Abstract
Cognitive behavior therapy (CBT) evolved from behavioral theory and developed to focus more on cognitive models that incorporated reappraisal of thinking errors and schema change strategies. This article will describe the key elements of CBT for schizophrenia and the current evidence of its efficacy and effectiveness. We conclude with a description of recent concepts that extend the theoretical basis of practice and expand the range of CBT strategies for use in schizophrenia. Mindfulness, meta-cognitive approaches, compassionate mind training, and method of levels are postulated as useful adjuncts for CBT with psychotic patients.
Keywords: cognitive behavior therapy, psychosis, schizophrenia, mindfulness, method of levels, meta-cognitive
Introduction
Cognitive behavior therapy (CBT) is an evidence-based talking therapy that attempts cognitive and behavioral change based on an individualized formulation of a client's personal history, problems, and world views. CBT as a treatment for schizophrenia can be understood within a wider framework of CBT as applied to a range of mental disorders such as anxiety, posttraumatic stress disorder (PTSD), and depression. The influences and fundamental building blocks upon which theory and practice are based are varied and far reaching, and in clinical practice, CBT sessions do not always look the same. As a result, CBT has been criticized as a set of techniques and tools. However, CBT is better understood in terms of a set of core principles that rely on a personalized conceptualization of an individual's problems to guide the application of techniques and strategies. CBT continues to evolve and develop through reciprocal relationships among theory, research, and practice.
Cognitive Behavior Therapy
Cognitive therapy for depression was first described in a clear manualized format by Aaron T. Beck in 1979.1 This manual that emphasized the need to focus on conscious thinking was a direct challenge to behaviorism and thus became termed the cognitive revolution or “second wave.” The theory developed by Beck built on behavioral principles in that it not only recognized how behavior was the result of learned contingencies between stimuli and events but also emphasized clear relationships between cognition, physiology, and emotion.
Beck based his early theory upon an assumption fundamental to psychoanalytical thinking, ie, that early life experiences and social environment can contribute to the development of adult emotional problems. He stressed the salience of early life experiences in forming beliefs or schemas about the self, other people, and the world. These beliefs were then thought to lead to certain cognitive distortions and negative styles of thinking. Beck2 postulated that through the examination of thought processes and by evaluating their accuracy, many negative emotional reactions due to inaccurate or distorted thinking could be reduced or extinguished.
The key elements of CBT as described by Beck included engaging the patient, collaboratively developing a problem list, and deciding on a clear goal for the therapy session. Once the goal had been decided on, a CBT technique would be used (eg, guided discovery and Socratic questioning [described below]) to identify distortions in thinking style. This would be followed by an agreed task (homework) for the patient to complete by themselves before the following appointment (eg, attempting to identify these distortions over the next week and trying to correct them). Regular feedback and asking the patient to provide a capsule summary (ie, personal understanding) of the session were also crucial elements. This therapy structure relied very much on collaborative working with the patient within an empirical methodology. A formulation (narrative of the person's history) was jointly generated to make sense of the emergence and maintenance of the problem at hand. This psychotherapy revolution placed the patient at the heart of the recovery process and introduced the concept of rational review of appraisal errors.
CBT Techniques
Beck used narrative formation or the development of a coherent personal story of one's experience as an explanatory framework to make hypotheses about the development, maintenance and links between different problems. There is evidence that developing such a narrative formation is a therapeutic process in itself and an essential aspect of recovery.3
Beck specified how thoughts and beliefs can be examined for their truth by questioning. He showed the usefulness of the “Socratic questioning” technique to encourage the probing of evidence, reason, and rationale. For example, a patient who believed that he was under surveillance was asked to give a rationale for his belief. The CBT therapist used questions to explore the individual's reasoning (eg, “How do you know that is happening?,” “Can you give me an example of that?,” “What do you think causes this to happen?,” “When you think it through now, are these reasons good enough?”).
Another technique commonly employed in CBT is “reality testing” where a patient will be encouraged to actively find evidence to test the reality base of a belief or assumption; a process which is done in collaboration with the therapist. For example, a person who believes in the existence of giant moths that will eat people might be encouraged to find some evidence-based information about moths and discover that these insects tend only to live for approximately 1–2 weeks and would be unable to bite a human as they have no teeth!
“Behavioral experiments” are another method frequently utilized in CBT whereby a “scientific experiment” can be set up to test a specific prediction. For example, a person who believes that his next door neighbor is communicating threats to him by coughing might set up an experiment in which he watches a television program to test alternative predictions that there are other reasons why people cough. The CBT therapist will facilitate the patient in developing awareness (guided discovery) of how people might cough due to smoking, allergy, or a chest infection. Once the patient can see that the people on the TV are possibly coughing for other reasons the patient can, then the local environment can begin to be explored, and the reality of the patient's ideas specifically about his or her neighbor's coughing can be explored.
Some might argue that behavioral experiments look no different to exposure or behavior modification, but they clearly illustrate the way in which the underlying theory of CBT has evolved from behavior to cognitive theory. Beck et al1 described how “For the behaviour therapist, the modification of behaviour is an end in itself; for the cognitive therapist it is a means to an end—namely cognitive change” (p119).
CBT for Schizophrenia
CBT for schizophrenia, as first described in a single case study by Beck in 1952,4 has subsequently been developed in the last 30 years from the traditional model of CBT for depression as described above.2,5 However, cognitive theory and interventions for anxiety, social phobia, PTSD, and obsessive-compulsive disorder (OCD) also find application within the practice of CBT for psychosis.
Earlier forms of CBT for schizophrenia relied primarily on behavioral strategies to affect change, with a secondary focus on the cognitive components. These earlier forms of CBT for schizophrenia focused on improving coping,6 building social and independent living skills, and increasing compliance using behavioral strategies such as linking tablet taking to another activity.7 Similarly, negative symptoms were targeted by providing graded activity programs.8 These approaches have continued to be applied where deficit symptoms of schizophrenia and improving functional outcomes are the main focus of intervention.9
For many years, it was assumed that the positive symptoms associated with schizophrenia lay outside of the realms of normal psychological functioning. Thus, the transition to incorporating more cognitive theory and techniques into practice came much later compared with CBT for nonpsychotic disorders.
