SYNOPSIS
Stillbirths, those with and without birth defects, are an important public health topic. The National Center on Birth Defects and Developmental Disabilities at the Centers for Disease Control and Prevention conducted two workshops during April and July 2005. Both workshops explored the challenges of conducting surveillance of stillbirths. Workshop participants considered an approach that added the surveillance of stillbirths, those with and without birth defects, as part of existing population-based birth defects surveillance programs in Iowa and Atlanta. The workshops addressed three key aspects for expanding birth defects programs to conduct active, population-based surveillance on stillbirths: (1) case identification and ascertainment, (2) data collection, and (3) data use and project evaluation. Participants included experts in pediatrics, obstetrics, epidemiology, maternal-fetal medicine, perinatology and pediatric pathology, midwifery, as well as practicing clinicians and pathologists. Expanding existing birth defects surveillance programs to include information of stillbirths could potentially enhance the data available on fetal death reports and also could benefit such programs by improving the ascertainment of birth defects.
Fetal deaths are an important public health problem with a tremendous emotional and psychological impact on families,1,2 and those that occur at 20 or more weeks of gestation (i.e., stillbirth or late fetal death) account for less than 1% of all births but nearly one-half of all perinatal deaths.3 In 2004, about 4.1 million live births and 25,655 stillbirths (fetal deaths at 20 or more weeks of gestation) were registered in the U.S.4 Significant racial disparity exists in the occurrence of stillbirths, with rates among non-Hispanic African American mothers at two to three times the rate of non-Hispanic white mothers.5–10 A number of risk factors for stillbirth have been identified, including low socioeconomic status, very young and advanced maternal age, obesity, multigravida, smoking, hypertension, diabetes, and congenital anomalies;11–23 however, the factors that contribute to most stillbirths remain unknown.24–26
One of the challenges to conducting epidemiologic studies of stillbirth has been the limited availability of reliable population-based surveillance data. By law, fetal deaths must be reported in the United States; however, reporting requirements and, to a lesser extent, the criteria used to define fetal death vary.27 As a result, the use of fetal death reports (FDRs) as a source of surveillance data has been problematic.27–36
In 2005, two birth defects surveillance programs, the Metropolitan Atlanta Congenital Defects Program (MACDP) and the Iowa Registry of Congenital and Inherited Disorders (IRCID), initiated pilot studies to examine the feasibility of leveraging the resources of existing birth defects surveillance programs to conduct surveillance of stillbirths. MACDP and IRCID are population-based birth defects surveillance systems that use active case finding methods to identify all infants or fetuses with birth defects. Trained abstractors regularly visit birth hospitals, pediatric hospitals, specialty clinics, and perinatal offices to systematically search available data sources for cases of birth defects.
MACDP was established in 1967 and is currently administered by the National Center on Birth Defects and Developmental Disabilities at the Centers for Disease Control and Prevention; it is described in detail elsewhere.37 IRCID was established in 1983 through the joint efforts of the University of Iowa, the Iowa Department of Public Health, and the Iowa Department of Human Services, and is located within the College of Public Health at the University of Iowa.38 The common objectives of these two stillbirth surveillance pilot projects are: (1) to evaluate the feasibility of expanding a population-based birth defects surveillance system to incorporate data from existing medical records on fetal deaths, (2) to monitor and report on the occurrence of fetal deaths in the surveillance population, (3) to serve as a registry for etiologic studies on fetal deaths, and (4) to serve as a resource for education and evaluation of prevention programs.
Using existing population-based birth defects registries that employ active case finding is a potentially novel approach to address the data gaps and limitations in FDRs. This approach is both advantageous and beneficial to birth defects surveillance programs for three primary reasons. First, it is more efficient because existing birth defects programs have the necessary infrastructure already in place to incorporate surveillance data on stillbirths. Second, existing programs that are responsible for surveillance of birth defects would benefit directly from these expanded activities because intensifying surveillance on stillbirths likely will increase the identification and ascertainment of birth defects.39 Third, this approach may guide our understanding of the etiology of deaths occurring at various gestational ages. Furthermore, these intensified surveillance activities have the potential to inform, complement, and enhance existing fetal/infant mortality programs, and such programs should be involved in the development, implementation, and utilization of these surveillance activities when possible.
