Abstract
The majority of clinical trials of cognitive-behavioral therapy (CBT) for schizophrenia have used individual therapy to target positive symptoms. Promising results have been found, however, for group CBT interventions and other treatment targets like psychosocial functioning. CBT for functioning in schizophrenia is based on a cognitive model of functional outcome in schizophrenia that incorporates dysfunctional attitudes (eg, social disinterest, defeatist performance beliefs) as mediators between neurocognitive impairment and functional outcome. In this report, 18 clinical trials of CBT for schizophrenia that included measures of psychosocial functioning were reviewed, and two-thirds showed improvements in functioning in CBT. The cognitive model of functional outcome was also tested by examining the relationship between social disinterest attitudes and functional outcome in 79 people with schizophrenia randomized to either group cognitive-behavioral social skills training or a goal-focused supportive contact intervention. Consistent with the cognitive model, lower social disinterest attitudes at baseline and greater reduction in social disinterest during group therapy predicted better functional outcome at end of treatment for both groups. However, the groups did not differ significantly with regard to overall change in social disinterest attitudes during treatment, suggesting that nonspecific social interactions during group therapy can lead to changes in social disinterest, regardless of whether these attitudes are directly targeted by cognitive therapy interventions.
Keywords: functioning, cognitive-behavioral treatment, social disinterest attitudes, group therapy
Introduction
The majority of published clinical trials of cognitive-behavioral therapy (CBT) for psychosis have targeted medication-resistant positive symptoms.1 While symptom reduction remains an important treatment goal in therapies for schizophrenia, clients, families, and advocacy groups frequently describe functional impairment in work, education, independent living, and socialization, as being of chief concern to them. Deficits in the performance of these critical real-world functioning activities are present in many neuropsychiatric conditions but are particularly common in schizophrenia.2 Disability in schizophrenia occurs even following successful treatment of the clinical symptoms of the illness.3 This disability sets in immediately after the first episode3 and persists into late life. Although aging in people with schizophrenia is typically associated with improvement in positive symptoms and reduced hospitalization, approximately 60% of older people with schizophrenia in the United States still reside in assisted care settings (eg, board-and-care homes).4 As a result, the vast majority of people with schizophrenia could potentially benefit from interventions targeting disability reduction. Interventions guided by research on the factors that contribute to functional impairment in schizophrenia are needed.5
Model of Functional Impairment in Schizophrenia
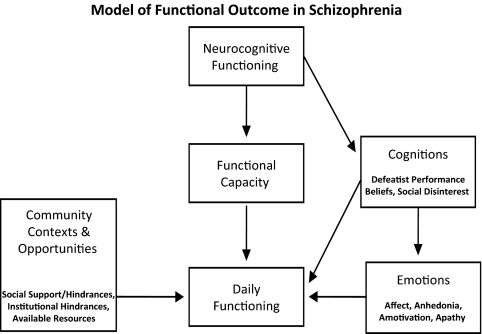
It is well established that neurocognitive deficits are associated with functional impairment in schizophrenia.6,7 However, deficits on neuropsychological tests account for only a moderate amount of variance in real-world functioning.8 The relationship between neurocognitive impairment and real-world outcome in schizophrenia is mediated by several factors. As shown in figure 1, there is clear evidence that neurocognitive impairment is strongly correlated with functional skill capacity, as measured on performance-based (role-play) measures.9,10 The correlation between functional capacity measures and measures of real-world functioning, however, is much weaker.9,10 This suggests that skill competence is necessary but not sufficient for actual real-world performance of skilled behaviors. A number of factors are likely to mediate the relationship between skill capacity and actual real-world functioning, including personal (eg, attitudes/expectations, anhedonia, motivation, moods, insight, etc) and environmental (eg, supports and hindrances) factors that clearly influence functional outcome.9,11,12 Failure to perform in the real world may be due to one or more of these factors.
Fig. 1.
Cognitive Model of Functional Outcome in Schizophrenia That Incorporates Cognitions, as Well as the Emotional Consequences of Cognitions, as Mediators Between Neurocognitive Impairment, Functional Capacity, and Functional Outcome.
The notion that patient expectations and performance beliefs can influence real-world functioning is a key component of the cognitive model that guides CBT interventions for functioning in schizophrenia, indeed, the premise that beliefs influence behaviors and emotions guides cognitive therapy interventions in general. Consistent with this model, Grant and Beck13 recently reported that dysfunctional performance beliefs and social attitudes play an important role in determining real-world functioning outcomes. Defeatist beliefs (eg, “I always fail,” “It's not worth the effort”) can interfere with performance of real-world functioning activities, despite intact skill capacity. In a path analysis, they found that defeatist beliefs mediated the relationship between neurocognitive impairment and poor functioning in people with schizophrenia and added significantly to the prediction of functioning above and beyond symptoms. Defeatist performance beliefs correlated with both neurocognitive impairment and the avoidance of constructive everyday activities. Emerging neurocognitive impairment associated with high risk for developing psychosis may lead to discouraging everyday failure experiences that lead to negative expectancies and defeatist beliefs. These defeatist beliefs become a critical intermediate process between neurocognitive and functional impairments.13
We (Granholm et al14) also assessed the relationships between neurocognitive impairment, defeatist beliefs about social interactions (eg, “I succeeded/failed,” “I was liked/rejected”), affect, and social functioning in 111 people with schizophrenia, using ecological momentary assessment methods. Participants completed a neuropsychological assessment battery and then completed electronic questionnaires on a personal digital assistant 4 times per day for 1 week. Individuals with more severe neurocognitive impairment were more likely to report negative attitudes about social interactions. In time-lagged hierarchical linear modeling analyses, more defeatist attitudes about social interactions at any point in a day were associated with less positive affect, which, in turn, was a strong predictor of fewer social interactions over subsequent hours. The link between neurocognitive vulnerabilities and social isolation, therefore, was mediated by defeatist beliefs about social interactions that were associated with reduced positive affect. Social anhedonia and reduced positive affect have been linked to poor functional outcome in other studies of schizophrenia and schizotypy.15,16 These findings that social attitudes and defeatist performance beliefs, as well as the negative emotional consequences of these beliefs, can impact real-world functioning in schizophrenia are consistent with the classic cognitive-behavioral model of the reciprocal direct effects thoughts have on feelings and behavior.17 CBT, therefore, can be used to improve functioning by modifying these beliefs that interfere with functional skill performance. In this report, CBT trials that examined functioning in schizophrenia were reviewed and the cognitive model of functioning in schizophrenia was tested by examining the relationship between social interest attitudes and functioning in schizophrenia.
