Abstract
Objectives
To measure the prevalence, predictors and post-hospitalization outcomes associated with the overlap syndrome of coexisting depression and incident delirium in older hospitalized patients.
Design
Secondary analysis of prospective cohort data from the control group of the Delirium Prevention Trial.
Setting
General medical service of an academic medical center. Follow-up interviews at one month and one year post-hospital discharge.
Participants
Four hundred and fifty nine patients aged 70 and over who were not delirious at hospital admission.
Measurements
Depressive symptoms assessed at hospital admission using the 15-item Geriatric Depression Scale (cutoff score of 6 used to define depression), daily assessments of incident delirium from admission to discharge using the Confusion Assessment Method. Activities of daily living at admission and one month post-discharge. New nursing home placement and mortality determined at one year.
Results
Of 459 participants, 23 (5%) had the overlap syndrome, 39 (9%) delirium alone, 121 (26%) depression alone and 276 (60%) neither condition. In adjusted analysis, patients with the overlap syndrome had higher odds of new nursing home placement or death at one year (adjusted odds ratio [AOR] 5.38, 95% confidence interval [CI] = 1.57– 18.38) and one month functional decline (AOR 3.30, 95% CI = 1.14–9.56) compared to patients with neither condition.
Conclusion
The overlap syndrome of depression and delirium is associated with significant risk of functional decline, institutionalization and death. Efforts to identify, prevent and treat this condition may reduce the risk of adverse outcomes in older hospitalized patients.
Keywords: Delirium, depression, mortality, nursing home placement
INTRODUCTION
Depressive symptoms are common in elderly hospitalized patients, with significant symptom levels occurring in 10 to 44% of patients.1–4 The presence of depressive symptoms during hospitalization is associated with adverse outcomes, a finding initially noted among select patient groups such as those with acute myocardial infarction.5,6 It is now recognized that among elderly patients hospitalized with a range of medical diagnoses, those with depressive symptoms are at increased risk of poor post-hospitalization outcomes including worse physical and mental health7, functional decline4 and increased mortality.2,8,9
Delirium, defined as an acute disorder of attention and global cognitive functioning, also occurs commonly in elderly hospitalized patients with prevalence estimates ranging from 12 to 31%.10–12 Delirium is known to be associated with adverse post-hospitalization outcomes including increased rates of functional decline,13,14 institutionalization13 and death.10,13,15,16
The presence of an overlap syndrome of depression and delirium in hospitalized patients has not been well studied, although depressive symptoms are an established risk factor for the development of delirium.17,18 Due to the high prevalence of depressive symptoms and delirium among elderly hospitalized patients and their association with poor post-hospitalization outcomes, the question of whether patients with an overlap of these two conditions are at even greater risk of adverse outcomes has clinical importance but has not been investigated previously. One prior study has found that the combination of depression and delirium, when combined with cognitive impairment, appears to worsen functional outcomes and rates of institutionalization and death among hip fracture patients.19
Our goal with this study was to close several gaps in current knowledge regarding the coexistence of depression and delirium among patients hospitalized on a medical service by assessing the prevalence and risk factors associated with this overlap syndrome, and by estimating the effect of this syndrome on the adverse outcomes of functional decline, nursing home placement and death. Our hypothesis was that patients with the overlap syndrome would have worse outcomes than those with either condition alone. Ultimately, we hoped that this study would identify a potentially high-risk group and lay the groundwork for future intervention studies to target this overlap syndrome.
METHODS
Sample
This study is a secondary analysis of data collected from patients in the control group of the Delirium Prevention Trial.11 Participants comprise a prospective cohort of consecutive patients aged 70 and over, admitted to the Yale New Haven Hospital general medical service from March 25, 1995 through March 18, 1998. Patients who were at intermediate or high risk of delirium but who were not delirious at admission were eligible to participate. The methodology of this study is described in more detail elsewhere.11 Over a three-year recruitment phase, 2434 potential participants were screened and 637 patients met inclusion criteria. Of these, 70 were excluded upon evaluation at hospital admission due to the presence of delirium or the inability to participate in interviews due to conditions such as profound dementia precluding reliable verbal communication, or aphasia. Operationally, if patients could not repeat critical information and demonstrate understanding of critical elements during the informed consent process for the study, they were not enrolled. Of 567 eligible patients admitted to the hospital, 469 agreed to participate and 461 survived hospitalization. Two participants were excluded due to lack of depression assessment upon admission, a primary predictor variable in our analysis, leaving 459 participants in our study sample. Informed consent for study participation was obtained from the patients or from a proxy (usually the closest relative or legal guardian) for those with substantial cognitive impairment, according to procedures approved by the institutional review board of the Yale University School of Medicine.