As a first step to planning for these pilot projects, two expert workshops were conducted during April and July 2005 to address three key aspects for active, population-based surveillance on stillbirths: (1) case identification and ascertainment, (2) data collection, and (3) data use and project evaluation. The primary objective for both workshops was to provide guidance on the implementation of the two pilot studies at IRCID and MACDP. Secondary discussion related to how other state-based birth defects surveillance programs might incorporate similar activities, including benefits and barriers. The objectives of the first workshop were to identify and address issues related to case definition and ascertainment, data collection and quality, and data use and project evaluation. The objective of the second workshop was to review approaches and challenges to the clinical-pathological aspects of stillbirth evaluation. Participants in these workshops included experts in obstetrics, maternal-fetal medicine, perinatology, midwifery, pediatrics, epidemiology, and pediatric pathology. This article summarizes the key findings of these two workshops.
CASE IDENTIFICATION AND ASCERTAINMENT
The first workshop addressed two essential issues: (1) establishing criteria for what to include as a stillbirth case and (2) identifying sources for case ascertainment. These issues were discussed to clarify active surveillance of stillbirths (or late fetal deaths) within the existing framework of each participating birth defects surveillance program.
Definitions
There is no universally accepted definition of stillbirth that includes the criteria for gestational age or birthweight. The World Health Organization defines fetal death as “death before the complete expulsion or extraction from its mother of a product of conception, irrespective of the duration of pregnancy; the death is indicated by the fact that after such separation, the fetus does not breathe or show any other evidence of life, such as beating of the heart, pulsation of the umbilical cord, or definite movement of voluntary muscles.”40 The 1992 Revision of the Model State Vital Statistics Act and Regulations (Model Law) further clarifies this definition: “Heartbeats are to be distinguished from transient cardiac contractions; respirations are to be distinguished from fleeting respiratory efforts or gasps.”41 The National Center on Health Statistics (NCHS) uses this adapted definition of fetal death. The Model Law further recommends the reporting of fetal deaths based on weight (≥350 grams) and gestational age (≥20 completed weeks of gestation).42 The majority of states require reporting at 20 weeks of gestation or longer, but reporting requirements vary by state.27
Workshop participants suggested two reasons to include the surveillance criteria of fetal deaths occurring at 20 or more weeks of gestation, or at 350 or more grams of weight, if the gestational age is not known. First, this inclusion is similar to the reporting requirements of most states and with the criteria NCHS uses when it reports national estimates on fetal death. Second, these gestational age and weight criteria reflect the lower limits that an active-based surveillance program could reasonably expect to capture. Fetal deaths that meet these criteria are usually managed in a hospital setting—sources of data with which active birth defects programs are already familiar.
Data on fetal deaths occurring at much lower gestational ages would require extensive resources to capture, and most programs would be unable to afford or justify the resources. It has been shown that lowering the gestational age range for reporting fetal deaths results in more complete reporting of fetal deaths. Moreover, because estimates of gestational age can be inexact, workshop participants suggested identifying and reviewing the records for fetal deaths beginning at 18 weeks of gestation to help improve the completeness of ascertainment for those deaths at 20 weeks of gestation and longer.4 It is possible that some fetal deaths recorded as occurring at 18 or 19 weeks of gestation may in fact be growth-restricted fetuses at 20 or more weeks of gestation. It is important to review these cases to render a judgment regarding inclusion based on information in the clinical record.
Stillbirths and induction of labor
Additional issues about case definition and inclusion concerned cases in which labor was induced with the intention of terminating the pregnancy. Cases in which labor induction is performed as medical management for intrauterine fetal death (IUFD) should, of course, be included as stillbirths, assuming the gestational age or birthweight criteria is met, as the fetus already has expired before the intervention. However, a fetal death certificate may be issued for induced termination of pregnancy (ITOP), or the purposeful termination of pregnancy for birth defects, inevitable losses (chorioamnionitis with preterm premature rupture of membranes and labor), and maternal medical complications (severe preeclampsia). These situations pose unique challenges for surveillance.
The Model Law includes the following definition for ITOP: “Induced termination of pregnancy means the purposeful interruption of an intrauterine pregnancy with the intention other than to produce a live born infant and which does not result in a live birth. This definition excludes management of prolonged retention of products of conception following fetal death.” The medical record, however, may not contain the information necessary to determine whether the fetus had expired prior to the medical intervention, such as documentation of absent fetal heart tones, or a statement clearly indicating a fetal demise had occurred.