Clinical Trials of CBT for Functioning in Schizophrenia
In a comprehensive meta-analysis of 35 CBT for psychosis clinical trials conducted between 1978 and 2006, Wykes et al. 1 recently showed that, although the vast majority of studies focused on positive symptoms as primary treatment targets, CBT for psychosis also had beneficial impact on various functioning outcomes. Fifteen of the studies reviewed included functioning measures and found that the average effect size for functional improvement (d = 0.378) was comparable to that for positive symptoms (d = 0.372). Respectable improvement in negative symptoms (d = 0.437) was also found across CBT studies.
A more in depth examination of the characteristics of clinical trials that included functional outcome measures is shown in table 1. We included the studies discussed in the Wykes et al1 review, as well as additional randomized clinical trials conducted since that review, that assessed functional outcomes. Review of these studies revealed a number of interesting patterns: (1) half of the clinical trials were conducted in the United Kingdom; (2) mean age in the majority of studies was between 30 and 40 years old, with only one study specifically recruiting young adults (mean age = 22 y) and one older adults (mean age = 54 y); (3) approximately 80% of studies were conducted with samples exclusively comprised of outpatient participants; (4) approximately two-thirds of studies targeted positive symptoms of psychosis as the primary treatment outcome; (5) social functioning was the most common functional outcome assessed and the Social Functioning Scale (SFS; Birchwood et al)18 was the most frequently used measure; (6) approximately two-thirds of trials were conducted using an individual therapy format, typically with individualized case formulations; (7) approximately two-thirds of studies showed significant gains in functioning following treatment; (8) interventions that resulted in limited to no improvement in patient functioning still showed beneficial effects in other domains, such as positive and negative symptom severity and distress, substance abstinence, hopelessness, self-esteem, and cognitive insight.
Table 1.
Functional Outcome in Clinical Trials of CBT for Psychosis
| Study | Country | Sample N (Mean Age, y) | Clinical Setting | Primary Target | Outcome Measures | Type of Treatment | Format | Length | Functional Gains | Other Treatment Gains |
| Bailer et al19 | Germany | 47 (36.4) | OP | F, Neg | DAS-M, | CBT | I | 24 sessions | DAS-M: × | Neg, perceptual abnormalities |
| Barrowclough et al20 | United Kingdom | 113 (38.83) | OP | Pos | GAF | CBT | G | 6 mo | GAF: × | Hopelessness, SES |
| Barrowclough et al21 | United Kingdom | 36 (31.1) | OP | F | SFS, GAF | CBT, MI, family | I | 9 mo | SFS: ×, GAF: √ | Pos, substance abstinence |
| Cather et al22 | United States | 30 (40.4) | OP | Pos, F | SFS | fCBT | I | 16 wk | SFS: × | Pos |
| Daniels23 | United States | 40 (33.7) | OP | F, Neg | CGI, QLS, BAT, GAF | IBT | G | 16 sessions | GAF: √; CGI, BAT, QLS: × | × |
| Durham et al24 | United Kingdom | 66 (36) | OP | Pos | GAS | CBT | I | 9 mo | GAS: × | Del severity |
| Garety et al25 | United Kingdom | 301 (38.1) | OP | Pos | TBM, SOFAS | CBT, family | I | 9 mo | TBM: ×, SOFAS: √ | Del distress |
| Gaudino and Herbert26 | United States | 40 (40) | IP | Pos | SDS | ACT | I | 3 sessions | SDS social scale: √ | Hal distress |
| Gumley et al27 | United Kingdom | 144 (36.2) | OP | Pos | SFS | CBT | I | 12 mo | SFS: √ | Hospitalization, Pos, Neg |
| Granholm et al28 | United States | 76 (53.8) | OP | F | ILSS, UPSA | CBSST | G | 24 sessions | UPSA: ×, ILSS: √ | Cognitive insight |
| Hall and Tarrier29 | United Kingdom | 25 (38) | IP | SES | SFS | CBT | I | 7 sessions | SFS: √ | SES, Dep, Pos, Neg |
| Jackson et al30 | Australia | 62 (22.3) | OP, IP | Pos, F | SOFAS | ACE | I | 14 wk | SOFAS: √ | × |
| Kingsep et al31 | Australia | 33 (—) | OP | SA | QLESQ | CBT | G | 12 sessions | QLESQ: √ | SA, GP |
| Penn et al32 | United States | 65 (40.6) | OP | Pos | SFS | CBT | G | 12 sessions | SFS: × | GP |
| Startup et al33 | United Kingdom | 90 (30.9) | IP | Pos | SFS, GAF | CBT | I | 13 sessions | SFS: √, GAF: √ | Pos, Neg |
| Tarrier et al34 | United Kingdom | 49 (42.77) | OP | Pos | SFS | CSE or PS | I | 5 wk | SFS: × | Pos |
| Wiersma et al35 | Holland | 76 (36.4) | OP | F | GSDS, WHOQoL | CBT, CT, family | I | 9 mo | GSDS social role: √, WHOQoL: √ | Quality of life, Pos, Dep, Disorg |
| Wykes et al36 | United Kingdom | 85 (39.6) | OP | P | SBS | CBT | G | 10 wk | SBS: √ | × |
Note: OP, outpatient; F, functioning; Neg, negative symptoms; DAS-M, Mannheimer Scale for Evaluation of Social Dysfunction; CBT, cognitive-behavioral therapy; I, Individual therapy; ×, no significant improvement; Pos, positive symptoms; GAF, Global Assessment of Functioning; G, group therapy; SES, self-esteem; SFS, Social Functioning Scale; MI, motivational interviewing; √, significant improvement; fCBT, functional cognitive-behavioral therapy; CGI, clinical global impressions; QLS, Quality-of-Life Scale; BAT; behavioral assessment task; IBT, interactive behavioral training; GAS; Global Assessment Scale; Del, delusion; TBM, time budget measure; SOFAS, Social and Occupational Functioning Assessment Scale; IP, inpatient; SDS, Sheehan Disability Scale; ACT, acceptance and commitment therapy; Hal, hallucination; ILSS, Independent Living Skills Survey; UPSA, UCSD performance-based skills assessment; CBSST, cognitive-behavioral social skills training; Dep, depression; ACE, active cognitive therapy for early psychosis; SA, social anxiety; QLESQ, Quality of Life Enjoyment and Satisfaction Questionnaire; GP, general psychopathology; CSE, coping strategy enhancement; PS, problem solving; GSDS; Gronigen Social Disabilities Schedule; WHOQoL; World Health Organization Quality of Life Schedule; CT, coping training; Disorg, disorganization; SBS, social behavior schedule.
