Abstract
Objectives
To compare outcome and resource utilisation among patients referred to the Amalthea Project, a liaison organisation that facilitates contact between voluntary organisations and patients in primary care, with patients receiving routine general practitioner care.
Design
Randomised controlled trial with follow up at one and four months.
Setting
26 general practices in Avon.
Participants
161 patients identified by their general practitioner as having psychosocial problems.
Main outcome measures
Primary outcomes were psychological wellbeing (assessed with the hospital anxiety and depression scale) and social support (assessed using the Duke-UNC functional social support questionnaire). Secondary outcomes were quality of life measures (the Dartmouth COOP/WONCA functional health assessment charts and the delighted-terrible faces scale), cost of contacts with the primary healthcare team and Amalthea Project, cost of prescribing in primary care, and cost of referrals to other agencies, over four months.
Results
The Amalthea group showed significantly greater improvements in anxiety (average difference between groups after adjustment for baseline −1.9, 95% confidence interval −3.0 to −0.7), other emotional feelings (average adjusted difference −0.5, −0.8 to −0.2), ability to carry out everyday activities (−0.5, −0.8 to −0.2), feelings about general health (−0.4, −0.7 to −0.1), and quality of life (−0.5, −0.9 to −0.1). No difference was detected in depression or perceived social support. The mean cost was significantly greater in the Amalthea arm than the general practitioner care arm (£153 v £133, P=0.025).
Conclusion
Referral to the Amalthea Project and subsequent contact with the voluntary sector results in clinically important benefits compared with usual general practitioner care in managing psychosocial problems, but at a higher cost.
Introduction
The white paper Saving Lives: Our Healthier Nation advocates promoting good mental health by drawing on community support structures, such as voluntary organisations, to help manage psychosocial problems.1 Such problems present major workload implications for primary care. Over three quarters of patients consulting their general practitioner admit to at least one psychosocial problem, and over one third report that psychosocial problems impact on their present health.2
It can, however, be difficult for general practitioners to help patients with psychosocial problems access the voluntary sector.3–6 Until the widespread introduction of counsellors into primary care,7 few contacts with general practitioners for psychosocial problems resulted in referrals to other professionals.8,9 Many general practitioners depend on pharmacological treatments for patients with even minor psychosocial stress.8 The failure to involve other services may reflect lack of availability of appropriate services. The Amalthea Project was commissioned in 1995 by general practitioners who wanted improved access to the numerous voluntary organisations with a potentially useful role in the management of psychosocial problems. This NHS funded project was set up to collect information about the voluntary sector. Referrals facilitators were employed to assess patients and recommend appropriate voluntary organisations. The project aimed to improve patients' quality of life and to decrease time spent by healthcare professionals dealing with psychosocial problems.
Perceptions of the project's usefulness and effectiveness in primary care were wide ranging, so Avon Health Authority commissioned a randomised study to compare referral to the Amalthea Project with routine general practitioner care.
Participants and methods
Patient recruitment and eligibility
Patients were recruited between August 1997 and September 1998 from 26 general practices in Avon with varied socioeconomic characteristics (Townsend scores −1.2 to 3.6).10 Eligible patients were those aged 16 years or over with psychosocial problems who general practitioners thought might benefit from contact with the voluntary sector (excluding patients unable to complete questionnaires owing to language difficulties, illiteracy, or learning disability).
Eligible patients were identified and randomised by their general practitioners by sequentially opening numbered sealed opaque envelopes that had been prepared in advance by the research team. Randomisation was stratified by general practice. Block randomisation was used, with general practitioners supplied with blocks of six (three intervention patients and three control patients). For logistical reasons patients were randomised before completing their baseline assessment. Ethical approval was obtained from the local research ethics committee. At recruitment the general practitioners recorded the patients' demographic details, history of mental health, and reasons for referral.
