Abstract
PURPOSE
Establish a relationship between vascular calcifications seen via mammography and coronary artery disease, estimate the risk ratios, and investigate the interrelationships between vascular calcification and other risk factors for coronary artery disease.
MATERIALS AND METHODS
This was a case-control study consisting of 40 women with coronary artery disease in the case group and 40 women without any history of coronary artery disease in the control group who were matched according to age. The study was approved by the Institution’s Research Ethics Committee (consent statement was obtained). Odds ratios and confidence intervals were calculated using univariate analysis. Interrelationships among other risk factors, such as arterial hypertension, dyslipidemia, smoking and diabetes mellitus, were calculated using multivariate analysis. A p <0.05 was considered to be significant for statistical analysis.
RESULTS
The mean ages for the case and control groups were 64.65 years and 63.88 years, respectively. In multivariate analysis, the only variables related to coronary artery disease were Vascular calcification [OR 4.71 (CI 1.36–16.33) p=0.014], family history [OR 5.76 (CI 1.58–21.03) p=0.008] and arterial hypertension [OR 15.92 (CI 3.12–81.14) p=0.001]. Although smoking and diabetes are important variables in the pathogenesis of coronary artery disease, these factors did not show statistically significant associations in this sample.
CONCLUSION
The presence of vascular calcifications seen via mammography was an independent risk factor for coronary artery disease, as were hypertension and a family history of coronary artery disease.
Keywords: Mammography, Vascular calcifications, Coronary artery disease
INTRODUCTION
Atherosclerosis is the principal cause of morbidity and mortality in Western countries, and coronary artery disease is its most frequent complication.1 It is believed that in the United States more than 12 million people have coronary artery disease. This disease consumes the greatest quantity of healthcare resources in developed countries.2 Although a large proportion of the associated risk factors for coronary artery disease are preventable, acute myocardial infarction is still the leading cause of death among women over the age of 40 years.3,4
Vascular calcifications that are seen via mammography are called Mönckeberg calcifications, and involve the middle layer of the arteries. These calcifications are generally diffuse and thin, and tend to involve the entire circumference of the peripheral arteries, making the vessels rigid with little capacity for distension.5,6 Calcifications are infrequent in patients less than 50 years old and are found in around 9.1% of mammograms.7 The prevalence of calcifications ranges from 9% to 17%, for the female population while the prevalence increases with age and exceeds 50% among women aged 65 years and above.8
Some studies have found associations between vascular calcifications in breast tissue and chronic diseases such as diabetes, systemic arterial hypertension, coronary artery disease, kidney failure, autonomic neuropathy and hypervitaminosis D.9–13
Although no ischemic or embolic events have been observed, the presence of calcifications in the middle layer of arteries is correlated with an increased risk of coronary artery disease and diabetes.14, 15 The clinical significance of Mönckeberg calcifications is controversial; however, they are commonly found in diabetic women and may be a predictive factor for cardiovascular events.16–18
Thus, the purpose of this study was to determine the nature of the relationship between vascular calcifications in breast tissue and coronary artery disease.
MATERIALS AND METHODS
Approval for this case-control study was obtained from the Research Ethics Committee. Eighty women were included in this study. They were all informed about the purpose of the study and signed a free and informed consent statement.
Inclusion criteria for the coronary artery disease group
Forty women with coronary artery disease who had undergone mammography during the preceding twelve months were included in the case group. Cases were defined as coronary artery disease cases if the disease had been confirmed by coronariography or the individuals had experienced at least one episode of acute myocardial infarction.
The electrocardiographic findings that constituted a diagnosis of acute myocardial infarction included: ST depression or T wave inversion without Q waves in cases of infarction without Q waves; new Q waves with hyper-acute T waves and ST elevation followed by T wave inversion in cases of infarction with T waves.
Inclusion criteria for the control group
The eligibility criteria for inclusion into the control group included: Individuals should have attended the outpatient mastology clinic to undergo mammography within the twelve months preceding the inclusion date, not have had any previous signs and symptoms of coronary artery disease, and have a normal electrocardiogram. The controls were matched to the cases according to age, plus or minus two years, which was ascertained at the time of mammography.