The extent to which ITOPs are misclassified as fetal deaths, and the circumstances in which they occur, are largely unknown. Workshop participants suggested that initial pilot studies investigate and further explore these issues about potential misclassification. Initial studies could use data from cases of birth defects medically managed by ITOPs ascertained by MACDP and IRCID for this purpose. These data are available and could be used to evaluate potential misclassification in FDRs. Participants also suggested that standardization of obstetrical documentation in these situations could prove helpful. Lastly, workshop participants suggested that guidelines and methods would need to be developed that incorporate all available clinical information to systematically determine inclusion status.
Out-of-hospital deliveries
Deliveries that occur outside of the hospital setting, in the absence of medical personnel, and then are presented to the hospital as a death are another consideration for case inclusion criteria. Under these circumstances, it is not always possible to determine whether the fetus was stillborn, or if the fetus lived for any length of time. In localities where a medical examiner is required to evaluate these deaths, information from their reports should be used to make this determination. If no medical examiner's report is available, then the information in the medical record can be used. In either case, a variable should indicate the location of delivery with documentation of the circumstances surrounding the delivery. This additional information will allow for these cases to be included in a surveillance system, as well as provide a method of evaluating and reporting these cases as a distinct group.
Assessment of gestational age
The workshop participants raised several issues regarding how gestational age is determined for fetal deaths. Often, the date of fetal death and the date of delivery are the same, but in some cases, the date of delivery may follow the date of fetal death by several days or longer—up to two weeks in some cases.43 From a clinical perspective, the most accurate method for determining gestational age is considered to be early ultrasonography in the first trimester using the crown-rump length for dating.44 If no early ultrasound is available, then the physician's estimate or the date of the patient's last menstrual period can be used. Information should also be recorded that indicates whether a pregnancy resulted from assisted reproductive technology. The accurate determination of gestational age has important implications for public health research.45 For surveillance purposes, the workshop participants suggested that all of these gestational age estimates be collected so that studies considering gestational age could be conducted using a variety of methods.
Case finding
Workshop participants indicated that multiple sources would be required to ensure comprehensive case ascertainment. While fetal death is a reportable event by law in the United States, studies have shown that early stillbirths (i.e., deaths during 20–27 weeks of gestation) are underreported.27,29 Furthermore, the extent to which ITOPs and nonviable live births are misclassified is not well documented. Therefore, additional sources are needed, and programs employing active case finding are methodologically well suited to fulfill this need.
Existing sources for case finding used by birth defects surveillance programs to identify birth defect cases also can be used to identify stillbirths. These existing sources include birth hospitals, labor and delivery units, genetic testing laboratories, and perinatal offices. The pathology departments of pediatric hospitals also can be used to identify fetuses referred for autopsy by a perinatal pathologist. For birth hospitals, the disease indices lists (i.e., International Classification of Diseases, Ninth or Tenth Revision) used by the abstractors to identify potential cases should be updated to include codes that reflect the occurrence of a possible IUFD. An IUFD diagnosed at a perinatal specialty office also can be captured, if such locations are visited, with case follow-up and abstraction performed at the referral hospital for management and delivery.
For the pilot phase of each project, workshop participants encouraged the inclusion of additional data sources to assess their ascertainment value. Examples included emergency room departments and emergency medical service logs to assess how pregnancy complications or home births resulting in stillbirth are managed in the emergency room. This assessment might be particularly beneficial in areas where home birthing is more common. In addition, outpatient clinics affiliated with a birth hospital should be visited to assess whether IUFD would be managed in these settings. Birthing hospitals located in the surrounding counties that could potentially serve the residents of a surveillance population should also be visited.
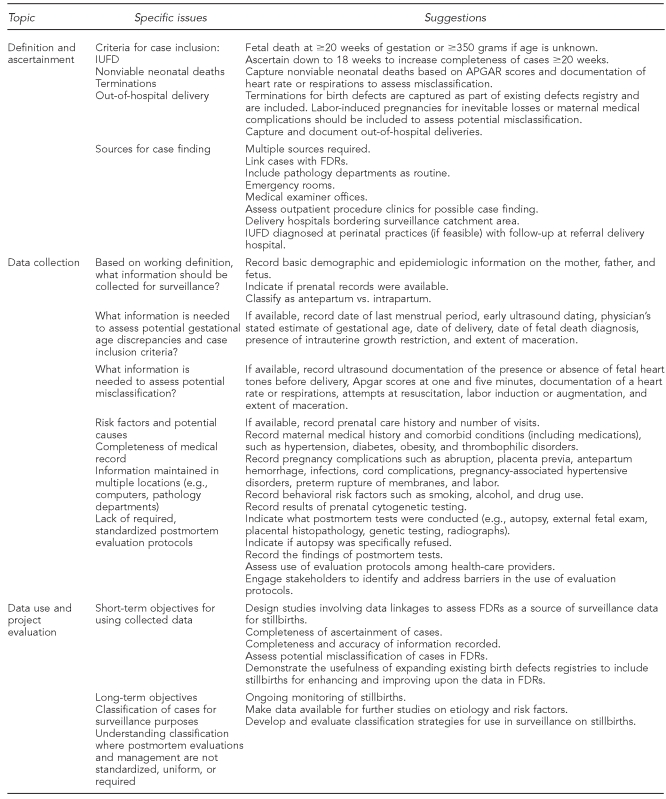
The findings regarding definitions and case ascertainment are summarized in the Figure.
