Abstract
High rates of psychiatric impairment in adults with 22q11DS suggest that behavioral trajectories of children with 22q11DS may provide critical etiologic insights. Past findings that report DSM diagnoses are extremely variable; moreover sex differences in behavior have not yet been examined. Dimensional CBCL ratings from 82 children, including 51 with the 22q11DS and 31 control siblings were analyzed. Strikingly consistent with rates of psychiatric impairment among affected adults, 25% percent of children with 22q11DS had high CBCL scores for Total Impairment, and 20% had high CBCL Internalizing Scale scores. Males accounted for 90% of high Internalizing scores and 67% of high Total Impairment scores. Attention and Social Problems were ubiquitous; more affected males than females (23% vs. 4%) scored high on Thought Problems. With regard to CBCL/DSM overlap, 20% of affected males as compared with 0 affected females had one or more high CBCL ratings in the absence of a DSM diagnosis. Behaviors of children with 22q11DS are characterized by marked sex differences when rated dimensionally, with significantly more males experiencing Internalizing and Thought Problems. Categorical diagnoses do not reflect behavioral differences between male and female children with 22q11DS, and may miss significant behavior problems in 20% of affected males.
Keywords: VCFS, DeGeorge, ADD/ADHD, Child Behaviour Check List, sex, neuropsychiatry
1. Introduction
22q11 Deletion Syndrome (22q11DS, also referred to as DiGeorge or Velocardiofacial Syndrome) is the most common interstitial deletion and occurs in approximately 1 in 5000 live births (Botto et al., 2003). The first investigators to characterize this syndrome and follow its developmental trajectory (Shprintzen et al., 1978) reported a 90% – 100% prevalence of early learning disabilities, behavioral differences, and, by early adulthood in approximately 10% of patients, severe psychopathology resembling psychosis with paranoid delusions (diagnostic criteria were not applied) (Shprintzen et al., 1981). A subsequent study (Pulver et al., 1994) of 14 affected adults ages 17 – 41 diagnosed by DSM criteria (Diagnostic and Statistical Manual of Mental Disorders, 3rd Edition, Revised, American Psychiatric Association) reported high rates of several DSM disorders, including anxiety disorders (36%), schizophrenia (29%) and mood disorders (21%). These findings, together with a report of higher than expected rates of 22q11DS among adults with schizophrenia (Karayiorgou et al., 1995) suggested that children with 22q11DS were at broadly increased risk of mental disorders, and also that 22q11DS may provide a new inroad to the genetics of mental disorders.
Increased risk of schizophrenia in this population has received the most attention, however studies using DSM criteria and structured methods for the diagnosis of children and adults have replicated elevated rates of several disorders (Table 1, studies arranged by sample mean age). Attention Deficit Disorder is the single most frequent and consistent diagnosis occurring at rates approximately 30% – 40% higher than the national average, currently estimated to be approximately 9% of school-age children (Froehlich et al., 2007). Rates of anxiety disorders, found in approximately 13% of the general population (Costello et al., 1996), and mood disorders, are similarly inflated although agreement regarding specific mood diagnoses is low. Schizophrenia-spectrum disorders in adult populations with 22q11DS are 30% higher than in the general population (≈1%), and become apparent as study sample age increases, reflecting the inclusion of patients who have reached age of maximum risk. Thus, many DSM disorders occur throughout the lifespan among a subgroup of patients with 22q11DS. Yet an early phenotype consistent with later severe mental illness has not yet been identified perhaps because of the approaches used to date.
Table 1.
Rates of DSM Comparison of DSM Findings: DSM Axis I Diagnoses in Children, Adolescents and Adults with 22q11DS
| N | Method | age range (mean ± sd) |
NO DSM Dx |
ADD/ ADHD |
ODD | Any Mood |
MDD | Dysth | Bipolar | Any Anxiety |
Phobia Spec/Soc |
OCD | GAD | Separation Anxiety |
Schizphr/ SchizAff/ NOS |
PDD/ Autism |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 201 | InterviewK-SADS | 6 – 20 (11.0 ± 4.3) | 40% (8/20) | 35% (7/20) | 25% (5/25) | 30% (6/20) | 20% (4/20) | 15% (3/20) | 5% (1/20) | 5% (1/20) | ||||||
| 282 | Computer DICA-P Interview K-SADS | 6 – 19 (12.3 ± 3.9) | not reported | 46% (14/28) | 43% (12/28) | 18% (5/28) | 11% (3/28) | 61% (17/28) | 11% (3/28) | 29% (8/28) | 21% (6/28) | |||||
| 323 | Interview DSM-IV | 5 – 33 (12.3 ± 6.4) | 38% (12/32) | 44% (14/32) | 6% (2/32) | 6% (2/32) | 31% (10/32) | |||||||||
| 254 | Interview SCID DICA | 5 – 34 (15.6 ± 7.0) | 4% (1/25) | 36% (9/25) | 8% (2/25) | 68% (17/25) | 4% (1/25) | 8% (2/25) | 56% (14/25) | 20% (5/25) | 4% (1/25) | 8% (2/25) | 12% (3/25) | 4% (1/25) | 8% (2/25) | |
| 255 | Interview CAPA | 13 – 25 (16.4 ± 2.0) | 24% (6/25) | 48% (12/25) | 36% (9/25) | 12% (3/25) | 16% (4/25) | 40% (10/25) | 8% (2/25) | 8% (2/25) | 32% (8/25) | |||||
| 436* | Interview K-SADS SCID | 6 – 40 (18.3 ± 3.0) | 7% (3/43) | 37% (16/43) | 16% (7/43) | 21% (9/43) | 65% (28/43) | 49% (21/43) | 33% (14/43) | 14% (6/43) | 16% (7/43) | 16% (7/43) | ||||
| 147 | Interview DIS PSE | 17 – 41 (26.4 ± 6.6) | 21% (3/14) | 21% (3/14) | 36% (5/14) | 29% (4/14) | 14% (2/14) | 29% (4/14) | ||||||||
| 508 | Interview SCAN | 17 – 52 (31 ± 10) | 58% (29/50) | 14% (7/50) | 12% (6/50) | 2% (1/50) | 30% (15/50) |
(Papolos et al., 1996)
(Baker & Skuse, 2005)
(Gothelf et al., 2004)
Lifetime diagnoses, rates for “Phobia Spec/Soc” and “Any Anxiety” personal communication 1/17/05, cited with permission.