Variables analyzed
The variables analyzed were defined as follows. Systemic arterial hypertension: Diastolic arterial pressure (DAP) ≥ 90 mmHg or systolic arterial pressure (SAP) ≥ 140 mmHg or regular use of pressure lowering medications. Diabetes mellitus: Fasting serum glucose ≥ 126 mg/dl; serum glucose two hours after intake of 75 g of glucose ≥ 200 mg/dl; random serum glucose ≥ 200 mg/ dl with symptoms of polyuria, polydipsia and unexplained weight loss; or use of hypoglycemic agents. Dyslipidemia: Total cholesterol ≥ 200 mg/dl, LDL cholesterol ≥ 130 mg/ dl and HDL cholesterol ≤ 40 mg/dl. Body mass index (BMI): Ratio of weight in kilograms (kg) to height in meters squared (m2). Obesity: BMI ≥ 25 kg/m2. Sedentary lifestyle: Patients who were not doing any physical activity or were doing it irregularly.
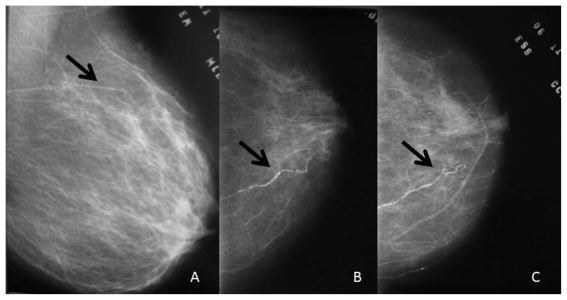
Vascular calcification in breast tissue was defined as the presence of parallel linear calcified deposits along the course of a vessel that was seen on at least one mammographic viewing plane. The intensity of the calcifications, number of vessels affected and the side affected were analyzed. The presence and intensity of the calcifications was graded as follows: Absent: No vascular calcifications; slight: Arteries with little calcification with distances greater than 10 mm between calcified areas (Figure 1a); moderate: Arteries clearly outlined by calcifications over a considerable proportion of their course (Figure 1b); and severe: Arteries extensively affected, seen to have almost continuous columns of calcification, with at least two branches also visible (Figure 1c). All mammograms were analyzed by only one observer.
Figure 1.
Classification of the intensity of vascular calcifications: a) slight: Arteries with few calcifications at large distances from each other (more than 10 mm); b) moderate: Arteries clearly outlined by calcifications over a considerable proportion of their course; c) severe: Arteries extensively affected, seen as almost continuous columns of calcification with at least two branches also visible
The number of calcified vessels was analyzed independently of the intensity of calcification. The laterality of the calcification was also analyzed and graded as unilateral, bilateral.
Statistical analysis
The data were typed into the dbase III database, and this was done twice to avoid typing errors. After compiling and checking the information, statistical analysis was performed using the SPSS 11.0.1 software. Univariate analysis was used to calculate odds ratios and confidence intervals for relationships between vascular calcifications and each of the factors already known to be involved in coronary artery disease. Multivariate analysis was also performed, by means of logistic regression, to estimate the interrelationships between different variables and coronary artery disease. P<0.05 was taken to be significant in this analysis.
RESULTS
In this study, the mean age was 64.65 years (SD ±8.49) in the case group and 63.88 (SD ±8.59) in the control group. Among the patients with coronary artery disease, 37 (92.5%) presented with hypertension, 15 (37.5%) with diabetes, 28 (70.0%) had a sedentary lifestyle and 27 (67.5%) had a family history of coronary artery disease. In the control group, 20 (50.0%) presented with hypertension, five (12.5%) with diabetes, 22 (55.0%) had a sedentary lifestyle and 18 (40.0%) had a family history of coronary artery disease.
In univariate analysis, there were statistically significant differences between the case group and the control group in relation to serum levels of total cholesterol (p=0.02), LDL cholesterol (p=0.01), fasting serum glucose (p<0.01), systolic arterial pressure levels (p=0.03), diastolic arterial pressure levels (p<0.01) and the number of cigarettes smoked per day (p=0.05). There was no statistically significant difference between the groups in relation to serum HDL cholesterol (p=0.62), BMI (p=0.68) or length of time with smoking habit (p=0.21).
The odds ratio (OR) for coronary artery disease, in relation to vascular calcifications in breast tissue seen via mammography, was 3.56. The odds ratios for the other risk factors analyzed were 4.20 for diabetes mellitus, 12.33 for arterial hypertension, and 2.53 for a family history of coronary artery disease. Sedentary lifestyle was not shown to be a risk factor in our study (Table 1).
Table 1.
