivariable regression demonstrated non-significant increases in the odds of reading impairment for unilateral (OR=1.13, p=0.69) and bilateral glaucoma subjects (OR =1.25, p=0.43), though bilateral glaucoma subjects in the highest quartile of better-eye visual field loss read slower (β=−32 words/minute, p=0.01) and were more often reading impaired than non-glaucoma controls (OR=3.8, p=0.04). Race, education, and visual acuity were important predictors of reading impairment.
Conclusions
High rates of spoken reading impairment were found throughout this elderly sample. Glaucoma was associated with slower reading and increased reading impairment with advanced bilateral field loss.
INTRODUCTION
Glaucoma affects 2% of U.S. adults over 40,1 and as many as 10% are glaucoma suspects.2 Determining who should be treated requires we understand when and how glaucoma produces disability. Classically, glaucoma was believed to have little functional significance except in advanced disease. However, little direct evidence exists to tell us when glaucoma produces vision-related disability.
Questionnaire-based studies, in which impairment is inferred from self-described visual difficulty, have been the most common approach to evaluate glaucoma-related impairment.3–5 Subjects report difficulties in many activities even when field loss is not severe. For example, though reading relies on central acuity more than the peripheral visual field (VF),6 one study found self-reported reading impairment with only 6 dB of unilateral VF loss.7 Such research offers important insight into perceived impairment, but confirmation of true disability through functional testing is lacking.
The Salisbury Eye Evaluation (SEE) was undertaken amongst the elderly residents of Salisbury, Maryland to directly test when eye disease produces disability.8 Previous analysis from this study population, for example, showed little impact of glaucoma on mobility until VF loss was bilateral.9 Here, we evaluate when and how glaucoma affects spoken reading speed in this population of older Americans.
METHODS
The protocol for round 4 of SEE was approved by the Johns Hopkins IRB. Data were collected between August 2001 and July 2003. Participants gave written informed consent prior to testing. All subjects had participated in earlier rounds of SEE, and were age 65–84 when the study began in 1993. Further description of subject enrollment is described elsewhere.10, 11
Testing of Visual function
Vision testing was performed under binocular conditions using the Early Treatment Diabetic Retinopathy Study chart transilluminated at 130 candelas/m2. Habitual correction was selected to most accurately reflect true daily visual function. Visual acuity was converted to logMAR units. Contrast sensitivity was measured for each eye as the number of letters correctly read on the Pelli-Robson chart with best correction.
Defining Glaucoma Status
All subjects were first evaluated for glaucoma through a screening examination. Subjects with suspicious findings returned for a definitive examination performed by a glaucoma specialist (DSF). Detailed description of the procedures used to determine glaucoma status have been previously described.9, 12
Screening Examination
All subjects able to attend the research site underwent VF testing using the Swedish interactive thresholding algorithm (SITA) fast 24-2 testing algorithm on the Humphrey Field Analyzer II (HFA2, Zeiss-Humphrey Systems, Dublin, CA). VF testing was repeated for abnormally high sensitivity, generalized sensitivity reduction, pattern standard deviation abnormality ( p<0.05), or borderline or abnormal glaucoma hemifield test classification. Dilated images of the optic nerve were obtained using the Discam camera (Marcher Enterprises Ltd., Hereford, United Kingdom). Patients who could not be imaged had a vertical cup-to-disc ratio recorded by the examiner. Recorded cup-to-disc ratios correlated highly with ratios measured from Discam images.9
Definitive glaucoma examination
Subjects meeting referral criteria12 returned for a second evaluation, which included repeat SITA fast VF testing on a HFA2, gonioscopy, dilated exam, and optic nerve photographs with a stereo fundus camera (Topcon America Corp., Paramus, NJ).
Glaucoma classification
Two glaucoma specialists (HDJ and DSF) reviewed the VF data, optic nerve images and medical records, and independently classified each patient as definite, probable, possible, or no glaucoma using consensus criteria.13–18 Disagreements were addressed by first having each reviewer re-evaluate the case, and then by open discussion of the case.
Glaucomatous optic nerve damage (excavation and neuroretinal rim loss) along with a clear VF defect was defined as definite glaucoma. Less certain glaucomatous VF loss and optic nerve features consistent with glaucoma (excavation, thinning of the neuroretinal rim, large cup-to-disc, or cup-to-disc ratio asymmetry) was classified as probable glaucoma. Lesser findings in the VFs and/or optic nerves were classified as possible or no glaucoma. Eyes were defined as having glaucoma if when graded as definite or probable glaucoma. All others were defined as having no glaucoma. Eyes with glaucoma were classified as having open angle, angle closure or secondary glaucoma. Eyes with secondary glaucoma were excluded.12
Clinic Examination and History
All participants completed standardized forms detailing demographic information (age, gender, race, education). Participants were asked if a physician had diagnosed them with a list of 15 medical conditions. The total number of these conditions was calculated as an overall measure of co-morbidity. Depressive symptoms were evaluated using part D of the General Health Questionnaire,19 with a positive response to any depression-related question indicating the presence of depressive symptoms. Cognition was assessed using the Mini-mental state exam (MMSE),20 with outputs graded by a possible score between 0 and 30.
