Abstract
Introduction
The long-term excess mortality associated with hip fracture remains controversial.
Methods
To assess the association between hip fracture and mortality, we used prospectively collected data on pre-fracture health and function from a representative sample of U.S. elders in the Medicare Current Beneficiary Survey (MCBS) to perform survival analyses with time-varying covariates.
Results
Among 25,178 MCBS participants followed for a median duration of 3.8 years, 730 sustained a hip fracture during follow-up. Both early (within 6 months) and subsequent mortality showed significant elevations in models adjusted only for age, sex and race. With additional adjustment for pre-fracture health status, functional impairments, comorbid conditions and socioeconomic status, however, increased mortality was limited to the first six months after fracture (hazard ratio [HR]: 6.28, 95% CI: 4.82, 8.19). No increased mortality was evident during subsequent follow-up (HR: 1.04, 95% CI: 0.88, 1.23). Hip-fracture-attributable population mortality ranged from 0.5% at age 65 among men to 6% at age 85 among women.
Conclusions
Hip fracture was associated with substantially increased mortality, but much of the short-term risk and all of the long-term risk was explained by the greater frailty of those experiencing hip fracture.
Keywords: attributable risk, hip fracture, mortality, osteoporosis
Hip fracture is one of the most highly visible and devastating consequences of osteoporosis. It is well-established that hip fractures are a major cause of morbidity and mortality in the elderly (1). More than 250,000 hip fractures occur annually in the U.S., and the direct medical cost associated with these fractures is estimated to exceed $20.6 billion each year (2). Unless preventive interventions are undertaken, the number of hip fractures and their associated costs are projected to increase dramatically due to the aging of the “baby-boomer” population (3). As costly new osteoporosis treatments become available, their economic value has been subjected to increasing scrutiny. To address this concern, a growing literature has weighed the costs of interventions relative to their effectiveness, as measured by impact on mortality and morbidity in formal cost-effectiveness analyses (4–6).
An important parameter in such models is the excess mortality ( i.e., deaths due to hip fracture that might be prevented). While there is considerable disagreement on this point, the high mortality rate following hip fracture is unquestioned (1). It appears that the hazard of death is greater immediately after the hip fracture and declines with time thereafter (7). Although studies that have examined short- vs. long-term mortality almost always have noted higher mortality within the first 6–12 months following the fracture (8–13), the extent to which long-term mortality is associated with hip fracture remains controversial. Some studies show persistent increased mortality (8, 12, 14, 15), while others suggest either no long-term elevated mortality (9) or only modestly elevated long-term mortality relative to that expected in older individuals (10, 11, 13, 16, 17).
The difficulty in attributing these excess deaths to the hip fracture per se relates to the fact that hip fractures tend to occur among those who face an already increased risk of death from other causes (18, 19). Thus, patients with hip fracture are often frail and may have very limited health and functional status prior to the fracture. Such characteristics are difficult to control for and may not have been adequately measured in prior studies. Indeed, previous studies have been limited by measures of coexisting illness or functional status, with many studies, including the Baltimore Hip Study and EPIDOS, relying on self-reported pre-fracture functional status (8, 12).
To help resolve this important issue, the current study examined the association between incident hip fracture and mortality, based on a nationally representative sample of U.S. elders and prospectively collected data on pre-fracture health and functioning. Our primary objective was to evaluate whether there is long-term excess mortality associated with hip fracture in the U.S. population ages 65 years and older. In addition, we examined whether hip fracture mortality differed by sex, race, age, institutionalization and health status.
METHODS
Study Population
We analyzed data collected from participants in the Medicare Current Beneficiary Survey (MCBS) who had one or more interviews between 1996 and 2000. The first interview in this time period was used to define cohort entry. MCBS is a longitudinal panel survey designed to provide a representative sample of all Medicare beneficiaries, including those who are institutionalized (20). Over the period 1997 to 1999, mean initial survey participation rates were 83% (21). By tracking individuals for up to four years (with three interviews per year) to collect data on health, function and socioeconomic status, MCBS provides detailed data on the population of elders in the U.S. ages 65 and older (22). For our study, we obtained updated MCBS cost and use files until subsequent hip fracture, death or exit from the MCBS panel.
Ascertainment of hip fracture
Hip fractures that occurred in this cohort after MCBS panel entry were identified using Medicare claims data from 1997 through 2001. Persons hospitalized with a primary diagnosis of hip fracture (ICD-9 code 820.xx) and no evidence of bone metastases or prior fracture complications (e.g., removal of hardware) were flagged as having a hip fracture.
Ascertainment of death
The cohort was tracked through 2001 for mortality outcomes. Death occurring within six months of hip fracture was defined as “early mortality,” while death occurring six months or more following a hip fracture was defined as “late mortality.” No information was available on cause of death.
Covariate Definitions
Covariate information came from both the MCBS interview data and Medicare Claims administrative data. Functional status, comorbid conditions, income, place of residence, self-reported health, marital and smoking status, and activities/instrumental activities of daily living were updated at each MCBS interview, until a person no longer participated in the survey or until a hip fracture occurred.
Functional Status
Activities of Daily Living (ADLs) were assessed for all participants. It was not possible to assess all Instrumental ADLs (IADLs) among facility-dwellers. Persons were considered to have a limitation in an activity if one was reported or if they indicated that they could not perform an activity due to health reasons. The severity of limitations in ADLs/IADLs was assessed based on the proportion of activities that were limited. Persons limited in only one activity were defined as having mild limitations; those with limitations in a third of the activities (up to two limitations) were defined as having moderate limitations; those with impairments in half of the activities (more than 2 but less than 4 limitations) were defined as having severe limitations; and those with limitations in two-thirds of the activities (4 to 6 limitations) were defined as having very severe limitations.
