Abstract
Background
As the numbers of HIV-positive diagnoses rise in South Africa, it is important to understand the determinants and consequences of HIV disclosure.
Methods
Cross-sectional survey from random community samples of men and women in urban and rural South Africa (n = 217 HIV-positive individuals, 89% female).
Results
Two thirds of all known HIV-infected adults in these communities had disclosed their status to sexual partner(s). On average, individuals who disclosed were 2 years older, higher in socioeconomic assets, and had known their HIV status 7 months longer than those who had not told their sexual partner(s). The “need for privacy” was the most cited reason (45%) for nondisclosure among those who had never disclosed. People who eventually disclosed their HIV status to sexual partner(s) were significantly more likely to report always or more frequently using condoms, reducing their number of sexual partners, and/or becoming monogamous. Among individuals who disclosed their HIV status, 77% reported increases in social support, with families providing the most support.
Conclusions
Disclosure is associated with reports of consequent safer sexual behavior and greater social support. Interventions might be informed by the costs and benefits of disclosure and differences in disclosure to sexual partner vs. to one’s social network.
Keywords: AIDS, behavior change, community sample, disclosure, HIV, social support, South Africa
South Africa has the most people living with HIV/AIDS in the world, with an HIV prevalence of nearly 20% among adults aged 15–49 years or an estimated 5.3 million infected individuals.1,2 Young people are at greatest risk for HIV infection, but it is estimated that less than one third of adults over age 15 have ever tested for HIV.3 Furthermore, young women (aged 15–24 years) are biologically and socially more vulnerable to HIV infections and are 4 times more likely to be HIV infected than are young men.3 One way to reduce the spread of HIV may be to encourage infected individuals to communicate their disease status to their sexual partner(s). Disclosure may reduce the transmission of HIV by raising awareness and decreasing risky behavior.4,5 However, not all South Africans share their diagnosis with others, and thus, to plan effective public programing and policy, it is important to determine the factors that influence an individual’s decision to disclose their HIV-positive status.6
Although disclosing sensitive information like HIV status has potential risks, such as abandonment, physical violence, or feelings of shame, worry, fear, or rejection,5 there are also several important advantages to disclosure. Disclosure may enable HIV-positive individuals to gain access to appropriate treatment, motivate them to change risky behavior patterns, and encourage their sexual partners to seek information and testing.4,7 Moreover, disclosure may increase opportunities to receive social support, which may help individuals cope and recover from physical illness, and attenuate depressive symptomology due to HIV-related physical symptoms.8–10
Historically, the majority of research on HIV disclosure has been conducted in AIDS populations in the United States.11 The limited research on disclosure in South Africa typically utilizes samples of convenience, such as pregnant women attending antenatal clinics or individuals sampled from HIV clinics,6,12–14 thus limiting the ability to describe effects in the wider community. The present study is the first, to our knowledge, to examine HIV disclosure in South Africa using a large randomly selected community sample of South African men and women. Data were gathered from Project Accept, a National Institute of Health–funded multicountry, randomized, and controlled HIV prevention trial in urban and rural South Africa.15 The urban site, Soweto, is a culturally diverse township of 2–3 million people located 15 km south of Johannesburg. In contrast, the rural site, Vulindlela, is in the KwaZulu-Natal region with approximately 40,000 residents and has a strong Zulu culture. The present study involved a one-time population-based survey conducted by Project Accept in 2003. The purpose of the present study was 3-fold: (1) to examine the factors associated with the decision to disclose, (2) to identify reasons for nondisclosure, and (3) to describe the consequences of disclosure of stigmatized test results in the context of South Africa.
METHODS
Design and Procedure
The present study employed a cross-sectional observational design, utilizing structured interviews conducted as part of baseline data for Project Accept (B. L. Genberg, M. Kulich, S. Kawichai, et al, unpublished data). A multistage sampling strategy began with complete household enumeration of 16 South African communities within 2 general regions, Soweto and Vulindlela, both chosen because of their high HIV prevalence and to represent urban and rural populations, respectively. Households were randomly selected, interviewers enumerated all persons in the household, and 1 household member between 18 and 32 years of age was randomly selected to be approached for the interview. Consenting participants were interviewed in the local language by trained community interviewers using a standardized protocol regarding topics such as participant demographics, sexual risk behaviors, HIV testing history, perceptions of HIV/AIDS stigma, and disclosure of HIV status. The overall response rate was high for both sites, 84.7% in Vulindlela and 84.5% in Soweto. Further details on the procedures of the Project Accept study are elaborated by B. L. Genberg, M. Kulich, S. Kawichai, et al.16
Measures
Measures of HIV Disclosure
The present study measured 2 primary forms of HIV disclosure as dependent variables: sex partner disclosure and network disclosure. We assessed sex partner disclosure as whether or not an HIV-positive individual reported disclosing their HIV status to their sexual partner (defined as a spouse, boy/girlfriend, casual partner, and/or commercial sex worker). To measure our second variable, network disclosure, we asked all participants in the study if they had disclosed their HIV-positive status to someone in any of the following 10 relationship categories: spouse, boy/girlfriend, casual partner, commercial sex worker, immediate family (parent, child, sibling, etc.), other relatives (aunt, uncle, cousins, etc.), friend, health practitioner, religious leader, or employer. Network disclosure was calculated by counting the number of relationship categories (of 10 possible) to which an HIV-positive individual disclosed their HIV status, demonstrating the more people that an individual discloses to, the more diverse their network.
