Abstract
We used data from the NICHD Study of Early Child Care and Youth Development and latent class analysis to model patterns of maternal depressive symptoms from infant age 1 month to the transition to adolescence (age 12), and then examined adolescent adjustment at age 15 as a function of the course and severity of maternal symptoms. We identified five latent classes of symptoms in these 1357 women while also taking into account sociodemographic measures: never depressed; stable subclinical; early-decreasing; moderately elevated; chronic. Women with few symptoms were more likely to be married, better educated, and in better physical health than women with more elevated symptoms. Family size and whether the pregnancy was planned also differentiated among classes. At age 15, adolescents whose mothers were in the chronic, elevated, and stable subclinical latent classes reported more internalizing and externalizing problems and acknowledged engaging in more risky behavior than did children of never-depressed mothers. Latent class differences in self-reported loneliness and dysphoria were also found. Finally, several significant interactions between sex and latent class suggested that girls whose mothers reported elevated symptoms of depression over time experienced more internalizing distress and dysphoric mood relative to their male counterparts. Discussion focuses on adolescent adjustment, especially among offspring whose mothers report stable symptoms of depression across their childhoods.
Keywords: maternal depressive symptoms, latent class analysis, longitudinal study, offspring adjustment, adolescent outcomes
A large literature links maternal depression and maternal depressive symptoms to poorer social and emotional outcomes in children across a wide age range from infancy to adolescence (see Goodman & Gotlib, 2002 for reviews). A comprehensive developmental model proposed to account for these associations by Goodman and Gotlib (1999) highlights several important factors. Along with the biological and genetic risk conferred by a depressed mother, characteristics of the depression itself, contextual risks that co-occur with maternal depression, qualities of parenting and the mother-child relationship, and child characteristics must be considered. In the current report we examine early sociodemographic risk factors and the chronicity and severity of maternal depressive symptoms from infancy to early adolescence (age 12) as predictors of offspring adjustment in middle adolescence (age 15).
Adolescent Adjustment and Maternal Depression
Adolescence represents a major life transition, one that may be especially difficult for offspring of depressed mothers, given the normative stresses of this developmental period (Steinberg & Silk, 2002). The experience of living with a depressed mother may place adolescents at particular risk for adjustment problems as they transition into adult-like roles and relationships, possibly with less parental support and less effective role models. Several recent studies indicate that adolescent offspring of depressed women show both more internalizing and externalizing problems than do adolescents whose mothers do not have a history of depression (Foster, Garber, & Durlak, 2008; Garber, Keiley, & Martin, 2002; Hammen & Brennan, 2003; Nelson, Hammen, & Brennan, 2003).
The chronicity and severity of maternal symptoms may also be important to consider when examining adjustment among adolescents whose mothers have a history of major depression or of depressive symptoms. However, with few exceptions, studies have not included measures of depression chronicity. Hammen and Brennan (2003) assessed adolescent outcomes as a function of the course, severity, and timing of maternal depression across childhood. They found that exposure either to a brief episode of major depression or to a more prolonged period of mild depression predicted diagnoses of adolescent depression at age 15, although findings on other disorders were equivocal and more subtle adjustment problems may have been overlooked. In the current paper, we consider adolescent internalizing and externalizing symptoms as predicted by the course and severity of their mothers’ depressive symptoms. We examine more general adjustment problems, in contrast to diagnoses of disorder, because subclinical levels of symptoms in adolescence may well be harbingers of later relationship and other difficulties (Sheeber, Davis, Leve, Hops, Tildesley, 2007). We focus on several self-reported adjustment outcomes at age 15 as a function of latent classes of maternal depressive symptoms and sociodemographic risk modeled from the time of the study child was one month old until the transition to adolescence at age 12.
The literature has tended to emphasize internalizing outcomes, especially depressive symptoms and/or diagnoses (Garber et al., 2002; Hammen, 1991; Hammen & Brennan, 2003), when examining adjustment in adolescents whose mothers have a history of depression. However, it is also reasonable to expect that children living in more stressful circumstances with depressed mothers, especially more chronically depressed mothers, will engage in more risk-taking and externalizing behavior in adolescence, given increased peer pressures and opportunities, parent-child conflict over autonomy and control, and less parental monitoring and supervision (Capaldi, 1992; Kim, Conger, Elder, & Lorenz, 2003; Steinberg & Silk, 2002; Wiesner & Kim, 2006). Moreover, adolescents with adjustment problems may also be more lonely and disengaged from peers than those who are better adjusted. Finally, there is accumulating evidence that internalizing and externalizing problems, including peer problems and risk-taking behavior, co-occur (Capaldi, 1992; Costello Mustillo, Erkanli, Keeler, & Angold, 2003;Wiesner & Kim, 2006) and that adolescent outcomes associated with family and psychosocial risks, including parental psychopathology, tend to be non-specific (Appleyard, Egeland, van Dulmen, & Sroufe, 2005; McMahon, Grant, Compas, Thurm, & Ey, 2003). Thus, we assessed several self-reported indicators of both internalizing and externalizing problems in adolescence: general internalizing problems, along with specific indicators of depression symptoms and loneliness, and general externalizing problems along with a more specific measure of risk-taking behavior. We expected that more severe and more chronic maternal depression symptoms would be reflected in adolescents’ self-reports of poorer adjustment at age 15. Our use of adolescent self-reports makes our outcome measures independent of maternal reports of depressive symptoms and the longitudinal nature of our data allows us to assess adolescent outcomes based on severity as well as stability or change in maternal symptoms. Adolescent Gender Differences in Adjustment Associated with Symptoms of Maternal Depression
The literature not only indicates that maternal depressive symptoms are likely to predict adjustment problems in offspring (Davies & Windle, 1997; Hammen, Shih, & Brennan, 2004), but also that girls and boys may respond differently to maternal distress. Furthermore, it is well-documented that boys are generally more prone to externalizing problems than girls across development from preschool age to adolescence (Costello et al., 2003; Offord, Boyle, Fleming, Monroe-Blum, & Rae-Grant, 1989), whereas sex differences in internalizing problems become evident by adolescence (Angold, Erklani, Silberg, Eaves, & Costello, 2002; Hankin et al., 1998; Nolen-Hoeksema & Girgus, 1994). These typical patterns may be exacerbated by maternal depressive symptoms, especially more chronic symptoms. For example, Davies and Windle (1997) found that family discord and maternal depression were both associated with depressive symptoms and delinquency in adolescent girls, but not boys and that among girls, marital discord and low family intimacy explained the link between maternal depressive symptoms and adolescent problems. Hankin, Mermelstein, and Roesch (2007) recently reported that an increase in depressive symptoms in adolescent females was associated with interpersonal stressors in both the peer group and family, potentially implicating maternal depression, marital conflict, and peer difficulties as especially important factors in girls’ reports of adjustment problems during adolescence.
Overall, several different gender-specific pathways to depression in girls have been proposed (e.g., Hankin et al., 2007; Hyde et al., 2008; Rudolph & Flynn, 2007). Although we are not in a position to test these competing models, they are consistent with the hypothesis that girls whose mothers are more chronically depressed or show increasing symptoms during their daughters’ transition to adolescence will report more depression and loneliness themselves relative to boys or to girls whose mothers report only low levels of depressive symptoms over time. In contrast, we expect boys whose mothers are depressed to acknowledge more externalizing problems relative to girls and relative to boys whose mothers do not report elevated depressive symptoms over time. These predictions are based on the well-documented associations between maternal depression and adolescent adjustment (Rudolph & Flynn, 2007), sex differences in patterns of adjustment difficulties in adolescence (Angold et al., 2002), and the consensus in the literature that family stress has nonspecific links to later problem behavior (McMahon et al., 2003). We do not make a specific prediction about sex differences in risk taking behavior. Thus, in the current report, we examine the interaction between child sex and maternal depression severity/chronicity in predicting self-reported adjustment outcomes in adolescence.
The Course of Maternal Depressive Symptoms
In Goodman and Gotlib’s (1999) model linking maternal depression to children’s functioning attention was paid not only to the presence of depressive symptoms, but also to characteristics of the depression itself including chronicity and severity. It is not surprising that children have poorer adjustment outcomes when their mothers’ depressive symptoms are more severe and/or prolonged (e.g., Campbell et al., 2004; Foster et al., 2008; Frye & Garber, 2005; Hammen & Brennan, 2003; NICHD ECCRN, 1999). More severe and more chronic depressive symptoms may indicate a higher genetic risk for poor adjustment in offspring and also are likely to be associated with less positive maternal behavior and higher levels of psychosocial risk (e.g., Nelson et al., 2003; NICHD ECCRN, 1999). Thus, children whose mothers report more chronic symptoms are also likely to be exposed to longer periods of less engaged and responsive parenting (Campbell, Matestic, von Stauffenberg, Mohan, & Kirchner, 2007) and family conflict (Garber & Little, 2001) than are children whose mothers do not report symptoms or report only short-lived symptoms. However, it is unclear whether more negative outcomes in adolescence are related to elevated concurrent depressive symptoms, the severity of symptoms, or their chronicity (Campbell et al., 2007; Hammen & Brennan, 2003; Weissman et al., 2006).