Clinical Conditions/Co-morbidities
Co-morbid conditions were assessed both through self-report of prior diseases in the MCBS survey and through administrative claims data using the Iezzoni Index (23). Iezzoni comorbidities were defined using diagnoses from both short-term hospital (MEDPAR) claims and evaluation and management (Part B) claims. To be considered valid, we required two Part B claims at least 7 days apart or any MEDPAR diagnosis. Each comorbid condition was assigned the date of first diagnosis of the specific condition. Once persons were assigned a comorbid condition, they were considered to have it from that point onward.
Statistical Analysis
Data on patient characteristics were re-weighted to reflect the U.S. Medicare population based on MCBS sampling weights. MCBS provides both cross-sectional and longitudinal weights (24). However, because we created a longitudinal cohort using multiple MCBS years, the weights applied were an average of MCBS cross-sectional weights.
Associations between baseline characteristics and incident hip fracture were assessed using chi-squared tests. To assess associations after adjustment for age, sex and race, logistic regression models were used. Comparisons of time to death from cohort entry between those who had incident hip fracture and those who did not were made using logrank tests.
Cox proportional hazards regression models with time-varying covariates were used to examine associations between hip fracture and mortality among MCBS survey participants followed through 2001. This model defines the hazard, λi (t, xi(t)), for individual i at time t with covariates xi(t) as follows: λi (t, xi(t))= λ0(t) exp{ xi (t) β}. Using this model, one time-varying covariate of interest was whether or not a hip fracture occurred. Following hip fracture, associations with early and late mortality were assessed using a post-fracture time period indicator of whether or not six months had passed from the incident fracture. Hazards were estimated under three covariate adjustment models. The first adjusted only for age, sex and race. The second added detailed patient-level data concerning health, functional status and socioeconomic status obtained from both MCBS and Medicare claims data. The third model included all but the socioeconomic variables contained in the second model (see Appendix for a complete list of covariates).
To assess the importance of pre-fracture health as a determinant of excess mortality, we estimated hazard ratios (HR) associated with hip fracture within strata defined by health status. In these analyses, health limitations (any vs. none) were defined on the basis of any reported limitations in ADL/IADLs and/or presence of any of the following comorbid conditions: Parkinson’s disease, stroke, rheumatoid arthritis, diabetes, dementia, cancer (solid tumors), lymphoma or leukemia, chronic pulmonary disease, coronary artery disease, congestive heart failure, peripheral vascular disease, severe chronic liver disease and chronic renal failure in the first interview year. Likewise, we examined the role of hip fracture as a contributor to excess mortality in analyses stratified by sex, race (black vs. non-black), age (<80 vs. 80+) and facility-dwelling status (facility-dweller vs. not).
To demonstrate the difference that careful adjustment for comorbid conditions, functional status and socioeconomic factors can have on estimates hip fracture-attributable population mortality, we computed attributable relative risk as pH*(HR-1)]/(pH*(HR-1)+1) (25), where pH is the probability of hip fracture at any given age and HR is the hazard ratio associated with incident hip fracture (a weighted average of hazards estimated for early and late mortality applied only in the year after the fracture occurred). The calculations were made first with hazards from the minimally adjusted model, which did not include health status or socioeconomic factors (Appendix, Model 1), and then with hazards from the fully adjusted model (Appendix, Model 2). The probability of hip fracture at any given age was based on data from Olmsted County, MN (26) and age-specific mortality estimates were taken from 2001 U.S. lifetables (27).
RESULTS
Study Population
A total of 25,178 MCBS survey participants were included in the analysis, with a median follow-up duration of 3.8years (interquartile range (IQR):2.2, 5.6 years). By the end of 2001, 730 had sustained a hip fracture following their first interview. The median time between the last pre-fracture interview and the incident fracture was 0.9 years (IQR: 0.3, 2.1) and the median post-fracture follow-up duration was 1.5 years (IQR: 2.4, 4.8 years).
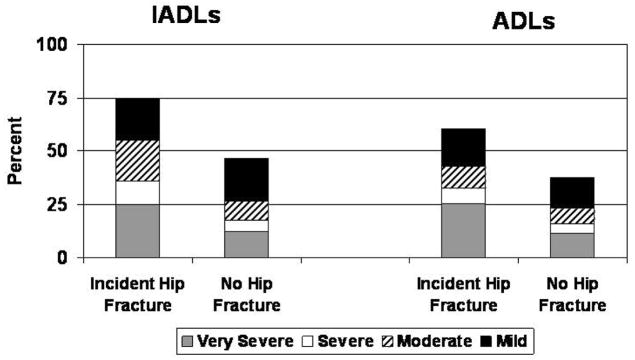
Compared to those without hip fracture, persons with incident hip fracture were older at cohort entry (average age of 82 vs. 76 years, p <0.001), more often female (74% vs. 58%, p <0.001), and most commonly white 95 % vs. 88 %, p <0.001). After adjustment for age, race, and sex, they reported living alone more frequently and were less likely to be HMO members (Table 1). At cohort entry, those who later sustained a hip fracture already reported more limitations and more severe limitations in ADLs and IADLs than those who did not fracture (Figure 1). After adjustment for age, sex and race, smoking status and self-reported health status at the initial interview did not differ between those who later sustained a hip fracture and those who did not; however, there were some differences in comorbid conditions (both self-reported and claims identified), as shown in Table 2.
Table 1.