Individual Background
Gender and age in years were included in the interview. Those individuals from Soweto were considered urban and those from Vulindlela were considered rural. Participants were classified “high” in socioeconomic assets if they owned a car; “medium” if they did not own a car but owned at least 2 of the following: drinking water in the house, refrigerator, or cellular phone; and “low” if they did not own any of the aforementioned assets.
HIV/AIDS Stigma Perception
A stigma scale was piloted and developed for Project Accept by Genberg et al.17 Twenty-one stigma items were rated on a 5-point Likert scale (1 = strongly disagree; 5 = strongly agree) with higher scores indicating higher perceptions of stigma. The measure of stigma was divided into 3 following subtypes: discrimination, defined as perceptions of discrimination HIV-positive individuals and their families faced in the community (7 questions, α = 0.80); shame, blame, and social isolation, defined as the devaluation, disgrace, and culpability attributed to HIV-positive individuals (9 questions, α = 0.77); and equity, characterized as the freedoms and rights HIV-positive individual have in the community (5 questions, α = 0.58).
Disease Progression
HIV Symptomatology was a dichotomous variable defined as whether or not the respondent stated that exhibiting HIV symptoms was a reason for seeking HIV testing. The time since diagnosis variable was calculated as the time in months between HIV diagnosis and the date of the interview.
Reasons for Nondisclosure
If individuals had not yet disclosed their HIV status to anyone, they were asked to choose as many reasons as applicable from the following: fear of rejection, fear of physical abuse, or because HIV is a private and personal matter.
Behavior Change as a Result of Disclosure
Participants were asked whether or not they took precautionary steps to protect against HIV transmission after testing and after disclosing their HIV status. Participants were asked to recall if they made the following sexual behavior changes posttest and postdisclosure: abstained from sex, always used condoms, used condoms more frequently, changed the way they selected sexual partners, limited the total number of sexual partners, or became monogamous.
Behavior change was analyzed in 2 ways. First, a between-subjects comparison was made between individuals who eventually disclosed to their sexual partner, and those who never told their sexual partner, on the types of behavior changes they made after testing (n = 210). Through this comparison, we were looking to see if individuals who eventually disclosed to their sexual partner differed in sexual behavior post-HIV test, compared with those who never disclosed. Second, we conducted a within-subjects comparison of individuals who chose to disclose to their sexual partners (n = 138), examining the responses given by respondents to questions of behavior change in 2 following contexts: (1) after they tested positive for HIV and (2) after they disclosed their status to a sexual partner. Thus, the study sought to examine whether disclosure had a unique effect on behavior change, over and above simply having been tested.
Perceived Social Support as a Result of Disclosure
We recorded the relationship between the HIV-positive person and the confidant of the HIV status disclosure (see network disclosure for the list of 10 relationship categories). If the participant stated that they had disclosed to a person in a particular relationship category, they were asked whether they received less, the same, or more support than before they disclosed.
RESULTS
To explore the correlates of HIV disclosure on sexual partner and network disclosure, logistic and Poisson regressions were used, respectively. Univariate analysis of the impact of the predicted correlates on sexual partner disclosure was further examined using t test for normally distributed continuous variables and χ2 tests for categorical variables. Behavioral change variables were categorical in nature and thus were analyzed using χ2 tests.
Description of HIV-Positive Sample
Table 1 shows the demographic characteristics of the sample, which included 215 HIV-positive individuals from Soweto (46%, n = 99) and Vulindlela (54%, n = 115). One individual did not specify whether he/she was from Vulindlela or Soweto. Two HIV-positive individuals were excluded from the analysis because of extensive missing data, leading to a final sample size of 215. Participants were an average age of 27 years (SD = 4, ranging from 18 to 32 years), 84% were single or never married, and 83% had 1 or more children in the household. A total of 77% of participants currently had a sexual partner and of those with sexual partners, 22% were cohabiting. Thus, our sample is consistent with a previous study which reported that a significant proportion of South Africans are unmarried but have sexual partners with whom they may have children.18 These women often support themselves through informal work, housekeeping, or from boyfriends. Although 72% of women had more than 11 years of education, most were unemployed (70%), a disparity that is typical of South Africa. On average, respondents had received their HIV-positive test results approximately 13 months (SD = 12.7) before the date of the interview, and approximately 42% of participants had known about their HIV status for at least 1 year. Comparing our sample of HIV-positive individuals to the larger community of HIV-negative or nontested individuals, HIV-positive individuals were more likely to be female (89% HIV positive vs. 55% in the general sample), from a rural area (54% vs. 43%), of lower socioeconomic assets (36% low vs. 26% low), and currently unemployed (70% vs. 41%).
TABLE 1.
