Abstract
Aim
This paper is a report of a study to identify critical thinking learning needs of new and experienced nurses.
Background
Concern for patient safety has grown worldwide as high rates of error and injury continue to be reported. In order to improve patient safety, nurses must be able to recognize changes in patient condition, perform independent nursing interventions, anticipate orders and prioritize.
Methods
In 2004–2006, a consecutive sample of 2144 newly hired nurses in a university-affiliated healthcare system completed the Performance Based Development System Assessment consisting of 10 videotaped vignettes depicting change in patient status. Results were reported as meeting or not meeting expectations. For nurses not meeting expectations, learning needs were identified in one of six sub-categories.
Results
Overall, 74.9% met assessment expectations. Learning needs identified for nurses not meeting expectations included initiating independent nursing interventions (97.2%), differentiation of urgency (67%), reporting essential clinical data (65.4%), anticipating relevant medical orders (62.8%), providing relevant rationale to support decisions (62.6%) and problem recognition (57.1%). Controlling for level of preparation, associate (P = 0.007) and baccalaureate (P < 0.0001) nurses were more likely to meet expectations as years of experience increased; a similar trend was not seen for diploma nurses (P = 0.10). Controlling for years of experience, new graduates were less likely to meet expectations compared with nurses with ≥10 years experience (P = 0.046).
Conclusion
Patient safety may be compromised if a nurse cannot provide clinically competent care. Assessments such as the Performance Based Development System can provide information about learning needs and facilitate individualized orientation targeted to increase performance level.
Keywords: competence, critical thinking, graduates, learning needs, nurses, patient safety, Performance Based Development System
Introduction
Concern for patient safety has grown worldwide as high rates of error and injury continue to be reported. A recent Commonwealth Fund international survey of six nations showed that between one-quarter and one-third of patients with health problems experienced medical, medication, or testing errors. A number of countries, including the United States of America, Australia, Canada, Germany, New Zealand and the United Kingdom, have identified a need for improvement in the coordination and delivery of care (Schoen et al. 2005) and a reduction in preventable medical errors (Kohn & Donaldson 2000).
Patient safety can be directly affected by the critical thinking ability of a nurse. Nurses must have the ability to recognize changes in patient condition, perform independent nursing interventions, anticipate orders and prioritize (Buerhaus et al. 2005). These actions require critical thinking ability, advanced problem-solving skills and the ability to communicate clearly (NACNEP 1996). Using root cause analysis, the Joint Commission on the Accreditation of Healthcare Organizational Standards (JCAHO) identified orientation, training, and competence assessment as top factors contributing to patient safety errors over the past 10 years (1995–2005) (JCAHO 2006).
New graduate nurses practise at the novice or advanced beginner level (Benner 1984). They are at the early stage of developing a skill set and applying critical thinking. Nursing shortages and budgetary issues may mean that initial orientation periods for new graduates are shortened (AORN 2006), a potential factor prompting the increase in errors. One means of determining whether new graduates and more experienced nurses can demonstrate the critical thinking ability necessary to ensure patient safety involves asking them to complete a performance-based evaluation.
Background
Patient safety
Patient safety is at the center of today’s healthcare system reform. According to the Institute of Medicine (IOM), more than 98,000 people in the United States of America (USA) die and more than one million patients suffer injuries each year (Kohn & Donaldson 2000). Thirty to 40 percent of every US dollar spent on healthcare is lost to inappropriate use, poor communication, and inefficiency (Proctor et al. 2005). The IOM aims for the 21st century healthcare system include providing safe, effective, patient-centered care that is timely, efficient, and equitable (IOM 2001).
Nursing competence plays a large role in assuring patient safety (IOM 2004). A majority of sentinel events occur in acute care settings, where new graduate nurses traditionally begin their professional careers (JCAHO 2006). According to the Joint Commission International Center for Patient Safety, over 70% of sentinel events reported resulted in a patient’s death and 10% resulted in loss of function (JCRINC 2007). The inability of a nurse to set priorities and work effectively and efficiently may delay patient treatment in a critical situation and result in serious life-threatening consequences (Redfern et al. 2002).
Competence
The definition of nursing competence has been extensively debated (Redfern et al. 2002). Competence can be the subject of objective evaluation which includes standardized measurement or subjective observational reporting. In the USA, the only universally accepted method of evaluating competence occurs at entry to practise via the National Council Licensure Examination-Registered Nurse or NCLEX-RN© (NCSBN 2007). This examination does not, however, address ongoing assessment, and there is no agreement on how continued assessment should be accomplished. Current measurement tools do not take into account the evolution of practice with experience or identify areas of weakness in which healthcare organizations should focus orientation or remediation efforts (NCSBN 2005). Therefore, the IOM has encouraged the development of more effective methods to identify and take action when providers are unsafe (Kohn & Donaldson 2000).
Benner (1984) argues that competency assessment should be grounded in actual practice, under pressure, and over time. She further argues that assessment should be related to patient outcome and be context-specific (Benner 1984). The Performance Based Development System (PBDS) assessment is an attempt to evaluate actual performance and remediate deficiencies within the orientation period.