Psychosocial interventions that primarily target functioning, like social skills training (SST), are typically more behaviorally oriented, rather than cognitively oriented, and are more commonly conducted in a group, rather than individual format. Wykes et al1did not find significant differences between studies that used group vs individual formats for any outcome. With regard to the studies in table 1, 4 of the 6 studies (66%) that used a group format found significant improvement in functioning on at least one measure, and 8 of the 12 studies (66%) that used an individual format found significant improvement in functioning. Therefore, functioning outcomes were similar in group and individual formats.
Groups and Social Disinterest
It is important to understand how groups can promote change in functioning. Groups can promote socialization and connections with peers struggling with common concerns. Groups can also impact social support systems and allow practice of communication and other social skills with peers, which may be important for interventions that target social functioning. In fact, regular supportive interactions with peers may provide a unique opportunity to modify important social attitudes and interest in interacting with others.
Meehl37 gave primary importance to social anhedonia as impacting social withdrawal and poor functioning in schizophrenia. Social anhedonia is characterized by social disinterest, lack of pleasure from social contact, and withdrawal. The importance of social disinterest and anhedonia has since been born out in more recent research. Consistent with the model in figure 1, social anhedonia has been found to be associated with poor functioning in schizophrenia15,38 and poor social competence in schizotypy.16,39,40 Group therapy may have greater potential than individual therapy for impacting attitude components of social anhedonia, like social disinterest, which, in turn, could impact change in social functioning. In groups, there is greater opportunity for supportive interactions with peers that can provide behavioral experiments that demonstrate the value of interacting with others to solve problems and achieve goals. In this study, the relationship between change in these important social attitudes and improved functioning in a group CBT intervention was investigated. We predicted that reduction in social disinterest in CBT would be associated with improved functioning.
Cognitive-Behavioral Social Skills Training
We developed a group therapy intervention for functional impairment in schizophrenia that combines CBT and SST components, called cognitive-behavioral social skills training (CBSST).41 Adding CBT to SST provides an opportunity to address thoughts that interfere with skill performance in the real world (eg, low self-efficacy, expectancy, and ability beliefs). CBSST was designed to help middle-aged and older people with schizophrenia attain personalized functioning goals. We conducted a randomized controlled trial comparing treatment as usual (TAU) with TAU plus group CBSST28 in middle-aged and older people with schizophrenia or schizoaffective disorder (mean age = 54 y). Intention-to-treat analyses showed significant treatment group effects for functioning, η2 = 0.09; skill mastery, η2 = 0.36; and cognitive insight, η2 = 0.11; at end of treatment, and participants in CBSST continued to show significantly greater skill knowledge (d = 0.61) and self-reported everyday functioning (d = 0.50) relative to participants in TAU at 1-year follow-up.42 Clients in CBSST + TAU, therefore, were able to learn cognitive-behavioral coping skills, showed improved functioning, and became more flexible and objective in their thinking about symptoms (improved cognitive insight). Given that functional impairments persist in this older, very chronic outpatient population, despite relatively good pharmacologic control of psychotic symptoms,4 the significant maintenance at 1-year follow-up of improvement in functioning is noteworthy.
Methods
Design
The purpose of this study was to examine the role of social disinterest attitudes in determining real-world outcome and examine whether group interventions can impact social attitudes to improve functional outcome. The study sample was drawn from 2 separate ongoing randomized clinical trials comparing group CBSST with a goal-focused supportive contact (GFSC) group intervention. One trial enrolled only middle-aged and older (>age 45 y) patients (N = 30), and the other trial enrolled patients aged 18 years or older (N = 49). The interventions were nearly identical in both trials, with the exception that in the all-ages trial, patients also met with one of the group therapists individually at the beginning of treatment and outlined a minimum of 2 personalized functional goals to focus on in group and then met with the same therapist individually every 3 months to discuss goal progress. In the older patient trial, recommended age-related modifications were incorporated, including focus on aging-relevant problems (eg, vision/hearing aids, role loss), and transportation was provided to therapy groups only in this trial. The goal of the study was to test the predictions of the cognitive model of functioning in schizophrenia by determining whether baseline social disinterest attitudes, as well as change in these attitudes in group therapy, predicted future functioning. The goal was not to determine the final outcome of these ongoing trials, with regard to treatment efficacy of CBSST. Broader clinical and functioning outcomes will be presented in future reports, when these trials are completed.
Participants
This study was approved by the Institutional Review Board of the University of California, San Diego, CA, and written informed consent was obtained from all participants or their legal guardians. Community-dwelling participants (N = 109) with either schizophrenia or schizoaffective disorder based on the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition)43 were recruited from treatment centers and residential settings throughout San Diego County, CA. Participants were excluded (N = 30, 28%) for completing less than 50% (18 sessions) of the intervention because we wanted to only include participants who had significant exposure to other individuals in groups, and 18 sessions ensured that participants were exposed to each of the 3 CBSST modules at least once (the modules described below are repeated). The following minimal inclusion/exclusion criteria were used to increase generalizability: age 18 years or older, no prior exposure to SST or CBT in the past 5 years, and level of care required at baseline does not interfere with outpatient group therapy participation (eg, partial or inpatient hospitalization for psychiatric, acute substance use, or physical illness). Hospitalized subjects were still invited to participate (or return to groups) when other forms of treatment no longer interfered with group attendance. Demographic and symptom characteristics of the 2 treatment groups are shown in table 2.
Table 2.