Characteristics of HIV-Positive Individuals in Soweto and Vulindlela, South Africa (n = 215)
| Percentages | n | |
|---|---|---|
| Female | 89 | 192 |
| Married | 14 | 31 |
| Currently have a sexual partner | 77 | 166 |
| Cohabiting with sexual partner | 22 | 36 |
| Living in an urban environment (Soweto) | 46 | 99 |
| Socioeconomic assets | ||
| Low | 36 | 78 |
| Medium | 52 | 112 |
| High | 12 | 25 |
| Highest level of education, yr | ||
| <7 | 8 | 18 |
| 8–10 | 20 | 42 |
| 11+ | 72 | 155 |
| Number of children in household | ||
| 0 | 17 | 37 |
| 1–2 | 54 | 116 |
| 3+ | 30 | 62 |
| Employment | ||
| Yes | 25 | 54 |
| No | 70 | 151 |
| Student | 5 | 9 |
Rates of HIV Disclosure
Most HIV-positive individuals (87%) disclosed their status to at least 1 person, but 13% reported that they had never disclosed their HIV status to anyone. Of those who disclosed, the majority (93%) disclosed to boy or girlfriends, 77% to family member, 59% to spouses, and 58% to health care professionals (Table 2). A total of 77 (36%) individuals did not disclose their HIV status to their sexual partners (if any) when they received their HIV diagnosis (due to the wording of the question regarding disclosure to sexual partners, we were unable to distinguish between individuals who did not disclose because they did not have a sexual partner to tell and those who had a sexual partner but chose not to disclose). HIV-positive individuals who disclosed their status did so to an average of 2.8 of 10 possible relationship categories (SD = 1.8) or on average to 42% (SD = 21.9) of the relationship categories in their available network. Of the 10 possible relationship categories, approximately 12% of individuals told at least 1 person, 23% told 2, 17% told 3, 17% told 4, and 18% told 5 or more categories of relationships.
TABLE 2.
Percentages of Disclosure to 10 Potential Relationship Categories and Changes in Social Support After Disclosure*
| Disclosed |
Social Support |
|||
|---|---|---|---|---|
| Categories of Relationships | Yes % (n) | More % (n) | Same % (n) | Less % (n) |
| Spouse | 59 (20/34) | 55 (11) | 20 (4) | 25 (5) |
| Boy/girlfriend | 93 (117/126) | 64 (71) | 25 (28) | 11 (12) |
| Casual partner | 14 (6/43) | 80 (4) | 0 | 20 (1) |
| Commercial sex worker | 0 (0/32) | 0 | 0 | 0 |
| Family | 77 (145/189) | 81 (118) | 14 (21) | 4 (6) |
| Other relatives | 38 (71/189) | 75 (53) | 23 (16) | 3 (2) |
| Friend | 49 (89/182) | 84 (74) | 14 (12) | 2 (2) |
| Health care professional | 58 (109/189) | 83 (90) | 16 (17) | 1 (1) |
| Religious leader | 13 (23/173) | 83 (19) | 17 (4) | 0 |
| Employer | 4 (3/70) | 75 (3) | 25 (1) | 0 |
| Overall Support | — | 77 (443) | 18 (103) | 5 (29) |
There are discrepancies in the number of individuals who answered the question on disclosure and those who answered questions on social support. For unknown reasons, some individuals did not choose to answer the support questions, leading to lower frequencies on these questions.
Correlates of Disclosure
Disclosure to Sexual Partner
To determine the correlates of HIV disclosure to sexual partner, we conducted a logistic regression using the dichotomous variable sex partner disclosure as the dependent variable and age, socioeconomic assets, gender, rural/urban setting, shame/blame/social isolation, discrimination, equity, HIV symptomology, and time since diagnosis as predictors (Table 3). The logistic regression was statistically significant, P < 0.001, with an R2 of 0.13 for Cox and Snell and 0.18 for Nagelkerk. We found that disclosure to sexual partner was significantly related to older age (β = 0.09), and a χ2 test confirmed that individuals who had disclosed to their sexual partner were significantly older (M = 27.5, SD = 3.8) than those who did not disclose to their sexual partner (M = 25.8, SD = 4.3), P < 0.01. Second, disclosure to sexual partner was related to higher socioeconomic assets (β = 0.55). Individuals who did not disclose their HIV status tended to be low in socioeconomic assets with 49% considered low, 42% medium, and only 8% in the high socioeconomic assets brackets. In contrast, individuals who did disclose their HIV status tended to be of medium socioeconomic status (29% low, 58% medium, and 14% of high socioeconomic assets). Third, a longer time since diagnosis was related to disclosure to sexual partner (β = 0.04). Of those individuals who did disclose to their sex partner (64% of all HIV-positive individuals), the average time gap was 16 months. In contrast, of those who did not disclose to their sex partner (36% of all HIV-positive individuals), the average length of time since diagnoses was 9 months, P < 0.01.
TABLE 3.