(Murphy, Jones, & Owen, 1999)
Differences in the symptom patterns of males and females with mental disorders are well-established (Piccinelli and Gomez-Homen, 1997) although these have not been explored in previous behavioral studies of children with 22q11DS. It is critical to do so. If present, such patterns could suggest important differences in the psychiatric etiology of males and females with 22q11DS. Moreover, unidentified differences in the behavior patterns of male and female children with 22q11DS at risk for later mental disorders might be expected to obscure their unique behavioral trajectories. Distinguishing behavior patterns in male and female children with 22q11DS is essential for understanding differences in the clinical needs of male and female at risk children.
A summary of past reports examining psychiatric disorders among patients with 22q11DS (Table 1.) reveals consistency of DSM domain summary rates (“any anxiety,” “any mood”), low consistency of rates for individual disorders, and high variability between studies overall, perhaps giving the impression that psychiatric symptoms in children with 22q11DS may not fit neatly into DSM syndrome categories.
For treatment purposes, DSM diagnoses are the definitive determination of affectedness. For developmental research however, ratings from empirically-based multi-dimensional taxonomies may be equally or more informative. The Child Behavior Checklist (CBCL) (Achenbach, 1979) is among the most widely used dimensional rating scales of child psychopathology. In contrast to DSM committee-consensus-defined syndromes, CBCL items were based on extremely large samples of behavior ratings, iteratively factor analyzed to identify “real-child” clusters of problem behaviors. It was not designed nor intended to overlap DSM diagnoses. Convergence of DSM diagnoses and CBCL clinically significant scores is reported to be approximately 60% (Kasius and Ferdinand, 1997), suggesting that DSM diagnoses alone can miss some severe behavioral problems in children and adolescents.
We report CBCL behavior ratings from 51 children with 22q11DS and 31 control siblings. The distributions of CBCL scale scores were examined and used to guide the choice of comparisons and statistical analyses. With regard to children with 22q11DS and sibling controls, we predicted group differences for three summary scale scores (Internalizing, Externalizing, Total Impairment). With regard to sex comparisons among children with 22q11DS, past studies have suggested that social and attention problems are ubiquitous in children with 22q11DS, and we did not expect sex differences on these CBCL scales. In the absence of any previous findings regarding behavioral differences between males and females with 22q11DS, we based our hypotheses on the clinical observations of our study team, and predicted elevated scores in males for the Withdrawn and Thought Problems scales. Algorithm-derived DSM diagnoses were completed for 35 of the children with 22q11DS. We compared these with CBCL ratings, and examined the overlap between CBCL-defined problem behaviors and DSM diagnoses in this subgroup of children with 22q11DS. Based on previous findings (Kasius and Ferdinand, 1997), we predicted overlap in 60% of cases, with the intention of paying special attention to false negatives.
2. METHODS
2.1. Participants
Eighty-two children were included in these analyses (mean age 9.2 ± 2.3), 51 with 22q11DS and 31 control siblings. Affected children ranged in age from 5.3 – 17.2 (mean 9.4 ± 2.8), siblings ranged in age from 6.1 – 13.5 (mean 6.1 – 13.5, 9.0 ± 2.1). The institutional review board of The Rockefeller University approved this project prior to data collection, and at one-year intervals. Parents learned of our project through website postings, brochures sent to genetic counselors, doctors’ offices, speech and language specialists, and parent support groups. All children were confirmed positive for the 22q11 deletion via florescence in situ hybridization (FISH) assay prior to enrollment in the study. Fluency in English was required for participation of both parents and children. Consent forms were sent to parents one month in advance of scheduled testing. The tests and testing procedures were explained to the parents by study staff and to child participants by their parents. Child verbal assent and parental informed consent were obtained on the morning of testing prior to the start of assessment procedures.
2.2. Procedures
CBCL data were collected as part of a larger study of neurocognitive and behavioral development in children with 22q11DS. Parents completed CBCL forms while their children participated in neurocognitive testing. Neurocognitive testing included the Stanford-Binet IQ Battery, NEPSY Neuropsychological Battery, Test of Everyday Attention, and additional measures assessing sensory motor gating, attention and executive function ability. A member of the study was available to answer parents’ questions regarding the meaning of particular items.