One approach to examining the course of depressive symptoms in mothers is to use cut-off scores on questionnaires to identify subgroups showing no elevated symptoms, episodic symptoms, or chronic symptoms (NICHD ECCRN, 1999). However, approaches that use criteria such as cut-scores to categorize individuals make the inherent assumption that clear, unambiguous observed subgroups exist. In contrast to subgroups where membership is relatively clear and unambiguous (e.g., males and females), arbitrary classification schemes may not properly account for the uncertainty in class membership. More sophisticated statistical approaches to modeling uncertainty in longitudinal latent classes (e.g., latent class growth analysis (LCGA), Nagin, 2005; growth mixture modeling, Muthén, 2002) are now available to describe the course and severity of symptoms simultaneously.
In a prior analysis using this data set, Campbell et al. (2007) used latent class growth analysis (Nagin, 2005) to model the course of depressive symptoms from one-month postpartum until the study child’s transition to first grade in a large normative sample of mothers and children participating in the NICHD Study of Early Child Care and Youth Development (SECCYD). Six trajectory classes of depressive symptoms were identified: three classes of women showed relatively stable symptoms that were low, moderate, or high; another three classes showed intermittent, increasing, or decreasing symptoms that were all elevated at moderate to high levels, but showed changing elevations over time. Maternal sensitivity and children’s adjustment at first grade (age 7) varied by trajectory class with children whose mothers showed increasing symptoms across the preschool years and during the transition to school faring worst. Trajectory classes also varied in sociodemographic risk which fully explained the differences in child adjustment outcomes as reported by first grade teachers. In the current report, we use the growth mixture modeling framework (Muthén, 2002), to identify latent classes which allows us to model heterogeneity in changes over time in maternal depression without having to specify a functional form for the change (i.e., linear, quadratic), thereby capturing the natural “ups-and-downs” within each class. This framework also allows us to take into account contextual risks (i.e., correlates of class membership) that co-occur with maternal depressive symptoms in a single-step analysis. We use this approach because it has more flexibility than trajectory analysis, given our interest in modeling longitudinal patterns of maternal depressive symptoms in tandem with contextual risks.
Correlates of Maternal Depressive Symptoms
Children raised in families with a depressed mother are exposed to less engaged parenting, chronic interpersonal stress, and also to a number of co-occurring sociodemographic risks (Hammen, 1991; Hammen et al., 2004) that have been linked independently to poor adjustment in childhood and adolescence (Appleyard et al., 2005). Women who are depressed are more likely to experience early parenting, an unplanned pregnancy, marital instability, and/or single parenting with further implications for educational attainment and financial security (Brown & Harris, 1978; Campbell et al., 2007; Cicchetti, Rogosch, & Toth, 1998; Dawson et al., 2003; Leadbeater, Bishop, & Raver, 1996; NICHD ECCRN, 1999; Seifer et al., 1996). Sociodemographic risk, marital instability, and single parenting, in turn, have all been associated with a range of internalizing and externalizing problems in adolescence (Appleyard et al., 2005; McMahon et al., 2003). Thus, it is not surprising that the effects of maternal depression on offspring are partly accounted for by the range of other stresses that co-occur with maternal depression (e.g., Cummings, Davies, & Campbell, 2000; Goodman & Gotlib, 1999; Hammen, 1991, 2002; Hammen et al., 2004).
Even in a relatively low risk sample of married women having their first child, Campbell, Cohn, Flanagan, Popper, and Meyers (1992) found that an unplanned pregnancy and low spouse support, likely markers of a dysfunctional relationship, were associated with depression in the postpartum period. Cicchetti et al. (1998) studied a sample of married middle class women seeking treatment for diagnosed major depression and found that family stress and conflict predicted parents’ ratings of children’s problems, whereas maternal depression per se did not. Thus, maternal depression, whether in families with (e.g., Leadbeater et al., 1996) or without (e.g., Campbell et al., 1992; Cicchetti et al., 1998) high levels of sociodemographic risk tends to occur in the context of other indicators of family stress and relationship difficulties. These risk factors also contribute to children’s poor outcomes via pathways that may include a mix of genetic risk, feelings of emotional insecurity, and low levels of social support from significant adults (Cummings et al., 2000; Downey & Coyne, 1990).
Because depressive symptoms, especially self-reported depressive symptoms assessed by questionnaire, are often confounded with sociodemographic risk one way to address these confounds is to model depressive symptoms longitudinally while simultaneously considering relevant sociodemographic risk factors. Thus, in the current report we used latent class analysis to model the course of maternal depressive symptoms over a 12-year period while also factoring sociodemographic indicators into the analysis as predictors of depression class membership via multinomial logit regression (see Muthén, 2002). Although it was possible that we would identify the same trajectories as found in Campbell et al. (2007), it was also possible that somewhat different trajectories would emerge, given the longer time frame (12 years versus 7 years) and the different analytic technique that also considered demographic factors as predictors of class membership in modeling trajectories, we did expect to find distinct classes showing low, moderate, and high levels of relatively stable symptoms as well as two to three classes showing variable levels of increasing and decreasing symptoms. Our interest was in describing the course of maternal depressive symptoms over the period from infancy to the transition to adolescence (age 12) in the context of demographic variables that tend to co-occur with depressive symptoms. Furthermore, our expectations were based on studies examining the course of depressive symptoms and of clinical diagnoses, that have identified some women showing both stable and severe symptoms, some with more mild, but persistent symptoms, and still others with declining or episodic patterns of symptoms over time (Hammen & Brennan, 2003; Kessing, 2008; Otto et al., 2007).
The latent class analysis of maternal depressive symptoms then provided the framework from which we could next examine the level (i.e., severity) and chronicity (i.e., stability) of maternal symptoms over time in relation to children’s social and emotional functioning in middle adolescence, i.e., at age 15. This approach to modeling maternal depressive symptoms also allowed us to assess increases or decreases in maternal symptoms in relation to adolescent adjustment. Although, as already noted, the links between maternal depression and poor adjustment are well-established, most studies have examined younger children (e.g., Brennan et al., 2000; Campbell et al., 2007; NICHD ECCRN, 1999; Cicchetti et al., 1998) and relatively few studies have specifically examined offspring adjustment in adolescence from the perspective of the chronicity and severity of maternal depressive symptoms across the entire life span of the child from early infancy to adolescence. As already noted, one exception is the work of Hammen and Brennan (2003) who studied the chronicity of maternal depression and adolescent adjustment, but their assessments of depression were based partly on reconstructions of the timing and severity of depressive episodes derived from interviews when adolescents were age 15. In contrast, our data are based on prospective assessments of symptoms obtained at regular intervals and do not involve retrospective reports.
The Current Study
In summary, using the NICHD SECCYD data set, we first use latent class analysis to model trajectories of maternal depressive symptoms from child age one month to age 12, as children transition into adolescence, controlling for potentially confounding sociodemographic variables obtained at the one month interview including maternal education, maternal age, marital status, number of children, maternal health, and whether the pregnancy was planned. Once we have described these longitudinal latent classes of maternal symptoms, we examine adolescent adjustment outcomes at age 15 with an emphasis on several indicators of internalizing and externalizing problems. We expect that adolescents whose mothers report either chronic depressive symptoms or depressive symptoms that increase across middle childhood and through the transition to adolescence will report more adjustment problems themselves than adolescents whose mothers report only low to moderate levels of symptoms over time; we also expect that there may be differential patterns of outcomes as a function of child sex, with boys of more chronically depressed mothers acknowledging more externalizing problems and girls with more chronically depressed mothers reporting more internalizing problems, especially depressive symptoms and loneliness.
Method
Participants
The analyses for this study are based on data from 1357 families participating in an ongoing, multi-site study, the NICHD Study of Early Child Care and Youth Development. Children participating in this study were born in 1991 in hospitals at 10 data collection sites across the U.S.: Little Rock, AR; Irvine, CA; Lawrence, KS; Boston, MA; Philadelphia, PA; Pittsburgh, PA; Charlottesville, VA; Morganton, NC; Seattle, WA; and Madison, WI. These children and their families were followed from birth through age 15.
Families were recruited during hospital visits to mothers shortly after their child’s birth. During selected 24-hour sampling intervals, 8,986 women giving birth were screened for eligibility and willingness to be contacted again. Of these women 5,416 (60%) agreed to be called in 2 weeks and met the following eligibility criteria: the mother was over 18 years of age and could speak English; the family did not plan to move within the next three years; the child was a singleton, was not hospitalized for more than 7 days, and did not have obvious disabilities; the mother did not have a known substance abuse problem. A total of 1,364 mothers, who completed a home interview when their infant was 1 month old, became the study participants. The recruited sample was diverse, including 24% ethnic minority children, 11% mothers with less than a high school education, and 14% single mothers. More details on sample recruitment and methods can be found at the study website (http://secc.rti.org/).