Critical thinking
Critical thinking has been discussed since the time of Socrates and its dimensions have been explored by numerous scholars from Thomas Aquinas to John Dewey (Facione 1990). However, it was not until the late 1980s that the nursing profession began to question how critical thinking relates to clinical practice and to evaluate ways to measure how effectively the educational system achieves critical thinking competence through its curriculum. This movement was started, in part, to address the directive of the US National League of Nursing to measure critical thinking as an outcome criterion for the accreditation of nursing programmes (AACN 1998; Rubenfeld & Scheffer 1999, Scheffer & Rubenfeld 2000, Simpson & Courtney 2002).
There is no widely accepted definition of critical thinking in the field of nursing, psychology, or education (Simpson & Courtney 2002). Scholars have found the concept very difficult to quantify and therefore to measure, leading to a wide array of interpretations (Hynes & Bennett 2004). In 1988, a Delphi panel was established at the request of the American Philosophical Association to synthesize expert opinion on the concept of critical thinking. The panel identified interpretation, analysis, evaluation, inference, explanation, and self-regulation as necessary components (Facione 1990).
The term critical thinking is often used interchangeably with problem-solving, clinical decision-making, and creative thinking in the nursing literature (Simpson & Courtney 2002). Problem-solving focuses on identification and resolution, whereas critical thinking goes beyond this and incorporates asking questions and critiquing solutions. The notion of clinical decision-making focuses attention on the clinical nature of a problem but falls short of facilitating understanding of the broader spectrum of the issue. Decision-making and critical thinking need to occur concurrently to produce reasoning, clarification, and potential solutions. Creative thinking is a combination of imagination and knowledge (Simpson & Courtney 2002). It helps one to understand solutions that have failed and is certainly part of the subset of skills necessary to be an effective critical thinker.
In order to advance practice, it is necessary to develop and evaluate strategies to help nurses develop essential skills. Most studies show that there is a progression in nursing students’ ability to critically think through their education tenure (Colucciello 1997, Thompson & Rebeschi 1999, Giddens & Gloeckner 2005). However, the literature does not identify specific areas of needed attention. In addition, most studies take place in the context of a nursing education programme, rather than following graduation (Colucciello 1997, May et al. 1999, Thompson & Rebeschi 1999, Beckie et al. 2001, Chau et al. 2001, Giddens & Gloeckner 2005). To develop in new graduates the responsibilities inherent in clinical practice most effectively, new approaches are needed, and these approaches should be objectively evaluated to determine their effectiveness prior to implementation.
The Performance Based Development System
The PBDS is designed to provide such an assessment (Performance Management Services, Inc. 2006). The Clinical Judgment portion of the PBDS assessment consists of 10 videotaped vignettes which depict common clinical problems that nurses may encounter on a medical-surgical unit (e.g. onset of dyspnea, anxiety, or change in mental status). Respondents are asked to view each vignette and then state, in writing, what they think the problem is, actions they would take in response, and their rationale. The PBDS assessment is designed to identify critical thinking learning needs and assist in the development of an individualized orientation action plan to prepare better nurses for safe clinical practice (Performance Management Services, Inc. 2006). Although the PBDS assessment has been in use since 1985 in over 500 healthcare organizations, reports of its use are limited to descriptive studies (del Bueno 2001, 2005, Performance Management Services, Inc. 2006).
Conceptual framework
The purpose of this study was to identify critical thinking learning needs of new and experienced nurses with varying levels of preparation (diploma, associate, baccalaureate degree). The expectation was that nurses having more years of experience and those prepared at the baccalaureate level would have a higher rate of meeting expectations on the PBDS assessment. The theoretical framework guiding this expectation was Patricia Benner’s Novice to Expert Model (Benner 1984). This model was developed through descriptive research using the Dreyfus Model of Skill Acquisition, which identified five levels of competence. These levels are novice, advanced beginner, competent, proficient and expert (Dreyfus 1980). The novice level applies to nurses who have no experience in the environment in which they are expected to perform (Benner 1984). For the purpose of this study, a novice was defined as a new nursing graduate with limited exposure to independently managing a critical situation who operates in a limited and prescribed way. An advanced beginner performs at a marginally acceptable level. At this level, nurses recognize the meaning of a critical situation but may not understand or anticipate the care needed. A competent practitioner begins to see their actions in terms of long-range planning (Benner 1984). A competent nurse is able to determine which aspects of a situation are considered more relevant. This practice level entails planning, considering, analyzing, and contemplating which action to take. After reaching the proficient level, a nurse begins to perceive the meaning of a situation through reflection on previous experience, and often modifies plans based on the response to the event. At the expert level, a nurse has an intuitive grasp of a critical situation and understands deeply what is needed to ensure resolution (Benner 1984).
The novice to expert framework is the basis for a number of clinical ladders in healthcare and is often used to formalize promotional structures and drive work role competencies (Benner 1984). In addition, it has served as a catalyst for staff development programmes with the aim of facilitating nursing excellence. The novice to expert framework has been applied to gain insight into managing clinical problems, practice skills, and communication through innovative teaching methods (Larew et al. 2006).
