SYNOPSIS
Objectives
Infant mortality is a major indicator of the health of a nation. We analyzed recent patterns and trends in U.S. infant mortality, with an emphasis on two of the greatest challenges: (1) persistent racial and ethnic disparities and (2) the impact of preterm and low birthweight delivery.
Methods
Data from the national linked birth/infant death datasets were used to compute infant mortality rates per 100,000 live births by cause of death (COD), and per 1,000 live births for all other variables. Infant mortality rates and other measures of infant health were analyzed and compared. Leading and preterm-related CODs, and international comparisons of infant mortality rates were also examined.
Results
Despite the rapid decline in infant mortality during the 20th century, the U.S. infant mortality rate did not decline from 2000 to 2005, and declined only marginally in 2006. Racial and ethnic disparities in infant mortality have persisted and increased, as have the percentages of preterm and low birthweight deliveries. After decades of improvement, the infant mortality rate for very low birthweight infants remained unchanged from 2000 to 2005. Infant mortality rates from congenital malformations and sudden infant death syndrome declined; however, rates for preterm-related CODs increased. The U.S. international ranking in infant mortality fell from 12th place in 1960 to 30th place in 2005.
Conclusions
Infant mortality is a complex and multifactorial problem that has proved resistant to intervention efforts. Continued increases in preterm and low birthweight delivery present major challenges to further improvement in the infant mortality rate.
Infant mortality is an important indicator of the health of a nation, as it is associated with a variety of factors such as maternal health, quality and access to medical care, socioeconomic conditions, and public health practices. The U.S. infant mortality rate generally declined throughout the 20th century.1–3 However, more recent data suggest at least a temporary halt in this decline in the first few years of the 21st century.4,5 The percentage of infants born preterm and at low birthweight continues to increase,6 and because infants born too small or too soon have higher mortality rates, this continued increase has a great impact on infant mortality.4,5 Also, large differences in infant mortality rates among racial/ethnic groups have persisted and even increased, suggesting that not all groups have benefited equally from social and medical advances.5,7
This article analyzes patterns and trends in U.S. infant mortality, emphasizing two of the greatest challenges to infant mortality prevention in the United States: (1) persistent and increasing differences by race/ethnicity and (2) the impact of preterm and low birthweight deliveries. Leading causes of infant mortality are also discussed, as are international comparisons of infant mortality rates.
METHODS
Data discussed in this article are based primarily on the linked birth/infant death datasets produced by the Centers for Disease Control and Prevention's National Center for Health Statistics (NCHS).5,8 In these datasets, information from the birth certificate is linked to information from the death certificate for each infant who dies in the United States. The purpose of the linkage is to use the many additional variables available from the birth certificate for infant mortality analysis.
We computed infant (<1 year of age) mortality rates per 100,000 live births for cause of death, and per 1,000 live births for all other variables. Although all variables were reported by all states, there was a change in the wording and formatting of the maternal smoking, prenatal care, and maternal education items between the 1989 and 2003 revisions of the U.S. Standard Certificate of Birth. Due to the staggered implementation of the 2003 revision among U.S. states, we included only data based on the 1989 revision (in use in 37 states, the District of Columbia, and New York City in 2005).5,6 More detailed information on the measurement of individual variables is available elsewhere.5,6,8 We excluded missing data before computing percentages.
Cause-of-death (COD) data were classified according to the Tenth Revision of the International Statistical Classification of Diseases and Related Health Problems.9 Leading CODs were ranked using the conventions outlined by NCHS and described in detail elsewhere.5
To more readily track the impact of preterm-related CODs, we created a grouping of preterm-related causes by identifying those that were a direct cause or consequence of preterm birth. COD categories were considered to be preterm-related when 75% or more of total infant deaths attributed to that cause were deaths of infants born preterm, and the cause was a direct consequence of preterm birth based on a clinical evaluation and review of the literature.10,11
RESULTS
Trends
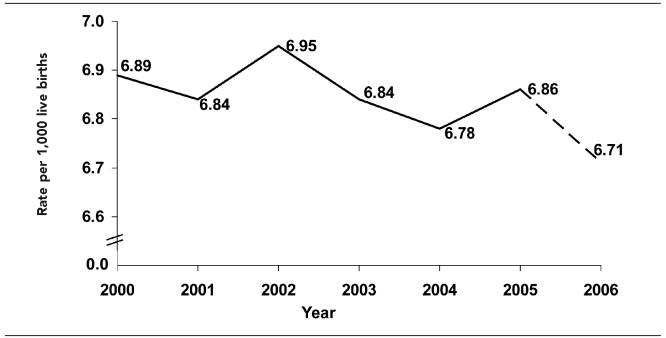
The U.S. infant mortality rate declined by 93% during the 20th century, from approximately 100 infant deaths per 1,000 live births in 190012 to 6.89 in 2000.5 After some small ups and downs from 2001 to 2004, including an increase in 2002,4 the U.S. infant mortality rate was 6.86 in 2005, not significantly different from the rate of 6.89 in 2000 (Figure 1). Preliminary data from 2006 suggest a 2% decline in the infant mortality rate from 2005 to 2006, driven in part by a decline for infants of Hispanic mothers. Mortality rates for infants of non-Hispanic white and non-Hispanic black mothers did not decline significantly from 2005 to 2006.13 Whether or not this decline continues into future years, the 2000–2005 plateau in the U.S. infant mortality rate represents the first period of sustained lack of decline in the U.S. infant mortality rate since the 1950s.4,14 Despite the large declines during the 20th century, the impact of infant mortality is still considerable. In 2005, there were 28,384 deaths to children younger than 1 year of age in the U.S.5
Figure 1.