Figure.
Summary of discussion issues and suggestions by topic during two workshops on stillbirth surveillance, April and July 2005
IUFD = intrauterine fetal death
FDR = fetal death report
DATA COLLECTION
Upon development of a working case definition for ascertainment of fetal deaths at ≥20 weeks of gestation, or ≥350 grams if the gestational age is not known, the panel of experts was asked what information should be collected. The panel was reminded that the collected information was for surveillance purposes, rather than research; thus, each program would be limited to medical chart review. Existing birth defects surveillance programs already contain the methods and infrastructure to collect basic demographic and epidemiologic information on the mother, the father, and the fetus. This information reflects the absolute minimum of data collection for monitoring purposes. Ample information must be collected to properly evaluate whether a case meets the inclusion criteria. This information includes the following: date of the last normal menses, early ultrasound dating, physician's estimate, date of delivery, date of fetal death diagnosis, presence of intrauterine growth restriction, and maceration.
For proper classification of pregnancy outcomes, additional information should be recorded. The presence of a heart rate or of definite respirations at delivery (recording Apgar scores or other documentation) will aid in properly differentiating between cases of fetal death and live births. Recording whether resuscitation efforts were attempted also will help to provide some clinical context to the delivery. Likewise, documentation of fetal heart tones (present or absent) on admission to labor and delivery, and if labor was induced or augmented, will aid in determining whether induction was conducted for medical management for fetal death, or as an intervention to terminate pregnancy because of a complication. If present, the degree of maceration also should be recorded. If the timing of death can be determined, it should be recorded to distinguish antepartum vs. intrapartum events.
A number of issues affect the availability and completeness of information in the medical record. The record may contain all or part of the prenatal obstetric history, and indicating whether this information was available at the time of abstraction, along with the number of prenatal visits, would be important. Postmortem evaluations such as autopsy, placental histopathology, radiographs, and cytogenetic and laboratory testing may have been conducted, and data collection and interpretation could be enhanced by indicating if these tests were done and whether the results were available at the time of abstraction. For a case in which test results could not be found in the medical record, other sources such as pathology, radiology, cytogenetic, and laboratory departments can be explored in an attempt to gather this information.
Postmortem evaluations pose special challenges for stillbirth surveillance. The collection of information in a systematic and consistent manner is important for the accurate and complete monitoring of stillbirths; however, there are no national standard guidelines or standard reporting procedures for evaluating stillbirths. Parental refusal, inadequate consenting procedures, reimbursement, and extensive fetal maceration also influence whether an adequate postmortem evaluation was performed. Placental histopathology, although frequently performed in cases of stillbirth, is often inadequate. The state of Iowa has made great progress in its attempt to overcome these limitations by developing and promoting a statewide stillbirth evaluation protocol. Use of the protocol is voluntary; however, a statewide perinatal care team regularly visits birthing hospitals to promote and provide education on using the protocol (Figure).
DATA USE AND PROJECT EVALUATION
Although two long-term strategic goals for these pilot projects are to establish ongoing enhanced surveillance of stillbirths and to provide a registry for further etiologic studies, the most immediate beneficial uses of the collected data would be for evaluative purposes to inform on many of the issues described previously. This information could be used to evaluate the limitations of vital statistical data as a source of surveillance data for stillbirths. These studies should provide guidance on completeness of case ascertainment, and they should evaluate the extent of potential misclassification of fetal deaths, live births, and ITOPs. This knowledge can be used to improve vital statistics programs.