Cognitive models outline how hallucinations and delusions can occur when anomalous experiences that are common to the majority of the population10 are misattributed in a way that has extreme and threatening personal meaning.11,12 These models specify the role of faulty beliefs, increased attention to threat-related stimuli, biased information processing of confirmatory evidence, and safety behaviors (ie, avoidance of specific situations) in the experience of positive symptoms. The emphasis is on distress resulting not necessarily from difficult experiences but the meaning placed on those very experiences. For example, an individual who experiences physical sensations of tingling and attributes this to job stress is likely to have a markedly different outcome to persons who believe that people at work are persecuting them and have planted microchips under their skin. Cognitive theory is based on the notion that the cognitive processes implicated in mood and anxiety disorders occur transdiagnostically.13 Research findings support the notion that psychotic symptoms can be conceptualized with reference to normal psychological processes, whereby the content of symptoms is understandable and amenable to CBT.14 For example, Chadwick et al15 built on the work of Beck in OCD to demonstrate that voices could be conceptualized as intrusive thoughts.
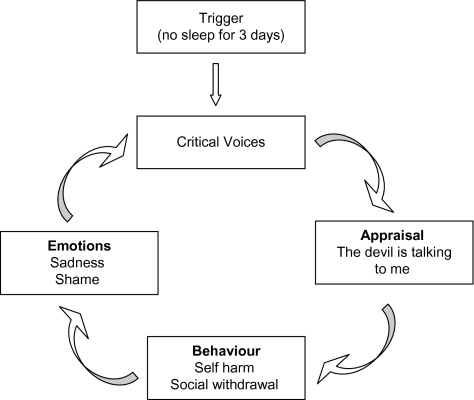
Kingdon and Turkington16 and Fowler et al17 described how CBT for disorders such as anxiety and depression could be applied in schizophrenia. There were some key amendments. Stigma was addressed by identifying the negative beliefs and assumptions people held about the diagnosis and prognosis of schizophrenia and then providing evidence that some of these experiences are actually fairly common in the general population (normalizing). In addition, the therapist provided alternative explanations, such as the role of stress, that provided more optimistic and hopeful perspectives.18 Compared with CBT for other disorders, the sessions were often shorter in length and much more flexible, and homework was simplified. The role of sleep disturbance, affect, and safety behaviors (eg, behaviors such as avoidance that maintained faulty beliefs) was identified to produce mini-formulations of positive symptom maintenance.19 Figure 1 presents an example demonstrating how critical hallucinations, triggered by sleep deprivation, are maintained by a negative appraisal, emotions of sadness and shame, and safety behaviors including social withdrawal.
Fig. 1.
Mini-formulation of Hallucination Maintenance.
Cognitive biases are directly addressed by CBT predominantly through focusing on the content of thoughts and styles of thinking. These include the jumping to conclusions error and biases in styles of judgment found in individuals with unusual beliefs (delusions) and the biases in attributional styles and attentional processing associated with hallucinations. In CBT, it is the individual's personal meaning, understanding, and coping with symptoms that are the focus of treatment. For example, individuals are facilitated in testing out the location of the hallucinations (internal vs external), carefully examining the appearance and behavior of suspected persecutors, and attempting homework that is pertinent to their stated goals.
The Evidence Base for CBT in Schizophrenia
There is now a considerable body of evidence that illustrates the efficacy of CBT for schizophrenia.20 Randomized controlled trials (RCTs) have shown moderate effect sizes for positive and negative symptoms at the end stages of therapy with sustained benefits over time.21 There is evidence that these research findings are also sustained in clinical settings22,23 and are cost effective.24 Virtually, all trials have been on patients with stabilized antipsychotic medication regimes; however, case series exist showing that there is a potential benefit of CBT being offered to patients who refuse medication treatment.25 Both hallucinations and delusions respond to CBT.26,27 Not only negative symptoms respond28 but also there is a durable effect at medium term follow-up.23 The cognitive models relating to these presentations have all been recently described in detail.29 Patients with substance misuse and other comorbidities are likely to be more difficult to engage and treat, but there are promising signs.30 CBT struggles more where people have difficulty identifying that they have mental health problems,31 delusional systems,32 or extreme primary negative symptoms.33 Similarly, when comorbidities accumulate, CBT effects are liable to be significantly less. Meta-analysis of Zimmermann et al34 found that acute presentations do better than chronic. However, people in acute episodes usually improve with standard nursing care or supportive counseling. CBT would seem to be of benefit in treating psychotic prodromes of mild/moderate severity and for those who are at ultrahigh risk of conversion or with severe symptomatology.35,36
On the basis of such consistent evidence over the last 10–15 years, in the UK and US, the National Institute for Clinical Excellence37 and The Schizophrenia Patient Outcomes Research Team38 guidelines, respectively, are recommending that CBT be offered routinely to individuals with residual symptoms of schizophrenia. More recently, further evidence is being provided that CBT is likely to be of particular benefit to individuals with recent onset of schizophrenia.37
Despite a clear message that CBT for psychotic symptoms appears to be beneficial, questions remain. The extent to which CBT is limited to effecting change only within the peripheral features (consequences) of the disorder, such as distress and behavioral reactions that contribute symptom maintenance or target more central mechanisms and processes hypothesized to underlie the specific symptoms of schizophrenia, is unclear. It is not clear whom CBT works for and when, raising further questions as to how therapeutic change occurs. Overall, what does the impact of CBT inform us about the nature of schizophrenia itself? These questions may partially be answered by pre- and post-CBT functional neuroimaging studies that are currently under way.
CBT and Functional Outcome
The cognitive model predicts improved functioning, and empirical studies support the efficacy of CBT in this regard. CBT can improve functioning even when symptoms do not improve, which is one reason it is consistent with recovery and an important adjunct to antipsychotic medication. CBT can be seen to be complementary to dopaminergic blockade that reduces the salience of environmental cues.39 Lieberman et al40 argued that atypical antipsychotic medication improved neurogenesis, and this would also complement a psychotherapy targeted on the acquisition of new skills.