Logistic Regression of Sexual Partner Disclosure With the 9 Predicted Correlates (n = 215)
| Variable | Beta (SE) | OR | 95% CI |
|---|---|---|---|
| Age | −0.09 (0.04)* | 1.10 | 1.02 to 1.18 |
| Gender | −0.19 (0.53) | 0.83 | 0.29 to 2.35 |
| Socioeconomic assets | 0.55 (0.26)* | 1.73 | 1.03 to 2.90 |
| Rural environment | −0.22 (0.34) | 0.80 | 0.41 to 1.57 |
| Shame, blame, social isolation | −0.04 (0.49) | 0.96 | 0.37 to 2.52 |
| Discrimination | 0.34 (0.21)† | 1.41 | 0.93 to 2.14 |
| Equity | −0.10 (0.38) | 0.90 | 0.43 to 1.91 |
| Time since diagnosis | 0.04 (0.02)* | 1.04 | 1.01 to 1.07 |
| HIV symptomotology | −0.51 (0.35) | 0.60 | 0.30 to 1.20 |
CI, confidence interval; OR, odds ratio.
P < 0.05 (2-tailed test).
P < 0.10.
Network Disclosure
To determine the correlates of network disclosure, a Poisson regression model was used and was statistically significant with likelihood ratio, P < 0.001. For this analysis, we examined how all participants in the sample disclosed to their social network by looking at 9 predicted correlates (Table 4). Living in an urban region (β = −0.21) was associated with more diverse network disclosure. Individuals living in a rural environment disclosed to fewer relationship categories (M = 2.46, SD = 1.55) than individuals from urban environments (M = 3.17, SD = 2.03). Furthermore, a χ2 test revealed that individuals in Soweto (urban) disclosed significantly more often to their sexual partner (72%) than individuals in Vulindlela (rural), who only disclosed to their sexual partner 57% of the time, P < 0.05. Second, discrimination (β = 0.11) was significantly correlated with network disclosure, indicating that disclosure to more categories of people in one’s social network was related to higher levels of perceived discrimination in the community, P < 0.05. Finally, testing for HIV because of HIV symptoms (β = 0.20) was significantly correlated with disclosing to more relationship categories in one’s social network, P < 0.05. Gender was not significantly related to either sexual partner disclosure or network disclosure.
TABLE 4.
Poisson Regression for Network Disclosure With the 9 Predicted Correlates (n = 215)
| Variable | Beta (SE) | 95% CI |
|---|---|---|
| Age | 0.01 (0.01) | −0.01 to 0.03 |
| Gender | 0.03 (0.13) | −0.24 to 0.29 |
| Socioeconomic assets | 0.07 (0.07) | −0.06 to 0.21 |
| Rural environment | −0.21 (0.09)* | −0.39 to −0.03 |
| Shame, blame, social isolation | 0.03 (0.13) | −0.23 to 0.28 |
| Discrimination | 0.11 (0.05)* | 0.00 to 0.22 |
| Equity | −0.07 (0.10) | −0.27 to 0.28 |
| Time since diagnosis | 0 (0) | −0.01 to 0.01 |
| HIV symptomotology | 0.21 (0.09)* | 0.02 to 0.39 |
CI, confidence interval.
P < 0.05 (2-tailed test).
Reasons for Nondisclosure
We examined several reasons why individuals (n = 20) never disclosed their HIV status. The most cited reason for nondisclosure was the need for privacy, with 45% of individuals who had never disclosed, noting this as a reason why they never revealed their HIV status. Fear of rejection was cited 15% of the time and fear of physical abuse 10% of the time.
Outcomes of Disclosure
Behavior change as a result of disclosure. After disclosure, the majority (82%) of participants asked their partner to get tested. The most frequent change in sexual behavior with regard to safer sexual interactions was that 81% of participants decided to have sex with only 1 partner, followed by using condoms during every sexual interaction (64%), using condoms more often (59%), reducing the number of sexual partners (56%), changing partner selection (54%), and abstaining from sex (20%).
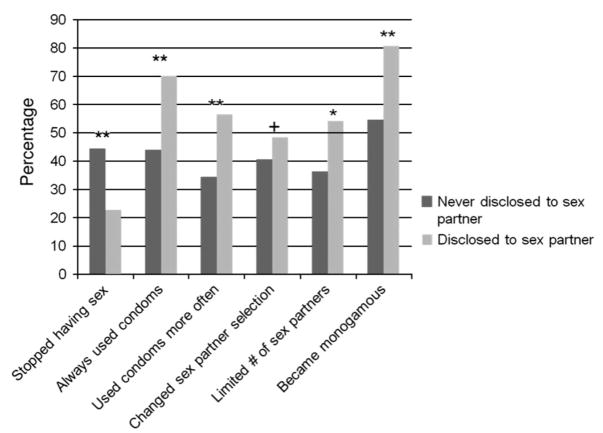
In the first set of behavior change analysis, we conducted a between-subjects χ2 test to compare the sexual behavior change of individuals who did and did not disclose with a sexual partner after receiving their HIV-positive diagnosis (Fig. 1). Results indicated that people who eventually told their sexual partner their HIV status were significantly more likely to report that they always used a condom (P < 0.001), used a condom more often (P < 0.01), limited their number of sexual partners (P < 0.05), and/or became monogamous (P < 0.001), compared with those who never told their partner. However, people who never disclosed their status were more likely to abstain from having sex than individuals who disclosed their status to their sexual partners (P < 0.001). On average, individuals who eventually told their partner made more positive behavior changes (M = 2.8/6, SD = 1.5) after receiving their HIV test results compared with those who never disclosed to their sexual partner (M = 2/6, SD = 1.6). In addition, we conducted a within-subjects χ2 test of how posttest sexual behavior differed from postdisclosure sexual behavior among people who disclosed to their sexual partner. We found that although none of the changes from post-HIV test to postdisclosure showed statistically significant change, in 4 of 6 behavior change categories, individuals who made any changes in their behavior made positive changes.