Baseline Participant Characteristics
| GFSC (N = 39) | CBSST (N = 40) | Statistical Analysis | |||||
| N | % | N | % | χ2 | df | P | |
| Male | 27 | 69 | 18 | 45 | 4.73 | 1 | .030 |
| Caucasian | 26 | 67 | 22 | 55 | 1.13 | 1 | .288 |
| Married | 2 | 5 | 3 | 8 | 0.19 | 1 | .665 |
| Assisted living | 26 | 67 | 20 | 50 | 2.26 | 1 | .133 |
| Mean |
SD |
Mean |
SD |
t |
df |
P |
|
| Baseline age (y) | 51.9 | 8.7 | 48.9 | 9.4 | 1.43 | 77 | .156 |
| PANSS total | 69.4 | 19.8 | 65.3 | 17.4 | 0.99 | 77 | .324 |
| RSAS Social Disinterest | 6.9 | 3.0 | 6.2 | 3.0 | 1.03 | 77 | .307 |
| ILSSa | 0.70 | 0.11 | 0.73 | 0.08 | 1.42 | 74 | .160 |
Note: GFSC = goal-focused supportive contact; CBSST = cognitive-behavioral social skills training; PANSS = Positive and Negative Syndrome Scale; RSAS = Revised Social Anhedonia Scale; ILSS = Independent Living Skills Survey.
GFSC (N = 38); CBSST (N = 38).
Interventions
Both group therapy interventions were delivered by 2 therapists with at least masters-level education (clinical psychology or social work) and at least 1-year experience with CBT interventions.
Cognitive-Behavioral Social Skills Training.
CBSST is described in detail elsewhere.41,42 CBSST is a group psychotherapy intervention that has 3 modules (challenging thoughts, asking for support, solving problems). In this study, each module had 6 weekly 2-hour sessions, and participants cycled through the sequence of 3 modules twice, for a total of 36 sessions, followed by 9 monthly booster sessions. Groups were led by 2 therapists. SST components were modified primarily from symptom management, communication role-play, and problem-solving SST modules available from psychiatric rehabilitation consultants.44 The CBT components were developed specifically for patients with schizophrenia.45,46 Cognitive interventions targeted beliefs about psychotic symptoms and negative attributions and self-efficacy beliefs that interfered with functioning behaviors. Aids to compensate for cognitive impairment were also added.
Goal-Focused Supportive Contact.
This control condition is a form of enhanced supportive contact that focused on functional goals and provided the same amount of therapist and group contact as CBSST. Weekly group sessions were semistructured and would typically consist of check-in and symptom review, followed by a flexible discussion of functioning goal attainment in a supportive, respectful manner. All participants were asked to work toward specific personalized functioning goals. Sessions typically included components of psychoeducation, empathy, and nondirective reinforcement of health, coping, and symptom management behaviors that grew out of group discussions. Participants were asked to think about how the discussions had bearing on their individual functioning goals and were encouraged to ask for the advice of other patients in achieving specific goals but were never trained to use any specific cognitive-behavioral coping strategy or skill set.
Outcome Measures
Independent Living Skills Survey.
The Independent Living Skills Survey (ILSS) is a comprehensive self-report measure of everyday functioning that indexed performance of adaptive real-world functioning behaviors.47 The 51-item questionnaire assesses functioning over the past month in 10 areas, but an ILSS composite score was computed as the average of 5 relevant functional domains (appearance and clothing, personal hygiene, health maintenance, transportation, and leisure and community). The 5 ILSS domains that were not used indexed domains not relevant to the majority of participants in this study who lived in board-and-care settings where cleaning and cooking services were provided (2 domains), and almost all were unemployed and receiving disability income that was managed by others (3 domains). Participants, therefore, did not have the opportunity to perform these skills, so a score could not be computed accurately, according to standard scoring rules for the ILSS.47
Social Disinterest.
Fifteen items with face validity (see Appendix) for assessing social disinterest in interacting with others were selected from the Revised Social Anhedonia Scale (RSAS48). The RSAS consists of 40 true/false items designed to assess social anhedonia, which is a heterogeneous construct that includes both social disinterest/amotivation and deficits in the ability to experience pleasure from social-interpersonal relationships.49,50 In order to more specifically tap attitudes of social disinterest, rather than emotional experiences, in the present study, items were selected to avoid items that reflected emotional aspects of social satisfaction and pleasure or general emotional dysregulation that might be tapped by the RSAS.51 Items that might reflect the frequency of actual social interactions were also avoided to reduce overlap with social functioning indexed on the ILSS. Other studies have employed a similar face validity item selection approach when using the RSAS.16 Cronbach's α coefficient for this subscale was .65 at baseline and .66 at end of treatment in the present study sample, which was comparable to internal consistencies found for subscales in factor-analytic studies of the RSAS (eg, in Blanchard et al51; α’s = .57–.70 across 4 factors).
Statistical Analyses
Linear regression models using SPSS (version 11.5) were estimated to examine relationships between attitudes and functioning. Group (coded: GFSC = −0.5, CBSST = +0.5), baseline RSAS social disinterest score, change in RSAS social disinterest between baseline and the end of treatment, and the interaction of group with RSAS social disinterest change were the independent variables used to predict ILSS composite at the end of treatment. To further examine the role change in RSAS social disinterest that had on functioning, the sample was split into 2 groups (clinically significant improvement on RSAS social disinterest defined as 25% reduction from baseline to end of treatment, improver ≥ 25% reduction, nonimprover < 25% reduction). Two-tailed t tests were used to test whether the improver group showed better functioning relative to the nonimprover group on the ILSS at the end of treatment in the full sample and within each treatment group.
Results
Completers and noncompleters did not differ significantly with regard to gender, race, living situation, marital status, PANSS total, ILSS (completer: mean = 0.72, SD = 0.10; noncompleter: mean = 0.70, SD = 0.12), t104 = 0.66, P = .510, or RSAS social disinterest scores (completer: mean = 6.52, SD = 3.01; noncompleter: mean = 6.67, SD = 2.88), t107 = 0.23, P = .818, at baseline. The mean education of completers (mean = 12.6, SD = 1.8) was on average 1 year greater than noncompleters (mean = 11.5, SD = 2.6), t107 = 2.54, P = .013, and the mean age of completers (mean = 50.4, SD = 9.2) was significantly greater than noncompleters (mean = 43.7, SD = 11.9), t107 = 3.12, P = .002. The difference in age was likely due to a lower dropout rate in the clinical trial that enrolled only older patients, where transportation to therapy was provided.