Developments in CBT for Schizophrenia
Ongoing research and practice of CBT have led to emerging evidence of other important factors in schizophrenia, in addition to thought content and thinking styles. These include the role of arousal,41 emotion,42 attachment and interpersonal issues,43,44 loss and trauma,45 self-esteem,46 and acceptance and self-to-self relating.47 These processes may potentially have a causal role in the development of the disorder and may contribute to the symptoms experienced in schizophrenia, the way in which these are expressed and the subsequent course of the disorder. The importance of these factors has been demonstrated in recovery approaches to psychosis, where there has been marked value in helping individuals to develop personal meaning and empowerment from their own psychotic experiences, acquire a sense of inner control and self-regulation, and enable emotional and cognitive change facilitating the attainment of goals and recovery.48 Appreciation of the heterogeneity and complexity of processes operating in schizophrenia beg a broader approach to treatment that incorporates evolving cognitive theory and practice.
Cognitive schema theory underlying CBT has thus evolved over the years, changing the way in which mental disorders are understood. This occurred in part due to criticisms of earlier theory underlying CBT having been developed on the basis of clinical caveats with no scientifically tested model of concepts such as “schemas.” This caused difficulties in relating clinical findings to the work of cognitive scientists who had developed theories of how the mind worked that were based on experimental observations and data. A common problem in CBT was in accounting for the gap that commonly occurs between logical reasoning and strong emotion (eg, persons can “know” rationally that they are not being followed by the mafia, but simultaneously they still “feel” that they are being followed and continue to be distressed). Cognitive science has developed our understanding of how people develop beliefs and emotions on the basis of 2 types of “knowledge.” Propositional knowledge is a kind of “rational knowledge”—based on referentially specific information (eg, facts and figures). The other is implicational knowledge that is the more abstract “knowing with the heart”—based on integrated information drawn through the senses (eg, sight, smell, taste, etc) that is involved in creating more elaborate schematic models of the self.49
Thus, there has been a shifting away from linear formulations of how irrational thoughts directly lead to maladaptive behaviors and negative emotions to an increased understanding of the complex interacting and self-regulating relationships between thoughts, behavior, feelings, and physical sensations.49 Practical application of theory within cognitive behavioral therapies has advocated a shift from predominantly challenging the content of negative thoughts and schemas to instead altering a person's relationship to both thoughts and feelings. In this sense, it is not necessarily the thought that is problematic but the way in which an individual thinks about their thoughts! For example, someone who responds to distressing intrusive thoughts by worrying and trying to suppress the intrusions increases his anxiety and attentional focus on these unwanted experiences. He is likely to suffer an exacerbation of the intrusions and greater distress and emotional disorder compared with someone who does not ruminate and distracts himself by listening to music.
There is a growing trend in CBT to focus less on changing faulty thinking and employ additional therapeutic methods to emphasize working with different components of schema, interpersonal relationships, emotional regulation, information processing (ie, attentional biases), and ways of relating to the self. Control is highlighted as having central importance within mental disorder. Interpersonal control can be regarded a developmental factor, loss of control is a consequence, and mental control is an important maintenance process. Control in other forms is also evident, such as the reduced interpersonal control often reported during therapy (collaborative or client-centered styles of therapy) and control of one's life as a goal or outcome for most people.50 This evolution in thinking and practice has lead to what has been increasingly referred to as the “third wave” after Hayes used it to describe acceptance and commitment therapy (ACT), a mindfulness-based therapy.51
The last 5–10 years has witnessed a general burgeoning of therapeutic approaches that push beyond original cognitive theory and extend to include an eclectic combination of theories and philosophical influences. Examples of third-wave approaches include mindfulness, meta-cognitive therapy (MCT), compassionate mind training (CMT), and the method of levels (MOL). The extent to which these approaches can be considered third wave is debatable as this suggests something “new” to CBT. These more recent CBTs have made some theoretical departures from traditional cognitive and behavioral theory, but the practical application of these approaches echoes the field. These more recent approaches are still in their infancy but have potential to influence the application of CBT for schizophrenia. Each approach will be described briefly.
Mindfulness-Based Approaches
Mindfulness approaches (ie, mindfulness-based stress reduction52 and mindfulness-based cognitive therapy [MBCT])53,54 have been used for a range of disorders and have a good developing evidence base.55 All involve training of the mind to disengage from unhelpful and automated patterns of thinking (“meta-cognition” is the term used to describe thinking about one's thinking). Each mindfulness-based approach is somewhat distinct with its own individual theoretical orientation and techniques. The commonality is an element of contemplation—the directing of attention or concentration, influenced by Eastern traditions of meditation such as Buddhism. Approaches might also involve the teaching of behaviors of kindness, compassion and generosity, the advocacy of empathic strategies (ie, being nonjudgmental and giving and resonating with another's suffering), and cognitive strategies of developing a mind set—a sense of self-betterment and personal transformation through openness or receptiveness. Instead of becoming preoccupied with difficult experiences (eg, hallucinations, unwanted memories, or thoughts), individuals are encouraged to focus attention on their experiences in order to develop different ways of relating to these thoughts and feelings, no matter how unpleasant they are. Attention to meta-cognitive processes is not new to traditional CBT where strategies for identifying cognitive errors and maladaptive thinking styles are frequently used. However, mindfulness differs in the way it places significantly greater emphasis on different aspects of meta-cognitive components of therapy. For example, persons who experience distressing critical voices might in traditional CBT be encouraged to utilize distraction techniques or reappraise their related thoughts. In mindfulness-based approaches, the person would be encouraged to engage with the voice with an emphasis on altering the emotional experiences associated with its presence. A case example is of a man who suffered from distressing command hallucinations for more than 20 years. Whenever the voices started up, he would respond with anger, pacing the room and shouting back at them. A mindful approach taught him that his unsuccessful attempts to avoid the experience led to him interpreting the voices as taunting him purposefully, which he would ruminate about and experience anger. He trained in accepting the presence of the voices and shifting his attention to them while adopting a nonjudgemental and indifferent attitude, leading to the voices being less distressing and less intrusive.
