INTRODUCTION
Disparities in health and disease between various segments of the population, such as racial and ethnic groups, have increasingly become a major focus of public health research, practice, and policy. Diet is a key contributor to disparities in many chronic diseases and conditions. Therefore, in order to address and ultimately eliminate health disparities, it is important to understand how various factors, including diet and nutrition, contribute to these disparities.
THE CHANGING RACIAL AND ETHNIC DEMOGRAPHIC PROFILES OF THE UNITED STATES
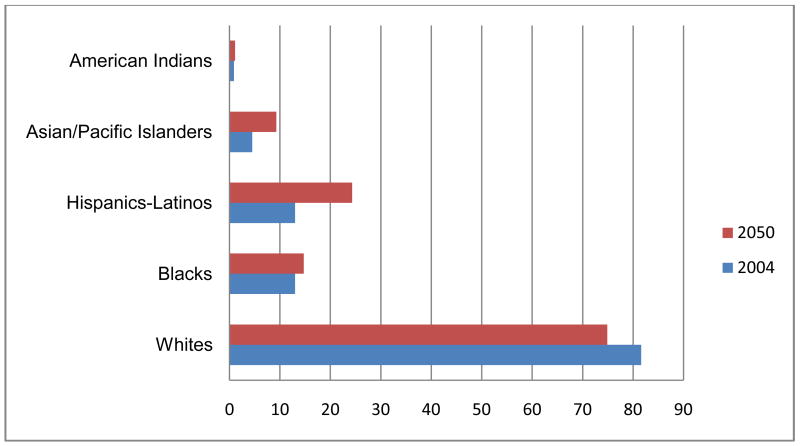
The United States (U.S.) has become increasingly diverse in the last century. According to the 2000 U.S. Census, approximately 30% of the population belongs to a racial or ethnic minority group. The U.S. Census Bureau projects that by the year 2100, non-Hispanic whites will make up only 40% of the U.S. population; much of this change is attributable to immigration patterns (1). In fact, the U.S. Census Bureau recently reported that by the year 2050, minorities -- those who identify themselves as Hispanic, black, Asian, American Indian, Native Hawaiian, Pacific Islander or mixed race -- will account for 54% of the U.S. population, which is projected to total 439 million that year. The Hispanic population is projected to nearly triple, from almost 47 million to 133 million, during the 2008–2050 period, and will jump from 15% to 30% of the population. Asians will increase from 5% of the U.S. population in 2008 to 9% by 2050. The black population is projected to rise from 14% in 2008 to 15% in 2050, while American Indians and Alaska Natives are projected to increase from 1.6% to 2% (2). Figure 1 shows the racial/ethnic breakdown of the U.S. in 2004 compared to 2050 U.S. Census Bureau projections. Given these changing demographics of the U.S. population, issues regarding diet- and health-related disparities are even more salient.
Figure 1.
U.S. Census Projections (%), 2004–2050
DEFINITION OF HEALTH DISPARITIES
The first attempt at an official definition for “health disparities” was in September 1999, in response to a White House initiative by then President Bill Clinton. In the year 2000, United States Public Law 106–525 (2000), also known as the “Minority Health and Health Disparities Research and Education Act,” which authorized the National Center for Minority Health and Health Disparities, provided a legal definition of health disparities: “A population is a health disparity population if there is a significant disparity in the overall rate of disease incidence, prevalence, morbidity, mortality or survival rates in the population as compared to the health status of the general population.” (3)
DEFINITION AND EXAMPLES OF DIET-RELATED DISPARITIES
Diet-related disparities can be defined as “differences in dietary intake, dietary behaviors, and dietary patterns in different segments of the population, resulting in poorer dietary quality and inferior health outcomes for certain groups and an unequal burden in terms of disease incidence, morbidity, mortality, survival, and quality of life.” Thus, diet-related disparities reflect differences in diet, as well as in the incidence, prevalence, mortality, and the burden of disease between and within specific population subgroups. Typically, racial and ethnic minority groups --defined here as Black or African American, Hispanic, Asian, and American Indian/Alaska natives -- experience diet-related disparities, and consequently tend to have poorer nutrient profiles and dietary behaviors and patterns relative to whites. These disparities are often defined as diets high in fat, particularly saturated fat; low in fruits, vegetables, and whole grains; and high in salt. However, it is important to note that while disparities are often defined on the basis of race and ethnicity, factors contributing to disparities may be more associated with socioeconomic status rather than ethnicity or race.