Infant mortality rate: United States, 2000–2006
Source: 2000–2005 data are from the linked birth/infant death data sets. 2006 data are from the preliminary mortality file.
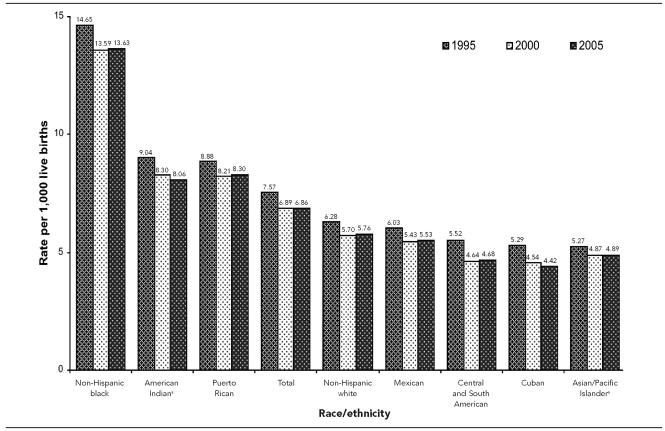
Racial and ethnic differences in infant mortality
There continue to be large variations in infant mortality rates among racial/ethnic groups (Figure 2). Non-Hispanic black mothers had the highest infant mortality rate (13.63), followed by Puerto Rican (8.30) and American Indian (8.06) mothers. Infant mortality rates were moderate for non-Hispanic white (5.76) and Mexican (5.53) mothers, and lowest for Cuban (4.42), Central and South American (4.68), and Asian/Pacific Islander (API) (4.89) mothers. As with the overall infant mortality rate, racial/ethnic-specific rates generally decreased from 1995 to 2000, but did not decrease from 2000 to 2005.
Figure 2.
Infant mortality rates by race and ethnicity of mother: United States, 1995, 2000, and 2005
aIndicates people of Hispanic and non-Hispanic origin
Factors frequently mentioned as contributing to racial/ethnic differences in infant mortality include differences in maternal preconception health, infection, income, access to quality health care, stress, racism, and social and cultural factors.7,15–18 However, the influence of an individual risk factor (e.g., maternal age or income) may vary considerably by race/ethnicity, suggesting different disease pathways and life experiences for women of different racial/ethnic groups.7,17,19 For example, due to worsening health profiles, black women may experience a larger negative effect of advancing maternal age on infant health than do white women.17 Conversely, it is hypothesized that a supportive cultural and family environment contributes to the low infant mortality rates for Mexican women, despite lower income and health insurance levels and a higher prevalence of most risk factors.5,6,20,21 Several risk factors for infant mortality are discussed in this article; however, these are only some of the factors affecting racial/ethnic differences, and even after consideration of these factors, much of the racial/ethnic differences in infant mortality remain unexplained.
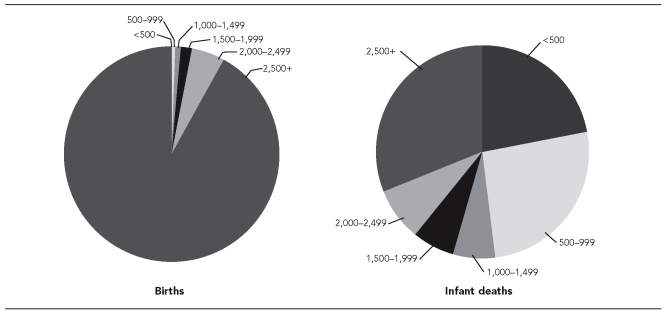
Variations in risk factors affect racial and ethnic differences
Differences in infant mortality by race/ethnicity reflect in part differences in maternal sociodemographic and behavioral risk factors. For example, infant mortality rates are higher than the U.S. average for teenagers, unmarried mothers, smokers, those with lower educational levels, those who had a fourth or higher birth order, or those who did not obtain adequate prenatal care.5 The racial/ethnic groups with the lowest infant mortality rates tended to have a smaller percentage of births to women with some or all of these characteristics, while the racial/ethnic groups with the highest infant mortality rates tended to have a higher percentage of births to women with some or all of these characteristics (Table 1). For example, API mothers (who had low infant mortality rates) were on average more educated and less likely to smoke or to have a teen or nonmarital birth. Conversely, a higher percentage of non-Hispanic black, Puerto Rican, and American Indian mothers (who had high infant mortality rates) did not receive adequate prenatal care, were unmarried or teenagers, or had not completed high school.
