Abstract
Aims
Therapeutic options for patients with recurrent cardiac ischemia following coronary artery bypass surgery may be limited and some patients may be considered nonrevascularizable. To further the understanding of this patient cohort, we performed a population-based study of post coronary bypass patients who developed recurrent angina.
Methods and Results
Patients who underwent coronary artery and bypass graft angiography at Mayo Clinic from 2001 – 2005 were identified. Medical records were reviewed to determine indication for angiography, and angiographic analysis was performed in all patients. Among 133,000 residents of Olmsted County, Minnesota, 347 post bypass patients with angina underwent coronary angiography from 2001 – 2005. Of those, 177 patients received further revascularization (145 PCI and 32 redo CABG) and the remaining 170 patients were managed medically. Revascularization was not associated with improvement in all cause or cardiac mortality. Multivariate analysis identified renal dysfunction, diabetes, and severe LV dysfunction but not the lack of revascularization as predictors of mortality.
Conclusion
In this population-based study, we identify a yearly incidence range of 17.9 to 33.2 patients with non-revascularizable angina following CABG per 100,000 population. Further revascularization was not associated with improved mortality or morbidity. Attempts to develop therapeutics for this population must consider the incidence and outcomes of this cohort.
Keywords: angina, percutaneous coronary intervention, surgery, angiography, non-operable
INTRODUCTION
Coronary artery disease (CAD) is a leading cause of death in the United States and is responsible for up to 700,000 deaths per year[1]. Ongoing advances in molecular and cellular biology have led to new approaches being developed to limit cardiac ischemia. These new approaches which include gene and cell delivery as well as novel mechanical approaches are generally studied in a population that is considered to be not amenable to other conventional treatment modalities. The majority of these patients have already had coronary artery bypass grafting (CABG) and many suffer from refractory angina. Additional therapies such as percutaneous coronary intervention (PCI) or additional CABG are often not able to be offered to these patients in spite of ongoing angina. The decision to not pursue further therapies is complex and includes multiple patient specific characteristics as well as physician specific factors, many of which are nonquantifiable. Patients with refractory angina who have exhausted most therapeutic options comprise a growing clinical entity and a therapeutic dilemma. For this study, we define non-revascularizable coronary disease following CABG as patients having ongoing angina despite optimal medical therapy following CABG deemed unamenable to further revascularization by conventional surgical or percutaneous means.
Currently, few data are available on the number of non-revascularizable patients. Data from the Third National Health and Nutrition Examination Survey in 1994 estimated 300,000 to 900,000 patients in the United States have refractory angina and suggested that 25,000 to 75,000 new cases are diagnosed annually[2]. These figures, despite being out of date, are still quoted with respect to statistics regarding refractory angina patients from the American College of Cardiology and American Heart Association (ACC/AHA) presently[3]. Mukherjee estimated that 100,000 to 200,000 patients per year may be eligible for new methods of revascularization based on estimates from a tertiary referral practice[4]. Population-based data estimating the true incidence of non-revascularizable coronary artery disease are unavailable. The demographics of prior clinical studies of non-revascularizable or so called “no-option” patients suggest that the majority (up to 92%) of non-revascularizable angina cases have had previous coronary artery bypass grafting[5,6].
The current study was performed to provide an understanding of this non-revascularizable group of patients in terms of demographics, incidence, and outcomes. We endeavored to determine a population-based incidence of non-revascularizable coronary artery disease concentrating on post CABG patients using the resources of the Olmsted County database, Rochester Epidemiology Project, and the Mayo Clinic Cardiac Catheterization Laboratory. Patients who underwent coronary and bypass graft angiography for angina from Olmsted County, Minnesota, from 2001 to 2005 were studied.
METHODS
The study was conducted in Olmsted County, Minnesota. Mayo Clinic and Olmsted Medical Center provided almost all medical care for the local population. These institutions have accumulated comprehensive records that contain high-quality information from all health care encounters including laboratory results, pathology reports, and autopsy results. The Rochester Epidemiology Project maintains extensive indexes based on clinical and histological diagnoses and surgical procedures for all providers of care to county residents, and all records are linked from all sources of care for this population. The study was approved by the Mayo Foundation Institutional Review Board. Patients refusing permission for medical records research were excluded as required by State of Minnesota Statute (N=44).