The CBCL represents an extensively standardized, empirically-based taxonomy of child problem behaviors. Composed of 112 items written for a 5th grade reading level, the scale takes approximately 20 minutes to complete. CBCL criteria for psychopathology are adjusted for age and sex, and, with one exception, each of the 112 items contributes to only one dimension. The presence of a clinically significant score on one scale does not hierarchically obviate the possibility of high scores on any or all other dimensions. To circumvent the bias that can result from a rater’s (i.e., parent’s) investment in the presence or absence of a given disorder, CBCL items are arranged alphabetically rather than by problem scale, and carefully worded to avoid implying categorical diagnostic categories.
The CBCL provides t-scores for eight individual problem scales (Withdrawn, Somatic Complaints, Anxiety/Depression, Social Problems, Thought Problems, Attention Problems, Delinquent Behavior, Aggressive Behavior), two summary dimensions including Internalizing (Withdrawn + Somatic Complaints + Anxious/Depressed ) and Externalizing (Delinquent Behavior + Aggressive Behavior), and a Total Impairment score (sum of eight problem scales), all with a mean of 50 and standard deviation of 10. T-scores were based on nationally-representative samples, and normed separately for boys and girls and by age group (ages 4 – 11 and ages 12 – 18). T-scores ≥ 70 are “clinically significant” (at or above the 98th percentile). The reliability and validity of the CBCL have been extensively documented (Achenbach, 1991).
Algorithm-derived DSM-IV diagnoses were obtained via parent interview using the Diagnostic Interview Schedule for Children – Version IV (Shaffer et al., 2000) from 35 of 51 parents of children with 22q11DS. The remaining 16 parents were unable to complete the diagnostic interview. All interviews were computer-assisted, conducted via telephone and administered by a PhD level psychologist. Length of interview depended on number of categories endorsed, and on average, required 2 hours to complete. All diagnostic data and summary reports were reviewed by a licensed psychologist following each DISC interview and again prior to data analysis.
2.3. Scoring, Database and Data Analysis
All data were entered and maintained in a Statview database and analyzed using Statview Version 3.0 for PC or SAS Version 6.0 for PC. All CBCL data were computer-scored. DSM diagnoses and their impairment scores were extracted from DISC clinical summary reports and entered and maintained in a Statview database.
Unpaired t-test was used to examine group mean age differences; chi-square was used to examine group sex distributions. Distribution and variance characteristics of all CBCL summary and problem scale scores were examined, and analyses were guided by data characteristics. When distributions were not skewed and variances did not differ, ANOVA was used to examine group by sex effects. When skewness was greater than |1|, and/or in the case of significant group variance differences that could not be corrected by log(base10) transformation, non-parametric statistics were used. Kruskal-Wallis was used when distributions were not skewed but variance differences were marked and not correctable by log transformation. Mann-Whitney U (robust to variance differences) was applied when distributions were similarly skewed. When groups differed with regard to both skew and variance, chi-square tests were used to compare frequencies of children with CBCL ≥ 98th percentile (t-scores ≥ 70).
3. RESULTS
Eighty-two children were included in these analyses. Mean age of groups did not differ (mean diff = 0.33, t = 0.56, P = 0.57) and sex distributions were approximately equivalent (χ2 = 1.9, df = 1, P < 0.17). Mean Composite IQ for children with 22q11DS was 88.7(standardization mean = 100, SD = 16), and thus within the normal range (within 1 SD from the standardization sample mean). Mean Composite IQ for sibling controls was 119.4, and thus slightly more than 1 SD above the standardization sample mean.
Summary score data (Internalizing, Externalizing and Total Impairment) and their distributions were examined by group (Table 2). Distributions by group were not skewed, and variances were approximately equivalent for Externalizing scale (var ratio30/50 = 0.75, p =0.38). An ANOVA of group by sex differences for Externalizing revealed a large effect for group (F = 21.9, P < 0.001, MSE 76.3) and no sex (F = 0.16, P = 0.69), or group by sex effect (F = 1.2, P = 0.29). However only two affected children had scores that were ≥ 98th percentile, thus while elevated overall, few affected children had clinically significant Externalizing behaviors.
Table 2.
