Abstract
The formation of more than trace amounts of ice in cells is lethal. The two contrasting routes to avoiding it are slow equilibrium freezing and vitrification. The cryopreservation of mammalian oocytes by either method continues to be difficult, but there seems a slowly emerging consensus that vitrification procedures are somewhat better for mouse and human oocytes. The approach in these latter procedures is to load cells with high concentrations of glass-inducing solutes and cool them at rates high enough to induce the glassy state. Several devices have been developed to achieve very high cooling rates. Our study has been concerned with the relative influences of warming rate and cooling rate on the survival of mouse oocytes subjected to a vitrification procedure. Oocytes suspended in an ethylene glycol-acetamide-Ficoll-sucrose solution were cooled to −196°C at rates ranging from 37°C/min to 1827°C/min between 20°C and −120°C, and for each cooling rate, warmed at rates ranging from 139°C/min to 2950°C/min between −70°C and −35°C. The results are unambiguous. If the samples were warmed at the highest rate, survivals were >80% over cooling rates of 187°C/min to 1827°C/min. If the samples were warmed at the lowest rate, survivals were near 0% regardless of the cooling rate. We interpret the lethality of slow warming to be a consequence of it allowing time for the growth of small intracellular ice crystals by recrystallization.
Keywords: cooling rate, cryopreservation, devitrification, mouse oocytes, recrystallization of intracellular ice, vitrification, warming rate
Introduction
The formation of more than trace amounts of ice in cells is a lethal event (Karlsson has calculated the limiting amount to be 2 to 4% of the water in hepatocytes [3]); consequently, successful cryopreservation demands that it be avoided. There are two routes for so doing. One is by slow equilibrium freezing; the other is by vitrification. In the former approach, ice forms first in the external medium. This causes the chemical potential of the water in the medium to drop below the chemical potential of the intracellular water. This differential represents an osmotic driving force for water to leave the cell and freeze externally. In slow equilibrium freezing, cells are cooled slowly enough so that the cell’s water content decreases sufficiently to keep its chemical potential in near equilibrium with the outside water and to fall to the equilibrium value before the cell has been cooled to a temperature that permits intracellular nucleation.
The vitrification approach is entirely different. In it, ice formation is avoided both in the medium and in the cells by suspending the cells in very high concentrations of solutes, including ones that permeate the cell, and cooling them at high rates to temperatures below −100°C. As a result the water in the system is converted from a liquid to a glass with no ice formation. The approach also requires high warming rates to ensure that the system does not convert from glass to ice during warming.
Many cell types have been successfully cryopreserved by the slow equilibrium approach. Examples include erythrocytes and most leucocytes, adult and embryonic stem cells, umbilical cord cells, most tissue culture lines, and (importantly) preimplantation embryos from more than 20 species of mammals. But some cell types cannot be cryopreserved by slow equilibrium methods, or yield poor survivals. The common reasons for failure are high chill sensitivity, the inability to maintain an intracellular supercooled state, and the disruption of complex cell-cell interactions by extracellular ice (EIF).
Currently, there is intense interest in developing procedures for effectively cryopreserving the human oocyte, but the results to date have not matched the interest. To date, only about 500 babies have been derived from cryopreserved oocytes as opposed to tens of thousands that have developed from frozen embryos. Although neither the slow freezing approach nor the vitrification approach have worked at all well, there is considerable debate over which approach shows the more promise. In the case of mouse and human oocytes there seems to be a developing consensus that vitrification procedures yield better survivals in terms of percentages of fertilization and development to blastocyst than do slow freezing procedures [1,9]. The matter was discussed in a recent International Conference on the Cryopreservation of the Human Oocyte held in Bologna, Italy, 26–29 November 2008. There, P. Levi-Setti presented meta-analyses indicating that the vitrification approach was yielding somewhat better results. One reason for the difficulty appears to be that the mature oocytes are arrested in metaphase II of meiosis with the chromosomes arrayed on a meiotic spindle. The spindle is composed of microtubulin and, like microtubules in general, it becomes disaggregated by being cooled to temperatures near 0°C. The question of whether irreversible spindle and cytoskeletal damage underlie cryopreservation difficulties was reviewed in some detail by G. Goticchio at that same conference. The conclusion was “possibly.” (see [17])
The premise in the vitrification approach has been that the higher the cooling rate, the greater the likelihood that true vitrification can be achieved. Consequently, a series of devices have been developed over the past decade that achieve cooling rates of ≥10,000°C/min by permitting the manipulation of very small volumes of ooycte suspensions. These include electron microscope grids [12], nylon mesh [13], open-pulled straw (OPS) [27], cryoloop [11], microdrop method [10,19], and cryotops [8,9]. The fact that the devices also yield very high warming is often noted by the authors, but only parenthetically.
The purpose of our current study was to experimentally separate out the relative importance of cooling and warming rate to the survival of mouse oocytes subjected to a vitrification procedure, and to determine the functional relationship between rate and survival. In this study, we have made use of the range of cooling and warming rates available with standard ¼ ml straws (<3,000°C/min). Later, we plan to extend this to these newer devices. In a preceding recent study [26], we examined the effect of warming rate on the survival of mouse oocytes “vitrified” by cooling at the single moderate rate deemed optimum by Kasai [4–6]. Here, we examine the interactions of a matrix of different cooling and warming rates higher and lower than the standard.
Beginning with the seminal work by Rall and Fahy [22] in developing a vitrification solution (VS1) containing dimethyl sulfoxide, acetamide, and propylene glycol, many variations have been developed and assessed in mouse and human oocytes. One group of these is the family of vitrification solutions developed by Kasai et al. for mouse embryos and oocytes [5,6]. When we began this series of studies on mouse oocytes in 2004 [15], we selected a variant named EAFS 10/10. It is based on ethylene glycol and acetamide as permeating cryoprotectants, supplemented with Ficoll and sucrose.
The terminology in the vitrification literature is rather ambiguous and imprecise. We shall try to remedy that here. We define vitrification as the conversion of the water in an aqueous solution to a glass without the formation of ice. Experimentally, vitrification of the medium is manifested by the lack of evolution of latent heat of fusion as measured by thermal analysis (used here) or differential scanning calorimetry. In some cases, it is observed in the x-ray diffraction pattern. In many cases, the literature defines it as a procedure that yields a clear transparent medium after cooling to < 120°C as opposed to an opaque sugar-like appearance. In nearly all cases, vitrification or lack thereof refers (or should refer) only to the extracellular medium. There is rarely any evidence in publications as to whether or not the cells themselves have vitrified. The little evidence that exists on this matter comes from electron microscopy on freeze-cleaved or freeze-substituted cells. Often, authors use the term vitrification to indicate a procedure involving the suspension of cells in high concentrations of glass-promoting solutes and rapid cooling, but without evidence as to whether vitrification has in fact occurred. We shall refer to that situation as a “vitrification procedure”.