Clinical and angiographic records were searched using administrative and clinical databases to identify all Olmsted County patients with prior CABG that underwent coronary and bypass graft angiography from January 1, 2001, to December 31, 2005. Complete medical records from consecutive post coronary bypass Olmsted County patients who underwent angiography from January 1, 2001, to December 31, 2005, were reviewed to determine the clinical indication for coronary angiography, clinical management decisions, and patient demographics. Standard care for these patients involved coordinated care between cardiologists and cardiac surgeons. As all patients included in the study were Olmsted County residents, prospective follow-up was performed in all patients until March 1, 2008, using the resources of the Rochester Epidemiology Project and the Mayo Clinic electronic medical records.
Patient characteristics recorded included the diagnoses of diabetes (type 1 and type 2), systemic hypertension, current cigarette smoking, prior PCI, or prior redo coronary bypass grafting. Chronic renal impairment was determined by previous established diagnosis, creatinine clearance (CrCl) < 60 ml/min, or ongoing hemodialysis.
Cineangiograms from consecutive post coronary bypass Olmsted County patients with angina during the period 2001–2005 were reviewed. This angiographic review was performed by two experienced interventional cardiologists to determine whether further revascularization was technically possible, either percutaneously or via coronary artery bypass surgery, and to assess the angiographic reasons for non-revascularization.
Statistical Analysis
Continuous variables are presented as mean ± standard deviation; discrete variables are reported as frequency (percent). Survival rates were estimated using Kaplan-Meier methods and are reported as percentage. Group comparisons are tested using Student’s t-test, Pearson’s chi-squared test, and the log-rank test, respectively. Cox proportional hazards models were used to calculate hazard ratios and their 95% confidence intervals. The incidence of non-revascularizable coronary artery disease in the post bypass population was calculated using the 92 cases (angiographically truly non-revascularizable) and 170 cases (not revascularized further) as the numerator and Olmsted County population as the denominator. The Olmsted County population was calculated based on yearly US Census projections from the 2000 Census. The rates were adjusted directly to the sex and age distributions from the US 2000 white population. Confidence intervals for the point estimates are based on a Poisson model[7]. All data was stored and analyzed using JMP software.
RESULTS
From 2001 to 2005 inclusive, a total of 545 Olmsted County residents underwent bypass graft angiography at the Mayo Clinic Catheterization Laboratory. Of these, 347 individual patients were referred with the clinical indication of angina. The remainder of the angiographic graft studies was performed for other indications such as pre-operative assessment or evaluation of left ventricular dysfunction.
Baseline Clinical Characteristics
Baseline characteristics of the 347 post coronary bypass patients who underwent graft studies for symptomatic angina are listed in Table 1. The majority of these patients (91%) were Canadian Cardiovascular Society (CCS) angina class III/IV. These 347 patients had characteristics of a high risk population: 69% were male, 37.5% had diabetes (type I and II), 36% had chronic renal impairment, 40% had had previous PCI, and 6% had undergone a second coronary artery bypass procedure. The mean left ventricular ejection fraction of the population was 50 ± 12%.
TABLE 1.