Table 1.
Percent of live births with selected maternal and infant characteristics by Hispanic origin of mother and race of mother for mothers of non-Hispanic origin: United States, 2005 linked file
aIncludes races/ethnicities not listed separately
bIncludes Aleuts and Eskimos
c<1,500 grams
d<2,500 grams
eBorn prior to 32 completed weeks of gestation
fBorn prior to 37 completed weeks of gestation
gData are based on the 1989 Revision of the U.S. Certificate of Live Birth; these data are not comparable with those based on the 2003 Revision of the U.S. Certificate of Live Birth. Excludes data from Florida, Idaho, Kansas, Kentucky, Nebraska, New Hampshire, New York State (excluding New York City), Tennessee, Texas, Vermont, and Washington.
hExcludes data for California, which does not report tobacco use on the birth certificate
Differences in income and access to health care among racial/ethnic groups may also contribute to differences in infant mortality. In 2005, nearly three times as many black, American Indian, and Hispanic children as non-Hispanic white children (<18 years of age) lived in families with incomes below the poverty level. Children of black, American Indian, and Hispanic families were also much less likely than non-Hispanic white children to have health insurance.22
Many of the risk factors discussed previously are also risk factors for preterm and/or low birthweight delivery, and they may affect infant mortality either directly or through the mechanism of preterm or low birthweight delivery. In 2005, the percentage of infants born preterm (<37 completed weeks of gestation) was substantially higher for non-Hispanic black (18.4%), Puerto Rican (14.3%), and American Indian (14.1%) mothers than for non-Hispanic white mothers (11.7%) (Table 1). Racial/ethnic differences in preterm and low birthweight delivery exert a strong influence on infant mortality, and are discussed in more detail in the following section.23,24
The contribution of preterm and low birthweight delivery to infant mortality
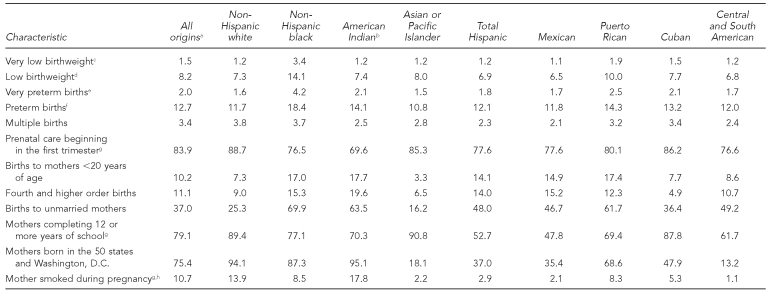
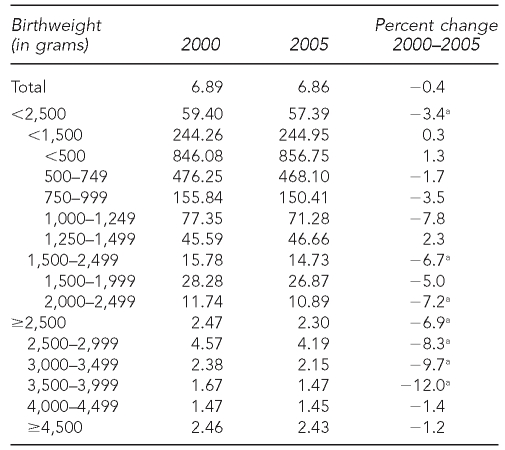
Birthweight and period of gestation are the two most important predictors of an infant's subsequent health and survival. Infants born too small or too soon have a much greater risk of death and disability than those born at full term (37 to 41 weeks of gestation) or with birthweights of 2,500 grams or more. Because of their much greater risk of death, infants born at the lowest birthweights and gestational ages have a large impact on overall infant mortality. For example, in 2005, infants born weighing less than 1,000 grams accounted for only 0.8% of births, but nearly half (48.2%) of all infant deaths (Figure 3). The infant mortality rate for very low birthweight infants (<1,500 grams) was 244.95 infant deaths per 1,000 live births, which was more than 100 times the rate of 2.30 for infants with birthweights of 2,500 grams or more (Table 2). About 86.0% of infants with birthweights of less than 500 grams died within the first year of life, although reporting of deaths among these very small infants may be incomplete.25 An infant's chances of survival increase rapidly with increasing birthweight. Infant mortality rates were lowest at birthweights of 3,000 to 4,999 grams.
Figure 3.
Percentage of live births and infant deaths by birthweight in grams: United States, 2005
Table 2.