With respect to events during warming, we define devitrification as the conversion of a glass to a highly viscous supercooled liquid. Crystallization is the conversion of this supercooled liquid to ice during warming. Recrystallization is the growth of larger ice crystals at the expense of smaller ones. Finally, there can be the probably rare case where the glass or viscous devitrified liquid warms to the melting point of ice without any ice forming. We shall refer to that process as “melting” by analogy to the terminology for silica glass.
Materials and methods
Collection of oocytes
Mature female ICR mice were induced to superovulate with intraperitoneal injections of 5 IU of equine chronic gonadotropin (eCG) (Sigma) and 5 IU of hCG (Sigma, St. Louis) given 48h apart. Ovulated unfertilized oocytes were collected from the ampullar portion of the oviducts at 13 h after hCG injection and were freed from cumulus cells by suspending them in modified phosphate-buffered saline (PB1) containing 0.5 mg/ml hyaluronidase followed by washing with fresh PB1 medium. These procedures were carried out under the University of Tennessee IACUC protocol 911-0607.
Composition of vitrification solution
The vitrification solution (EAFS 10/10) was developed by Pedro et al. [20] for cryopreservation of mouse oocytes at metaphase II stage. It consists of 10% (v/v) ethylene glycol (EG) and 10.7% (w/v) acetamide dissolved in a stock consisting of 30% (w/v) Ficoll 70 and 0.5 M sucrose in PB1 medium. The final concentration of sucrose and Ficoll are 0.4 M and 24% (w/v), respectively. Its mass composition was given in a previous report [26]; namely, 3.23 molal EG and 3.27 molal acetamide as the highly permeating cryoprotectants [21], and 0.150 molal salts (as NaCl) and 0.720 molal sucrose as impermeable solutes, plus 20.68 weight % of Ficoll and 0.166 weight % of bovine serum albumin.
Vitrification procedure
With the oocytes being maintained at 25°C, the following solutions were successively aspirated into 0.25-ml straws (IMV Technologies, L’Aigle, France): A 60 mm column of PB1 medium containing 0.5 M sucrose, a 20 mm column of air, a mm column of EAFS 10/10, a 5 mm column of air, and a 12 mm column of EAFS 10/10 to contain the oocytes. The oocytes were transferred to successive drops of EAFS 10/10 at 25°C and 3 to 6 were transferred by micropipette into the 12 mm column of EAFS 10/10 in each straw. The end of the straw opposite the polyvinyl alcohol plug was then heat sealed. Two minutes after first introducing the oocytes into EAFS 10/10, the straws were cooled by one of the cooling procedures explained below.
Achieving various cooling rates – Physical set up and procedure
The purpose of this study was to determine the effect of cooling rates and warming rates on the survival of EAFS 10/10-vitrified mouse oocytes. The different cooling protocols are listed in Table 1. Protocol 5 is the standard procedure used in Dr. Kasai and Dr. Edashige’s laboratory and in our laboratory.
Table 1.
Protocol of each cooling procedures
| Protocol No. | 1/4 ml straw was covered with | Cooled by | Cooling ratea ± S.E. (°C/min) |
|---|---|---|---|
| 1 | 1/2 ml straw + double glassc | LN2 vaporf | 37±0 |
| 2 | 1/2 ml straw + glassd | LN2 vaporf | 62±3 |
| 3 | glasse | LN2 vaporf | 75±4 |
| 4 | 1/2 ml straw | LN2 vaporf | 145±3 |
| 5b | none | LN2 vaporf | 187±6 |
| 6 | 1/2 ml straw | LN2 | 522±54 |
| 7 | none | LN2 | 1827±214 |
The cooling rates were determined from 20 °C to −120 °C. N = 5
This procedure is the standard procedure used in our laboratory, and Kasai’s and Edashige’s laboratory.
1/4 ml sample straw was covered with a 1/2 ml straw, a 7 mm OD × 90 mm glass tube, and a 10 mm OD × 90 mm glass tube.
1/4 ml sample straw was covered with a 1/2 ml straw and a 7 mm OD × 90 mm glass tube.
1/4 ml sample straw was covered with 7 mm OD × 90 mm glass tube.
The straw was placed horizontally on a Styrofoam disk (14 cm diameter, 1.5 cm thick) floated on the surface of LN2 in a 4 litre Dewar flask for > 5 min before being immersed in LN2.
To determine the cooling rates with each procedure, a 36 gauge copper-constantan thermocouple was inserted into a standard IMV 1/4 ml straw containing a 50 mm column of EAFS 10/10 solution. The thermocouple was attached to a Fluke (2190A) Digital Thermometer (Seattle, WA). It outputs about three temperature reading per second (the exact output rate was determined by stop watch for each run). The outputs were fed into a PC computer with Windows XP using the Hyperterminal program provided, and transferred to the computer disk. Changes in temperature vs. time were recorded from 25°C to about −180°C, but the cooling rates listed in the right hand column of Table 1 were based on the time taken to traverse the range of 20°C to −120°C.
Cooling procedures 1–5 involved cooling in liquid nitrogen (LN2) vapor. Naked 1/4 ml straws or straws surrounded by various outer tubes were placed horizontally on a 1.5 cm thick Styrofoam disk floated on the surface of LN2 in a Dewar flask for at least 6 min before being immersed in LN2. The difference among procedures 1–4 was whether their straw was covered by a bigger 0.5-ml straw (procedure 4) or by glass tubes of various dimensions (procedures 1–3). The glass tubes used were either 7 mm O.D.×90 mm or 10 mm O.D. ×90 mm.
Plots of the resulting temperatures and times permitted calculations of the cooling rates. At many of the cooling rates there were rather abrupt changes in slope that were evidence of freezing of the EAFS 10/10 solution. To confirm that these changes in slope were in fact due to ice formation, cooling protocols 1, 5, and 6 were replicated in our differential scanning calorimeter (DSC). The set up and procedures for DSC have been described previously [7,25].
Achieving various warming rates
With each of the seven cooling rates, samples were warmed at the five different rates shown in Table 2; namely, 139, 476, 1220, 2170, and 2950°C/min . The details of achieving these various warming rates have been published previously [26]. Procedure 5 is the standard method developed and used by Dr. Kasai and Dr. Edashige laboratory, as well as by us. It involves removing a 1/4 ml straw from LN2, holding it in room temperature air for 10 sec, and then abruptly immersing it in a 25°C water bath. We have found it yields a warming rate of 2950°C/min [26].
Table 2.
Protocol of each warming procedure
| Protocol | Air at 23°C–25°C |
Covered | Water |
Warming ratea | ||
|---|---|---|---|---|---|---|
| ‥ | Time (sec.) | stirringb | ⋯ | Temp. (°C) | stirringb,c | ± S.E. (°C/min) |
| 1 | 60 | - | none | N/A | N/A | 139±7 |
| 2 | 10 | - | strawd | 25 | + | 476±18 |
| 3 | 10 | - | mineral oile | 25 | + | 1220±97 |
| 4 | 10 | - | none | 0 | + | 2170±114 |
| 5 | 10 | - | none | 25 | + | 2950±119 |
The warming rates were calculated between −70°C and −35°C.