The study
Aim
The aim of the study was to identify critical thinking learning needs of new and experienced nurses.
The specific objectives were to (1) describe the overall rate at which nurses meet expectations on the PBDS assessment; (2) examine the relationship between meeting PBDS expectations and years of nursing experience controlling for preparation level; and (3) examine the relationship between meeting PBDS expectations and nurses’ preparation level (diploma, associate, baccalaureate) controlling for years of nursing experience.
Design
The study was a post hoc retrospective analysis of PBDS assessment data collected prospectively during the initial 2 weeks of employment of 2144 newly hired nurses.
Participants
All nurses employed by the same university healthcare system from 1 January 2004 to 30 September 2006 were eligible for inclusion in the study. The healthcare system which provided the de-identified data included 19 acute care, specialty, community and regional hospitals located in southwestern Pennsylvania, USA. All newly hired nurses were assessed using the PBDS in order to customize their orientation at the beginning of their employment tenure.
The sample included nurses prepared at the diploma, associate or baccalaureate level. Diploma programmes offer hospital-based nursing preparation that is typically 2 years in length; courses in the programme are taught by hospital-based educators and may include some college credit. Graduates receive a nursing diploma and are prepared to function at the staff nurse level in hospitals or inpatient facilities. Associate degree programmes are provided by a community college and are typically 2 years in length. Graduates receive an associate degree and are prepared to function at the staff nurse level in hospitals or inpatient facilities. Baccalaureate-prepared nurses attend a 4-year programme offered by a college or university. Graduates receive a baccalaureate degree and are prepared to assume leadership roles in hospitals, inpatient facilities and community settings (All Star Directories, Inc. 2002–2008).
We achieved a power of 90% to detect an effect size (W) of 0.0813 using a chi-square test of independence with 3 d.f. (Specific Aim 2) and 90% power to detect an effect size (W) of 0.0768 using a chi-square test of independence with 2 d.f. (Specific Aim 3) for two-sided hypothesis testing at a statistical significance level of 0.05. Specific Aim 1 was descriptive and not included in sample size estimates.
Data collection
Data were obtained from files of the Nursing Education Department and included demographic data and hard copy summaries of the PBDS assessments. Data regarding the number of individuals who took the PBDS, years of experience, level of preparation and ratings (met, did not meet expectations) were obtained (Table 1). Hard copy records of nurses who did not meet expectations on the assessment were identified. All personal identifiers were removed and de-identified hard copies of the assessment were forwarded to the research team for analysis.
Table 1.
Frequency counts and percentages by degree and years of experience in nursing (n = 2144) Characteristic Newly hired nurses, n = 2144
| Performance Based Development System |
|||
|---|---|---|---|
| Characteristic | Newly hired nurses, n = 2144 | Met expectations n = 1605 (74.9%) | Did not meet expectations n = 539 (25.1%) |
| Educational preparation | |||
| Diploma | 674 (31.4%) | 518 (76.9) | 156 (23.1) |
| Associate | 880 (41.0%) | 637 (72.4) | 243 (27.6) |
| Baccalaureate | 590 (27.6%) | 450 (76.3) | 140 (23.7) |
| Experience | |||
| ≤1 year | 1211 (56.5%) | 866 (71.5) | 345 (28.5) |
| >1 but <5 years | 197 (9.2%) | 152 (77.2) | 45 (22.8) |
| ≥5 but <10 years | 211 (9.8%) | 158 (74.9) | 53 (25.1) |
| ≥10 years | 525 (24.5%) | 429 (81.7) | 96 (18.3) |
Performance Based Development System Assessment were administered and rated based on the process developed by Performance Management Services, Inc. (2006). Responses were rated by nurses who, by comparing respondents’ answers to model answers, determined if they met or did not meet expectations in the following six subcategories: problem recognition, reports essential clinical data, initiates independent nursing interventions, differentiation of urgency, anticipates relevant medical orders, and provides relevant rationale to support decisions (Table 2). For example, if a nurse was presented with a clinical case in which the patient was recovering from surgery and receiving blood products and experienced an elevated temperature, hives, and chills, it would be expected that they would recognize that the patient was having a blood transfusion reaction, report essential clinical findings to the physician, and prepare to treat the patient based on the orders received.
Table 2.