Trial arms
Patients randomised to the Amalthea Project were referred by their general practitioner, who they were able to continue seeing as usual. Three project facilitators from different backgrounds were trained and supervised by the organisation. Patients were offered an initial assessment within seven days of referral and were followed up on one or more occasions to provide support and to encourage attendance at recommended local and national voluntary organisations. Occasionally, statutory organisations were suggested or new support groups, such as one for single mothers, established.
Patients randomised to the control group received routine care from their general practitioner.
Assessments
The patients supplied data before treatment (baseline assessment) and one and four months after randomisation (follow up assessments). They completed the baseline assessment after randomisation, usually before leaving the practice. Questionnaires for follow up assessment were mailed to patients. Non-responders were sent a further two postal questionnaires.
To maximise response rates in the group of patients known to be poor responders brief, self report measures were chosen as outcome measures.11 Primary outcomes were psychological wellbeing, assessed with the hospital anxiety and depression scale,12 and social support, assessed with the Duke-UNC functional social support questionnaire.13 Secondary outcomes were facets of quality of life, assessed with the Dartmouth COOP/WONCA functional health assessment charts14 and the delighted-terrible faces scale.15
Statistical analysis
We analysed data on an intention to treat basis, using SPSS for Windows. For all primary and secondary outcomes we carried out repeated measures analyses of covariance for follow up scores at one and four months after adjustment for baseline. These analyses investigated the differences between the two follow up scores and their average. To allow for multiple comparisons we adjusted the secondary outcome analyses using the Bonferroni correction.
Economic data
During the follow up period data were collected on the number and duration of contacts with members of the primary healthcare team, prescribing in primary care, and referrals to other agencies. Details of contacts with facilitators were recorded for intervention patients.
Economic analysis
We compared the NHS resource utilisation of patients in the two groups by economic analysis. Resources measured were primary care time and Amalthea time, prescribing in primary care (all drugs and mental health drugs), and referrals to other agencies (excluding voluntary agencies). We calculated the costs of the primary healthcare team members' time from unit costs of health and social care.16 Amalthea time was costed at £14 per hour, based on annual running costs (including on costs—that is, essential associated costs such as employer's national insurance contributions on salaries) of the organisation and number of weeks worked in a year. Referral costs were based on prices set by NHS trusts in Avon. All costs were for the period 1997-8. As the data were not normally distributed, the total cost of each group was compared using the Mann-Whitney test.
Results
Recruitment
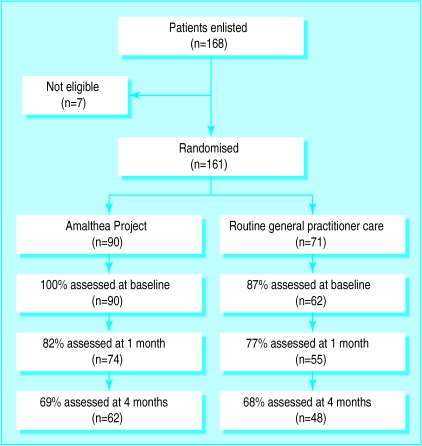
Overall, 168 patients were recruited to the trial. One patient did not meet the entry criteria, and in six patients from two practices there was evidence that the randomisation process had not been properly understood in the early stages of the study. Thus 161 patients were included, of whom 90 were randomly allocated to the intervention arm and 71 to the control arm (figure).
Voluntary sector contacts for the Amalthea group
National Schizophrenia Fellowship
Counselling on Alcohol and Drugs
Alcoholics Anonymous
Over Eaters Anonymous
Local eating disorders group
Triumph over Phobia
Womankind
Counselling Network
CRUSE
RELATE
Befrienders International
Local carer support group
Princess Royal Trust for Carers
Royal British Legion
Crisis
Migraine Trust
Local assertiveness training group
National Society for the Prevention of Cruelty to Children
Multiple Sclerosis Society
Disability Living Foundation
British Trust for Conservation Volunteers
Citizens Advice Bureau
Local meet a mum association
Local toddler group
Local social group for the elderly
University of the Third Age
Brunelcare
Battle against Tranquillisers
Women's Royal Voluntary Service
Baseline comparability
The study arms were broadly similar at baseline (table 1). In the Amalthea group patients were slightly more likely to be male and younger than patients in the general practitioner group. The most common problems leading to referral in both arms were anxiety or stress, depression, and interpersonal or relationship difficulties (table 2).