+ = yes and − = no.
NA, not applicable.
The 0.25 ml sample straws were inserted into pre-cooled (< −110˚C) 0.5 ml straws before being plunged into water at 25°C.
The sample straws (at < −110°C) were dipped for ∼1 sec. in mineral oil at 25°C before being plunged into water at 25°C.
(From Seki and Mazur [26]
Criteria of survival of oocytes subject to vitrification procedures in EAFS 10/10
After freezing and thawing or vitrifying and melting, the contents were expelled into a watch glass by flushing the straw with 0.8 ml of 0.5 mol/l sucrose solution. The oocytes were then pipetted into fresh 0.5 mol/l sucrose solution. Approximately 10 min later, they were transferred to fresh PB1 medium lacking sucrose, and then transferred to and cultured in modified M16 medium [20] for 2 hrs. (For simplicity, this will henceforth be referred to as M16).
Viability was assessed at three time points based on osmotic responsiveness and morphological normality. First, the oocytes were examined during the 10 min in PB1/sucrose. Membrane-intact oocytes were expected to shrink with time because the sucrose is hypertonic. Second and third, they were examined after being placed in M16 and after two hours incubation. They fall into two binary groups: Degenerate oocytes are clearly non-viable. The others are indistinguishable from fresh oocytes, and we know from past experiments that the plasma membranes in this latter group are intact and function normally with respect to their osmotic response to hypertonic and hypotonic media, and with respect to their ability to remain supercooled in the presence of external ice. The ability to manifest these characteristics after two hours in M16 is considered a rather stringent test of viability. Still other criteria of normality are given in [15, pp. 48–49]. They mostly deal with measures of the integrity of the plasma membrane.
Statistics
Error figures in tables and error bars in graphs are standard errors (standard deviations of the mean). Tests of significance were carried out by 1-way ANOVA using Graphpad Software’s Instat, V. 3.02 followed by the Tukey-Kramer Multiple Comparison Test.
Results
Cooling rates of EAFS 10/10 vitrification solutions in 0.25-ml straws with seven different procedures
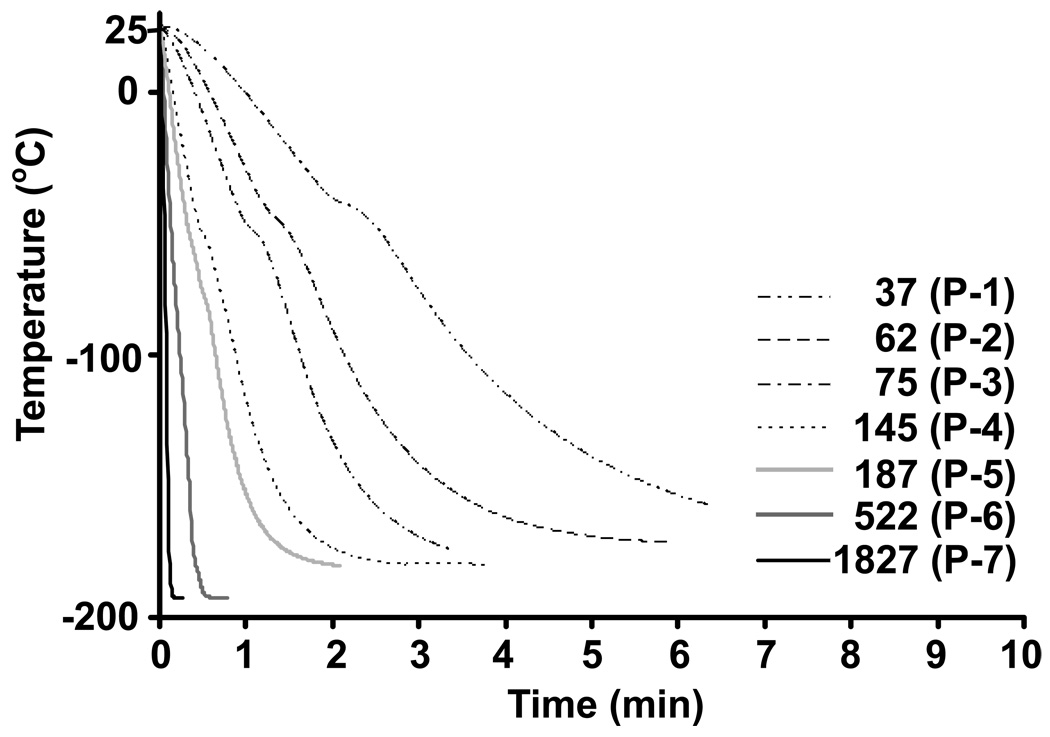
Figure 1 shows the plots of the temperature of the EAFS 10/10 solution in straws as a function of time for each of the 7 cooling procedures. The two highest rates (522°C/min and 1827°C/min; Protocols 6 and 7) were produced by directly immersing the straws with/without a covering 0.5-ml straw into LN2. The other five protocols involved cooling with LN2 vapor and produced the low cooling rates of 37°C to 187°C/min.
Fig. 1.
Cooling rates of EAFS 10/10 vitrification solutions in 0.25-ml straws with 7 different procedures. Each cooling procedure was repeated five times.