Evaluation of Reading Speed
Reading speed was tested in room lighting between 400 and 600 lux.8 Reading material was at 6th–9th grade level. Subjects read aloud short passages of non-scrolling text displayed on a computer screen. Words extended across several lines, and subjects were asked to read the material as quickly as possible. The number of correctly stated words read over 15 seconds was used to calculate the reading speed. Words read incorrectly or out of order were not counted. Reading speed was evaluated for 4 text sizes ranging from 0.131° (pharmacy label print) to 0.525° (small newspaper heading size). Statistical analysis focused primarily on reading speed for 0.26° print (newspaper print size).
Statistical Analysis
Linear associations between reading speed and continuous covariates were verified by superimposing linear fit and lowess models. Binocular acuity required log transformation to achieve a linear relationship with reading speed. Reading speed increased linearly with education levels up to 14 years, but was flat for greater values. Education was analyzed as a simple linear covariate, as nearly identical were observed when a linear spline term was introduced.
The impact of glaucoma on spoken reading speed and reading impairment was determined through univariate analyses and multivariable linear and logistic regression. Reading impairment was defined as a reading speed less than 90 words/minute, below which fluent reading is difficult.21 Variables included in multivariable analysis were selected using a pre-determined model of factors believed to influence reading speed, and incorporating factors identified in age-adjusted bivariable analyses.
VF tests were classified as reliable or unreliable using the revised criteria from the Ocular Hypertension Treatment Study.22 The first VF was chosen for analysis except when the second, but not the first, VF was reliable. Mean deviations ≥ +2 dB were converted to +2 dB in the analysis. Subjects who completed a VF in only one eye, and who had a best corrected acuity worse than 20/100 in the second eye, were assigned a mean deviation of −30 dB for the second eye.
RESULTS
1,253 individuals participated in round 4 of SEE, and glaucoma status was defined for 1,214 subjects (96.9%). Seventy-six subjects (6.3%) had unilateral glaucoma, and 74 (6.1%) had bilateral glaucoma. The reading evaluation was completed by 1,154 subjects 190 with known glaucoma status (95.1%). Subjects not performing the reading test were older, less educated and more cognitively impaired. Additionally, they had more depressive symptoms, worse acuity, and lower contrast sensitivity, and were more often male and African-American (Table 1). Subjects with bilateral, but not unilateral, glaucoma completed the reading evaluation less frequently than non-glaucoma controls (86.5% vs. 95.6%, p=0.001). Of the 10 bilateral glaucoma subjects not participating in the reading evaluation, 7 had binocular acuities of 20/40 or better, while 3 had binocular acuities of 20/100 or worse. Six subjects (5 with unilateral and 1 with bilateral glaucoma) had secondary glaucoma and were excluded from subsequent analyses.
Table 1.
Characteristics of Salisbury Eye Evaluation round 4 subjects by participation in reading evaluation.
| Characteristic | Participated (n=1154) | Did not participate (n=60) | p value |
|---|---|---|---|
| Age, mean (SD) | 79.7 (4.5) | 80.9 (4.7) | 0.04 |
| Male, % | 39.9 | 50.0 | 0.03 |
| African American, % | 22.1 | 50.0 | 0.02 |
| Last Grade Completed, mean (SD) | 11.8 (3.2) | 8.2 (4.5) | <0.001 |
| MMSE score, mean (SD) | 26.0 (3.3) | 20.2 (5.6) | <0.001 |
| Depressive symptoms, % | 6.9 | 15.0 | 0.02 |
| # comorbid conditions, mean (SD) | 2.2 (1.5) | 2.2 (1.5) | 0.90 |
| LogMAR Acuity, mean (SD) | 0.06 (0.21) | 0.27 (0.43) | <0.001 |
| Contrast Sensitivity, mean (SD) | 33.0 (4.3) | 27.5 (10.7) | <0.001 |
| Glaucoma Status, # subjects (% total) | |||
| None | 1017 (95.6) | 47 (4.4) | REF |
| Unilateral | 73 (96.1) | 3 (3.9) | 0.76 |
| Bilateral | 64 (86.5) | 10 (13.5) | 0.003 |
SD = Standard deviation; MMSE = Mini-mental state examination; LogMAR Acuity = logarithm of the minimal angle of resolution. Acuity refers to binocular acuity with habitual correction.
Contrast sensitivity expressed as number of letters correctly read on Pelli-Robson chart in better eye with best correction.
Age was tested using the Student’s t-test; all others reflect p values for odds of participation in bivariable logistic regression model with age.
Compared to non-glaucoma controls of similar age, bilateral glaucoma subjects had lower acuity and MMSE scores, and were twice as likely to be African-American (Table 2). Unilateral, but not bilateral, glaucoma subjects were more frequently male than non-glaucoma controls. Both unilateral and bilateral glaucoma subjects were older and had worse contrast sensitivity and VF loss than controls. Subjects with unilateral and bilateral glaucoma were not significantly different than controls with regards to education, depressive symptoms, and medical comorbidity.
Table 2.
