Abstract
Orbital solitary fibrous tumor (SFT) is a rare tumor originating from the mesenchyme. We describe the clinical presentations, radiological and operative findings, and pathological features of a patient with orbital SFT. The patient was a 46-year-old female who presented with progressive proptosis advanced for 20 months. On ophthalmological examination, no visual impairment was detected, but left eye was found to be obviously protruded on exophthalmometry. Orbital magnetic resonance imaging showed a 2.5 × 2 × 2 cm, intensely enhanced mass in the left orbit, which compressed the eyeball forward and the optic nerve downward. The patient underwent frontal craniotomy with superior orbitotomy and gross total resection was performed for the tumor. The histopathological diagnosis including immunohistochemistry was a SFT. After the surgery, proptosis was markedly relieved without visual impairment. Although orbital SFT is extremely rare, it should be considered in the differential diagnosis of orbital tumors. Clinical presentations such as painless proptosis and CD34 immunoreactivity play a significant role in differentiating orbital SFT from other spindle-cell neoplasms of the orbit.
Keywords: Orbital, Solitary fibrous tumor, Mesenchymal origin tumor, CD34
INTRODUCTION
Solitary fibrous tumor (SFT) is a rare spindle-cell tumor of mesenchymal origin that arises most often in the pleura, but may also occur at other organs, including lung, mediastinum, pericardium, peritoneum, retroperitoneal space, pelvis, adrenal gland, kidney, liver, periosteum, salivary gland, thyroid gland, lacrimal gland, breast, nasopharynx, orbit, urogenital system, skin, meninges and spinal cord3,10,11,13,14,19,21,24,27,33). Since the first report of orbital SFT by Westra et al.34) in 1994, fewer than 60 cases of orbital SFTs have been reported to date. Orbital SFT has possibly been underdiagnosed in the past, because of its rarity in extrapleural organs and histological similarity to other spindle cell tumors. Currently, with the development of immunohistochemical method, the number of reported cases have been increasing9). One of the most common symptoms is unilateral painless proptosis, which can be accompanied by visual disturbance, palpable orbital mass, ocular mobility disturbance, hyperglobus or blepharoptosis from the secondary mass effect in the orbit24). As a general rule, orbital SFT shows an indolent and nonaggressive clinical course. It is known that a complete cure can be achieved with gross total resection2,15,17).
CASE REPORT
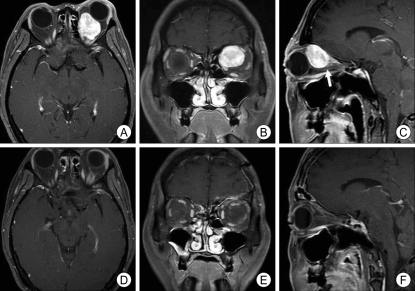
A 46-year-old female presented with a 20 months history of progressive proptosis. On ophthalmologic examination, normal visual acuity, normal visual field and full range of extraocular movement were present. On fundoscopy, there were no findings indicating optic nerve atrophy or papilledema. On exophthalmometry, the exophthalmos of the left eye was measured as 18 mm. Orbital computed tomography (CT) scan showed a 2.5 × 2 × 2 cm sized well-demarcated left extraconal superomedial orbital mass (Fig. 1). No evidence of calcification or bony destruction was observed. Orbital magnetic resonance images (MRI) showed a mass located in the upper and medial quadrant of the left orbit with low signal intensity on T1-weighted images and mixed signal intensity on T2-weighted images, which was enhanced strongly with gadolinium (Fig. 2). The mass was compressing the eyeball forward and the optic nerve downward. The patient underwent left frontal craniotomy with superior orbitotomy under cerebrospinal fluid lumbar drainage. Opening periorbita exposed fat tissue, which was carefully dissected laterally and levator palphebrae muscle underneath was retracted away from the midline. Then, a well demarcated solid mass was identified occupying the left orbit superoposteriorly. The mass was located within a clear dissecting plane isolated from the underlying extraocular muscles with no evidence of local invasion. It was too hard to be grinded with an ultrasonic aspirator. Instead, we removed it with piecemeal fashion using a knife on a step-by-step basis until gross total resection was obtained. After the removal of the mass gross totally, we checked extraocular muscles, optic nerve and ophthalmic artery undamaged, and the surgical procedure was finished after suturing periorbita. Pathological examination disclosed a spindle-cell tumor in a dense fibrous tissue. Immunohistochemical stains of the tumor demonstrated a positive staining for vimentin and CD34 but negative for smooth muscle actin (SMA), cytokeratin and S-100 protein (Fig. 3). With these data, it was finally diagnosed as a SFT. After the surgery, proptosis was completely relieved with visual acuity and the function of all extraocular muscles remained intact. Three months after surgery, there was no enhanced mass on orbital MRI (Fig. 2).
