Abstract
INTRODUCTION
In 2003, the waiting time for routine scrotal assessment approached 6 months in our hospital. The patients' diagnostic pathway was not uniform and involved several delays between general practitioner, radiologist and urologist. If malignancy was suspected, patients were seen and assessed within 2 weeks. However, it was possible for patients with unsuspected malignancy to have their diagnosis delayed.
PATIENTS AND METHODS
Funding was provided by the NHS Modernisation Agency's Action On Urology project. Men who were referred by their general practitioner (GP) with a testicular or scrotal condition would be reviewed in a one-stop joint sonographer and urology nurse specialist clinic provided entirely within the urology department with rapid open access. Data were prospectively collected for 2 years. Source of referral, suspected diagnosis, findings and outcome were recorded.
RESULTS
A total of 1017 patients attended the clinic over this period; of these, 203 (4%) were referred under the ‘2-week wait’ criteria. Of patients attending the clinic, 79% were discharged to GP care, 8% were added to the waiting list for a surgical procedure and 20% were referred with ‘testicular lump’. Eleven patients were suspected to have testicular tumour on ultrasound and proceeded to orchidectomy in this period. One patient (0.1%) was found to have an unsuspected seminoma. The waiting time for all scrotal ultrasound examinations has fallen from 22 to 2 weeks. The waiting times for intravenous urography and general ultrasound were also significantly reduced following the introduction of this service (P = 0.005).
CONCLUSIONS
The majority of patients passing through this clinic are the ‘worried-well’ with benign scrotal pathology. They can now be seen within 2 weeks regardless of whether their GP suspects testicular tumour. This reduces anxiety in this large group of patients freeing capacity elsewhere in the diagnostic imaging department.
Keywords: One-stop testicular clinic, Audit
Prior to August 2004, general practitioners (GPs) in East Suffolk were able to investigate patients with scrotal disorders in several ways. Direct referral to the diagnostic imaging department for testicular ultrasound scan followed by a report by fax or mail involved several delays for the patient in the diagnostic pathway. Following this, referral to the urology department may then have ensued, resulting in further diagnostic delay. Alternatively, imaging was arranged after consultation with a senior urologist, resulting in two separate department visits on three occasions in addition to their initial GP consultation. In 2003, the diagnostic imaging department received 560 requests for scrotal ultrasonography, and the waiting time for such a scan, if routine, was in excess of 20 weeks. It was possible, however, if the index of suspicion was high, for the investigation to be performed on the same day as the consultation.
It was believed that the varied systems for patient evaluation provided neither the best quality service nor utilised resources with maximum efficiency. As such, the patient pathway was redesigned to provide a one-stop service in an attempt to provide rapid and simpler diagnosis and instigation of definitive treatment. Funding was provided by the NHS Modernisation Agency's Action On Urology project. Men who were referred by their GP with a testicular or scrotal condition would be reviewed in a joint sonographer and urology nurse specialist clinic provided entirely within the urology department with rapid open access. This service was to be provided in parallel with established urology general out-patient sessions where consultant urologists would be present to offer immediate review if required. The expected benefits were reduced demand on out-patient clinics and diagnostic imaging (and improved access, therefore, for other imaging), reduced transport costs through fewer clinic visits, convenience of a one-stop service and reduction in clerical and administrative time. A protocol was developed by a nurse specialist, urologist, GP and radiologist; initially, all outcomes were supervised and reviewed by the consultant. Data from the clinic were collected prospectively, and we now present 2-year outcome data review from this clinic.
Patients and Methods
All adult males with scrotal swellings or discomfort were accepted to the clinic. The referring clinician recorded their provisional diagnosis on the request form. Referral type (‘2-week wait’, urgent letter or routine appointment), ultrasound diagnosis and outcome were also noted. All patients had an initial clinical assessment by the urological nurse specialist (UNS) followed by scrotal ultrasound performed by an ultrasonographer using a Hitachi 5500 console with 7.5 MHz testicular transducer. The UNS was directly supervised by a senior urologist for the first 280 cases (8 months). Following this period, urological input was given when requested by the UNS or prior to listing for a surgical procedure.
Results
A total of 1017 patients were seen over the 2-year period. Of these, 203 (20%) were referred simply as a ‘scrotal lump’ and 41 (4%) with an accompanying suspected urological cancer ‘2-week wait’ proforma.
