Abstract
Accurate assessment of the individual risk for psychotic disorders has great value. We need to determine the reliability and rate of conversion to a psychotic disorder in clinical samples before we can recommend a risk syndrome diagnosis for general practice. The assessment of risk carries its own risks, including stigmatization and inappropriate treatment, potentially leading to adverse outcomes.
Keywords: psychosis, psychotic disorder, schizophrenia, risk syndrome, prodrome
Introduction
The burden of psychotic disorders is considerable. They are associated with significant disability, morbidity, and mortality, resulting in drastically reduced life expectancy.1 While these facts are sobering, there is hope that psychotic disorders can be prevented.2 Most psychotic disorders are now viewed as an evolving pathology of the human brain, shaped by genetic risk factors and environmental stressors. The long trajectory of brain maturation and the remarkable plasticity in response to injury have created reasonable hope that we can intervene and prevent mental illness. To achieve such an ambitious goal, we need reliable methods of early detection and accurate risk assessment.
How can we get there? First, we need to define the timeline of a psychotic disorder. This requires diagnostic criteria to separate a risk stage from the disorder. Second, we need to identify which risk factors can predict the subsequent emergence of a psychotic disorder. Finally, we need to assess risk factors reliably and in time for intervention and prevention.
The Timeline of a Psychotic Disorder
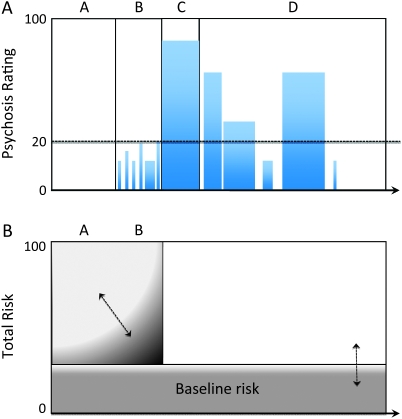
Let us assume that we have the ability to accurately record all signs and symptoms of psychosis throughout the life of an individual. We will define psychosis as (a) reality distortion (delusion and hallucination), (b) disorganized thought/language, and (c) markedly abnormal psychomotor behavior (such as stupor and mutism). We also have a dimensional rating scale that allows us to reliably assess the degree of psychosis. Each observation of psychosis can then be recorded in a graph, such as the one shown in figure 1A. On the y-axis we rate the degree of psychosis (on a scale from 0 to 100, with 20 being defined as the diagnostic threshold) and on the x-axis we map out the development of the illness. Then we can distinguish at least 4 stages.
A. The asymptomatic risk stage: Each person is at risk, even before the onset of symptoms. For example, the lifetime morbid risk for schizophrenia is 7.2 per 10001 and increases if first-degree relatives are affected or if certain environmental stressors are present.
B. The symptomatic risk stage: Most psychotic disorders emerge slowly, first with symptoms that are either mild or infrequent. Low-level psychosis can be diagnosed in a significant number of individuals and is often embedded into prevailing culture.3 The threshold separating low-level psychosis from the diagnosis of a psychotic disorder is arbitrary. In figure 1A, it is set at 20%, but it could be set at any point on the y-axis. For clinical purposes, however, the threshold needs to be reliable and meaningful for a person who seeks or needs treatment.
C. The first episode: The diagnosis of a psychotic disorder necessitates the crossing of a severity threshold. The criteria that define this threshold vary between psychotic disorders. For example, the diagnosis of schizophrenia requires the presence of more than one psychotic symptom, whereas delusional disorder is defined by the presence of nonbizarre delusions without other signs of psychosis.4 Clinical conditions with pervasive psychotic symptoms that do not reach the diagnostic threshold include schizophrenia spectrum disorders such as schizotypal personality disorder.5
D. Long-term course: The course of a psychotic disorder is highly variable. Short presentations of psychosis are captured in diagnoses such as brief psychotic disorder or schizophreniform disorder. The diagnostic criteria for either schizophrenia or schizoaffective disorder are fulfilled when psychotic symptoms remain above the diagnostic threshold for a significant period of time. For any given type of psychotic disorder, the long-term course varies considerably and may include remissions as well as relapses. The ultimate outcome of psychotic disorders is variable as well. Even a diagnosis of schizophrenia, the most severe psychotic disorder, does not determine fate because a significant number of affected individuals will have extended periods of remission or even full restitution to the premorbid level of functioning.