Of the 1,364 participants constituting the original sample, 1,357 mothers and children were included in the current study because maternal reports of depressive symptoms were available at the one-month assessment. To make use of this large sample and account for missing data, full information maximum likelihood estimation was used based on the assumption that the probability of missingness may depend on data that are observed (i.e., non-missing) but do not depend on the values of the data that are missing (i.e. missing-at-random, Schafer & Graham, 2002).
Overview of Data Collection
Data were initially collected when the children were 1 month old and again at 6, 15, 24, 36, 54 months and at first, third, fifth, and sixth grades (i.e., at 7, 9, 11, and 12 years of age). Children and families were followed again at age 15 years. Home visits were conducted when the study children were 1 month old. During this visit, demographic information including maternal age and education level, and mother’s marital status was collected. Information regarding mothers’ health and the planned/unplanned status of their pregnancy was also obtained.
Maternal reports of depression were obtained using the Center for Epidemiological Studies Depression Scale (CES-D) when children were 1, 6, 15, 24, 36, and 54 months and at each assessment from first through sixth grade (i.e., at ages 7 through 12), for a total of 10 assessments. Outcome measures were derived from adolescent self-reports obtained at the age 15 laboratory visit.
Measures
Demographics
During the 1 month interview, mothers reported on their age at the time of the study child’s birth and on the number of years of school completed, which was used as an index of maternal education. Marital status (married to the study child’s father vs. not married to the study child’s father) at the time of the child’s birth was also determined at the 1 month interview as were mother’s ethnicity (white, non-white) and the study child’s birthorder. During the 1 month interview mothers were asked whether the pregnancy was planned (yes/no, 1/0) and whether they had been happy about the pregnancy (yes/no, 1/0). These two items were highly correlated (.87) and were therefore combined into a score that could range from 0 to 2. Finally, mothers were asked to rate their overall health on a 4-point scale from 1= excellent to 4= poor.
Maternal Depressive Symptoms
At each interview, mothers completed the CES-D (Radloff, 1977), a reliable and valid 20-item scale that assesses depressive symptoms manifest in the past two weeks. Mothers’ scores on the CES-D correlated moderately over time (r’s from .33 to .58) and internal consistency was high at each assessment (α’s from .88 to .91). Most women (89%) completed the CES-D five times or more.
Outcome Measures in Adolescence
Adolescent self-reports of adjustment were obtained during the laboratory visit at age 15. The Children’s Depression Inventory (short form, Kovacs, 2001) was completed (α = .81) Adolescents were presented with 10 sets of three statements and asked to indicate which one best described their feelings over the last two weeks. Items tap dysphoric mood, lack of pleasure, and low self-esteem, with higher scores reflecting more depressed mood.
Self-reported loneliness was assessed with the 16-item Loneliness and Social Dissatisfaction Questionnaire (Asher, Hymel, & Renshaw, 1984) (α = .91). Items assess feelings of loneliness, social adequacy, and estimations of peer status and are rated on a 5-point scale from “not at all true” to “always true”.
Adolescents also completed the Youth Self-Report Form (Achenbach, 1991) which assesses self-reported behavioral and emotional problems. The current analysis included only the 31 items making up the Internalizing scale (α = .89) and the 30 items comprising the Externalizing scale (α = .86). The Internalizing scale includes the narrow band Anxious/Depressed, Social Withdrawal, and Somatic Complaints scales. The Externalizing scale is made up of the Aggression and Delinquency narrow band scales. Adolescents were asked to rate how well each item described their behavior in the last 6 months on a 3-point scale from “not true” (0) to “very true or often true” (2).
Finally adolescents reported on their engagement in risky behaviors on a measure designed specifically for this study, combining items used by other investigators in Fast Track, New Hope, and other studies of adolescent risk-taking (Conger & Lorenz, 1994; Halpern-Felsher, Biehl, Kropp, & Rubenstein, 2004; Kaplow et al., 2004). Adolescents were asked how often in the past year they had engaged in a series of mildly to seriously risky behaviors (e.g., skipped school without permission, taken part in gang fight, smoked marijuana, sold drugs, had sexual intercourse). Items were originally rated on a 3-point scale from 0= never, 1=once or twice, 2 = more than twice. Because of skewness in the data, scores were recoded to 0= none and 1 or 2 = some. The coefficient alpha based on 53 items was .89.
Results
Overview of data analysis
Our primary research questions centered on (a) describing the number and nature of latent classes of maternal depressive symptoms assessed longitudinally while simultaneously considering sociodemographic indicators, and (b) examining the relation between the maternal depression classes and adolescent outcomes at age 15. These research questions were addressed in a two-stage analysis framework; first, conditional latent class analysis (CLCA; Muthén, 2002) was used to model latent classes of maternal depression symptoms, that is to identify qualitatively distinct patterns over time in depressive symptoms from the child’s first month of life through age 12 (sixth grade). In CLCA, the interest is in unobserved or hidden patterns within a set of longitudinal data from which multiple sets of latent groupings or classes emerge. These trajectory classes can then be simultaneously modeled as latent nominal outcome variables (via the multinomial logit modeling framework) and/or as predictors by which differences in other outcomes can be modeled. Next, after the latent depression classes were identified and described, the “LCA with distal outcomes” framework (Muthén & Muthén, 1998-2006) was used in order to examine whether there was systematic variation in distal child outcomes at age 15 (i.e., YSR internalizing, CDI, loneliness, YSR externalizing, risky behavior) across maternal depression classes. Outcomes were also examined to determine whether there were statistical interactions between depression class and adolescent gender.
We used this framework (as opposed to creating class membership dummy variables from the CLCA analysis) in order to properly model the impact of uncertainty in latent class membership on child outcomes. All analyses were conducted in Mplus v5 (Muthén & Muthén, 1998-2007). In all analyses, site was modeled as a nesting variable in order to account for non-independence of observations due to nesting among individuals within sites via the “type = complex” option in Mplus using robust maximum likelihood estimation (Yuan & Bentler, 2000); robust ML also models parameters of interest under the assumption that missingness is predictable by variables that are observed but (conditionally) unrelated to the values that are missing (i.e., missing-at-random; Schafer & Graham, 2002).
Latent class analysis
Latent class analysis was used to model the course of maternal depression symptoms from the time the study child was one-month old until age 12 years, and several one-month demographic measures were also included as predictors of the latent classes. CES-D scores at each assessment (child age 1, 6, 15, 24, 36, and 54 months, and 7, 9, 11, and 12 years) were used in the analyses, with adjustments for missing data using full information maximum likelihood. One-month predictors included ethnicity (white, non-white), maternal age at the study child’s birth, maternal years of education, child sex, maternal health (rated on 4-point scale), whether the pregnancy was planned/welcomed, birth order of the study child, and marital status (married, not married).
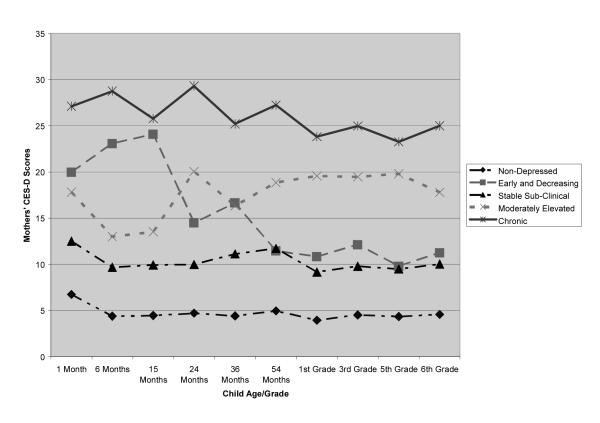
A series of CLCA models, with varying numbers of classes, were fit to the longitudinal CES-D data in order to assess: (a) the optimal number of latent classes that underlie the data, (b) the form of changes over time in depressive symptoms within each latent class, and (c) key sociodemographic predictors of latent class membership. Based on two statistics used to assess comparative model fit in latent class models (Bayesian Information Criterion, entropy), five latent classes of maternal depressive symptoms were identified varying in both level (i.e., severity) of symptoms and pattern over time. Fit statistics are summarized in Table 1 and the latent classes are depicted in Figure 1. Descriptive statistics on CES-D scores by assessment and latent class are presented in Table 2.
Table 1.
Conditional Latent Class Analysis - Global Fit Statistics
| Classes | BIC | Entropy |
|---|---|---|
| Three | 76654 | .843 |
| Four | 76534 | .807 |
| Five | 76401 | .816 |
| Six | -a | - |
Notes. BIC = Bayesian Information Criterion (lower values indicate superior model).
The sixth class had a N of 0.
Figure 1.
Latent classes of maternal depressive symptoms
Table 2.