FIGURE 1.
The χ2 test of post-HIV test behavior change comparing individuals who disclosed to their partner vs. those who never disclosed. +P, 0.10, *P, 0.05, **P, 0.01 (2-tailed tests).
Perceived Social Support as a Result of Disclosure
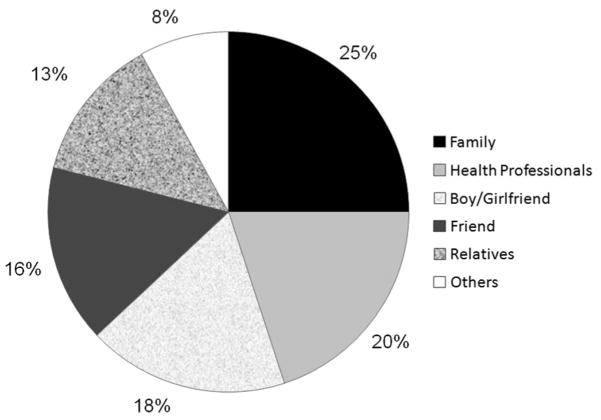
Social support was measured for 10 possible relationship categories in an individual’s social network (Table 2). For all relationships, the majority of individuals reported receiving more support after disclosing their HIV status (77% of all types of support given) as opposed to the same amount of support (18%) or less support (5%). We were interested in which social network members were providing the most amount of support to the majority of the HIV-positive individuals in our sample. Participants were allowed to choose multiple support sources of the 10 relationship categories. In both rural and urban areas, immediate families were the greatest source of support with 25% of all support being provided by families. Doctors were reported to be supportive for 20% of individuals, boy/girlfriends supported 18%, and friends supported 16% of HIV-positive individuals (Fig. 2).
FIGURE 2.
Total amount of support (in percentages) provided to HIV-positive individuals by members of their social networks (n = 215). Participants had the option of choosing multiple sources of support (range 0–6). The category “other” incorporated casual partners, spouse, commercial sex worker, religious leader, and employer.
For each relationship category, we examined whether the support provided had increased, decreased, or remained the same after disclosure. The greatest increase in support was reported as received by friends (84%), followed closely by doctors (83%), religious leaders (83%), family members (81%), and other relatives (75%). Interestingly, respondents reported less increase in social support from sexual partners such as boy/girlfriends (64%) and spouses (55%). Indeed, sexual partners in general were more likely to decrease their social support for the HIV-positive individual, with spouses decreasing support 25% and boy/girlfriends decreasing support 11% of the time, as opposed to nonsexual relationships where decreases in support averaged only 3%.
DISCUSSION
On average, the majority of HIV-positive individuals in both the urban and rural settings disclosed their status to at least 1 person. Yet, of those who tested positive, 13% of the respondents in our sample had never disclosed their HIV test results to anyone. Furthermore, more than one third of all HIV-infected adults never disclosed to their sexual partners. We found that patterns of disclosure differed for sexual partners vs. network disclosure. Paralleling previous research mainly conducted in the United States, being older,19,20 having higher socioeconomic assets,21 and longer time since diagnosis21,22 were associated with sexual partner disclosure. In comparison, disclosure to one’s social network was associated with living in an urban rather than rural area, HIV symptomology, and greater perceptions of discrimination in the community.
The most common reason individuals did not share their HIV status, cited about half the time, was out of desire for privacy—a finding consistent with current US literature on nondisclosure.23 Our finding that only 64% of individuals disclosed to their sexual partners was similar to a sample of men and women attending a clinic in Soweto (62%)24 but is lower than rates of disclosure to sexual partners found in Cape Town (78%)12 and Johannesburg (79%).14 This may indicate that studies of clinical populations may overestimate levels of disclosure compared with community-based estimates or that clinical populations disclose more often.
Our results indicate that sexual behavior differs between disclosers and nondisclosers, such that disclosers were more likely to make positive sexual behavior changes after testing positive for HIV. In addition, disclosure had a small but unique and positive effect on individual’s sexual behavior, above and beyond the effects of testing for HIV. Because the heart of promoting HIV disclosure lies in the hope that it will be associated with less sexually risky behavior, these findings suggest that disclosing to others may not only lead to safer outcomes after HIV testing but also safer health behaviors after disclosure. Furthermore, consistent with previous research in Africa, we were encouraged to find that a large majority of HIV-positive individuals asked their sexual partners to test for HIV.25
The majority of HIV-positive individuals reported receiving more social support after disclosure, which is important, given the negative stigma surrounding the disease. Social support has been linked to many positive outcomes such as buffering psychological and emotional distress,26–28 promoting more adaptive HIV coping strategies such as spiritual resilience and community involvement,29 and even positive effects on the immune system, which in turn influence mortality risk and survival.30–32 However, in our sample, 13% of individuals who disclosed to their sexual partners were met with less support. Because decreases in social support may have tangible effects on quality of life and disease trajectory, further research is needed to specify the reasons why these individuals received less support.