Subcategory rating matrix for model Performance Based Development System Assessment
| Subcategory | Category | Expected answer (met expectations) | Experienced nurse (>1 year’s experience) | New graduate (≤1 year’s experience) |
|---|---|---|---|---|
| 1 | Problem recognition | Recognizes blood transfusion reaction | Included | Included |
| 2 | Reports essential clinical data | Reports elevated temperature, hives, and chills to the physician | Included | Included |
| 3 | Initiates independent nursing interventions | Stops the blood immediately, checks the blood type and sends it for analysis, monitors vital signs, provides reassurance and comfort to the patient | Included | Included |
| 4 | Differentiate urgency | Notifies the physician immediately of the situation | Included | Included |
| 5 | Anticipates relevant medical orders | Anticipates intravenous fluids, administration of antihistamine and antipyretic medications | Included | Not Included |
| 6 | Provides relevant rationale | Appropriate rationale stated for each subcategory | Shared with preceptor | Shared with preceptor |
| Overall rating = met expectations | Experienced nurses = must meet expectations on subcategory 1–5 New graduate = must meet expectations on subcategory 1–4. Subcategory 6 is rated as met/did not meet expectations; rating is shared with unit preceptor but not included in overall rating |
|||
The PBDS overall assessment rating (met or did not meet expectations) was developed using a three-step process. Those taking the assessment were first given a preset amount of time to view a series of 10 videotaped vignettes depicting common clinical problems and write their responses. The nurse rater next determined if the nurse met expectations for each vignette using the method illustrated in Table 2. Using an organizational algorithm reflecting patterns of inconsistency and safety in the answers that was based on the ability to meet expectations in each of the subcategories, the nurse rater then determined an overall assessment rating (met/did not meet expectations) for each nurse. When learning needs were identified, they were included in a summary given to the preceptor, along with an action plan to guide clinical orientation activities. The individual summary and action plan was sent to the unit manager and nurse educator to share with the orientee and preceptor. The nurse raters (n = 5) all had Master’s degrees and over 10 years of clinical experience, and completed 9–12 months of PBDS rater training. Annual assessments were performed to determine inter-rater reliability and to validate rater competence. One nurse was assigned to rate all subcategories of each assessment. The department rates over 1000 PBDS assessments per year.
Validity and reliability
Reliability and validity of the PBDS assessment have been reported in previous publications (del Bueno 1990, 1994, 2001, 2005). Reliability estimates for the clinical vignettes, obtained using an equivalence approach, averaged 94% for individuals tested in parallel situations (del Bueno 1990).
Ethical considerations
Approval for the study was obtained from a university institutional review board. Study data were de-identified; therefore participant consent was not required.
Data analysis
Descriptive statistics were calculated using SPSS, version 14.0. Descriptive data were available for the entire sample and included years of experience, academic preparation, and the overall assessment rating. Of the 539 nurses who did not meet expectations, 103 (19.1%) did not have complete subcategory scores and therefore were excluded when analyzing these scores. The chi-square test for independence likelihood ratio and Pearson chi-square were used to analyze differences in years of experience and level of preparation. The likelihood ratio was used because of the large sample size. The level of statistical significance was set a priori at 0.05.
Results
Of the sample, 31.4% were diploma graduates, 41.0% associate degree graduates and 27.6% baccalaureate graduates (Table 1). The majority (56.5%) were new graduates, defined as having ≤1 year of experience, while 24.5% had 10 or more years of experience.
Meeting PBDS expectations and areas of deficiency
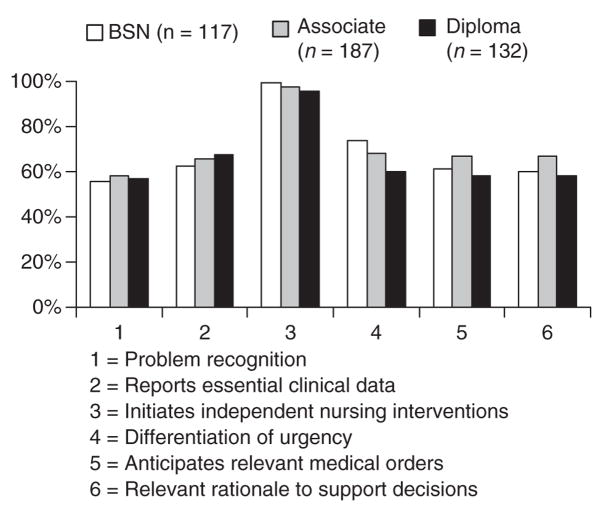
The majority of newly hired nurses (74.9%) met expectations on the PBDS assessment. Of those who did not meet expectations, 436 (81%) had complete subcategory information. PBDS results indicated that 97.2% did not initiate appropriate nursing interventions, 67.0% did not differentiate urgency, 65.4% did not report essential clinical data, 62.8% did not anticipate relevant medical orders, 62.6% did not understand their decision rationale and 57.1% were deficient in problem recognition. Figure 1 summarizes the percentage of newly hired nurses not meeting expectations by subcategory and level of preparation.
Figure 1.
Percentage of the sample (n = 436) not meeting expectations by subcategory and level of preparation.
Meeting PBDS expectations and years of experience
New graduates comprised 56.5% (n = 1211) of the sample. The remaining nurses were categorized into >1 but <5 years of experience (n = 197), ≥5 but <10 years of experience (n = 211) and ≥10 years of experience (n = 525). Years of experience differed statistically significantly in those meeting or failing to meet expectations (χ2 = 21.631, d.f. = 3, P < 0.0004): those with the least experience had the highest rate of not meeting expectations, while those with the most experience had the lowest rate.