Characteristics of Salisbury Eye Evaluation round 4 subjects who completed the reading evaluation analyzed by glaucoma status.
| Characteristic | No Glaucoma (n=1017) | Unilateral Glaucoma (n=68) | Bilateral Glaucoma (n=64) |
|---|---|---|---|
| Age, mean (SD) | 79.5 (4.5) | 80.8 (4.3)1 | 81.2 (4.6)2 |
| Male gender, % | 39.3 | 51.51 | 37.5 |
| African American, % | 20.0 | 25.0 | 51.63 |
| Last grade completed, mea (SD) | 11.9 (3.1) | 11.7 (3.2) | 11.2 (3.8) |
| MMSE score, mean (SD) | 26.1 (3.2) | 26 (2.8) | 24.5 (3.8)3 |
| Depressive symptoms, % | 6.8 | 10.3 | 4.7 |
| # comorbid conditions, mean (SD) | 2.2 (1.4) | 2.2 (1.5) | 2.5 (1.7) |
| LogMAR acuity, mean (SD) | 0.05 (0.20) | 0.11 (0.26) | 0.13 (0.27)1 |
| CS, worse eye, mean (SD) | 30.2 (7.5) | 26.1 (10.1)3 | 24.5 (10.5)3 |
| CS, better eye, mean (SD) | 33.4 (3.9) | 31.6 (4.9)2 | 29.4 (6.4)3 |
| MD worse eye, dB (SD) | −4.0 (6.2) | −8.5 (7.6)3 | −12.7 (9.5)3 |
| MD better eye, dB (SD) | −1.6 (3.8) | −3.4 (4.8)3 | −8.8 (9.1)3 |
SD = standard deviation; MMSE = Mini-mental state examination; logMAR = logarithm of the minimal angle of resolution; CS = contrast sensitivity; MD =mean deviation.
Acuity refers to binocular acuity with habitual correction.
Contrast sensitivity expressed as number of letters correctly read on Pelli-Robson chart in better eye with best correction.
P ≤ 0.05
P ≤ 0.01
P ≤ 0.001 when compared to no glaucoma group.
Age was tested with student’s t-test; all others reflect age-adjusted p-values derived from bivariable linear or logistic regression.
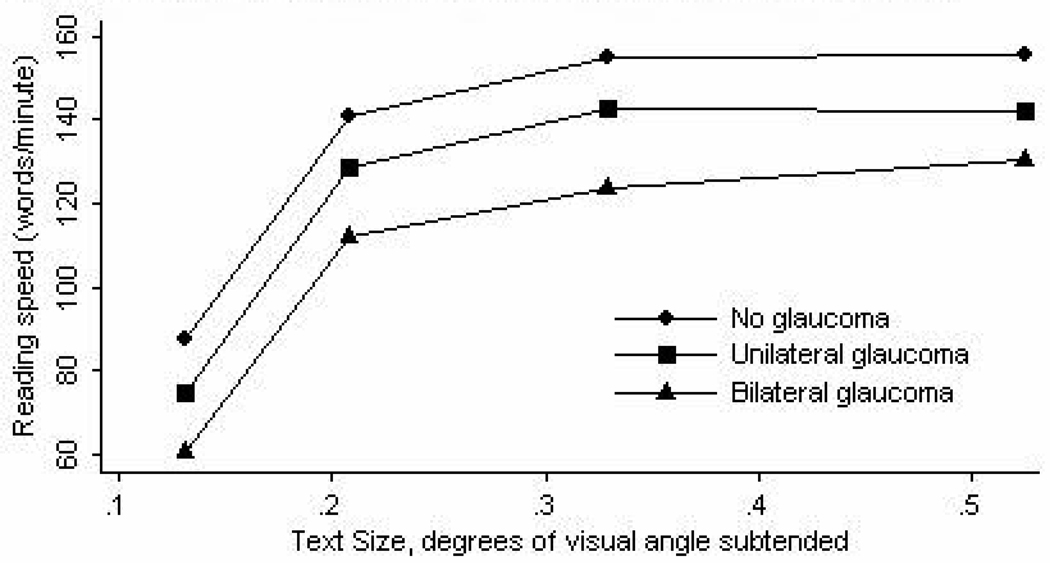
Reading speed for newspaper-sized text was first calculated by glaucoma status in a univariate analysis (Table 3). Subjects with unilateral glaucoma showed similar reading speeds and odds of reading impairment when compared to subjects without glaucoma. Subjects with bilateral glaucoma read 29 words/minute slower than those without glaucoma (p<0.001), and had roughly twice the odds of reading impairment (p=0.006). In all subjects, reading speed increased across evaluated text sizes (Figure 1). To confirm that differences in reading speed were not specific for a single text size, univariate analyses were repeated using individual subjects’ best reading speed (the highest reading speed for all tested text sizes). Lower reading speeds and higher odds of impairment were again observed for subjects with bilateral, but not unilateral, glaucoma (Table 3). Reading speed also decreased with black race, lower education, impaired cognition (lower MMSE score), more medical comorbidities, depressive symptoms, and lower binocular acuity (Table 4).
Table 3.