Demographic characteristics at first interview by incident hip fracture status and observed mortality by characteristic and hip fracture status
| Characteristic | Proportion with Characteristic by Hip Fracture Status: | Mortality by Characteristic and Hip Fracture Status: | ||
|---|---|---|---|---|
| Incident Hip Fracture (N=730) | No Hip Fracture (N=24,448) | Incident Hip Fracture N (%) | No Hip Fracture N (%) | |
| Age, %* | ||||
| 65–74 | 23% | 53% | 22/112 (17%)§ | 1314/10601 (12%) |
| 75–84 | 42% | 35% | 100/298 (31%)§ | 2564/9390 (25%) |
| 85+ | 34% | 11% | 150/320 (47%)§ | 2484/4457 (54%) |
| Gender, %* | ||||
| Female | 74% | 58% | 183/538 (30%)§ | 3539/14276 (20%) |
| Male | 26% | 43% | 89/192 (42%)§ | 2823/10172 (24%) |
| Race, %* | ||||
| White | 95% | 88% | 259/688 (34%)§ | 5529/21219 (22%) |
| Black | 4% | 8% | 11/31 (34%) | 641/2287 (24%) |
| Asian | <1% | 2% | -- | 62/372 (12%) |
| Other | 1% | 2% | -- | 130/570 (19%) |
| Place of Residence, % | ||||
| Facility | 12% | 5% | 64/109 (61%) | 1408/1811 (77%) |
| Community | 88% | 95% | 208/621 (30%)§ | 4954/22637 (19%) |
| Lives Alone, %+ | 45% | 31% | 98/301 (31%)§ | 1803/7504 (21%) |
| Education, % | ||||
| Less than high school | 39% | 34% | 125/302 (39%)§ | 2764/9029 (27%) |
| High school education | 26% | 29% | 14/62 (21%) | 441/2989 (12%) |
| Some college | 12% | 14% | 30/113 (24%)§ | 749/4030 (16%) |
| 4+ years college | 17% | 17% | 23/78 (25%)§ | 635/3194 (16% |
| Education missing | 6 % | 6% | 34/57 (58%)§ | 677/1389 (58%) |
| Annual Income, % | ||||
| < $15,000 | 54% | 40% | 171/422 (38%)§ | 3650/10838 (29%) |
| $15–45,000 | 36% | 45% | 16/45 (32%)§ | 525/2769 (16%) |
| > $45,000 | 9 % | 12% | 15/55 (21%) | 393/2560 (13%) |
| Missing | 1% | 4% | -- | 29/462 (5%) |
| HMO participation, %+ | ||||
| Private HMO | 4% | 8% | -- | 286/1694 ( 14%) |
| Medicare HMO | 3% | 16% | -- | 779/3717 (17%) |
| None | 93% | 76% | 255/678 (34%)§ | 5297/19037 (23%) |
| Medigap Insurance coverage, %+ | ||||
| None | 32% | 36% | 83/229 (33% )§ | 2872/9110 (26%) |
| Privately or privately+ employee-purchased | 42% | 34% | 90/276 (30%)§ | 1740/8112 (19%) |
| Employer-sponsored | 26% | 30% | 62/163 (31%)§ | 1223/6503 (16%) |
| Medicare entitlement due to disability | 1% | 2% | -- | 95/442 (22%) |
| Medicaid | 18% | 11% | 67/146 (43%) | 1383/3271 (36%) |
p-value<0.05;
p < 0.05 for association between characteristic and hip fracture incidence after adjusting for age, sex and race;
p < 0.05 for the logrank test comparing mortality between those with and without incident hip fracture within each row;
suppressed because n<11.
Figure 1.
Proportion of subjects at cohort entry with any limitations in Activities of Daily Living (ADLs) and Instrumental Activities of Daily Living (IADLs) and severity of impairment.
Table 2.
Health characteristics by incident hip fracture and mortality status.
| Characteristic | Proportion with characteristic by fracture status: | Mortality by characteristic and fracture status: | ||
|---|---|---|---|---|
| Incident Hip Fracture (N=730) | No Hip Fracture (N=24,448) | Incident Hip Fracture N (%) | No Hip Fracture N (%) | |
| Smoking status | ||||
| Previous smoker | 35% | 46% | 99/248 (35%)§ | 2641/10888 (21%) |
| Current smoker | 11% | 12% | 22/65 (29%)§ | 696/2555 (24%) |
| Health status | ||||
| Excellent health | 12% | 16% | 26/87 (25%)§ | 448/3629 (10%) |
| Good health | 57% | 59% | 147/413 (32%)§ | 2821/14049 (17%) |
| Fair, poor or missing health | 32% | 25% | 99/230 (39%)§ | 3093/6770 (41%) |
| Body Mass Index (BMI)+ | ||||
| Low (<21kg/m2 men, <20 women) | 8% | 3% | 28/65 (42%) | 537/889 (55%) |
| High (>32 kg/m2men, >30 women) | 8% | 18% | 19/52 (32%)§ | 727/3956 (16%) |
| Self-reported conditions | ||||
| Previous hip fracture+ | 11% | 4% | 28/81 (31%) | 638/1255 (45%) |
| Parkinson’s disease | 3% | 2% | 12/25 (45%) | 264/467 (51%) |
| Stroke | 17% | 11% | 63/132 (46%)§ | 1404/3065 (41%) |
| Osteoarthritis | 12% | 10% | 123/310 (37%)§ | 3083/11169 (22%) |
| Osteoporosis | 20% | 12% | 49/148 (31%)§ | 878/3073 (24%) |
| Vision problems | 11% | 8% | 38/90 (41%)§ | 932/2236 (37%) |
| Diabetes mellitus | 14% | 17% | 41/101 (34%) | 1485/4301 (30%) |
| Dementia | 11% | 5% | 55/95 (59%) | 1129/1625 (65%) |
| Iezzoni comorbidities determined from claims data | ||||
| Cancer solid tumors | 2% | 2 % | 22/49 (44%) | 592/1323 (42%) |
| Lymphomas or leukemia | <1% | <1% | -- | 81/122 (65%) |
| Chronic pulmonary+ | 6% | 3% | 52/113 (43%) | 856/1789 (44%) |
| Coronary artery disease | 3% | 2 % | 27/64 (41%) | 518/1793 (33%) |
| Congestive heart failure+ | 4% | 2 % | 56/103 (51%) | 1133/1793 (60%) |
| Peripheral vascular disease+ | 3% | 1 % | 18/42 (37%)§ | 418/830 (47%) |
| Severe chronic liver | <1% | <1% | -- | 28/42 (40%) |
| Diabetes w/end organ damage | 1% | 1% | -- | 199/469 (40%) |
| Functional impairment+ | 1% | <1% | 14/25 (56%) | 163/256 (62%) |
| Chronic renal failure | 1% | <1% | 14/20 (59%) | 227/305 (71%) |
| Nutritional deficiency+ | 1% | <1% | 21/31 (64%) | 259/330 (78%) |
| Schizophrenia | <1% | <1% | -- | 33/63 (49%) |
p < 0.05 for association between characteristic and hip fracture incidence after adjusting for age, sex and race;
p < 0.05 for the logrank test comparing mortality between those with and without incident hip fracture within each row;
suppressed because n<11.