Infant mortality rates by birthweight, United States, 2000 and 2005 linked files
aSignificant at p<0.05
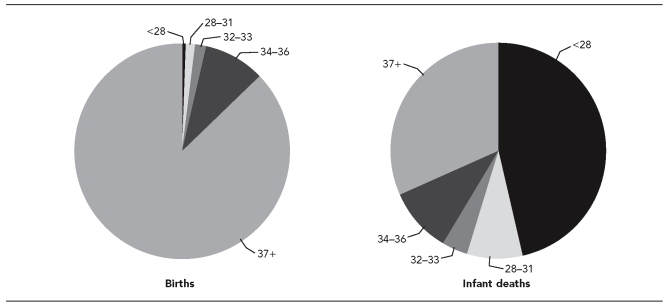
We found a similar pattern when examining data by period of gestation. In 2005, 0.8% of births occurred at <28 weeks of gestation, but they accounted for nearly half (46.4%) of infant deaths (Figure 4). The risk of infant death generally decreases as the length of gestation increases.5,26 The infant mortality rate for very preterm infants (<32 weeks) was 183.24, 75 times the rate of 2.43 for full-term infants. Still, infants born only a few weeks early have a substantially increased risk of death when compared with full-term infants.27–29 For example, the infant mortality rate for late preterm infants (those born at 34–36 weeks of gestation) is 7.30, three times the rate for full-term infants. Even within the term period, infants born at 37–39 weeks of gestation have mortality rates that are 30.0% higher than those born at 40–41 weeks of gestation.5
Figure 4.
Percentage of live births and infant deaths by weeks of gestation: United States, 2005
Explaining infant mortality trends and the recent plateau
The infant mortality rate for a given population can be partitioned into two key components: (1) the distribution of births by birthweight and (2) birthweight-specific mortality rates (the mortality rate for infants at a given weight). A change in either component can lead to a change in the overall infant mortality rate.
The percentage of low birthweight (<2,500 grams) births has increased from a low of 6.8% in 1985 to 7.6% in 2000 and 8.2% in 2005.5,6 However, from 1985 to 2000, birthweight-specific infant mortality rates declined for all birthweight categories. The infant mortality rate continued to decline from 1985 to 2000 because declines in birthweight-specific infant mortality rates were large enough to offset the increase in the percentage of low birthweight births. However, from 2000 to 2005, the decline in the infant mortality rate for very low birthweight (<1,500 grams) infants halted (Table 2).5,8 Although infant mortality rates for moderately low birthweight (1,500–2,499 grams) and normal birthweight (≥2,500 grams) infants did decline from 2000 to 2005, the plateauing in the infant mortality rate for very low birthweight infants (which account for more than half of all infant deaths), coupled with the continuing increase in the percentage of low birthweight births, was enough to halt the historic decline in infant mortality in the U.S. that took place during the 20th century.
Much research, programmatic, and advocacy work during the past two decades has been devoted to preventing preterm and low birthweight delivery;26,30,31 yet, the percentage of infants born preterm or at low birthweight has continued to rise. A portion of the increase is related to an increase in multiple births (in part due to increases in the use of assisted reproductive technologies32); however, the percentage of preterm and low birthweight births also increased among singletons.6 Spontaneous preterm labor is a complex problem with multiple etiologies that has challenged researchers and clinicians for decades.26,33 Another factor that has received relatively little attention is the effect of increases in medical interventions, such as cesarean section and induction of labor, on the preterm birth rate. Changes in medical interventions have been demonstrated to affect the percentage of preterm and low birthweight births in the United States and other countries.6,27,33–35 From 1990 to 2005, the percentage of singleton preterm births delivered by cesarean increased by 44% (from 25% to 36%), while the percentage with induction of labor more than doubled (from 7% to 16%).6,8
Leading causes of infant death
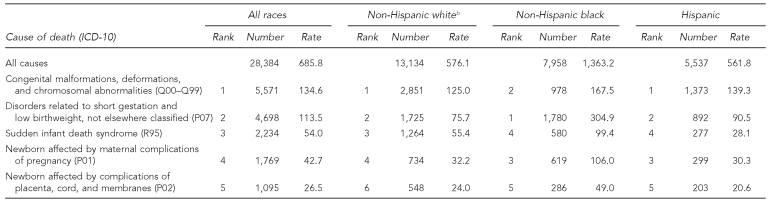
The leading cause of infant death in 2005 was congenital malformations, accounting for 20% of all infant deaths. “Disorders related to short gestation and low birthweight, not elsewhere classified” was the second leading COD (17%), followed by sudden infant death syndrome (SIDS) (8%), Newborn affected by maternal complications of pregnancy (maternal complications) (6%), and Newborn affected by complications of placenta, cord, and membranes (cord complications) (4%). Together, the five leading CODs for infants accounted for 54% of all infant deaths in the U.S.(Table 3).