Reading outcomes by glaucoma status in the fourth round of the Salisbury Eye Evaluation, univariate analysis.
| Size 2 Text | Best Read Text | |||||||
|---|---|---|---|---|---|---|---|---|
| Glaucoma Status | Reading speed, words/min (SD) |
p value | Reading impaired (%) |
p value | Reading speed words/min (SD) |
p value | Reading impaired (%) |
p value |
| None | 141 (56) | REF | 16.7 | REF | 168 (48) | REF | 7.0 | REF |
| Unilateral | 130 (65) | 0.12 | 22.1 | 0.26 | 158 (53) | 0.11 | 10.3 | 0.3 |
| Bilateral | 112 (69) | <0.001 | 32.8* | 0.001 | 141 (64) | <0.001 | 21.9* | <0.001 |
min = minute; SD = standard deviation.
Size 2 text corresponds to newspaper sized print.
Best-read text refers to the text read most quickly for a given subject.
Reading impairment defined as a reading speed ≤ 90 words/minute.
Frequency of reading impairment increases to 35.8% for size 2 text, and 25.4% if the 3 bilateral glaucoma subjects with binocular acuity of 20/100 or worse, and who did not participate in the reading test, are assumed to be reading impaired.
Figure 1. Reading speed vs. text size by glaucoma status.
Table 4.
Impact of demographic, health-related, and vision-related variables on reading speed amongst participants of the Salisbury Eye Evaluation fourth round, age-adjusted analysis.
| Reading Speed (words/minute) |
Reading Impairment | ||||||
|---|---|---|---|---|---|---|---|
| Variable | Increment | β | 95% CI | p value | OR | 95% CI | P value |
| Age | +5 years | −15 | −19 to −11 | <0.001 | 1.5 | 1.3 to 1.8 | <0.001 |
| Race | Black | −41 | −48 to −33 | <0.001 | 4.0 | 2.9 to 5.6 | <0.001 |
| Education level | +4 years | 26 | 22 to 30 | <0.001 | 0.38 | 0.31 to 0.47 | <0.001 |
| MMSE score | +5 points | 35 | 31 to 40 | <0.001 | 0.30 | 0.24 to 0.38 | <0.001 |
| Number comorbidities | +1 | −4 | −7 to −2 | <0.001 | 1.1 | 1.0 to 1.3 | 0.01 |
| Depressive symptoms | Yes | −21 | −34 to −9 | 0.001 | 2.2 | 1.3 to 3.6 | 0.002 |
| Visual Acuity | +0.1 logMAR | −17 | −18 to −15 | <0.001 | 2.4 | 2.1 to 2.8 | <0.001 |
| Mean deviation | +1 dB | ||||||
| Better Eye | 5.3 | 4.7 to 6.0 | <0.001 | 0.82 | 0.79 to 0.86 | <0.001 | |
| Worse Eye | 3.6 | 3.1 to 4.0 | <0.001 | 0.89 | 0.87 to 0.91 | <0.001 | |
| Contrast Sensitivity | +5 letters | ||||||
| Better Eye | 39 | 36 to 42 | <0.001 | 0.11 | 0.09 to 0.17 | <0.001 | |
| Worse Eye | 18 | 16 to 20 | <0.001 | 0.43 | 0.48 to 0.59 | <0.001 | |
OR = Odds ratio; MMSE – Mini-mental state examination, logMAR = logarithm of the minimal angle of resolution for binocular acuity with habitual correction.
β values were derived from a univariate regression for age, and from bivariable linear regression analyses including age for all other variables. Odds ratios were determined from simple logistic regression analysis for age, and from bivariable logistic regression analyses including age for all other variables.
Multivariable regression models evaluating reading speed as a function of glaucoma, age, race, education, and MMSE score demonstrated no difference in reading speed for subjects with unilateral (95% CI = −18 to 6 words/minute, p=0.3), or bilateral glaucoma (95% CI = −22 to 4 words/minute, p=0.16) when compared to subjects without glaucoma (Table 5). Subjects with unilateral or bilateral glaucoma demonstrated similar odds of reading impairment when compared to non-glaucoma subjects (p≥0.4 for both).
Table 5.
Outcomes of multivariable regression analyses modeling reading speed on glaucoma status and demographic, healthrelated, and vision-related variables in round 4 of the Salisbury Eye Evaluation.
| Reading Speed (words/minute) | Reading Impairment | ||||||
|---|---|---|---|---|---|---|---|
| Variable | Increment | β | 95% CI | p | OR | 95% CI | p |
| A. Variables tested from simplified regression models* | |||||||
| Glaucoma Status | |||||||
| None | REF | - | - | REF | - | - | |
| Unilateral | Yes | −6 | −18 to 6 | 0.3 | 1.2 | 0.6 to 2.4 | 0.6 |
| Bilateral | Yes | −9 | −22 to 4 | 0.16 | 1.3 | 0.7 to 2.6 | 0.4 |
| Bilateral, highest quartile better-eye VF damage |
Yes | −32† | −56 to −7 | 0.01 | 3.8 | 1.1 to 13.1 | 0.04 |
| B. Variables derived from complete regression model** | |||||||
| Age | +5 years | −3 | −6 to 0 | 0.06 | 1.2 | 0.7 to 1.9 | 0.5 |
| Race | Black | −24 | −30 to −18 | <0.001 | 2.7 | 1.7 to 4.4 | <0.001 |
| Education level | +4 years | 10 | 7 to 13 | <0.001 | 0.67 | 0.52 to 0.88 | 0.003 |
| MMSE score | +5 points | 19 | 14 to 23 | <0.001 | 0.80 | 0.59 to 1.08 | 0.15 |
| Number comorbidities | +1 | −2 | −3 to 0 | 0.03 | 1.1 | 0.96 to 1.26 | 0.14 |
| Depressive symptoms | Yes | 4 | −6 to 13 | 0.7 | 0.65 | 0.29 to 1.43 | 0.3 |
| Visual Acuity, logMAR | +0.1 | −15 | −16 to −14 | <0.001 | 1.8 | 1.6 to 2.0 | <0.001 |
OR = Odds ratio; MMSE – Mini-mental state examination, logMAR = logarithm of the minimal angle of resolution for binocular acuity with habitual correction.