Assessments
All study assessments were conducted by research nurses or masters level interviewers with a minimum of five years experience in conducting research-related interviews in older adults.
Sociodemographic Characteristics
Baseline interviews at hospital admission provided information on self-reported patient age, sex, race, education, marital status and place of residence (nursing home vs. other).
Additional Covariates
History of depression and antidepressant use upon hospital admission were based on review of the hospital record.
Depression
Depressive symptoms were measured on admission using the 15-item Geriatric Depression Scale (GDS).20 Scores range from 0–15 with higher scores indicating more depressive symptoms. The 15-item GDS has a sensitivity of 92% and specificity of 81% using a cutoff score of five, for clinical diagnoses of major depression.21 The GDS has been shown to be a reliable measure of depressive symptoms even among those with cognitive impairment.22 We defined depression on hospital admission as a GDS score of 6 or greater, also a commonly used cutoff score,2,4,19 in order to increase the specificity of our depression designation.
Delirium
Patients were assessed upon admission and daily until hospital discharge for the presence of delirium using the confusion assessment method (CAM) diagnostic algorithm.11 The CAM is based on four criteria for delirium found in the Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised. Full criteria for delirium consist of: 1) acute onset and fluctuating course of symptoms, 2) inattention, and either 3) disorganized thinking or 4) altered level of consciousness. The CAM has been shown to have a sensitivity over 0.94 and specificity over 0.90 for psychiatric diagnosis of delirium in a sample of older hospitalized patients.23
The Overlap Syndrome of Depression and Delirium
We grouped participants according to the presence or absence of depression on admission and delirium during hospitalization. Four categories were created: 1) no depression or delirium, 2) depression alone, 3) delirium alone, 4) overlap syndrome of depression and delirium.
Mental Status, Functional Status, Medical Comorbidity
The Mini-Mental State Examination (MMSE)24 was administered at hospital admission to assess mental status. Scores range from 0 to 30 with higher scores indicating higher cognitive status. Self-reported functional status was assessed upon admission using the basic activities of daily living (ADL) scale (range 0–7, 0 best).25 Medical record abstraction was used to obtain the Charlson Comorbidity Index score26, antidepressant use prior to admission and history of depression.
Outcomes
Our outcomes were: 1) the loss of the ability to perform two or more ADLs at one month post-discharge compared to baseline assessment; 2) new nursing home placement at any time up to one year post-discharge; 3) death at any time up to one year post-discharge, and 4) combined outcome of new nursing home placement or death at any time up to one year post-discharge. One-month interviews to assess ADLs were conducted with either the patient or a surrogate if the patient was unable to be interviewed. The combined new nursing home placement or death outcome measure was used in order to capture both post-hospitalization outcomes and to avoid any potential inferential error that might arise because patients who die are no longer at risk of nursing home placement. This approach has been used in many previous studies.13,19,22,27 Nursing home admission was determined using Medicare claims, the State of Connecticut Nursing Facility Registry and follow-up family interviews. Mortality status was obtained from follow-up family interviews, daily monitoring of local obituaries and the Social Security Death Index. Deaths and dates of death were confirmed using death certificates, review of medical records, and Medicare enrollment and claims databases. For both outcomes of nursing home placement and death, multiple sources were mainly used for confirmation and verification of outcome dates, and there was a very high level of agreement across all sources.
Statistical Analyses
Descriptive statistics including means and proportions were calculated for the baseline characteristics of the overall sample and within each of the four depression and delirium categories. Differences in characteristics between the four groups were tested using chi-square tests for categorical measures and one-way analysis of variance for continuous measures. For descriptive statistics and comparisons across groups, the ADL measure was dichotomized as the presence of any ADL impairment vs. no impairment. We used logistic regression models to identify patient characteristics associated with the overlap syndrome of depression and delirium, with and without adjustment for potential confounders.
The frequency of outcomes was measured within each depression and delirium category. For each outcome, frequencies across the depression and delirium categories were then evaluated using a non-parametric test for trend. Multivariable logistic regression was used to identify independent predictors of the overlap syndrome of depression and delirium. A nominal variable was created from the depression and delirium categories. This variable was used to test the effect of depression alone, delirium alone and the overlap syndrome on each outcome, compared to neither condition using multivariable logistic regression. All multivariable models were adjusted for sociodemographic characteristics, baseline ADL impairment, Charlson Comorbidity Index score, Mini-Mental State Examination score, history of antidepressant use, history of depression and nursing home residence. Using a method described by Rothman28, we calculated a synergy index to evaluate for the presence of a synergistic relationship between the risk factors of depression and delirium on our four outcomes. A Cox proportional-hazards regression model was used to test the association between our four depression and delirium groups and time to the combined outcome of new nursing home placement or death in the year following hospital discharge. After assessing the adequacy of the proportionality assumption by visually inspecting log-log plots of the survival function over depression and delirium groups, and confirming that none of the lines crossed,29 hazards ratios with 95% confidence intervals were calculated. All statistical analyses were performed using STATA SE version 10.0 (STATA Corporation, College Station, TX).