Chadwick and colleagues have applied MBCT to working with people with psychotic symptoms with evidence that this is a feasible intervention that can be useful and beneficial for some people.56,57 They have also been using mindfulness-based CBT in group format.58
Acceptance and Commitment Therapy
Theory behind ACT59 draws on relational frame theory, behavior analysis, and influences from mindfulness. ACT does not encourage people to control intrapersonal activities (thoughts, feelings, etc) as in traditional CBT but teaches them to “just notice,” accept, and encompass internal events. It emphasizes identifying an individual's personal values and encouraging them to act on these. In the process of facilitating people to discover personal meaning and value within their life, ACT strives to increase psychological flexibility. Pankey and Hayes60 provided a thorough overview of how ACT can be applied to working with people with psychosis. They advocated helping people to use strategies to cope with psychotic experiences, such as cognitive distancing (getting people to treat their beliefs as hypothetical statements as opposed to facts), acceptance, and valued action. They argue that the focus in traditional CBT on reducing specific symptoms might paradoxically make them worse. They emphasized instead intervening on a person's willingness to have symptoms and reduce attempts to act on them. Pankey and Hayes60 also stated that the approach can be helpful with people who might have limited cognitive ability. ACT has been used with a wide range of populations and disorders although evidence of its efficacy on the basis of high-quality clinical trials with adequate scope and follow-up are limited. Hayes et al61 provided an overview of the literature summarizing that ACT is so far proving to be applicable and acceptable across a broad range of problems of varying severity, effect sizes appearing greater for more severe problems. For psychosis, Bach and Hayes62 demonstrated that ACT significantly reduced hallucinations and hospitalization days. These findings were replicated by Gaudiano and Herbert.63 Application of mindfulness-based techniques, such as ACT, is more commonly being augmented into CBT as a treatment for psychosis.64
Compassionate Mind Training
CMT is an approach to be delivered within traditional CBT but with an additional emphasis on increasing awareness of negative self-to-self relating. It draws its theoretical links from evolutionary social ranking theory.65 CMT specifically targets shame and self-criticism from the point of view that this can act as an internal hostile signal stimulating submissive and negative affective responses that can maintain psychiatric disorders.47,66 The key principles of CMT are to facilitate individuals caring for their own well-being, becoming sensitive to and accepting of their own needs and distress, and to respond toward themselves with warmth and compassion.67 Techniques are used such as “2-chair technique” where the “inner bully” is interviewed, giving a “voice” to a person's critical self-talk and facilitating a functional analysis of self-attacking. Many traditional CBT techniques such as Socratic questioning are also employed with the aim of reframing self-criticism changing the tone of the associated emotional experience and developing more compassionate beliefs and sensitivity to the self. Working with the patient's mental imagery (eg, altering the mental image of the inner bully) is also employed as a significant therapeutic aid in CMT.68These strategies are particularly important when working with psychotic symptoms. Self-criticism and negative self-to-self relating have been demonstrated to be particularly relevant, especially in instances where comorbid anxiety and affective disorder are present.69–71 Self-attacking is a psychological vulnerability factor increasing potential for relapse.71,72 Voices are believed to operate like external social relationships and might often resemble an individual's social sense of being powerless and controlled by others.43,73
There is a clear theoretical basis for using CMT within CBT for psychotic symptoms and thus a promising outlook for its inclusion as a therapeutic strategy for symptoms common in schizophrenia.44,74 Research establishing further the application of CMT in psychosis is underway.
Meta-cognitive therapy
MCT75 is theoretically based on the Self-regulatory Executive Function model.76 From this perspective, disorder is considered to occur as a result of thinking style and the way in which people control their thoughts (meta-cognition). MCT specifies that it is verbal styles of thinking (worry and rumination), the focus of attention on threat and negative information, and meta-cognitive actions of thought suppression and avoidance that lead to disorder. It is by targeting these meta-cognitive processes in treatment that MCT aims to change the way in which people experience and regulate their thoughts. In this sense, MCT is a departure from traditional CBT insofar as it focuses exclusively on the cognitive with no emphasis on behavioral features of treatment. MCT involves teaching people alternative skills to experience their thoughts utilizing techniques such as attention training and altering meta-cognitive beliefs that worrying is necessary or those thoughts cannot be controlled or are dangerous. There have been several studies evaluating the effectiveness of MCT providing emerging evidence of positive effects of MCT for people with generalized anxiety disorder, PTSD, OCD, and depression with stable effects at follow-up.77,78 Further studies are required with follow-up of more than 12 months and with larger comparative RCTs. Valmaggia et al79 recently applied an 8-session course of attentional training treatment in a single case to treat auditory hallucinations in the context of a diagnosis of schizophrenia, resulting in symptom reduction and increased perceived control and mastery of the hallucinations. This example demonstrated how someone who was distressed by repeated abusive hallucinatory voices experienced being very much at their beck and call. He felt that he had no control over them and was unable to function in social settings due to their presence. He was trained over 6 weeks to practice daily focusing his attention on different types of auditory stimuli. His ability to focus on the radio, clock, and traffic steadily improved. When he began to use this new skill he found that he had much more control over the voices and began to engage more in social activity. MCT is a promising development with the potential for application to schizophrenia.
The Method of Levels
MOL is a therapy based on the principles of perceptual control theory (PCT),80,81 which provides an account of the mechanisms of change within psychotherapy.82–84 It is a significant theoretical departure from CBT. PCT specifies that people do not seek to control their behavior but their perceptual experiences, where the goal is to make what is perceived from the environment match with “internal standards” (or goals).85 Internal standards (conceptualized as being somewhat analogous to schemas in CBT) are organized in hierarchical control systems with higher goals (standards) at the top (eg, “to be close to people”) that set a series of lower goals at the levels below (eg, “spend time with others”). Emotional difficulties and unwanted perceptual experiences (eg, paranoid beliefs) arise as people often have multiple goals that are prone to conflict with one another—eg, “to be close to other people versus to stay safe by avoiding being to close to others.”86,87
PCT postulates that the essential feature of successful change within CBT (or any other psychotherapy) is the shifting of a person's awareness to higher perceptual levels (goals) so that conflict in control systems can be reorganized.88 In this sense, MOL does not claim to be a new therapy but capitalizes on what it considers to be the effective ingredient of therapy—the mobility of “mental (meta-cognitive) awareness.”81,89
During a session of MOL, the patients choose to talk about any problem they wanted to discuss. The therapist observes shifts in their awareness, (identified through disruptions to the flow of conversation such as changes in gesture, tone of voice, or dialogue flow) and directs the patient's attention to these by asking them about associated background thoughts, images, or other perceptual experiences. This helps them to become aware of the higher goals and standards leading to their problems so that conflict can be reorganized. The redirecting of awareness is similar to the traditional CBT strategies such as Socratic questioning. However, in MOL, other traditional structures of CBT (formulations, advice, homework tasks, formal assessments, etc) are seen to be less relevant and potentially intrusive to meta-cognitive processing81 and the linking of cognition, affect, and emotion in an “online” experiential way.