Baseline Characteristics of Olmsted County Post Coronary Bypass Patient Population with angina undergoing coronary and graft angiography at Mayo Clinic 2001–2005
| n=347 | |
|---|---|
| Age (yrs) | 72 ± 10 |
| Men | 237/347 (69%) |
| Smokers (current) | 23/347 (7%) |
| Type 1 diabetes | 26/347 (7.5%) |
| Type 2 diabetes | 96/347 (30%) |
| Systemic hypertension | 303/347 (88%) |
| Statin Tx | 346/347 (99.7%) |
| Chronic renal failure | 123/347 (36%) |
| Ejection Fraction | 50% ± 12 |
| Prior PCI* | 138/347 (40%) |
| Prior CABG† | 347/347 (100%) |
| Prior Redo CABG | 22/347 (6%) |
Percutaneous coronary intervention
Coronary artery bypass grafting
Of the initial 347 patients, a clinical decision was made following angiography to revascularize 177 patients while the remaining 170 patients were treated medically. Further revascularization was defined as any revascularization procedure, percutaneous or surgical, performed after the index coronary and bypass graft(s) angiography and included 145 with PCI and 32 with CABG. Comparisons of baseline characteristics between those revascularized and those treated medically are listed in Table 2. Both groups had a mean age of 72 years, were predominantly male with no significant differences between groups in the incidence of diabetes mellitus, systemic hypertension, or chronic renal failure. However, the percentage of patients in the group that received further revascularization having had two or more coronary artery bypass graft operations was significantly higher (p=0.03) than the group that did not undergo further revascularization.
TABLE 2.
Baseline Characteristics of Olmsted County Post Coronary Bypass Patient Population with angina undergoing coronary and graft angiography at Mayo Clinic 2001–2005 – Not revascularized further versus Revascularized further.
| Not revascularized further | Revascularized further | ||
|---|---|---|---|
| n=177 | n=170 | ||
| Age (yrs) | 72± 11 | 72± 10 | p=0.63 |
| Men | 110 (65%) | 127 (72%) | p=0.18 |
| Smokers (current) | 12 (7%) | 10 (6%) | p=0.47 |
| Type 1 Diabetes | 12 (7%) | 14 (8%) | p=0.70 |
| Type 2 Diabetes | 51 (30%) | 45 (26%) | |
| Systemic hypertension | 153 (90%) | 151 (87%) | p=0.34 |