RESULTS
Characteristics of the overall study sample are displayed in Table 1. The mean age of the 459 participants was 80 years, and the majority were female, white and not married. The mean number of years of education was less than 12. A small number of participants (6%) lived in a nursing home prior to hospital admission. Some degree of functional impairment was evident in over one third of participants at hospital admission (35%) as measured by at least one deficit in the ability to perform ADL tasks. The average score on the Charlson Comorbidity Index was over 2, indicating a moderate degree of medical comorbidity, and the average MMSE score was over 23. Close to one fifth (19%) of participants had a reported history of depression and 9% were taking antidepressant medication at the time of hospital admission.
Table 1.
Characteristics of study sample
| N = 459 | |
| Age in years, mean (± SD) | 80 (6.5) |
| Male, n (%) | 182 (40) |
| Non-white race, n (%) | 69 (15) |
| Years of education, mean (± SD) | 11 (3.7) |
| Unmarried, n (%) | 302 (66) |
| Nursing home residence prior to hospitalization, n (%) | 28 (6) |
| Any activity of daily living impairment, n (%) | 161 (35) |
| Charlson Comorbidity Index, mean (± SD) | 2.7 (2.2) |
| Mini-Mental State Examination score*, mean (± SD) | 23.3 (4.9) |
| Antidepressant use upon admission, n (%) | 43 (9) |
| History of depression, n (%) | 85 (19) |
range 0–30
SD = standard deviation.
Table 2 displays the characteristics of the study sample according to the presence of depression on admission or incident delirium during hospitalization. The majority of participants (60%) had neither depression nor delirium, 26% had depression alone, 9% had delirium alone and 5% had the overlap syndrome of both depression and delirium. Comparisons across the four groups revealed significant differences in sociodemographic characteristics (race, education, nursing home residence) and clinical measures (ADL impairment, comorbidity, MMSE scores, antidepressant use and history of depression). In general, clinical differences can be summarized as revealing that participants with neither depression nor delirium had lesser degrees of functional impairment, medical comorbidity, cognitive impairment, prior depression or depression treatment than those participants in the other groups. In addition, patients with the overlap syndrome were more likely to have resided in a nursing home prior to admission, to have functional impairment, a history of depression, higher levels of medical comorbidity and cognitive impairment when compared to all other patients.
Table 2.
Characteristics of Depression and Delirium Groups
| No depression or delirium N= 276 (60%) |
Depression alone N=121 (26%) |
Delirium alone N=39 (9%) |
Overlap syndrome N=23 (5%) |
P value* | |
|---|---|---|---|---|---|
| Age in years, mean (± SD) | 80 (6.3) | 79 (6.3) | 81 (7.4) | 81 (6.2) | 0.22 |
| Male, n (%) | 114 (41.3) | 43 (35.5) | 17 (43.6) | 8 (34.8) | 0.65 |
| Non-white race, n (%) | 42 (15.2) | 13 (10.7) | 12 (30.8) | 2 (8.7) | 0.02 |
| Years of education, n (%) | 11.5 (3.7) | 10.7 (3.3) | 9.6 (3.9) | 10.0 (3.1) | 0.003 |
| Unmarried, n (%) | 179 (64.9) | 76 (62.8) | 28 (71.8) | 17 (73.9) | 0.61 |
| Nursing home residence prior to hospitalization, n (%) | 10 (3.6) | 10 (8.26) | 4 (10.3) | 4 (17.4) | 0.02 |
| Any activity of daily living impairment, n (%) | 65 (23.6) | 60 (49.6) | 19 (48.7) | 16 (69.6) | <0.001 |
| Charlson Comorbidity Index, mean ± (SD) | 2.5 (2.1) | 3.0 (2.0) | 3.1 (2.2) | 4.1 (2.9) | 0.001 |
| Mini-Mental State Examination, mean (± SD) | 24.2 (4.7) | 23.2 (4.2) | 18.8 (5.4) | 20.3 (4.4) | <0.001 |
| Antidepressant use upon hospital admission, n (%) | 17 (6.2) | 17 (14.1) | 6 (15.4) | 3 (13.0) | 0.04 |
| History of depression, n (%) | 33 (12.1) | 34 (28.6) | 10 (25.6) | 8 (34.8) | <0.001 |
| GDS** score, mean (± SD) | 2.65 (1.6) | 8.40 (2.2) | 2.67 (1.5) | 8.91 (2.4) | <0.001 |
| Hospital length of stay (days), mean (± SD) | 7.13 (4.3) | 7.13 (4.3) | 16.08 (13.6) | 12.13 (7.9) | <0.001 |
One-way ANOVA for continuous variables, chi square test for categorical variables
Geriatric Depression Scale, range 0–15
SD = standard deviation
All of the baseline characteristics were examined as potential predictors of the overlap syndrome of depression and delirium using multivariable logistic regression analysis. Significant predictors included the presence of at least one ADL impairment compared to no impairment (adjusted odds ratio [AOR] 1.31, 95% Confidence interval (CI) =1.06–1.61) and a higher Charlson Comorbidity Index score (AOR 1.27, 95% CI =1.06–1.52). Although nursing home residence, history of depression and lower cognitive status were associated with the overlap syndrome in bivariate analysis, they did not remain significant in adjusted analysis.