Families provided the greatest overall amount of support and community members such as friends or doctors showed the most increases in social support after disclosure, especially compared with sexual partners. This finding is consistent with further analysis we conducted, indicating that family disclosure was related to experiencing HIV symptomology (marginally significant) and age (significant). Given that young people are more likely to be living at home, it was not surprising that being younger was significantly associated with family disclosure. Furthermore, as individuals grow sicker and their disease progressed, they were more likely to disclose to their families and in turn depend on them for social support.33 Considering the centrally supportive role of the family, interventions could focus on strengthening their capacity, for example, by teaching skills for coping with AIDS stigma and training on caregiving.
When identifying the factors associated with HIV disclosure, our findings demonstrate the importance of considering the level of analysis. Results indicated that individual-level factors were influential for sexual partner compared with community-level factors for network disclosure. Regarding disclosure to sexual partners, younger, poorer, and more recently diagnosed individuals were less likely to disclose their HIV status. Unfortunately, the young and poor populations are already likely to be at high risk for transmission and thus are in even greater danger because they are less likely to disclose their HIV status. Thus, HIV interventions would need to consider nondisclosure as a potential additional risk factor for this high-risk population.
Our findings on network disclosure may be beneficial in developing targeted interventions by focusing on community-level variables such as perceived community labeling, gossiping, and stigma that occurs in more rural settings. In smaller, tight-knit rural communities, strong social ties facilitate the flow of social information, such that when individuals disclose their HIV status, an entire community may be privy to the information. In contrast, the large and anonymous nature of the urban environment may stifle this communication flow. This may explain in part why individuals may be more likely to disclose in an urban setting, as there would be less opportunity for stigma and social isolation. Furthermore, given that rural environments often have limited options for medical treatment, individuals may not see any additional benefits from disclosure to a wider network.
The association between higher perceptions of discrimination and lower levels of network disclosure confirms that HIV is more than an infection of the body, but often leads to detrimental social victimization (given the cross-sectional nature of the dataset, the direction of causality between discrimination and network disclosure cannot be known. However, we argue that it is highly unlikely that discrimination leads to network disclosure, rather that network disclosure contributes to higher perceptions of discrimination).34 Ndinda et al31 found that although South African community members knew how to treat HIV-positive individuals, often their actual treatment was quite stigmatizing. Thus, given our finding that HIV disclosure can lead to important benefits such as increased social support and reduced risky behavior, HIV interventions that are encouraging disclosure must recognize the potential stigmatizing cost of disclosure and help prepare HIV-positive individuals to cope with any negative consequences.
Women are both disproportionately infected and bear the burden of caring for HIV-infected persons.35 This reality is reflected in our sample, with over 8 times as many women as men reporting to be HIV positive. Surprisingly, although the majority of HIV-positive individuals in the sample were women, gender was not significantly associated with either sex partner or network disclosure. Because the number of men in the present study was low, it is difficult to draw definitive conclusions on gender differences. Random sampling studies including more HIV-positive South African men would help to clarify the effect of gender.
The current study has several important strengths. In contrast to most research in this area, which has focused on clinical HIV populations, the present study used data collected from randomized probability samples of community members, thus allowing for a greater representativeness and generalizability of findings. In addition, this study included data from both rural and urban areas, allowing for comparisons and insight into ways that interventions may be targeted for each area. Yet, a few limitations of the current research should be addressed. To better grasp the complex factors that influence the decision to test and disclose, additional questions should be included in future studies, such as assessments of behavioral intention, length of partner relationship, time since disclosure, partner reaction to disclosure, type of social support (instrumental, emotional, informational, etc.), and the HIV status of the sexual partner or other network members who were informed. In addition, the baseline dataset used for this study did not involve actual HIV testing; rather retrospective self-reported HIV status was used which may have led to underreporting. Because disclosure is a process rather than an event that occurs at 1 point in time, 1 potential follow-up to the current study would be to investigate disclosure from a longitudinal perspective.
CONCLUSIONS
The decision to disclose one’s HIV diagnosis is a difficult and often stressful process because the potential costs of disclosure, such as social stigma and burden on others, must be weighed against potential benefits, such as social support and reduced risky sexual behavior.23 The present findings suggest that HIV disclosure may mediate reduced risk. However, future studies of disclosure must focus on the larger social and cultural context of HIV prevention.36 Nonetheless, the present study identified some of the factors that facilitate and hinder disclosure of HIV status, which may inform interventions for increasing testing and disclosure in South Africa, thus helping to reduce the spread and transmission of HIV. Furthermore, public education efforts and public health care providers may profit from gaining further insight on the costs and benefits of disclosure. As the HIV epidemic continues to rise in the South African population, it will become all the more important to develop effective interventions to assist HIV-positive individuals in disease disclosure decisions and sexual risk reduction.
