In the treatment of chronic biliary tract disease, repetitive access to the extrahepatic and intrahepatic biliary tree may be desirable or even life-saving. This will be demonstrated by an experience with a patient who had recurrent ductal strictures and intrahepatic sludge formation. A method was devised to permit repeated entry into the intrahepatic and extrahepatic biliary ducts and, thus, to irrigate and instrument these structures at will.
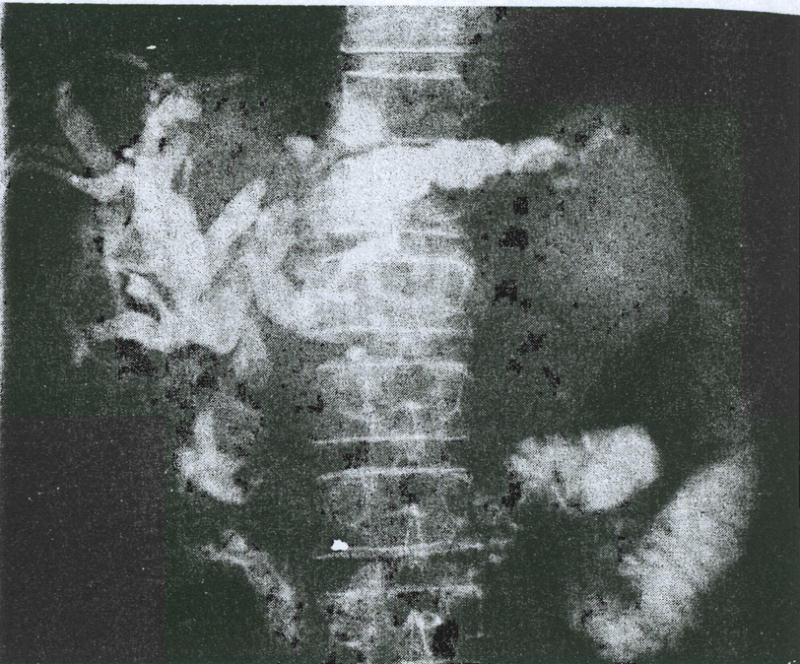
A 74 year old white male had a history of recurrent biliary duct disease dating from a cholecystectomy in 1937. A common duct reconstruction with choledochoduodenostomy was performed in 1945. This was revised twice in the next 18 years. Between 1963 and 1973, three more operations were performed for extrahepatic biliary obstruction and removal of intrahepatic debris. He was first operated upon by us in January 1973, because of jaundice, fever and recurrent bacteremia. His previous choledochoduodenostomy was stenotic, there was marked intrahepatic ductal dilatation (Fig. 2) and chalklike debris crammed all the intrahepatic ducts. Choledochoduodenostomy was reperformed just below the bifurcation of the duct. As much of the sludge was removed as possible, but the cleansing was known to be incomplete. Within six months, the symptoms began to recur sporadically. Between 18 and 24 months postoperatively, the serum bilirubin increased to 12 milligrams per 100 milliliters. Ascites and other evidence of biliary cirrhosis were now present. Retrograde cholangiography demonstrated a patent anastomosis and a greatly dilated biliary duct system.
Fig. 2.

The massively dilated intrahepatic biliary tree visualized by percutaneous transhepatic cholangiography prior to operation in 1973.
TECHNIQUE
Operation was undertaken through a previously used right subcostal incision. Through a small anterior duodenotomy, the choledochoduodenostomy constructed 24 months earlier was found to be widely patent. However, the intrahepatic duct system above this point was again completely filled with soft debris which formed a cast extending into the smaller intrahepatic radicles. A large amount of this debris was removed.
A Silastic (silicone rubber) tube, 0.192 inch in diameter, was inserted through the same duodenotomy incision, passing one limb up the main right duct and out through the liver substance, as described by Smith. The other limb was brought through the left duct and lobe. The two limbs were joined externally with a connecting tube, as shown in Figure 1a).
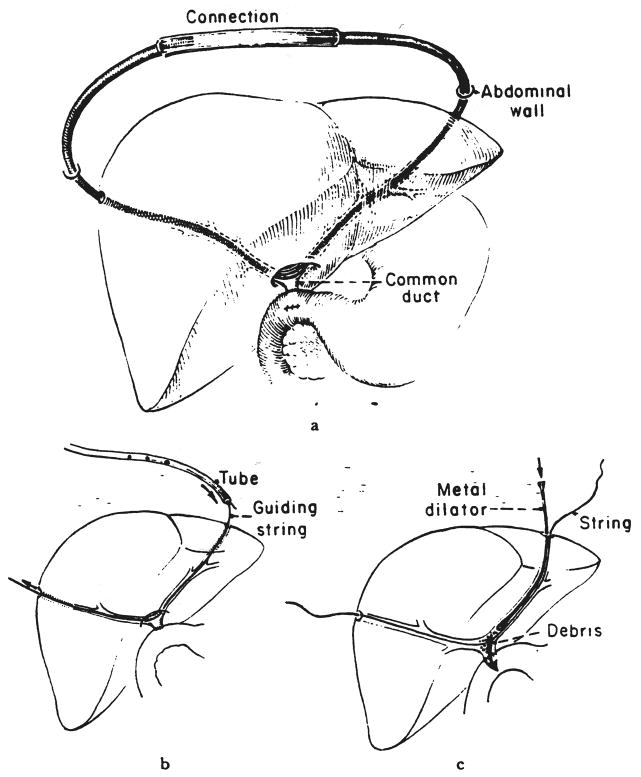
Fig. 1.