Data linkage is a useful methodology for this work. It is well known that the recording of birth defects on birth certificates is unreliable;46,47 however, limited information is available about the reporting of defects on fetal death certificates.28,32,34 Using active birth defects programs as a comparison, the sensitivity, specificity, and positive predictive value of FDRs to record birth defects can be assessed. Likewise, the variables appearing on the FDRs can be benchmarked against active-based data abstraction methods to assess the records' completeness and accuracy. Fundamentally, an evaluation of these projects needs to show improvement of currently available information on FDRs, as well as improvements in the quantity and quality of data collected. Lastly, collaboration with stakeholders can be beneficial for raising awareness, promoting education, and developing and communicating prevention strategies (Figure).
DISCUSSION
Existing birth defects surveillance programs provide the necessary infrastructure and methodology to expand their surveillance capabilities to include stillbirths. Workshop participants agreed that clear definitions describing both ascertainment and reporting criteria of cases need to be established, with guidelines describing a systematic approach to reviewing the data. These guidelines should be consistent with the current approaches outlined in the Model Law and employed by NCHS for fetal deaths. These guidelines should include clear definitions and how to record the information sometimes necessary to distinguish among nonviable live births, antepartum and intrapartum fetal deaths, and ITOPs.
The collection of data for enhanced surveillance of stillbirths can be challenging and has many limitations and barriers to obtaining complete and accurate information. The extent of information to be collected will depend largely on program capabilities; however, basic demographic information is a minimum for data collection. Recommendations are needed to develop a standardized dataset for population-based surveillance of stillbirths. The ideal dataset would potentially reflect all available information necessary to inform on strategies to reduce risk factors, potential causes, and associated conditions with each event. Fetal autopsy and placental histopathology are two essential components to an adequate evaluation, but often they are not routinely performed in a systematic fashion. Long-term strategies involving multiple stakeholders are needed to improve the quality of data generated and recorded when stillbirth occurs. These strategies include the development of guidelines for postmortem evaluation, along with awareness, education, and training for health-care providers in the appropriate use of these protocols and guidelines. Likewise, ongoing awareness and training are needed at the state level to educate providers on the various reporting requirements for fetal death.
Although stillbirth is a relatively common occurrence compared with other adverse pregnancy outcomes, existing data sources are inadequate for population-based estimates on risk factors and for determining potential causes of stillbirth. Expanding existing population-based birth defects surveillance programs to include surveillance on stillbirths is one approach to address these data gaps. This approach has three potential advantages and benefits. The first is efficiency. Existing birth defects programs with active case finding have the necessary infrastructure already in place to incorporate surveillance data on stillbirths. For some programs, minimal effort would be needed for methodology and data collection revisions for this expansion; whereas others might require more intensive efforts. Significant legal, financial, and operational barriers will potentially pose formidable challenges for some state-based programs, and appropriate training for abstractors to begin these new activities would need to be readily implemented. This training would require standardization and need to include education on various maternal-fetal health issues, to include obstetric complication and placental pathology correlates.
Second, existing programs responsible for the surveillance of birth defects would benefit directly from these expanded activities. It is believed that congenital anomalies contribute to approximately 20%–25% of stillbirths,21,48 and increasing the ascertainment of stillbirths in these programs would help to further ensure the completeness of birth defects information. Third, this approach would enlighten efforts on etiology for gestational age at death. Fetal deaths occurring at ≥20 weeks of gestation are thought to have different etiologies from earlier losses, and understanding the spectrum of potential causes in these later deaths will help with potential public health and clinical prevention strategies.
CONCLUSIONS
The suggestions and ideas resulting from these workshops are invaluable for planning the expansions of MACDP and IRCID to begin surveillance on stillbirths. Case definition and inclusion criteria are essential first steps to improving complete and accurate classification of pregnancy outcome. Multiple sources of information are needed for case finding. At a minimum, basic demographic and epidemiologic data should be collected. Additional information will be valuable to enlighten a number of issues: to provide a better understanding of risk factors and potential causes, to demonstrate the need for uniform and systematic evaluation guidelines and protocols, and to provide information to stakeholders for various purposes. Preliminary results from the MACDP and IRCID projects will illustrate the potential contributions that enhancing current stillbirth surveillance activities will provide, justifying the additional costs and resources needed for implementation and project maintenance.