A review of differences in diet across various segments of the population is beyond the scope of this commentary. Nonetheless, it is instructive to highlight some examples of diet-related disparities. For example, according to the Behavioral Risk Factor Surveillance Survey, only 21.3% of African Americans consume fruits and vegetables ≥5 times per day, the lowest of any U.S. racial or ethnic group (4). According to results from NHANES III (1999–2002), non-Hispanic blacks were 43% (odds ratio: 0.57, 95% CI: 0.46–0.70) and Hispanics were 5% (odds ratio: 0.95, 95 CI: 0.81–1.11) less likely than whites to meet USDA fruit and vegetable guidelines (5). There are also within-racial and ethnic group disparities. For example, Lancaster et al reported that compared to Hispanic and non-Hispanic blacks born outside the, U.S. born blacks consume more total energy, total and saturated fat, and less fiber and calcium (6). Similarly, Ramirez et al reported that Mexican American men living in Texas had poorer diets and a higher prevalence of obesity compared to Latino men in California and Cuban Americans (7). These examples highlight the importance of measuring diet in all population groups, and if possible, within racial/ethnic subgroups as well.
HEALTH IMPLICATIONS OF DIET-RELATED DISPARITIES
Given that diet is etiologically linked to many health conditions, one consequence of diet-related disparities is that groups that experience these disparities also tend to have higher incidence, morbidity, and mortality rates and poorer survival for many diet-related chronic diseases and conditions, including cardiovascular disease, hypertension, cancer, Type II diabetes, and obesity. For example, African Americans develop hypertension at an earlier age, tend to have more severe high blood pressure, and are less likely to receive treatment (8). With few exceptions, cancer incidence and mortality rates are highest for African Americans compared to whites and other minority groups (9). Type II diabetes is epidemic among Native Americans (10). Obesity, as well as other cardiovascular disease risk factors such as metabolic syndrome and diabetes are prevalent in Hispanics (11). Clearly, diet-related disparities are a major contributor to differences, i.e., adverse health outcomes in racial/ethnic minorities compared to whites.
CONTRIBUTORS TO DIET-RELATED DISPARITIES
In order to design effective dietary counseling and nutrition intervention and education programs, it is important to identify the myriad of factors and characteristics that may affect dietary intake and dietary behavior. Factors that contribute to diet-related disparities among population subgroups are multifaceted and complex, and include individual, environmental, social, cultural, and behavioral attributes. Key contributors to diet-related disparities are summarized in Table 1. The discussion below highlights some examples.
Table 1.
Contributors to Diet-related Disparities
| Domains of Social Inequality |
Demographic Characteristics |
Psychosocial Factors |
Environmental Influences |
Cultural Preferences |
|---|---|---|---|---|
|
|
|
|
|
Domains of social inequality
Factors related to social inequality, such as race/ethnicity, racism, the physical environment, language barriers, disability, immigrant status, and residence (urban versus rural) undoubtedly play critical roles in diet-related disparities. For example, lack of access to supermarkets with fresh produce can result in lower fruit and vegetable consumption, and the inability to communicate in English or leave one’s home due to a disability can lead to consumption of less healthy foods.
Demographic characteristics such as age, gender, employment status, education, income, and family structure/composition are associated with dietary intake, and consequently contribute to disparities as well. For example, younger age has been shown to be associated with higher fat intake (12), while older age is correlated with higher fruit and vegetable intakes in African Americans (13). Other characteristics that have been found to be associated with high fat intake include being employed (12), lower education, low income, and having young children in the household (14). Nonetheless, it is important to note that results examining associations of demographic characteristics with dietary behavior are not always consistent across studies.