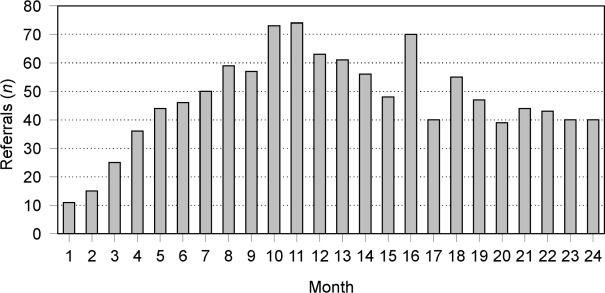
Referrals from GPs initially increased, from 10 in the first month of the study to a peak of 74 in month 11. By month 24, referrals had reduced to approximately 40 per month (Fig. 1).
Figure 1.
GP referrals to one-stop service per month.
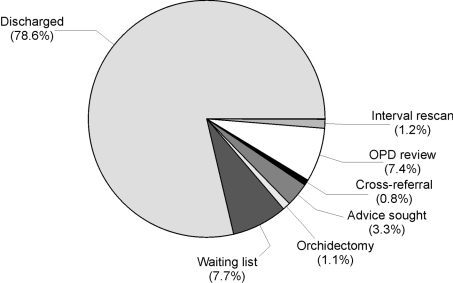
Of 1017 patients seen, 799 (78.6%) were discharged without further intervention, 78 (7.6%) were listed for surgery for benign disease (such as epididymal cyst excision, hydrocoele repair, varicocoelectomy or hernia repair), and 75 (7.3%) were given medical treatment with a view to interimout-patient review for conditions such as epididymitis. Eleven patients (1.1%) underwent radical orchidectomy for suspected malignancy. Thirty-four (3.3%) were initially discussed with a senior urologist following which 18 were discharged; the remainder were re-scanned after an interval or reviewed in out-patient clinic after medical treatment. The distribution of outcome is illustrated in Figure 2.
Figure 2.
Final outcome of cohort of 1017 patients.
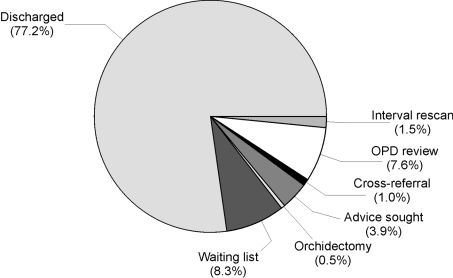
Data were subanalysed to compare outcome in the direct supervision period (August 2004 to April 2005; n = 281) with the indirectly supervised period (n = 736). The outcome distribution was almost identical (Fig. 3).
Figure 3.
Outcome destination in the indirect supervision period.
Outcomes were broadly similar in the two studied periods. As expected, slightly more patients required advice on their management in the indirect supervision period (3.9% versus 1.8%). Of these 34 patients, 18 were then discharged directly from clinic, bringing the total discharged to approximately 80%, in line with the data in Table 2. There was no statistically significant difference between the outcome distribution for these periods.
Table 2.
Direct supervision
| Patient destination | n | % |
|---|---|---|
| Discharged | 231 | 82.2 |
| Waiting list (benign) | 17 | 6.0 |
| Orchidectomy | 7 | 2.5 |
| Advice sought | 5 | 1.8 |
| Cross-referral | 1 | 0.4 |
| OPD review | 19 | 6.8 |
| Interval re-scan | 1 | 0.4 |
Table 1.
Indirect supervision
| Patient destination | n | % |
|---|---|---|
| Discharged | 568 | 77.2 |
| Waiting list (benign) | 61 | 8.3 |
| Orchidectomy | 4 | 0.5 |
| Advice sought | 29 | 3.9 |
| Cross-referral | 7 | 1.0 |
| OPD review | 56 | 7.6 |
| Interval re-scan | 11 | 1.5 |
During this time period, 11 orchidectomies for suspected testicular tumour were performed. Table 3 outlines the referral method and histology.
Table 3.
Referral type and histology for 11 radical orchidectomies performed.
| Patient | Histology | Referral method |
|---|---|---|
| 1 | Teratoma | Urgent letter |
| 2 | Seminoma | Routine (?cyst) |
| 3 | Seminoma | Urgent letter |
| 4 | Teratoma | Urgent letter |
| 5 | Combined | Urgent ultrasonography request |
| 6 | Seminoma | ‘2-week wait proforma’ |
| 7 | Benign | ‘2-week wait proforma’ |
| 8 | Teratoma | Urgent letter |
| 9 | Teratoma | ‘2-week wait proforma’ |
| 10 | Seminoma | ‘2-week wait proforma’ |
| 11 | Non-Hodgkin's lymphoma | ‘2-week wait proforma’ |
Of the 11 orchidectomies, 10 were for malignant disease, mostly seminoma or teratoma. Ten (91%) were initially referred with a suspicion of malignancy. One patient was referred as a routine request for investigation of an apparent epididymal cyst. Clinical examination in this case was not suggestive of malignancy.