| Statin Tx | 170 (100%) | 176 (99%) | p=0.32 |
| Chronic renal failure | 68 (40%) | 56 (32%) | p=0.11 |
| Ejection Fraction | 47%±13 | 48%±13 | p=0.17 |
| Prior PCI* | 68 (40%) | 70 (40%) | p=1.0 |
| Prior Redo CABG† | 6 (3%) | 16 (9%) | p=0.03 |
| LIMA graft patency | 87.2% | 83.3% | p=0.12 |
| Class I/II angina | 18 (11%) | 13 (6%) | p=0.15 |
| Class III/IV angina | 152 (89%) | 164 (94%) | |
Percutaneous coronary intervention
Coronary artery bypass grafting
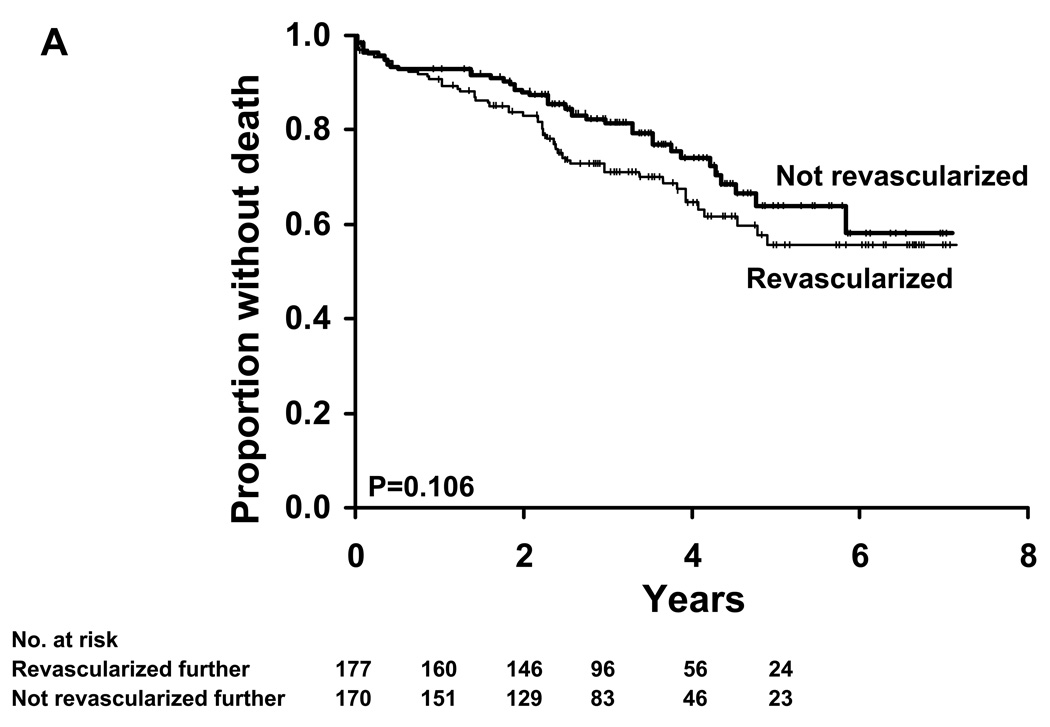
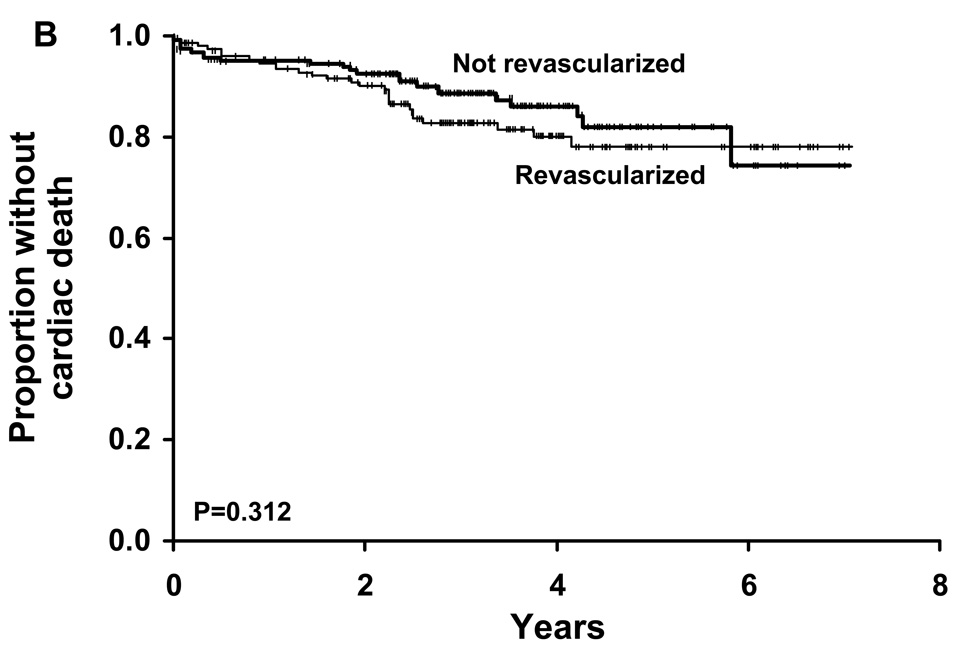
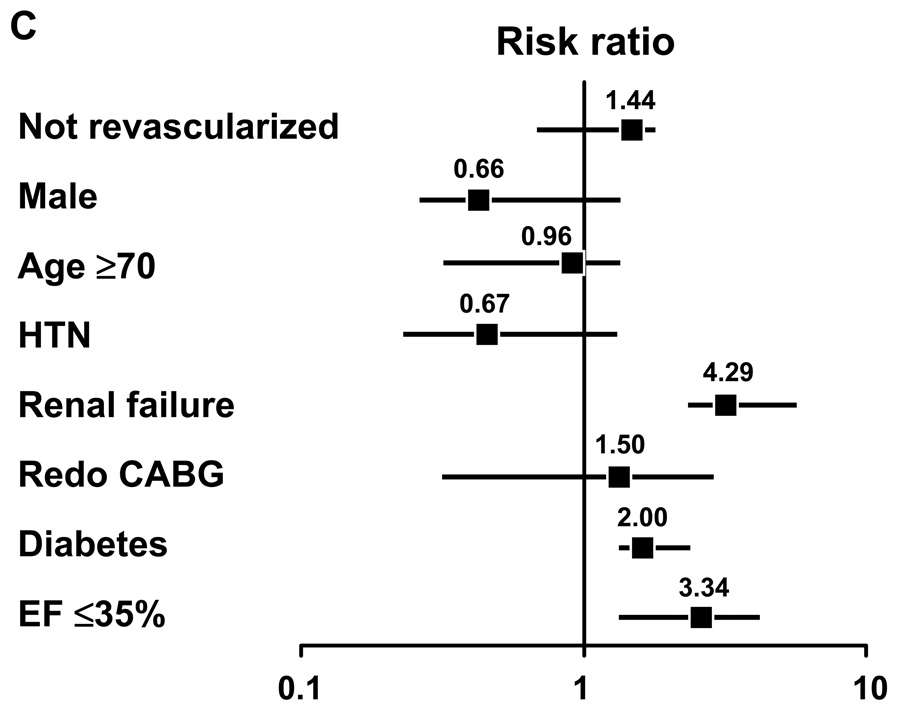
The median duration of follow-up in both groups was 3.2 years (interquartile range 0.60 – 5.45 years). Estimated all cause mortality did not differ between the two groups (23.2% in the revascularized group and 31.1% for the group that did not undergo further revascularization) (p=0.08). Using the log-rank test to compare these two Kaplan-Meier survival curves, no significant difference was found (p=0.1, Figure A). In addition, no differences were demonstrated in terms of cardiac mortality (Figure B) between the groups. Multivariate analysis identified the presence of chronic renal failure, diabetes mellitus, and severe LV dysfunction (LV ejection fraction less than or equal to 35%) were independent predictors of mortality (Figure C). Lack of revascularization was not a predictor of mortality in this analysis. Taken together, these data do not provide support that revascularization improves mortality in this population.
Figure A. Kaplan Meier survival analysis: All cause mortality.
Kaplan Meier survival analysis was performed on the group that did not receive further revascularization and the group that was revascularized further in terms of all cause mortality. Using the log-rank p value to compare these curves, there was no significant difference between the two groups in terms of survival (p=0.106).
Figure B. Kaplan Meier survival analysis: Cardiac mortality.
Kaplan Meier survival analysis was performed on the group that did not receive further revascularization and the group that was revascularized further in terms of cardiac mortality. Using the log-rank p value to compare these curves, there was no significant difference between the two groups in terms of survival (p=0.312).