Table 3.
Infant deaths and mortality ratesa for the five leading causes of infant death by race and Hispanic origin of mother: United States, 2005 linked file
aRates are per 100,000 live births in specified group.
bFor Non-Hispanic white women, accidents (unintentional injuries) were the fifth leading cause of death, with 583 deaths and a rate of 25.6.
ICD-10 = International Classification of Diseases, Tenth Revision
The infant mortality rate from congenital malformations decreased by 5% from 2000 to 2005, and the SIDS rate decreased by 13%, although this change may be due in part to changes in the way SIDS is diagnosed by the medical community.36 However, for CODs with a high percentage of deaths to low birthweight infants, infant mortality rates either plateaued or increased from 2000 to 2005.5
Preterm-related causes of death
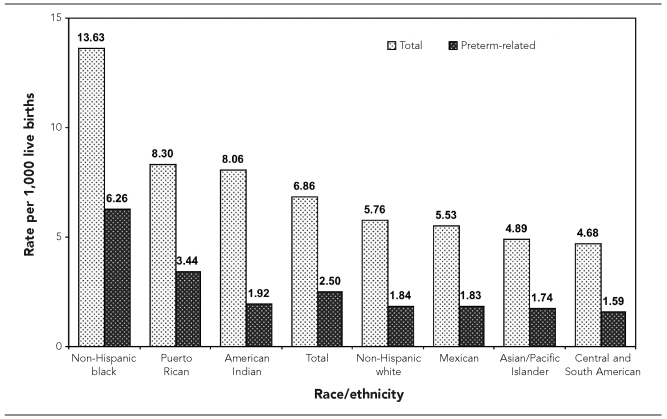
In 2005, 10,364 out of a total of 28,384 infant deaths in the U.S. were due to preterm-related CODs. The percentage of infant deaths that were preterm-related increased from 35% in 2000 to 37% in 2005.5,11 The impact of preterm-related infant mortality was high for all racial/ethnic groups; however, some groups were disproportionately affected. For example, nearly half (46%) of infant deaths to non-Hispanic black women and 41% of infant deaths to Puerto Rican women were preterm-related, compared with 32% for non-Hispanic white women.5 Preterm-related infant mortality rates were 3.4 times higher for non-Hispanic black (6.26) than for non-Hispanic white (1.84) mothers (Figure 5). In fact, in 2005, the preterm-related infant mortality rate for non-Hispanic black mothers was higher than the total infant mortality rate for non-Hispanic white, Mexican, Central and South American, and API women. The preterm-related infant mortality rate for Puerto Rican mothers (3.44) was 87% higher than for non-Hispanic white mothers.
Figure 5.
Total and preterm-related infant mortality rates by race/ethnicity of mother: United States, 2005
NOTE: Preterm-related deaths are those in which the infant was born preterm (<37 completed weeks of gestation) with the underlying cause of death assigned to one of the following International Classification of Diseases, 10th Revision categories: K550, P000, P010, P011, P015, P020, P021, P027, P070–P073, P102, P220–229, P250–279, P280, P281, P360–P369, P520–P523, P77.
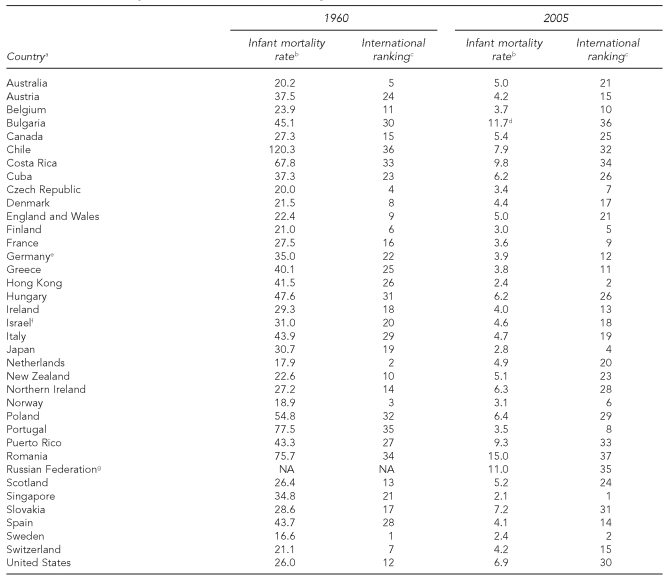
International comparisons of infant mortality
During the past few decades, the decline in infant mortality in the U.S. has been slower than for most other developed countries. As a result, the United States' international ranking in infant mortality has fallen from 12th lowest in 1960 to 23rd lowest in 1990, to 30th lowest in 2005.37 Selected Scandinavian (e.g., Sweden, Norway, Finland) and East Asian (e.g., Japan, Hong Kong, Singapore) countries generally had the lowest infant mortality rates (<3.5) (Table 4). The percentage of low birthweight births is higher in the U.S. than in most other developed countries.38 Variations in infant mortality rates among countries may also reflect differences in the sociodemographic characteristics of the population, income and income inequality, access to health-care services, and social supports for children and families.39–41
Table 4.