A 2 (treatment groups) × 2 (baseline vs end-of-treatment assessment time) analysis of variance showed that RSAS social disinterest scores did not change significantly between baseline and end of treatment for the full sample (F1,77 = 0.81, P = .371), and the effects of treatment group (F1,77 = 1.65, P = .203) and the group × time interaction were not significant (F1,77 = 0.03, P = .854). The proportion of participants with clinically significant change in RSAS scores also did not differ significantly between the treatment groups (CBSST = 38% improver, GFSC = 28% improver, χ2 = 0.77, P = .379). At the group level, therefore, the extent of overall change in social disinterest attitudes was comparable between the 2 treatment conditions.
Table 3 presents the results of the linear regression model. RSAS social disinterest scores and self-reported everyday functioning (ILSS composite) were not significantly correlated at baseline (r = −.10, P = .387). However, baseline RSAS social disinterest scores and change in RSAS social disinterest scores were statistically significant predictors of self-reported everyday functioning (ILSS) at end of treatment. Higher baseline RSAS social disinterest scores significantly predicted worse functioning at the end of treatment. In addition, subjects who showed greater reduction in RSAS social disinterest attitudes during treatment showed better functioning at end of treatment. The group × RSAS change score interaction was not significant, indicating that the effect of change in social disinterest attitudes on functioning did not differ between treatment groups. Surprisingly, social disinterest was not correlated with the number of group therapy sessions attended (dropout) for the total sample, r = −.18, P = .108, N = 79; CBSST group, r = −.08, P = .634, N = 40; or GFSC group, r = −.29, P = .079, N = 39.
Table 3.
Linear Regression Model of Treatment Group and Social Disinterest Predictors of Everyday Functioning (Independent Living Skills Survey) at End of Treatment
| β | Std β | t | P | |
| Group (CBSST vs GFSC) | .001 | .009 | 0.08 | .938 |
| Baseline social disinterest | −.008 | −.290 | −2.28 | .026 |
| Change in social disinterest | −.010 | −.339 | −2.68 | .009 |
| Group × change in social disinterest | .002 | .041 | 0.37 | .715 |
Note: Full model: R2 = 0.106, F4,74 = 2.19, P = .079. CBSST, cognitive-behavioral social skills training; GFSC, goal-focused supportive contact.
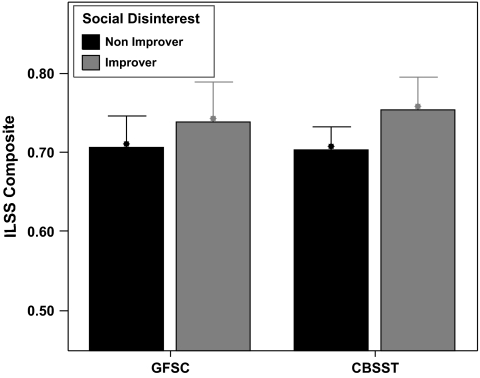
Figure 2 displays mean ILSS scores at end of treatment for RSAS social disinterest improvers and nonimprovers (≥25% reduction during treatment = improvers) within each treatment group. Comparison (t tests) of improver and nonimprover subgroups showed that improvers had significantly better functioning on the ILSS relative to nonimprovers (mean difference = 0.043, t77 = 2.14, P = .035) at the end of treatment for the full sample. Within the CBSST group, improvers showed significantly better functioning than nonimprovers on the ILSS (mean difference = 0.050, t38 = 2.19, P = .035). Within the GFSC group, the difference between improvers and nonimprovers was not significant (mean difference = 0.033, t37 = 0.95, P = .347).
Fig. 2.
Self-reported Everyday Functioning on the Independent Living Skills Survey (ILSS) Composite Score at End of Treatment Is Shown for Social Disinterest Improvers and Nonimprovers in Each Treatment Group (CBSST, cognitive-behavioral social skills Training; GFSC, goal-focused supportive contact). Meaningful improvement in social disinterest was defined as >25% reduction on the Revised Social Anhedonia Scale social disinterest items during treatment. Improvers differed significantly from nonimprovers only in the CBSST group, t38 = 2.19, P = .035.
Discussion
Groups can impact important social disinterest attitudes that are associated with functional outcome. About one-third of participants in each group showed at least 25% reduction in RSAS social disinterest attitudes, and this extent of change in social disinterest was associated with significant improvement in everyday functioning. Social disinterest was significantly associated with poorer functional outcome at end of treatment, and reduction in social disinterest during group therapy was significantly associated with better functional outcome in treatment for both treatment conditions. Increase in social interest, therefore, can occur in both CBT and control conditions that include contact with therapists and peers in a supportive group therapy environment focused on a common concern for improved functioning. CBSST also did not change social attitudes to a greater extent than GFSC. This finding suggests that enhanced supportive group interventions that involve working with peers and therapists to achieve goals can impact important social attitudes, regardless of whether these attitudes are directly targeted using cognitive interventions.
The finding that social disinterest was linked to poorer functional outcome is consistent with prior research showing that social anhedonia is associated with poorer functional outcome in schizotypy and schizophrenia.15,16,38–40 Moreover, the finding that reduction in social disinterest components of social anhedonia over the course of group therapy was associated with better functional outcome at the end of treatment may suggest a causal link between these attitudes and functioning, which could not be concluded on the basis of prior cross-sectional studies alone. Previous longitudinal studies also support a possible causal link between social anhedonia and future poor functional outcome in schizophrenia-spectrum disorders.40 It is possible, however, that functional status can influence social disinterest attitudes. Indeed, this may be a reciprocal relationship (ie, increased social interest leads to improved functioning that leads to more frequent positive social interactions, which further improve social interest, etc).