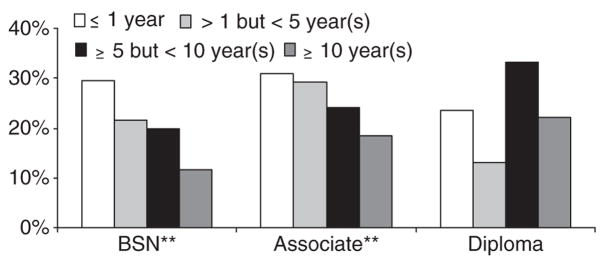
Controlling for level of preparation (diploma, associate, baccalaureate), rates at which nurses met expectations differed statistically significantly in those prepared at associate (χ2 = 12.085, d.f. = 3, P = 0.007) and baccalaureate levels (χ2 = 18.498, d.f. = 3, P < 0.0001) based on years of experience. Of these, 29.6% of the new graduates prepared at the baccalaureate level did not meet expectations on the PBDS, whereas only 11.5% with ≥10 years did not meet expectations (Figure 2). At the associate level 31.0% of the new graduates did not meet expectations whereas 18.3% with ≥10 years did not meet expectations. In contrast, there were no statistically significant differences in the rate of meeting expectations for nurses prepared at the diploma level based on years of experience (χ2 = 6.259, d.f. = 3, P = 0.100).
Figure 2.
Percentage of the sample (n = 539) not meeting expectations on the Performance Based Development System by years of experience and degree.
Meeting PBDS expectations and level of preparation
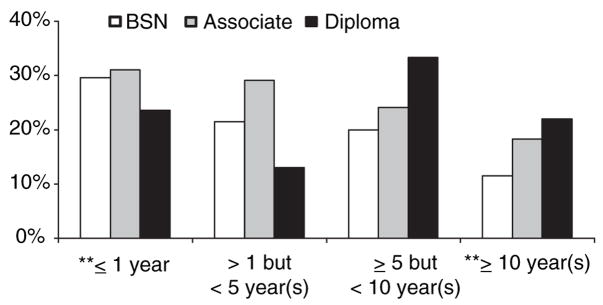
There was no statistically significant difference in the rate of meeting or not meeting expectations with regard to level of preparation when the data were analyzed for the total sample (χ2 = 4.886, d.f. = 2, P = 0.087). However, on controlling for years of experience, new graduates (χ2 = 6.158, d.f. = 2, P = 0.046) and nurses with ≥10 years of experience (χ2 = 6.179, d.f. = 2, P = 0.046) differed statistically significantly in pass rates (in those with ≥10 years of experience, the likelihood ratio was statistically significant at P = 0.046, but the Pearson chi-square was not (P = 0.055). New graduates prepared at the associate level did not meet expectations 31.0% of the time as compared with the baccalaureate (29.6%) and the diploma (23.6%) prepared graduates (Figure 3). In nurses with ≥10 years of experience, those prepared at the diploma level did not meet expectations 22.0% of the time as compared with the associate (18.3%) and baccalaureate (11.5%).
Figure 3.
Percentage of the sample (n = 539) not meeting expectations on the Performance Based Development System by degree and years of experience.
Discussion
Study limitations
This study had a number of limitations. The analysis was limited to data collected at the time of the PBDS assessment, i.e. level of preparation and years of nursing experience. Additional information on age, gender, prior healthcare experience in addition to nursing, employment location, and length of employment was not available. These and other potential predictor variables should be considered in future studies. The six subcategories delineating the reasons that newly hired nurses did not meet expectations on the assessment did not have complete data in 19.1% of cases. It is possible that these individuals differed from others with complete subcategory data. Finally, the assessment was based on simulated vignettes, and it is possible that actual clinical decision-making may have differed from the stated actions.
Discussion of results
The results suggest that a substantial minority of these newly hired nurses had identified learning needs with regard to their ability to make appropriate decisions when asked to assess a clinically focused vignette. Overall, approximately 25% of nurses participating in the assessment were not able to recognize the clinical problem, safely prioritize care and implement independent nursing interventions. They appeared to have difficulty reporting relevant clinical data and anticipating medical orders, and were not able to convey clearly a rationale for their decision-making. It is unclear from the assessment process whether this resulted from lack of knowledge, lack of sufficient time to respond, or not completely presenting their rationale in writing. Nevertheless, it emphasizes the importance of continued assessment, mentoring and coaching to improve and validate decision-making skills.
The percentage of new graduates not meeting expectations in the present study did not fall within the range of previously published results (del Bueno 2005). In a study by del Bueno (2005), from a sample size of 10,988 inexperienced nurses (<1 year of experience) sampled between 1995 and 2004, between 65% and 76% did not meet expectations on the PBDS assessment. Of the 20,413 experienced nurses sampled in the same study, those not meeting expectations ranged between 8% and 69%. Experienced nurses not meeting expectations in the present study ranged from 18.3% to 25.1%. Areas of deficiency on subcategories from their reports were consistent with the present study.