The waiting time for all testicular ultrasound examinations, whether for suspected benign or malignant disease, in July 2006 was 2 weeks. The mean number of scans performed per year was 509.
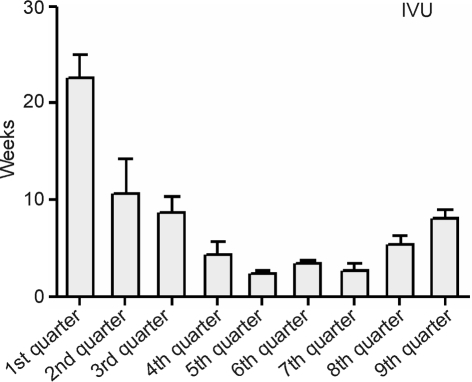
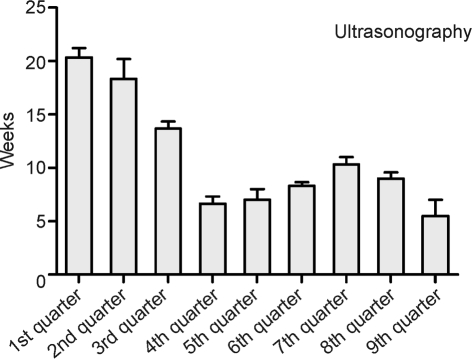
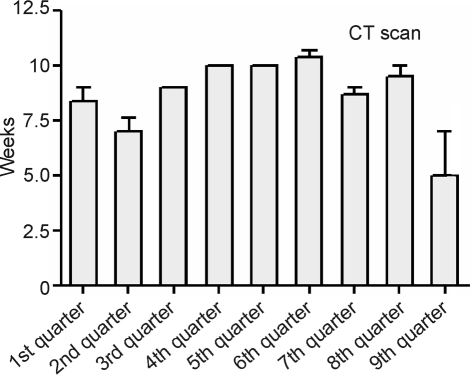
The waiting times for radiological investigations (CT, IVU, general ultrasound) were analysed in 3-month blocks over the 2-year study and mean waiting times compared. Waiting times for IVU and ultrasound were significantly reduced in the second quarter compared to the first (P = 0.0005, one-way ANOVA with Tukey post-test comparison; Fig. 4A,B). This difference was maintained for the duration of the study. In contrast, there was no effect on the waiting time for CT (Fig. 4C).
Figure 4.
Waiting times for radiological investigations. Mean (SD) monthly wait for (A) IVU, (B) general ultrasound, and (C) CT scan displayed per 3-month (quarter) period.
Discussion
In January 2005, all Action On Urology projects were subjected to peer review. Due to a delay in recruitment of a sonographer, data for only 4 months of the one-stop clinic were available for discussion. At that point, the number of scans had increased from 35 to 53 per month, principally due to a large backlog of requests in the diagnostic imaging department which needed to be processed. The waiting time had reduced from 22 weeks to 7 weeks against a target of 2 weeks. There were many perceived improvements to the service, such as reduced patient anxiety through education and the re-assurance of a normal or benign scan, one visit where there were previously three, and as a result, faster diagnosis in general, as well as for those labelled low risk but who are subsequently found to have cancer. Easy referral for GPs and instant-access ultrasound for urologists in their parallel general clinics was considered beneficial, and it was noted that capacity within general ultrasound is increased for other procedures. Quicker investigation, and hence treatment, reduces the risk of clinical complications and must be beneficial to the service as a whole.
The peer review raised several concerns, however. It was suggested that an improved service stimulated demand, and that there was no clear evidence that testicular ultrasound is more re-assuring than clinical examination alone. The review pointed out that recruitment of a sonographer was difficult. In conclusion, at that time, it was doubted whether the project was ‘clinically sound’ as there was increased demand with questionable benefit.
The recommendation was that this was probably not necessary for the majority of patients, that demand was high as GPs may not be confident to offer re-assurance and that ease of access created needless extra work.
Eighteen months later, with a more representative accumulation of data, it is possible to re-appraise this clinic, update outcome figures, and offer alternative conclusions.
Our data show that the performance of the UNS is identical with or without direct supervision. The waiting time for all ultrasonography scans is now 2 weeks, as planned in the initial proposal. The average number of scans performed is now 509 per year comparing favourably with 560 in 2003 under the previous system. This would suggest that, once the initial surge in demand combined with backlog clearing had passed, the workload returned to a steady state similar to that in 2003 and refutes the claim that our improved service simply stimulates demand.