Fig. 1.
Timeline and Risk Assessment for a Psychotic Disorder. (A) The timeline of a psychotic disorder includes the asymptomatic risk stage (A), the symptomatic risk stage (B), the first episode (C), and the long-term course (D). The degree of psychosis is plotted, with a range from 0 to 100, on the y-axis, and a threshold of 20 is defined as the diagnostic cutoff value. For illustrative purposes, the x-axis is not drawn to scale (eg, the asymptomatic risk stage lasts much longer than the symptomatic risk stage). (B) The assessment of risk for a psychotic disorder includes baseline risk factors, distal risk factor during the asymptomatic risk stage, and proximal risk factors during the symptomatic risk stage. Examples for these risk factors are listed in table 1. The arrows indicate that baseline, distal, and proximal risk factors may vary over time for each individual, creating a unique total risk score.
With the luxury of continuous observation, the graph in figure 1A can be recorded online, as events happen. Alternatively, it can be constructed retrospectively, assuming total recall for all periods of life. Neither is realistic and we have to rely on the retrospective epidemiological study of cohorts diagnosed with psychotic disorders. Such studies have provided us with promising leads for a prospective assessment of risk for a psychotic disorder.
Risk Factors for Psychosis
The lifetime prevalence of psychotic disorders is 3%.6 Various genetic and environmental factors contribute to this baseline risk in the population and can accumulate, thereby significantly elevating the risk for a given individual. Table 1 lists some of the risk factors for psychosis and distinguishes (1) risks that may exert their effect at any time, ie, before or after the onset of the illness, (2) risks that occur early on in life, ie, during the asymptomatic risk stage, and (3) risks that develop in close proximity to the transition into disease, ie, during the symptomatic risk stage.
Baseline risk factors: The level of baseline risk is determined by a set of individual biological and environmental factors. Family history and gender are examples of baseline risk factors for psychotic disorders. The risk increases several folds if a person has a first-degree relative with a history of a psychotic disorder. For the monozygotic twin of a person with schizophrenia, the probability to develop schizophrenia is 50% (in figure 1B, this would raise the baseline risk to half maximum). The baseline risk factor might have a temporal profile (eg, the variable expression of risk genes throughout brain development) but is not a priori linked to one time point in the life of a person at risk. In addition, baseline risk factors remain relevant even after the first episode of a psychotic disorder because they might predict illness course, response to treatment, and ultimately the outcome of the illness.
Distal risk factors: Perturbations of normal brain development at various time points (eg, in utero, perinatally, or postnatally) are well-established risk factors for psychotic disorders. While the mechanism of these effects is not well understood, they do have implications for clinical practice. For example, the preventive measure of proper maternal nutrition limits the number of schizophrenia cases.7 Exposure to drugs, such as marijuana, is another example of a distal risk factor that increases the risk for schizophrenia.
Proximal risk factors: The emergence of subthreshold psychotic symptoms is a significant risk factor for a psychotic disorder.8 But not all individuals with subthreshold psychotic symptoms will ultimately be diagnosed with a psychotic disorder. In fact, quite a few go on to develop other psychiatric disorders or none at all. In addition to subthreshold psychotic symptoms, other psychopathological changes have also been linked to a psychotic disorder.9 Proximal risk factors can be (a) combined into a global risk factor and (b) operationalized in rating scales.
Table 1.