Acknowledgments
The authors thank the other members of the steering committee who helped develop the format and agenda for this meeting, including James Kucik and Janet Cragan of the Centers for Disease Control and Prevention (CDC). The authors also appreciate the other meeting participants who contributed to this work: Coleen Boyle, CDC; Jamie Frias, CDC; James Hanson, National Institutes of Health (NIH); Peggy Honein, CDC; Carol Hogue, Emory University; Namita Joshi, CDC; Emily Kahn, Georgia Division of Public Health; Mark Klebanoff, NIH; Cynthia Moore, CDC; Kim Piper, Iowa Department of Public Health; Sonja Rasmussen, CDC; Courtney Rowland, CDC; Donna Strobino, Johns Hopkins University, Bloomberg School of Public Health; Carrie Shapiro-Mendoza, CDC; Michael Varner, University of Utah; Pat Collins, Piedmont Hospital in Atlanta; Ruth Fretts, Harvard Medical School; Julie Giese, Piedmont Hospital; Michael Lindsey, Emory University; Hilat Pinar, Brown Medical School; Uma Reddy, NIH; Richard Robbins, Northside Hospital in Atlanta; Carolyn Salafia, Columbia University; and Robert Silver, University of Utah. The authors also thank Gloria Franklin and Stephanie Henry for organizing the meeting logistics and travel arrangements for the participants.
Footnotes
The suggestions and ideas expressed in this article were formulated during two meetings entitled, “The Metropolitan Atlanta Stillbirth Surveillance Workshop.” The first meeting was held on April 26, 2005, and the second on July 14, 2005.
The findings and conclusions in this article are those of the authors and do not necessarily represent the official views of CDC.
REFERENCES
- 1.McClure EM, Wright LL, Goldenberg RL, Goudar SS, Parida SN, Jehan I, et al. The global network: a prospective study of stillbirths in developing countries. Am J Obstet Gynecol. 2007;197(247):e1–5. doi: 10.1016/j.ajog.2007.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Silver RM. Fetal death. Obstet Gynecol. 2007;109:153–67. doi: 10.1097/01.AOG.0000248537.89739.96. [DOI] [PubMed] [Google Scholar]
- 3.Goldenberg RL, Kirby R, Culhane JF. Stillbirth: a review. J Maternal Fetal Neonatal Med. 2004;16:79–94. doi: 10.1080/14767050400003801. [DOI] [PubMed] [Google Scholar]
- 4.MacDorman MF, Munson ML, Kirmeyer S. Fetal and perinatal mortality, United States, 2004. Natl Vital Stat Rep. 2007 Oct 11;56:1–20. [PubMed] [Google Scholar]
- 5.Racial/ethnic trends in fetal mortality—United States, 1990–2000. MMWR Morb Mortal Wkly Rep. 2004;53(24):529–32. [PubMed] [Google Scholar]
- 6.Reddy UM. Prediction and prevention of recurrent stillbirth. Obstet Gynecol. 2007;110:1151–64. doi: 10.1097/01.AOG.0000287616.71602.d0. [DOI] [PubMed] [Google Scholar]
- 7.Salihu HM, Kinniburgh BA, Aliyu MH, Kirby RS, Alexander GR. Racial disparity in stillbirth among singleton, twin, and triplet gestations in the United States. Obstet Gynecol. 2004;104:734–40. doi: 10.1097/01.AOG.0000139944.15133.e3. [DOI] [PubMed] [Google Scholar]
- 8.Yuan H, Platt RW, Morin L, Joseph KS, Kramer MS. Fetal deaths in the United States, 1997 vs 1991. Am J Obstet Gynecol. 2005;193:489–95. doi: 10.1016/j.ajog.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 9.Allen CL, Hulsey TM, Hulsey TC. The influence of race on fetal outcome. Am J Perinatol. 2005;22:245–8. doi: 10.1055/s-2005-867089. [DOI] [PubMed] [Google Scholar]
- 10.Sharma PP, Salihu HM, Oyelese Y, Ananth CV, Kirby RS. Is race a determinant of stillbirth recurrence? Obstet Gynecol. 2006;107(2 Pt 1):391–7. doi: 10.1097/01.AOG.0000196501.32272.44. [DOI] [PubMed] [Google Scholar]
- 11.Andreasen KR, Andersen ML, Schantz AL. Obesity and pregnancy. Acta Obstet Gynecol Scand. 2004;83:1022–9. doi: 10.1111/j.0001-6349.2004.00624.x. [DOI] [PubMed] [Google Scholar]
- 12.Atalah E, Castro R. [Maternal obesity and reproductive risk] Rev Med Chil. 2004;132:923–30. doi: 10.4067/s0034-98872004000800003. [DOI] [PubMed] [Google Scholar]