Effect of cooling rate on whether the EAFS 10/10 medium freezes or vitrifies
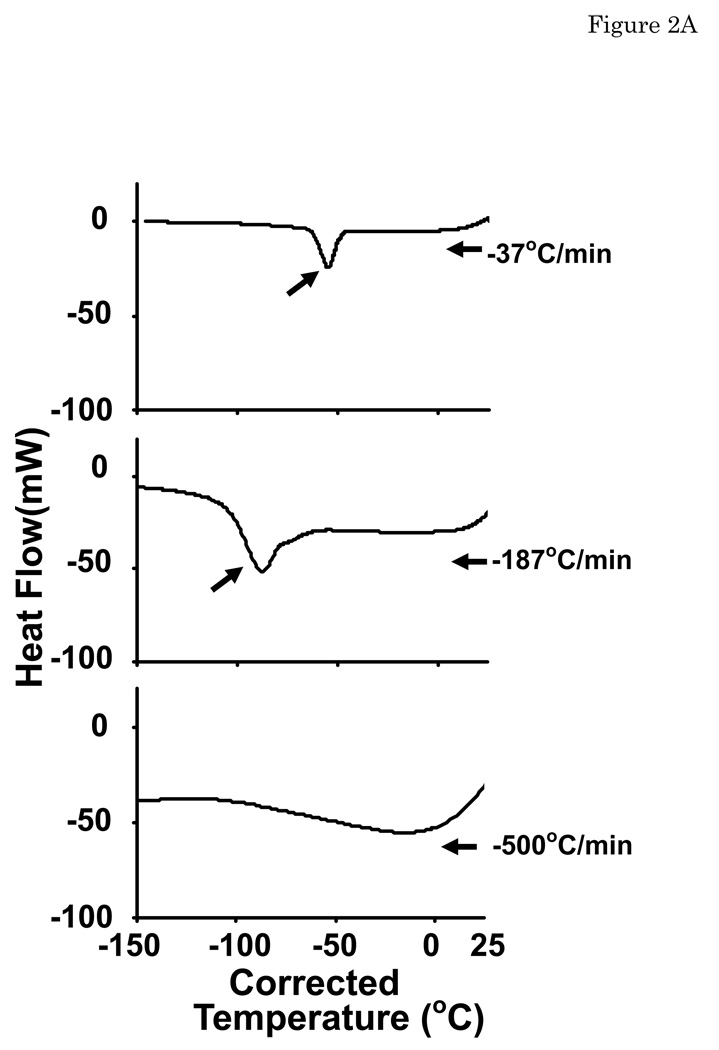
Fig. 1 shows that with cooling rates of 37, 62, 75, 145 and 187°C/min, a change in the temperature-time slope occurred at −40, −45, −49, −50, and −67°C. This is a consequence of the onset of ice formation in the EAFS 10/10 solution. No change in slope was observed in samples cooled at 522°C/min and 1827°C/min, suggesting that they have vitrified. This was confirmed by the appearance of samples at −196°C after being cooled in straws at 187°C/min or 1827°C/min. The latter were completely clear. The former looked like diluted skim milk. The conclusions were also confirmed by the DSC thermograms in Fig. 2A of EAFS 10/10 solutions cooled at 37°C, 187°C and 500°C/min. With cooling rates of 37°C/min and 187°C/min, exotherms began to be generated at −45°C and −75°C. At a cooling rate of 500°C/min, no exotherms were visible indicating that the medium vitrified. For a cooling rate of 37°C/min, the onset of freezing occurred at −40°C and −45°C with the thermocouple and DSC approaches, respectively. With a cooling rate of 187°C/min, it occurred at −67°C and −75°C, respectively. With cooling at 500°C/min neither method detected an exotherm. These observations show that EAFS 10/10 solution vitrified at high cooling rates but did not do so at low cooling rates. Our conclusion is that the standard Kasai/Edashige “vitrification” procedure, which cools samples at 187°C/min, does not vitrify the EAFS 10/10 solution or does not do so completely. We do not know what occurs inside the oocytes.
Fig. 2.
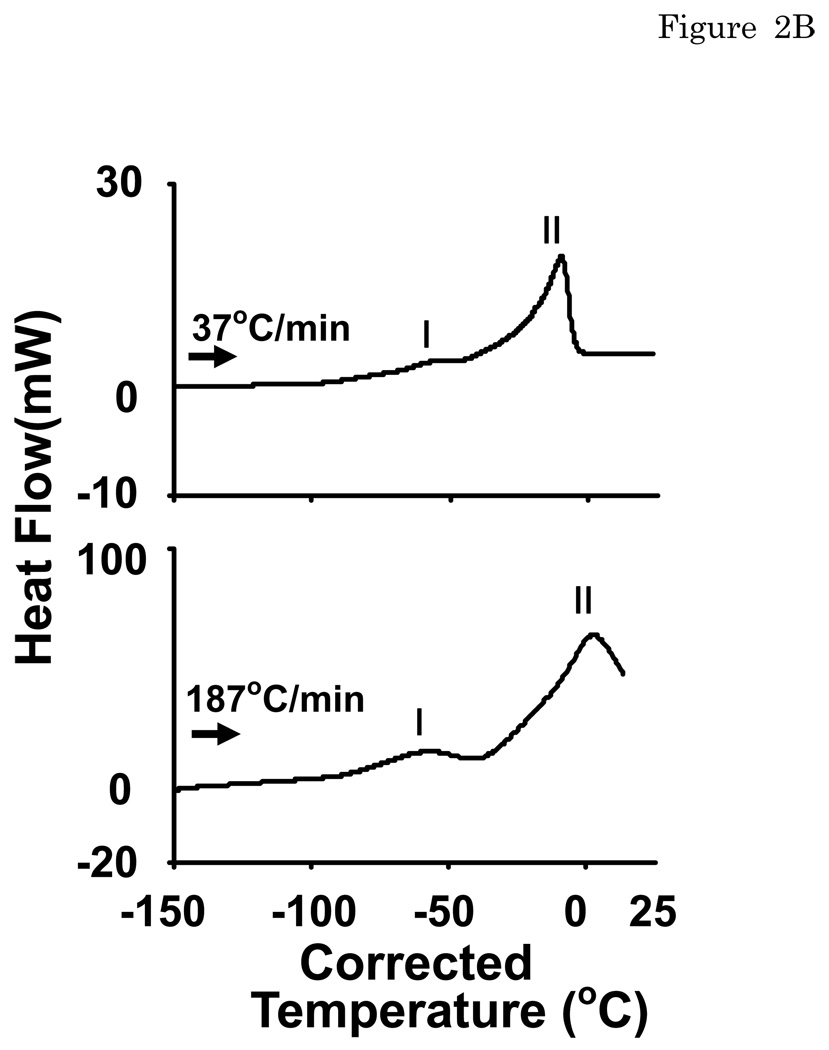
DSC thermograms of a drop of EAFS 10/10 (A) cooled at 37, 187, 500 °C/min and (B) warmed at the same rate they were cooled. A downward peak is exothermic. The arrows indicate whether the thermogram involved cooling or warming. The temperatures on the abscissa have been corrected for the instrument and thermal lags induced by cooling and warming rates greater than the initial calibration– see Methods and [25].
The temperatures on the abscissas of Fig. 2A are corrected for the fact that the temperatures displayed by the DSC lag the true temperatures by an amount that increases with increasing cooling rate. The formulas for the correction are given by Seki et al. [25]. With a cooling rate of 187°C/min the correction amounts to 16.3°C. The formulas were developed from calibrations run at up to 150°C/min; consequently, they should apply accurately at a cooling rate of 187°C/min. The same corrected temperatures are used for the bottom plot in Fig. 2A even though that cooling rate of 500°C/min far exceeds the calibration range. In this case, errors in the true temperature make no difference since no exothermic peaks were observed.
Thermal events in EAFS 10/10 during warming
In Fig. 1 of a recent paper [26], we published time-temperature curves for EAFS 10/10 samples in ¼ ml straws warmed at various rates after being cooled at 187°C/min to −196°C. The warming rates ranged from 139°C/min to 3280°C/min. The only thermal event observed was progressive melting of the solution above about −35°C. But since the data in the present Fig. 1 and Fig. 2A show that samples cooled 187°C/min undergo freezing and not vitrification, the results in Fig. 1 of the previous paper are to be expected.