A note about socioeconomic characteristics…
Socioeconomic factors, particularly education and income, are key contributors to diet-related disparities; in fact, it has been suggested that the effects of socioeconomic status on disparities are stronger than those of race and ethnicity (15,16). Regardless of which characteristic might be a stronger contributor, the importance of socioeconomic factors cannot be overstated. For example, level of education impacts knowledge of dietary recommendations and which foods are healthy versus less healthy, while income affects whether a person can afford to purchase healthy foods.
Psychosocial factors
There is increasing evidence that psychosocial factors may affect dietary intakes, and consequently chronic disease risk. In one study, high self-efficacy (defined as confidence in one’s ability to do a certain behavior) was associated with higher fruit and vegetable and lower fat consumption (17–21). Belief in a relationship between diet and disease is correlated with healthy dietary intakes, as is high self-rated health, knowledge of dietary recommendations, strong social support (from family members and/or friends) and familiarity with nutritional guidelines, such as the U.S. food guide pyramid (17,20,21,22,23).
Environmental factors
Our environment can have an appreciable effect on diet behavior. Environmental influences on what and how we eat include the availability of healthy food choices (e.g., proximity to fast food restaurants), convenience of purchasing healthy foods (e.g., access to healthy shopping establishments), and costs of healthy foods (e.g., it is often less expensive to purchase unhealthy snack foods compared to fruits and vegetables). Learned behaviors (e.g., childhood dietary patterns) also influence current/adult behaviors. Finally, family members and peers can affect one’s diet, for example, a person may choose to eat certain foods in order to “fit in” or so that they are not viewed as “different” (14,24).
Cultural Factors
It is widely acknowledged that cultural factors influence dietary preferences and behavior, particularly in minority populations. Most factors examining the influence of culture on diet have been conducted in African Americans. Studies have shown that, in general, African Americans accept or are comfortable with larger body sizes (25–27), which may limit the extent to which healthy eating efforts are sustained. African Americans may also feel less guilty about overeating and tend to consider eating a social experience. On a positive note, they are less likely (relative to their White counterparts) to practice unhealthy dietary behaviors, such as over-exercising or purging. For example, in a study of 1,709 White, African American, and Latina women in which respondents reported their weight loss behaviors during the previous 30 days, including using diet pills, exercising, purging (vomiting, laxatives, diuretics), and dieting, Brietkopt and colleagues reported that African Americans were least likely to practice these behaviors compared with whites and Latinas (28).
Dietary acculturation
Dietary acculturation can be defined as the extent to which immigrants adopt the dietary patterns of their host countries (29). The process of acculturation, and dietary acculturation in particular, is highly complex, and associations of acculturation with diet are often inconsistent and are not always in the expected direction and do not fit a set or expected pattern (29–31). Ayala et al (32) recently published results of a systematic review examining associations of diet with various measures of acculturation, such as acculturation score, years in the United States, birthplace, generational status, and language use in Hispanics. They noted that several relationships were consistent irrespective of how acculturation was measured: no relationship with intake of dietary fat and percent energy from fat; the less versus more acculturated consumed more fruit, rice, beans, and less sugar and sugar-sweetened beverages. However, other observed relationships depended on the measure of acculturation used in the study.
Similarly, two articles in this issue of the Journal are illustrative. Dave and colleagues report that in a sample of Hispanic children aged 5–12 years (n=184), higher rates of acculturation were associated with lower fruit and vegetable intake in the home. In other studies, higher levels of acculturation have been positively associated with fruit and vegetable intake (29–31). The results reported by Bothwell et al, who examined correlates of underreporting of food intake among Mexican/Mexican American women was more consistent with the existing body of knowledge in this area, finding that underreporters were more likely to be overweight or obese and older.
Acculturation undoubtedly contributes to diet-related disparities. However, it is a process that is multidimensional, dynamic, and complex and varies considerably depending on a variety of personal, cultural, and environmental attributes. It is vital that these factors be carefully considered and taken into account in the design of research studies and counseling, intervention, and education programs.
