Abstract
Tubular ectasia of the rete testis is a pathologically benign process with complex and varied aetiology. It must be differentiated from neoplastic disease of the testis clinically with patient age, mode of presentation, tumour marker status and the characteristic ultrasound and Doppler study findings. Awareness and diagnosis of this clinical entity can prevent unnecessary surgical intervention in these patients.
Keywords: Tubular ectasia, Rete testis, Ultrasonography, Colour Doppler imaging
Tubular ectasia of the rete testis is a rare, benign, cystic lesion of the testis.1 As only 5% of intratesticular tumours are benign, their significance in clinical practice is important as the primary differential diagnosis is a testicular neoplasm.2 The use of ultrasonography and colour Doppler imaging is vital in its identification and, therefore, may avoid unnecessary orchidectomy.3 We report a case of tubular ectasia of the rete testis conservatively managed with the aid of ultrasonography and colour Doppler and explore recent literature behind this uncommon clinical entity.
Case report
A 64-year-old man with metastatic prostate cancer requiring goserelin acetate injections (Zoladex®) presented with a 4-month history of painless left testicular enlargement. On physical examination, the left testicle appeared both larger and firmer than the right. Both testicles were non-tender with no palpable lesion identified.
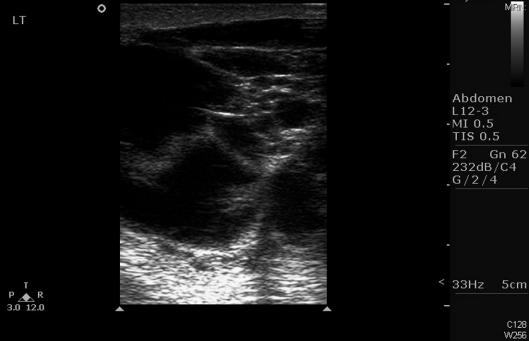
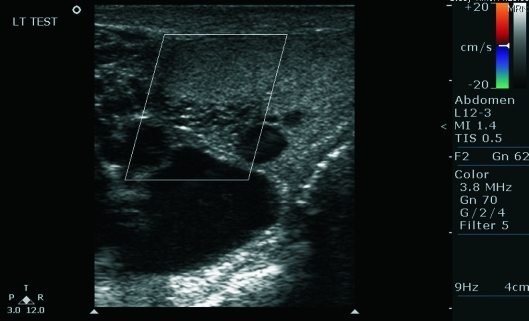
Serum tumour markers for testicular malignancy were not elevated and a scrotal ultrasound scan revealed a left testis of normal dimensions with multiple fluid filled tubular structures at its posterolateral border (Fig. 1). There were associated multiple anechoic foci within the testicular parenchyma together with a loculated left hydrocoele. Both epididymi and the right testis had normal appearances. Doppler studies showed no evidence of alteration in blood flow (Fig. 2). Overall, the appearance of the left testis was highly suggestive of intratesticular cysts with tubular ectasia of the rete testis. The patient was managed conservatively and repeat scrotal ultrasound scans at 1, 3 and 6 months demonstrated no change in pathology. Serum tumour markers during this period were also unremarkable. He continues on-going follow-up of his prostate cancer.
Figure 1.
Longitudinal view of the left hemiscrotum demonstrating a dilated rete testis and multiple, low-reflective cystic tubules.
Figure 2.
Longitudinal view of the left hemiscrotum demonstrating cystic changes with absent blood flow within the mediastinum testis on Doppler study.
Discussion
The rete testis is a complex anastomosis of seminiferous tubules located in the mediastinum testis. Their drainage is via several efferent ductules which open to form the head of the epididymis.
Tubular ectasia of the rete testis is a benign clinical entity in which cystic dilation of rete testis results from partial or complete obliteration of the efferent ducts. These spermatozoa-containing cysts communicate with the tubular system into the epididymis.