Fig. 1.
Orbital computed tomography (CT) scan showing 25 × 20 × 20 mm sized well-demarcated extraconal superomedial orbital mass. A : Precontrast CT scan. B : Postcontrast CT scan showing intensely enhancing mass.
Fig. 2.
A, B and C : Preoperative orbital magnetic resonance image (MRI) show that optic nerve (white arrow at C) are compressed and downward displaced by strong enhancing mass located in the upper and medial quadrant of the left orbit. D, E and F : On MRI performed 3 months later, removal state of left retrobulbar mass and relieved state of proptosis of the left eyeball were seen.
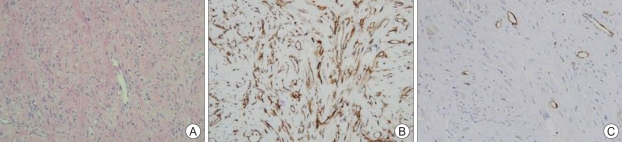
Fig. 3.
A : Spindle cell tumor with a characteristic cracking artifact between cells and collagen (H & E, ×200). B : Strong and diffuse positivity to CD34 (×200). C : Negativity to smooth muscle actin (×200).
DISCUSSION
Patient suffering orbital SFT presents usually with unilateral proptosis and a strongly enhancing, well-circumscribed mass on MRI. Other orbital neoplasms, such as fibrous histiocytoma, nerve sheath meningioma, schwannoma and hemangiopericytoma, share a similar clinical presentation. Furthermore, spindle-cell tumors in orbit have microscopic resemblance to SFT which exhibit focal hemangiopericytoma-like staghorn, fibrous histiocytoma-like storiform pattern, synovial sarcomatous and neural-like palisading regional architecture1). For these reasons, it is possible that former orbital SFT have been misdiagnosed. Recently, however, advanced immunohistochemical techniques have facilitated a clear distinction.
On immunohistochemical findings, SFT has the strong and diffuse positivity to CD34, vimentin and BCL2, and negativity to desmin, cytokeratin, factor VIII related antigen, S-100 protein, muscle specific actin and SMA8,10,15,29). Smooth muscle tumors such as leiomyoma and leiomyosarcoma, on the other hand, show the positivity to actin and desmin, and negativity to CD34 and BCL2. Neural tumors such as schwannoma and neurofibroma show focal positivity to BCL2 and CD34, and strong positivity to S-100 protein22,29).
Strong and consistent CD34 immunoreactivity in SFT can be the important clue for histopathological distinction from other spindle shaped cell tumors, such as meningioma, fibrous histiocytoma, schwannoma and hemangiopericytoma2,8,10,12,15,18). Of these tumors, a differential diagnosis to hemangiopericytoma with SFT is mandatory because hemangiopericytoma has malignant clinical course with recurrence rate of 83%, rate of distant metastasis of 27%, mortality rate of 22%, as opposed to general benign nature of SFT4,31). The hemangiopericytoma is typically composed of small, oval to slightly spindle shaped cells, and it also has a lot of branching, thin-walled vessels of varying caliber and "staghorn" vascular pattern. Immunohistochemical analysis of hemangiopericytoma reveals strong positivity to vimentin, factor XIIIa and Leu-7, and weak positivity to desmin and cytokeratin which are similar characteristics sharing with SFT. However, SFT shows strong positivity to CD34, while hemangiopericytoma shows weak positivity25,30).