Table 1.
Characteristics of patients at baseline. Values are numbers (percentages) unless stated otherwise
| Characteristic | Amalthea group (n=90) | General practitioner group (n=71) |
|---|---|---|
| Sex: | ||
| Female | 65 (72) | 56 (79) |
| Male | 25 (28) | 15 (21) |
| Mean (SD) age in years (range): | ||
| All patients | 40.8 (15.5, 17-86) | 45.6 (16.8, 18-86) |
| Marital status: | ||
| Single | 23 (26) | 14 (22) |
| Married or cohabiting | 40 (44) | 29 (45) |
| Widowed | 7 (8) | 7 (11) |
| Divorced or separated | 20 (22) | 14 (22) |
| Data missing | 0 | 7 |
| Social class: | ||
| I and II | 13 (15) | 11 (18) |
| III manual and non manual | 22 (25) | 15 (25) |
| IV and V | 9 (10) | 4 (7) |
| Economically inactive | 44 (50) | 31 (51) |
| Data missing | 2 | 10 |
| History of mental illness: | ||
| Yes | 18 (24) | 12 (25) |
| Data missing | 16 | 22 |
Table 2.
Number and nature of reasons for referral of patients. Values are numbers (percentages) unless stated otherwise
| Amalthea group (n=90) | General practitioner group (n=71) | |
|---|---|---|
| Mean No of reasons for referral (SD, range) | 2.9 (1.4, 1-8) | 2.6 (1.4, 1-6) |
| Reasons for referral: | ||
| Interpersonal or relationship difficulties | 50 (56) | 35 (49) |
| Anxiety or stress | 60 (67) | 41 (58) |
| Bereavement or loss | 22 (24) | 18 (25) |
| Depression | 49 (54) | 29 (41) |
| Social isolation | 27 (30) | 21 (30) |
| Financial problems | 21 (23) | 17 (24) |
| Psychological adjustment to illness | 12 (13) | 15 (21) |
| Substance misuse | 11 (12) | 4 (6) |
| Other reasons | 6 (7) | 5 (7) |
Non-responders
At the one month follow up the only significant differences between responders and non-responders were that the non-responders were younger (mean difference in age 6.9 years, 95% confidence interval 1.6 to 12.1) and more likely to have been referred for substance misuse (P=0.04). The only significant differences at the four month follow up were that non-responders were younger (5.6 years, 0.3 to 11.0) and more likely to have been referred for psychological maladjustment to physical illness (P=0.001).
Process measures
The mean number of contacts with a facilitator was 1.7 (SD 1.2, range 0-6). Seventeen (19%) patients referred to the project could not be contacted. Of those contacted, 71 (97%) received an initial assessment and 58 (80%) received further contact. A wide variety of organisations were recommended to the patients (box).
Primary and secondary outcome measures
Table 3 shows the mean baseline and follow up scores. Baseline scores were missing for nine control patients; six were uncontactable and three declined to complete the questionnaires. Table 4 shows differences between means for the two groups averaged across the two follow up periods, adjusted for baseline score. Significant differences existed between the groups for one primary and six secondary outcome measures at the combined follow up period. The Amalthea group showed greater improvement on the hospital anxiety and depression scale, the COOP/WONCA functional health assessment charts for pain, feelings, daily activities, change in health, and overall health, and the delighted-terrible faces scale. With the Bonferroni correction (corrected α=0.00625) these differences remained significant except for the change in health scale. There was no evidence that the between group differences changed across the two follow up periods (P values for the relevant group by time interactions ranged from 0.05 to 0.77). Adjustment for demographic variables with some imbalances between arms (age and sex) had no impact on results in table 4.
Table 3.