Comparison of CBCL Ratings of Children with 22q11DS and Control Siblings
| 22q11> | Sibs≫ | |||||||
|---|---|---|---|---|---|---|---|---|
| Median(Mean) | IQR | Skew | n (%) ≥ 70 | Median(Mean) | IQR | Skew | n (%) ≥ 70 | |
| Withdrawn | 56 (58.2) | 14.00 | .9 | 8 (15.7) | 50 (51.5) | 0 | 2.6* | 0 |
| Somatic Complaints | 54 (57.4) | 10.50 | 1.2* | 8 (15.7) | 50 (51.4) | 3.00 | 2.9* | 0 |
| Anxiety/Depression | 54 (57.2) | 13.00 | 1.1* | 7 (13.7) | 50 (51.5) | 0 | 2.3* | 0 |
| Social Problems | 62 (62.4) | 14.50 | .3 | 12 (23.5) | 50 (50.4) | 0 | 1.6* | 0 |
| Thought Problems | 58 (61.1) | 15.75 | 1.2* | 7 (13.7) | 50 (50.7) | 0 | 2.7* | 0 |
| Attention Problems | 65 (63.7) | 12.75 | .2 | 13 (25.5) | 50 (51.3) | .75 | 2.9* | 0 |
| Delinquency | 50 (54.8) | 9.00 | 1.5* | 1 ( 2.0) | 50 (50.8) | 1.00 | 2.6* | 0 |
| Aggression | 53 (55.6) | 8.50 | 1.9* | 3 ( 5.9) | 50 (51.1) | .75 | 3.3* | 0 |
| Total with any subscale score ≥ 70 22 (43.1%) | 0 | |||||||
| Internalizing Scale | 52 (55.1) | 18.0 | .2 | 10 (19.6) | 43 (43.6) | 8.5 | .5 | 0 |
| Externalizing Scale | 52 (53.0) | 11.75 | .8 | 2 ( 3.9) | 42 (43.6) | 12.0 | .6 | 0 |
| Total Impairment | 60 (59.7) | 16.75 | −.8 | 12 (23.5) | 41 (42.1) | 10.5 | −.2 | 0 |
|
| ||||||||
| 22q11 Males< | 22q11 Females≪ | |||||||
| Median(Mean) | IQR | Skew | n (%) ≥ 70 | Median(Mean) | IQR | Skew | n (%) ≥ 70 | |
| Withdrawn | 59.5 (61.7) | 16.00 | .4 | 7 (26.9) | 50 (54.7) | 7.0 | 1.7* | 1 ( 4.0) |
| Somatic Complaints | 56 (60.4) | 22.00 | .7 | 7 (26.9) | 54 (54.3) | 8.00 | 1.6* | 1 ( 4.0) |
| Anxiety/Depression | 57 (60.3) | 18.00 | .5 | 6 (23.1) | 50 (54.0) | 4.00 | 2.0* | 1 ( 4.0) |
| Social Problems | 67 (64.7) | 14.00 | .1 | 7 (26.9) | 57 (60.0) | 14.00 | .7 | 5 (20.0) |
| Thought Problems | 64 (65.7) | 3.00 | .8 | 6 (23.1) | 58 (56.4) | 8.00 | .5 | 1 ( 4.0) |
| Attention Problems | 65 (64.8) | 11.00 | .3 | 6 (23.1) | 63 (62.4) | 16.00 | .3 | 7 (28.0) |
| Delinquency | 54 (55.7) | 9.00 | 1.4* | 1 ( 3.8) | 50 (53.8) | 7.00 | 1.2* | 0 |
| Aggression | 54.5 (56.5) | 10.00 | 1.9* | 2 ( 7.7) | 50 (54.6) | 7.50 | 1.3* | 1 ( 4.0) |
| Total with any subscale score ≥ 70 14 (53.8%) | 8 (32%) | |||||||
| Internalizing Scale | 62 (62.3) | 19.75 | −.4 | 9 (34.6) | 51.5 (51.9) | 8.50 | 1.3* | 1 ( 4.0) |
| Externalizing Scale | 53 (54.9) | 9.75 | .5 | 1 ( 3.8) | 50 (53.2) | 11.50 | .5 | 1 ( 4.0) |
| Total Impairment | 66 (65.1) | 10.75 | −.8 | 9 (34.6) | 55.5 (57.9) | 15.50 | .4 | 3 (12.0) |
> n = 51, 22q11
n = 31, Control Siblings
> | 1| = benchmark for significant skewedness
< n = 26, 22q11 Males
n = 25, 22q11 Females
Internalizing and Total Impairment scores were not skewed, however group variances for each differed significantly (Internalizing: var ratio30/50 =.34, P = 0.001; Total Impairment: var ratio30/50=.35, P = 0.002). Log transformation did not resolve the differences in either case, and Kruskal-Wallis Test was used to examine group by sex differences for Internalizing and Total Impairment. For Internalizing, large group differences were found (H = 21.5, df = 3, P < 0.001), and mean rank values suggested that the effect was attributable to a large overall group difference, and markedly elevated scores among affected males (mean ranks: sib males = 26.9, sib females = 29.1, 22q males = 57.6, 22q females = 41.1). A similar pattern of effects for Total Impairment was evident (H = 43.8, df = 3, P < 0.001), with mean rank values indicating a large overall group difference, and markedly elevated scores among affected males (mean ranks: sib males = 18.0, sib females = 21.9, 22q males = 61.5, 22q females = 46.7).
Comparisons of groups for individual problem scales were not possible due to marked skewing, variance differences, and no occurrences of clinically significant CBCL scores among control siblings.
Sex Comparisons in Children with 22q11DS
Examination of data for Withdrawn and Thought Problems scales revealed significant positive skewing among affected females for Withdrawn scale; distributions for Thought Problems were not significantly skewed, however variances differed markedly (var ratio25/24 = 3.2, P = 0.006) and log transformation did not resolve the difference. Chi-square was used to test for sex differences in the frequency of children at or above clinical significance on Withdrawn scale. A significant difference was found (χ2 = 5.1, df = 1, P < 0.024); 27% of males as compared with 4% of females had CBCL Withdrawn scores at or above the 98th percentile. Mann-Whitney U was used to test for sex differences among affected children on Thought Problems scale, and a significant effect was found (U = 152.0, z = 3.3, P = 0.001; mean rank males = 32.7, females = 19.1); 23% of males as compared with 4% of females had CBCL Thought Problem scores at or above the 98th percentile.
Examination of summary data (Table 2.) also suggested similar increases in clinically significant scale scores among males on Somatic Complaints and Anxiety/Depression, suggesting that the high Internalizing scales of males were attributable to high frequencies on all three contributing problem scales (and not due to elevated rates on only, for example, Withdrawn). To confirm this we conducted unplanned tests of these differences. Distributions among females were skewed for Somatic Complaints and Anxiety/Depression, and variances differed significantly (Somatic Complaints, var ratio25/24 = 3.9, p =0.001; Anxiety/Depression var ratio25/24 = 2.5, P = 0.029). Chi-square was used and sexes differed significantly for Somatic Complaints (χ2 = 5.1, df = 1, P < 0.025) and Anxiety/Depression (χ2 = 3.9, df = 1, P < 0.048).