Figure C. Multivariate analysis for mortality in all patients.
Multivariate analysis for mortality with risk ratio showing presence of chronic renal failure, diabetes mellitus and ejection fraction less than or equal to 35% are independent predictors of mortality.
Subgroup Analysis
Angiographic analysis of the group that did not undergo further revascularization was performed by two experienced interventional cardiologists. It should be noted that all patients in this group had demonstrable ischemia on functional echocardiographic or nuclear studies. After detailed angiographic analysis, 92 patients were classified as being technically non-revascularizable by conventional percutaneous or surgical means. The predominant reasons for non-revascularizability included the presence of chronic total occlusions, degenerated saphenous vein grafts, and diffuse disease extending beyond the graft insertion (Table 3). The remaining 78 patients in the group, despite suffering from angina and having proven functional ischemia, had adequately functioning grafts to all major epicardial territories making further PCI or surgical revascularization unnecessary. It is likely that these patients represented manifestations of microvascular coronary artery disease.
TABLE 3.
Non revascularizable Olmsted County Post Coronary Bypass Patient Population- Reason Patients were not considered suitable for PCI* or CABG† by angiographic analysis
| n=92 | ||
|---|---|---|
| Poor distal targets: | 66 | (72.5%) |
| Chronic total occlusion: | 85 | (93.4%) |
| Multiple restenosis: | 6 | (6.5%) |
| Degenerated saphenous vein graft: | 62 | (68.1%) |
| Disease beyond graft insertion: | 41 | (53.9%) |
Percutaneous coronary intervention
Coronary artery bypass grafting
The all cause mortality rate of this group of patients (n=92) that were technically non-revascularizable from a technical and angiographic point of view was 34.7%. The cardiac mortality rate was 21.7%. When compared with the revascularized group, there was no statistical difference in all cause (p=0.13) or cardiac mortality (p=0.34).