Infant mortality rates and international rankings: selected countries, 1960 and 2005
Source: National Center for Health Statistics. Health, United States 2008, with chartbook on trends in the health of Americans. Hyattsville (MD): National Center for Health Statistics; 2009.
aRefers to countries, territories, cities, or geographic areas with at least 1 million population and with “complete” counts of live births and infant deaths as indicated in the United Nations Demographic Yearbook.
bInfant deaths per 1,000 live births
cRankings are from lowest to highest infant mortality rates (IMRs). Countries with the same IMR receive the same rank. The country with the next highest IMR is assigned the rank it would have received had the lower-ranked countries not been tied, i.e., skip a rank.
dData are for 2004, as 2005 data are not yet available.
eRates presented for the years prior to the reunification of Germany were calculated by combining information from the Federal Republic of Germany and the German Democratic Republic.
fIncludes data for East Jerusalem and Israel residents in certain other territories under occupation by Israeli military forces since June 1967
gExcludes infants born alive after less than 28 weeks of gestation, of less than 1,000 grams birthweight, and less than 35 centimeters in length, who die within seven days of birth
NA = not available
International comparisons of infant mortality can be influenced by differences in reporting of fetal and infant deaths, particularly for the smallest infants that die around the time of birth.41–44 The countries included in Table 4 are those designated by the United Nations as having >90% complete reporting of infant deaths;45 still, differences in reporting may have an impact. However, there is little evidence that differences in reporting have increased over time in a way that would affect the U.S. disproportionately, and little reason to doubt that the U.S. decline in the international rankings since 1960 is real, although the actual magnitude may be affected by reporting practices. Also, given the magnitude of differences in infant mortality rates (with 22 countries reporting rates ≤5.0 in 2005), it appears unlikely that differences in reporting of infant deaths account for all or most of the United States' relatively low international ranking.
DISCUSSION
Despite the dramatic decline in infant mortality during the 20th century, the U.S. infant mortality rate appears to have plateaued in the first few years of the 21st century. The U.S. infant mortality rate did not decline from 2000 to 2005, but appears to have declined by 2% in 2006 based on preliminary data. Racial and ethnic differences in infant mortality rates have persisted and increased, as have the percentages of preterm and low birthweight deliveries. After decades of improvement, the infant mortality rate for very low birthweight infants remained unchanged between 2000 and 2005. Infant mortality rates from congenital malformations and SIDS declined from 2000 to 2005; however, rates for preterm-related causes increased.5,11 The U.S. international ranking in infant mortality fell from 12th in 1960 to 30th in 2005.
CONCLUSION
Infant mortality is a complex and multifactorial problem that has shown little improvement in the past several years, despite programmatic efforts. Further efforts to lower the U.S. infant mortality rate should focus on preventing preterm and low birthweight deliveries, and on reducing the large and persistent differences in infant mortality rates by race and ethnicity. These two goals are closely interrelated, as excess mortality from low birthweight births accounts for much of the black/white infant mortality gap. Although successes have been noted in local and regional intervention programs,30 on the national level, both of these goals have proved remarkably resistant to intervention efforts. However, the low infant mortality rates in other developed countries suggest that further lowering of the U.S. infant mortality rate is achievable.
REFERENCES
- 1.Wegman ME. Infant mortality in the 20th century: dramatic but uneven progress. J Nutr. 2001;131:S401–8. doi: 10.1093/jn/131.2.401S. [DOI] [PubMed] [Google Scholar]
- 2.Achievements in public health, 1900–1999: healthier mothers and babies. MMWR Morb Mortal Wkly Rep. 1999;48(38):849–58. [PubMed] [Google Scholar]
- 3.Guyer B, Freedman MA, Strobino DM, Sondik EJ. Annual summary of vital statistics: trends in the health of Americans during the 20th century. Pediatrics. 2000;106:1307–17. doi: 10.1542/peds.106.6.1307. [DOI] [PubMed] [Google Scholar]
- 4.MacDorman MF, Martin JA, Mathews TJ, Hoyert DL, Ventura SJ. Explaining the 2001–02 infant mortality increase: data from the linked birth/infant death data set. Natl Vital Stat Rep. 2005 Jan 24;53:1–23. [PubMed] [Google Scholar]
- 5.Mathews TJ, MacDorman MF. Infant mortality statistics from the 2005 period linked birth/infant death data set. Natl Vital Stat Rep. 2008 Jul 30;57:1–32. [PubMed] [Google Scholar]
- 6.Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Kirmeyer S, et al. Births: final data for 2005. Natl Vital Stat Rep. 2007 Dec 5;56:1–104. [PubMed] [Google Scholar]
- 7.Krieger N, Rehkopf DH, Chen JT, Waterman PD, Marcelli E, Kennedy M. The fall and rise of U.S. inequities in premature mortality: 1960–2002. PLoS Med. 2008;5:e46. doi: 10.1371/journal.pmed.0050046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Center for Health Statistics. Period linked birth/infant death data files. [cited 2008 Apr 28]. Available from: URL: http://www.cdc.gov/nchs/about/major/dvs/Vitalstatsonline.htm.