Univariate analysis of factors presumed to present a risk for coronary artery disease
| Variables | Coronary artery disease | Non-coronary artery disease | X2 | p | OR (95% CI) |
|---|---|---|---|---|---|
| Diabetes | 15 (37.5%) | 5 (12.5%) | 668 | 0.01 | 4.20 (1.35–13.07) |
| Hypertension | 37 (92.5%) | 20 (50.0%) | 17.64 | <0.01 | 12.33 (3.26–46.63) |
| Sedentary lifestyle | 28 (70.0%) | 22 (55.0%) | 1.92 | 0.16 | 1.91 (0.76–4.79) |
| Family history | 27 (67.5%) | 18 (40.0%) | 4.11 | 0.04 | 2.53 (1.02–6.30) |
| Vascular calcification | 23 (57.5%) | 11 (27.5%) | 7.36 | <0.01 | 3.56 (1.40–9.08) |
When vascular calcifications were found to be present in breast tissue via mammography, they were always bilateral. There was a statistically significant difference in the intensity of the calcifications between the two groups, as shown in Table 2. The median number of calcified vessels was three in the case group and none in the control group (p<0.01).
Table 2.
Analysis of the intensity of calcifications seen on mammograms according to the groups
| Calcification intensity | Coronary artery disease | Non-coronary artery disease |
|---|---|---|
| No calcification | 17 (42.5%) | 30 (75%) |
| Slight | 13 (32.5%) | 7 (17.5%) |
| Moderate | 7 (17.5%) | 3 (7.5%) |
| Severe | 3 (7.5%) | 0 |
P=0.018
In multivariate analysis, it was observed that only family history (OR 5.76), arterial hypertension (OR 15.92) and vascular calcifications in breast tissue (OR 4.71) were risk factors for the occurrence of coronary artery disease. Smoking and diabetes were not independently associated with the risk of coronary artery disease (Table 3).
Table 3.
Multivariate analysis of factors presumed to present a risk of coronary artery disease
| Variable | OR | Std. Err | z | p | (95% CI) |
|---|---|---|---|---|---|
| History of heart disease | 5.76 | 3.80 | 2.65 | 0.008 | (1.58–21.03) |
| Smoking | 4.78 | 4.59 | 1.63 | 0.103 | (0.72–31.45) |
| Hypertension | 15.92 | 13.23 | 3.33 | 0.001 | (3.12–81.14) |
| Diabetes | 3.10 | 2.17 | 1.62 | 0.105 | (0.78–12.24) |
| Vascular calcification | 4.71 | 2.98 | 2.45 | 0.014 | (1.36–16.33) |
DISCUSSION
Vascular calcifications in breast tissue usually have a lipid component and resemble calcifications seen in other arteries. The mechanism of deposition is still unknown6.
In our analysis, we found that the presence of vascular calcifications in breast tissue seen via mammography was an independent risk factor for coronary artery disease. Some previous studies have also found such an association. In previous studies, 16 to 31% of women with coronary artery disease presented with vascular calcifications seen via mammography.19–21 In a study of 131 women in 2007, Ferreira et al. found an odds ratio of 2.96 (CI 1.25–7.30),19 which was slightly lower than the odds ratio of 3.56 (CI 1.40–9.08) that was found in the present study.
One interesting finding was that, when present, the vascular calcifications in breast tissue were bilateral, thus showing that the atherosclerotic process and consequent vascular calcification was affecting the entire arterial system.
Age was not an important risk factor in this study, given that the study design involved matching the patients in the case and control groups by age.
Univariate analysis showed that all of the investigated factors (except BMI) were associated with coronary artery disease; however, after multivariate analysis, it was observed that some factors that are known to be associated with coronary artery disease1,3 lost their statistical significance, among which were smoking and diabetes.
One likely explanation for this finding was presented by Çetin et al., who showed that diabetic women also had a greater risk of vascular calcifications in breast tissue.10 In our analysis, the association between vascular calcifications in breast tissue and coronary artery disease was greater than the association between diabetes and coronary artery disease. This correlation may explain the loss of statistical significance between diabetes and coronary artery disease in the multivariate analysis. Apart from being a risk factor for coronary artery disease, vascular calcifications in breast tissue may also indicate the presence of diabetes.10,22 Vascular calcifications are frequently associated with abnormalities in bone metabolism, dyslipidemia and chronic inflammation.23
In addition to vascular calcifications in breast tissue, systemic arterial hypertension and a family history of coronary artery disease were also independent risk factors for coronary artery disease. Systemic arterial hypertension was the risk factor that showed the greatest association with coronary artery disease.