Adjusted CES-D Scores over Time by Maternal Depression Class
| Maternal Depression Class |
|||||
|---|---|---|---|---|---|
| Child Age | Never Depressed | Early Decreasing |
Stable Subclinical |
Moderately Elevated |
Chronic |
| 1 month | 6.73 | 19.99 | 12.51 | 17.81 | 27.11 |
| 6 months | 4.39 | 23.09 | 9.69 | 12.99 | 28.75 |
| 15 months | 4.46 | 24.09 | 9.93 | 13.53 | 25.79 |
| 24 months | 4.71 | 14.50 | 9.98 | 20.05 | 29.31 |
| 36 months | 4.41 | 16.66 | 11.13 | 16.34 | 25.20 |
| 54 months | 4.96 | 11.46 | 11.73 | 18.86 | 27.24 |
| 7 years | 3.95 | 10.84 | 9.17 | 19.57 | 23.83 |
| 9 years | 4.53 | 12.14 | 9.80 | 19.47 | 24.97 |
| 11 years | 4.35 | 9.81 | 9.49 | 19.80 | 23.26 |
| 12 years | 4.58 | 11.26 | 10.04 | 17.80 | 24.99 |
Notes: Scores are adjusted for missing data via EM Algorithm-adjusted means and covariances. Scores are also adjusted by the following covariates: maternal education, race/ethnicity, maternal age, maternal health (at 1 month post-partum), study child birth order, marital status (at 1 month post-partum) and planned pregnancy (yes/no). N’s = 671, 59, 416, 145, and 66 respectively.
Consistent with prior analyses of this data set, a small percentage of women (4.7%, n=66) reported high levels of symptoms across the entire 12-year period of the study. Although their symptoms fluctuated slightly, they were consistently elevated well above the established cut-off of 16 on the CES-D which designates potentially clinically-significant symptoms, suggesting that their symptoms were relatively chronic and severe. A second group of mothers reported moderate symptoms over time, with a drop to subclinical levels at 6 and 15 months that then rose again at 24 months and remained moderately elevated through age 12 (moderately elevated, 10.9%, n=145). Although the women in this latent class generally reported lower symptom levels than women in the chronic and severe class, after 24 months they too were consistently above the clinical cut-off of 16. A third group showed symptoms that were elevated in the postpartum period above the clinical cut-off and then increased slightly over the first year; their symptoms then declined at 24 months and continued to decline to moderate, subclinical levels throughout early childhood, remaining at relatively lower levels through the child’s transition to school and early adolescence (early decreasing, 5.1%, n=59). Two large groups of women reported stable levels of symptoms, either moderate, subclinical levels or very low levels. The stable subclinical group, comprising 30.8% of the sample (n= 416), reported some symptoms that were always below the clinical cut-off, but also were consistently higher than the levels of symptoms reported by the 671 (48.5%) women in the never depressed group who reported scores of 7 or lower at every assessment. Overall, then, about 80% of the women in the sample reported symptom levels that were consistently below the clinical cut-off of 16, whereas about 20% of women reported symptoms that were either moderately or highly elevated early only, consistently from toddlerhood onward, or chronically.
Predictors of Latent Class
The probability of being in a particular latent class was partly conditional on early sociodemographic measures assessed with multinomial logit estimates. Descriptive statistics on demographic indicators are provided in Table 3. In general, as expected, the women in the never depressed class had the highest levels of demographic resources (education and income), were more likely to be married, to report better health, and to have fewer children. When the four latent classes of women who reported at least subclinical symptoms were compared to the never depressed class as the reference group, maternal health, marital status, and educational level were the most consistent predictors of membership in the never depressed group. Women who never reported elevated symptoms were more likely to be married (p<.001), were better educated (p<.01), and reported being in better health (p<.001) in contrast to women who reported higher levels of depressive symptoms who were more likely to be unmarried, lower in education, and to report more health problems. In contrast, women in the stable subclinical class were older (p<.05) and had fewer children (p<.05), but they also were more likely to report that their pregnancy was not planned (p<.05).
Table 3.
Demographics by Maternal Depression Class
| Maternal Depression Class |
|||||
|---|---|---|---|---|---|
| Never Depressed | Early Decreasing |
Stable Subclinical |
Moderately Elevated |
Chronic | |
| Demographics | |||||
| Maternal Health | 3.65 (.02) | 3.22 (.12) | 3.39 (.03) | 3.26 (.07) | 2.86 (.10) |
| Planned Pregnancy | 1.43 (.04) | .89 (.23) | .93 (.08) | .82 (.15) | 1.00 (.13) |
| Birth Order | 1.78 (.04) | 2.46 (.46) | 1.80 (.06) | 1.82 (.13) | 1.91 (.16) |
| % Married | 92.6% | 65.0% | 68.1% | 49.2% | 50.1% |
| % White | 92.1% | 78.0% | 75.7% | 64.3% | 77.7% |
| Maternal Age | 29.70 (.24) | 28.02 (1.15) | 27.87 (.59) | 23.69 (.83) | 24.62 (.81) |
| % Female | 46.9% | 43.6% | 56.8% | 49.1% | 47.1% |
Notes: Values are adjusted for missing data via EM Algorithm-adjusted means and covariances. N’s = 671, 59, 416, 145, and 66 respectively.
In a second set of analyses, the chronic severe latent class was considered the reference group and compared with the three other classes reporting elevated symptoms (i.e., early decreasing, moderately elevated, and stable subclinical). Mothers who reported chronic severe symptoms also were more likely to report health problems than other women with elevated symptoms (p<.01). The women with stable subclinical symptoms were older than women in the chronic severe class (p<.001), and they were also more likely than those in the chronic severe class to indicate that their pregnancies were unplanned (p<.05).
Adolescent Outcomes as a Function of Latent Classes of Maternal Depressive Symptoms
The relation between maternal depression classes and age 15 adolescent outcomes, and the extent to which they varied across child gender were of interest; all 5 outcomes were examined simultaneously and were allowed to covary with each other (i.e., multivariate distal outcomes). The correlations among adolescent outcome measures ranged from .046 for loneliness and risky behavior to .646 between YSR internalizing and CDI dysphoric mood. YSR internalizing and externalizing scores were correlated at only a modest level (r = .451). However, the multivariate analysis of outcome measures controlled for their inter-correlations. When the effect of child gender on outcomes varied across maternal depression class, it was considered to be analogous to a depression class by gender interaction effect on age 15 child outcomes. Descriptive statistics on adolescent outcome measures, unadjusted for covariates, by maternal depression latent class are summarized in Table 4. Cross-class differences in age 15 child outcome means (i.e., depression class main effects) and cross-class differences in the relation between child gender and age 15 outcomes (i.e., gender by depression class interaction effects) were tested using the Model Constraint feature in Mplus v5; this was done because the Model Constraint feature allows for tests of differences across classes while accounting for uncertainty in class membership (i.e., via cross-class parameter covariances; see e.g., Morgan-Lopez & Fals-Stewart, 2007, p. 593). We calculated effect sizes for key main effects using the approach of converting z statistics to r2s as found in Rosenthal and Rosnow (1991).
Table 4.
Adolescent-Reported Outcomes by Maternal Depression Class
| Maternal Depression Class |
|||||
|---|---|---|---|---|---|
| Never Depressed | Early Decreasing |
Stable Subclinical |
Moderately Elevated |
Chronic | |
| CDI Age 15 | 1.45 (.24) | 1.83 (1.44) | 2.52 (.56) | 2.77 (.96) | 2.54 (.83) |
| Loneliness 15 | 24.76 (.72) | 25.26 (5.01) | 27.75 (1.62) | 30.08 (3.02) | 27.45 (2.86) |
| Internalizing 15 | 44.91 (1.05) | 45.05 (6.04) | 49.51 (2.23) | 51.30 (2.92) | 49.75 (2.54) |
| Externalizing 15 | 47.02 (.88) | 47.56 (3.02) | 51.59 (1.69) | 52.76 (2.03) | 51.03 (2.08) |
| Risky Behavior 15 | 5.00 (.36) | 5.61 (.84) | 6.68 (.71) | 9.17 (1.25) | 8.30 (1.18) |
Notes: Values are adjusted for missing data via EM Algorithm-adjusted means and covariances (but are not adjusted for covariates).
Adolescents’ Depressive Symptoms
Adolescents with mothers in the chronic depression class (mean = 3.062, SE = .701; difference = 1.745 (.781), z = 2.23, p= 0.026, r2 = .009) and the stable subclinical class (mean = 2.720, SE = .288; difference = 1.403 (.449), z = 3.12, p = 0.002, r2 = .013) reported significantly higher levels of depressive symptoms at age 15 than did children of never-depressed mothers (mean = 1.317, SE = .200). The means included in the text are slightly different from the means in Table 4 because they are adjusted for covariates.