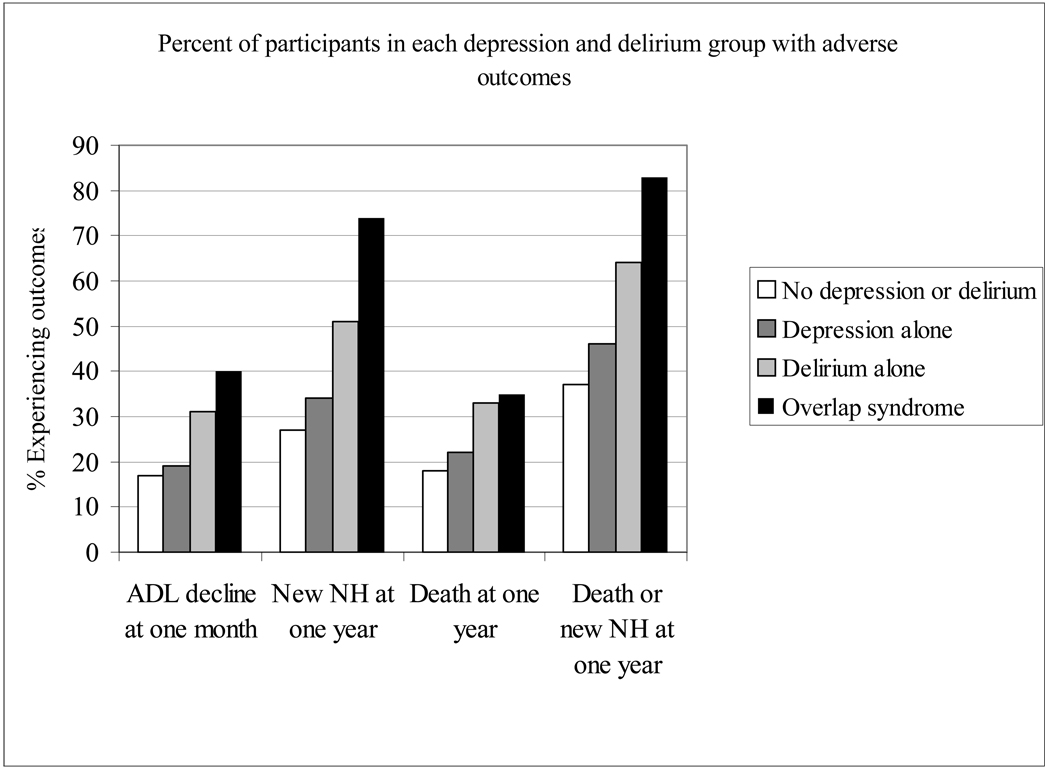
The percent of participants in each of the depression and delirium categories who experienced each of the outcomes are displayed in figure 1. For each outcome (increase of 2 of more ADL impairments at one month, nursing home placement, death, nursing home placement or death), frequencies increased across the depression and delirium groups such that the lowest rates occurred among participants with neither condition and increased sequentially among those with depression alone, delirium alone and the overlap syndrome of depression and delirium. Non-parametric tests of trend were highly significant across these categories for all outcomes (p<0.01).
Figure 1. Outcomes by Depression and Delirium Groups.
ADL decline defined as increase of 2 or more activities of daily living (ADL) deficits at one month compared to baseline.