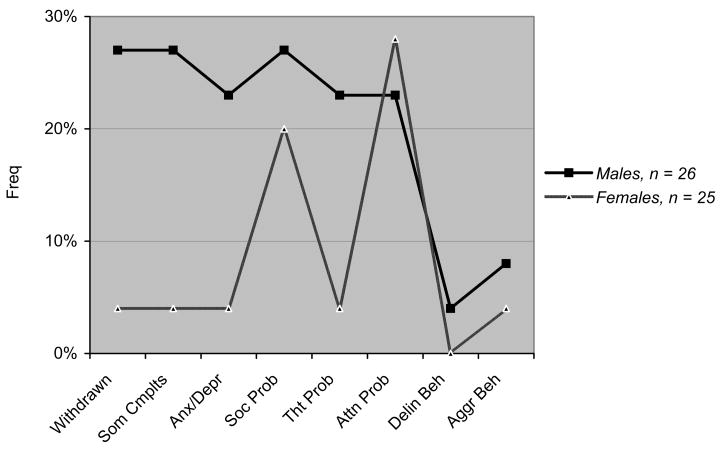
To summarize, all group median scores were below the level of clinical significance, thus group differences were attributable to the elevated scores of a subgroup of affected children. As compared with control siblings, significantly more children with 22q11DS have marked behavioral problems on CBCL Internalizing and Total Impairment, largely accounted for by the high scores in 25% and 20% of males, respectively. Relative to typically-developing controls Externalizing is elevated, but for 96% of affected children their scores are below the level of clinical significance. When individual problem scales are considered, significantly more males have CBCL scores ≥ 98th percentile on all three problem scales contributing to Internalizing (Withdrawn, Somatic Complaints, Anxiety/Depression), and significantly more males as compared with females have CBCL Thought Problems scores ≥ 98th percentile.
DSM Diagnoses in Children with 22q11DS
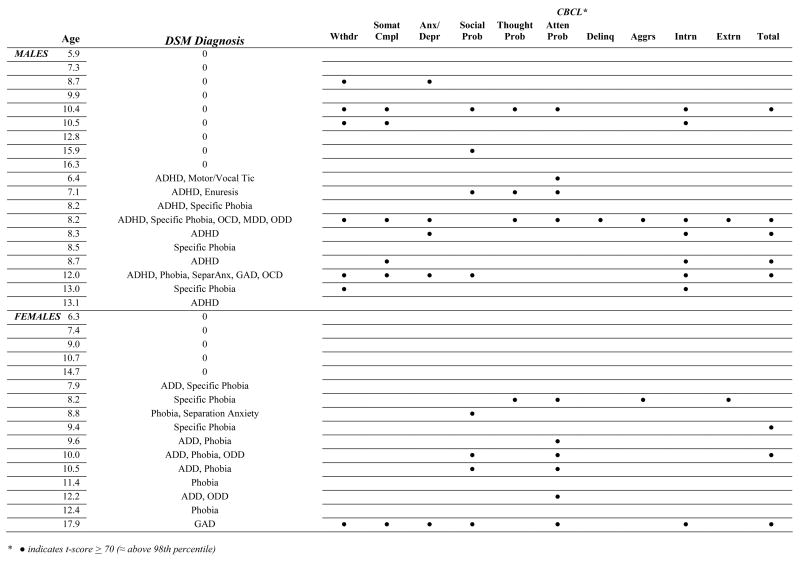
Table 3. shows DSM algorithm-derived diagnoses and mean impairment scores obtained for 35 children with 22q11DS ranging in age from 5.9 to 17.9, mean age of 10.1 (± 3.0). Figure 1. illustrates the overlap by sex of CBCL clinically significant scores and DSM diagnoses for 35 children with 22q11DS. Chi-square analysis was used to test this overlap and it was significant (χ2 = 4.9, df = 1, P < 0.03); 67% of children with clinically significant CBCL scores also met criteria for a DSM diagnosis. We then compared diagnostic overlap in males and females. Among females, DSM detected problem behaviors in the absence of clinically significant CBCL scores in 3 children, all three of whom met DSM criteria for phobia with mild impairment, while one had a co-morbid diagnosis of ADHD. Clinically significant CBCL scores were found for 12 of 15 females with a DSM diagnosis, and were not found among females without a DSM diagnosis.
Table 3.