Mortality following Hip Fracture
Crude Mortality
Crude mortality by the end of 2001 differed according to whether or not a hip fracture had occurred. Altogether, there were 5,690 deaths in the cohort. Among those with hip fracture, 40% had died and 50% of those deaths occurred within six months of the hip fracture. Among those without hip fracture, 22% had died. Comparisons of time to death from the initial survey between those with and without incident hip fracture showed significant differences for most demographic and health characteristics as shown in Tables 1 and 2.
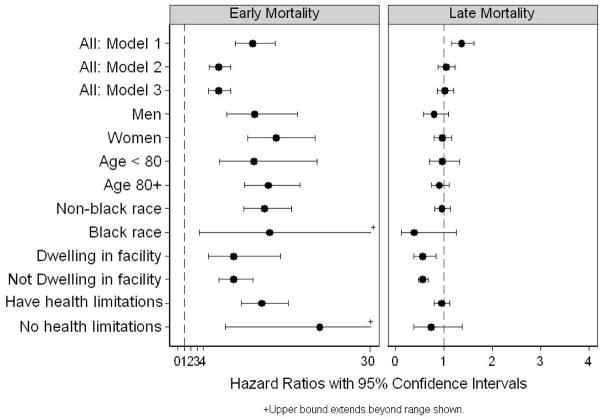
Early (< 6 months) and Late Mortality
The likelihood of both early (HR:11.6, 95%CI: 8.9, 15.1) and late mortality (HR: 1.37, 95%CI: 1.16, 1.62) following hip fracture was significant when adjustment was limited to age, sex and race (Figure 2, Model 1). When the analysis included adjustment for pre-fracture functional status, socioeconomic status, facility residence, body mass index, other self-reported comorbid conditions and overall health status (Figure 2, Model 2), only mortality within six months was significantly increased (HR: 6.28, 95%CI: 4.82, 8.20). Late mortality risk was not elevated (HR: 1.04, 95%CI: 0.88, 1.23). Hazard ratios for early mortality were unchanged with the addition of socioeconomic status variables (Figure 2, Model 3), and hazard ratios for late mortality were nearly identical (HR: 1.02, 95%CI: 0.87, 1.21). In analyses that examined mortality following hip fracture within subgroups defined by sex, race (black vs. non-black), age (<80 vs. 80+), facility-dwelling status (institutional vs. community dweller), and health status (limitations vs. no limitations), we found no evidence that either early or late mortality following hip fracture was affected by these factors (Figure 2).
Figure 2.
Hazard ratios and 95% confidence intervals for early (within 6 months) and late (beyond 6 months) mortality following hip fracture. Models 1, 2, and 3 include all subjects. Model 1 adjusts for age, sex, and race; Model 2 adjusts for age, sex, race, functional status, comorbid conditions and socioeconomic variables; Model 3 adjusts for age, sex, race, functional status, and comorbid conditions. Results for specified strata show hip fracture hazard ratios under Model 2.
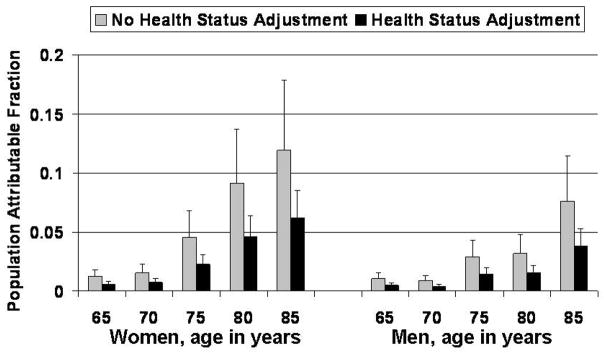
Fraction of Population Mortality Attributable to Hip Fracture
The proportion of mortality attributable to hip fracture was higher for women than men, increased with age and was markedly lower when hazard ratios were adjusted for health status (Figure 3).
Figure 3.
Proportion of mortality in the population that is attributable to hip fracture by age and sex when adjustment is limited to age, sex and race (no health status adjustment) and when health status, and comorbid conditions are also included (health status adjustment). Error bars show upper 95% confidence interval.
DISCUSSION
Mortality following hip fracture has been the focus of many investigations carried out over the past 25 years (1). Although it is well-recognized that mortality is elevated following hip fracture, controversy remains regarding the extent to which mortality may be reduced through hip fracture prevention because those at highest risk of hip fracture are frail and elderly and already at increased mortality risk. Our analysis of an MCBS survey cohort, a representative sample of the U.S. Medicare population, indicates that hip fracture is associated with excess early mortality, but we found no evidence of excess mortality risk beyond the first six months following fracture. This is important, because estimates of the impact of hip fracture prevention on population health may be exaggerated if excess long-term mortality is assumed when this is not appropriate.
Our finding of high excess mortality close to the time of fracture is consistent with other reports (7–12, 28–31). Regardless of study design, investigations that have examined mortality by time since hip fracture have noted the highest excess risk closest to the time of fracture. The duration of the early elevated excess risk is most commonly reported as six months, but ranges from 3 months to 12 months.