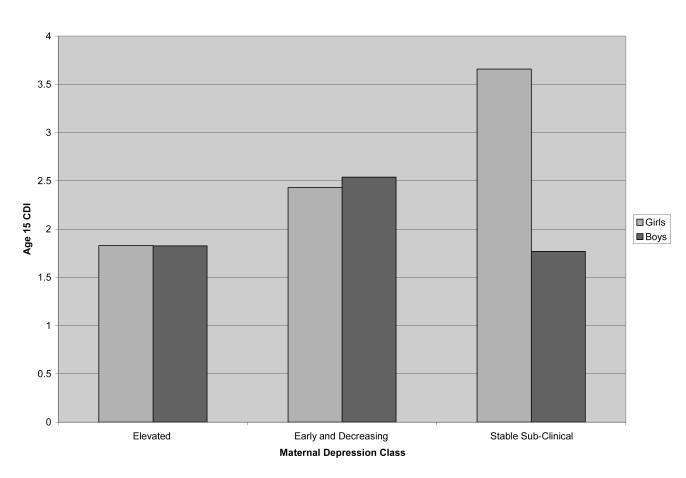
However, there were also differences in the impact of gender on age 15 depression scores across maternal depression class. Gender by depression class interactions were observed between a) the moderately elevated and stable sub-clinical classes (difference = -1.884 (.961), z = -1.961, p=.050) and b) the stable sub-clinical class and the early and decreasing class (difference = 1.280 (.588), z = 2.177, p=.029); within these three classes, only the gender effect within the stable sub-clinical class was significant, with girls significantly higher than boys in self-reported depressive symptoms at age 15 (gender simple effect for the stable sub-clinical class = 1.886 (.449), z = 4.20, p<.001) in contrast to the other two latent classes in which boys and girls had similar CDI scores. These results are depicted graphically in Figure 2.
Figure 2.
Latent class by gender interaction in reports of depressive symptoms (CDI) at age 15.
Loneliness
Children of mothers in the elevated class (mean = 27.983, SE = 1.450; difference = 3.066 (1.381), z = 2.20, p = .026, r2 = .006) and the stable subclinical class (mean = 27.634, SE = .763; difference = 2.717 (1.143), z = 2.37, p= .017, r2 = .005) reported significantly higher levels of loneliness at age 15 than did children of never-depressed mothers (mean = 24.917, SE = .540). The gender by latent class interactions were not significant.
Internalizing Symptoms
Compared to adolescents of mothers in the never-depressed class (mean = 44.971, SE = .684), adolescents with mothers in the elevated depression class (mean = 49.252, SE = 1.430; difference = 4.281 (1.378), z = 3.106, p=.002, r2 = .011), the chronic depression class (mean = 50.675, SE = 1.896; difference = 5.704 (2.141), z = 2.664, p=.008, r2 = .010), and the stable subclinical class (mean = 49.342, SE = .915; difference = 4.371 (1.411), z = 3.09, p=.002, r2 = .010) reported higher internalizing symptoms at age 15. There was also a gender by maternal depression class interaction effect driven by a) differences between adolescents whose mothers were in the chronic class and the early-decreasing class (gender by class interaction = 12.068 (5.75), p= .036) and b) the chronic class and the never-depressed class (gender by class interaction = 8.128 (3.98), p=.041); gender differences were greatest among adolescents whose mothers were in the chronic depression class, with girls significantly higher than boys (p=.032) whereas gender effects were not significant in the other classes (See Figure 3).
Figure 3.
Latent class by gender interaction in reports of internalizing symptoms (YSR) at age 15
Externalizing Symptoms
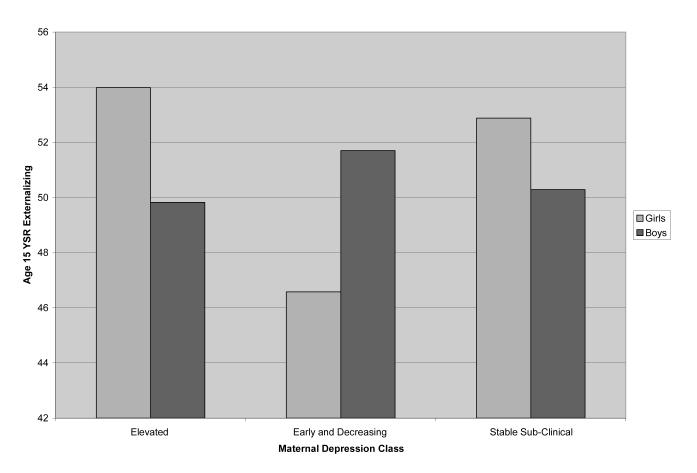
A similar pattern emerged for adolescents’ self-reports of externalizing symptoms. Adolescents whose mothers reported elevated (mean = 51.913, SE = 1.385; difference = 4.94 (1.26), z = 3.91, p<.001, r2 = .018), chronic (mean = 50.619, SE = 1.495; difference = 3.63 (1.64), z = 2.20, p=.027, r2 = .007) or stable subclinical depression symptoms (mean = 51.587, SE = .740; difference = 4.60 (1.07), z = 4.268, p<.001, r2 = .017) reported more externalizing problems at age 15 than did adolescents whose mothers never endorsed elevated depression symptoms (mean = 46.987, SE = .566).
There were also differences in the impact of gender on age 15 externalizing problems across maternal depression class. First, the gender → externalizing link was significantly different across a) the elevated class and the early-decreasing class (gender by class interaction = 9.28 (4.55), z = 2.03, p=.042) and b) the early-decreasing class and the stable sub-clinical class (gender by class interaction = -7.71 (3.79), z = -2.03, p=.042). Within the elevated class, girls unexpectedly had (non-significantly) higher levels of externalizing than boys (gender difference = 4.16, SE = 2.67, p=ns), while within the early-decreasing class boys were higher than girls (though this difference was also non-significant within class; gender difference = -5.12, SE = 3.47, p=ns.). However, girls in the stable sub-clinical class did report significantly higher externalizing problems (although the difference in the magnitude was smaller than the magnitude in the other two classes; gender difference = 2.59, SE = 1.30, z = 1.994, p=.046) than boys (See Figure 4).
Figure 4.
Latent class by gender interaction in reports of externalizing symptoms (YSR) at age 15
Risky Behavior
Adolescents whose mothers were in the elevated class (mean = 9.07, SE = 1.17; difference = 4.48 (1.19), z = 3.73, p<.001, r2 = .016), the chronic class (mean = 7.96, SE = 1.04; difference = 3.33 (1.06), z = 3.12, p=.002, r2 = .014) and the stable sub-clinical class (mean = 7.34, SE = .477; difference = 2.71 (.598), z = 4.53, p<.001, r2 = .020) all reported engaging in significantly more risky behavior at age 15 than the adolescents whose mothers were in the never-depressed class (mean = 4.62, SE = .244). These cross-class differences in age 15 risky behavior were consistent across gender (i.e., there were no gender by maternal depression class interaction effects).
Discussion
The results of this study indicate that patterns of maternal depressive symptoms studied longitudinally from infant age one month until children made the transition to adolescence (age 12) were associated with adolescents’ self-reports of social and emotional adjustment at age 15. Over and above early sociodemographic risk, more chronic and prolonged maternal symptoms that were evident from infancy to early adolescence, predicted adolescents’ self-reports of general internalizing and externalizing problems, as well as more specific indicators of dysphoria, loneliness, and risk-taking behavior. Importantly, although chronic and severe maternal symptoms were associated with more self-reported problems in adolescent offspring as expected, this was also true for the group of teens whose mothers reported either moderately elevated symptoms or chronic symptoms that were at a subclinical level and elevated only in comparison to mothers who never reported elevated symptoms. Thus, our findings indicate that chronic symptoms in mothers at varying levels of severity predict poorer offspring adjustment in contrast to adolescents whose mothers never reported elevated depressive symptoms. However, somewhat inconsistent with this picture, the group of teens whose mothers reported early and decreasing symptoms did not differ on any outcome measure from teens whose mothers reported no significant symptoms. This is difficult to explain because mothers in the early and decreasing latent class reported symptoms that were never below those reported by mothers showing chronic subclinical symptoms.
Although other studies have linked maternal depressive symptoms to adolescent adjustment difficulties (Foster et al., 2008; Frye & Garber, 2005; Hammen & Brennan, 2003), this is the first study of which we are aware to study the course of maternal symptoms prospectively at regular intervals from infancy to adolescence and then to utilize adolescents’ own reports of their adjustment to assess outcomes. The results point to the importance of ongoing maternal symptoms that may be a marker of genetic risk and also co-occur with family stress and less engaged and supportive parenting (Foster et al., 2008; Goodman & Gotlib, 1999; Sheeber et al., 2007). Hammen and Brennan (2003) likewise examined adolescent outcomes in their epidemiological sample followed prospectively, using retrospective reports to assess the timing of maternal depression. They found that either chronic, but mild symptoms or more severe, but short-lived symptoms were associated with offspring diagnoses of depression. The current study is consistent with their findings in implicating chronic maternal symptoms, even at subclinical levels, as a predictor of poorer adjustment in adolescence. Our results also indicate that a range of internalizing and externalizing problems are differentially predicted by the pattern and severity of maternal depressive symptoms. Furthermore, when interactions between patterns of maternal depressive symptoms and adolescent adjustment were found, they indicated that girls whose mothers reported ongoing symptoms of depression acknowledged more adjustment difficulties in adolescence than did boys.