DSM IV Diagnoses by Gender for 35 Children with 22q11DS
| N = 35 | Impairment MN (SD) | Males n = 19 | Females n = 16 | |
|---|---|---|---|---|
| ANY Diagnosis | 60% (21) | 9.4 | 53% (10) | 69% (11) |
| ADD/ADHD | 37% (13) | 9.2 (2.9) | 42% (8) | 31% (5) |
| Inattentive | 37% (13) | 42% (8) | 31% (5) | |
| Hyper/Impul | 11% ( 4) | 15% (3) | 6% (1) | |
| ODD | 11% ( 4) | 9.0 (8.5) | 11% (2) | 13% (2) |
| Conduct Disorder | 0 | |||
|
| ||||
| Any Anxiety | 43% (15) | 26% (5) | 63% (9) | |
| Specific Phobia | 40% (14) | 3.5 (2.4) | 26% (5) | 56% (9) |
| Social Phobia | 0 | |||
| Agoraphobia | 0 | |||
| OCD | 6% (2) | 11.5 (.71) | 11% (2) | 0 |
| GAD | 6% (2) | 14.0 (2.8) | 5% (1) | 6% (1) |
| Separation Anx | 6% (2) | 13.5 (2.1) | 5% (1) | 6% (1) |
| Panic | 0 | |||
| PTSD | 0 | |||
|
| ||||
| Any Mood | 3% (1) | 5% (1) | 0 | |
| MDD | 3% (1) | 12.0 | 5% (1) | 0 |
| Dysthymia | 3% (1) | 17.0 | 0 | 1 (6%) |
| Bipolar | 0 | |||
| Mania | 0 | |||
| Hypomania | 0 | |||
|
| ||||
| Enuresis | 3% (1) | 0 | 5% (1) | 0 |
| Encopresis | 0 | |||
| Motor Tic | 3% (1) | 4.0 | 5% (1) | 0 |
| Tourette’s | 0 | |||
| Trichotillomania | 0 | |||
| Mutism | 0 | |||
| Anorexia | 0 | |||
| Bulimia | 0 | |||
| Pica | 0 | |||
|
| ||||
| Schizophrenia | 0 | |||
| PDD/Autism | 0 | |||
Figure 1.
Comparison of CBCL Scores and DSM Diagnoses
Males were very similar to females in all respects except for one. Like the females, DSM diagnoses indicated problem behaviors in the absence of clinically significant CBCL scores in 3 male children, and all three met DSM criteria for phobia with mild impairment, and one had co-morbid ADHD. Clinically significant CBCL scores were found in 8 of 11 males with a diagnosis DSM. However, unlike the females, 21% of males overall, and 44% of males without a diagnosis, had clinically significant CBCL scores.
4. DISCUSSION
This study included 82 children, 51 with 22q11DS and 31 control siblings with similar mean age and sex distributions. An initial review of the CBCL summary data revealed that none of the summary or problem scale score medians were at or above the level of clinical significance (t-score ≥ 70, 98th percentile). Thus, significant group differences would suggest elevated frequencies of individual children with clinically significant scores, and did not indicate significant impairment among a majority of children with the 22q11DS.
Comparisons of children with 22q11DS and control siblings revealed broad differences. Externalizing scale scores differed between groups, however only two of fifty-one affected children (4%) had clinically significant scores, modifying the interpretation of this finding. For Internalizing and Total Impairment scales, 20% and 24% of children with 22q11DS, respectively, had scores at or above the level of clinical significance. With regard to individual problem scales, a substantial proportion of both males and females had severe Social Problems and Attention Problems, while a very low percentage of males and females with 22q11DS had problems related to delinquent or aggressive behavior. No controls had scores in the clinically significant range.
Sex comparisons among children with 22q11DS revealed a unique pattern of impairment among affected males that has not been previously reported. Substantially greater proportions of males had clinically significant scores on Internalizing, on each of the problem scales that comprise Internalizing, (Withdrawn, Somatic Complaints, Anxiety/Depression subscales) and on Thought Problems. Table 1 shows the contrast in CBCL profiles of affected males and females, and illustrates that the early behavioral phenotype of children with 22q11DS is markedly influenced by sex.
The rate of any DSM diagnosis for 35 children in this sample (60%) closely approximated previous reports based on samples with similar mean ages (Arnold et al., 2001; Niklasson et al., 2001). (Note: as sample mean age and/or standard deviations increase, variability of diagnostic rates increases). The rate of Attention Deficit Hyperactivity Disorder in this sample (37%) is close to those reported in other studies, supporting the conclusion that ADHD is the most stable and consistent diagnosis in patients with 22q11DS. Additional studies of adults with 22q11DS are needed to examine how frequently ADHD in this population continues into adulthood.
Rates of anxiety disorders vary broadly across previous studies regardless of sample mean age, and range from 5% – 65%. This could reflect uncertainty regarding the “best-fit” DSM categorization for reported behavior problems. Our rates closely approximated two of eight previous studies (Table 1). Rates of mood disorders also varied broadly across studies, from 14% – 68%. In this sample, we found one of the lowest rates of mood disorders reported thus far (3%), possibly attributable to the low mean age and narrower age range of this sample. Of special note, behavioral differences among males were not evident in the rates of DSM disorders. The only sex difference suggested is in the higher rate of Specific Phobia among females.
When clinically significant CBCL scores were compared with DSM diagnoses, further evidence of behavioral differences in males emerged. Overlap between clinically significant CBCL ratings and DSM diagnoses was 67% overall, closely approximating previous findings (Kasius and Ferdinand, 1997). In both males (3) and females (3) positive for a DSM diagnosis and negative for a clinically significant CBCL score, all met criteria for DSM Specific Phobia, and two (1 male, 1 female) had co-morbid ADHD. On the other hand, while males had substantially higher rates of clinically significant CBCL scores, fewer met DSM criteria for any disorder, and unlike females, nearly half of males with no DSM diagnosis had CBCL scores at or above the 98th percentile.