Outcome studies for MOL indicate that it is an effective and acceptable psychotherapy with benefits at end of therapy and in short-term follow-up studies.88,90,91 These studies have been based only in community clinics, and larger controlled trials are required. However, Carey et al88 advocate that this approach appears to be especially useful for people with unusual perceptual experiences and complex problems—particularly when engagement is difficult, people feel “stuck” and are unclear about their problems—and for people who might have difficulty with remembering past events. MOL can be considered an MCT that can be delivered in pure form or within traditional CBT.92 This makes it ideal for application within schizophrenia, and preliminary case studies have demonstrated its utility when delivered within the traditional CBT format.93 Research specifically applying MOL to working with psychotic symptoms is underway.
Conclusion
Cognitive models have much to offer in aiding our understanding of the maintenance of the core symptoms of schizophrenia. Cognitive behavioral therapies based on these models have been demonstrated to be effective and valuable treatments for a range of positive and negative symptoms. However, theoretical developments and advances in cognitive treatments of disorders such as anxiety and depression have also helped to reveal a more complex picture of the transdiagnostic processes operating in schizophrenia. It is becoming clear that it is necessary to develop a broader conceptualization and treatment approach to psychotic symptoms that encompasses the heterogeneity and multifaceted nature of the disorder. Recent developments in cognitive treatments branded as third-wave approaches illustrate the advantage of not only targeting the content of thoughts and beliefs but also developing alternative methods of changing the way in which people relate to their thoughts and feelings. Collectively, they present a positive and encouraging developing evidence base with promising results. Evidence of the applicability of such approaches to schizophrenia is apparent, and further research is required to examine the wider feasibility and potential as a treatment for psychosis. These developments should be regarded as evolving cognitive therapies as opposed to a new wave. It is important to view CBT as a range of therapies and increase our understanding of how they might be applied to specific problems and circumstances, where efficacy is best understood through multifaceted and individualized formulations of patients.
References
- 1.Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Therapy of Depression. New York, NY: Guilford Press; 1979. [Google Scholar]
- 2.Beck AT. Cognitive Therapy and the Emotional Disorders. New York, NY: International Universities Press; 1976. [Google Scholar]
- 3.Roe D, Davidson L. Self and narrative in schizophrenia: time to author a new story. Med Humanit. 2005;31:89–94. doi: 10.1136/jmh.2005.000214. [DOI] [PubMed] [Google Scholar]
- 4.Beck AT. Successful outpatient psychotherapy of a chronic schizophrenic with a delusion based on borrowed guilt. Psychiatry. 1952;42:312–319. doi: 10.1080/00332747.1952.11022883. [DOI] [PubMed] [Google Scholar]
- 5.Beck AT. Depression: Clinical, Experimental and Theoretical Aspects. New York, NY: Harper and Row; 1967. [Google Scholar]
- 6.Tarrier N. Psychological treatment of schizophrenic symptoms. In: Kavanagh D, editor. Schizophrenia: An Overview and Practical Handbook. London, UK: Chapman & Hall; 1992. [Google Scholar]
- 7.Weiden EJ, Mott T, Curcio N. Recognition and management of neuroleptic noncompliance. In: Shriqui CL, Nasrallah HA, editors. Contemporary Issues in the Treatment of Schizophrenia. Washington, DC: American Psychiatric Press; 1995. pp. 411–434. [Google Scholar]
- 8.Meichenbaum D, Cameron R. Training schizophrenics to talk to themselves: a means of developing attentional controls. Behav Ther. 1973;4:515–534. [Google Scholar]
- 9.Hogarty GE, Anderson CM, Reiss DJ, et al. Family psychoeducation, social skills and training, and maintenance chemotherapy in the aftercare treatment of schizophrenia: II. Two-year effects of a controlled study on relapse and adjustment. Arch Gen Psychiatry. 1991;48:340–347. doi: 10.1001/archpsyc.1991.01810280056008. [DOI] [PubMed] [Google Scholar]
- 10.Johns LC, van Os J. The continuity of psychotic experiences in the general population. Clin Psychol Rev. 2001;21:1125–1141. doi: 10.1016/s0272-7358(01)00103-9. [DOI] [PubMed] [Google Scholar]
- 11.Morrison AP. The interpretation of intrusions in psychosis: an integrative cognitive approach to hallucinations and delusions. Behav Cogn Psychother. 2001;29:257–276. [Google Scholar]
- 12.Garety PA, Kuipers E, Fowler D, Freeman D, Bebbington PE. A cognitive model of positive symptoms of psychosis. Psychol Med. 2001;31:189–195. doi: 10.1017/s0033291701003312. [DOI] [PubMed] [Google Scholar]
- 13.Harvey A, Watkins ER, Mansell W, Shafran R. Cognitive Behavioural Processes Across Psychological Disorders: A Transdiagnostic Approach to Research and Treatment. Oxford, UK: Oxford University Press; 2004. [Google Scholar]
- 14.Yusupoff L, Tarrier N. Coping strategy enhancement for persistent hallucinations and delusions. In: Haddock G, Slade PD, editors. Cognitive-Behavioural Interventions With Psychotic Disorders. London, UK: Routledge; 1996. pp. 71–85. [Google Scholar]