Our findings suggest that, as would be anticipated, nurses with more years of experience were more likely to meet expectations on the PBDS assessment. However, there were differences related to level of preparation. Specifically, those with more experience who were prepared at the baccalaureate or associate level fared better on the assessment than experienced nurses with diploma level preparation. This finding may have resulted from differences in the scope of experience and/or commitment to continuing education fostered by the educational programme. Whether these or other reasons explain the differences are speculative, as our data did not suggest an explanation. This finding is not consistent with previous studies reporting PBDS results. In a study published in 2005, del Bueno reported that after 10 years of analysis there are no consistent findings which indicate differences in clinical judgment ability based on educational preparation or credentialing. Our findings, nevertheless, support a difference in testing outcome based on level of preparation. Further exploration is needed to determine the potential reasons for our results. Possible explanations include the value of and access to advancement via nursing education, the organizational emphasis placed on continuing education, or previous clinical experience.
What is already known about this topic.
Critical thinking, advanced problem-solving, and expert communication skills are an integral part of nursing practice and should be developed through nursing education programmes.
Many nurses with a year or less of experience fail to meet expectations on the Performance Based Development System Assessment.
What this paper adds.
Approximately 25% of newly hired nurses had deficiencies in critical thinking ability, including problem recognition, reporting essential clinical data, initiating independent nursing interventions, anticipating relevant medical orders, providing relevant rationale to support decisions, and differentiation of urgency.
Nurses prepared at the baccalaureate and associate level were more likely to meet expectations on the assessment as years of experience increased; a similar trend was not seen for diploma nurses.
New graduates were less likely to meet assessment expectations compared with nurses with 10 years’ experience or more.
Implications for practice and/or policy.
PBDS can assist in providing information about critical thinking learning needs and facilitate individualized orientation.
Further study is needed to identify areas of critical thinking deficiency and begin to test objective, innovative educational strategies that enhance critical thinking in the nursing population.
Our findings support Benner’s conceptualization in her novice to expert framework (Benner 1984). Nurses with more experience were better able to identify appropriate actions when viewing the clinical vignettes, as would be expected. While it is of concern that a substantial minority of newly hired nurses did not meet expectations, it is important to emphasize that 75% were able to state actions that indicated their ability to manage critical situations independently and anticipate the care needed. They were able to prioritize clinical needs, consider potential actions and modify the plan of care based on prior experience. As might be anticipated, new graduates had a higher rate of not meeting expectations and struggled with the ability to make and implement independent nursing interventions in these same clinical scenarios.
Alternative critical thinking assessment methods are coming into vogue, e.g. high fidelity human simulation (HFHS) (Henrichs et al. 2002, Nehring et al. 2002, Parr & Sweeney 2006). HFHS may be a better option for assessing critical thinking and decision-making as it provides evaluation activities that are more interactive and offers the added benefit of debriefing to facilitate learning (Henrichs et al. 2002, Feingold et al. 2004, Bearnson & Wiker 2005, O’Donnell et al. 2005, Trossman 2005). Like the PBDS assessment, the HFHS can be used as a group learning tool without patient risk (Schwid et al. 2002). HFHS provides a more realistic assessment that includes the ability to assess blood pressure, palpable pulses, heart sounds, breath sounds. In addition, it offers the ability to programme responses that mimic physiological actions and patient responses to the timing and selection of interventions (Euliano 2001, Lupien & George-Gay 2001, Kozlowski 2004). Accordingly, HFHS may facilitate assessment of critical thinking and decision-making (Duchscher 2003). Studies comparing the various methods of assessment remain few in number and therefore it is not possible to determine objectively which approach is the most valid and cost-effective for assessing the learning needs of new graduates and experienced nurses.
Conclusion
Assessments such as PBDS can provide information about learning needs and facilitate individualized orientation targeted to increase performance level. Evaluation of clinical competence is difficult, as there are few measures that capture how a nurse will perform in an actual clinical emergency when rapid decisions must be made in a complex and emotionally charged environment. Further research is needed to identify further specific areas of deficiency and begin to test objective, innovative educational strategies to enhance the critical thinking ability of both new graduates and experienced nurses. Although a time-intensive endeavor, the outcome has the potential to contribute greatly to the advancement of nursing practice and safe patient care.
Acknowledgments
Funding
The lead author was recipient of the T-32 Technology Grant: Research in Chronic and Critical Illness (T32 NR008857) Pre-Doctoral Fellowship for Doctoral Study at the University of Pittsburg, PA, USA.
Footnotes
Author contributions
LJF, CW, SW, TZ and LH were responsible for the study conception and design. LJF, CW and LH performed the data collection. LJF, TZ and LH performed the data analysis. LJF were responsible for the drafting of the manuscript. LJF, CW, SW, TZ and LH made critical revisions to the paper for important intellectual content. TZ provided statistical expertise. SW and LH provided 0 technical or material support. LH supervised the study. CW provided other contributions.
Contributor Information
Laura J. Fero, Doctoral Candidate, University of Pittsburgh School of Nursing, Pennsylvania, USA.
Catherine M. Witsberger, Clinical Nurse Educator, Nursing Education and Research, University of Pittsburgh Medical Center, Pennsylvania, USA.
Susan W. Wesmiller, Director, Nursing Education and Research, University of Pittsburgh Medical Center, Pennsylvania, USA.
Thomas G. Zullo, Professor Emeritus, Dental Public Health, University of Pittsburgh, Pennsylvania, USA.