With regard to DSM diagnoses, the behavior problems of children with 22q11DS seem to most closely approximate ADHD and Phobia (of relatively mild impairment), however CBCL scores suggest a much broader array of serious behavior problems among some children. DSM diagnoses among females identified well those girls with behavioral problems, and problems indicated by CBCL clinically significant scores (predominance of attention and social problems) were roughly consistent with the DSM diagnoses assigned. DSM diagnoses however did not detect 21% of males with significant behavioral problems, particularly with regard to Internalizing behaviors (Withdrawn, Somatic Complaints, Anxiety/Depression).
While no previous published studies have compared CBCL ratings of children with 22q11DS and typically-developing control siblings, four previous studies have compared CBCL data from children with the 22q11DS to controls with developmental learning delays and without a known genetic abnormality. Three of these reports included standard scores facilitating data comparisons. In one study, CBCL summary and problem scale score means of 31 children with 22q11DS and 24 speech/language-impaired controls (ages 6 – 11) were compared. Elevated scores only on Withdrawn problem behavior scale were found (Swillen et al., 2001). The second study compared CBCL summary and problem scale score means of 28 children with 22q11DS and 29 developmentally delayed children matched for age and IQ range, and no differences were found (Feinstein et al., 2002). Group similarities suggested that the behavioral profiles of children with 22q11DS were not unique to their genetic condition. However, several uncontrolled factors could have influenced results.
Distributions and variances of CBCL scale scores in these previous studies of children with 22q11DS were not reported. While CBCL summary scale data (Internalizing, Externalizing, Total Impairment) are more likely to be normally distributed, CBCL problem scale score distributions frequently are not normally distributed (Achenbach, 1991). Additionally, variance differences between groups are common and violate the assumptions of parametric statistics. Similar to the data presented here, no mean scores in the past studies were at the level of clinical significance (t-score ≥ 70), and the frequencies of scores at or above this level were not reported. Furthermore, sex effects have not been previously examined and, if present, could obscure results. Finally, a third study reporting CBCL data of children with 22q11DS (Bearden et al., 2005) suggests the possibility of another influencing factor. In a comparison of CBCL ratings in two genetic subtypes of children with 22q11DS (COMT Val/-vs. Met/- functional polymorphism), children with the Val/- genotype had markedly higher behavioral ratings on Total Impairment and Internalizing scales, and smaller though significant differences on Withdrawn, Social Problems and Delinquency problem scales. While this study also used parametric statistics, when replicated, the combined effect of sex and Val/- on early behavior may be important to examine.
Several issues should be considered in the interpretation of these findings. The CBCL is a parent rating scale. While the CBCL authors included several safeguards to reduce rater bias (discussed above) it cannot be eliminated entirely, and could influence results. Replications are necessary to determine the extent to which the findings here reported represent the behavioral profiles of males and females with 22q11DS. Potentially biasing factors may be more likely to confound categorical diagnoses, where the disorders being queried are relatively transparent to an informant who recognizes diagnostic nomenclature. Rates of DSM disorders among children with 22q11DS vary widely. More studies with matched methods including children of a relatively restricted age range are needed. Past studies have examined the association between IQ and behavior (e.g., Kusche et al. 1993; Cook et al., 1994; Goodman 1995; Loney et al. 1998; Dietz et al., 1999). These studies raise very interesting possibilities regarding a “third variable” simultaneously influencing neurocognitive and behavioral development. While we are very interested in studies of this kind, examining the interaction of these constructs was beyond the scope of this paper, and IQ was reported only for descriptive purposes.
The interpretation of the Somatic Scale among children with possible co-morbid medical conditions requires special consideration. Prior to data analyses, Somatic scale scores were individually examined for affected children with and without ongoing medical conditions. No obvious score differences were apparent, and informal comparisons of scale scores were consistent with these observations. Furthermore, the pattern of high scores among affected children paralleled those of the other scales contributing to Internalizing summary scale. Had male and female affected children scored uniformly high on the Somatization scale, the interpretation of results would have been different. With regard to this issue, it is also important to note that the CBCL is an atheoretical measure of early problems that cluster together in children. High scores are not intended to carry any implication regarding the source of rated behaviors.
DSM diagnoses were available for only 70% of affected children, and cell sizes were too small to statistically examine the specificity of DSM overlap with individual CBCL problem scales. A larger sample would have allowed for greater specification. Limited cell sizes allowed for only a descriptive interpretation of overlap data. This sample was predominantly Caucasian. Additional studies are needed to determine the relevance of these findings to other races.
CBCL ratings for one-quarter of affected children in this sample indicated severe behavioral impairment with special vulnerability to social and attention problems, and among males, to severe internalizing behavior and thought problems. More than one-half of affected children met DSM criteria for one or more disorders. This suggests substantial clinical need among a subgroup of children with 22q11DS that should be addressed separately from their ongoing academic and possible medical needs. All children with 22q11DS should be routinely screened for these disorders and appropriate treatment provided.
With regard to research, following replication, the findings presented here might be useful for hypothesizing risk in longitudinal studies, and for further examining, prospectively and retrospectively, associations between sex and behavior in 22q11DS, and the contribution of sex to psychiatric outcome. How many prospectively identified children are at risk of later severe mental illness can only be determined with longitudinal data that characterize young children into the age of maximum risk. For the welfare of the majority of children with 22q11DS that will never develop a severe mental illness, it is essential that conclusions are carefully examined, and pointedly conservative. It is critical to avoid regarding all children with 22q11DS as having “a little tendency” toward severe mental illness. Research findings are quickly reinterpreted for websites accessed by parents and educators. Inaccurate psychiatric stereotypes can fuel stigma and wrongful assumptions by educators and professionals, which could seriously limit children’s potential for academic and social advancement.