- 9.World Health Organization. International Statistical Classification of Diseases and Related Health Problems, Tenth Revision. Geneva: WHO; 1992. [PubMed] [Google Scholar]
- 10.Callaghan WM, MacDorman MF, Rasmussen SA, Qin C, Lackritz EM. The contribution of preterm birth to infant mortality rates in the United States. Pediatrics. 2006;118:1566–73. doi: 10.1542/peds.2006-0860. [DOI] [PubMed] [Google Scholar]
- 11.MacDorman MF, Callaghan WM, Mathews TJ, Hoyert DL, Kochanek KD. Trends in preterm-related infant mortality by race and ethnicity, United States, 1999–2004. Int J Health Serv. 2007;37:635–41. doi: 10.2190/HS.37.4.c. [DOI] [PubMed] [Google Scholar]
- 12.Meckel RA. Save the babies: American public health reform and the prevention of infant mortality, 1850–1929. Ann Arbor (MI): University of Michigan Press; 1998. [Google Scholar]
- 13.Heron MP, Hoyert DL, Xu J, Scott C, Tejada-Vera B. Deaths: preliminary data for 2006. Natl Vital Stat Rep. 2008 Jun 11;56:1–52. [Google Scholar]
- 14.National Center for Health Statistics. Vital statistics of the United States, 1993, vol II: mortality, part A. Hyattsville (MD): National Center for Health Statistics; 2002. [Google Scholar]
- 15.Fiscella K. Racial disparity in infant and maternal mortality: confluence of infection and microvascular dysfunction. Matern Child Health J. 2004;8:45–54. doi: 10.1023/b:maci.0000025726.53515.65. [DOI] [PubMed] [Google Scholar]
- 16.Hogan VK, Njoroge T, Durant TM, Ferre CD. Eliminating disparities in perinatal outcomes—lessons learned. Matern Child Health J. 2001;5:135–40. doi: 10.1023/a:1011357317528. [DOI] [PubMed] [Google Scholar]
- 17.Geronimus AT. Black/white differences in the relationship of maternal age to birthweight: a population-based test of the weathering hypothesis. Soc Sci Med. 1996;42:589–97. doi: 10.1016/0277-9536(95)00159-x. [DOI] [PubMed] [Google Scholar]
- 18.Collins JW, Jr, David RJ, Handler A, Wall S, Andes S. Very low birthweight in African American infants: the role of maternal exposure to interpersonal racial discrimination. Am J Public Health. 2004;94:2132–8. doi: 10.2105/ajph.94.12.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Colen CG, Geronimus AT, Bound J, James SA. Maternal upward socioeconomic mobility and black-white disparities in infant birthweight. Am J Public Health. 2006;96:2032–9. doi: 10.2105/AJPH.2005.076547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hummer RA, Powers DA, Pullum SG, Gossman GL, Frisbie WP. Paradox found (again): infant mortality among the Mexican-origin population in the United States. Demography. 2007;44:441–57. doi: 10.1353/dem.2007.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gonzales-Quintero VH, Tolaymat L, Luke B, Gonzalez-Garcia A, Duthely L, O'Sullivan MJ, et al. Outcome of pregnancies among Hispanics—revisiting the epidemiologic paradox. J Reprod Med. 2006;51:10–4. [PubMed] [Google Scholar]
- 22.DeNavas-Walt C, Proctor BD, Hill Lee C. Income, poverty, and health insurance coverage in the United States: 2005. Current Population Reports P60-231. Washington: U.S. Government Printing Office; 2006. [Google Scholar]
- 23.Luke B, Brown MB. The changing risk of infant mortality by gestation, plurality, and race: 1989–1991 versus 1999–2001. Pediatrics. 2006;118:2488–97. doi: 10.1542/peds.2006-1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schempf AH, Branum AM, Lukacs SL, Schoendorf KC. The contribution of preterm birth to the black-white infant mortality gap, 1990 and 2000. Am J Public Health. 2007;97:1255–60. doi: 10.2105/AJPH.2006.093708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Paulson J, Ramsini W, Conrey E, Duffy R, Cooper MP. Unregistered deaths among extremely low birthweight infants—Ohio, 2006. MMWR Morb Mortal Wkly Rep. 2007;56(42):1101–3. [PubMed] [Google Scholar]
- 26.Institute of Medicine. Preterm birth: causes, consequences, and prevention. Washington: National Academies Press; 2006. [PubMed] [Google Scholar]
- 27.Davidoff MJ, Dias T, Damus K, Russell R, Bettegowda VR, Dolan S, et al. Changes in the gestational age distribution among U.S. singleton births: impact of rates of late preterm birth, 1992 to 2002. Semin Perinatol. 2006;30:8–15. doi: 10.1053/j.semperi.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 28.McIntire DD, Leveno KJ. Neonatal mortality and morbidity rates in late preterm births compared with births at term. Obstet Gynecol. 2008;111:35–41. doi: 10.1097/01.AOG.0000297311.33046.73. [DOI] [PubMed] [Google Scholar]
- 29.Tomashek KM, Shapiro-Mendoza CK, Davidoff MJ, Petrini JR. Differences in mortality between late-preterm and term singleton infants in the United States, 1995–2002. J Pediatr. 2007;151:450–6. doi: 10.1016/j.jpeds.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 30.National Healthy Start Association. Strategic plan 2005–2008. Washington: National Healthy Start Association; 2006. [Google Scholar]
- 31.March of Dimes. March of Dimes seeks answers to premature birth [press release]; 2008 Feb 11. [cited 2008 May 12]. Available from: URL: http://www.marchofdimes.com/aboutus/22684_28768.asp.