Leslie A. Hoffman, Professor and Chair, Department of Acute/Tertiary Care, University of Pittsburgh School of Nursing, Pennsylvania, USA.
References
- AACN. The Essentials of Baccalaureate Education for Professional Nursing Practice. American Association of Colleges of Nursing; Washington, D.C: 1998. [Google Scholar]
- All Star Directories, Inc. Your Guide to Nursing Education and Careers. 2002–2008 Retrieved from http://www.allnursingschools.com on 14 March, 2008.
- AORN. Perioperative Orientation Resources: A Guide to Orientation, Recruitment, and Retention. 2006 Retrieved from http://www.aorn.org/Education/EducationResources/PerioperativeOrientationResources/ on 11 November 2006.
- Bearnson CS, Wiker KM. Human patient simulators: a new face in baccalaureate nursing education at Brigham Young University. Journal of Nursing Education. 2005;44(9):421–425. doi: 10.3928/01484834-20050901-07. [DOI] [PubMed] [Google Scholar]
- Beckie TM, Lowry LW, Barnett S. Assessing critical thinking in baccalaureate nursing students: a longitudinal study. Holistic Nursing Practice. 2001;15(3):18–26. doi: 10.1097/00004650-200104000-00006. [DOI] [PubMed] [Google Scholar]
- Benner P. From Novice to Expert: Excellence and Power in Clinical Nursing Practice. Prentice Hall Health, Upper Saddle River; 1984. [Google Scholar]
- del Bueno D. Experience, education, and nurses’ ability to make clinical judgments. Nursing Health Care. 1990;11(6):290–294. [PubMed] [Google Scholar]
- del Bueno D. Why can’t new grads think like nurses? Nurse Educator. 1994;19(4):9–11. doi: 10.1097/00006223-199407000-00008. [DOI] [PubMed] [Google Scholar]
- del Bueno D. Buyer beware: the cost of competence. Nursing Economics. 2001 19/6(November/December):250–257. [Google Scholar]
- del Bueno D. A crisis in critical thinking. Nurse Educator Perspectives. 2005;26(5):278–282. [PubMed] [Google Scholar]
- Buerhaus PI, Donelan K, Ulrich BT, Norman L, Williams M, Dittus R. Hospital RNs’ and CNOs’ perceptions of the impact of the nursing shortage on the quality of care. Nursing Economics. 2005;23(5):214–221. [PubMed] [Google Scholar]
- Chau JP, Chang AM, Lee IF, Ip WY, Lee DT, Wootton Y. Effects of using videotaped vignettes on enhancing students’ critical thinking ability in a baccalaureate nursing programme. Journal of Advanced Nursing. 2001;36(1):112–119. doi: 10.1046/j.1365-2648.2001.01948.x. [DOI] [PubMed] [Google Scholar]
- Colucciello ML. Critical thinking skills and dispositions of baccalaureate nursing students – a conceptual model for evaluation. Journal of Professional Nursing. 1997;13(4):236–245. doi: 10.1016/s8755-7223(97)80094-4. [DOI] [PubMed] [Google Scholar]
- Dreyfus S. A Five-Stage Model of the Mental Activities Involved in Direct Skill Acquisition. University of California; Berkeley: 1980. [Google Scholar]
- Duchscher JE. Critical thinking: perceptions of newly graduated female baccalaureate nurses. Journal of Nursing Education. 2003;42(1):14–27. doi: 10.3928/0148-4834-20030101-06. [DOI] [PubMed] [Google Scholar]
- Euliano TY. Small group teaching: clinical correlation with a human patient simulator. Advances in Physiology Education. 2001;25(1–4):36–43. doi: 10.1152/advances.2001.25.1.36. [DOI] [PubMed] [Google Scholar]
- Facione PA. Critical Thinking: A Statement of Expert Consensus for Purposes of Educational Assessment and Instruction. The California Academic Press; Millbrae, CA: 1990. [Google Scholar]
- Feingold CE, Calaluce M, Kallen MA. Computerized patient model and simulated clinical experiences: evaluation with baccalaureate nursing students. Journal of Nursing Education. 2004;43(4):156–163. doi: 10.3928/01484834-20040401-03. [DOI] [PubMed] [Google Scholar]
- Giddens J, Gloeckner GW. The relationship of critical thinking to performance on the NCLEX-RN. Journal of Nursing Education. 2005;44(2):85–89. doi: 10.3928/01484834-20050201-08. [DOI] [PubMed] [Google Scholar]
- Henrichs B, Rule A, Grady M, Ellis W. Nurse anesthesia students’ perceptions of the anesthesia patient simulator: a qualitative study. AANA Journal. 2002;70(3):219–225. [PubMed] [Google Scholar]
- Hynes P, Bennett J. About critical thinking. Dynamics. 2004;15(3):26–29. [PubMed] [Google Scholar]
- IOM. Crossing the Quality Chasm: A New Health System for the 21st Century. National Academy Press: Washington D.C; 2001. [PubMed] [Google Scholar]
- IOM. Insuring America’s Health: Principles and Recommendations. National Academy Press; Washington D.C.: 2004. [PubMed] [Google Scholar]
- JCAHO. Root Causes of Sentinel Events. 2006 Retrieved from http://www.jointcommission.org/SentinelEvents/Statistics/ on 8 September 2006.