Risk Factors for Psychotic Disorders
| Time of Assessment | Risk Factor | Examples |
| At any time | Genes | DISC1 |
| Family history | 50% concordance for MZ twins | |
| Gender | Bimodal risk profile in females | |
| Culture | Immigrant status | |
| Living environment | Urbanicity | |
| Distal to illness onset | Abnormal fetal development | Maternal malnutrition |
| Abnormal cognitive development | Low IQ | |
| Early drug use | MJ before age 13 | |
| Proximal to illness onset | Mental status changes | Attenuated psychotic symptoms, basic symptoms |
| Biomarker | Decrease of cortical gray matter, elevated DA release |
Note: This list of risk factors is not exhaustive but is meant to illustrate 3 different types of risk factors. MZ, monozygotic; MJ, marijuana; DA, dopamine.
Emerging technologies such as structural and functional neuroimaging are being explored to delineate a temporal profile of brain changes during the symptomatic (or even asymptomatic) risk state. For example, subtle deficits in cortical volume10 and an abnormally elevated release of dopamine11 have been associated with the later emergence of a psychotic disorder.
Prodrome vs Risk Syndrome
The period of subthreshold psychosis before the first episode of a psychotic disorder is often referred to as the prodrome. The prodrome is, by definition, the nascent stage of a disorder (hence the term latent schizophrenia).
In contrast, a risk syndrome is not necessarily linked to a disorder. The value of a risk syndrome increases with the accuracy in predicting future outcomes (eg, metabolic syndrome leading to diabetes or cardiovascular disease; mild cognitive impairment leading to dementia), but the conversion to disease is, by definition, less than 100%.
In short, a prodrome is part and parcel of the disorder (see figure 1), a risk syndrome is not. A prodrome can be diagnosed only after the disorder has declared itself. In contrast, a risk syndrome can be diagnosed prospectively.
The Assessment of Risk
How can clinicians and researchers currently assess the risk for a psychotic disorder? First, they can review demographic and historical information to establish baseline and proximal risk factors. Examples include a detailed family history, genetic testing for mutations and risk alleles, and a thorough developmental history, starting with events in utero. Second, they can assess the cumulative risk of several factors. A striking example is the combination of early cannabis use and certain risk alleles, leading to a significantly increased risk for schizophrenia.12 Third, they can look for changes of sensation, thinking, affect, and volition as proximal risk factors. These mental status changes are typically minor variants of fully developed psychotic symptoms.
Several research groups have developed global risk factors, relying primarily on proximal clinical risk syndromes.13 For example, the Structured Interview for Prodromal Syndromes includes a family history questionnaire and rates 4 domains (positive, negative, disorganization, and general symptoms) of psychopathology with the 19-item Scale of Prodromal Symptoms.14 Others have focused on basic symptoms, defined as the earliest subjectively experienced symptoms of psychosis, including changes in volition and affect, peculiar changes of thinking, speech, and perception, and genuine psychotic symptoms.9
The Risk Syndrome for Psychotic Disorders
Is the current state of risk assessment for psychotic disorders mature enough to warrant inclusion in diagnostic systems such as the Diagnostic and Statistical Manual of Mental Disorders and International Classification of Diseases? What evidence do we want to see?
First, the assessment has to be feasible in clinical practice. For example, we cannot screen the general population and need to define a target population, such as help-seeking individuals. Second, the diagnosis has to be reliable, not only in the research setting but also in clinical practice. This will require education about the subtle differences between subthreshold and diagnostic psychotic symptoms. Third, the diagnosis has to be valid. For example, does the risk syndrome predict course and outcome, response to treatment, and biomarkers such as cortical volume or dopamine release? Fourth, the social, legal, and medical consequences of diagnosing a risk syndrome need to be evaluated. How do we protect individuals, who will not progress to a psychotic disorder, from bias and stigma? Will the diagnosis of a risk syndrome for psychotic disorders be sufficient for the Federal Drug Administration (FDA) to approve therapeutic interventions (similar to the attempts to gain FDA approval for conditions such as mild cognitive impairment and metabolic syndrome)? Finally, there are several ethical implications: What is the value of risk assessment without proper options for intervention? What to do when a person does not want to know the individual risk?