NH = nursing home.
ptrend <0.01 for all outcomes
To examine the independent effect of depression, delirium and the overlap syndrome on our outcomes, we utilized multivariable logistic regression. The results of these analyses are displayed in Table 3, along with the number of participants experiencing each outcome. Participants with depression alone were not at increased risk of poor outcomes compared to those without depression or delirium. Compared to participants with neither depression nor delirium, those with delirium alone had higher odds of nursing home placement as well as nursing home placement or death. Participants with the overlap syndrome had significantly higher odds of three outcomes: one month ADL decline, nursing home placement and the combined outcome of nursing home placement or death, compared to those with neither condition. Those participants with the overlap syndrome had higher odds of both of the latter two outcomes compared to those with delirium alone. In other words, the combination of depression and delirium conferred greater odds of poor outcomes than either delirium or depression alone. Neither depression, delirium, nor the overlap syndrome, were associated with increased odds of death alone in adjusted analysis (depression AOR 1.10, 95% CI 0.60–2.02; delirium AOR 1.32, 95% CI 0.56–3.08; overlap syndrome AOR 0.97, 95% CI 0.33–2.83). To further test the relationship between depression and delirium on the combined outcome of new NH placement or death during the year following hospital discharge, we performed a Cox proportional hazards analysis, adjusting for all covariates included in the multivariable logistic regression analyses. These results demonstrate that compared to those participants without depression or delirium the adjusted hazard ratios (AHR) and 95% confidence intervals (CI) were as follows for those with depression alone (AHR 1.19, 95% CI = 0.84 –1.68), delirium alone (AHR 1.74, 95% CI = 1.07 – 2.84), and the overlap syndrome (AHR 2.39, 95% CI = 1.40 – 4.05). For all or our outcomes, we calculated a synergy index, which estimates the potential synergy or antagonism between depression and delirium on our outcomes. All values were all close to the null value of 1, indicating that there was neither synergy nor antagonism. These results suggest that depression and delirium do not act along the same pathways in contributing to increased risk of adverse outcomes, but rather act additively and independently.
Table 3.
Adjusted predictors of one month decline in activities of daily living (ADL), nursing home placement or combined nursing home placement or death at one year, N=459
| One month ADL decline* | New nursing home placement at one year** | New nursing home placement or death at one year | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n | AOR | 95% CI | n | AOR | 95% CI | n | AOR | 95% CI | |
| No depression or delirium | 45 | 1.00 | 72 | 1.00 | 103 | 1.00 | |||
| Depression alone | 23 | 1.31 | 0.71–2.42 | 38 | 1.22 | 0.72–2.08 | 56 | 1.34 | 0.82–2.19 |
| Delirium alone | 12 | 1.64 | 0.71–3.80 | 18 | 2.49 | 1.06–5.83 | 25 | 2.61 | 1.15–5.90 |
| Overlap syndrome | 8 | 3.30 | 1.14–9.56 | 14 | 5.06 | 1.63–15.73 | 19 | 5.38 | 1.57–18.38 |
Increase of 2 or more activities of daily living (ADL) deficits at one month compared to baseline
Twenty-eight participants who resided in the nursing home prior to hospital admission not eligible for outcome
AOR = Adjusted odds ratio
Models adjusted for the following covariates: age, sex, race, education, marital status, nursing home residence prior to hospitalization (ADL outcome only), ADL impairment at baseline, Charlson Comorbidity Index, Mini Mental State Examination score, antidepressant upon hospital admission, history of depression.
Adjusted results for outcome of death at one year were not significant, see text for details
DISCUSSION
In this cohort of elderly patients hospitalized on a general medical service, we found that the overlap syndrome of depression and delirium was present in one of every twenty patients. Patients with the overlap syndrome had five fold higher odds of nursing home placement or death at one year and three fold higher odds of one-month functional decline compared to patients with neither depression nor delirium. In addition, the odds of adverse outcomes were higher for patients with the overlap syndrome than for those with either depression or delirium alone. These results remained significant after adjusting for sociodemographic characteristics, as well as measures of functional status, medical comorbidity and cognitive function. Factors placing patients at higher risk for the overlap syndrome of depression and delirium included a higher degree of baseline functional impairment and medical comorbidity.
In our sample of patients, 26% had depression alone, 9% had delirium alone and 5% had the overlap syndrome of depression and delirium. Although participants in our cohort were selected to be at moderate to high risk of delirium at baseline, the rates of depression and delirium identified in this study are similar to those found in other studies of hospitalized patients.1–3, 10–12 Although prior work has documented adverse outcomes associated with depression and delirium during hospitalization, our outcomes are difficult to compare to these studies due to differences in follow-up time frames and the specific outcomes measured. Thus, this analysis provides new information regarding post-hospitalization events to bolster previous research.
The strengths of the current study include the prospective identification of depression and delirium using well-validated, standardized methods. We identified incident delirium with a state-of-the-art delirium measurement utilized by experienced, trained research staff. Moreover, the prospective design offered an important advantage for this study; because we measured depressive symptoms at the baseline assessment, prior to the development of delirium, the effects of delirium do not obscure the validity of our depression measure. Finally, we used only the control group of the previous intervention trial, which represented a true prospective epidemiologic cohort for this study.