Acknowledgments
Acknowledgment is due to the US National Institute of Mental Health who funded Project Accept and to the University of California, Los Angeles AIDS Institute and National Science Foundation who provided funding for the present study. We thank the communities that partnered with us in conducting this research and all study participants for their contributions. We also thank Project Accept study staff and volunteers at all participating institutions for their work and dedication.
Supported by the US National Institute of Mental Health as a cooperative agreement, through contracts U01MH066687 (Johns Hopkins University), U01MH066688 (Medical University of South Carolina), U01MH066701 [University of California, Los Angeles (UCLA)], and U01MH066702 (University of California, San Francisco). In addition, this work was supported by the HIV Prevention Trials Network (HPTN Protocol 043) of the Division of AIDS of the US National Institute of Allergy and Infectious Diseases and by the Office of AIDS Research of the US National Institutes of Health. In addition, L.H.W. was supported by a Graduate Research Fellowship Award from the National Science Foundation and a seed grant from the UCLA AIDS Institute and the UCLA Center for AIDS Research (AI28697).
Footnotes
Presented in part at Center for HIV Identification, Prevention and Treatment Services HIV Research: The Next Generation, April 7, 2008, Los Angeles, CA, and at Unite for Sight Conference, April 12–14, 2008, New Haven, CT.
Views expressed are those of the authors and not necessarily those of sponsoring agencies.
References
- 1.United Nations Programme on HIV/AIDS. AIDS Epidemic Update. Geneva, Switzerland: United Nations Programme on HIV/AIDS; 2007. [Google Scholar]
- 2.United Nations Programme on HIV/AIDS. Report on the Global AIDS Epidemic. Geneva, Switzerland: United Nations Programme on HIV/AIDS; 2006. [Google Scholar]
- 3.Shisana O, Rehle T, Simbayi L, et al. South African national HIV prevalence, HIV incidence, behaviour and communication survey. Cape Town, South Africa: Human Sciences Research Council; Published 2005. [Google Scholar]
- 4.Medley A, Garcia-Moreno C, McGill S, et al. Rates, barriers and outcomes of HIV serostatus disclosure among women in developing countries: implications for prevention of mother-to-child transmission programmes. Bull World Health Organ. 2004;82:299–307. [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Gender Dimensions of HIV Status Disclosure to Sexual Partners: Rates, Barriers and Outcomes: A Review Paper. Geneva, Switzerland: World Health Organization; 2004. [Google Scholar]
- 6.Norman A, Chopra M, Kadiyala S. Factors related to HIV disclosure in 2 South African communities. Am J Public Health. 2007;97:1775–1781. doi: 10.2105/AJPH.2005.082511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Serovich JM. A test of two HIV disclosure theories. AIDS Educ Prev. 2001;13:355–364. doi: 10.1521/aeap.13.4.355.21424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cohen S. Psychosocial models of the role of social support in the etiology of physical disease. Health Psychol. 1988;7:269–297. doi: 10.1037//0278-6133.7.3.269. [DOI] [PubMed] [Google Scholar]
- 9.Hays RB, Turner H, Coates TJ. Social support, AIDS-related symptoms, and depression among gay men. J Consult Clin Psychol. 1992;60:463–469. doi: 10.1037//0022-006x.60.3.463. [DOI] [PubMed] [Google Scholar]
- 10.Waddell EN, Messeri PA. Social support, disclosure, and use of antiretroviral therapy. AIDS Behav. 2006;10:263–272. doi: 10.1007/s10461-005-9042-x. [DOI] [PubMed] [Google Scholar]
- 11.Greene K, Derlega VJ, Yep GA, et al. Privacy and Disclosure of HIV in Interpersonal Relationships: A Sourcebook for Researchers and Practitioners. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; 2003. [Google Scholar]
- 12.Olley BO, Seedat S, Stein DJ. Self-disclosure of HIV serostatus in recently diagnosed patients with HIV in South Africa. Afr J Reprod Health. 2004;8:71–76. [PubMed] [Google Scholar]
- 13.Simbayi LC, Kalichman SC, Strebel A, et al. Disclosure of HIV status to sex partners and sexual risk behaviours among HIV-positive men and women, Cape Town, South Africa. Sex Transm Infect. 2007;83:29–34. doi: 10.1136/sti.2006.019893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Skogmar S, Shakely D, Lans M, et al. Effect of antiretroviral treatment and counselling on disclosure of HIV-serostatus in Johannesburg, South Africa. AIDS Care. 2006;18:725–730. doi: 10.1080/09540120500307248. [DOI] [PubMed] [Google Scholar]