At the group level, mean self-reported everyday functioning and social attitudes did not differ significantly between treatment groups in these preliminary end-of-treatment analyses. Several other clinical trials (for reviews, see Gould et al52 and Rector and Beck53), including our own prior CBSST trial (Granholm et al28,42), found larger treatment group differences at follow-up than at end of treatment. Supportive contact conditions clearly have active ingredients that can lead to smaller CBT treatment effect sizes, at least while patients still have contact with peers and/or therapists in a therapy context. Penn et al54 have discussed the potential active ingredients of supportive contact control conditions for schizophrenia, including social support, therapeutic alliance with the therapists, and changes in social cognition. These authors note that the association between social support and mental health is well established and that limited social networks in people with schizophrenia are associated with poorer outcomes. Given their empty social networks, people with schizophrenia may be particularly responsive to interactions with therapists, and particularly normalizing relationships with peers in group, where they can learn that rewarding social relationships are possible and helpful for achieving functioning goals and improved quality of life. The mechanism by which social support affects outcome is not known, but Penn et al55 point out that supportive interactions with others can provide stress-buffering information about how one is perceived by others (“reflective appraisals”) that can challenge low self-esteem beliefs and interactions that challenge attributional biases about the negative intentions of others and one's place of importance in the world. Supportive groups may provide positive relationships that can increase confidence and change attitudes about others.
This study had several limitations. The sample size was relatively small, and this was only a preliminary report of findings from an ongoing trial, so conclusions about CBSST treatment efficacy would be premature. In addition, the functioning measure employed was a self-report measure. A more objective indicator or performance-based functioning measure might provide a more accurate estimate of everyday functioning, but the ILSS was sensitive to change in CBSST in our prior clinical trial.28 Also, the RSAS social disinterest subscale created has not been empirically validated as a measure of social disinterest, but the subscale had acceptable internal consistency, and it was essential to create an RSAS subscale that was restricted to nonemotion items tapping attitudes and not social functioning, per se. Finally, no significant group differences were found and a no-therapy control group was not included, so changes in social interest and functioning cannot be specifically attributed to group therapy. The purpose of the study, however, was not to report on CBSST treatment efficacy but to further examine the contribution of cognitive factors to functional outcome in schizophrenia in the context of a cognitive model of functional outcome in schizophrenia. Our prior clinical trial did include a pharmacotherapy-only condition (TAU) and found significantly better functioning on the same outcome measure (ILSS) in CBSST relative to TAU.28
Conclusions
The use of CBT to improve functioning in people with schizophrenia is based on empirical support for a cognitive model of functional outcome in schizophrenia that incorporates cognitions, as well as the emotional consequences of cognitions, as mediators between neurocognitive impairment and functional outcome in schizophrenia. The majority of clinical trials of CBT for schizophrenia have shown significant improvement in functional outcome in people with schizophrenia, regardless of whether functioning was the primary treatment target. Consistent with a cognitive model of functioning in schizophrenia, groups may have active ingredients involving social support with peers that provide a unique opportunity to challenge and modify social disinterest attitudes associated with poor social functioning, regardless of whether these attitudes are directly targeted by cognitive interventions.
Appendix—Social Disinterest Items
My relationships with other people never get very intense. (True)
I prefer hobbies and leisure activities that do not involve other people. (True)
When others try to tell me about their problems and hang-ups, I usually listen with interest and attention. (False)
There are things that are more important to me than privacy. (False)
I prefer watching television to going out with other people. (True)
I like to make long distance phone calls to friends and relatives. (False)
I sometimes become deeply attached to people I spend a lot of time with. (False)
People sometimes think I'm shy when I really just want to be left alone. (True)
People who try to get to know me better usually give up after awhile. (True)
I could be happy living all alone in a cabin in the woods or mountains. (True)
I'm much too independent to really get involved with other people. (True)
There are few things more tiring than to have a long, personal discussion with someone. (True)
I don't really feel very close to my friends. (True)
I find that people too often assume that their daily activities and opinions will be interesting to me. (True)
I attach very little importance to having close friends. (True)
References
- 1.Wykes T, Steel C, Everitt B, Tarrier N. Cognitive behavior therapy for schizophrenia: effect sizes, clinical models, and methodological rigor. Schizophr Bull. 2008;34:523–537. doi: 10.1093/schbul/sbm114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wiersma D, Wanderling J, Dragomirecka E, et al. Social disability in schizophrenia: its development and prediction over 15 years in incidence cohorts in six European centres. Psychol Med. 2000;30:1155–1167. doi: 10.1017/s0033291799002627. [DOI] [PubMed] [Google Scholar]