Outcome measures at baseline and at follow up at one and four months
| Outcome measure | No for whom data available
|
Mean (SD) score
|
|||
|---|---|---|---|---|---|
| Amalthea group (n=90) | General practitioner group (n=71) | Amalthea group (n=90) | General practitioner group (n=71) | ||
| Hospital anxiety and depression scale | |||||
| Anxiety: | |||||
| Baseline | 90 | 62 | 14.0 (3.1) | 13.6 (3.8) | |
| 1 month | 74 | 55 | 11.8 (3.9) | 12.4 (4.3) | |
| 4 months | 62 | 48 | 10.6 (4.2) | 12.7 (4.3) | |
| Depression: | |||||
| Baseline | 90 | 62 | 9.8 (3.6) | 10.7 (4.5) | |
| 1 month | 74 | 55 | 8.5 (3.8) | 8.9 (4.3) | |
| 4 months | 62 | 48 | 7.1 (4.5) | 9.4 (4.9) | |
| DUKE-UNC functional social support scale | |||||
| Confidant support: | |||||
| Baseline | 87 | 59 | 15.4 (5.7) | 16.2 (5.7) | |
| 1 month | 73 | 55 | 14.8 (5.6) | 15.4 (6.4) | |
| 4 months | 61 | 48 | 13.8 (5.7) | 15.4 (6.1) | |
| Affective support: | |||||
| Baseline | 86 | 59 | 8.1 (3.4) | 9.0 (3.8) | |
| 1 month | 73 | 52 | 8.3 (3.5) | 8.5 (4.1) | |
| 4 months | 60 | 44 | 8.1 (3.5) | 8.8 (4.1) | |
| COOP/WONCA functional health assessment charts | |||||
| Pain: | |||||
| Baseline | 89 | 60 | 3.0 (1.4) | 3.0 (1.3) | |
| 1 month | 74 | 54 | 2.7 (1.3) | 3.3 (1.1) | |
| 4 months | 62 | 47 | 2.6 (1.4) | 3.1 (1.3) | |
| Physical fitness: | |||||
| Baseline | 87 | 62 | 3.1 (1.1) | 3.2 (1.2) | |
| 1 month | 73 | 55 | 3.2 (1.0) | 3.3 (1.2) | |
| 4 months | 62 | 48 | 2.9 (1.1) | 3.2 (1.1) | |
| Feelings: | |||||
| Baseline | 89 | 62 | 4.4 (0.7) | 4.5 (0.8) | |
| 1 month | 74 | 55 | 3.6 (1.0) | 3.8 (1.0) | |
| 4 months | 62 | 48 | 3.3 (1.2) | 3.9 (1.0) | |
| Daily activities: | |||||
| Baseline | 89 | 62 | 3.2 (1.0) | 3.3 (1.0) | |
| 1 month | 74 | 54 | 2.8 (1.0) | 3.1 (1.0) | |
| 4 months | 62 | 48 | 2.4 (1.0) | 3.1 (1.0) | |
| Social activities: | |||||
| Baseline | 89 | 62 | 3.2 (1.2) | 3.4 (1.3) | |
| 1 month | 74 | 54 | 2.9 (1.2) | 2.9 (1.3) | |
| 4 months | 62 | 48 | 2.6 (1.2) | 3.1 (1.3) | |
| Change in health: | |||||
| Baseline | 88 | 62 | 3.2 (1.0) | 3.4 (0.9) | |
| 1 month | 73 | 54 | 2.7 (0.9) | 2.9 (0.9) | |
| 4 months | 62 | 48 | 2.7 (1.0) | 3.1 (1.1) | |
| Overall health: | |||||
| Baseline | 88 | 62 | 3.9 (0.8) | 4.1 (0.8) | |
| 1 month | 73 | 54 | 3.6 (0.9) | 3.9 (0.7) | |
| 4 months | 62 | 48 | 3.5 (1.1) | 4.0 (0.9) | |
| Delighted-terrible faces scale | |||||
| Baseline | 89 | 62 | 3.9 (0.9) | 4.0 (0.9) | |
| 1 month | 73 | 53 | 3.3 (1.0) | 3.5 (1.0) | |
| 4 months | 62 | 48 | 3.0 (1.1) | 3.6 (1.0) | |
Table 4.