We have now extended this somewhat. Fig. 2B shows warming DSC thermograms for EAFS 10/10 cooled and warmed at 37°C/min and cooled and warmed at 187°C/min. Only two peaks are observed, and both are endothermic. We believe that the low-temperature peak (Peak I) represents initial melting when the temperature rises above the eutectic point. The higher temperature peak (Peak II) represents standard progressive melting of the EAFS 10/10 as the temperature continues to rise above the eutectic point. There are no endotherms or exotherms at still lower temperatures that would be indicative of vitrification or devitrification. But then none would be expected, since as indicated by Fig. 2A, both these cooling rates (37°C/min and 187°C/min) resulted in EIF–not vitrification.
Instead, one needs to examine the thermal events during the slow warming of samples cooled rapidly enough for the medium to definitely vitrify; e.g., those cooled at 1827°C/min. This cooling rate is not achievable with our DSC-7. Consequently, our only option to achieve that high rate was to cool a column of EAFS 10/10 in a straw containing a thermocouple by plunging the straw directly into LN2.. When was done and followed by warming at a much lower rate (139°C/min), we examined the tresulting time-temperature plots for evidence of a Tg endotherm indicative of devitrification or a low-temperature exotherm indicative of crystallization. Neither were observed, possibly because the method is not sufficiently sensitivie.
Survival of oocytes in EAFS 10/10 vs. the cooling rate and warming rate
Fig. 3A plots the survival of the oocytes as a function of cooling rate with separate curves for each of the warming rates. The specific numerical values and the standard errors of this matrix are given in Table 3. The first point is that survival rises to a maximum with increasing cooling rate, and then either falls or plateaus with a further increase in cooling rate. For the four lowest warming rates, maximum survival occurs at a cooling rate of 187°C/min, which happens to be the rate used in Kasai et al’s standard “vitrification” procedure. The second point is that the numerical value of the maximum survival depends critically on the warming rate. The slower the warming, the lower is the maximum survival. For example, it is 70% for samples warmed at 2170°C/min but only 10% for samples warmed at 139°C/min. Furthermore, the overall pattern of survival rises with increasing warming rate. A third point is that when straws are warmed at the lowest rate used (139°C/min), survivals are only 0 to 10% irrespective of the cooling rate. Conversely, when straws are warmed at the highest rate used (2950°C/min), survivals exceed 65% irrespective of the cooling rate and they exceed 80% with cooling rates ≥ 187°C/min. The final point is that the EAFS 10/10 solution has undergone freezing at cooling rates of 37°C/min and 187°C/min but has apparently vitrified at the higher cooling rates. We see no effect on survival of whether the medium vitrified or not.
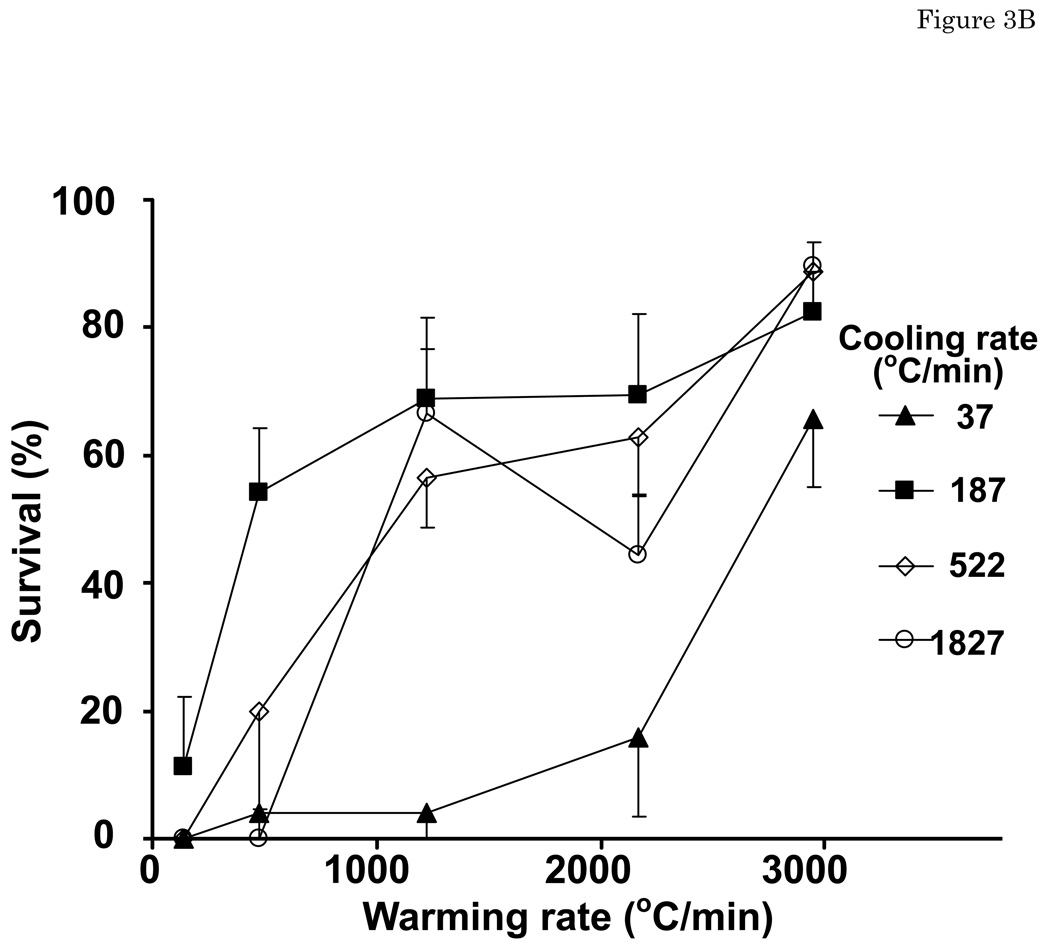
Fig. 3.
(A) The survival of EAFS 10/10-vitrified oocytes warmed at 139, 476, 1220, 2170, 2950 °C/min as a function of the cooling rate. (B) The survival of EAFS 10/10-vitrified oocytes cooled at 37, 187, 522, 1827°C/min as a function of the warming rate. The filled symbols depict conditions where the EAFS 10/10 solution froze; the open symbols depict where it vitrified.
Table 3.