- 32.Wright VC, Chang J, Jeng G, Chen M, Macaluso M. Assisted reproductive technology surveillance—United States, 2004 [published erratum appears in MMWR Morb Mortal Wkly Rep 2007;56(26):658] MMWR Surveill Summ. 2007;56(SS-6):1–22. [PubMed] [Google Scholar]
- 33.Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371:75–84. doi: 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ananth CV, Vintzileos AM. Medically indicated preterm birth: recognizing the importance of the problem. Clin Perinatol. 2008;35:53–67. doi: 10.1016/j.clp.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 35.Bettegowda VR, Dias T, Davidoff MJ, Damus K, Callaghan WM, Petrini JR. The relationship between cesarean delivery and gestational age among U.S. singleton births. Clin Perinatol. 2008;35:309–23. doi: 10.1016/j.clp.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 36.Malloy MH, MacDorman MF. Changes in the classification of sudden unexpected infant deaths: United States, 1992–2001. Pediatrics. 2005;115:1247–53. doi: 10.1542/peds.2004-2188. [DOI] [PubMed] [Google Scholar]
- 37.National Center for Health Statistics. Health, United States, 2008, with chartbook on trends in the health of Americans. Hyattsville (MD): National Center for Health Statistics; 2009. [Google Scholar]
- 38.Organisation for Economic Cooperation and Development. OECD health data, 2008. Paris: OECD. 2008. [cited 2008 Apr 28]. Also available from: URL: http://www.oecd.org/document/33/0,3343,en_2825_293564_34973665_1_1_1_1,00.html.
- 39.Chung HJ, Muntaner C. Politicial and welfare state determinants of infant and child health indicators: an analysis of wealthy countries. Soc Sci Med. 2006;63:829–42. doi: 10.1016/j.socscimed.2006.01.030. [DOI] [PubMed] [Google Scholar]
- 40.Macinko JA, Starfield B. Wage inequality, the health system, and infant mortality in wealthy industrialized countries, 1970–1996. Soc Sci Med. 2004;58:279–92. doi: 10.1016/s0277-9536(03)00200-4. [DOI] [PubMed] [Google Scholar]
- 41.Martin JA, Kung H-C, Mathews TJ, Hoyert DL, Strobino DM, Guyer B, et al. Annual summary of vital statistics: 2006. Pediatrics. 2008;121:788–801. doi: 10.1542/peds.2007-3753. [DOI] [PubMed] [Google Scholar]
- 42.Graafmans WC, Richardus JH, MacFarlane A, Rebagliato M, Blondel B, Berloove-Vanhorick SP, et al. Comparability of published perinatal mortality rates in Western Europe: the quantitative impact of differences in gestational age and birthweight criteria. BJOG. 2001;108:1237–45. doi: 10.1111/j.1471-0528.2001.00291.x. [DOI] [PubMed] [Google Scholar]
- 43.Lack N, Zeitlin J, Krebs L, Kunzel W, Alexander S. Methodological difficulties in the comparison of indicators of perinatal health across Europe. Eur J Obstet Gynecol Reprod Biol. 2003;111(Suppl 1):S33–44. doi: 10.1016/j.ejogrb.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 44.MacFarlane A, Gissler M, Bolumar F, Rasmussen S. The availability of perinatal health indicators in Europe. Eur J Obstet Gynecol Reprod Biol. 2003;111(Suppl 1):S15–32. doi: 10.1016/j.ejogrb.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 45.United Nations. 2004 demographic yearbook. New York: United Nations; 2007. [cited 2008 Apr 28]. Also available from: URL: http://unstats.un.org/unsd/demographic/products/dyb/dybsets/2004%20DYB.pdf. [Google Scholar]