- 15.Chadwick PD, Birchwood MJ, Trower P. Cognitive Therapy for Delusions, Voices and Paranoia. Chichester, UK: Wiley; 1996. [Google Scholar]
- 16.Kingdon DG, Turkington D. Cognitive-Behavioural Therapy of Schizophrenia. Hove, UK: Lawrence Erlbaum; 1994. [DOI] [PubMed] [Google Scholar]
- 17.Fowler D, Garety P, Kuipers E. Cognitive-Behaviour Therapy for psychosis: Theory and Practice. Chichester, UK: Wiley; 1995. [Google Scholar]
- 18.Harrison G, Hopper K, Craig T, et al. Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry. 2001;178:506–517. doi: 10.1192/bjp.178.6.506. [DOI] [PubMed] [Google Scholar]
- 19.Morrison AP. Cognitive behaviour therapy for psychotic symptoms of schizophrenia. In: Tarrier N, Wells A, Haddock G, editors. Treating Complex Cases: The Cognitive Behavioural Therapy Approach. London, UK: Wiley; 1998. pp. 195–216. [Google Scholar]
- 20.Wykes T, Steel C, Everitt B, Tarrier N. Cognitive behavior therapy for schizophrenia: effect sizes, clinical models, and methodological rigor. Schizophr Bull. 2008;34:523–537. doi: 10.1093/schbul/sbm114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gould RA, Meuser KT, Bolton E, Mays V, Goff D. Cognitive therapy for psychosis in schizophrenia: an effect size analysis. Schizophr Res. 2001;48:335–342. doi: 10.1016/s0920-9964(00)00145-6. [DOI] [PubMed] [Google Scholar]
- 22.Turkington D, Kingdon D, Turner T. Effectiveness of a brief cognitive-behavioural therapy intervention in the treatment of schizophrenia. Br J Psychiatry. 2002;180:523–527. doi: 10.1192/bjp.180.6.523. [DOI] [PubMed] [Google Scholar]
- 23.Turkington D, Kingdon D, Rathod S, Hammond K, Pelton J, Mehta R. Outcomes of an effectiveness trial of cognitive-behavioural intervention by mental health nurses in schizophrenia. Br J Psychiatry. 2006;189:36–40. doi: 10.1192/bjp.bp.105.010884. [DOI] [PubMed] [Google Scholar]
- 24.Malik N, Kingdon D, Pelton J, Mehta R, Turkington D. Effectiveness of brief cognitive-behavioral therapy for schizophrenia delivered by mental health nurses: relapse and recovery at 24 months. J Clin Psychiatry. 2009;70:201–207. doi: 10.4088/jcp.07m03990. [DOI] [PubMed] [Google Scholar]
- 25.Christodoulides T, Dudley R, Brown S, Turkington D, Beck AT. Cognitive behaviour therapy in patients with schizophrenia who are not prescribed antipsychotic medication: a case series. Psychol Psychother. 2008;81:199–207. doi: 10.1348/147608308X278295. [DOI] [PubMed] [Google Scholar]
- 26.Sensky T, Turkington D, Kingdon D, et al. A randomized controlled trial of cognitive-behaviour therapy for persistent symptoms in schizophrenia resistant to medication. Arch Gen Psychiatry. 2000;57:165–172. doi: 10.1001/archpsyc.57.2.165. [DOI] [PubMed] [Google Scholar]
- 27.Tarrier N, Yusupoff L, Kinney C, et al. A randomised controlled trial of intensive cognitive behaviour therapy for chronic schizophrenia. Br Med J. 1998;317:303–307. doi: 10.1136/bmj.317.7154.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rector NA, Seeman MV, Segal ZV. Cognitive therapy for schizophrenia: a preliminary randomized controlled trial. Schizophr Res. 2003;63:1–11. doi: 10.1016/s0920-9964(02)00308-0. [DOI] [PubMed] [Google Scholar]
- 29.Beck AT, Rector NA, Stolar NM, Grant PM. Schizophrenia: Cognitive Theory, Research, and Therapy. New York, NY: Guilford Press; 2009. [Google Scholar]
- 30.Barrowclough C, Haddock G, Beardmore R, et al. Evaluating integrated MI and CBT for people with psychosis and substance misuse: recruitment, retention and sample characteristics of the MIDAS trial. Addict Behav. In press doi: 10.1016/j.addbeh.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 31.Naeem F, Kingdon D, Turkington D. Predictors of Response to Cognitive Behaviour Therapy in the Treatment of Schizophrenia: A Comparison of Brief and Standard Interventions. Cognitive Therapy and Research. 2008;32(5):651–656. [Google Scholar]
- 32.Garety P, Fowler D, Kuipers E, et al. London-East Anglia randomized controlled trial of cognitive behavioural therapy for psychosis II: predictors of outcome. Br J Psychiatry. 1997;171:420–426. doi: 10.1192/bjp.171.5.420. [DOI] [PubMed] [Google Scholar]
- 33.Garety PA, Fowler D, Kuipers E. Cognitive-behavioral therapy for medication-resistant symptoms. Schizophr Bull. 2000;26:73–86. doi: 10.1093/oxfordjournals.schbul.a033447. [DOI] [PubMed] [Google Scholar]
- 34.Zimmermann G, Favrod J, Trieu VH, Pomini V. The effects of cognitive behavioral treatment on the positive symptoms of schizophrenia spectrum disorders: a meta-analysis. Schizophr Res. 2005;77:1–9. doi: 10.1016/j.schres.2005.02.018. [DOI] [PubMed] [Google Scholar]
- 35.McGorry PD, Phillips LJ, Yung AR, et al. A randomized controlled trial of interventions in the pre-psychotic phase of psychotic disorders. Schizophr Res. 2000;41:9. [Google Scholar]
- 36.Morrison AP, French P, Walford L, et al. A randomized controlled trial of cognitive therapy for the prevention of psychosis in people at ultra-high risk. Br J Psychiatry. 2004;185:281–287. doi: 10.1192/bjp.185.4.291. [DOI] [PubMed] [Google Scholar]
- 37. National Institute of Clinical Excellence. Schizophrenia: Core interventions in the treatment of schizophrenia in primary and secondary care. London: Department of Health; 2002. [Google Scholar]
- 38.Lehman AF, Kreyenbuhl J, Buchanan RW, et al. The Schizophrenia Patient Outcomes Research Team (PORT): updated treatment recommendations 2003. Schizophr Bull. 2004;30:193–217. doi: 10.1093/oxfordjournals.schbul.a007071. [DOI] [PubMed] [Google Scholar]