Survival of mouse oocytes after cooling in EAFS10/10 to −196°C at each of four rates and warmed at each of five rates
| Warming rate | Cooling rate (°C/min) |
|||
|---|---|---|---|---|
| 37 | 187 | 522 | 1827 | |
| 139 | 0.0 ± 0.0 A, a | 11.1 ± 11.1 A, a | 0.0 ± 0.0 A, a | 0.0 ± 0.0 A,a |
| (0/15, N = 3) | (2/17, N = 6) | (0/15, N = 3) | (0/13, N = 3) | |
| 476 | 4.0 ± 4.0 A, a | 54.3 ± 9.9 B,ab | 20.0 ±15.5 AB, ab | 0.0 ± 0.0 A, a |
| (1/25, N = 5) | (12/21, N = 7) | (5/25, N = 5) | (0/25, N = 5) | |
| 1220 | 4.0 ± 4.0 A, a | 68.8 ± 12.8 B, b | 56.4 ± 7.5 B, bc | 66.7 ± 9.9 B,b |
| (1/25, N = 5) | (17/24, N = 7) | (31/53, N = 11) | (36/53, N = 12) | |
| 2170 | 15.8 ± 12.3 A, a | 69.4 ± 12.7 B,b | 62.9 ± 9.2 AB,c | 30.0 ± 14.1 AB,ab |
| (4/28, N = 6) | (14/21, N = 6) | (22/35, N = 7) | (17/39, N = 8) | |
| 2950 | 65.8 ± 10.7 A,b | 82.5 ± 6.3 * A,b | 88.9 ± 7.7 A,c | 89.6 ± 3.7 A,b |
| (24/38, N = 8) | (33/40, N = 8) | (27/31, N = 6) | (33/38, N = 6) | |
The data are % survival ± S.E.M. The first sets of ratios in parentheses are the ratios of the number of surviving oocytes to the number frozen or vitrified. N is the number of replicate straws.
Values with different superscripts were significantly different (P < 0.05) by one-way ANOVA. Capital letters shows the differences of survivals with the same warming rate and various cooling rate, and small letters shows those with various warming rates and the same cooling rate.
Dr. Kasai’s standard procedure.
Fig. 3B is a reciprocal plot of survival vs. warming rate with separate curves for each of the four cooling rates. It clearly illustrates the critical role played by the warming rate. With the highest warming rate (2950°C/min), survivals exceed 65% regardless of the cooling rate and regardless of whether a given cooling rate has resulted in the freezing or in the vitrification of the EAFS 10/10 solution. With the lowest warming rate (139°C/min), survivals are 0 to 10% regardless of the cooling rate and regardless of whether the medium has frozen or vitrified.
Discussion
Survival vs. the state of the medium and the state of the cells
In vitrification procedures, the assumption is that cell survival will be highest if the water in the cells and in the medium does not undergo ice formation. That is not the case in our experiments with respect to the medium; survival can be high independently of whether or not the medium freezes (Fig 3). It freezes with cooling rates of 37 and 187°C/min; it vitrifies with cooling rates > 500°C/min (522 and 1827°C/min). A cooling rate of 187°C/min is the standard rate used in Kasai’s and Edashige’s laboratories and ours for EAFS 10/10; yet, extracellular ice is formed in his procedure. We have no evidence on the relationship between cooling rate and whether the cells themselves undergo IIF or vitrify, although it could well be that cells will vitrify at lower rates than the medium due to the presence of high concentrations of macromolecules within them.
The dominant effect of warming rate on survival
With the partial exception of the lowest cooling rate of 37°C/min, survival depended almost entirely on the warming rate (Fig. 3B). The faster the warming the higher the survival. At the highest warming rate of 2950°C/min, survivals are above 80% at all cooling rates between 187–1827°C/min. They are almost 70% even with cooling rate of 37°C/min. This holds regardless of whether the medium vitrifies or freezes, and is contrary to the usual belief and to current efforts. Most current efforts are devoted to achieving very high cooling rate using open-pulled straws, cryoloops, and cryotops. Publications often include some discussion of the possible contribution of warming rate, but there have been few experimental attempts to separate the relative importance of each. Fortunately, devices that yield very high cooling rate also in general produce very high warming rate.
There are two published cases where the relative importance of high cooling rate and high warming rate has been assessed. One is in Drosophila eggs [14]. There, the percentages of 12 hr eggs that developed to the tracheal stage after rapid (110,000°C/min) or slow (74°C/min) cooling to −200°C was similar and relatively high (46 and 39%) if subsequent warming was rapid but was zero if the subsequent warming was slow (49°C/min). Another case is in mouse embryos. Rall [23] reported that the survival of mouse 8-cell embryos in several vitrification solutions was 80% or higher with cooling rates ranging from < 20°C/min to > 1,000°C/min when the embryos were warmed rapidly at 200 to 2,500°C/min but dropped off rapidly when the warming rate was lowered below 200°C/min.
In a recent paper, Jin et al [2] have examined the effect of warming rate and subzero hold temperatures on the survival of early mouse morulae subjected to a similar vitrification procedure to that used here. Aside from the difference in developmental stage, their experimental conditions were similar to some of ours. One difference is that the closest of their vitrification solutions to ours (EFS 20) lacks the 10.7% acetamide in EAFS10/10 but has double the concentration of EG. They used two cooling rates, which were basically our protocols 5 and 7 in Table 1 (They report cooling rates of 300 and 2,000°C/min, respectively vs. our values of 187°C/min and 1830°C/min.). They used two warming rates. In one, the straws were held in room temperature air as with our warming protocol 1 (Table 2). They estimate the warming rate to be 170°C/min; we found it to be 140°C/min. In their second, rapid, warming, procedure, the straws were immersed in water at 25°C. They estimate the warming rate to be 1,200°C/min; we found it to be 2,950°C/min (Table 2, protocol 5).
They found, as we have for oocytes, that the survival of the morulae was very sensitive to warming rate or to holds at intermediate subzero temperatures during warming. With rapid warming at 1,200°C/min, survivals were 60%; with slow warming at 170°C/min. they were 9%. If rapid warming from −196°C/min was interrupted by a 3 min hold at −80°C, −60°C, or −40°C, survival dropped to 0%. Their result for holding at −80°C is very different from ours. We find no drop in survival even after 60 hrs at −80°C.
What is the explanation for the relative lack of effect of cooling rate and the dominant effect of warming rate?