- 13.Bell R, Parker L, MacPhail S, Wright C. Trends in the cause of late fetal death, 1982–2000. BJOG. 2004;111:1400–7. doi: 10.1111/j.1471-0528.2004.00296.x. [DOI] [PubMed] [Google Scholar]
- 14.Chu SY, Kim SY, Lau J, Schmid CH, Dietz PM, Callaghan WM, et al. Maternal obesity and risk of stillbirth: a metaanalysis. Am J Obstet Gynecol. 2007;197:223–8. doi: 10.1016/j.ajog.2007.03.027. [DOI] [PubMed] [Google Scholar]
- 15.Dafallah SE, Yousif EM. Diabetes mellitus during pregnancy. Fetal outcome. Saudi Med J. 2004;25:2041–2. [PubMed] [Google Scholar]
- 16.Efkarpidis S, Alexopoulos E, Kean L, Liu D, Fay T. Case-control study of factors associated with intrauterine fetal deaths. MedGenMed. 2004;6:53. [PMC free article] [PubMed] [Google Scholar]
- 17.Fretts RC. Etiology and prevention of stillbirth. Am J Obstet Gynecol. 2005;193:1923–35. doi: 10.1016/j.ajog.2005.03.074. [DOI] [PubMed] [Google Scholar]
- 18.Gennaro S. Overview of current state of research on pregnancy outcomes in minority populations. Am J Obstet Gynecol. 2005;192:S3–10. doi: 10.1016/j.ajog.2005.02.014. [DOI] [PubMed] [Google Scholar]
- 19.Heffner LJ. Advanced maternal age—how old is too old? N Engl J Med. 2004;351:1927–9. doi: 10.1056/NEJMp048087. [DOI] [PubMed] [Google Scholar]
- 20.Norwitz ER, Edusa V, Park JS. Maternal physiology and complications of multiple pregnancy. Semin Perinatol. 2005;29:338–48. doi: 10.1053/j.semperi.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 21.Pauli RM, Reiser CA. Wisconsin Stillbirth Service Program: II. Analysis of diagnoses and diagnostic categories in the first 1,000 referrals. Am J Med Genet. 1994;50:135–53. doi: 10.1002/ajmg.1320500205. [DOI] [PubMed] [Google Scholar]
- 22.Salihu HM, Shumpert MN, Aliyu MH, Alexander MR, Kirby RS, Alexander GR. Stillbirths and infant deaths associated with maternal smoking among mothers aged > or =40 years: a population study. Am J Perinatol. 2004;21:121–9. doi: 10.1055/s-2004-823776. [DOI] [PubMed] [Google Scholar]
- 23.Shaaban LA, Al-Saleh RA, Alwafi BM, Al-Raddadi RM. Associated risk factors with ante-partum intra-uterine fetal death. Saudi Med J. 2006;27:76–9. [PubMed] [Google Scholar]
- 24.Hefler LA, Hersh DR, Moore PJ, Gregg AR. Clinical value of postnatal autopsy and genetics consultation in fetal death. Am J Med Genet. 2001;104:165–8. doi: 10.1002/ajmg.1588. [DOI] [PubMed] [Google Scholar]
- 25.Newton D, Coffin CM, Clark EB, Lowichik A. How the pediatric autopsy yields valuable information in a vertically integrated health care system. Arch Pathol Lab Med. 2004;128:1239–46. doi: 10.5858/2004-128-1239-HTPAYV. [DOI] [PubMed] [Google Scholar]
- 26.Horn LC, Langner A, Stiehl P, Wittekind C, Faber R. Identification of the causes of intrauterine death during 310 consecutive autopsies. Eur J Obstet Gynecol Reprod Biol. 2004;113:134–8. doi: 10.1016/S0301-2115(03)00371-3. [DOI] [PubMed] [Google Scholar]
- 27.Martin JA, Hoyert DL. The National Fetal Death File. Semin Perinatol. 2002;26:3–11. doi: 10.1053/sper:2002.29834. [DOI] [PubMed] [Google Scholar]
- 28.Duke CW, Alverson C, Correa A. Fetal death certificates as a source of surveillance data for stillbirths with birth defects. Public Health Rep. 2007;122:664–9. doi: 10.1177/003335490712200514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goldhaber MK. Fetal death ratios in a prospective study compared to state fetal death certificate reporting. Am J Public Health. 1989;79:1268–70. doi: 10.2105/ajph.79.9.1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Honein MA, Paulozzi LJ. Birth defects surveillance: assessing the “gold standard”. Am J Public Health. 1999;89:1238–9. doi: 10.2105/ajph.89.8.1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hoyert DL, Martin JA. Vital statistics as a data source. Semin Perinatol. 2002;26:12–6. doi: 10.1053/sper.2002.29835. [DOI] [PubMed] [Google Scholar]