Most cases seen in the one-stop clinic are benign, and more than 80% are discharged. No patients have re-attended in the short follow-up period. This is suggestive, although not conclusive, of patient satisfaction and reassurance which, in itself, is beneficial.
One pressing reason for a more liberal approach to testicular ultrasound application is the rare finding of a testicular tumour presenting later than optimal having been labelled as benign disease after clinical examination. Guthrie and Fowler1 showed that testicular ultrasound has a 98% sensitivity and 99.8% specificity for a diagnosis of malignancy in a series of patients referred for scrotal ultrasound. They found that 8 of 610 (1.3%) patients with a clinical diagnosis of epididymal disease made mostly by urologists were subsequently found on ultrasound to have a testicular malignancy, calling into question the reliability of physical examination. They concluded that all patients with scrotal symptoms should be evaluated by ultrasound. Other smaller studies have conflicting conclusions with regard to the value of more wide-spread use of scrotal ultrasonography. Older et al.2 showed that ultrasonography changed the clinical diagnosis of urologists in 32% of cases. Adeyoju et al.,3 in a series of 48 men, found that scanning changed the diagnosis in 27%, but altered treatment in only 4 patients. As no tumours were missed in 48 men, they concluded that routine ultrasonography was inappropriate. In our series, one patient was referred with benign disease and subsequently was found to have a seminoma. This equates to an approximate 1:1000 risk of missing tumour without this system. Guthrie and Fowler1 scanned 1494 patients in all and thus have a rate of 8/1494 or approximately 5:1000 pick-up rate for unsuspected malignancy. It is not possible to comment on the effectiveness of routine scrotal ultrasound using data from small series. It could be argued that routine ultrasound is unnecessary for all, and that only those with a suspicion of malignancy should be scanned. This approach, however, relies on the non-specialist to determine the likelihood of testicular cancer. Recently, a prospective study compared the clinical findings of GPs with hospital urologists over a 6-month period of referrals for scrotal pathology.4 Fifty-three patients were referred under the ‘2-week wait’ rule, of whom 9 (17%) had testicular cancer. Fourteen cancers in total were diagnosed in this period of which 3 were referred as ‘soon’ or ‘routine’ resulting in a delay to diagnosis of 56–75 days. Increasing inappropriate referrals under a ‘2-week wait’ banner reduce service capacity for those who genuinely need to be seen urgently. In their study, Foster et al.4 state that 81% of the ‘2-week wait’ referrals in retrospect were felt to be inappropriately referred at this priority. Without specialist training, or indeed, access to ultrasound, it can be difficult to exclude a diagnosis of cancer, a problem which is not unique to urology.5,6 Removing diagnostic uncertainty by allowing open access to a one-stop service reduces delay for all patients and, in doing so, prevents the delay in management of testicular tumour masquerading as benign scrotal disease. This is one of the principles set out in the Department of Health Modernisation Agency document, Ten High Impact Changes.7 While it was one of the aims of this clinic to provide early diagnosis of testicular cancer, it could be argued that the standard ‘2-week-wait’ referral protocol would not have missed any clinically apparent cases (Table 3), a credit to the referring GPs. A different population of referring practitioners may have generated an alternative outcome.
Only one cancer was found by chance (patient 2; Table 3). Taken together, this suggests that the reconfiguration would change the pick-up rate for cancer in 1:1000 cases (or 9% of cancers), on its own perhaps unlikely to justify the change in practice. Faster diagnosis is clearly achieved for the majority of patients who have benign pathology, however.
It has been demonstrated in our diagnostic imaging department that streamlining services through reducing scrotal ultrasound delay has freed capacity in other areas, which in turn reduced waiting time for other imaging such as general ultrasound and IVU. Such increased capacity in other radiology services could, no doubt, be achieved by other reconfiguration of services, but not with the additional benefits of an open-access clinic.
One-stop services are well established practise for haematuria,8–10 as well as in other specialties,11–13 and have been suggested by some authors as a possibility for testicular pathology,4,14 but have not been accepted in this setting as yet. With little evidence that ‘2-week wait’ initiatives impact on survival,15,16 and growing pressure to find alternative mechanisms of improving services in general, one-stop approaches are a logical progression.
The peer review process concluded that demand is stimulated for questionable clinical benefit. These data would suggest that, after an initial surge in demand, a steady state has been reached with demand less than that seen before the change in 2004. Patients now have the convenience of a one-stop service, with faster diagnosis, and less anxiety. The lack of re-attenders on this short follow-up is suggestive of the re-assurance of a normal scrotal ultrasound. Finally, since the waiting time for all ultrasound of the scrotum has been reduced to 2 weeks, the occasional patient who may harbour testicular malignancy, but is labelled as benign disease, can be identified early. We consider these combined improvements to be clinically beneficial.