Although the cells do not undergo significant osmotic dehydration during cooling even at the lowest rate used (37°C/min) [16, Fig. 1.9], they have lost 72% of their initial water prior to “vitrification” as result of exposure to the hyperosmotic concentrations of the impermeable solutes in EAFS 10/10 (sucrose and Ficoll) [26]. The cell water can undergo two options during cooling: either it freezes or it vitrifies. If it freezes, the resulting crystals can be small or large. There are three options during warming: (1) if large intracellular ice crystals have formed during cooling, we expect survival to be near zero after warming independent of the warming rate. That is clearly not the case with our experiments. (2) If small intracellular ice crystals have formed during cooling, and if those crystals are small enough to be innocuous, we expect slow warming to be more damaging than rapid because slow warming allows time for recrystallization of ice. Recrystallization is the conversion of small ice crystals into large ones as a result of differences in surface free energy. For mouse oocytes in a 2 M EG/PBS solution we have determined that at −80°C it becomes first detectible in four hours as a slight intracellular blackening that increases progressively over the ensuing 24 hrs. The rate of darkening increases 5-fold with each 5°C rise in temperature [24,26]. Blackening to any extent is lethal, and thus slow warming would be expected to be lethal, which is the case. (3) If intracellular water has vitrified during cooling, it will first devitrify during warming when the temperature rises above the glass transformation temperature, Tg; i.e., it will convert from the glassy state back to a highly viscous supercooled state. Then at a slightly higher temperature, the viscous supercooled liquid will crystallize. The consequences of further warming will depend on the ice crystal size at this point and the rate of warming. If the crystals are small and the rate of warming is low, the crystals will grow by recrystallization with lethal results. If the crystals are small and warming is sufficiently rapid, recrystallization may be blocked, and the cells will survive. If the initial crystals are large, the rate of recrystallization will be greatly impeded, but the cells will have been irreversibly injured at that point irrespective of the subsequent warming rate.
In theory, (2) and (3) could be sharply distinguished calorimetrically. In (3), crystallization during warming should be accompanied by an exotherm slightly above Tg as latent heat is released during the conversion of supercooled liquid to ice. In practice, such measurements would be difficult because of the high concentration of cells required and because of the difficulty in distinguishing the thermal contributions of IIF from those of EIF.
Although a clear discrimination between (2) and (3) is not currently available, we believe the evidence favors (2), recrystallization, as the mechanism of death; First, while possible, it is difficult to believe that cellular vitrification occurs with a cooling rate of only 37°C/min. Second, we have found that oocytes subjected to Kasai’s optimum vitrification procedure in EAFS 10/10 show undiminished survival for at least one week at −80°C [26]. A temperature of −80°C is some 40°C above Tg, so if cells had vitrified during cooling, they should have devitrified during the hold. The fact that survival showed no diminution after holding at −80°C for up to a week means that devitrification (the conversion from a glass to a super viscous supercooled liquid) per se was harmless. However, during the hold one would also expect the supercooled cytoplasm to be converted to small ice crystals and, based on our data for oocytes in 2 M EG [26], one would expect these small crystals to recrystallize. The fact that survival was unaffected by the hold leads to the conclusion that, unlike oocytes in 2 M EG, recrystallization did not occur in oocytes in EFAS 10/10 at −80°C. Unfortunately, this conclusion can not be tested experimentally, because on the Linkam cryostage, the EAFS 10/10 solution is so opaque after EIF that one can barely discern the oocytes, much less determine whether they blacken.
Comments on survival
Our operational definition of a surviving cell has been a cell that exhibits normal morphology and normal osmotic response after experimental treatment and a subsequent 2–4 hours incubation in M16 medium.
In the 20 treatment sets in Table 3, there are three yielding survivals of 82–90% and four yielding survivals of 63 to 69% based on these criteria. What we do not know is whether these high survivals would prevail if survival were based on functional assays. In the case of the optimized procedure developed by Kasai which we have determined yields a cooling rate of 187°C/min and a warming rate of 2950°C/min, he has evidence that morphological and functional assays agree well. For that specific set of conditions, he has found that 84% of oocytes vitrified by his EAFS 10/10 procedure and then dezonated developed to the two-cell stage after in vitro fertilization, nearly equal to 89% for untreated controls (personal communication). On the other hand, in comparing survivals of bovine oocytes “vitrified” in open pulled straw and cryotops, Morató et al. [18] found that although immediate post-thaw or post-melting morphologies are similar, the percent developing to blastocyst differs considerably with the two techniques. Although we can not currently confirm that high survivals based on our post M16 incubation criterion equate with high functional survival, we can say with assurance that low survivals based on our criteria do equate with low functional survival.
We plan in the near future to initiate tests of the functional survivals of those conditions in the matrix in Table 3 that resulted in high survivals based in osmotic and morphological criteria.
We also do not know whether or not IIF occurs at the lower two cooling rate (37 and 187oC/min) that result in the freezing of the medium. It is quite possible that the cells themselves do vitrify, for they contain significant amounts of protein and other macromolecules that may act to enhance the glass forming ability of the intracellular EG and acetamide.
Decoupling of cooling and warming rates
As we have indicated, the emphasis of those who are pursuing the vitrification route to the cryopreservation of mouse and human oocytes is to achieve higher and higher cooling rates by the use of devices like cryoloops and cryotops that permit the manipulation of very small volumes of oocytes suspensions. Clearly, the underlying assumption of the users is that high survivals demand the avoidance of IIF during cooling by converting water to glass, and the higher the cooling rate, the more likely that conversion. Yet in two prior studies with 8-cell mouse embryos [23] and Drosophila embryos [14], now 23 and 15 years old, it was clearly shown that survivals after “vitrification” procedures depended on high warming rates–not on high cooling rates. That conclusion is now emphasized strongly in the present study involving mouse oocytes.
Each of the three studies involves different cell types and uses different vitrification solutions; consequently, we can’t yet be certain whether this dependence on warming rate is solution-dependent and whether it is cell-dependent. Our guess is that the former will be at most be secondarily so. Although differing in details, the many published vitrification solutions have in common that the solute concentrations exceed 6 M, that the media contain both permeating and nonpermeating solutes, and that the latter commonly include high concentrations of macromolecules like PVP or Ficoll. Pragmatically, in one sense, it is fortunate that the devices that are being used to achieve very high cooling rates also produce very high warming rates. Mechanistically, that has not been fortunate for it has resulted in confounding of whether cooling rate or warming rate are the important operatives. Furthermore, it is quite possible that the optimum cooling rate with respect to survival could be considerably lower than the very high cooling rates (>10,000°C/min) obtained with these devices. Nor has it been fortunate conceptually. If the primary cause of injury or death in a vitrification procedure is ice recrystallization during warming and not the failure to vitrify during cooling, the potential remedies may be quite different.