- 39.Howes OD, Kapur S. The dopamine hypothesis of schizophrenia: version III–the final common pathway. Schizophr Bull. 2009;35:549–562. doi: 10.1093/schbul/sbp006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lieberman JA, Tollefson GD, Charles C, et al. Antipsychotic drug effects on brain morphology in first-episode psychosis. Arch Gen Psychiatry. 2005;62:361–370. doi: 10.1001/archpsyc.62.4.361. [DOI] [PubMed] [Google Scholar]
- 41.Morrison AP, Wells A. Metacognition across disorders: a comparison of patients with hallucinations, delusions, and panic disorder with non-patients. Behav Res Ther. 2003;41:251–256. doi: 10.1016/s0005-7967(02)00095-5. [DOI] [PubMed] [Google Scholar]
- 42.Freeman D, Garety PA. Connecting neurosis to psychosis: the direct influence of emotion on delusions and hallucinations. Behav Res Ther. 2005;41:923–947. doi: 10.1016/s0005-7967(02)00104-3. [DOI] [PubMed] [Google Scholar]
- 43.Birchwood M, Meaden A, Trower P, Gilbert P, Plaistow J. The power and omnipotence of voices: subordination and entrapment by voices and significant others. Psychol Med. 2000;30:337–344. doi: 10.1017/s0033291799001828. [DOI] [PubMed] [Google Scholar]
- 44.MacBeth A, Schwannauer M, Gumley A. The association between attachment style, social mentalities, and paranoid ideation: an analogue study. Psychol Psychother. 2008;81:79–94. doi: 10.1348/147608307X246156. [DOI] [PubMed] [Google Scholar]
- 45.Read J, Perry BD, Moskowitz A, Connolly J. The contribution of early traumatic events to schizophrenia in some patients: a traumagenic neurodevelopmental model. Psychiatry. 2001;64:319–345. doi: 10.1521/psyc.64.4.319.18602. [DOI] [PubMed] [Google Scholar]
- 46.Barrowclough C, Tarrier N, Humphreys L, Ward J, Gregg L, Andrews B. Self-esteem in schizophrenia: the relationship between self-evaluation, family attitudes and symptomatology. J Abnorm Psychol. 2003;112:92–99. [PubMed] [Google Scholar]
- 47.Gilbert P, Birchwood M, Gilbert J, et al. An exploration of evolved mental mechanisms for dominant and subordinate behaviour in relation to auditory hallucinations in schizophrenia and critical thoughts in depression. Psychol Med. 2001;31:1117–1127. doi: 10.1017/s0033291701004093. [DOI] [PubMed] [Google Scholar]
- 48.Gumley A, White CA, Power K. An interacting cognitive subsystems model of relapse and the course of psychosis. Clin Psychol Psychother. 1999;6:261–278. [Google Scholar]
- 49.Teasdale JD. Emotion and two kinds of meaning: cognitive therapy and applied cognitive science. Behav Res Ther. 1993;31:339–354. doi: 10.1016/0005-7967(93)90092-9. [DOI] [PubMed] [Google Scholar]
- 50.Mansell W, Carey TA. A century of psychology and psychotherapy. Is an understanding of ‘control’ the missing link between theory, research and practice? Psychol Psychother. In press doi: 10.1348/147608309X432526. [DOI] [PubMed] [Google Scholar]
- 51.Hayes SC. Acceptance and commitment, relational frame theory, and the third wave of behavior therapy. Behav Ther. 2004;35:639–665. doi: 10.1016/j.beth.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 52.Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress. New York, NY: Delacorte; 1990. [Google Scholar]
- 53.Teasdale JD, Segal ZV, Williams JMG, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J Consult Clin Psychol. 2000;68:615–623. doi: 10.1037//0022-006x.68.4.615. [DOI] [PubMed] [Google Scholar]
- 54.Segal ZV, Williams JMG, Teasdale JD. Mindfulness-Based Cognitive Therapy for Depression. London, UK: Guilford; 2002. [Google Scholar]
- 55.Allen NB, Chamber R, Knight W. Mindfulness-based psychotherapies: a review of conceptual foundations, empirical evidence and practical considerations. Aust N Z J Psychiatry. 2006;40:285–294. doi: 10.1080/j.1440-1614.2006.01794.x. [DOI] [PubMed] [Google Scholar]
- 56.Chadwick P. Person Based Cognitive Therapy for Distressing Psychosis. Chichester, UK: John Wiley & Sons; 2006. [Google Scholar]
- 57.Abba N, Chadwick P, Stevenson C. Responding mindfully to distressing psychosis: a grounded theory analysis. Psychother Res. 2008;18:77–87. doi: 10.1080/10503300701367992. [DOI] [PubMed] [Google Scholar]
- 58.Chadwick P, Newman Taylor K, Abba N. Mindfulness groups for people with psychosis. Behav Cogn Psychother. 2005;33:351–359. [Google Scholar]
- 59.Hayes SC. A contextual approach to behavior change. In: Jacobson N, editor. Psychotherapists in Clinical Practice: Cognitive and Behavioral Perspectives. New York, NY: Guildford; 1987. pp. 327–387. [Google Scholar]
- 60.Pankey J, Hayes SC. Acceptance and commitment therapy for psychosis. Int J Psychol and Psycholog Ther. 2003;3:311–328. [Google Scholar]
- 61.Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther. 2006;44:1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 62.Bach P, Hayes SC. The use of acceptance and commitment therapy to prevent the rehospitalization of psychotic patients: a randomized controlled trial. J Consult Clin Psychol. 2002;70:1129–1139. doi: 10.1037//0022-006x.70.5.1129. [DOI] [PubMed] [Google Scholar]
- 63.Gaudiano BA, Herbert JD. Acute treatment of inpatients with psychotic symptoms using acceptance and commitment therapy: pilot results. Behav Res Ther. 2006;44:415–437. doi: 10.1016/j.brat.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 64.Gaudiano BA. Cognitive behavior therapies for psychotic disorders: current empirical status and future directions. Clin Psychol. 2005;12:33–50. [Google Scholar]