Beware of stereotypes…
As noted above, it is important to be aware of the fact that there is considerable heterogeneity within racial and ethnic groups. For example, “Asian Americans” are not a single homogenous group, although the tendency is to classify them as such. Rather they are a heterogeneous group of persons having origins from the most diverse and populous continent in the world – the Asian continent includes 20 countries, more than 30 ethnic groups, and 200 dialects (33). When such diverse groups are considered one entity in research or in practice, one consequence is that distinct cultural, demographic, socioeconomic, generational, linguistic attributes are blurred; this can have the effect of masking the range of differences in educational and socioeconomic levels. For instance, while Asian Americans are often defined as one of the highest income minority groups in the U.S., the Hmong have a much lower per capita income ($6,000) compared to the U.S. as a whole ($21,587). (34).
Another relatively prevalent stereotype is that Asian Americans are “healthy”. However, while it has been documented that Asian Americans generally consume more fruits and vegetables than other populations, they are also among the least likely to exercise. For example, according to data from the Centers from Disease Control, only 38.6% of the Native Hawaiian or Pacific Islander (NHOPI) met physical activity recommendations in 2001–2003, compared to 45.8% of the U.S. as a whole (35). These data also point to the fact that while it is often possible to identify a cluster of healthy behaviors that track together, such as healthy eating, physical activity, non-smoking, and use of preventive health services, this is not always the case. Such nuances and possible stereotypes and biases should be thoughtfully evaluated in research studies, practice, and the establishment of policies around diet-related disparities.
STRATEGIES TO REDUCE DIET-RELATED DISPARITIES
While it might appear to be a daunting task, there are several strategies and approaches that nutritionists and dietetic professionals and nutrition researchers can undertake to accelerate solutions towards eliminating diet-related disparities (Table 2).
Table 2.
Strategies for Addressing Diet-related Disparities
| Individual-level approaches | ||||
|---|---|---|---|---|
| Nutrition education and dietary intervention programs that are targeted/tailored based on | Address cultural and environmental attributes | Innovative approaches for delivering nutrition education and interventions, e.g., | Novel channels for delivering intervention/education programs, e.g., | Identify strategies for improving recruitment/retention in interventions |
|
|
|
|
|
| Societal-level approaches | ||||
| ||||
Individual or micro-level strategies
At the individual level, it is imperative that nutrition education, dietary counseling, and intervention programs to improve diet among populations that experience disparities be targeted specifically to the populations or population sub-groups of interest, taking into account factors such as demographic characteristics, psychosocial factors, environmental attributes, and literacy. In addition, these programs need to highlight culturally salient features and other factors that affect food preferences, and should be culturally adapted to the population of interest. Examples of such culturally appropriate features include adapting successful theoretical or behavioral frameworks to various racial/ethnic groups, providing information on healthy modifications of traditional meals, approaches to increase the palatability of “healthy” foods (to address the perception that “healthy” foods do not taste good), and hiring study staff that participants can identify with on a socio-cultural basis.
Program delivery also plays a critical role in its success. It is important to identify innovative and novel venues for delivering nutrition education and intervention programs, such as churches, elementary and secondary schools, minority-serving colleges and universities, and the Internet. Finally, recruitment and retention of study participants is vital. Approaches that have been found to enhance recruitment of African Americans in research studies include identifying prospective participants through religious institutions, community networks, senior centers, and by door-to-door canvassing (36,37). Involving the participant’s family and peer network into the program, incorporating social support as a program component, and hiring ethnically-matched study staff can bolster recruitment and enhance retention.
A note about minority participation in research studies…
Given their disproportionate burden of disease and disease risk factors, including poor diets, it is vital that members of racial and ethnic minority population groups be adequately represented in research studies so that these disparities can be studied, addressed, and ultimately eliminated. Moreover, to develop culturally appropriate dietary interventions and education programs, it is necessary to collect information on determinants of behavior and behavior change specific to the population of interest. However, minority populations are usually underrepresented in clinical trials, surveillance, and prevention studies. Nonetheless, it is a considerable challenge to try to address diet-related disparities without adequate data from all the populations of interest, because results relevant to whites cannot necessarily be assumed to be applicable to non-white populations as well.