In contrast to several studies that report significant long-term excess mortality (8, 12, 14, 15, 31), we found no evidence of excess mortality beyond six months following fracture. A prominent difference between those reports and ours is the nature of the study population. Our study population is representative of the elderly U.S. population and includes those who are institutionalized. Thus, our study cohort differs in health from the community-dwelling ambulatory elderly cohorts that have been the focus of other reports (12, 18). The extent to which a healthy cohort may influence estimates of long-term excess mortality is exemplified by Magaziner et al. (8) who highlighted the potential for long-term excess mortality in those with few ADL/IADL impairments or with few comorbid conditions. This may help explain divergent findings from our nationally representative cohort of elders, for which no long-term excess was observed, and findings from healthier longitudinal cohorts such as EPIDOS (12), for which continued excess risk was noted.
Differing methodological approaches to characterizing excess mortality in other studies may also have resulted in higher long-term risks than those we report. In particular, studies that rely on comparisons between mortality in hip fracture patients relative to age- and sex-specific expected mortality in the general population (13, 32, 33) may not have adequately accounted for the pre-fracture frailty and illness in those who sustain a hip fracture relative to their peers. As a result, these studies may suggest a much greater adverse health impact associated with fracture than is warranted. Likewise, case-control studies matched on age and a retrospective review of health conditions are unlikely to adequately control for pre-fracture health (15, 31, 34).
Our ability to adjust for detailed pre-fracture functional status using prospectively collected longitudinal data in a nationally representative sample is a key strength of our study. As with any longitudinal study, however, our findings are predicated on the quality of follow-up over the period studied. An in-depth evaluation of the impact of non-response on MCBS survey estimates over the period 1997 to 1999 showed favorable initial participation and follow-up rates (83% participation, with panel attrition of 11%, 5%, and 3% in the initial, second and third survey years). Both initial non-response and attrition were lower among those in poor versus better health. Current MCBS non-response procedures have been found to substantially reduce or eliminate potential non-response bias (21).
Our analysis of mortality following hip fracture did not account for clinical presentation, the timing or type of fracture repair, which have been the focus of other studies (35–38). Still, the difference in mortality attributable to hip fracture when considering only age, sex, and race in comparison to more fully adjusted estimates highlights the importance of pre-fracture health and functional status as an important predictor of death. We note that whether or not socioeconomic factors were included in the analyses had no impact on mortality following hip fracture (Model 2 and Model 3 comparison). Although attributable mortality increases with age, it is reduced by approximately 50% when pre-fracture health, functional status and factors other than age, sex and race alone are considered. For example, to estimate the number of potentially preventable deaths in the elderly U.S. population, we applied our estimates of attributable risk to the total number of deaths observed in the Medicare population (ages 65 and older who were not covered by managed care) in the year 2000. When only adjusting for age, sex and race, 79,370 of 971,570 deaths among women and 27,890 of 764,350 deaths among men were attributable to hip fracture. When adjusting for pre-fracture health status, the number of deaths attributable to hip fracture dropped to 40,690 in women and 13,930 in men. Thus, although short-term mortality may be prevented through hip fracture prevention, the extent to which longevity in the community may be improved by treatment remains uncertain (10, 17, 18).
Our analyses of the impact of hip fracture on short- and long-term excess mortality for specific population subgroups may provide some additional insights. Although we found evidence of higher mortality in men than in women (see Appendix for main effects of sex), a finding consistent with other reports (15, 32, 33, 39–42), mortality between men and women did not appear to differ according to whether or not a hip fracture occurred. This finding contrasts with a report from the 15-year longitudinal Cardiovascular Health Study that found only 6-month excess mortality in men, but 4-year excess mortality in women (43) Although our stratified analysis indicated potentially worse hip fracture mortality for non-blacks compared to blacks and for non-facility dwellers compared to facility-dwellers, these did not appear to differ according to whether or not a hip fracture occurred. Larger studies based on Medicare Claims data (42, 44), have reported significant sex and race interactions, with black females having the poorest outcomes, but we did not have sufficient power to examine sex-race interactions in our population. In addition, we did not have sufficient power to examine such interactions in the context of early and late excess hip fracture mortality risks.
Although our analysis focuses on excess mortality following hip fracture, excess mortality following other fractures is also of concern (33). Separating out the effects of comorbid conditions from fracture complications is challenging. Unfortunately, the difficulty in accurately identifying vertebral fractures in claims data precludes a similar analytic approach to estimating excess vertebral mortality risk using the MCBS survey cohort.
In summary, although it may be possible to prevent a subset of early deaths, preventable excess long-term mortality is likely to be quite modest and therefore difficult to identify in any study using conventional statistical approaches unless an extremely large population is studied (10). Our study indicates that fracture prevention may be of limited benefit in extending overall life expectancy due to the multiple competing mortality risks faced by the frail elderly.
Acknowledgments
This study was supported by NIH grant AG12262, U.S. Public Health Service. The authors thank Ms. Loretta Pearson for editorial assistance and a comprehensive literature review and Ms. Margaret Grove for assistance with figure preparation.
Appendix
APPENDIX.