- 32.Lydon-Rochelle MT, Cardenas V, Nelson JL, Tomashek KM, Mueller BA, Easterling TR. Validity of maternal and perinatal risk factors reported on fetal death certificates. Am J Public Health. 2005;95:1948–51. doi: 10.2105/AJPH.2004.044305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Northam S, Knapp TR. The reliability and validity of birth certificates. J Obstet Gynecol Neonatal Nurs. 2006;35:3–12. doi: 10.1111/j.1552-6909.2006.00016.x. [DOI] [PubMed] [Google Scholar]
- 34.Greb AE, Pauli RM, Kirby RS. Accuracy of fetal death reports: comparison with data from an independent stillbirth assessment program. Am J Public Health. 1987;77:1202–6. doi: 10.2105/ajph.77.9.1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kirby RS. The coding of underlying cause of death from fetal death certificates: issues and policy considerations. Am J Public Health. 1993;83:1088–91. doi: 10.2105/ajph.83.8.1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lammer EJ, Brown LE, Anderka MT, Guyer B. Classification and analysis of fetal deaths in Massachusetts. JAMA. 1989;261:1757–62. [PubMed] [Google Scholar]
- 37.Correa-Villasenor A, Cragan J, Kucik J, O'Leary L, Siffel C, Williams L. Metropolitan Atlanta Congenital Defects Program; 40th anniversary edition. Birth Defects Res A Clin Mol Teratol. 2007;79:65–92. doi: 10.1002/bdra.10111. [DOI] [PubMed] [Google Scholar]
- 38.Romitti PA, Sutphen SM. Iowa Birth Defects Registry annual report. Iowa City (IA): University of Iowa; 2000. [Google Scholar]
- 39.Forrester MB, Merz RD. Inclusion of early fetal deaths in a birth defects surveillance system. Teratology. 2001;64(Suppl 1):S20–5. doi: 10.1002/tera.1080. [DOI] [PubMed] [Google Scholar]
- 40.World Health Organization. International statistical classification of diseases and related health problems: tenth revision. 2nd ed. Geneva: WHO; 1992. [PubMed] [Google Scholar]
- 41.Department of Health and Human Services (US) Model State Vital Statistics Act and Regulations. 1992 revision. DHHS Publication No. (PHS) 95-1115.
- 42.Kowaleski J. State definitions and reporting requirements for live births, fetal deaths, and induced terminations of pregnancy (1997 revision) Hyattsville (MD): National Center for Health Statistics; 1997. [Google Scholar]
- 43.Genest DR, Singer DB. Estimating the time of death in stillborn fetuses: III. External fetal examination: a study of 86 stillborns. Obstet Gynecol. 1992;80:593–600. [PubMed] [Google Scholar]
- 44.Dietz PM, England LJ, Callaghan WM, Pearl M, Wier ML, Kharrazi M. A comparison of LMP-based and ultrasound-based estimates of gestational age using linked California livebirth and prenatal screening records. Paediatr Perinat Epidemiol. 2007;21(Suppl 2):S62–71. doi: 10.1111/j.1365-3016.2007.00862.x. [DOI] [PubMed] [Google Scholar]
- 45.Wingate MS, Alexander GR, Buekens P, Vahratian A. Comparison of gestational age classifications: date of last menstrual period vs. clinical estimate. Ann Epidemiol. 2007;17:425–30. doi: 10.1016/j.annepidem.2007.01.035. [DOI] [PubMed] [Google Scholar]
- 46.Kirby RS. The quality of data reported on birth certificates. Am J Public Health. 1997;87:301. doi: 10.2105/ajph.87.2.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Watkins ML, Edmonds L, McClearn A, Mullins L, Mulinare J, Khoury M. The surveillance of birth defects: the usefulness of the revised US standard birth certificate. Am J Public Health. 1996;86:731–4. doi: 10.2105/ajph.86.5.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Korteweg FJ, Gordijn SJ, Timmer A, Erwich JJHM, Bergman KA, Bouman K, et al. The tulip classification of perinatal mortality: introduction and multidisciplinary inter-rater agreement. BJOG. 2006;113:393–401. doi: 10.1111/j.1471-0528.2006.00881.x. [DOI] [PubMed] [Google Scholar]