Risk assessment has the potential to lift the burden of psychotic disorders but we need to be careful not to make matters worse.
Acknowledgments
The author is a member of the DSM-V Work Group on Psychotic Disorders. The opinions expressed here do not necessarily reflect the consensus of the DSM-V Work Group or Task Force.
References
- 1.McGrath J, Saha S, Chant D, Welham J. Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiol Rev. 2008;30:67–76. doi: 10.1093/epirev/mxn001. [DOI] [PubMed] [Google Scholar]
- 2.Insel TR. Translating scientific opportunity into public health impact: a strategic plan for research on mental illness. Arch Gen Psychiatry. 2009;66:128–133. doi: 10.1001/archgenpsychiatry.2008.540. [DOI] [PubMed] [Google Scholar]
- 3.van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. 2009;39:179–195. doi: 10.1017/S0033291708003814. [DOI] [PubMed] [Google Scholar]
- 4.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed, Washington, DC: American Psychiatric Publishing; 2000. revised. [Google Scholar]
- 5.Siever LJ, Davis KL. The pathophysiology of schizophrenia disorders: perspectives from the spectrum. Am J Psychiatry. 2004;161:398–413. doi: 10.1176/appi.ajp.161.3.398. [DOI] [PubMed] [Google Scholar]
- 6.Perala J, Suvisaari J, Saarni SI, et al. Lifetime prevalence of psychotic and bipolar I disorders in a general population. Arch Gen Psychiatry. 2007;64:19–28. doi: 10.1001/archpsyc.64.1.19. [DOI] [PubMed] [Google Scholar]
- 7.Susser E, St Clair D, He L. Latent effects of prenatal malnutrition on adult health: the example of schizophrenia. Ann N Y Acad Sci. 2008;1136:185–192. doi: 10.1196/annals.1425.024. [DOI] [PubMed] [Google Scholar]
- 8.Woods SW, Addington J, Cadenhead KS, et al. Validity of the prodromal risk syndrome for first psychosis: findings from the North American Prodrome Longitudinal Study. Schizophr Bull. doi: 10.1093/schbul/sbp027. April 21, 2009; doi:10.1093/schbul/sbp027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schultze-Lutter F. Subjective symptoms of schizophrenia in research and the clinic: the basic symptom concept. Schizophr Bull. 2009;35:5–8. doi: 10.1093/schbul/sbn139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pantelis C, Velakoulis D, McGorry PD, et al. Neuroanatomical abnormalities before and after onset of psychosis: a cross-sectional and longitudinal MRI comparison. Lancet. 2003;361:281–288. doi: 10.1016/S0140-6736(03)12323-9. [DOI] [PubMed] [Google Scholar]
- 11.Howes OD, Montgomery AJ, Asselin MC, et al. Elevated striatal dopamine function linked to prodromal signs of schizophrenia. Arch Gen Psychiatry. 2009;66:13–20. doi: 10.1001/archgenpsychiatry.2008.514. [DOI] [PubMed] [Google Scholar]
- 12.Henquet C, Di Forti M, Morrison P, Kuepper R, Murray RM. Gene-environment interplay between cannabis and psychosis. Schizophr Bull. 2008;34:1111–1121. doi: 10.1093/schbul/sbn108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Olsen KA, Rosenbaum B. Prospective investigations of the prodromal state of schizophrenia: review of studies. Acta Psychiatr Scand. 2006;113:247–272. doi: 10.1111/j.1600-0447.2005.00697.x. [DOI] [PubMed] [Google Scholar]
- 14.Miller TJ, McGlashan TH, Rosen JL, et al. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr Bull. 2003;29:703–715. doi: 10.1093/oxfordjournals.schbul.a007040. [DOI] [PubMed] [Google Scholar]