The article by Davis and colleagues in this issue of the Journal highlights this issue by reporting that a brief dietary screener developed primarily for Caucasian, adolescent girls (ages 11–18) was not appropriate for an overweight Latina female adolescent population. Such data are very important, because in studies of diet and diet-related disparities, researchers often use instruments or methodologies that have been used in primarily white populations in non-white populations without adaptation to the new population under study, which can clearly produce erroneous, unreliable, and/or invalid data. This issue of the Journal also includes an article that provides valuable descriptive data that can be used to develop research projects and identify policy initiatives that can be used to reduce diet-related disparities. Kranz and colleagues describe the extent to which 2–12 years olds living in medically underserved areas meet food group recommendations for fruits, vegetables, grains, dairy, meat/meat alternatives by age group and body weight status, and not surprisingly, found that with the exception of the meat group, the proportion of children meeting the food group intake recommendations was low. These articles clearly highlight the need for more studies that include appreciable numbers of racial and ethnic minority populations.
Societal or macro-level strategies
A number of changes at the societal or policy level can be useful in improving the diets and health of minority populations and eliminating diet-related disparities. These include increasing healthy food options in low-income neighborhoods, increasing healthy options in schools, built environments to encourage physical activity, and addressing other barriers to healthy behavior change, such as poverty and unemployment.
CONCLUSIONS
Racial and ethnic minority populations in the U.S. have high incidence, prevalence, and mortality and poor survival from diet-related chronic diseases, usually much higher than rates seen in other U.S. racial/ethnic groups. Differences in dietary intake and dietary behavior are a key contributor to these disease-related disparities. The elimination of health, diet-, and other health behavior-related disparities is a major healthcare priority in the U.S. To effectively address diet-related disparities specifically, it is important to note that 1) racial/ethnic minorities living in the U.S. are highly diverse group, and 2) a myriad of factors, including demographic, environmental, lifestyle, cultural, and societal attributes affect food preferences and dietary behaviors. Therefore, research efforts, as well as nutrition education and intervention initiatives aimed at reducing and ultimately eliminating diet-related disparities should be versatile, innovative, multi-component, and multi-faceted, and must include adequate and representative numbers of the population of interest. Importantly, they should be adapted and/or tailored to the specific group(s) under study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.U.S. Census Bureau. [Accessed December 10, 2008]; http://www.census.gov/
- 2.U.S. Census Bureau Report. [Accessed December 10, 2008];2008 http://www.census.gov/Press-Release/www/releases/archives/population/012496.html.
- 3.PUBLIC LAW 106–525—NOV. 22, 2000 http://frwebgate.access.gpo.gov/cgi-bin/getdoc.cgi?dbname=106_cong_public_laws&docid=f:publ525.106.pdf Accessed December 10, 2008.
- 4. [Accessed December 12, 2008];Behavioral Risk Factor Surveillance Survey, 2000 Nationwide Results. http://www.cdc.gov/brfss/index.htm.
- 5.Casagrande SS, Wang Y, Anderson C, Gary TL. Have Americans increased their fruit and vegetable intake? The trends between 1988 and 2002. Am J Prev Med. 2007 Apr;32(4):257–63. doi: 10.1016/j.amepre.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 6.Lancaster KJ, Watts SO, Dixon LB. Dietary intake and risk of coronary heart disease differ among ethnic subgroups of black Americans. J Nutr. 2006 Feb;136(2):446–51. doi: 10.1093/jn/136.2.446. [DOI] [PubMed] [Google Scholar]
- 7.Ramirez AG, Suarez L, Chalela P, Talavera GA, Marti J, Trapido EJ, Villarreal R, Pérez-Stable EJ. Cancer risk factors among men of diverse Hispanic or Latino origins. Prev Med. 2004 Aug;39(2):263–9. doi: 10.1016/j.ypmed.2004.03.034. [DOI] [PubMed] [Google Scholar]
- 8.Hollar D, Agatston AS, Hennekens CH. Hypertension: trends, risks, drug therapies and clinical challenges in African Americans. Ethn Dis. 2004;14(4):S2-23–5. [PubMed] [Google Scholar]
- 9.American Cancer Society. [Accessed December 10, 2008];Cancer facts and figures 2008. [Atlanta: American Cancer Society. 2008 URL: http://www.cancer.org/downloads/STT/2008CAFFfinalsecured.pdf.