β values were derived from multiple linear regression analysis. Odds ratios were determined from multiple logistic regression analysis.
Results were obtained from regression models designed to determine the effect of glaucoma. To allow comparison of glaucoma subjects to non-glaucoma controls, each glaucoma groups was tested in a separate model. All models included age, race, MMSE score and education as covariates.
Results are derived from a complete regression model designed to predict reading speed and impairment.
Effect eliminated (β=+4, p=0.7) when visual acuity is incorporated into the regression model.
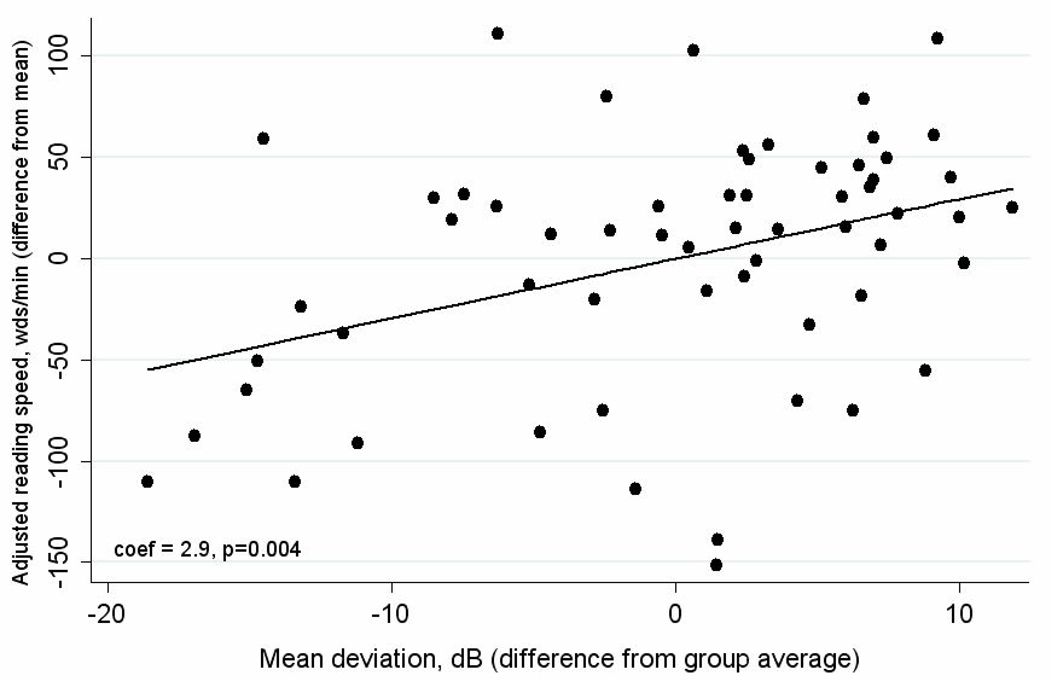
To assess whether impairment might occur only in those with severe bilateral glaucoma, regression models were created to assess the effect of better-eye mean deviation on reading speed. As VF loss may affect reading through acuity, models were constructed with and without visual acuity. Reading speed decreased with better-eye mean deviation (β=−2.9 words/min/dB VF loss, p=0.004) without acuity in the model (Figure 2). This effect disappeared (p>0.8) with acuity in the model, suggesting that the effect of field loss on reading speed is mediated through loss of visual acuity. We also analyzed reading speed in bilateral glaucoma subjects by quartile of better-eye VF loss. In order of most severe to least severe, reading speeds were 74, 118, 120, and 147 words/minute while average better-eye mean deviations were −22.5, −8.5, −3.6 and −0.7 dB. Multivariable regression models demonstrated that, for the most severely affected quartile of bilateral glaucoma subjects, reading speed was 32 words/minute slower than subjects without glaucoma (95% CI = −56 to −7 words/minute, p=0.01), and the odds of reading impairment were 3.8 fold higher (95% CI = 1.1 to 13.1, p=0.04). Small, non-significant effects on reading speed were noted when binocular acuity was added to the model, when subjects in the middle 2 quartiles of VF loss were analyzed, or when the most severely affected quartile of unilateral glaucoma subjects were affected (p>0.4 for all).
Figure 2. Reading speed vs. mean deviation in bilateral glaucoma (n=60).
Mean reading speed for these subjects was 115 words/minute, and average better-eye mean deviation was −8.8 dB.