- 65.Gilbert P. Depression: The Evolution of Powerlessness. Hove, UK: Erlbaum; 1992. [Google Scholar]
- 66.Gilbert P. Compassion. London, UK: Routledge; 2005. [Google Scholar]
- 67.Gilbert P. Compassionate Mind. London, UK: Constable & Robinson, Ltd; 2009. [Google Scholar]
- 68.Gilbert P, Proctor S. Compassionate mind training for people with high shame and self criticism: overview and pilot study of a group therapy approach. Clin Psychol Psychother. 2006;13:353–379. [Google Scholar]
- 69.Iqbal Z, Birchwood M, Chadwick P, Trower P. Cognitive approach to depression and suicidal thinking in psychosis: 2. Testing the validity of a social rank model. Br J Psychiatry. 2000;177:522–528. [PubMed] [Google Scholar]
- 70.Karatzias T, Gumley AI, Power KG, O'Grady M. Illness appraisals and self-esteem as correlates of anxiety and affective co-morbid disorders in schizophrenia. Compr Psychiatry. 2007;48:371–375. doi: 10.1016/j.comppsych.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 71.Gumley AI, O'Grady M, Power KG, Schwannauer M. Negative beliefs about illness and self-esteem: a comparison of socially anxious and non-socially anxious individuals with psychosis. Aust N Z J Psychiatry. 2004;38:960–964. doi: 10.1080/j.1440-1614.2004.01487.x. [DOI] [PubMed] [Google Scholar]
- 72.Gumley AI, Karatzias A, Power KG, Reilly J, McNay L, O'Grady M. Early intervention for relapse in schizophrenia: impact of cognitive behavioural therapy on negative beliefs about psychosis and self-esteem. Br J Clin Psychol. 2006;45:247–260. doi: 10.1348/014466505X49925. [DOI] [PubMed] [Google Scholar]
- 73.Birchwood M, Gilbert P, Gilbert J, et al. Interpersonal and role-related schema influence the relationship with the dominant ‘voice’ in schizophrenia: a comparison of three models. Psychol Med. 2004;34:1571–1580. doi: 10.1017/s0033291704002636. [DOI] [PubMed] [Google Scholar]
- 74.Mayhew SL, Gilbert P. Compassionate mind training with people who hear malevolent voices: a case series report. Clin Psychol Psychother. 2008;15:113–138. doi: 10.1002/cpp.566. [DOI] [PubMed] [Google Scholar]
- 75.Wells A. Meta-cognition and worry: a cognitive model of generalized anxiety disorder. Behav Cogn Psychother. 1995;23:301–320. [Google Scholar]
- 76.Wells A, Matthews G. Attention and Emotion: A Clinical Perspective. Hove, UK: Erlbaum; 1994. [Google Scholar]
- 77.Wells A, King P. Metacognitive therapy for generalized anxiety disorder: an open trial. J Behav Ther Exp Psychiatry. 2006;37:206–212. doi: 10.1016/j.jbtep.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 78.Wells A. Mindfulness approaches in cognitive behavior therapy. Behav Cogn Psychother. 2008;36:659–666. [Google Scholar]
- 79.Valmaggia L, Bouman T, Schuurman I. Attentional training with auditory hallucinations: a case study. Cogn Behav Pract. 2007;14:127–133. [Google Scholar]
- 80.Powers WT. Behavior: The Control of Perception. New York, NY: Hawthorne; 1973. [Google Scholar]
- 81.Carey T, Scitl C. Method of Levels: How to Do Psychotherapy Without Getting in the Way. Hayward, CA: Living Control Systems Publishing; 2005. [Google Scholar]
- 82.Carver CS, Scheier MF. Control theory: a useful conceptual framework for personality-social, clinical, and health psychology. In: Baumeister RF, editor. The Self in Social Psychology. New York, NY: Psychology Press; 2008. [PubMed] [Google Scholar]
- 83.Mansell W. Control theory and psychopathology: an integrative approach. Psychol Psychother. 2005;78(pt 2):141–178. doi: 10.1348/147608304X21400. [DOI] [PubMed] [Google Scholar]
- 84.Higginson S, Mansell W. What is the mechanism of psychological change? A qualitative analysis of six individuals who experienced personal change and recovery. Psychol Psychother. 2008;81(pt 3):309–328. doi: 10.1348/147608308X320125. [DOI] [PubMed] [Google Scholar]
- 85.Powers WT. Control theory: a model of organisms. Syst Dyn Rev. 1990;6:1–20. [Google Scholar]
- 86.Powers WT. Living Control Systems III: The Fact of Control. Escondido, CA: Benchmark Publications; 2008. [Google Scholar]
- 87.Carey TA. Conflict, as the Achilles heel of perceptual control, offers a unifying approach to the formulation of psychological problems. Counsel Psychol Rev. 2008;23:5–16. [Google Scholar]
- 88.Carey TA, Carey M, Mullan RJ, Spratt CG, Spratt MB. Assessing the statistical and personal significance of the method of levels. Behav Cogn Psychother. 2009;37:311–324. doi: 10.1017/S1352465809005232. [DOI] [PubMed] [Google Scholar]
- 89.Carey T. Hold That Thought! A Short Introduction to the Method of Levels. Chapel Hill, NC: Newview Publications; 2008. [Google Scholar]
- 90.Carey TA, Mullan RJ. Patients taking the lead: a naturalistic investigation of a patient led approach to treatment in primary care. Counsel Psychol Q. 2007;20:1–14. [Google Scholar]
- 91.Carey TA, Mullan RJ. Evaluating the method of levels. Counsel Psychol Q. 2008;21:1–10. [Google Scholar]
- 92.Mansell W. Perceptual control theory as an integrative framework and method of levels as a cognitive therapy: what are the pros and cons? The cognitive behaviour therapist. In press [Google Scholar]
- 93.Tai S. Learning About Conflict and Losing Control. British Association of Behaviour and Cognitive Psychotherapists 36th Annual Conference, Edinburgh, UK, 17 July 2008. Edinburgh, UK: British Association of Behaviour and Cognitive Psychotherapists; 2008. [Google Scholar]