These same associations were found by Crystal et al., who found that the presence of calcifications, seen via mammography, was significantly associated with the existence of coronary artery disease and that family history had the highest odds ratio. Variables such as age, diabetes mellitus and menopause were less significant than the presence of vascular calcifications.24
Although smoking is an important risk factor for coronary artery disease, data from this study did not show any association between smoking and the presence of vascular calcifications in breast tissue. Another study also did not find this association.14
The purpose of this study was to evaluate the association between coronary artery disease and vascular calcifications seen via mammography. The data obtained herein demonstrated a significant association between vascular calcifications and coronary artery disease that was independent of other known risk factors. This finding suggests that mammography might be a very important screening method for coronary artery disease in women. Mammography is an already important imaging method for breast cancer, but this study suggests that it is also useful for testing for other chronic-degenerative diseases.
REFERENCES
- 1.American Heart Association. Heart disease and stroke statistics. Circulation. 2007;115:e69–e171. doi: 10.1161/CIRCULATIONAHA.106.179918. [DOI] [PubMed] [Google Scholar]
- 2.Selwyn AP, Braunwald E. Ischemic heart disease. In: Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL, Isselbacher KJ, editors. Harrison’s: principles of internal medicine. 16th ed. McGraw-Hill Companies; 2004. pp. 1434–44. [Google Scholar]
- 3.Mosca L, Banka CL, Benjamin EJ, Berra K, Bushnell C, Dolor RJ, et al. Evidence-Based Guidelines for Cardiovascular Disease Prevention in Women: 2007 Update. Circulation. 2007;115:1481–501. doi: 10.1161/CIRCULATIONAHA.107.181546. [DOI] [PubMed] [Google Scholar]
- 4.Favarato MLCS, Favarato D, Hueb WA, Aldrighi JM. Quality of life in patients with coronary artery disease: comparison between genders. Rev Assoc Med Bras. 2006;52: 236–41. doi: 10.1590/s0104-42302006000400023. [DOI] [PubMed] [Google Scholar]
- 5.Kim H, Greenberg JS, Javitt MC. Breast Calcifications due to Mönckeberg medial calcific sclerosis. Radiographics. 1999;19:1401–3. doi: 10.1148/radiographics.19.5.g99se221401. [DOI] [PubMed] [Google Scholar]
- 6.Schoppet M, Al-Fakhri N, Franke FE, Katz N, Barth PJ, Maisch B, et al. Localization of osteoprotegerin, tumor necrosis factor-related apoptosis-inducing ligand and receptor activator of nuclear factor-kappaB ligand in Mönckeberg’s sclerosis and atherosclerosis. J Clin Endocrinol Metab. 2004;89:4104–12. doi: 10.1210/jc.2003-031432. [DOI] [PubMed] [Google Scholar]
- 7.Van Noord PA, Beijerinck D, Kemmerenen JM, Graaf Y. Mammograms may convey more than breast cancer risk: breast arterial calcification and arteriosclerotic related diseases in women of DOM cohort. Eur J Cancer Prev. 1996;5:483–7. [PubMed] [Google Scholar]
- 8.Reddy J, Son H, Smith SJ, Paultre F, Mosca L. Prevalence of breast arterial calcification in an ethnically diverse population of women. Ann Epidemiol. 2005;15:344–50. doi: 10.1016/j.annepidem.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 9.Maas AHEM, Van der Schouw Y, Mali WPTM, Van der Graaf Y. Prevalence and determinants of breast arterial calcium in women at high risk of cardiovascular disease. Am J Cardiol. 2004;94:655–8. doi: 10.1016/j.amjcard.2004.05.036. [DOI] [PubMed] [Google Scholar]