- 3.Robinson DG, Woerner MG, McMeniman M, Mendelowitz A, Bilder RM. Symptomatic and functional recovery from a first episode of schizophrenia or schizoaffective disorder. Am J Psychiatry. 2004;161:473–479. doi: 10.1176/appi.ajp.161.3.473. [DOI] [PubMed] [Google Scholar]
- 4.Jeste DV, Twamley EW, Eyler Zorrilla LT, Golshan S, Patterson TL, Palmer BW. Aging and outcome in schizophrenia. Acta Psychiatr Scand. 2003;107:336–343. doi: 10.1034/j.1600-0447.2003.01434.x. [DOI] [PubMed] [Google Scholar]
- 5.Bellack AS, Green MF, Cook JA, et al. Assessment of community functioning in people with schizophrenia and other severe mental illness: a white paper based on an NIMH-sponsored workshop. Schizophr Bull. 2007;33:805–822. doi: 10.1093/schbul/sbl035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Green MF, Kern RS, Haeton RK. Longitudinal studies of cognition and functional outcome in schizophrenia: implications for MATRICS. Schizophr Res. 2004;72:41–51. doi: 10.1016/j.schres.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 7.Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr Bull. 2000;26:119–136. doi: 10.1093/oxfordjournals.schbul.a033430. [DOI] [PubMed] [Google Scholar]
- 8.Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry. 1996;153:321–330. doi: 10.1176/ajp.153.3.321. [DOI] [PubMed] [Google Scholar]
- 9.Bowie CR, Reichenberg A, Patterson TL, Heaton RK, Harvey PD. Determinants of real-world functional performance in schizophrenia subjects: correlations with cognition, functional capacity, and symptoms. Am J Psychiatry. 2006;163:418–425. doi: 10.1176/appi.ajp.163.3.418. [DOI] [PubMed] [Google Scholar]
- 10.Keefe RS, Poe M, Walker TM, Kang JW, Harvey PD. The Schizophrenia Cognition Rating Scale: an interview-based assessment and its relationship to cognition, real-world functioning, and functional capacity. Am J Psychiatry. 2006;163:426–432. doi: 10.1176/appi.ajp.163.3.426. [DOI] [PubMed] [Google Scholar]
- 11.Brekke JS, Kay DD, Kee KS, Green MF. Biosocial pathways to functional outcome in schizophrenia. Schizophr Res. 2005;80:213–225. doi: 10.1016/j.schres.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 12.Heaton RK, Marcotte TD, Rivera-Mindt M, et al. The impact of HIV-associated neuropsychological impairment on everyday functioning. J Int Neuropsychol Soc. 2004;10:317–331. doi: 10.1017/S1355617704102130. [DOI] [PubMed] [Google Scholar]
- 13.Grant PM, Beck AT. Defeatist beliefs as a mediator of cognitive impairment, negative symptoms, and functioning in schizophrenia. Schizophr Bull. 2009;35:798–806. doi: 10.1093/schbul/sbn008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Granholm E, Swendsen J, Loh C. Negative social interaction appraisals, mood, and social functioning in schizophrenia. Schizophr Bull. 2009;35:330–331. [Google Scholar]
- 15.Blanchard JJ, Mueser KT, Bellack AS. Anhedonia, positive and negative affect, and social functioning in schizophrenia. Schizophr Bull. 1998;24:413–423. doi: 10.1093/oxfordjournals.schbul.a033336. [DOI] [PubMed] [Google Scholar]
- 16.Brown LH, Silvia PJ, Myin-Germeys I, Kwapil TR. When the need to belong goes wrong: the expression of social anhedonia and social anxiety in daily life. Psychol Sci. 2007;18:778–782. doi: 10.1111/j.1467-9280.2007.01978.x. [DOI] [PubMed] [Google Scholar]
- 17.Beck AT. Thinking and depression: idiosyncratic content and cognitive distortions. Arch Gen Psychiatry. 1963;9:324–333. doi: 10.1001/archpsyc.1963.01720160014002. [DOI] [PubMed] [Google Scholar]
- 18.Birchwood M, Smith J, Cochrane R, Wetton S, Copestake S. The social functioning scale. The development and validation of a new scale of social adjustment for use in family intervention programmes with schizophrenic patients. Br J Psychiatry. 1990;157:853–859. doi: 10.1192/bjp.157.6.853. [DOI] [PubMed] [Google Scholar]
- 19.Bailer J, Takats I, Westermeier C. Efficacy of individualized cognitive-behavioral therapy for schizophrenic patients with negative symptoms and social disabilities: a controlled trial. Z Klin Psychol Psychother. 2001;30:268–278. [Google Scholar]
- 20.Barrowclough C, Haddock G, Lobban F, et al. Group cognitive behavioral therapy for schizophrenia: randomised controlled trial. Br J Psychiatry. 2006;189:1–7. doi: 10.1192/bjp.bp.106.021386. [DOI] [PubMed] [Google Scholar]
- 21.Barrowclough C, Haddock G, Tarrier N, et al. Randomized controlled trial of motivational interviewing, cognitive behaviour therapy, and family intervention of patients with co-morbid schizophrenia and substance use disorder. Am J Psychiatry. 2001;158:1706–1713. doi: 10.1176/appi.ajp.158.10.1706. [DOI] [PubMed] [Google Scholar]
- 22.Cather C, Penn D, Otto M, Yovel I, Mueser K, Goff D. A pilot study of functional cognitive behavioral therapy (fCBT) for schizophrenia. Schizophr Res. 2005;74:201–209. doi: 10.1016/j.schres.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 23.Daniels L. A group cognitive-behavioral and process-oriented approach to treating the social impairment and negative symptoms associated with chronic mental illness. J Psychother Pract Res. 1998;7:167–176. [PMC free article] [PubMed] [Google Scholar]
- 24.Durham RC, Guthrie M, Morton RV, et al. Tayside-Fife clinical trial of cognitive-behavioural therapy for medication-resistant psychotic symptoms: results to 3-month follow-up. Br J Psychiatry. 2003;182:303–311. doi: 10.1192/bjp.182.4.303. [DOI] [PubMed] [Google Scholar]
- 25.Garety PA, Kuipers L, Fowler D, Chamberlain F, Dunn G. Cognitive behavioural therapy for drug resistant psychosis. Br J Psychiatry. 1994;67:259–271. doi: 10.1111/j.2044-8341.1994.tb01795.x. [DOI] [PubMed] [Google Scholar]
- 26.Gaudino B, Herbert J. Acute treatment of inpatients with psychotic symptoms using acceptance and commitment therapy: pilot results. Behav Res Ther. 2006;44:415–437. doi: 10.1016/j.brat.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 27.Gumley A, O'Grady M, McNay L, Reilly J, Power KG, Norrie J. Early intervention for relapse in schizophrenia: results of a 12-month randomised controlled trial of cognitive behavioural therapy. Psychol Med. 2003;33:419–431. doi: 10.1017/s0033291703007323. [DOI] [PubMed] [Google Scholar]