An additional multivariable model was constructed to define the most important predictors of reading speed and impairment (Table 5). This model included all variables believed to be predictive of reading speed from the age-adjusted analysis, including those which did not necessarily confound the association between glaucoma and reading. In this model, black race, education level and visual acuity were important predictors of reading speed and reading impairment, while lower MMSE score and medical comorbidities were associated with lower reading speeds, though not with higher odds of reading impairment.
DISCUSSION
In this population-based sample of elderly Americans, spoken reading speed was not affected by glaucoma until disease was bilateral with advanced field loss (mean deviation ≤−17 dB) in both eyes. This level of glaucoma damage occurred in roughly 10% of glaucoma subjects, and nearly 1% of all participants. The effect of VF loss on spoken reading speed did not persist independent of visual acuity, suggesting that glaucoma affects reading through visual acuity lost from central field damage.
In the present study, reading impairment occurred at a higher level of glaucomatous VF loss than suggested by questionnaire-based studies.4, 23–32 Such studies evaluated subjects with broadly-distributed unilateral and bilateral VF loss, and consistently reported statistically significant correlations between the presence and/or extent of glaucoma and self-reported reading impairment. Two large population-based studies, one from the current cohort23 and one from the Los Angeles Latino Eye Study,24 both reported that near-vision tasks such as reading were affected in persons with bilateral glaucoma, with little24 or no23 impairment in those with unilateral glaucoma. Our results, however, suggest that spoken reading is only affected in those with advanced bilateral disease.
In deciding when reading is truly affected by glaucoma, we feel that our findings deserve more weight, as direct measurement of reading function avoids many of the problems inherent in questionnaire-based research. Questionnaire-based studies generally group reading with other near vision activities, whereas reading was studied as an isolated activity in our study. Additionally, the clinical relevance of self reported visual disability is difficult to gauge in questionnaire-based work, as score values hold little inherent meaning. In contrast, our work provides direct measures of reading speed and impairment, allowing for a more meaningful comparison between groups. Finally, direct functional assessment avoids the potential for information bias inherent in questionnaire-based studies, in which awareness of an eye disease or blurry vision from an undiagnosed condition may result in poorer ratings of visual function even when performance remains unaffected.
Our finding that glaucoma only affects reading speed when field loss is bilateral and severe corroborates the idea that reading is primarily a task of central vision, and would be unlikely to be affected except in patients with VF loss near fixation. Indeed, studies in normal subjects have found normal reading speeds with central windows of vision only four characters wide.6 Decreased contrast sensitivity resulting from glaucoma may also worsen reading, though normal individuals tolerate contrast reduction up to ten-fold with little effect on reading speed, suggesting that only the most advanced glaucoma would affect reading speed through contrast sensitivity loss.33
Our evaluation of reading does not fully recapitulate reading under normal conditions, leaving open the possibility that physiological reading is more affected by glaucoma than observed in the current study. Patients read straight ahead instead of looking down towards a page, which may minimize the impact of inferior VF loss. Additionally, material was presented as dark letters against a bright white screen, creating a higher level of contrast than normally present. Reading speed was measured for short durations, and may have missed the impact of fatigue incurred by glaucoma patients. Reading also involves tasks not measured in standard reading tests such as scanning documents for relevant text, and skimming documents for quick assimilation of information. Performing these tasks may require a greater functional field of vision than straight ahead reading, and might result in self-reported reading difficulties. Finally, non-participants in the reading test more frequently had characteristics of slower readers, suggesting that many of the poorest readers may have been excluded from our analysis. The bilateral glaucoma group had greater numbers of non-participants, suggesting that the true reading speed in this group may be lower than reported. Analysis of this group suggests that most of the non-participation in this group is a result of advanced cognitive impairment, though three subjects likely did not participate because of poor binocular central acuity.
We identified several additional variables which significantly affected spoken reading speed. While age had a substantial effect on reading speed in the univariate analysis, multivariable analysis demonstrated only a borderline impact for age itself, but significant impacts for age-related variables such as cognition and medical comorbidity. Lower levels of education were associated with slower reading speeds, and race persisted as a significant predictor of reading speed even after adjusting for education. Elderly African-Americans likely received a lower quality education, possibly accounting for the slower reading in blacks independent of education level. As reading out loud was necessary to measure reading speed, racial differences in speaking rates could account for the difference in the measured reading rate, though patients were asked to read passages as quickly as they could. As previously reported,8 visual acuity remained the most significant predictor of reading speed, with reading speed decreasing 15 words/minute, and the odds of reading impairment increasing nearly 80% for each 0.1 logMAR unit (corresponding to roughly 1 line of Snellen acuity).
These data from a population-based, elderly sample demonstrate high overall rates of reading impairment, with 1 in 8 white subjects and 1 in 3 African-American subjects reading impaired. Regression analyses demonstrate no impact of glaucoma on spoken reading speed until the disease is bilateral with severe VF loss in both eyes. Future work should evaluate reading in glaucoma subjects under more realistic conditions to further explore if reading impairment is more prevalent than reported here.
ACKNOWLEDGMENTS
Thanks to Dr. Harry A. Quigley for his critical comments on the manuscript. This work was supported by NIH grants EY01765, AG10184, and EY015025.