Estimate of incidence of post-CABG non-revascularizable coronary artery disease
The community–based nature of this study enabled us to estimate an incidence of non-revascularizable coronary artery disease. The group of 92 patients with no revascularization potential (based on detailed angiographic analysis) and the group of 170 patients who did not receive further revascularization formed the basis of our estimates. Adjusting for age and sex for differences between the Olmsted County population and the US white 2000 population yields an annual incidence of post-surgical non-revascularizable coronary artery disease of 17.9 per 100,000 (95% CI 14.2–21.6) equating to 50,000 (95% CI 40,000–61,000) non-revascularizable angina cases per year with respect to the angiographically non-revascularizable patient cohort. If all 170 patients who did not undergo further revascularization despite angina are included, this yields an annual incidence of post-surgical non-revascularizable coronary artery disease of 33.2 per 100,000 (95% CI 28.2 – 38.3) or approximately 93,000 (95% CI 79,000 – 110,000) non-revascularizable angina cases per year following bypass per year when adjusted to the US population as of April 1, 2000. Hence, our estimate of post-CABG non-revascularizable coronary artery disease is between 50,000 to 93,000 patients per year.
DISCUSSION
In order to effectively translate novel therapies to patients with advanced ischemic heart disease following CABG, the burden and outcomes of such patients must be defined. In this population-based study of patients with symptomatic angina referred for coronary angiography post CABG, further revascularization did not reduce all cause or cardiac mortality. Multivariate analysis identified diabetes, renal dysfunction, and severe reduction of LV ejection fraction as predictors of mortality. These results must be considered in the translation of novel therapeutics which might target ischemia.
Of those patients in this cohort treated medically, a non-revascularizable group of 92 patients post bypass based on angiographic analysis from Olmsted County over a 5-year period from 2001–2005 was defined. A further 78 patients who did not undergo further revascularization as all conduits to all major epicardial territories were patients still suffer from angina despite medical management. Adjusting for age and sex for differences between the Olmsted County population and the US white 2000 population yields a yearly incidence rate of non-revascularizable coronary artery disease following bypass of 17.9 per 100,000 (95% CI 14.2–21.6) to 33.2 per 100,000 (95% CI 28.2 – 38.3). This incidence provides a population-based estimate of approximately 50,000 (95% CI 40,000–61,000) to 93,000 (95% CI 79,000 – 110,000) patients with non-revascularizable angina following bypass per year in the United States as a whole.
Comparison to Previous Work
The population-based estimate of 50,000 to 93,000 patients per year with non-revascularizable angina following bypass is the first estimate of its kind. Mukherjee et al reviewed 500 patients with known or suspected coronary artery disease undergoing coronary angiography between January and May 1998. They concluded that 59 symptomatic patients (12%) were not suitable for PCI or CABG. Extrapolation to the US population yielded a range of 100,000 to 200,000 patients/year. The estimate quoted was calculated as a percentage of all patients that underwent coronary angiography in 1996 regardless of clinical indication. The vast majority of patients reviewed (83%) were tertiary referrals and, therefore, did not reflect a community based estimate[4]. It must be stated that the above study had broader inclusion criteria than our study which included only post coronary artery bypass patients. Data from the Third National Health and Nutrition Examination Survey estimates 300,000 to 900,000 patients in the United States have refractory angina, and 25,000 to 75,000 new cases are diagnosed annually[2].