- 28.Granholm E, McQuaid JR, McClure FS, et al. A randomized, controlled trial of cognitive behavioral social skills training for middle-aged and older outpatients with chronic schizophrenia. Am J Psychiatry. 2005;162:520–529. doi: 10.1176/appi.ajp.162.3.520. [DOI] [PubMed] [Google Scholar]
- 29.Hall PL, Tarrier M. The cognitive-behavioral treatment of low self-esteem in psychotic patients: a pilot study. Behav Res Ther. 2003;41:317–332. doi: 10.1016/s0005-7967(02)00013-x. [DOI] [PubMed] [Google Scholar]
- 30.Jackson HJ, Mcorry PD, Killackey E, et al. Acute-phase and 1-year follow-up results of a randomized controlled trial of CBT versus Befriending for first-episode psychosis: the ACE project. Psychol Med. 2008;38:725–735. doi: 10.1017/S0033291707002061. [DOI] [PubMed] [Google Scholar]
- 31.Kingsep P, Nathan P, Castle D. Cognitive behavioural group treatment for social anxiety in schizophrenia. Schizophr Res. 2003;63:121–129. doi: 10.1016/s0920-9964(02)00376-6. [DOI] [PubMed] [Google Scholar]
- 32.Penn DL, Meyer PS, Evans E, Wirth RJ, Cai K, Burchinal M. A randomized controlled trial of group cognitive-behavioral therapy vs. enhanced supportive therapy for auditory hallucinations. Schizophr Res. 2009;109:52–59. doi: 10.1016/j.schres.2008.12.009. [DOI] [PubMed] [Google Scholar]
- 33.Startup M, Jackson M, Bendix S. North Wales randomized controlled trial of cognitive behaviour therapy for acute schizophrenia spectrum disorders: outcomes at 6 and 12 months. Psychol Med. 2004;34:413–422. doi: 10.1017/s0033291703001211. [DOI] [PubMed] [Google Scholar]
- 34.Tarrier N, Beckett R, Harwood S, Baker A, Yusupoff L, Ugarteburu I. A controlled trial of two cognitive-behavioural methods of treating drug-resistant residual psychotic symptoms in schizophrenic patients: I. Outcome. Br J Psychiatry. 1993;162:524–532. doi: 10.1192/bjp.162.4.524. [DOI] [PubMed] [Google Scholar]
- 35.Wiersma D, Jenner J, Nienhuis F, van de Willige G. Hallucination focused integrative treatment improves quality of life in schizophrenia patients. Acta Psychiatr Scand. 2004;109:194–201. doi: 10.1046/j.0001-690x.2003.00237.x. [DOI] [PubMed] [Google Scholar]
- 36.Wykes T, Hayward P, Thomas N, et al. What are the effects of group cognitive behaviour therapy for voices? A randomised control trial. Schizophr Res. 2005;77:201–210. doi: 10.1016/j.schres.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 37.Meehl PE. Schizotaxia, schizotypy, schizophrenia. Am Psychol. 1962;17:827–838. [Google Scholar]
- 38.Katsanis J, Iacono WG, Beiser M, Lacey L. Clinical correlates of anhedonia and perceptual aberration in first-episode patients with schizophrenia and affective disorder. J Abnorm Psychol. 1992;101:184–191. doi: 10.1037//0021-843x.101.1.184. [DOI] [PubMed] [Google Scholar]
- 39.Beckfeld DF. Interpersonal competence among college men hypothesized to be at risk for schizophrenia. J Abnorm Psychol. 1985;94:397–404. doi: 10.1037//0021-843x.94.3.397. [DOI] [PubMed] [Google Scholar]
- 40.Kwapil TR, Miller MB, Zinser MC, Chapman J, Chapman LJ. Magical ideation and social anhedonia as predictors of psychosis proneness: A partial replication. J Abnorm Psychol. 1997;106:491–495. doi: 10.1037//0021-843x.106.3.491. [DOI] [PubMed] [Google Scholar]
- 41.McQuaid JR, Granholm E, McClure FS, et al. Development of an integrated cognitive behavioral and social skills training intervention for older patients with schizophrenia. J Psychother Pract Res. 2000;9:149–156. [PMC free article] [PubMed] [Google Scholar]
- 42.Granholm E, McQuaid JR, McClure FS, et al. Randomized controlled trial of cognitive behavioral social skills training for older people with schizophrenia: 12-month follow-up. J Clin Psychiatry. 2007;68:730–737. doi: 10.4088/jcp.v68n0510. [DOI] [PubMed] [Google Scholar]
- 43.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-P), Version 2. New York, NY: Biometrics Research, New York State Psychiatric Institute; 1994. [Google Scholar]
- 44.Psychiatric Rehabilitation Consultants Modules in the UCLA Social and Independent Living Skill Series. Camarillo: Psychiatric Rehabilitation Consultants; 1991. [Google Scholar]
- 45.Kingdon DG, Turkington D. Cognitive therapy of schizophrenia. New York, NY: The Guilford Press; 2005. [Google Scholar]
- 46.Beck AT, Rector NA, Stolar N, Grant P. Schizophrenia: Cognitive Theory, Research, and Therapy. New York, NY: The Guilford Press; 2009. [Google Scholar]
- 47.Wallace CJ, Liberman RP, Tauber R, Wallace J. The independent living skills survey: a comprehensive measure of the community functioning of severely and persistently mentally ill individuals. Schizophr Bull. 2000;26:631–658. doi: 10.1093/oxfordjournals.schbul.a033483. [DOI] [PubMed] [Google Scholar]
- 48.Eckblad ML, Chapman LJ, Chapman JP, Mishlove M. The Revised Social Anhedonia Scale. Unpublished Test. Madison, WI: University of Wisconsin; 1982. [Google Scholar]
- 49.Leak GK. An examination of the construct validity of the social anhedonia scale. J Pers Assess. 1991;56:84–95. doi: 10.1207/s15327752jpa5601_8. [DOI] [PubMed] [Google Scholar]
- 50.Blanchard JJ, Gangestad SW, Brown SA, Horan WP. Hedonic capacity and schizotypy revisited: a taxometric analysis of social anhedonia. J Abnorm Psychol. 2000;109:87–95. doi: 10.1037//0021-843x.109.1.87. [DOI] [PubMed] [Google Scholar]
- 51.Lewandowski KE, Barrantes-Vidal N, Nelson-Gray RO, Clancy C, Kepley HO, Kwapil TR. Anxiety and depression symptoms in psychometrically identified schizotypy. Schizophr Res. 2006;83:225–235. doi: 10.1016/j.schres.2005.11.024. [DOI] [PubMed] [Google Scholar]
- 52.Gould RA, Mueser KT, Bolton E, Mays V, Goff D. Cognitive therapy for psychosis in schizophrenia: an effect size analysis. Schizophr Res. 2001;48:335–342. doi: 10.1016/s0920-9964(00)00145-6. [DOI] [PubMed] [Google Scholar]
- 53.Rector NA, Beck AT. Cognitive behavioral therapy for schizophrenia: an empirical review. J Nerv Ment Dis. 2001;189:278–287. doi: 10.1097/00005053-200105000-00002. [DOI] [PubMed] [Google Scholar]
- 54.Penn DL, Mueser KT, Tarrier N, et al. Supportive therapy for schizophrenia: possible mechanisms and implications for adjunctive psychosocial treatments. Schizophr Bull. 2004;30:101–112. doi: 10.1093/oxfordjournals.schbul.a007055. [DOI] [PubMed] [Google Scholar]