It is important to keep in mind, however, that despite the pattern of significant differences in adolescent adjustment outcomes across maternal depression latent classes, scores on adolescent self-report measures were consistently below clinical cut-offs on the CDI and YSR Internalizing and Externalizing scales. The descriptive data presented in Table 4 suggest that there is more variability in self-reported risky behavior and loneliness than the CDI and YSR, but these measures do not include clinical cut-offs. These findings make it clear that we are talking about variations in offspring adjustment that are generally within the normal range rather than identifying clinically significant problems. In addition, we recognize that our effects sizes are relatively small. Several features of the analytic model, however, must be considered when evaluating these small effects. First, we controlled for a number of covariates reflecting sociodemographic risk which themselves are likely to be correlated with adolescent outcomes; second, the outcomes themselves were moderately inter-correlated; and, third, in latent class models the standard errors for all parameters are typically inflated as a consequence of uncertainty in class membership, which in turn lead to smaller test statistics. Despite these caveats, the findings suggest that variability in adolescent adjustment is related to variations over time in maternal depressive symptoms, over and above sociodemographic indicators.
Overall, regardless of gender, adolescents whose mothers reported chronic symptoms of depression across childhood at differing levels of severity reported not only more internalizing symptoms, but also more dysphoria and/or loneliness. Contrary to expectation, both boys and girls whose mothers were in the moderately elevated and stable subclinical latent classes reported feeling lonelier, possibly suggesting more difficulties in the peer group as well as less support from family. Similarly, both boys and girls in the chronic latent class reported higher levels of dysphoric mood than adolescents whose mothers were never depressed and boys and girls with mothers in the elevated and stable subclinical classes both reported elevated levels of internalizing symptoms relative to those whose mothers were never depressed. Thus, we obtained fewer gender differences in adolescent self-reports at age 15 than we anticipated, suggesting that chronic symptoms in mothers in tandem with the relatively higher levels of sociodemographic risk that accompanied ongoing maternal symptoms predicted more anxiety, depression, somatic complaints and loneliness at age 15 regardless of gender. The two sex by latent class interactions were consistent with predictions in that girls whose mothers were in the chronic class reported more internalizing symptoms relative to boys and girls whose mothers were in the stable subclinical class reported higher levels of dysphoria than their male counterparts. Although this may suggest that some girls were more sensitive to the effects of maternal depression, the overall pattern of findings across measures, latent classes, and gender is only weakly supportive of this possibility.
It is also noteworthy that adolescents whose mothers reported chronic, elevated, and stable subclinical symptoms likewise reported engaging in more externalizing and risky behavior than did adolescents whose mothers never reported depressive symptoms. The one significant interaction effect suggested that girls whose mothers reported subclinical symptoms were higher on this measure than boys in this group. Although we expected to find elevations on externalizing and risky behavior as a function of maternal depression latent class, we anticipated that boys would be higher on these adjustment indicators than girls and that we would be likely to find an interaction between maternal depression latent class and child gender with boys higher than girls when their mothers were more chronically depressed. Although results supported the hypothesis of elevated externalizing problems, the gender interactions were inconsistent with expectation. Overall, our results suggest that when maternal symptoms are prolonged, both boys and girls report some adjustment difficulties in adolescence.
We modeled latent classes of maternal depressive symptoms in tandem with sociodemographic measures, thereby providing a description of demographic risk factors that co-occurred with longitudinal symptom patterns. Consistent with prior studies linking sociodemographic risk to depressive symptoms (e.g., Brown & Harris, 1978; Cicchetti et al., 1998; Dawson et al., 2003; Hammen, 1991, 2002), women who reported elevated symptoms were less likely to be married, had less education, and reported being in poorer physical health than women who never endorsed symptoms of depression. Depressed women may report feeling physically unwell, either because of reporter bias or because their depression is partly manifest in physical symptoms including aches and pains. Conversely, chronic health problems may contribute to feelings of despondency and sadness. Our data do not permit us to tease apart the direction of effects between physical health and sad mood, but this issue is important to consider in future studies examining the course of depressive symptoms in women. However, from the perspective of a child growing up with a chronically distressed mother, the cause of the distress may be less important than the fact that symptoms of depression are evident over time.
Women with elevated symptoms of depression in our sample, especially those with either moderately elevated or chronic severe symptoms, not only reported more health problems, but they were also less likely to be married at the time the study child was born. Whereas over 90% of the women with very low symptoms were married at the time of the study child’s birth, only about half the women in the two most stable and elevated symptom groups were married. Thus, they were more likely than never-depressed mothers to lack the benefits of spouse support, both emotionally and in terms of child care (Hopkins & Campbell, 2008); lack of adequate social support and help with childrearing have been associated with postpartum adjustment in other studies (Campbell et al., 1992). The lack of a relationship with a partner at the time of the study child’s birth may reflect the severity of dysfunction, in that depressive symptoms may have impaired these women’s ability to remain in a stable relationship with the infant’s biological father. In the current community sample, sociodemographic risk was quite stable (NICHD ECCRN, 2004). Furthermore, when we examined the marital status of these women at adolescent age 15 in relation to adolescent adjustment (data not shown), differences in adolescent outcomes remained the same. This suggests that being single at the time of the study child’s birth is in itself a robust marker of sociodemographic risk. However, it remains unclear whether the risk reflects primarily the severity of the depressive symptoms and/or lack of financial and social support.
Number of children (Brown & Harris, 1978) and planning for the pregnancy (Campbell et al., 1992) also may be linked to patterns of depressive symptoms in childbearing women. In our data, women who reported elevated depressive symptoms that decreased by the end of the study child’s second year to a subclinical level (early-decreasing) also had the most children. Although this difference was not significant once other covariates were controlled, their symptom levels may reflect the stresses of coping with several young children, and their symptoms may have abated somewhat as their older children entered school and became more self-sufficient.
In contrast, women who reported symptoms that were consistently stable, but subclinical were more likely than women who endorsed very low symptoms (never-depressed) to have fewer children, but to describe their pregnancy as unplanned. They were also older, but only 68% were married at the time of the study child’s birth. Other research has noted a link between an unplanned pregnancy and clinically diagnosed postpartum depression in low risk married women having their first child (Campbell et al., 1992). In the current study this link was more subtle because the women reported only subclinical, albeit stable, levels of depressive symptoms. This may suggest that women with chronic dysphoria are less likely to plan ahead and take precautions to avoid becoming pregnant than better functioning women, so the unplanned pregnancy may be a result of the chronic sad mood or it may be a sign of relationship difficulties. However, these women with stable subclinical symptoms were also more likely to report that their pregnancy was unplanned than were women in the chronic, severe depression latent class, complicating the interpretation of this intriguing finding.
Taken together, however, our data suggest that there are distinct patterns of maternal depressive symptoms over this 12-year period that are also related to sociodemographic risk and maternal physical health, with some women showing either subclinical or potentially clinically significant symptoms over the first twelve years of the study child’s life. Approximately 80% of the women in the sample never acknowledged symptoms above the accepted clinical cut-off score on our assessment measure, the CES-D, whereas the remaining 20% reported elevated symptoms at least some of the time, with some mothers showing a decline in symptoms by 24 months, and others showing either increases or high and stable symptoms. However, 31% of women reported symptom levels that while below the clinical cut-off of 16 on the CES-D, were still substantially elevated relative to the women in the never depressed group. Overall, then, a substantial number of children were being raised in a family where the mother reported either potentially clinically elevated levels of depressive symptoms or subclinical levels of symptoms that were still persistent. Their children’s adjustment at age 15 appeared to reflect something about being raised with a mother showing consistently elevated symptoms, as across the chronic, moderately elevated, and stable subclinical latent classes, adolescents reported both more internalizing (including loneliness and dysphoria) and externalizing symptoms (including more risk-taking) than did offspring of women who never reported elevated symptoms.
It should be noted that in this paper we identified five latent classes of maternal depressive symptoms, whereas Campbell et al. (2007) identified six trajectories of symptoms using a different analytic technique. Several factors may account the slight discrepancies in patterns of maternal symptoms in these two analyses which both used the NICHD data set. The 2007 paper followed women from birth until their children were in first grade, that is for seven years, whereas in the current paper women were followed over a 12 year period. Thus, it is possible that fewer classes of symptoms emerged over this longer period of time. For example, the intermittent and moderate increasing trajectory groups identified by Campbell et al. (2007) may have merged into the moderately elevated group identified in the current analysis. Furthermore, the current analysis included sociodemographic indicators in modeling latent classes, in contrast to the earlier paper which utilized only CES-D scores to identify trajectories. In addition, in the Campbell et al. (2007) paper, only mothers with at least two CES-D scores were included (n = 1261), whereas the current analyses included all study mothers with a CES-D score at 1 month (n = 1363). The current analyses were, therefore, conducted on a somewhat larger sample. Despite these differences in analytic approach, the results are relatively similar in that both sets of analyses identified about 80% of mothers as showing very low to subclinical levels of symptoms over time, a small group showing chronic symptoms, and another 15-16% showing elevated, albeit variable patterns of symptoms over time.