- JCRINC. Preparing New Nurses with Effective Orientation, Training, and Education. 2007 Retrieved from http://www.jcrinc.com/8906/ on 19 August 2007.
- Kohn LC, Donaldson MS. To Err Is Human: Building a Safer Health System. National Academy Press: Washington, D.C; 2000. [PubMed] [Google Scholar]
- Kozlowski R. Smart dummies. Sarasota/Manatee Business. 2004 August;:24–29. [Google Scholar]
- Larew C, Lessans S, Spunt D, Foster D, Covington BG. Innovations in clinical simulation: application of Benner’s theory in an interactive patient care simulation. Nurse Educator Perspectives. 2006;27(1):16–21. [PubMed] [Google Scholar]
- Lupien AE, George-Gay B. Fuszard’s Innovative Teaching Strategies in Nursing: High-fidelity Patient Simulation. 3. Aspen Publishers, Inc; Gaithersburg: 2001. [Google Scholar]
- May BA, Edell V, Butell S, Doughty J, Langford C. Critical thinking and clinical competence: a study of their relationship in BSN seniors. Journal of Nursing Education. 1999;38(3):100–110. doi: 10.3928/0148-4834-19990301-04. [DOI] [PubMed] [Google Scholar]
- NACNEP. Report to the Secretary of the Department of Health and Human Services on the Basic Registered Nurse Workforce. Health Resources and Services Administration, Bureau of Health Professions, Division of Nursing; Rockville, MD: 1996 . [Google Scholar]
- NCSBN. Meeting the Ongoing Challenge of Continued Competence. Chicago, IL: 2005. [Google Scholar]
- NCSBN. National Council of State Boards of Nursing. 2007 Retrieved from http://www.ncsbn.org on 16 November 2007.
- Nehring W, Lashley F, Ellis W. Critical incident nursing management using human patient simulators. Nursing Education Perspectives. 2002;23(2):128–132. [Google Scholar]
- O’Donnell J, Beach M, Hoffman LA. Human Simulation Training in the ICU: Applicability, Value, and Disadvantage. University of Pittsburgh School of Nursing; Pittsburgh, PA: 2005. [Google Scholar]
- Parr MB, Sweeney NM. Use of human patient simulation in an undergraduate critical care course. Critical Care Nurse Quarterly. 2006;29(3):188–198. doi: 10.1097/00002727-200607000-00003. [DOI] [PubMed] [Google Scholar]
- Performance Management Services, Inc. What is PBDS? 2006 Retrieved from http://www.pmsi-pbds.com on 11 July 2007.
- Proctor P, Compton W, Grossman J, Fanjiang G. Building a Better Delivery System: A New Engineering/Health Care Partnership; Washington, DC: Institute of Medicine and National Academy of Engineering, The Nationals Academies Press; 2005. [PubMed] [Google Scholar]
- Redfern S, Norman I, Calman L, Watson R, Murrells T. Assessing competence to practice in nursing: a review of the literature. Research Papers in Education. 2002;17(1):51–77. [Google Scholar]
- Rubenfeld M, Scheffer B. Critical Thinking in Nursing: An Interactive Approach. 2. Lippincott; Philadelphia: 1999. [Google Scholar]
- Scheffer BK, Rubenfeld MG. A consensus statement on critical thinking in nursing. Journal of Nursing Education. 2000;39(8):352–359. doi: 10.3928/0148-4834-20001101-06. [DOI] [PubMed] [Google Scholar]
- Schoen MS, Osborn R, Huynh PT, Doty M, Zapert K, Peugh MA, Davis K, et al. Taking the pulse of health care systems: experiences of patients with health problems in six countries. Health Affairs Web Exclusive. 2005 3 November;2005:509– 525. doi: 10.1377/hlthaff.w5.509. [DOI] [PubMed] [Google Scholar]
- Schwid HA, Rooke GA, Carline J, Steadman RH, Murray WB, Olympio M, et al. Evaluation of anesthesia residents using mannequin-based simulation: a multiinstitutional study. Anesthesiology. 2002;97(6):1434–1444. doi: 10.1097/00000542-200212000-00015. [DOI] [PubMed] [Google Scholar]
- Simpson E, Courtney M. Critical thinking in nursing education: literature review. International Journal of Nursing Practice. 2002;8(2):89–98. doi: 10.1046/j.1440-172x.2002.00340.x. [DOI] [PubMed] [Google Scholar]
- Thompson C, Rebeschi LM. Critical thinking skills of baccalaureate nursing students at program entry and exit. Nursing and Health Care Perspectives. 1999;20(5):248–252. [PubMed] [Google Scholar]
- Trossman S. Bold new world: technology should ease nurses’ jobs, not create a greater workload. American Journal of Nursing. 2005;105(5):75–77. doi: 10.1097/00000446-200505000-00034. [DOI] [PubMed] [Google Scholar]