REFERENCES
- 1.Friedman DS, Wolfs RC, O'Colmain BJ, Klein BE, Taylor HR, West S, Leske MC, Mitchell P, Congdon N, Kempen J Eye Diseases Prevalence Research Group. Prevalence of open-angle glaucoma among adults in the United States. Arch Ophthalmol. 2004;122(4):532–538. doi: 10.1001/archopht.122.4.532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leibowitz HM, Krueger DE, Maunder LR, Milton RC, Kini MM, Kahn HA, Nickerson RJ, Pool J, Colton TL, Ganley JP, Loewenstein JI, Dawber TR. The Framingham Eye Study monograph: An ophthalmological and epidemiological study of cataract, glaucoma, diabetic retinopathy, macular degeneration, and visual acuity in a general population of 2631 adults, 1973–1975. 1980;24 Suppl:335–610. [PubMed] [Google Scholar]
- 3.Gutierrez P, Wilson MR, Johnson C, Gordon M, Cioffi GA, Ritch R, Sherwood M, Meng K, Mangione CM. Influence of glaucomatous visual field loss on health-related quality of life. Arch Ophthalmol. 1997;115(6):777–784. doi: 10.1001/archopht.1997.01100150779014. [DOI] [PubMed] [Google Scholar]
- 4.Parrish RK., 2nd Visual impairment, visual functioning, and quality of life assessments in patients with glaucoma. Trans Am Ophthalmol Soc. 1996:94919–1028. [PMC free article] [PubMed] [Google Scholar]
- 5.Spaeth G, Walt J, Keener J. Evaluation of quality of life for patients with glaucoma. Am J Ophthalmol. 2006;141(1 Suppl):S3–S14. doi: 10.1016/j.ajo.2005.07.075. [DOI] [PubMed] [Google Scholar]
- 6.Legge GE, Pelli DG, Rubin GS, Schleske MM. Psychophysics of reading--I. Normal vision. Vision Res. 1985;25(2):239–252. doi: 10.1016/0042-6989(85)90117-8. [DOI] [PubMed] [Google Scholar]
- 7.McKean-Cowdin R, Wang Y, Wu J, Azen SP, Varma R Los Angeles Latino Eye Study Group. Impact of Visual Field Loss on Health-Related Quality of Life in Glaucoma The Los Angeles Latino Eye Study. Ophthalmology. 2007 doi: 10.1016/j.ophtha.2007.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.West SK, Rubin GS, Broman AT, Munoz B, Bandeen-Roche K, Turano K. How does visual impairment affect performance on tasks of everyday life? The SEE Project. Salisbury Eye Evaluation. 2002;120(6):774–780. doi: 10.1001/archopht.120.6.774. [DOI] [PubMed] [Google Scholar]
- 9.Friedman DS, Freeman E, Munoz B, Jampel HD, West SK. Glaucoma and mobility performance: the Salisbury Eye Evaluation Project. Ophthalmology. 2007;114(12):2232–2237. doi: 10.1016/j.ophtha.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 10.Rubin GS, West SK, Munoz B, Bandeen-Roche K, Zeger S, Schein O, Fried LP. A comprehensive assessment of visual impairment in a population of older Americans. The SEE Study. Salisbury Eye Evaluation Project. Invest Ophthalmol Vis Sci. 1997;38(3):557–568. [PubMed] [Google Scholar]
- 11.Munoz B, West S, Rubin GS, Schein OD, Fried LP, Bandeen-Roche K. Who participates in population based studies of visual impairment? The Salisbury Eye Evaluation project experience. Ann Epidemiol. 1999;9(1):53–59. doi: 10.1016/s1047-2797(98)00026-x. [DOI] [PubMed] [Google Scholar]
- 12.Friedman DS, Jampel HD, Munoz B, West SK. The prevalence of open-angle glaucoma among blacks and whites 73 years and older: the Salisbury Eye Evaluation Glaucoma Study. Arch Ophthalmol. 2006;124(11):1625–1630. doi: 10.1001/archopht.124.11.1625. [DOI] [PubMed] [Google Scholar]
- 13.Tielsch JM, Sommer A, Katz J, Royall RM, Quigley HA, Javitt J. Racial variations in the prevalence of primary open-angle glaucoma. The Baltimore Eye Survey. JAMA. 1991;266(3):369–374. [PubMed] [Google Scholar]
- 14.Varma R, Ying-Lai M, Francis BA, Nguyen BB, Deneen J, Wilson MR, Azen SP. Prevalence of open-angle glaucoma and ocular hypertension in Latinos: the Los Angeles Latino Eye Study. 2004;111(8):1439–1448. doi: 10.1016/j.ophtha.2004.01.025. [DOI] [PubMed] [Google Scholar]
- 15.Coffey M, Reidy A, Wormald R, Xian WX, Wright L, Courtney P. Prevalence of glaucoma in the west of Ireland. 1993;77(1):17–21. doi: 10.1136/bjo.77.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dielemans I, Vingerling JR, Wolfs RC, Hofman A, Grobbee DE, de Jong PT. The prevalence of primary open-angle glaucoma in a population-based study in The Netherlands. The Rotterdam Study. 1994;101(11):1851–1855. doi: 10.1016/s0161-6420(94)31090-6. [DOI] [PubMed] [Google Scholar]