The strengths of this study include the large sample followed prospectively from the study child’s birth, the frequent assessment of maternal depressive symptoms over a 12-year period, and the use of independent self-report measures to assess offspring adjustment in adolescence, 15 years after initial study recruitment. Moreover, the large community sample, selected for a study of child care rather than depression, means that this sample is relatively unbiased in terms of the issues under investigation in this report. However, this study also has several limitations including the reliance on questionnaire measures rather than diagnostic interviews to assess both maternal depressive symptoms and children’s outcomes. The inclusion of diagnostic interviews was beyond the scope of this study which focused on normal development in the context of family and child care experiences. Thus, our discussion focuses only on symptom levels and not diagnosable disorder. In addition, adolescent adjustment, even when poor relative to the offspring of mothers in the never-depressed latent class, was well below a clinical level of distress. In addition, we did not assess stressful life events in the family that may partly account for the course of maternal depressive symptoms and for offspring functioning. We also did not include a measure of stress in the adolescent’s life that may have contributed to adolescent difficulties. Moreover, it is well-documented that stress and depression go together in complex ways because people who are more dysphoric and irritable may generate as well as respond to stressful life events (Hammen et al., 2004; Rudolph & Flynn, 2007). Thus, this descriptive, longitudinal study does not elucidate mechanisms that may account for either the chronicity of maternal depression symptoms or the links between maternal symptoms and adolescent adjustment. In addition, we do not have data on whether mothers received treatment for their depression. Unfortunately, we also could not address the influence of race and ethnicity on either latent classes of maternal depressive symptoms or on adolescent outcomes. There may be cultural influences over and above basic sociodemographic indicators that influence both maternal mood and adolescent adjustment that were not captured in our measures.
A further limitation of this study is our inability to assess the degree to which the familiality of dysphoria and other adjustment difficulties that is evident in our data reflects genetic risk, environmental risk, or their interaction. Relatedly, we are unable to assess the degree to which child effects were operating. However, evidence from one twin study indicates that even with controls for genetic variation, parenting and other environmental risks that co-occur with mother’s depressive symptoms, maternal depression predicts adjustment difficulties in children (Kim-Cohen, Moffitt, Taylor, Pawlby, & Caspi, 2005). Future research with this data set that includes molecular genetic studies of adolescents and mothers may permit us to pursue this issue. Finally, analyses that examine more proximal family processes will be necessary to delineate the degree to which the quality of the mother-child relationship, the father-child relationship, and family social support, as well as events in the adolescent’s wider social network converge to either exacerbate problems or protect adolescents with chronically dysphoric mothers from developing more severe problems.
Acknowledgments
This study is directed by a Steering Committee and supported by NICHD through a cooperative agreement (U10), which calls for scientific collaboration between the grantees and the NICHD staff. The content is solely the responsibility of the named authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institutes of Health, or individual members of the Network. Current members of the Steering Committee of the NICHD Early Child Care Research Network, listed in alphabetical order, are: Jay Belsky (Birkbeck University of London), Cathryn Booth-LaForce (University of Washington), Robert H. Bradley (University of Arkansas at Little Rock), Celia A. Brownell (University of Pittsburgh) , Margaret Burchinal (University of North Carolina, Chapel Hill), Susan B. Campbell (University of Pittsburgh), Elizabeth Cauffman (University of California, Irvine), Alison Clarke-Stewart (University of California, Irvine), Martha Cox (University of North Carolina, Chapel Hill), Robert Crosnoe (University of Texas, Austin), James A. Griffin (NICHD Project Scientist and Scientific Coordinator), Bonnie Halpern-Felsher (University of California, San Francisco), Willard Hartup (University of Minnesota), Kathryn Hirsh-Pasek (Temple University), Daniel Keating (University of Michigan, Ann Arbor), Bonnie Knoke (RTI International), Tama Leventhal (Tufts University), Kathleen McCartney (Harvard University), Vonnie C. McLoyd (University of North Carolina, Chapel Hill), Fred Morrison (University of Michigan, Ann Arbor), Philip Nader (University of California, San Diego), Marion O’Brien (University of North Carolina, Greensboro), Margaret Tresch Owen (University of Texas, Dallas), Ross Parke (University of California, Riverside), Robert Pianta (University of Virginia), Kim M. Pierce (University of Wisconsin-Madison), A. Vijaya Rao (RTI International), Glenn I. Roisman (University of Illinois at Urbana-Champaign), Susan Spieker (University of Washington), Laurence Steinberg (Temple University), Elizabeth Susman (Pennsylvania State University), Deborah Lowe Vandell (University of California, Irvine), and Marsha Weinraub (Temple University).
We express our appreciation to the study coordinators at each site who oversaw the data collection, the research assistants who collected the data, and especially to the mothers and children who cooperated so willingly with our repeated requests for information.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/journals/abn.
Contributor Information
Susan B. Campbell, University of Pittsburgh
Antonio A. Morgan-Lopez, RTI International
References
- Achenbach TM. Manual for the Youth Self-Report and 1991 Profile. University of Vermont Department of Psychiatry; Burlington, VT: 1991. [Google Scholar]
- Angold A, Erklani A, Silberg J, Eaves L, Costello EJ. Depression scale scores in 8-17 year-olds: Effects of age and gender. Journal of Child Psychology and Psychiatry. 2002;43:1052–1063. doi: 10.1111/1469-7610.00232. [DOI] [PubMed] [Google Scholar]
- Appleyard K, Egeland B, van Dulmen M, Sroufe LA. When more is not better: The role of cumulative risk in child behavior outcomes. Journal of Child Psychology and Psychiatry. 2005;46:235–245. doi: 10.1111/j.1469-7610.2004.00351.x. [DOI] [PubMed] [Google Scholar]
- Asher SR, Hymel S, Renshaw RD. Loneliness in children. Child Development. 1984;55:1456–464. [Google Scholar]
- Brown GW, Harris TO. The social origins of depression. Free Press; London: 1978. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Brownell CA, Hungerford A, Spieker S, Mohan R, Blessing JS. The course of maternal depressive symptoms and maternal sensitivity as predictors of attachment security at 36 months. Development and Psychopathology. 2004;16:231–252. doi: 10.1017/s0954579404044499. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Cohn JF, Flanagan C, Popper S, Meyers T. The course and correlates of postpartum depression during the transition to parenthood. Development and Psychopathology. 1992;4:29–47. [Google Scholar]
- Campbell SB, Matestic P, von Stauffenberg C, Mohan R, Kirchner T. Trajectories of maternal depressive symptoms, maternal sensitivity, and children’s functioning at school entry. Developmental Psychology. 2007;43:1202–1215. doi: 10.1037/0012-1649.43.5.1202. [DOI] [PubMed] [Google Scholar]
- Capaldi DM. The co-occurrence of conduct problems and depressive symptoms in early adolescent boys: II. A 2-year follow-up at grade 8. Development and Psychopathology. 1992;4:125–144. doi: 10.1017/s0954579499001959. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Toth SL. Maternal depressive disorder and contextual risk: Contributions to the development of attachment insecurity and behavior problems in toddlerhood. Development and Psychopathology. 1998;10:283–300. doi: 10.1017/s0954579498001618. [DOI] [PubMed] [Google Scholar]
- Conger RD, Elder GH. Families in troubled times: Adapting to changes in rural America. Aldine de Gruyter; New York: 1994. [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Davies PT, Campbell SB. Developmental psychopathology and family process. Guilford Press; New York: 2000. [Google Scholar]
- Davies PT, Windle M. Gender specific pathways between maternal depressive symptoms, family discord, and adolescent adjustment. Developmental Psychology. 1997;33:657–668. doi: 10.1037//0012-1649.33.4.657. [DOI] [PubMed] [Google Scholar]
- Dawson G, Ashman SB, Panagiotides H, Hessl D, Self J, Yamada E, et al. Preschool outcomes of children of depressed mothers: Role of maternal behavior, contextual risk, and children’s brain activity. Child Development. 2003;74:1158–1175. doi: 10.1111/1467-8624.00599. [DOI] [PubMed] [Google Scholar]