Several caveats should be acknowledged. Our study was conducted at a single site, which may limit the generalizability of our findings. In addition, because we deliberately excluded patients with delirium on hospital admission, our estimates of the prevalence of the overlap syndrome may underestimate rates found in other hospital settings. While our results suggest that NH residents may be at high risk of the overlap syndrome, the small numbers of NH residents in our study limits these findings. The validity of some of our measures deserves comment. First, our measure of ADL impairment was based on self-report. Second, there is some concern regarding the reliability and validity of the GDS in patients with dementia,22,30,31 although the GDS has been established as a valid measure of mild-to-moderate depressive symptoms in patients with mild-to-moderate dementia.31 Since the use of the GDS rather than a clinical diagnostic algorithm for depression raises the potential for misclassification, we recognize this as a limitation of this study. However, as patients who deny cognitive deficits have been shown to also deny depressive symptoms31, any misclassification bias among these patients would likely lead to an underestimation of depression. What mitigates this limitation is that the GDS has been used in similar patient populations in other research,2,4 and is easily replicated in hospital environments. Finally, the presence of depressive symptoms may have interfered with or influenced the identification of delirium in this group, such as by introducing difficulties with cognitive testing in the depressed patients. This possibility, however, was limited by the strict criteria used for identification of delirium, and is also unlikely because depression was previously identified as an important risk factor for delirium in this same population.17
Our findings have clinical relevance for those caring for elderly hospitalized patients. Although estimates suggest that depressive symptoms and delirium are common in such patients, these conditions are often unrecognized,32–34 and contribute independently to poor outcomes. Our results highlight the importance of continued efforts to identify patients with these symptoms in order to prevent adverse outcomes. The occurrence of delirium during hospitalization can be reduced with the implementation of specific protocols11,35 and our results suggest that among patients with baseline depression, such prevention may confer a particular benefit. Although depression and delirium were measured during hospitalization in our study, these conditions may require continued evaluation and treatment after hospital discharge. The majority of patients found to have either major or minor depression during medical hospitalization remain symptomatic one year after hospital discharge.36 The effects of delirium in the post-acute setting can also be long-lasting, requiring treatment and vigilance to avoid complications such as the development of geriatric syndromes, functional decline or new medical conditions.37,38
Recognition of the increased risk for adverse outcomes in hospitalized patients with the overlap syndrome of depression and delirium may aid in post-hospitalization planning. Our findings suggest that the co-occurrence of these conditions substantially impairs functional recovery from acute illness and hospitalization. These patients may require more intensive rehabilitation services, either at home or in post-acute facilities in light of the higher likelihood of ADL decline at one month post-discharge. We hypothesize that the higher rates of nursing home placement or death at one year in patients with the overlap syndrome may be partially related to their impaired functional recovery, a known risk factor for nursing home placement and death in patients after hospitalization.39,40 Both depression and delirium can impair functional recovery after hospitalization4,13,37 and the combination is likely to have a particularly deleterious effect perhaps due to increased difficulty in participation in rehabilitative activities.
In summary, this study documents the prevalence, predictors and selected adverse outcomes associated with the overlap of depression and delirium, a syndrome not previously studied, among a cohort of elderly hospitalized patients. Our findings indicate that this syndrome carries significant risk for functional decline as well as nursing home placement and death at one year. Patients with the overlap syndrome appear to be at higher risk of these adverse outcomes than those with either depression or delirium alone. Our results suggest that depression and delirium act in an additive and independent fashion to produce higher rates of adverse outcomes. Future research will be needed to elucidate specific mechanisms underlying this increased risk.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the assistance of Gail McAvay PhD, and Peilin Shi PhD, in access to and preparation of elements of the analytic dataset. Dr McAvay and Dr Shi have provided written consent for this acknowledgement.
Funding sources: Funded in part by grants R21AG025193 and K24AG00949 from the National Institute on Aging, and the Aging Brain Center, Institute for Aging Research, Hebrew Senior Life. Dr. Inouye holds the Milton and Shirley F. Levy Family Chair
Sponsor’s role: none
Footnotes
Conflict of interest: The authors report no conflicts of interest.