Technique of U tube placement. a, The U tube is in place with the ends joined by a connecting tube. b, To change the U tube, the Silastic tube is withdrawn with a trailing heavy silk suture, which is used to pull through another tube. c, The right and left ducts as well as the anastomosis can be obturated and dilated with a Bakes dilator.
The drainage tube was not disturbed for a week. Irrigations were then begun through one of the limbs. The placement of three holes in the tube at strategic intrahepatic locations allowed the saline solution to reach all portions of the liver. A month after operation, the tube could be removed while drawing a string through the tract. Under fluoro-scope control, Bakes dilators were introduced through the right and left tracts to obturate the choledochoduodenostomy (Figs. 1b and c and 3). At first, this was necessary once a week because of the piling up of sludge on the liver side of the choledochoduodenal anastomosis. With the passage of time, the bile became more normal in appearance, the precipitation of the debris became visibly less, and the number of necessary dilatations decreased to once per month. After each such treatment, the string was used to draw a fresh, perforated Silastic tube through the liver into the desired position.
Fig. 3.
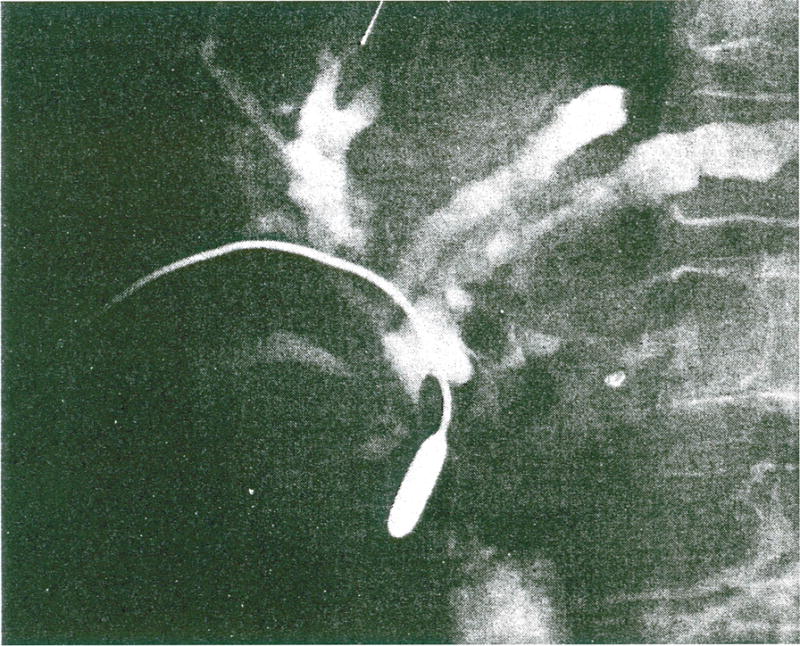
The Bakes dilator passed through the choledochoduodenal anastomosis (Fig. 1c).
Postoperatively, the patient had a steady decrease in bilirubin. There has been no episode of cholangitis in the five postoperative months, during which time the intrahepatic ducts have slowly assumed a more normal appearance (Fig. 4). It is planned to leave the U tube in place for the balance of the patient’s lifetime.
Fig. 4.
Postoperatively, the biliary ducts have slowly come to assume a more normal anatomy. During instrumentation, roentgenologic evaluation can be achieved by dripping contrast medium into the intrahepatic tract.
SUMMARY
This surgical technique has permitted re-entry into the intrahepatic and extrahepatic biliary tree for the purpose of dilatation and the manual propulsion of debris through a ductal anastomosis. The method undoubtedly has other applications in the treatment of complicated biliary duct problems.
Acknowledgments
This work was supported by research grants from the Veterans Administration, by Grants No. AI-AM-08898 and AM-07772 from the National Institutes of Health and by Grants No. RR-00051 and RR-00069 from the General Clinical Research Centers Program of the Division of Research Resources, National Institutes of Health.
References
- Smith R. Hepaticojejunostomy with transhepatic intubation. Br J Surg. 1964;51:186. doi: 10.1002/bjs.1800510307. [DOI] [PubMed] [Google Scholar]