- 17.Leske MC, Connell AM, Schachat AP, Hyman L. The Barbados Eye Study. Prevalence of open angle glaucoma. 1994;112(6):821–829. doi: 10.1001/archopht.1994.01090180121046. [DOI] [PubMed] [Google Scholar]
- 18.Mitchell P, Smith W, Attebo K, Healey PR. Prevalence of open-angle glaucoma in Australia. The Blue Mountains Eye Study. 1996;103(10):1661–1669. doi: 10.1016/s0161-6420(96)30449-1. [DOI] [PubMed] [Google Scholar]
- 19.Goldberg DP, Hillier VF. A scaled version of the General Health Questionnaire. Psychol Med. 1979;9(1):139–145. doi: 10.1017/s0033291700021644. [DOI] [PubMed] [Google Scholar]
- 20.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 21.Whittaker SG, Lovie-Kitchin J. Visual requirements for reading. Optom Vis Sci. 1993;70(1):54–65. doi: 10.1097/00006324-199301000-00010. [DOI] [PubMed] [Google Scholar]
- 22.Keltner JL, Johnson CA, Cello KE, Bandermann SE, Fan J, Levine RA, Kass MA, Gordon MO Ocular Hypertension Treatment Study Group. Visual field quality control in the Ocular Hypertension Treatment Study (OHTS) J Glaucoma. 2007;16(8):665–669. doi: 10.1097/IJG.0b013e318057526d. [DOI] [PubMed] [Google Scholar]
- 23.Freeman EE, Munoz B, West SK, Jampel HD, Friedman DS. Glaucoma and Quality of Life. The Salisbury Eye Evaluation. doi: 10.1016/j.ophtha.2007.04.050. In press. [DOI] [PubMed] [Google Scholar]
- 24.Los Angeles Latino Eye Study Group. McKean-Cowdin R, Varma R, Wu J, Hays RD, Azen SP. Severity of visual field loss and health-related quality of life. Am J Ophthalmol. 2007;143(6):1013–1023. doi: 10.1016/j.ajo.2007.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nelson P, Aspinall P, Papasouliotis O, Worton B, O'Brien C. Quality of life in glaucoma and its relationship with visual function. J Glaucoma. 2003;12(2):139–150. doi: 10.1097/00061198-200304000-00009. [DOI] [PubMed] [Google Scholar]
- 26.Sherwood MB, Garcia-Siekavizza A, Meltzer MI, Hebert A, Burns AF, McGorray S. Glaucoma's impact on quality of life and its relation to clinical indicators. A pilot study. Ophthalmology. 1998;105(3):561–566. doi: 10.1016/S0161-6420(98)93043-3. [DOI] [PubMed] [Google Scholar]
- 27.Bechetoille A, Arnould B, Bron A, Baudouin C, Renard JP, Sellem E, Brouquet Y, Denis P, Nordmann JP, Rigeade MC, Bassols A, Benmedjahed K, Guillemin I, Rouland JF. Measurement of health-related quality of life with glaucoma: validation of the Glau-QoL(c) 36-item questionnaire. Acta Ophthalmol Scand. 2007 doi: 10.1111/j.1600-0420.2007.00999.x. [DOI] [PubMed] [Google Scholar]
- 28.Mills RP. Correlation of quality of life with clinical symptoms and signs at the time of glaucoma diagnosis. Trans Am Ophthalmol Soc. 1998:96753–96812. [PMC free article] [PubMed] [Google Scholar]
- 29.Mills RP, Janz NK, Wren PA, Guire KE. Correlation of visual field with quality-of-life measures at diagnosis in the Collaborative Initial Glaucoma Treatment Study (CIGTS) J Glaucoma. 2001;10(3):192–198. doi: 10.1097/00061198-200106000-00008. [DOI] [PubMed] [Google Scholar]
- 30.Broman AT, Munoz B, Rodriguez J, Sanchez R, Quigley HA, Klein R, Snyder R, West SK. The impact of visual impairment and eye disease on vision-related quality of life in a Mexican-American population: proyecto VER. 2002;43(11):3393–3398. [PubMed] [Google Scholar]
- 31.Janz NK, Wren PA, Lichter PR, Musch DC, Gillespie BW, Guire KE. Quality of life in newly diagnosed glaucoma patients : The Collaborative Initial Glaucoma Treatment Study. Ophthalmology. 2001;108(5):887–897. doi: 10.1016/s0161-6420(00)00624-2. discussion 898. [DOI] [PubMed] [Google Scholar]
- 32.Ringsdorf L, McGwin G, Jr, Owsley C. Visual field defects and vision-specific health-related quality of life in African Americans and whites with glaucoma. J Glaucoma. 2006;15(5):414–418. doi: 10.1097/01.ijg.0000212252.72207.c2. [DOI] [PubMed] [Google Scholar]
- 33.Legge GE, Rubin GS, Luebker A. Psychophysics of reading--V. The role of contrast in normal vision. Vision Res. 1987;27(7):1165–1177. doi: 10.1016/0042-6989(87)90028-9. [DOI] [PubMed] [Google Scholar]