- 10.Çetin M, Çetin R, Tamer N, Kelekçi S. Breast arterial calcifications associated with diabetes and hypertension. J Dia Comp. 2004;18:363–6. doi: 10.1016/j.jdiacomp.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 11.Young MJ, Adams JE, Anderson GF, Boulton AJ, Cavanagh PR. Medial arterial calcification in the feet of diabetic patients and matched non-diabetic control subjects. Diabetologia. 1993;36:615–21. doi: 10.1007/BF00404070. [DOI] [PubMed] [Google Scholar]
- 12.Forst T, Pfutzner A, Kann P, Lobmann R, Schafer H, Beyer J. Association between diabetic-autonomic-C-fibre-neuropathy and medial wall calcification and the significance in the outcome of trophic foot lesions. Exp Clin Endocrinol Diabetes. 1995;103:94–8. doi: 10.1055/s-0029-1211335. [DOI] [PubMed] [Google Scholar]
- 13.Moe SM, O’Neill KD, Duan D, Ahmed S, Chen NX, Leapman SB, et al. Medial artery calcification in ERSD patients is associated with deposition of bone matrix proteins. Kidney Int. 2002;61:638–47. doi: 10.1046/j.1523-1755.2002.00170.x. [DOI] [PubMed] [Google Scholar]
- 14.Lehto S, Niskanen L, Suhonen M, Ronnemaa T, Laakso M. Medial artery calcification: a neglected harbinger of cardiovascular complications in non–insulin-dependent diabetes mellitus. Arterioscler Thromb Vasc Biol. 1996;16:978–83. doi: 10.1161/01.atv.16.8.978. [DOI] [PubMed] [Google Scholar]
- 15.Shanahan CM, Cary NRB, Salisbury JR, Proudfoot D, Weissberg PL, Edmonds ME. Medial localization of mineralization-regulating proteins in association with Mönckeberg’s sclerosis: evidence for smooth muscle cell-mediated vascular calcification. Circulation. 1999;100:2168–76. doi: 10.1161/01.cir.100.21.2168. [DOI] [PubMed] [Google Scholar]
- 16.Iribarren C, Go AS, Tolstykh I, Sidney S, Johnston SC, Spring DB. Breast vascular calcification and risk of coronary heart disease, stroke, and heart failure. J Women’s Health (Larchmt) 2004;13:381–9. doi: 10.1089/154099904323087060. [DOI] [PubMed] [Google Scholar]
- 17.Nisakanen L, Siitonen O, Suhonen M, Uusitupa MI. Medial artery calcification predicts cardiovascular mortality in patients with NIDDM. Diabetes Care. 1994;17:1252–6. doi: 10.2337/diacare.17.11.1252. [DOI] [PubMed] [Google Scholar]
- 18.Moshyedi AC, Puthawala AH, Kurlan RJ, Leary DH. Breast arterial calcification: association with coronary artery disease. Radiology. 1995;194:181–3. doi: 10.1148/radiology.194.1.7997548. [DOI] [PubMed] [Google Scholar]
- 19.Ferreira EMPF, Szejnfeld J, Faintuch S. Correlation between intramammary arterial calcifications and CAD. Acad Radiol. 2007;14:144–50. doi: 10.1016/j.acra.2006.10.017. [DOI] [PubMed] [Google Scholar]
- 20.Topal U, Kaderli A, Topal NB, Ozdemir B, Yeşilbursa D, Cordan J, et al. Relationship between the arterial calcification detected in mammography and coronary artery disease. Eur J Radiol. 2007;63:391–5. doi: 10.1016/j.ejrad.2007.01.035. [DOI] [PubMed] [Google Scholar]
- 21.Kemmeren JM, Beijerinck D, Noord PAV, Banga JD, Deurenber JJM, Pameijer FA, et al. Breast arterial calcifications: association with diabetes mellitus and cardiovascular mortality. Radiology. 1996;201:75–78. doi: 10.1148/radiology.201.1.8816524. [DOI] [PubMed] [Google Scholar]
- 22.Dale PS, Richards M, Mackie GC. Vascular calcifications on screening mammography identify women with increased risk of coronary artery disease and diabetes. Am J Surg. 2008;196:537–40. doi: 10.1016/j.amjsurg.2008.06.012. [DOI] [PubMed] [Google Scholar]
- 23.Canabal A, Sabate J, Salgueira M, Palma A. Cardiovascular risk in women with chronic renal failure: mammographic study of vascular calcifications. Radiologia. 2008;50:54–60. doi: 10.1016/s0033-8338(08)71929-5. [DOI] [PubMed] [Google Scholar]
- 24.Crystal P, Crystal E, Leor J, Friger M, Katzinovitch G, Strano S. Breast arterial calcium on routine mammography as a potential marker for increased risk of cardiovascular disease. Am J Cardiol. 2000;86:216–7. doi: 10.1016/s0002-9149(00)00860-2. [DOI] [PubMed] [Google Scholar]