Figure 2.
Frequencies of Clinically Significant CBCL Scores (≥ 98th Percentile) in Males and Females with 22q11DS
Acknowledgments
This research was supported by a grant from the Child Health and Human Development Branch of the National Institutes of Health (K08–HD040321, CS) and also by a General Clinical Research Center grant (M01–RR00102) from the National Center for Research Resources, National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM. The Child Behavior Profile: An empirically based system for assessing children’s behavioral problems and competencies. International Journal of Mental Health. 1979;7:24 – 42. [Google Scholar]
- Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 Profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- Arnold PD, Siegel-Bartelt J, Cytrynbaum C, Teshima I, Schachar R. Velo-cardio-facial syndrome: Implications of microdeletion 22q11 for schizophrenia and mood disorders. American Journal of Medical Genetics. 2001;105(4):354–362. doi: 10.1002/ajmg.1359. [DOI] [PubMed] [Google Scholar]
- Bearden CE, Jawad AF, Lynch DR, Monterossso JR, Sokol S, McDonald-McGinn DM, Saitta SC, Harris SE, Moss E, Wang PP, Zackai E, Emanuel BS, Simon TJ. Effects of COMT genotype on behavioral symptomatology in the 22q11.2 Deletion Syndrome. Child Neuropsychology. 2005;11(1):109–17. doi: 10.1080/09297040590911239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botto LD, May K, Fernhoff PM, Correa A, Coleman K, Rasmussen SA, Merritt RK, O’Leary LA, Wong LY, Elixson EM, Mahle WT, Campbell RM. A population-based study of the 22q11.2 deletion: phenotype, incidence, and contribution to major birth defects in the population. Pediatrics. 2003;112(1 Pt 1):101–7. doi: 10.1542/peds.112.1.101. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Angold A, Burns BJ, Stangl DK, Tweed DL, Erkanli A, Worthman CM. The Great Smoky Mountains Study of Youth. Goals, design, methods, and the prevalence of DSM-III-R disorders. Archives of General Psychiatry. 1996;53:1129 – 1136. doi: 10.1001/archpsyc.1996.01830120067012. [DOI] [PubMed] [Google Scholar]
- Feinstein C, Eliez S, Blasey C, Reiss AL. Psychiatric disorders and behavioral problems in children with velocardiofacial syndrome: Usefulness as phenotypic indicators of schizophrenia risk. Biological Psychiatry. 2002;51(4):312–318. doi: 10.1016/s0006-3223(01)01231-8. [DOI] [PubMed] [Google Scholar]
- Froehlich TE, Lanphear BP, Epstein JN, Barbaresi WJ, Katusic SK, Kahn RS. Prevalence, Recognition, and Treatment of Attention-Deficit/Hyperactivity Disorder in a National Sample of US Children. Archives of Pediatric and Adolescent Medicine. 2007;161:857–864. doi: 10.1001/archpedi.161.9.857. [DOI] [PubMed] [Google Scholar]
- Karayiorgou M, Morris MA, Morrow B, Shprintzen RJ, Goldberg R, Borrow J, Gos A, Nestadt G, Wolyniec PS, Lasseter VK, et al. Schizophrenia susceptibility associated with interstitial deletions of chromosome 22q11. Proceedings of the National Academy of Sciences of the United States of America. 1995;92(17):7612–6. doi: 10.1073/pnas.92.17.7612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasius MC, Ferdinand RF. Associations between different diagnostic approaches for child and adolescent psychopathology. Journal of Child Psychology and Psychiatry. 1997;38(6):625–632. doi: 10.1111/j.1469-7610.1997.tb01689.x. [DOI] [PubMed] [Google Scholar]
- Niklasson L, Rasmussen P, Oskarsdottir S, Gillberg C. Neuropsychiatric disorders in the 22q11 deletion syndrome. Genetics in Medicine. 2001;3(1):79–84. doi: 10.1097/00125817-200101000-00017. [DOI] [PubMed] [Google Scholar]
- Piccinelli M, Gomez-Homen F. Gender differences in the epidemiology of affective disorders and schizophrenia. Geneva: World Health Organization; 1997. [Google Scholar]
- Pulver AE, Nestadt G, Goldberg R, Shprintzen RJ, Lamacz M, Wolyniec PS, Morrow B, Karayiorgou M, Antonarakis SE, Housman D, et al. Psychotic illness in patients diagnosed with velo-cardio-facial syndrome and their relatives. Journal of Nervous & Mental Disease. 1994;182(8):476–8. doi: 10.1097/00005053-199408000-00010. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39(1):28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Shprintzen RJ, Goldberg RB, Lewin ML, Sidoti EJ, Berkman MD, Argamaso RV, Young D. A new syndrome involving cleft palate, cardiac anomalies, typical facies, and learning disabilities: velo-cardio-facial syndrome. Cleft Palate J. 1978;15(1):56 – 62. [PubMed] [Google Scholar]
- Shprintzen RJ, Goldberg RB, Young D, Wolford L. The velo-cardio-facial syndrome: a clinical and genetic analysis. Pediatrics. 1981;67(2):167–72. [PubMed] [Google Scholar]
- Swillen A, Devriendt K, Ghesquiere P, Fryns JP. Children with a 22q11 deletion versus children with a speech-language impairment and learning disability: behavior during primary school age. Genetic Counseling. 2001;12(4):309–17. [PubMed] [Google Scholar]