REFERENCES
- 1.McCusker J, Cole M, Dufouil C, et al. The prevalence and correlates of major and minor depression in older medical inpatients. J Am Geriatr Soc. 2005;53:1344–1353. doi: 10.1111/j.1532-5415.2005.53404.x. [DOI] [PubMed] [Google Scholar]
- 2.Covinsky KE, Kahana E, Chin MH, et al. Depressive symptoms and 3-year mortality in older hospitalized medical patients. Ann Intern Med. 1999;130:563–569. doi: 10.7326/0003-4819-130-7-199904060-00004. [DOI] [PubMed] [Google Scholar]
- 3.Koenig HG, George LK, Peterson BL, et al. Depression in medically ill hospitalized older adults: prevalence, characteristics, and course of symptoms according to six diagnostic schemes. Am J Psychiatry. 1997;154:1376–1383. doi: 10.1176/ajp.154.10.1376. [DOI] [PubMed] [Google Scholar]
- 4.Covinsky KE, Fortinsky RH, Palmer RM, et al. Relation between symptoms of depression and health status outcomes in acutely ill hospitalized older persons. Ann Intern Med. 1997;126:417–425. doi: 10.7326/0003-4819-126-6-199703150-00001. [DOI] [PubMed] [Google Scholar]
- 5.Frasure-Smith N, Lesperance F, Talajic M. Depression following myocardial infarction. Impact on 6-month survival. JAMA. 1993;270:1819–1825. [PubMed] [Google Scholar]
- 6.Rumsfeld JS, Jones PG, Whooley MA, et al. Depression predicts mortality and hospitalization in patients with myocardial infarction complicated by heart failure. Am Heart J. 2005;150:961–967. doi: 10.1016/j.ahj.2005.02.036. [DOI] [PubMed] [Google Scholar]
- 7.McCusker J, Cole M, Ciampi A, et al. Major depression in older medical inpatients predicts poor physical and mental health status over 12 months. Gen Hosp Psychiatry. 2007;29:340–348. doi: 10.1016/j.genhosppsych.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 8.Roach MJ, Connors AF, Dawson NV, et al. Depressed mood and survival in seriously ill hospitalized adults. The SUPPORT Investigators. Arch Intern Med. 1998;158:397–404. doi: 10.1001/archinte.158.4.397. [DOI] [PubMed] [Google Scholar]
- 9.Koenig HG, George LK, Larson DB, et al. Depressive symptoms and nine-year survival of 1,001 male veterans hospitalized with medical illness. Am J Geriatr Psychiatry. 1999;7:124–131. [PubMed] [Google Scholar]
- 10.Pompei P, Foreman M, Rudberg MA, et al. Delirium in hospitalized older persons: outcomes and predictors. J Am Geriatr Soc. 1994;42:809–815. doi: 10.1111/j.1532-5415.1994.tb06551.x. [DOI] [PubMed] [Google Scholar]
- 11.Inouye SK, Bogardus ST, Jr., Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340:669–676. doi: 10.1056/NEJM199903043400901. [DOI] [PubMed] [Google Scholar]
- 12.Levkoff SE, Evans DA, Liptzin B, et al. The occurrence and persistence of symptoms among elderly hospitalized patients. Arch Intern Med. 1992;152:334–340. doi: 10.1001/archinte.152.2.334. [DOI] [PubMed] [Google Scholar]
- 13.Inouye SK, Rushing JT, Foreman MD, et al. Does delirium contribute to poor hospital outcomes? A three-site epidemiologic study. J Gen Intern Med. 1998;13:234–242. doi: 10.1046/j.1525-1497.1998.00073.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Murray AM, Levkoff SE, Wetle TT, et al. Acute delirium and functional decline in the hospitalized elderly patient. J Gerontol. 1993;48:M181–M186. doi: 10.1093/geronj/48.5.m181. [DOI] [PubMed] [Google Scholar]
- 15.Curyto KJ, Johnson J, TenHave T, et al. Survival of hospitalized elderly patients with delirium: a prospective study. Am J Geriatr Psychiatry. 2001;9:141–147. [PubMed] [Google Scholar]
- 16.Leslie DL, Zhang Y, Holford TR, et al. Premature death associated with delirium at 1- year follow-up. Arch Intern Med. 2005;165:1657–1662. doi: 10.1001/archinte.165.14.1657. [DOI] [PubMed] [Google Scholar]
- 17.McAvay GJ, Van Ness PH, Bogardus ST, Jr., et al. Depressive symptoms and the risk of incident delirium in older hospitalized adults. J Am Geriatr Soc. 2007;55:684–691. doi: 10.1111/j.1532-5415.2007.01150.x. [DOI] [PubMed] [Google Scholar]
- 18.Leung JM, Sands LP, Mullen EA, et al. Are preoperative depressive symptoms associated with postoperative delirium in geriatric surgical patients? J Gerontol A Biol Sci Med Sci. 2005;60:1563–1568. doi: 10.1093/gerona/60.12.1563. [DOI] [PubMed] [Google Scholar]