A one-stop service is not a rod for your back. We recommend it as a standard of care.
References
- 1.Guthrie JA, Fowler RC. Ultrasound diagnosis of testicular tumours presenting as epididymal disease. Clin Radiol. 1992;46:397–400. doi: 10.1016/s0009-9260(05)80686-5. [DOI] [PubMed] [Google Scholar]
- 2.Older RA, Omary RA, Watson LR. The impact of sonography on the diagnosis of scrotal disorders. J Urol. 1997;158:479–80. [PubMed] [Google Scholar]
- 3.Adeyoju AB, Collins GN, Pollard AJ, Liaw J, Brooman PJ, O'Reilly PH. A prospective evaluation of scrotal ultrasonography in clinical practice. BJU Int. 2000;86:87–8. doi: 10.1046/j.1464-410x.2000.00704.x. [DOI] [PubMed] [Google Scholar]
- 4.Foster PW, Ritchie AW, Jones DJ. Prospective analysis of scrotal pathology referrals – are referrals appropriate and accurate? Ann RColl Surg Engl. 2006;88:363–6. doi: 10.1308/003588406X106540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Debnath D, Dielehner N, Gunning KA. Guidelines, compliance, and effectiveness: a 12 months' audit in an acute district general healthcare trust on the two week rule for suspected colorectal cancer. Postgrad Med J. 2002;78:748–51. doi: 10.1136/pmj.78.926.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martin JP, Gabe SM, Pitcher MC, Jacyna MR. Referral patterns to a district general hospital gastroenterology outpatient clinic: implications for the ‘two-week target’. Int J Clin Pract. 2002;56:26–8. [PubMed] [Google Scholar]
- 7.NHS Modernisation Agency. Ten High Impact Changes. London: Department of Health; 2004. [Google Scholar]
- 8.Lynch TH, Waymont B, Dunn JA, Hughes MA, Wallace DM. Rapid diagnostic service for patients with haematuria. Br J Urol. 1994;73:147–51. doi: 10.1111/j.1464-410x.1994.tb07482.x. [DOI] [PubMed] [Google Scholar]
- 9.Hasan ST, German K, Derry CD. Same day diagnosticservice for new cases of haematuria – a district general hospital experience. Br J Urol. 1994;73:152–4. doi: 10.1111/j.1464-410x.1994.tb07483.x. [DOI] [PubMed] [Google Scholar]
- 10.Rockall AG, Newman-Sanders AP, al-Kutoubi MA, Vale JA. Haematuria. Postgrad Med J. 1997;73:129–36. doi: 10.1136/pgmj.73.857.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Glancy DG, Card M, Sylvester PA, Thomas MG, Durdey P, Callaway M, et al. Fast-track barium enema: meeting the two-week wait rule for patients with suspected colorectal cancer. Colorectal Dis. 2005;7:241–4. doi: 10.1111/j.1463-1318.2005.00761.x. [DOI] [PubMed] [Google Scholar]
- 12.Chohan DP, Goodwin K, Wilkinson S, Miller R, Hall NR. How has the ‘two-week wait’ rule affected the presentation of colorectal cancer? Colorectal Dis. 2005;7:450–3. doi: 10.1111/j.1463-1318.2005.00821.x. [DOI] [PubMed] [Google Scholar]
- 13.Kumar S, Osman IS, Woolard CJ, Cameron AE. ‘Fast track’ carotid duplex scanning in a district general hospital. Ann R Coll Surg Engl. 2000;82:167–70. [PMC free article] [PubMed] [Google Scholar]
- 14.Allen D, Popert R, O'Brien T. The two-week-wait cancer initiative in urology: useful modernization? J R Soc Med. 2004;97:279–81. doi: 10.1258/jrsm.97.6.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hanna SJ, Muneer A, Khalil KH. The 2-week wait for suspected cancer: time for are think? Int J Clin Pract. 2005;59:1334–9. doi: 10.1111/j.1368-5031.2005.00687.x. [DOI] [PubMed] [Google Scholar]
- 16.Spahos T, Hindmarsh A, Cameron E, Tighe MR, Igali L, Pearson D, et al. Endoscopy waiting times and impact of the two week wait scheme on diagnosis and outcome of upper gastrointestinal cancer. Postgrad Med J. 2005;81:728–30. doi: 10.1136/pgmj.2004.031104. [DOI] [PMC free article] [PubMed] [Google Scholar]