Orbital SFT often has some analogy with optic nerve sheath meningioma on the radiologic findings, for which a differential diagnosis is important clinically. In cases of SFT, there are no findings such as psammoma body, whorl formation of tumor cells or amorphous calcification, which are commonly found in meningiomas. Besides, in meningioma, focal staining to BCL2 or CD34, and intense staining to cytokeratin were observed25,28-30). On symptomatology, optic nerve sheath meningioma, as it gradually increases in size, usually causes a disturbance in the blood flow to the adjacent area of the optic nerve23). For this reason, visual symptoms and signs including impairment of visual field and acuity, disturbance in color vision and development of diplopia tend to occur earlier than proptosis. The majority of patients with orbital SFT, however, present with unilateral painless proptosis as the initial clinical feature because of the mass effect compressing both eyeball and optic nerve.
The probability of local recurrence related to incomplete resection has led surgical en bloc removal to be recommended as the treatment of choice in SFT2,5,13,14,21,24,27). No previous studies have demonstrated the effect of chemotherapy or radiotherapy6,7,26). The possibility for malignant transformation is closely associated with histologic features2). The findings, such as nuclear atypia, increased cellularity, necrosis and greater than 4 mitoses/10 high-power fields, are suggestions of the malignant potential of SFT32). The prognosis in SFT, however, most likely depends upon complete resection rather than histologic findings because the clinical behavior of SFT is not in agreement with the histologic prognostic factors in all cases16,20,24).
The most frequent clinical presentation of orbital SFT is unilateral painless proptosis, which led the ophthalmologists to report most of the cases so far. In majority, orbital SFT originated from lacrimal glands according to the previous reports, in which orbitotomy alone could give successful surgical results17,21,24,26,35). But, SFT arising from mesenchymal orbital connective tissue could have its location within the retro-orbital space where frontal craniotomy with superior orbitotomy is essential like what is performed to remove optic nerve sheath meningioma.
CONCLUSION
We experienced a rare case of orbital SFT. Although extremely rare, orbital SFT should be included in the differential diagnosis of a well-circumscribed and intensely enhancing orbital mass on MRI. Clinical presentation such as painless proptosis and CD34 immunoreactivity play a significant role in differentiating orbital SFT from other spindle-cell neoplasms of the orbit.
References
- 1.Ali SZ, Hoon V, Hoda S, Heelan R, Zakowski MF. Solitary fibrous tumor. A cytologic-histologic study with clinical, radiologic, and immunohistochemical correlations. Cancer. 1997;81:116–121. doi: 10.1002/(sici)1097-0142(19970425)81:2<116::aid-cncr5>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 2.Bernardini FP, de Conciliis C, Schneider S, Kersten RC, Kulwin DR. Solitary fibrous tumor of the orbit : is it rare? Report of a case series and review of the literature. Ophthalmology. 2003;110:1442–1448. doi: 10.1016/S0161-6420(03)00459-7. [DOI] [PubMed] [Google Scholar]
- 3.Brunnemann RB, Ro JY, Ordonez NG, Mooney J, El-Naggar AK, Ayala AG. Extrapleural solitary fibrous tumor : a clinicopathologic study of 24 cases. Mod Pathol. 1999;12:1034–1042. [PubMed] [Google Scholar]
- 4.Carneiro SS, Scheithauer BW, Nascimento AG, Hirose T, Davis DH. Solitary fibrous tumor of the meninges : a lesion distinct from fibrous meningioma. A clinicopathologic and immunohistochemical study. Am J Clin Pathol. 1996;106:217–224. doi: 10.1093/ajcp/106.2.217. [DOI] [PubMed] [Google Scholar]