Difference between mean outcome measure scores of patients in two arms of trial from repeated measures analysis of covariance after adjustment for baseline score
| Outcome measure | Differences for combined follow up period (95% CI) | P value |
|---|---|---|
| Hospital anxiety and depression scale | ||
| Anxiety | −1.9 (−3.0 to −0.7) | 0.002 |
| Depression | −0.9 (−1.9 to 0.2) | 0.116 |
| DUKE-UNC functional social support scale | ||
| Confidant support | −0.9 (−2.4 to 0.6) | 0.221 |
| Affective support | −0.3 (−1.2 to 0.7) | 0.594 |
| COOP/WONCA functional health assessment chart | ||
| Pain | −0.5 (−0.8 to −0.1) | 0.005 |
| Physical fitness | −0.3 (−0.6 to 0.05) | 0.098 |
| Feelings | −0.5 (−0.8 to −0.2) | 0.003 |
| Daily activities | −0.5 (−0.8 to −0.2) | 0.001 |
| Social activities | −0.3 (−0.6 to 0.1) | 0.195 |
| Change in health | −0.3 (−0.6 to −0.03) | 0.030 |
| Overall health | −0.4 (−0.7 to −0.1) | 0.003 |
| Delighted-terrible faces | −0.5 (−0.9 to −0.1) | 0.006 |
Economic measures
The economic analysis is summarised in table 5. Patients in both groups had equal numbers of contacts with primary care. The Amalthea group received more prescriptions for all drugs, and mental health drugs in particular. Antidepressants were the most frequently prescribed mental health drugs (65% in Amalthea group and 78% in control group), followed by anxiolytics and hypnotics (25% and 22%). The Amalthea group had fewer referrals to other agencies, including mental health agencies, but the total cost (including facilitators' time) was significantly greater than in the control group (Mann-Whitney P=0.025).
Table 5.
Mean and range of resource utilisation for patients in two arms of trial
| Outcome measure | Amalthea group (n=89)* | General practitioner group (n=68)† |
|---|---|---|
| No of contacts with primary healthcare team | 4.4 (1-13) | 4.4 (1-13) |
| Cost of contacts with primary healthcare team (£) | 61 (14-188) | 69 (9-202) |
| No of prescriptions | 3.2 (0-30) | 2.9 (0-16) |
| No of mental health prescriptions | 1.9 (0-30) | 0.9 (0-8) |
| Cost of prescriptions (£) | 25 (0-169) | 22 (0-209) |
| No of referrals | 0.3 (0-2) | 0.5 (0-4) |
| No of mental health referrals | 0.2 (0-2) | 0.3 (0-2) |
| Cost of referrals (£) | 21 (0-146) | 42 (0-322) |
| Total cost of primary healthcare team contacts, prescribing, and referrals (£) | 107 (14-340) | 133 (10-452) |
| Cost of time of Amalthea Project facilitator (£) | 47 (0-173) | 0 |
| Total cost (£) | 153 (33-413) | 133 (10-452) |
Data missing for one patient.
Data missing for three patients.
Discussion
Primary care and the voluntary sector
The difficulties establishing a productive partnership between primary care and the voluntary sector are well acknowledged.3–6 The Amalthea Project is not the only scheme set up to encourage closer links.3,17 It is, however, the first to be assessed by both a randomised controlled trial and economic evaluation.
Study findings
This study shows beneficial effects on patients' wellbeing. Compared with routine care, referral to the project reduced anxiety and other emotional problems. Patients felt more positive about their health, life in general, and ability to carry out everyday activities. In contrast to anxiety, symptoms of depression benefited equally from usual care and referral to the project. This could be because anxiety or stress was the most common reason for referral (with mean baseline anxiety scores higher than mean baseline depression scores in both arms) and so formed the main focus for management by the project. The study provides no evidence for beneficial effects on perceived social support. Control patients were more likely to be referred to other agencies. These agencies may have been equally effective at improving perceived social support.