- 10.Egede LE, Dagogo-Jack S. Epidemiology of type 2 diabetes: focus on ethnic minorities. Med Clin North Am. 2005 Sep;89(5):949–75. viii. doi: 10.1016/j.mcna.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 11.Davidson JA, Kannel WB, Lopez-Candales A, Morales L, Moreno PR, Ovalle F, Rodriguez CJ, Rodbard HW, Rosenson RS, Stern M. Avoiding the looming Latino/Hispanic cardiovascular health crisis: a call to action. Ethn Dis. 2007 Summer;17(3):568–73. [PubMed] [Google Scholar]
- 12.Kayrooz K, Moy TF, Yanek LR, Becker DM. Dietary fat patterns in urban African American women. Community Health. 1998;23(6):453–69. doi: 10.1023/a:1018710208684. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=pubmed&cmd=Search&term=%22Satia%2DAbouta+J%22%5BAuthor%5D. [DOI] [PubMed]
- 13.McClelland JW, Demark-Wahnefried W, Mustian RD, Cowan AT, Campbell MK. Fruit and vegetable consumption of rural African Americans: baseline survey results of the Black Churches United for Better Health 5 A Day Project. Nutr Cancer. 1998;30(2):148–57. doi: 10.1080/01635589809514655. [DOI] [PubMed] [Google Scholar]
- 14.Eyler AA, Haire-Joshu D, Brownson RC, Nanney MS. Correlates of fat intake among urban, low income African Americans. Am J Health Behav. 2004;28(5):410–7. doi: 10.5993/ajhb.28.5.3. [DOI] [PubMed] [Google Scholar]
- 15.Adler NE, Rehkopf DH. U.S. disparities in health: descriptions, causes, and mechanisms. Annu Rev Public Health. 2008;29:235–52. doi: 10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]
- 16.Bahr PR. Race and nutrition: an investigation of Black-White differences in health-related nutritional behaviours. Sociol Health Illn. 2007 Sep;29(6):831–56. doi: 10.1111/j.1467-9566.2007.01049.x. [DOI] [PubMed] [Google Scholar]
- 17.Watters JL, Satia JA, Galanko JA. Associations of psychosocial factors with fruit and vegetable intake among African-Americans. Public Health Nutr. 2007 Jul;10(7):701–11. doi: 10.1017/S1368980007662284. [DOI] [PubMed] [Google Scholar]
- 18.Watters JL, Satia JA, Kupper LL. Correlates of antioxidant nutrients and oxidative DNA Damage differ by race in a cross-sectional study of healthy African American and White adults. Nutrition Research. 2008;28:535–576. doi: 10.1016/j.nutres.2008.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Campbell MK, Demark-Wahnefried W, Symons M, Kalsbeek WD, Dodds J, Cowan A, Jackson B, Motsinger B, Hoben K, Lashley J, Demissie S, McClelland JW. Fruit and vegetable consumption and prevention of cancer: the Black Churches United for Better Health project. Am J Public Health. 1999 Sep;89(9):1390–6. doi: 10.2105/ajph.89.9.1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Campbell MK, Symons M, Demark-Wahnefried W, Polhamus B, Bernhardt JM, McClelland JW, Washington C. Stages of change and psychosocial correlates of fruit and vegetable consumption among rural African-American church members. Am J Health Promot. 1998 Jan-Feb;12(3):185–91. doi: 10.4278/0890-1171-12.3.185. [DOI] [PubMed] [Google Scholar]
- 21.Van Duyn MA, Kristal AR, Dodd K, Campbell MK, Subar AF, Stables G, Nebeling L, Glanz K. Association of awareness, intrapersonal and interpersonal factors, and stage of dietary change with fruit and vegetable consumption: a national survey. Am J Health Promot. 2001 Nov–Dec;16(2):69–78. doi: 10.4278/0890-1171-16.2.69. [DOI] [PubMed] [Google Scholar]
- 22.Satia JA, Galanko J, Siega-Riz A. Fast food restaurant eating is associated with dietary intake, demographic, psychosocial, and behavioral factors among African Americans in North Carolina. Public Health Nutr. 2004;7(8):1089–1096. doi: 10.1079/PHN2004662. [DOI] [PubMed] [Google Scholar]