- 5.Cassarino DS, Auerbach A, Rushing EJ. Widely invasive solitary fibrous tumor of the sphenoid sinus, cavernous sinus, and pituitary fossa. Ann Diagn Pathol. 2003;7:169–173. doi: 10.1016/s1092-9134(03)00016-9. [DOI] [PubMed] [Google Scholar]
- 6.Clayton AC, Salomäo DR, Keeney GL, Nascimento AG. Solitary fibrous tumor : a study of cytologic features of six cases diagnosed by fine-needle aspiration. Diagn Cytopathol. 2001;25:172–176. doi: 10.1002/dc.2032. [DOI] [PubMed] [Google Scholar]
- 7.Dietrich CG, Roeb E, Breuer E, Matern S. [Solitary fibrous thoracic wall tumor. Progression with percutaneous radiotherapy] Dtsch Med Wochenschr. 2001;126:12–15. doi: 10.1055/s-2001-9884. [DOI] [PubMed] [Google Scholar]
- 8.England DM, Hochholzer L, McCarthy MJ. Localized benign and malignant fibrous tumors of the pleura. A clinicopathologic review of 223 cases. Am J Surg Pathol. 1989;13:640–658. doi: 10.1097/00000478-198908000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Festa S, Lee HJ, Langer P, Klein KM. Solitary fibrous tumor of the orbit : CT and pathologic correlation. Neuroradiology. 1999;41:52–54. doi: 10.1007/s002340050705. [DOI] [PubMed] [Google Scholar]
- 10.Fukunaga M, Ushigome S, Nomura K, Ishikawa E. Solitary fibrous tumor of the nasal cavity and orbit. Pathol Int. 1995;45:952–957. doi: 10.1111/j.1440-1827.1995.tb03421.x. [DOI] [PubMed] [Google Scholar]
- 11.Galié M, Tieghi R, Cavazzini L, Clauser L. Solitary fibrous tumor of the orbit : a case report. Int J Oral Maxillofac Surg. 2005;34:331–333. doi: 10.1016/j.ijom.2004.05.011. [DOI] [PubMed] [Google Scholar]
- 12.Giuffre I, Faiola A, Bonanno E, Liccardo G. Solitary fibrous tumor of the orbit. Case report and review of the literature. Surg Neurol. 2001;56:242–246. doi: 10.1016/s0090-3019(01)00597-3. [DOI] [PubMed] [Google Scholar]
- 13.Glazer-Hockstein C, Syed NA, Warhol M, Gausas RE. Malignant solitary fibrous tumor metastatic to the orbit. Ophthal Plast Reconstr Surg. 2004;20:471–473. doi: 10.1097/01.iop.0000144786.56696.98. [DOI] [PubMed] [Google Scholar]
- 14.Hayashi S, Kurihara H, Hirato J, Sasaki T. Solitary fibrous tumor of the orbit with extraorbital extension : case report. Neurosurgery. 2001;49:1241–1245. doi: 10.1097/00006123-200111000-00042. [DOI] [PubMed] [Google Scholar]
- 15.Heathcote JG. Pathology update : solitary fibrous tumour of the orbit. Can J Ophthalmol. 1997;32:432–435. [PubMed] [Google Scholar]
- 16.Jang JW, Kim CH, Yoo CW, Moon JG. Intracranial solitary fibrous tumor. J Korean Neurosurg Soc. 2006;39:64–67. [Google Scholar]
- 17.Kim HY, Lee SY, Kang SJ, Kim HJ. Solitary fibrous tumor of the orbit : a poorly-recognized orbital lesion. Acta Ophthalmol Scand. 1999;77:704–708. doi: 10.1034/j.1600-0420.1999.770621.x. [DOI] [PubMed] [Google Scholar]
- 18.Krishnakumar S, Subramanian N, Mohan ER, Mahesh L, Biswas J, Rao NA. Solitary fibrous tumor of the orbit : a clinicopathologic study of six cases with review of the literature. Surv Ophthalmol. 2003;48:544–554. doi: 10.1016/s0039-6257(03)00087-0. [DOI] [PubMed] [Google Scholar]
- 19.Lucci LM, Anderson RL, Harrie RP, Mamalis N, Coffin C, Crandall DC. Solitary fibrous tumor of the orbit in a child. Ophthal Plast Reconstr Surg. 2001;17:369–373. doi: 10.1097/00002341-200109000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Martin AJ, Fisher C, Igbaseimokumo U, Jarosz JM, Dean AF. Solitary fibrous tumours of the meninges : case series and literature review. J Neurooncol. 2001;54:57–69. doi: 10.1023/a:1012553119349. [DOI] [PubMed] [Google Scholar]
- 21.Meyer D, Riley F. Solitary fibrous tumor of the orbit : a clinicopathologic entity that warrants both a heightened awareness and an atraumatic surgical removal technique. Orbit. 2006;25:45–50. doi: 10.1080/01676830500506101. [DOI] [PubMed] [Google Scholar]