The total cost of care was significantly greater in the Amalthea group. Amalthea patients received more mental health prescriptions, which could partly explain the benefits observed, although most prescriptions were for antidepressants rather than anxiolytics. Psychological interventions in primary care can, but do not necessarily, result in savings in mental health prescribing.18
Methodological issues
Despite efforts to recruit all suitable patients, the numbers potentially eligible but not recruited are unknown. The problems with participation of general practitioners in randomised controlled trials are well reported.19,20 Some general practitioners regarded the project as a good thing and were reluctant to recruit patients to a trial with only a 50% chance of referral to the service. We anticipated that each general practitioner would recruit at least six patients. In fact most used half or less of their six randomisation envelopes. This accounted for most of the between arm imbalance in numbers; unintentional non-sequential opening of randomisation envelopes accounted for the remainder. Random allocation was reliably maintained, however.
The number of patients excluded from the study because they were illiterate or could not speak or read English is unknown. Such patients could have considerable psychosocial problems and their exclusion may limit the generalisability of our findings.
The general practices recruited were not a random sample. Participating doctors were likely to be more interested in the research question and may have managed psychosocial problems more actively, which could have attenuated the estimate of effectiveness of the intervention.
Our follow up period, chosen to minimise losses to follow up, could be criticised for being too short. It seemed unlikely that differences not apparent at four months would emerge later, as the project intervention is immediate and short lived, although voluntary sector contact may be ongoing. The proportion of patients lost to follow up at one and four months was similar in both arms. A 32% loss to follow up at four months could have resulted in bias, in an unknown direction, but was much as expected for this group of patients.11
Our entry criteria were broad and relied on general practitioners' definitions of psychosocial problems in the absence of an acceptable standard diagnostic system.21 Stricter entry criteria might have limited recruitment to the study as well as its external validity.
Voluntary sector and patients' costs were not included. The omission of data on contact with the voluntary sector is a limitation of our study. Without such data it is difficult to determine the extent to which the success of the intervention was due to the contact patients had with the project itself as opposed to with the voluntary agencies suggested to them.
Conclusion
Our study provides evidence to support referral of patients with psychosocial problems to a referrals facilitator, who arranges contact with voluntary organisations. Patients were less anxious but their care was more costly and contact with primary care was not reduced. Voluntary sector costs need to be assessed further, but our trial suggests a role for referrals facilitators in the management of psychosocial problems in primary care.
What is already known on this topic
The management of patients with psychosocial problems in primary care has major workload implications
The voluntary sector is rarely involved, despite the potentially useful role it has to play
Several schemes have been set up to encourage links between primary care and the voluntary sector; their effectiveness has not been assessed by randomised controlled trials and economic evaluation
What this paper adds
Referral to a service that facilitates contact between primary care and the voluntary sector is better than usual general practitioner care in improving the wellbeing of patients with psychosocial problems
Referral had no effect on patients' perceived social support, did not save time in primary care, and was more costly than usual general practitioner care
Referrals facilitators could have a role in the management of psychosocial problems in primary care, although voluntary sector costs need further assessment
Supplementary Material
Figure.
Trial profile of Amalthea Project
Acknowledgments
We thank the general practices and Amalthea Project facilitators for their help with data collection, Tim Peters for statistical advice, Kate Baxter and Luke Archard for health economics advice, and Chris Salisbury and Tom Fahey for helpful comments on this paper.
Editorial by Crombie and Coid
Footnotes
Funding: Avon Health Authority.