Comparisons with prior studies must consider that the range of 50,000 to 93,000 non-revascularizable post coronary bypass patients per year in this study certainly underestimates the entire non-revascularizable population as some such patients will not have had previous bypass. Furthermore, not all post coronary bypass patients with angina will undergo coronary and graft angiography in the “real world”. However, the vast majority of (85–95%) patients enrolled in prospective studies such as the Vascular Endothelial Growth Factor in Ischemia for Vascular Angiogenesis (VIVA) Trial[5] and the FGF Initiating Revascularization Trial (FIRST)[6], which enrolled so-called “no option” angina patients, had previous coronary artery bypass grafting performed. These estimates must be considered when defining the ultimate need for new therapies as well as the effort and time needed to recruit such patients for clinical trials, particularly given the high number of co-morbidities.
Outcomes
The lack of difference in all-cause and cardiac mortality between the group of patients receiving further revascularization and those that did not over the follow-up period is notable. Patients with a history of remote CABG pose numerous challenges when they develop angina as progression of native coronary artery disease leaves fewer options for redo CABG and graft attrition diminishes the chances for successful PCI. Brener et al demonstrated that revascularization in post coronary bypass patients is associated with poor long-term outcome with a mortality rate of 25% at 5 years[8]. The method of repeat revascularization has little to do with long-term mortality[9]. It must be remembered that patients included in our study are frequently high risk with significant co-morbidities, very distinct from the risk factor profile of patients enrolled in randomized controlled trials. Of note, approximately 68% of our non-revascularizable population had a severely degenerated graft as one of the determinants of their non-suitability for further revascularization. The periprocedural and 6-month outcomes of percutaneous interventions to vein grafts using distal embolic protection devices are indeed improving[10]. High risk features of vein grafts for PCI, which included diffusely diseased grafts over 8 years and co-existent severe distal disease beyond the graft insertion precluded many of our patients from invasive treatment. Currently there are no published data on symptomatic post coronary bypass patients treated with medical treatment versus surgical or percutaneous revascularization. However, when patients present with symptomatic multivessel coronary artery disease after CABG, the choice of revascularization method or lack of revascularization is dictated mostly by anatomical considerations[8].
The subgroup analysis is also interesting in that 92 patients were classified as non-revascularizable based on anatomical and technical criteria after angiographic analysis. The remaining 78 patients despite having chronic angina and presence of ischemia were deemed not to require further PCI or surgical intervention after angiographic assessment. Theoretically, these patients may be experiencing angina from impaired coronary flow reserve secondary to microvascular ischemia. Consideration of these patients furthers the spectrum of non-revascularizability in terms of macrovascular and microvascular non-revascularizable coronary artery disease.
Limitations
Our study has several limitations. The racial and ethnic composition of Olmsted County limits generalizability to other groups. The Olmsted County population is predominantly white Caucasian with 10.8% of the population greater than 65 years. However, no regional population can be representative of the United States as a whole as illustrated by the known regional variations in heart disease rates. To this end, however, it should be underscored that Olmsted County cardiovascular disease trends parallel national trends, thus supporting the generalizability of our data[11]. The adjusted incidence of coronary artery bypass surgery at the Mayo Clinic on Olmsted County patients from 2001 to 2005 was 145.8 per 100,000 population. This is an important fact to take into account in relation to the USA as a whole. It must be stated that the selection of post coronary bypass patients was non-randomized but included all patients from Olmsted County with angina undergoing coronary and graft angiography. This rate of post bypass coronary angiography will have an impact on our incidence of non-revascularizable coronary artery disease, but we feel it reflects the current modern management of angina and coronary ischemia in the post-CABG patient. It must be also stated that this study reflects non-revascularizable coronary artery disease in relation to the post coronary artery bypass grafting population, and therefore, projection of these results to patients without previous CABG is not possible. The ability to detect differences in outcomes between the groups is attenuated by the small numbers in the study.
Conclusions
We estimate a population-based adjusted incidence of patients with post-bypass non-revascularizable angina of 17.9 to 33.2 per 100,000 adjusting for age and sex differences between the Olmsted County population and the US white 2000 population. This equates to approximately 50,000 (95% CI 40,000–61,000) to 93,000 (95% CI 79,000 – 110,000) cases per year in the United States as a whole. We found no significant difference in all cause mortality or cardiac mortality between the group that underwent further revascularization and those that did not. Such patients may be candidates for novel or investigational therapies. Further epidemiologic research characterizing the incidence and prevalence of advanced, symptomatic non-revascularizable coronary artery disease is needed.