- 22.Miettinen M, Shekitka KM, Sobin LH. Schwannomas in the colon and rectum : a clinicopathologic and immunohistochemical study of 20 cases. Am J Surg Pathol. 2001;25:846–855. doi: 10.1097/00000478-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Miller NR. New concepts in the diagnosis and management of optic nerve sheath meningioma. J Neuroophthalmol. 2006;26:200–208. doi: 10.1097/01.wno.0000235569.19131.ac. [DOI] [PubMed] [Google Scholar]
- 24.O'Donovan DA, Bilbao JM, Fazl M, Antonyshyn OM. Solitary fibrous tumor of the orbit. J Craniofac Surg. 2002;13:641–644. doi: 10.1097/00001665-200209000-00009. [DOI] [PubMed] [Google Scholar]
- 25.Perry A, Scheithauer BW, Nascimento AG. The immunophenotypic spectrum of meningeal hemangiopericytoma : a comparison with fibrous meningioma and solitary fibrous tumor of meninges. Am J Surg Pathol. 1997;21:1354–1360. doi: 10.1097/00000478-199711000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Polito E, Tosi M, Toti P, Schurfeld K, Caporossi A. Orbital solitary fibrous tumor with aggressive behaviorThree cases and review of the literature. Graefes Arch Clin Exp Ophthalmol. 2002;240:570–574. doi: 10.1007/s00417-002-0486-7. [DOI] [PubMed] [Google Scholar]
- 27.Romer M, Bode B, Schüknecht B, Schmid S, Holzmann D. Solitary fibrous tumor of the orbit--two cases and a review of the literature. Eur Arch Otorhinolaryngol. 2005;262:81–88. doi: 10.1007/s00405-003-0731-7. [DOI] [PubMed] [Google Scholar]
- 28.Rosenberg AE, O'Connell JX, Dickersin GR, Bhan AK. Expression of epithelial markers in malignant fibrous histiocytoma of the musculoskeletal system : an immunohistochemical and electron microscopic study. Hum Pathol. 1993;24:284–293. doi: 10.1016/0046-8177(93)90039-j. [DOI] [PubMed] [Google Scholar]
- 29.Suster S, Fisher C, Moran CA. Expression of bcl-2 oncoprotein in benign and malignant spindle cell tumors of soft tissue, skin, serosal surfaces, and gastrointestinal tract. Am J Surg Pathol. 1998;22:863–872. doi: 10.1097/00000478-199807000-00008. [DOI] [PubMed] [Google Scholar]
- 30.Suzuki SO, Fukui M, Nishio S, Iwaki T. Clinicopathological features of solitary fibrous tumor of the meninges : an immunohistochemical reappraisal of cases previously diagnosed to be fibrous meningioma or hemangiopericytoma. Pathol Int. 2000;50:808–817. doi: 10.1046/j.1440-1827.2000.01120.x. [DOI] [PubMed] [Google Scholar]
- 31.Tihan T, Viglione M, Rosenblum MK, Olivi A, Burger PC. Solitary fibrous tumors in the central nervous system. A clinicopathologic review of 18 cases and comparison to meningeal hemangiopericytomas. Arch Pathol Lab Med. 2003;127:432–439. doi: 10.5858/2003-127-0432-SFTITC. [DOI] [PubMed] [Google Scholar]
- 32.Vallat-Decouvelaere AV, Dry SM, Fletcher CD. Atypical and malignant solitary fibrous tumors in extrathoracic locations : evidence of their comparability to intra-thoracic tumors. Am J Surg Pathol. 1998;22:1501–1511. doi: 10.1097/00000478-199812000-00007. [DOI] [PubMed] [Google Scholar]
- 33.Warraich I, Dunn DM, Oliver JW. Solitary fibrous tumor of the orbit with epithelioid features. Arch Pathol Lab Med. 2006;130:1039–1041. doi: 10.5858/2006-130-1039-SFTOTO. [DOI] [PubMed] [Google Scholar]
- 34.Westra WH, Gerald WL, Rosai J. Solitary fibrous tumor. Consistent CD34 immunoreactivity and occurrence in the orbit. Am J Surg Pathol. 1994;18:992–998. doi: 10.1097/00000478-199410000-00003. [DOI] [PubMed] [Google Scholar]
- 35.Wright JE, Stewart WB, Krohel GB. Clinical presentation and management of lacrimal gland tumours. Br J Ophthalmol. 1979;63:600–606. doi: 10.1136/bjo.63.9.600. [DOI] [PMC free article] [PubMed] [Google Scholar]