Competing interests: None declared.
website extra: The sample size calculation appears on the BMJ's website www.bmj.com
References
- 1.Secretary of State for Health. Saving lives: our healthier nation. London: Stationery Office; 1999. [Google Scholar]
- 2.Gulbrandsen P, Hjortdahl P, Fugelli P. General practitioners' knowledge of their patients' psychosocial problems: multipractice questionnaire survey. BMJ. 1997;314:1014–1018. doi: 10.1136/bmj.314.7086.1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Black ME. Self help groups and professionals—what is the relationship? BMJ. 1988;296:1485–1486. doi: 10.1136/bmj.296.6635.1485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Black N. Partnership for health: voluntary organisations and the NHS. BMJ. 1988;296:82. doi: 10.1136/bmj.296.6615.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Payne M, Clayton S. Voluntary organisations: an underused asset. Br J Gen Pract. 1987;37:339–340. [PMC free article] [PubMed] [Google Scholar]
- 6.Graham N. GPs and voluntary organisations. Br J Gen Pract. 1995;45:272–273. [Google Scholar]
- 7.Sibbald B, Addington-Hall J, Brenneman D, Freeling P. Counsellors in English and Welsh general practices: their nature and distribution. BMJ. 1993;306:29–33. doi: 10.1136/bmj.306.6869.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whitehouse CR. A survey of the management of psychosocial illness in general practice in Manchester. Br J Gen Pract. 1987;37:112–115. [PMC free article] [PubMed] [Google Scholar]
- 9.Verhaak PFM, Wennink HJ. What does a doctor do with psychosocial problems in primary care? Int J Psychiatry Med. 1990;20:151–162. doi: 10.2190/WHGG-2KQG-65GN-57YJ. [DOI] [PubMed] [Google Scholar]
- 10.Gordon D, Forrest R. People and places 2; social and economic distinctions in England. Bristol: School for Advanced Urban Studies and Bristol Statistical Monitoring Unit; 1995. [Google Scholar]
- 11.Harvey I, Nelson SJ, Lyons RA, Unwin C, Monaghan S, Peters TJ. A randomised controlled trial and economic evaluation of counselling in primary care. Br J Gen Pract. 1998;48:1043–1048. [PMC free article] [PubMed] [Google Scholar]
- 12.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 13.Broadhead WE, Gehlbach SH, De Gruy FV, Kaplan BH. The Duke-UNC functional social support questionnaire. Measurement of social support in family medicine patients. Med Care. 1988;26:709–723. doi: 10.1097/00005650-198807000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Nelson F, Wasson J, Kirk J, Keller A, Clark D, Dietrich A. Assessment of function in routine clinical practice: description of the COOP chart method and preliminary findings. J Chronic Dis. 1987;40:55–63. doi: 10.1016/s0021-9681(87)80033-4. [DOI] [PubMed] [Google Scholar]
- 15.Andrews FM, Withey SB. Developing measures of perceived quality of life: results from several national surveys. Soc Indicators Res. 1974;1:1–26. [Google Scholar]
- 16.Netten A, Dennett J. Unit costs of health and social care. Kent: Personal Social Services Research Unit; 1997. [Google Scholar]
- 17.Baker D, Tucker C. The liaison between voluntary organisations and general practice: part II—the liaison officer's scheme. Bristol: Bristol University; 1996. [Google Scholar]
- 18.Fletcher J, Fahey T, McWilliam J. Relationship between the provision of counselling and the prescribing of antidepressants, hypnotics and anxiolytics in general practice. Br J Gen Pract. 1995;45:467–469. [PMC free article] [PubMed] [Google Scholar]
- 19.Tognoni G, Alli C, Avanzini F, Bettelli G, Colombo F, Corso R, et al. Randomised clinical trials in general practice: lessons from a failure. BMJ. 1991;303:969–971. doi: 10.1136/bmj.303.6808.969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fairhurst K, Dowrick C. Problems with recruitment in a randomised controlled trial of counselling in general practice: causes and implications. J Health Serv Res Policy. 1996;1:77–80. doi: 10.1177/135581969600100205. [DOI] [PubMed] [Google Scholar]
- 21.Sharp DJ, King M. Classification of psychosocial disturbance in general practice. Br J Gen Pract. 1989;39:356–358. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.