Acknowledgements
We are indebted to Megan Crouch and Traci Paulson for their technical support with this manuscript.
Source of Funding: National Institutes of Health (HL 75566)
Footnotes
Conflict of Interest:
None declared.
References
- 1.US Department of Health and Human Services. the Centers for Disease Control and Prevention, National Center for Health Statistics. National Vital Statistics Report. 2002;50:8.
- 2.National Center for Health Statistics. Plan and operation of the Third National Health and Nutrition Examination Survey. Series 1: programs and collection procedures. Vital Health Statistics 1. 1988–1994;32:1–407. [PubMed]
- 3.Rosamond W, Flegal K, Friday G, Furie K, Go A, Greenlund K, et al. Heart disease and stroke statistics--2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115:e69–e171. doi: 10.1161/CIRCULATIONAHA.106.179918. [DOI] [PubMed] [Google Scholar]
- 4.Mukherjee D, Bhatt DL, Roe MT, Patel V, Ellis SG. Direct myocardial revascularization and angiogenesis--how many patients might be eligible? Am J Cardiol. 1999;84:598–600. doi: 10.1016/s0002-9149(99)00387-2. A598. [DOI] [PubMed] [Google Scholar]
- 5.Henry TD, Annex BH, McKendall GR, Azrin MA, Lopez JJ, Giordano FJ, et al. The VIVA trial: Vascular endothelial growth factor in Ischemia for Vascular Angiogenesis. Circulation. 2003;107:1359–1365. doi: 10.1161/01.cir.0000061911.47710.8a. [DOI] [PubMed] [Google Scholar]
- 6.Simons M, Annex BH, Laham RJ, Kleiman N, Henry T, Dauerman H, et al. Pharmacological treatment of coronary artery disease with recombinant fibroblast growth factor-2: double-blind, randomized, controlled clinical trial. Circulation. 2002;105:788–793. doi: 10.1161/hc0802.104407. [DOI] [PubMed] [Google Scholar]
- 7.Bergstrahl EJ, Offord KP, Chu C-P, Beard CM, O'Fallon WM, Melton L., Jr . Rochester, Minn: Mayo Clinic; 1992. Calculating incidence, prevalence and mortality rates for Olmsted County, Minnesota residents: An update. [Google Scholar]
- 8.Brener SJ, Lytle BW, Casserly IP, Ellis SG, Topol EJ, Lauer MS. Predictors of revascularization method and long-term outcome of percutaneous coronary intervention or repeat coronary bypass surgery in patients with multivessel coronary disease and previous coronary bypass surgery. Eur Heart J. 2006;27:413–418. doi: 10.1093/eurheartj/ehi646. [DOI] [PubMed] [Google Scholar]
- 9.Stephan WJ, O'Keefe JH, Jr, Piehler JM, McCallister BD, Dahiya RS, Shimshak TM, et al. Coronary angioplasty versus repeat coronary artery bypass grafting for patients with previous bypass surgery. J Am Coll Cardiol. 1996;28:1140–1146. doi: 10.1016/S0735-1097(96)00286-0. [DOI] [PubMed] [Google Scholar]
- 10.Halkin A, Masud AZ, Rogers C, Hermiller J, Feldman R, Hall P, et al. Six-month outcomes after percutaneous intervention for lesions in aortocoronary saphenous vein grafts using distal protection devices: results from the FIRE trial. Am Heart J. 2006;151 doi: 10.1016/j.ahj.2005.09.018. 915 e911-917. [DOI] [PubMed] [Google Scholar]
- 11.Gerber Y, Jacobsen SJ, Frye RL, Weston SA, Killian JM, Roger VL. Secular trends in deaths from cardiovascular diseases: a 25-year community study. Circulation. 2006;113:2285–2292. doi: 10.1161/CIRCULATIONAHA.105.590463. [DOI] [PubMed] [Google Scholar]