- 15.Khumalo-Sakutukwa G, Morin SF, Fritz K, et al. Project Accept (HPTN 043): a community-based intervention to reduce HIV incidence in populations at risk for HIV in sub-Saharan Africa and Thailand. J Acquir Immune Defic Syndr. 2008;49:422–431. doi: 10.1097/QAI.0b013e31818a6cb5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Genberg BL, Kulich M, Kawichai S, et al. HIV risk behaviors in sub-Saharan Africa and Northern Thailand: baseline behavioral data from Project Accept. J Acquir Immune Defic Syndr. 2008;49:309–319. doi: 10.1097/QAI.0b013e3181893ed0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Genberg BL, Kawichai S, Chingono A, et al. Assessing HIV/AIDS stigma and discrimination in developing countries. AIDS Behav. 2007;12:772–780. doi: 10.1007/s10461-007-9340-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jewkes R, Vundule C, Maforah F, et al. Relationship dynamics and teenage pregnancy in South Africa. Soc Sci Med. 2001;52:733–744. doi: 10.1016/s0277-9536(00)00177-5. [DOI] [PubMed] [Google Scholar]
- 19.Niccolai LM, Dorst D, Myers L, et al. Disclosure of HIV status to sexual partners: predictors and temporal patterns. Sex Transm Dis. 1999;26:281–285. doi: 10.1097/00007435-199905000-00008. [DOI] [PubMed] [Google Scholar]
- 20.O’Brien ME, Richardson-Alston G, Ayoub M, et al. Prevalence and correlates of HIV serostatus disclosure. Sex Transm Dis. 2003;30:731–735. doi: 10.1097/01.OLQ.0000079049.73800.C2. [DOI] [PubMed] [Google Scholar]
- 21.Batterham P, Rice E, Rotheram-Borus MJ. Predictors of serostatus disclosure to partners among young people living with HIV in the pre- and post-HAART eras. AIDS Behav. 2005;9:281–287. doi: 10.1007/s10461-005-9002-5. [DOI] [PubMed] [Google Scholar]
- 22.Mansergh G, Marks G, Simoni JM. Self-disclosure of HIV infection among men who vary in time since seropositive diagnosis and symptomatic status. AIDS. 1995;9:639–644. doi: 10.1097/00002030-199506000-00017. [DOI] [PubMed] [Google Scholar]
- 23.Derlega VJ, Winstead BA, Greene K, et al. Reasons for HIV disclosure/nondisclosure in close relationships: testing a model of HIV-disclosure decision making. J Soc Clin Psychol. 2004;23:747–767. [Google Scholar]
- 24.Nachega JB, Lehman DA, Hlatshwayo D, et al. HIV/AIDS and antiretroviral treatment knowledge, attitudes, beliefs, and practices in HIV-infected adults in Soweto, South Africa. J Acquir Immune Defic Syndr. 2005;38:196–201. doi: 10.1097/00126334-200502010-00011. [DOI] [PubMed] [Google Scholar]
- 25.Brou H, Djohan G, Becquet R, et al. When do HIV-infected women disclose their HIV status to their male partner and why? A study in a PMTCT programme, Abidjan. PLoS Med. 2007;4:1912–1920. doi: 10.1371/journal.pmed.0040342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Donenberg GR, Pao M. Youths and HIV/AIDS: psychiatry’s role in a changing epidemic. J Am Acad Child Adolesc Psychiatry. 2005;44:728–747. doi: 10.1097/01.chi.0000166381.68392.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Green G. Editorial review: Social support and HIV. AIDS Care. 1993;5:87–104. doi: 10.1080/09540129308258587. [DOI] [PubMed] [Google Scholar]
- 28.Kalichman SC, DiMarco M, Austin J, et al. Stress, social support, and HIV-status disclosure to family and friends among HIV-positive men and women. J Behav Med. 2003;26:315–332. doi: 10.1023/a:1024252926930. [DOI] [PubMed] [Google Scholar]
- 29.Simoni JM, Demas P, Mason HRC, et al. HIV disclosure among women of African descent: associations with coping, social support, and psychological adaptation. AIDS Behav. 2000;4:147–158. [Google Scholar]
- 30.Berkman LF. The role of social relations in health promotion. Psychosom Med. 1995;57:245–254. doi: 10.1097/00006842-199505000-00006. [DOI] [PubMed] [Google Scholar]
- 31.Berkman LF. Social support, social networks, social cohesion and health. Soc Work Health Care. 2000;31(2):3–14. doi: 10.1300/J010v31n02_02. [DOI] [PubMed] [Google Scholar]
- 32.Michael YL, Berkman LF, Colditz GA, et al. Social networks and health-related quality of life in breast cancer survivors: a prospective study. J Psychosom Res. 2002;52:285–293. doi: 10.1016/s0022-3999(01)00270-7. [DOI] [PubMed] [Google Scholar]
- 33.Ndinda C, Chimbwete C, McGrath N, et al. Community attitudes towards individuals living with HIV in rural KwaZulu-Natal, South Africa. AIDS Care. 2007;19:92–101. doi: 10.1080/09540120600888378. [DOI] [PubMed] [Google Scholar]
- 34.Mills EA. From the physical self to the social body: expressions and effects of HIV-related stigma in South Africa. J Community Appl Soc Psychol. 2006;16:498–503. [Google Scholar]
- 35.Fund UNP. Women and HIV/AIDS: Confronting the Crisis. New York, NY: United Nations Population Fund; 2004. [Google Scholar]
- 36.Simoni JM, Pantalone DW. Secrets and safety in the age of AIDS: does HIV disclosure lead to safer sex? Top HIV Med. 2004;12(4):109–118. [PubMed] [Google Scholar]