Hazard ratios (95% confidence intervals) estimated for each model.
| Variable | Model 1§ | Model 2§ | Model 3§ |
|---|---|---|---|
| Incident hip fracture¥ | 12 (8.9, 15) | 6.3 (4.8, 8.2) | 6.3 (4.8, 8.2) |
| Six or more months from hip fracture¥ | 0.1 (0.1, 0.2) | 0.2 (0.1, 0.3) | 0.2 (0.1, 0.2) |
| Age 65–69 female | - | - | - |
| Age 65–69 Male | 2.2 (1.7, 2.8) | 2.1 (1.6, 2.8) | 2.2 (1.7, 2.9) |
| Age 70–74 male | 2.4 (1.9, 3.2) | 2.2 (1.7, 2.8) | 2.2 (1.7, 2.8) |
| Age 70–74 female | 1.6 (1.3, 2.1) | 1.4 (1.1, 1.8) | 1.4 (1.1, 1.8) |
| Age 75–79 male | 3.8 (3.0, 4.8) | 2.9 (2.3, 3.7) | 2.9 (2.3, 3.7) |
| Age 75–79 female | 2.2 (1.8, 2.9) | 1.7 (1.3, 2.2) | 1.6 (1.3, 2.1) |
| Age 80–84 male | 6.3 (4.9, 7.9) | 3.8 (3.0, 4.9) | 3.7 (3.0, 4.9) |
| Age 80–84 female | 4.2 (3.3, 5.3) | 2.5 (2.0, 3.2) | 2.3 (1.8, 2.9) |
| Age 85+ male | 12.0 (9.2, 15.0) | 5.3 (4.1, 6.7) | 5.3 (4.1, 6.7) |
| Age 85+ female | 9.0 (7.2, 11.3) | 3.5 (2.8, 4.5) | 3.5 (2.9, 4.7) |
| Black race | 1.3 (1.1, 1.4) | 0.9 (0.8, 1.0) | 1.0 (0.8, 1.1) |
| No HMO | - | ||
| Private HMO | 0.8 (0.7, 1.0) | ||
| Medicare HMO | 1.0 (0.9, 1.1) | ||
| Self-purchased Medigap insurance coverage | - | ||
| Employee sponsored insurance | 1.0 (0.9, 1.1) | ||
| No supplemental coverage | 1.4 (1.3, 1.6) | ||
| Medicare entitled due to disability | 1.1 (0.8, 1.5) | ||
| Medicaid | 0.9 (0.8, 1.0) | ||
| Previous hip fracture | 1.0 (0.9, 1.2) | 1.1 (0.9, 1.2) | |
| Never smoked | - | ||
| Ever smoked | 1.2 (1.1, 1.3) | ||
| Smoke now | 1.6 (1.4, 1.8) | ||
| Excellent health | - | - | |
| Good health | 1.3 (1.1, 1.6) | 1.4 (1.2, 1.6) | |
| Fair/poor/missing health | 1.9 (1.6, 2.9) | 2.0 (1.7, 2.4) | |
| No IADL limitations | - | - | |
| Low IADL | 1.3 (1.2, 1.5) | 1.3 (1.2, 1.5) | |
| Medium IADL | 1.5 (1.3, 1.7) | 1.5 (1.3, 1.8) | |
| High IADL | 1.6 (1.4, 1.9) | 1.7 (1.4, 2.0) | |
| Very high IADL | 2.0 (1.8, 2.4) | 2.2 (1.9, 2.5) | |
| No ADL limitations | - | - | |
| Low ADL | 1.5 (1.3, 1.7) | 1.5 (1.3, 1.7) | |
| Medium ADL | 1.5 (1.3, 1.8) | 1.5 (1.3, 1.8) | |
| High ADL | 1.5 (1.3, 1.8) | 1.5 (1.3, 1.8) | |
| Very high ADL | 2.0 (1.8, 2.4) | 2.1 (1.8, 2.4) | |
| Low BMI | 1.6 (1.4, 1.8) | 1.6 (1.4, 1.8) | |
| Normal BMI | - | - | |
| High BMI | 0.8 (0.7, 0.9) | 0.7 (0.7, 0.8) | |
| Married | 0.8 (0.7, 0.9) | ||
| Income<$15,000/yr | - | ||
| Income $15–30,000/yr | 1.0 (0.9, 1.1) | ||
| Income $30–45,000/yr | 1.0 (0.8, 1.1) | ||
| Income >$45,000/yr | 0.9 (0.7, 1.0) | ||
| Income missing | 0.5 (0.3, 1.0) | ||
| < HS education | - | ||
| HS education | 1.1 (1.0, 1.2) | ||
| Some college | 1.0 (0.9, 1.2) | ||
| College | 1.1 (1.0, 1.3) | ||
| Missing education | 1.2 (1.0, 1.4) | ||
| Lives alone | 0.8 (0.7, 0.9) | ||
| Lives in facility | 1.3 (1.2, 1.5) | 1.7 (1.5, 1.9) | |
| Parkinson’s disease | 1.1 (0.9, 1.4) | 1.1 (0.9, 1.3) | |
| History* of stroke | 1.2 (1.1, 1.3) | 1.2 (1.1, 1.3) | |
| History of arthritis | 1.0 (0.8, 1.1) | 1.0 (0.8, 1.1) | |
| History of osteoporosis | 0.9 (0.8, 1.0) | 1.0 (0.8, 1.0) | |
| Vision limitations | 1.0 (0.9, 1.1) | 1.0 (0.9, 1.1) | |
| History of diabetes** | 1.3 (1.2, 1.4) | 1.3 (1.2, 1.4) | |
| History of dementia | 1.2 (1.1, 1.4) | 1.2 (1.1, 1.4) | |
| Solid tumors | 2.1 (1.9, 2.4) | 2.0 (1.8, 2.3) | |
| Lymphomas | 3.2 (2.4, 4.4) | 3.3 (2.4, 4.4) | |
| Chronic pulmonary disease | 1.3 (1.2, 1.5) | 1.3 (1.2, 1.5) | |
| Coronary artery disease | 0.9 (0.8, 1.1) | 0.9 (0.8, 1.0) | |
| Congestive heart failure | 2.0 (1.7, 2.2) | 1.9 (1.7, 2.1) | |
| Peripheral vascular disease | 1.2 (1.0, 1.4) | 1.2 (1.0, 1.4) | |
| Severe chronic liver disease | 2.2 (1.3, 3.6) | 2.1(1.3, 3.5) | |
| Chronic renal failure | 1.9 (1.6, 2.4) | 1.9 (1.5, 2.3) | |
| Nutritional deficiency | 2.1 (1.7, 2.5) | 2.1 (1.7, 2.5) | |
| Functional impairment | 1.0 (0.8, 1.2) | 0.9 (0.7, 1.2) | |
| Schizophrenia | 1.4 (0.9, 2.3) | 1.4 (0.9, 2.3) |
Models include all variables for which a hazard ratio is shown.