- Downey G, Coyne JC. Children of depressed parents: An integrative review. Psychological Bulletin. 1990;108:50–76. doi: 10.1037/0033-2909.108.1.50. [DOI] [PubMed] [Google Scholar]
- Foster CJE, Garber J, Durlak J. Current and past maternal depression, maternal interaction behaviors, and children’s externalizing and internalizing symptoms. Journal of Abnormal Child Psychology. 2008;36:527–537. doi: 10.1007/s10802-007-9197-1. [DOI] [PubMed] [Google Scholar]
- Frye AA, Garber J. Relations among maternal depression, maternal criticism, and adolescents’ externalizing and internalizing symptoms. Journal of Abnormal Child Psychology. 2005;33:1–11. doi: 10.1007/s10802-005-0929-9. [DOI] [PubMed] [Google Scholar]
- Garber J, Keiley MK, Martin NC. Developmental trajectories of adolescents’ depressive symptoms: Predictors of change. Journal of Consulting and Clinical Psychology. 2002;70:79–95. doi: 10.1037//0022-006x.70.1.79. [DOI] [PubMed] [Google Scholar]
- Garber J, Little SA. Emotional autonomy and adolescent adjustment. Journal of Adolescent Research. 2001;16:355–371. [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Goodman S, Gotlib I. Children of depressed parents: Mechanisms of risk and implications for treatment. American Psychological Association; Washington, DC: 2002. [Google Scholar]
- Halpern-Felsher BL, Biehl M, Kropp RY, Rubenstein ML. Differences between adolescents with different smoking experiences and intentions. Preventive Medicine. 2004;39:559–567. doi: 10.1016/j.ypmed.2004.02.017. [DOI] [PubMed] [Google Scholar]
- Hammen C. Depression runs in families: The social context of risk and resilience in children of depressed parents. Springer-Verlag; New York: 1991. [Google Scholar]
- Hammen C. The context of stress in families of children with depressed parents. In: Goodman S, Gotlib I, editors. Children of depressed parents: Mechanisms of risk and implications for treatment. American Psychological Association; Washington, DC: 2002. pp. 175–199. [Google Scholar]
- Hammen C, Brennan PA. Severity, chronicity, and timing of maternal depression and risk for adolescent diagnoses in a community sample. Archives of General Psychiatry. 2003;60:253–258. doi: 10.1001/archpsyc.60.3.253. [DOI] [PubMed] [Google Scholar]
- Hammen C, Shih JH, Brennan PA. Intergenerational transmission of depression: test of an interpersonal stress model in a community sample. Journal of Consulting and Clinical Psychology. 2004;72:511–522. doi: 10.1037/0022-006X.72.3.511. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: Emerging gender differences in a longitudinal study. Journal of Abnormal Psychology. 1998;107:128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Mermelstein R, Roesch L. Sex differences in adolescent depression: stress exposure and reactivity models. Child Development. 2007;78:279–295. doi: 10.1111/j.1467-8624.2007.00997.x. [DOI] [PubMed] [Google Scholar]
- Hopkins J, Campbell SB. Development and validation of a scale to assess social support in the postpartum period. Archives of Women’s Mental Health. 2008;11:57–65. doi: 10.1007/s00737-008-0212-5. [DOI] [PubMed] [Google Scholar]
- Hyde JS, Mezulis AH, Abramson LY. The ABCs of depression: Integrating affective, biological, and cognitive models to explain the gender difference is depression. Psychological Review. 2008;115:291–313. doi: 10.1037/0033-295X.115.2.291. [DOI] [PubMed] [Google Scholar]
- Kaplow J, Curran PJ, Dodge K, the Conduct Problems Prevention Research Group Child, parent, and peer predictors of early-onset substance use: A multisite longitudinal study. Journal of Abnormal Child Psychology. 2002;30:199–216. doi: 10.1023/a:1015183927979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessing LV. Severity of depressive episodes during the course of depressive disorder. British Journal of Psychiatry. 2008;192:290–293. doi: 10.1192/bjp.bp.107.038935. [DOI] [PubMed] [Google Scholar]
- Kim KJ, Conger RD, Elder GH, Jr., Lorenz FO. Reciprocal influences between stressful life events and adolescent internalizing and externalizing problems. Child Development. 2003;74:127–143. doi: 10.1111/1467-8624.00525. [DOI] [PubMed] [Google Scholar]
- Kim-Cohen J, Moffitt TE, Taylor A, Pawlby SJ, Caspi A. Maternal depression and children’s antisocial behavior: Nature and nurture effects. Archives of General Psychiatry. 2005;62:173–181. doi: 10.1001/archpsyc.62.2.173. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Manual for the Children’s Depression Inventory. Multi-Health Systems; North Tonawanda, NY: 2001. [Google Scholar]
- Leadbeater BJ, Bishop SJ, Raver CC. Quality of mother-toddler interactions, maternal depressive symptoms, and behavior problems in preschool children of adolescent mothers. Developmental Psychology. 1996;32:280–288. [Google Scholar]
- McMahon SD, Grant KE, Compas BE, Thurm AE, Ey S. Stress and psychopathology in children and adolescents: is there evidence of specificity? Journal of Child Psychology and Psychiatry. 2003;44:107–133. doi: 10.1111/1469-7610.00105. [DOI] [PubMed] [Google Scholar]
- Morgan-Lopez AA, Fals-Stewart W. Analytic methods for modeling longitudinal data from rolling therapy groups with membership turnover. Journal of Consulting and Clinical Psychology. 2007;75:580–593. doi: 10.1037/0022-006X.75.4.580. [DOI] [PubMed] [Google Scholar]
- Muthén B. Beyond SEM: General latent variable modeling. Behaviormetrika. 2002;29:81–117. [Google Scholar]
- Muthén LK, Muthén BO. Mplus Users Guide. Fourth Edition Muthén & Muthén; Los Angeles: 1998-2006. [Google Scholar]
- Nagin DS. Group-based modeling of development. Harvard University Press; Cambridge, MA: 2005. [Google Scholar]
- Nelson DR, Hammen C, Brennan PA, Ullman JB. The impact of maternal depression on adolescent adjustment: The role of expressed emotion. Journal of Consulting and Clinical Psychology. 2003;71:935–944. doi: 10.1037/0022-006X.71.5.935. [DOI] [PubMed] [Google Scholar]
- NICHD Early Child Care Research Network The course of maternal depressive symptoms, maternal sensitivity, and child outcomes. Developmental Psychology. 1999;35:1297–1310. doi: 10.1037//0012-1649.35.5.1297. [DOI] [PubMed] [Google Scholar]
- NICHD Early Child Care Research Network Trajectories of aggression from toddlerhood to middle childhood: Predictors, correlates, and outcomes. Monographs of the Society for Research in Child Development. 2004;69 doi: 10.1111/j.0037-976x.2004.00312.x. whole no. 4. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Girgus JS. The emergence of gender differences in depression during adolescence. Psychological Bulletin. 1994;115:424–443. doi: 10.1037/0033-2909.115.3.424. [DOI] [PubMed] [Google Scholar]
- Offord DR, Boyle MH, Fleming JE, Monroe-Blum H, Rae-Grant N. The Ontario Child Health Study: Summary of selected results. Canadian Journal of Psychiatry. 1989;34:483–491. doi: 10.1177/070674378903400602. [DOI] [PubMed] [Google Scholar]
- Otto MW, Teachman BA, Cohen LS, Soares CN, Vitonis AF, Harlow BL. Dysfunctional attitudes and episodes of major depression: predictive validity and temporal stability in never-depressed, depressed, and recovered women. Journal of Abnormal Psychology. 2007;116:475–483. doi: 10.1037/0021-843X.116.3.475. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rosenthal R, Rosnow RL. Essentials of behavioral research: methods and data analysis. 2nd ed McGraw Hill; New York: 1991. [Google Scholar]
- Rudolph KD, Flynn M. Childhood adversity and youth depression: influence of gender and pubertal status. Development and Psychopathology. 2007;19:497–521. doi: 10.1017/S0954579407070241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Seifer R, Sameroff A, Dickstein S, Keitner G, Miller I, Rasmussen S, Hayden M. Parental psychopathology, multiple contextual risks, and one-year outcomes in children. Journal of Clinical Child Psychology. 1996;25:423–435. [Google Scholar]
- Sheeber LB, Davis B, Leve C, Hops H, Tildesley E. Adolescents’ relationships with their mothers and fathers: Associations with depressive disorder and subdiagnostic symptomatology. Journal of Abnormal Psychology. 2007;116:144–154. doi: 10.1037/0021-843X.116.1.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L, Silk JS. Parenting adolescents. In: Borenstein MH, editor. Handbook of parenting. 2nd ed Vol. I. Children and parenting. Erlbaum; Mahwah, NJ: 2002. pp. 103–133. [Google Scholar]
- Weissman MM, Pilowsky DJ, Wickramartne PJ, Talati A, et al. Remissions in maternal depression and child psychopathology: A STAR*D-Child report. Journal of the American Medical Association. 2006;295:1389–1398. doi: 10.1001/jama.295.12.1389. [DOI] [PubMed] [Google Scholar]
- Wiesner M, Kim HK. Co-occurring delinquency and depressive symptoms of adolescent girls and boys: A dual trajectory modeling approach. Developmental Psychology. 2006;42:1220–1235. doi: 10.1037/0012-1649.42.6.1220. [DOI] [PubMed] [Google Scholar]
- Yuan KH, Bentler PM. Three likelihood-based methods for mean and covariance structure analysis with non-normal missing data. Sociological Methodology. 2000;30:165–200. [Google Scholar]