- 23.Satia JA, Galanko J, Neuhouser ML. Food nutrition label use is associated with diet-related psychosocial factors and dietary intake among African Americans in North Carolina. J Am Diet Assoc. 2005 Mar;105(3):392–402. doi: 10.1016/j.jada.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 24.Vitolins MZ, Quandt SA, Bell RA, Arcury TA, Case LD. Quality of diets consumed by older rural adults. J Rural Health. 2002;18(1):49–56. doi: 10.1111/j.1748-0361.2002.tb00876.x. [DOI] [PubMed] [Google Scholar]
- 25.Boyington JE, Carter-Edwards L, Piehl M, Hutson J, Langdon D, McManus S. Cultural attitudes toward weight, diet, and physical activity among overweight African American girls. Prev Chronic Dis. 2008 Apr;5(2):A36. [PMC free article] [PubMed] [Google Scholar]
- 26.Kumanyika SK, Gary TL, Lancaster KJ, Samuel-Hodge CD, Banks-Wallace J, Beech BM, Hughes-Halbert C, Karanja N, Odoms-Young AM, Prewitt TE, Whitt-Glover MC. Achieving healthy weight in African-American communities: research perspectives and priorities. Obes Res. 2005 Dec;13(12):2037–47. doi: 10.1038/oby.2005.251. [DOI] [PubMed] [Google Scholar]
- 27.Kumanyika SK. Obesity in African Americans: biobehavioral consequences of culture. Ethn Dis. 1998 Winter;8(1):93–6. [PubMed] [Google Scholar]
- 28.Breitkopf CR, Berenson AB. Correlates of weight loss behaviors among low-income African-American, Caucasian, and Latina women. Obstet Gynecol. 2004;103(2):231–9. doi: 10.1097/01.AOG.0000110244.73624.b1. [DOI] [PubMed] [Google Scholar]
- 29.Satia-Abouta J, Patterson RE, Neuhouser ML, Elder J. Dietary Acculturation: Applications to Nutrition Research and Dietetics. J Am Diet Assoc. 2002;102:1105–1118. doi: 10.1016/s0002-8223(02)90247-6. [DOI] [PubMed] [Google Scholar]
- 30.Lv N, Cason KL. Dietary pattern change and acculturation of Chinese Americans in Pennsylvania. J Am Diet Assoc. 2004 May;104(5):771–8. doi: 10.1016/j.jada.2004.02.032. [DOI] [PubMed] [Google Scholar]
- 31.Park SY, Murphy SP, Sharma S, Kolonel LN. Dietary intakes and health-related behaviours of Korean American women born in the USA and Korea: the Multiethnic Cohort Study. Public Health Nutr. 2005 Oct;8(7):904–11. doi: 10.1079/phn2005740. [DOI] [PubMed] [Google Scholar]
- 32.Ayala GX, Baquero B, Klinger S. A systematic review of the relationship between acculturation and diet among Latinos in the United States: implications for future research. J Am Diet Assoc. 2008 Aug;108(8):1330–44. doi: 10.1016/j.jada.2008.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen MS., Jr Cancer prevention and control among Asian and Pacific Islander Americans: findings and recommendations. Cancer. 1998;831:856–1864. [Google Scholar]
- 34.United States Census Bureau. [Accessed December 1, 2008];Asian American heritage month. 2004 May; Available at URL: http://www.census.gov/press-release/www.release/archives/facts_for_features_special_edition.
- 35.Centers for Disease Control and Prevention. Physical activity among Asians and Native Hawaiian or other Pacific Islanders - 50 states and the District of Columbia, 2001–2003. MMWR Morbid Mortal Wkly Rep. 2004;53:756–760. [PubMed] [Google Scholar]
- 36.UyBico SJ, Pavel S, Gross CP. Recruiting vulnerable populations into research: a systematic review of recruitment interventions. J Gen Intern Med. 2007 Jun;22(6):852–63. doi: 10.1007/s11606-007-0126-3. Epub 2007 Mar 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annu Rev Public Health. 2006;27:1–28. doi: 10.1146/annurev.publhealth.27.021405.102113. [DOI] [PubMed] [Google Scholar]