Early mortality hazard ratio is that associated with incident hip fracture; the late mortality hazard ratio reported in the text combines the hazard for incident hip fracture with that for those who are six or more months from hip fracture.
“History of” in a comorbidity variable indicates that information came from self-reported MCBS data.
Diabetes is indicated as present if either identified using Iezzoni codes or in the MCBS based on participant self-report of “history of diabetes.”
References
- 1.Melton LJ., III Adverse outcomes of osteoporotic fractures in the general population. J Bone Miner Res. 2003;18:1139–1141. doi: 10.1359/jbmr.2003.18.6.1139. [DOI] [PubMed] [Google Scholar]
- 2.Vanness D, Tosteson A. Estimating the opportunity costs of osteoporosis in the United States. Topics Geriatric Rehab. 2005;21:4–16. [Google Scholar]
- 3.Office of the Surgeon General. Bone Health and Osteoporosis: A report of the Surgeon General. U.S. Department of Health and Human Services; Rockville, MD: 2004. [PubMed] [Google Scholar]
- 4.Kanis JA, Borgstrom F, Zethraeus N, Johnell O, Oden A, Jonsson B. Intervention thresholds for osteoporosis in the UK. Bone. 2005;36:22–32. doi: 10.1016/j.bone.2004.08.018. [DOI] [PubMed] [Google Scholar]
- 5.Kanis JA, Johnell O, Oden A, Borgstrom F, Johansson H, De Laet C, Jonsson B. Intervention thresholds for osteoporosis in men and women: a study based on data from Sweden. Osteoporos Int. 2005;16:6–14. doi: 10.1007/s00198-004-1623-4. [DOI] [PubMed] [Google Scholar]
- 6.Tosteson AN, Jonsson B, Grima DT, O’Brien BJ, Black DM, Adachi JD. Challenges for model-based economic evaluations of postmenopausal osteoporosis interventions. Osteoporos Int. 2001;12:849–857. doi: 10.1007/s001980170036. [DOI] [PubMed] [Google Scholar]
- 7.Melton LJ, 3rd, Therneau TM, Larson DR. Long-term trends in hip fracture prevalence: the influence of hip fracture incidence and survival. Osteoporos Int. 1998;8:68–74. doi: 10.1007/s001980050050. [DOI] [PubMed] [Google Scholar]
- 8.Magaziner J, Lydick E, Hawkes W, Fox KM, Zimmerman SI, Epstein RS, Hebel JR. Excess mortality attributable to hip fracture in white women aged 70 years and older. Am J Public Health. 1997;87:1630–1636. doi: 10.2105/ajph.87.10.1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wolinsky FD, Fitzgerald JF, Stump TE. The effect of hip fracture on mortality, hospitalization, and functional status: a prospective study. Am J Public Health. 1997;87:398–403. doi: 10.2105/ajph.87.3.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kanis JA, Oden A, Johnell O, De Laet C, Jonsson B, Oglesby AK. The components of excess mortality after hip fracture. Bone. 2003;32:468–473. doi: 10.1016/s8756-3282(03)00061-9. [DOI] [PubMed] [Google Scholar]
- 11.Johnell O, Kanis JA. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int. 2004;15:897–902. doi: 10.1007/s00198-004-1627-0. [DOI] [PubMed] [Google Scholar]
- 12.Empana JP, Dargent-Molina P, Breart G. Effect of hip fracture on mortality in elderly women: the EPIDOS prospective study. J Am Geriatr Soc. 2004;52:685–690. doi: 10.1111/j.1532-5415.2004.52203.x. [DOI] [PubMed] [Google Scholar]
- 13.Richmond J, Aharonoff GB, Zuckerman JD, Koval KJ. Mortality risk after hip fracture. J Orthop Trauma. 2003;17:53–56. doi: 10.1097/00005131-200301000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Cauley JA, Thompson DE, Ensrud KC, Scott JC, Black D. Risk of mortality following clinical fractures. Osteoporos Int. 2000;11:556–561. doi: 10.1007/s001980070075. [DOI] [PubMed] [Google Scholar]
- 15.Forsen L, Sogaard AJ, Meyer HE, Edna T, Kopjar B. Survival after hip fracture: short- and long-term excess mortality according to age and gender. Osteoporos Int. 1999;10:73–78. doi: 10.1007/s001980050197. [DOI] [PubMed] [Google Scholar]
- 16.Zuckerman JD. Hip fracture. N Engl J Med. 1996;334:1519–1525. doi: 10.1056/NEJM199606063342307. [DOI] [PubMed] [Google Scholar]
- 17.Johnell O, Kanis JA, Oden A, Sernbo I, Redlund-Johnell I, Petterson C, De Laet C, Jonsson B. Mortality after osteoporotic fractures. Osteoporos Int. 2004;15:38–42. doi: 10.1007/s00198-003-1490-4. [DOI] [PubMed] [Google Scholar]
- 18.Browner WS, Pressman AR, Nevitt MC, Cummings SR. Mortality following fractures in older women. The study of osteoporotic fractures. Arch Intern Med. 1996;156:1521–1525. [PubMed] [Google Scholar]
- 19.Poor G, Atkinson EJ, O’Fallon WM, Melton LJ., 3rd Determinants of reduced survival following hip fractures in men. Clin Orthop Relat Res. 1995:260–265. [PubMed] [Google Scholar]
- 20.Services CfMaM (2006) Medicare Current Beneficiary Survey (MCBS). In.