- 19.Givens JL, Sanft TB, Marcantonio ER. Functional recovery after hip fracture: the combined effects of depressive symptoms, cognitive impairment, and delirium. J Am Geriatr Soc. 2008;56:1075–1079. doi: 10.1111/j.1532-5415.2008.01711.x. [DOI] [PubMed] [Google Scholar]
- 20.Sheikh J, Yesavage J. GDS: Recent evidence and development of a shorter version. Clin Gerontol. 1986;5:165–172. [Google Scholar]
- 21.Lyness JM, Noel TK, Cox C, et al. Screening for depression in elderly primary care patients. A comparison of the Center for Epidemiologic Studies-Depression Scale and the Geriatric Depression Scale. Arch Intern Med. 1997;157:449–454. [PubMed] [Google Scholar]
- 22.Koehler M, Rabinowitz T, Hirdes J, et al. Measuring depression in nursing home residents with the MDS and GDS: an observational psychometric study. BMC Geriatr. 2005;5:1. doi: 10.1186/1471-2318-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113:941–948. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 24.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 25.Katz S, Downs TD, Cash HR, et al. Progress in development of the index of ADL. Gerontologist. 1970;10:20–30. doi: 10.1093/geront/10.1_part_1.20. [DOI] [PubMed] [Google Scholar]
- 26.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 27.Marcantonio ER, Flacker JM, Michaels M, et al. Delirium is independently associated with poor functional recovery after hip fracture. J Am Geriatr Soc. 2000;48:618–624. doi: 10.1111/j.1532-5415.2000.tb04718.x. [DOI] [PubMed] [Google Scholar]
- 28.Rothman KJ. Synergy and antagonism in cause-effect relationships. Am J Epidemiol. 1974;99:385–388. doi: 10.1093/oxfordjournals.aje.a121626. [DOI] [PubMed] [Google Scholar]
- 29.Kleinbaum D, Klein M. Survival Analysis: A self-learning text. New York: Springer; 2005. [Google Scholar]
- 30.Debruyne H, Van Buggenhout M, Le Bastard N, et al. Is the geriatric depression scale a reliable screening tool for depressive symptoms in elderly patients with cognitive impairment? Int J Geriatr Psychiatry. 2009 doi: 10.1002/gps.2154. [DOI] [PubMed] [Google Scholar]
- 31.Feher EP, Larrabee GJ, Crook TH., 3rd Factors attenuating the validity of the Geriatric Depression Scale in a dementia population. J Am Geriatr Soc. 1992;40:906–909. doi: 10.1111/j.1532-5415.1992.tb01988.x. [DOI] [PubMed] [Google Scholar]
- 32.Cepoiu M, McCusker J, Cole MG, et al. Recognition of depression in older medical inpatients. J Gen Intern Med. 2007;22 doi: 10.1007/s11606-006-0085-0. 559-264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cole MG. Delirium in elderly patients. Am J Geriatr Psychiatry. 2004;12:7–21. [PubMed] [Google Scholar]
- 34.Inouye SK, Foreman MD, Mion LC, et al. Nurses' recognition of delirium and its symptoms: comparison of nurse and researcher ratings. Arch Intern Med. 2001;161:2467–2473. doi: 10.1001/archinte.161.20.2467. [DOI] [PubMed] [Google Scholar]
- 35.Marcantonio ER, Flacker JM, Wright RJ, et al. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc. 2001;49:516–522. doi: 10.1046/j.1532-5415.2001.49108.x. [DOI] [PubMed] [Google Scholar]
- 36.Cole MG, McCusker J, Ciampi A, et al. The prognosis of major and minor depression in older medical inpatients. Am J Geriatr Psychiatry. 2006;14:966–975. doi: 10.1097/01.JGP.0000224327.16963.9f. [DOI] [PubMed] [Google Scholar]
- 37.Marcantonio ER, Kiely DK, Simon SE, et al. Outcomes of older people admitted to postacute facilities with delirium. J Am Geriatr Soc. 2005;53:963–969. doi: 10.1111/j.1532-5415.2005.53305.x. [DOI] [PubMed] [Google Scholar]
- 38.Marcantonio ER, Simon SE, Bergmann MA, et al. Delirium symptoms in post-acute care: prevalent, persistent, and associated with poor functional recovery. J Am Geriatr Soc. 2003;51:4–9. doi: 10.1034/j.1601-5215.2002.51002.x. [DOI] [PubMed] [Google Scholar]
- 39.Rudberg MA, Sager MA, Zhang J. Risk factors for nursing home use after hospitalization for medical illness. J Gerontol A Biol Sci Med Sci. 1996;51:M189–M194. doi: 10.1093/gerona/51a.5.m189. [DOI] [PubMed] [Google Scholar]
- 40.Inouye SK, Peduzzi PN, Robison JT, et al. Importance of functional measures in predicting mortality among older hospitalized patients. JAMA. 1998;279:1187–1193. doi: 10.1001/jama.279.15.1187. [DOI] [PubMed] [Google Scholar]