Their clinical significance lies in the distinction between other cystic lesions of the testis. Non-neoplastic cystic lesions are of two main groups: (i) those that arise from the tunica albuginea, which are generally palpable and do not communicate with the tubular system; and (ii) intratesticular cysts, of which tubular ectasia of the rete testis are an example.4 These must be differentiated from malignant testicular tumours, with particular reference to teratomas which are known to present as cystic masses within the testicular parenchyma.3
Tubular ectasia of the rete testis often represent an asymptomatic finding in men older than 55 years with unremarkable physical examination of the testes.5 The process is bilateral in approximately one-third of cases, however, it can be asymmetrical in presentation.6
The normal rete testis on ultrasonography is visualised as a region of poor echogenicity at the hilum of the testis with finger-like projections into the parenchyma.7 Tubular ectasia of the rete testis has a characteristic appearance on ultrasonography with a dilated rete testis and multiple, low-reflective, elongated, cystic swellings, usually a few millimetres in diameter. There is no demonstrable vascular flow within the mediastinum testis on Doppler studies differentiating it from an intratesticular varicocoele.7 The diagnosis can be made with a greater degree of confidence if the process is bilateral, the lesion is in the mediastinum testis, and in the presence of epididymal cysts.3,5
The pathogenesis is thought to be due to obstruction at the level of, or distal to, the efferent ductules at the epididymal head. This subsequently leads to dilation in the proximal ductal system manifesting as tubular ectasia.5
A histological study of 218 post mortem cases revealed tubular ectasia of the rete testis in 26 men, 20 of whom had evidence of obstruction in the epididymis or in the intratesticular excretory ducts.8 Aetiological factors are, therefore, varied. Mechanical compression from epididymal cysts or spermatocoeles, testicular, epididymal or spermatic cord tumours, long-standing epididymitis or traumatic haemocoeles are the most common cause. However, ischaemic, hormonal (liver cirrhosis) and congenital malformations (cryptorchidism and polyorchidism) are all thought to play a role in their respective patients.8–10
Recently, tubular ectasia of the rete testis has been observed in patients with chronic kidney disease undergoing prolonged (> 30 months) haemodialysis or peritoneal dialysis. It is thought that retention of calcium oxalate crystals has a role in the pathogenesis in these patients.11 Similar post surgical changes to the rete testis have also been reported following vasectomy, epididymal cyst excision and epididymectomy.9
Conclusions
Tubular ectasia of the rete testis is a pathologically benign process with complex and varied aetiology. It must be differentiated from neoplastic disease of the testis clinically with patient age, mode of presentation, tumour marker status and the characteristic ultrasound and Doppler study findings. Awareness and diagnosis of this clinical entity can prevent unnecessary surgical intervention in these patients.
References
- 1.Older RA, Watson LR. Tubular ectasia of the rete testis: a benign condition with a sonographic appearance that may be misinterpreted as malignant. J Urol. 1994;152:477. doi: 10.1016/s0022-5347(17)32769-6. [DOI] [PubMed] [Google Scholar]
- 2.Moghe PK, Brady AP. Ultrasound of testicular epidermoid cysts. Br J Radiol. 1999;72:942–5. doi: 10.1259/bjr.72.862.10673943. [DOI] [PubMed] [Google Scholar]
- 3.Dogra VS, Gottlieb RH, Rubens DJ, Liao L. Benign intratesticular cystic lesions: US features. Radiographics. 2001;21(Suppl):S273–81. doi: 10.1148/radiographics.21.suppl_1.g01oc15s273. [DOI] [PubMed] [Google Scholar]
- 4.Colangelo SM, Fried K, Hyacinthe LM, Fracchia JA. Tubular ectasia of the rete testis: an ultrasound diagnosis. Urology. 1995;45:532–4. doi: 10.1016/S0090-4295(99)80031-4. [DOI] [PubMed] [Google Scholar]
- 5.Tartar MV, Trambert MA, Balsara ZN, Mattrey RF. Tubular ectasia of the testis: sonographic and MR imaging appearance. AJR Am J Roentgenol. 1993;160:539–42. doi: 10.2214/ajr.160.3.8430548. [DOI] [PubMed] [Google Scholar]
- 6.Rouviere O, Bouvier R, Pangaud C, Jeune C, Dawahra M, Lyonnet D. Tubular ectasia of the rete testis: a potential pitfall in scrotal imaging. Eur Radiol. 1999;9:1862–8. doi: 10.1007/s003300050936. [DOI] [PubMed] [Google Scholar]
- 7.Stewart VR, Sidhu PS. The testis: the unusual, the rare and the bizarre. Clin Radiol. 2007;62:289–302. doi: 10.1016/j.crad.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 8.Nistal M, Mate A, Paniagua R. Cystic transformation of the rete testis. Am J Surg Pathol. 1996;20:1231–9. doi: 10.1097/00000478-199610000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Jimenez-Lopez M, Ramirez-Garrido F, Lopez-Gonzalez Garrido JD, Mantas-Avila JA, Nogueras-Ocana M, Jimenez-Verdejo A, et al. Dilatation of the rete testis: ultrasound study. Eur Radiol. 1999;9:1327–9. doi: 10.1007/s003300050842. [DOI] [PubMed] [Google Scholar]
- 10.Rajbabu K, Morel JC, Thompson PM, Sidhu P. Multi-cystic (rete testis) supernumerary testis in polyorchidism with underlying microlithiasis: ultrasound appearances. Aust Radiol. 2007;51(Suppl):B56–8. doi: 10.1111/j.1440-1673.2007.01840.x. [DOI] [PubMed] [Google Scholar]
- 11.Nistal M, Jiménez-Heffernan JA, Garcia-Viera M, Paniagua R. Cystic transformation and calcium oxalate deposits in rete testis and efferent ducts in dialysis patients. Hum Pathol. 1996;27:336–41. doi: 10.1016/s0046-8177(96)90105-7. [DOI] [PubMed] [Google Scholar]