- 21.Kautter J, Khatutsky G, Pope GC, Chromy JR, Adler GS. Impact of nonresponse on Medicare Current Beneficiary Survey estimates. Health Care Financ Rev. 2006;27:71–93. [PMC free article] [PubMed] [Google Scholar]
- 22.Adler GS. A profile of the Medicare Current Beneficiary Survey. Health Care Financ Rev. 1994;15:153–163. [PMC free article] [PubMed] [Google Scholar]
- 23.Iezzoni LI, Shwartz M, Moskowitz MA, Ash AS, Sawitz E, Burnside S. Illness severity and costs of admissions at teaching and nonteaching hospitals. Jama. 1990;264:1426–1431. [PubMed] [Google Scholar]
- 24.Center for Medicare and Medicaid Services. Medicare Current Beneficiary Survey (MCBS) 2007 http://www.cms.hhs.gov/MCBS/
- 25.Benichou J. A review of adjusted estimators of attributable risk. Stat Methods Med Res. 2001;10:195–216. doi: 10.1177/096228020101000303. [DOI] [PubMed] [Google Scholar]
- 26.Melton LJ, 3rd, Crowson CS, O’Fallon WM. Fracture incidence in Olmsted County, Minnesota: comparison of urban with rural rates and changes in urban rates over time. Osteoporos Int. 1999;9:29–37. doi: 10.1007/s001980050113. [DOI] [PubMed] [Google Scholar]
- 27.Arias E. In National vital statistics reports. National Center for Health Statistics; Hyattsville, MD: 2004. United States life tables, 2001. [PubMed] [Google Scholar]
- 28.Miller CW. Survival and ambulation following hip fracture. J Bone Joint Surg Am. 1978;60:930–934. [PubMed] [Google Scholar]
- 29.Dahl E. Mortality and life expectancy after hip fractures. Acta Orthop Scand. 1980;51:163–170. doi: 10.3109/17453678008990781. [DOI] [PubMed] [Google Scholar]
- 30.Kreutzfeldt J, Haim M, Bach E. Hip fracture among the elderly in a mixed urban and rural population. Age Ageing. 1984;13:111–119. doi: 10.1093/ageing/13.2.111. [DOI] [PubMed] [Google Scholar]
- 31.Farahmand BY, Michaelsson K, Ahlbom A, Ljunghall S, Baron JA. Survival after hip fracture. Osteoporos Int. 2005;16:1583–1590. doi: 10.1007/s00198-005-2024-z. [DOI] [PubMed] [Google Scholar]
- 32.Trombetti A, Herrmann F, Hoffmeyer P, Schurch MA, Bonjour JP, Rizzoli R. Survival and potential years of life lost after hip fracture in men and age-matched women. Osteoporos Int. 2002;13:731–737. doi: 10.1007/s001980200100. [DOI] [PubMed] [Google Scholar]
- 33.Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999;353:878–882. doi: 10.1016/S0140-6736(98)09075-8. [DOI] [PubMed] [Google Scholar]
- 34.Meyer HE, Tverdal A, Falch JA, Pedersen JI. Factors associated with mortality after hip fracture. Osteoporos Int. 2000;11:228–232. doi: 10.1007/s001980050285. [DOI] [PubMed] [Google Scholar]
- 35.Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: is delay before surgery important? J Bone Joint Surg Am. 2005;87:483–489. doi: 10.2106/JBJS.D.01796. [DOI] [PubMed] [Google Scholar]
- 36.Weller I, Wai EK, Jaglal S, Kreder HJ. The effect of hospital type and surgical delay on mortality after surgery for hip fracture. J Bone Joint Surg Br. 2005;87:361–366. doi: 10.1302/0301-620x.87b3.15300. [DOI] [PubMed] [Google Scholar]
- 37.Orosz GM, Magaziner J, Hannan EL, Morrison RS, Koval K, Gilbert M, McLaughlin M, Halm EA, Wang JJ, Litke A, Silberzweig SB, Siu AL. Association of timing of surgery for hip fracture and patient outcomes. JAMA. 2004;291:1738–1743. doi: 10.1001/jama.291.14.1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cornwall R, Gilbert MS, Koval KJ, Strauss E, Siu AL. Functional outcomes and mortality vary among different types of hip fractures: a function of patient characteristics. Clin Orthop Relat Res. 2004:64–71. doi: 10.1097/01.blo.0000132406.37763.b3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jensen JS, Tondevold E. Mortality after hip fractures. Acta Orthop Scand. 1979;50:161–167. doi: 10.3109/17453677908989751. [DOI] [PubMed] [Google Scholar]
- 40.Fransen M, Woodward M, Norton R, Robinson E, Butler M, Campbell AJ. Excess mortality or institutionalization after hip fracture: men are at greater risk than women. J Am Geriatr Soc. 2002;50:685–690. doi: 10.1046/j.1532-5415.2002.50163.x. [DOI] [PubMed] [Google Scholar]
- 41.Wehren LE, Hawkes WG, Orwig DL, Hebel JR, Zimmerman SI, Magaziner J. Gender differences in mortality after hip fracture: the role of infection. J Bone Miner Res. 2003;18:2231–2237. doi: 10.1359/jbmr.2003.18.12.2231. [DOI] [PubMed] [Google Scholar]
- 42.Jacobsen SJ, Goldberg J, Miles TP, Brody JA, Stiers W, Rimm AA. Race and sex differences in mortality following fracture of the hip. Am J Public Health. 1992;82:1147–1150. doi: 10.2105/ajph.82.8.1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Robbins JA, Biggs ML, Cauley J. Adjusted mortality after hip fracture: From the cardiovascular health study. J Am Geriatr Soc. 2006;54:1885–1891. doi: 10.1111/j.1532-5415.2006.00985.x. [DOI] [PubMed] [Google Scholar]
- 44.Fisher ES, Baron JA, Malenka DJ, Barrett JA, Kniffin WD, Whaley FS, Bubolz TA. Hip fracture incidence and mortality in New England. Epidemiology. 1991;2:116–122. doi: 10.1097/00001648-199103000-00005. [DOI] [PubMed] [Google Scholar]