Acknowledgment
Reviewer #1 provided detailed comments on the manuscript indicating that he/she had read it carefully. The comments and suggestions were very helpful and we appreciate them.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain
Statement of funding: Research supported by National Institutes of Health grant R01-RR 18470
References
- 1.Gardner DK, Sheehan CB, Rienzi L, Katz-Jaffe M, Larman MG. Analysis of oocyte physiology to improve cryopreservation procedures. Theriogenology. 2007;67:64–72. doi: 10.1016/j.theriogenology.2006.09.012. [DOI] [PubMed] [Google Scholar]
- 2.Jin B, Kusanagi K, Ueda M, Seki S, Valdez DM, Jr, Edashige K, Kasai M. Formation of extracellular and intracellular ice during warming of vitrified mouse morulae and its effect on embryo survival. Cryobiology. 2008;56:233–240. doi: 10.1016/j.cryobiol.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 3.Karlsson JOM, Cravalho EG, Rinkes IHB, Tompkins RG, Yarmush ML, Toner M. Nucleation and growth of ice crystals inside cultured hepatocytes during freezing in the presence of dimethyl sulfoxide. Biophysical J. 1993;65:2524–2536. doi: 10.1016/S0006-3495(93)81319-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kasai M. Cryopreservation of mammalian embryos. Molecular Biotechnology. 1997;7:173–179. doi: 10.1007/BF02761753. [DOI] [PubMed] [Google Scholar]
- 5.Kasai M, Komi JH, Takakamo A, Tsudera H, Sakurai T, Machida T. A simple method for mouse embryo cryopreservation in a low toxicity vitrification solution, without appreciable loss of viability. J Reprod. Fertil. 1990;89:91–97. doi: 10.1530/jrf.0.0890091. [DOI] [PubMed] [Google Scholar]
- 6.Kasai M, Zhu SE, Pedro PB, Nakamura K, Sakurai T, Edashige K. Fracture damage of embryos and its prevention during vitrification and warming. Cryobiology. 1996;33:459–464. doi: 10.1006/cryo.1996.0046. [DOI] [PubMed] [Google Scholar]
- 7.Kleinhans FW, Guenther JF, Roberts DM, Mazur P. Analysis of intracellular ice nucleation in Xenopus oocytes by differential scanning calorimetry. Cryobiology. 2006;52:128–138. doi: 10.1016/j.cryobiol.2005.10.008. [DOI] [PubMed] [Google Scholar]
- 8.Kuwayama M. Highly efficient vitrification for cryopreservation of human oocytes and embryos: The Cryotop method. Theriogenology. 2007;67:73–80. doi: 10.1016/j.theriogenology.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 9.Kuwayama M, Vajta G, Kato O, Leibo SP. Highly efficient vitrification method for cryopreservation of human oocytes. Reproductive Biomedicine Online. 2005;11:300–308. doi: 10.1016/s1472-6483(10)60837-1. [DOI] [PubMed] [Google Scholar]
- 10.Landa V, Teplá O. Cryopreservation of mouse 8-cell embryos in microdrops. Folia Biol (Praha) 1990;36:153–158. [PubMed] [Google Scholar]
- 11.Lane M, Gardner DK. Vitrification of mouse oocytes using a nylon loop. Mol. Reprod. Develop. 2001;58:342–347. doi: 10.1002/1098-2795(200103)58:3<342::AID-MRD13>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 12.Martino A, Songsasen N, Leibo SP. Development into blastocysts of bovine oocytes cryopreserved by ultra-rapid cooling. Biol. Reprod. 1996;54:1059–1069. doi: 10.1095/biolreprod54.5.1059. [DOI] [PubMed] [Google Scholar]
- 13.Matsumoto H, Jiang JY, Tanaka T, Sasada H, Sato E. Vitrification of large quantities of immature bovine oocytes using nylon mesh. Cryobiology. 2001;42:139–144. doi: 10.1006/cryo.2001.2309. [DOI] [PubMed] [Google Scholar]
- 14.Mazur P, Cole KW, Schreuders PD, Mahowald AP. Contributions of cooling and warming rate and developmental stage to the survival of Drosophila embryos cooled to −205° C. Cryobiology. 1993;30:45–73. doi: 10.1006/cryo.1993.1006. [DOI] [PubMed] [Google Scholar]
- 15.Mazur P, Seki S, Pinn IL, Kleinhans FW, Edashige K. Extra- and intracellular ice formation in mouse oocytes. Cryobiology. 2005;51:29–53. doi: 10.1016/j.cryobiol.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 16.Mazur P. Principles of cryobiology. In: Fuller BJ, Lane N, Benson EE, editors. Life in the Frozen State. Boca Raton, FL: CRC Press; 2004. pp. 3–65. [Google Scholar]
- 17.Mazur P, Leibo SP, Seidel GE., Jr Cryopreservation of the germplasm of animals used in biological and medical research: Importance, impact, status, and future directions. Biology of Reproduction. 2008;78:2–12. doi: 10.1095/biolreprod.107.064113. [DOI] [PubMed] [Google Scholar]
- 18.Morató R, Izquierdo D, Paramio MT, Mogas T. Cryotops versus open-pulled straws (OPS) as carriers for the cryopreservation of bovine oocytes: Effects on spindle and chromosome configuration and embryo development. Cryobiology. 2008;57:137–141. doi: 10.1016/j.cryobiol.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 19.Papis K, Shimizu M, Izaike Y. A highly efficient modified vitrification method, for Day 3 in vitro produced bovine embryos. Cryo-Letters. 1999;20:203–206. [Google Scholar]
- 20.Pedro PB, Zhu SE, Makino N, Sakurai T, Edashige K, Kasai M. Effects of hypotonic stress on the survival of mouse oocytes and embryos at various stages. Cryobiology. 1997;35:150–158. doi: 10.1006/cryo.1997.2034. [DOI] [PubMed] [Google Scholar]
- 21.Pedro PB, Yokoyama E, Zhu SE, Yoshida N, Valdez DM, Jr, Tanaka M, Edashige K, Kasai M. Permeability of mouse oocytes and embryos at various developmental stages to five cryoprotectants. J. Reprod. Develop. 2005;51:235–246. doi: 10.1262/jrd.16079. [DOI] [PubMed] [Google Scholar]
- 22.Rall WF, Fahy GM. Ice-free cryopreservation of mouse embryos at −196°C by vitrification. Nature. 1985;313:573–575. doi: 10.1038/313573a0. [DOI] [PubMed] [Google Scholar]
- 23.Rall WF. Factors affecting the survival of mouse embryos cryopreserved by vitrification. Cryobiology. 1987;24:387–402. doi: 10.1016/0011-2240(87)90042-3. [DOI] [PubMed] [Google Scholar]
- 24.Seki S, Mazur P. Kinetics and activation energy of recrystallization of intracellular ice in mouse oocytes subjected to interrupted rapid cooling. Cryobiology. 2008;56:171–180. doi: 10.1016/j.cryobiol.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seki S, Kleinhans FW, Mazur P. Intracellular ice formation in yeast cells vs. cooling rate: Predictions from modeling vs. experimental observations by differential scanning calorimetry. Cryobiology. 2009;58:157–165. doi: 10.1016/j.cryobiol.2008.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Seki S, Mazur P. Effect of warming rate on the survival of vitrified mouse oocytes and on the recrystallization of intracellular ice. Biology of Reproduction. 2008;79:727–737. doi: 10.1095/biolreprod.108.069401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vajta G, Booth PJ, Holm P, Greve T, Callesen H. Successful vitrification of early stage bovine in vitro produced embryos with the open pulled straw (OPS) method. Cryo-Letters. 1997;18:191–195. [Google Scholar]